Falls Prevention in Elderly: Translating Evidence into Practice
VerifiedAdded on 2022/10/04
|7
|5869
|17
Report
AI Summary
This report, published in the Hong Kong Med J in 2015, addresses the critical issue of falls prevention in the elderly, emphasizing the importance of translating evidence into practice. It highlights the prevalence of falls in the elderly population and the common pitfall of treating injuries without addressing the underlying causes. The report advocates for a proactive approach, including risk factor identification using mnemonics, and fall assessment through history-taking and tests like the timed up-and-go test. Evidence-based interventions such as multi-component exercises, Tai Chi, environmental modifications, medication review, vitamin D supplementation, and cardiovascular management are discussed. The report also provides practical strategies, including exercise programs, Tai Chi promotion, environmental interventions, medication reviews, and vitamin D supplementation, and stresses the significance of interdisciplinary intervention. The report underscores the importance of addressing the multifaceted nature of fall risk and encourages a holistic approach to improve the quality of life for the elderly population. The document is available on Desklib, a platform that provides AI-based study tools for students.
165Hong Kong Med J⎥ Volume 21 Number 2⎥ April 2015⎥ www.hkmj.org
A B S T R A C T
Falls are a common problem in the elderly. A common
error in their management is that injury from the fall
is treated, without finding its cause. Thus a proactive
approach is important to screen for the likelihood of
fall in the elderly. Fall assessment usually includes a
focused history and a targeted examination. Timed
up-and-go test can be performed quickly and is able
to predict the likelihood of fall. Evidence-based fall
prevention interventions include multi-component
group or home-basedexercises,participationin
Tai Chi, environmental modifications, medication
review, management of foot and footwear problems,
vitamin D supplementation,and managementof
cardiovascularproblems.If possible,these are
best implementedin the form of multifactorial
intervention. Bone health enhancementfor
residentialcare home residentsand appropriate
community patients, and prescription of hip
Falls prevention in the elderly: translati
evidence into practice
Introduction
Falls and imbalance occur commonly in the elderly
and fall/instability is indeed one of the ‘giants’ in
geriatric medicine.1 A fall is often defined as an event
that results in the patient or a body part of the patient
coming to rest inadvertently on the ground or other
surface lower than the body.2 In Hong Kong, the
prevalence in the elderly of having at least one fall in
the preceding 12 months is between 18% and 19.3%,
with 75.2% sustaining injuries and 7.2% having a
serious injury.3,4 Those who fall have significantly
more hospitalisations and clinic visits as well as
accidentand emergencydepartmentvisits than
those who do not. Fear of falling, loss of confidence
in walking, social isolation, and depression can also
occur. Fall is a predictor for decreased functional
state and risk factor for institutionalisation,5 and
the elderly who are prone to falling consume more
health care resources than non-fallers each year.6
Pitfalls in fall management
Despite the potentiallysevereconsequencesof
falls, under-reporting by the elderly is common.7
Individuals may attributefalling to the ageing
process or they may not report falls because of the
fear of being restricted in their activities or being
institutionalised following a fall. Some older people,
especiallythose with cognitiveimpairment,may
Hong Kong Med J 2015;21:165–71
DOI: 10.12809/hkmj144469
James KH Luk *, TY Chan, Daniel KY Chan
1 JKH Luk *, FHKCP, FHKAM (Medicine)
2 TY Chan, FHKCP, FHKAM (Medicine)
3 DKY Chan, MD, FRACP
1 Department of Medicine and Geriatrics, Fung Yiu King Hospital, Hong
Kong
2 Department of Medicine and Geriatrics, Kwong Wah Hospital, Yaumatei,
Hong Kong
3 Faculty of Medicine, University of New South Wales, Ingham Institute;
Aged Care & Rehab, Bankstown Hospital, Australia
* Corresponding author: lukkh@ha.org.hk
This article was
published on 27 Feb
2015 at www.hkmj.org.
forget the event and consequently fail to inform the
health care team. Alternatively, in the absence of a
obvious injury, physicians may be unaware of falls.
A drawback to the management of falls is that
consequences, such as fractures or head injuries, a
treated without finding the cause of the fall. Unless
all the underlying risk factors are addressed, falls a
very likely to recur.
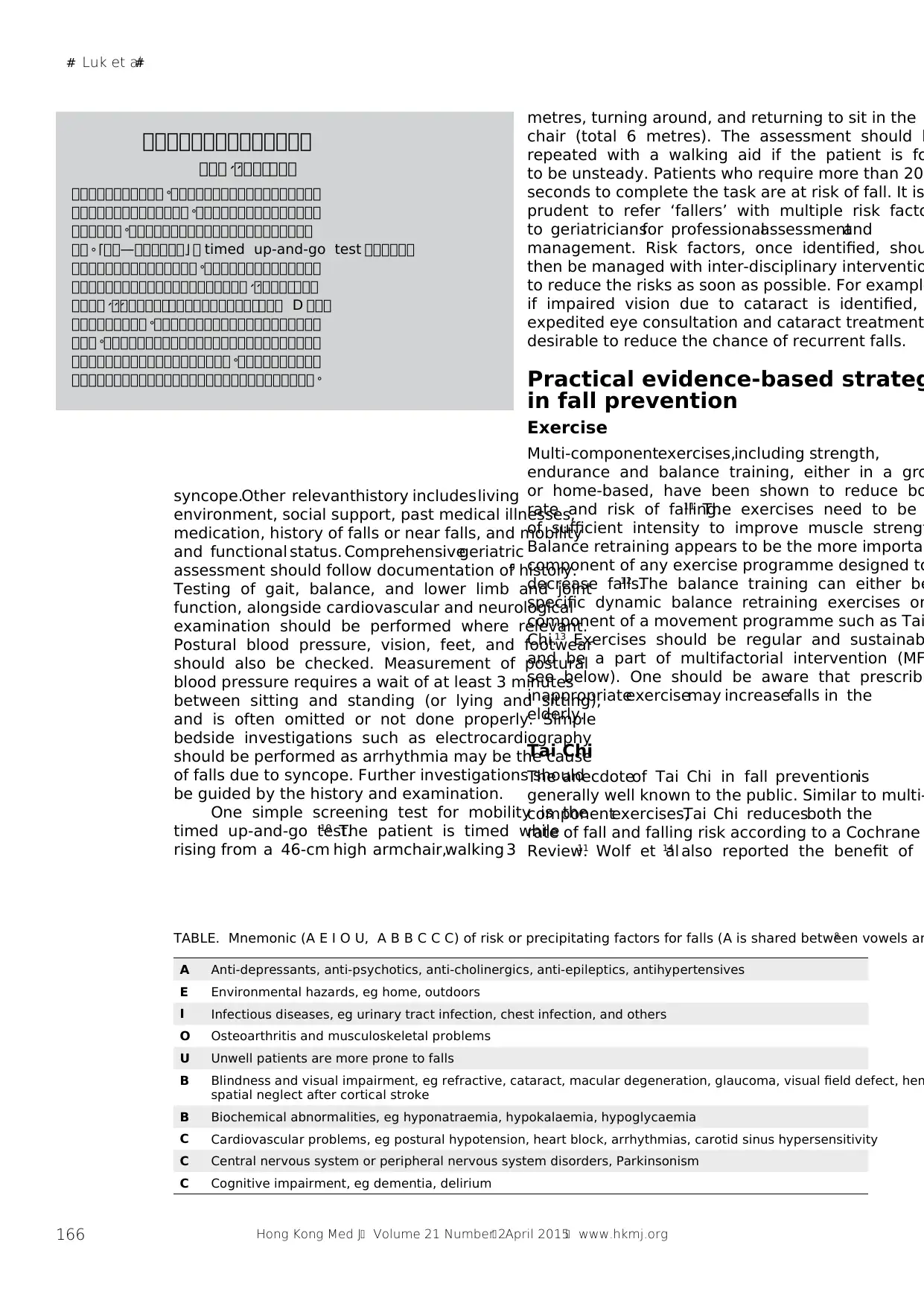
Knowing the risk/precipitating
factors for falls
The first step in fall prevention is to identify th
risk or precipitating factors for falls. Age by its
is an important risk factor, but not the only on
Falls in the elderly are often due to the interaction
of multiple risk factors. One practical way to h
clinicians identify risk or precipitating factors is to
use a mnemonic. One such mnemonic is shown in
the Table.8
Fall assessment
As falls are usually under-reported,a proactive
approach is to ask “Have you had a fall in the past
6 months?”at every encounterwith an elderly
patient. Initial medical assessmentinvolves a
focused history-taking, detailing the circumstances
of fall, precipitating factors, and consequences.
witnesscan be helpful to identify unrecognised
MEDICAL PRACTICECME
protectors for residential care home residents a
also recommended.Multifactorial intervention
may also be useful in a hospitaland residential
care home setting. Use of physical restraints is not
recommended for fall prevention.
A B S T R A C T
Falls are a common problem in the elderly. A common
error in their management is that injury from the fall
is treated, without finding its cause. Thus a proactive
approach is important to screen for the likelihood of
fall in the elderly. Fall assessment usually includes a
focused history and a targeted examination. Timed
up-and-go test can be performed quickly and is able
to predict the likelihood of fall. Evidence-based fall
prevention interventions include multi-component
group or home-basedexercises,participationin
Tai Chi, environmental modifications, medication
review, management of foot and footwear problems,
vitamin D supplementation,and managementof
cardiovascularproblems.If possible,these are
best implementedin the form of multifactorial
intervention. Bone health enhancementfor
residentialcare home residentsand appropriate
community patients, and prescription of hip
Falls prevention in the elderly: translati
evidence into practice
Introduction
Falls and imbalance occur commonly in the elderly
and fall/instability is indeed one of the ‘giants’ in
geriatric medicine.1 A fall is often defined as an event
that results in the patient or a body part of the patient
coming to rest inadvertently on the ground or other
surface lower than the body.2 In Hong Kong, the
prevalence in the elderly of having at least one fall in
the preceding 12 months is between 18% and 19.3%,
with 75.2% sustaining injuries and 7.2% having a
serious injury.3,4 Those who fall have significantly
more hospitalisations and clinic visits as well as
accidentand emergencydepartmentvisits than
those who do not. Fear of falling, loss of confidence
in walking, social isolation, and depression can also
occur. Fall is a predictor for decreased functional
state and risk factor for institutionalisation,5 and
the elderly who are prone to falling consume more
health care resources than non-fallers each year.6
Pitfalls in fall management
Despite the potentiallysevereconsequencesof
falls, under-reporting by the elderly is common.7
Individuals may attributefalling to the ageing
process or they may not report falls because of the
fear of being restricted in their activities or being
institutionalised following a fall. Some older people,
especiallythose with cognitiveimpairment,may
Hong Kong Med J 2015;21:165–71
DOI: 10.12809/hkmj144469
James KH Luk *, TY Chan, Daniel KY Chan
1 JKH Luk *, FHKCP, FHKAM (Medicine)
2 TY Chan, FHKCP, FHKAM (Medicine)
3 DKY Chan, MD, FRACP
1 Department of Medicine and Geriatrics, Fung Yiu King Hospital, Hong
Kong
2 Department of Medicine and Geriatrics, Kwong Wah Hospital, Yaumatei,
Hong Kong
3 Faculty of Medicine, University of New South Wales, Ingham Institute;
Aged Care & Rehab, Bankstown Hospital, Australia
* Corresponding author: lukkh@ha.org.hk
This article was
published on 27 Feb
2015 at www.hkmj.org.
forget the event and consequently fail to inform the
health care team. Alternatively, in the absence of a
obvious injury, physicians may be unaware of falls.
A drawback to the management of falls is that
consequences, such as fractures or head injuries, a
treated without finding the cause of the fall. Unless
all the underlying risk factors are addressed, falls a
very likely to recur.
Knowing the risk/precipitating
factors for falls
The first step in fall prevention is to identify th
risk or precipitating factors for falls. Age by its
is an important risk factor, but not the only on
Falls in the elderly are often due to the interaction
of multiple risk factors. One practical way to h
clinicians identify risk or precipitating factors is to
use a mnemonic. One such mnemonic is shown in
the Table.8
Fall assessment
As falls are usually under-reported,a proactive
approach is to ask “Have you had a fall in the past
6 months?”at every encounterwith an elderly
patient. Initial medical assessmentinvolves a
focused history-taking, detailing the circumstances
of fall, precipitating factors, and consequences.
witnesscan be helpful to identify unrecognised
MEDICAL PRACTICECME
protectors for residential care home residents a
also recommended.Multifactorial intervention
may also be useful in a hospitaland residential
care home setting. Use of physical restraints is not
recommended for fall prevention.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
# Luk et al#
166 Hong Kong Med J⎥ Volume 21 Number 2⎥ April 2015⎥ www.hkmj.org
預預預預預預預預預預預預預預
預預預 預預預預預預預、、
預預預預預預預預預預預 預預預預預預預預預預預預預預預預預預。
預預預預預預預預預預預預預預 預預預預預預預預預預預預預預預。
預預預預預預 預預預預預預預預預預預預預預預預預預預預預預。
預預 預預—預預預預預預 預。「 」 timed up-and-go test 預預預預預預
預預預預預預預預預預預預預預預 預預預預預預預預預預預預預預。
預預預預預預預預預預預預預預預預預預預預預 預預預預預預預預、、
預預預預 預預預預預預預預預預預預預預預預預預預預預、、、 D 預預預
預預預預預預預預預 預預預預預預預預預預預預預預預預預預預預。
預預預 預預預預預預預預預預預預預預預預預預預預預預預預預預。
預預預預預預預預預預預預預預預預預預預 預預預預預預預預預預。
預預預預預預預預預預預預預預預預預預預預預預預預預預預預預。
syncope.Other relevanthistory includes living
environment, social support, past medical illnesses,
medication, history of falls or near falls, and mobility
and functional status. Comprehensivegeriatric
assessment should follow documentation of history.9
Testing of gait, balance, and lower limb and joint
function, alongside cardiovascular and neurological
examination should be performed where relevant.
Postural blood pressure, vision, feet, and footwear
should also be checked. Measurement of postural
blood pressure requires a wait of at least 3 minutes
between sitting and standing (or lying and sitting),
and is often omitted or not done properly. Simple
bedside investigations such as electrocardiography
should be performed as arrhythmia may be the cause
of falls due to syncope. Further investigations should
be guided by the history and examination.
One simple screening test for mobility is the
timed up-and-go test.10 The patient is timed while
rising from a 46-cm high armchair,walking 3
metres, turning around, and returning to sit in the
chair (total 6 metres). The assessment should b
repeated with a walking aid if the patient is fo
to be unsteady. Patients who require more than 20
seconds to complete the task are at risk of fall. It is
prudent to refer ‘fallers’ with multiple risk facto
to geriatriciansfor professionalassessmentand
management. Risk factors, once identified, shou
then be managed with inter-disciplinary interventio
to reduce the risks as soon as possible. For example
if impaired vision due to cataract is identified,
expedited eye consultation and cataract treatment
desirable to reduce the chance of recurrent falls.
Practical evidence-based strateg
in fall prevention
Exercise
Multi-componentexercises,including strength,
endurance and balance training, either in a gro
or home-based, have been shown to reduce bo
rate and risk of falling.11 The exercises need to be
of sufficient intensity to improve muscle strengt
Balance retraining appears to be the more importan
component of any exercise programme designed to
decrease falls.12 The balance training can either be
specific dynamic balance retraining exercises or
component of a movement programme such as Tai
Chi.13 Exercises should be regular and sustainab
and be a part of multifactorial intervention (MF
see below). One should be aware that prescribi
inappropriateexercisemay increasefalls in the
elderly.
Tai Chi
The anecdoteof Tai Chi in fall preventionis
generally well known to the public. Similar to multi-
componentexercises,Tai Chi reducesboth the
rate of fall and falling risk according to a Cochrane
Review.11 Wolf et al14 also reported the benefit of
TABLE. Mnemonic (A E I O U, A B B C C C) of risk or precipitating factors for falls (A is shared between vowels an8
A Anti-depressants, anti-psychotics, anti-cholinergics, anti-epileptics, antihypertensives
E Environmental hazards, eg home, outdoors
I Infectious diseases, eg urinary tract infection, chest infection, and others
O Osteoarthritis and musculoskeletal problems
U Unwell patients are more prone to falls
B Blindness and visual impairment, eg refractive, cataract, macular degeneration, glaucoma, visual field defect, hem
spatial neglect after cortical stroke
B Biochemical abnormalities, eg hyponatraemia, hypokalaemia, hypoglycaemia
C Cardiovascular problems, eg postural hypotension, heart block, arrhythmias, carotid sinus hypersensitivity
C Central nervous system or peripheral nervous system disorders, Parkinsonism
C Cognitive impairment, eg dementia, delirium
166 Hong Kong Med J⎥ Volume 21 Number 2⎥ April 2015⎥ www.hkmj.org
預預預預預預預預預預預預預預
預預預 預預預預預預預、、
預預預預預預預預預預預 預預預預預預預預預預預預預預預預預預。
預預預預預預預預預預預預預預 預預預預預預預預預預預預預預預。
預預預預預預 預預預預預預預預預預預預預預預預預預預預預預。
預預 預預—預預預預預預 預。「 」 timed up-and-go test 預預預預預預
預預預預預預預預預預預預預預預 預預預預預預預預預預預預預預。
預預預預預預預預預預預預預預預預預預預預預 預預預預預預預預、、
預預預預 預預預預預預預預預預預預預預預預預預預預預、、、 D 預預預
預預預預預預預預預 預預預預預預預預預預預預預預預預預預預預。
預預預 預預預預預預預預預預預預預預預預預預預預預預預預預預。
預預預預預預預預預預預預預預預預預預預 預預預預預預預預預預。
預預預預預預預預預預預預預預預預預預預預預預預預預預預預預。
syncope.Other relevanthistory includes living
environment, social support, past medical illnesses,
medication, history of falls or near falls, and mobility
and functional status. Comprehensivegeriatric
assessment should follow documentation of history.9
Testing of gait, balance, and lower limb and joint
function, alongside cardiovascular and neurological
examination should be performed where relevant.
Postural blood pressure, vision, feet, and footwear
should also be checked. Measurement of postural
blood pressure requires a wait of at least 3 minutes
between sitting and standing (or lying and sitting),
and is often omitted or not done properly. Simple
bedside investigations such as electrocardiography
should be performed as arrhythmia may be the cause
of falls due to syncope. Further investigations should
be guided by the history and examination.
One simple screening test for mobility is the
timed up-and-go test.10 The patient is timed while
rising from a 46-cm high armchair,walking 3
metres, turning around, and returning to sit in the
chair (total 6 metres). The assessment should b
repeated with a walking aid if the patient is fo
to be unsteady. Patients who require more than 20
seconds to complete the task are at risk of fall. It is
prudent to refer ‘fallers’ with multiple risk facto
to geriatriciansfor professionalassessmentand
management. Risk factors, once identified, shou
then be managed with inter-disciplinary interventio
to reduce the risks as soon as possible. For example
if impaired vision due to cataract is identified,
expedited eye consultation and cataract treatment
desirable to reduce the chance of recurrent falls.
Practical evidence-based strateg
in fall prevention
Exercise
Multi-componentexercises,including strength,
endurance and balance training, either in a gro
or home-based, have been shown to reduce bo
rate and risk of falling.11 The exercises need to be
of sufficient intensity to improve muscle strengt
Balance retraining appears to be the more importan
component of any exercise programme designed to
decrease falls.12 The balance training can either be
specific dynamic balance retraining exercises or
component of a movement programme such as Tai
Chi.13 Exercises should be regular and sustainab
and be a part of multifactorial intervention (MF
see below). One should be aware that prescribi
inappropriateexercisemay increasefalls in the
elderly.
Tai Chi
The anecdoteof Tai Chi in fall preventionis
generally well known to the public. Similar to multi-
componentexercises,Tai Chi reducesboth the
rate of fall and falling risk according to a Cochrane
Review.11 Wolf et al14 also reported the benefit of
TABLE. Mnemonic (A E I O U, A B B C C C) of risk or precipitating factors for falls (A is shared between vowels an8
A Anti-depressants, anti-psychotics, anti-cholinergics, anti-epileptics, antihypertensives
E Environmental hazards, eg home, outdoors
I Infectious diseases, eg urinary tract infection, chest infection, and others
O Osteoarthritis and musculoskeletal problems
U Unwell patients are more prone to falls
B Blindness and visual impairment, eg refractive, cataract, macular degeneration, glaucoma, visual field defect, hem
spatial neglect after cortical stroke
B Biochemical abnormalities, eg hyponatraemia, hypokalaemia, hypoglycaemia
C Cardiovascular problems, eg postural hypotension, heart block, arrhythmias, carotid sinus hypersensitivity
C Central nervous system or peripheral nervous system disorders, Parkinsonism
C Cognitive impairment, eg dementia, delirium
# Falls prevention in the elderly#
167Hong Kong Med J⎥ Volume 21 Number 2⎥ April 2015⎥ www.hkmj.org
10-form Tai Chi in a randomised controlled trial
(RCT). Tai Chi is a combination of strength and
balance training, with a certain aerobic element.15
In Hong Kong, most people practise the full form
that should theoretically be at least effective, if not
better. This can be promoted as a territory-wide
health recommendation. Nonetheless, not all Tai
Chi programmes improve balance. One local RCT
revealed no difference in the number of falls between
a Tai Chi group and controls after 12 months.16
Environmental interventions
Home modificationscan effectivelyreduce risk
of falls in the community,11 and include removal
of floor mats, painting the edge of steps, reducing
glare,installinghandles,and improvinglighting.
Occupational therapists can provide expert advice
in this area. For older people with fall risk who live
at home, especially those who are usually alone,
installation of a safety alarm is recommended so help
can be summoned should an accident occur.
Medication review
Polypharmacyis common among older people
who often have multiple co-morbidities, and is an
independent variable that has been linked to falls in
older people.17 Many drugs, psychotropic medications
and antihypertensive agents in particular, are related
to falls. The use of psychotropic medication should
be confined to patients who do not respond to non-
pharmacological intervention and the lowest dosage
should be prescribed. Periodic review of indications
and side-effectsshould be undertaken:gradual
withdrawal of psychotropic medication can reduce
rate of falls in community-dwelling elderly people.11
Nonethelessdrug withdrawalis a complicated
interventionthat should be implementedby an
experienced clinician after carefully weighing the
risks and benefits.A standardisedand explicit
medicinereview tool such as the Beers Criteria
for PotentiallyInappropriateMedicationUse in
Older Adults and STOPP (Screening Tool of Older
Person’spotentiallyinappropriatePrescriptions)
may be useful in reducing falls in older people but
the effectiveness of these approaches has not been
proven by RCTs.18,19 Although drug withdrawal
is beneficial, studies that include RCTs show that
many withdrawals (eg sleeping pills) are reversed
and patientsresumeprevioustherapy.Ongoing
monitoring is therefore essential.20
Foot and footwear
Foot and footwear problems are common but are
often ignored.Footwearinfluencesbalanceand
risk of falls. High-heeled shoes have been shown
to increasefalls in older people.Anti-slip shoe
devices effectively reduce outdoor falls in slippery
conditions.21 A systematic review recommends that
elderly individuals wear shoes with a low heel and
firm slip-resistant soles, both inside and outside the
home.22 Podiatrists, and prosthetics and orthotics
professionalscan give valuableadvice in this
respect. A recent RCT has shown that multifaceted
podiatry intervention with foot orthoses, footwear
advice, education, and foot and ankle exercises can
reduce the rate of falls in community-dwelling older
people.23
Vitamin D supplement
The benefit of vitamin D in falls/fractures extends
beyond improvedbone health. Vitamin D can
strengthen muscle and hence reduce falls. Meta-
analysis has shown that supplemental vitamin D at
a dose of 700 IU to 1000 IU a day reduces the risk of
falling among older individuals by 19%.24 The current
opinion is that in community-dwellingelderly,
vitamin D supplementation reduces the rate of falls
or risk of falling in a subgroup of people with low
vitamin D levels but its benefit is absent in people
without deficiency.11 In the institutionalised elderly,
vitamin D supplementationappearsto be more
effective in reducing falls and the recommendation
is to prescribe vitamin D with or without calcium
supplements to older people with low vitamin D
levels or those who are institutionalised.11 Despite
theserecommendations,most studieshave been
conducted in western countries that experience a
quite different duration and intensity of sunshine to
Hong Kong. Whether the benefit of vitamin D in fall
prevention applies equally to Hong Kong Chinese
populationis not known. Most public hospital
laboratories in Hong Kong do not have the means
to investigate vitamin D levels and clinicians are
required to send blood samples to private laboratories
for vitamin D level assay at a cost. Thus in the public
health sector,mass screeningof the elderlyfor
vitamin D deficiency prior to supplementation is
impractical. The pragmatic approach is to encourage
a healthy balanced diet that is rich in vitamin D. For
older people who are at risk of fall, especially those
in residential care home for the elderly (RCHE), a
dose of 800 IU of vitamin D3 per day with or without
calcium supplementation is recommended, provided
there is no contra-indication.11 The clinician should
also ask whether the older person is taking any over-
the-countervitamin D–containingdrugs before
commencing supplementation, as excess vitamin D
may result in hypercalcaemia.
Correction of vision
Poor visual acuity caused by presbyopia, cataract,
maculardegenerationor glaucoma,reductionin
depth perception and contrast sensitivity are risk
factors for falls.25 Maximising vision with cataract
surgery is effective in fall prevention. In a UK RCT
167Hong Kong Med J⎥ Volume 21 Number 2⎥ April 2015⎥ www.hkmj.org
10-form Tai Chi in a randomised controlled trial
(RCT). Tai Chi is a combination of strength and
balance training, with a certain aerobic element.15
In Hong Kong, most people practise the full form
that should theoretically be at least effective, if not
better. This can be promoted as a territory-wide
health recommendation. Nonetheless, not all Tai
Chi programmes improve balance. One local RCT
revealed no difference in the number of falls between
a Tai Chi group and controls after 12 months.16
Environmental interventions
Home modificationscan effectivelyreduce risk
of falls in the community,11 and include removal
of floor mats, painting the edge of steps, reducing
glare,installinghandles,and improvinglighting.
Occupational therapists can provide expert advice
in this area. For older people with fall risk who live
at home, especially those who are usually alone,
installation of a safety alarm is recommended so help
can be summoned should an accident occur.
Medication review
Polypharmacyis common among older people
who often have multiple co-morbidities, and is an
independent variable that has been linked to falls in
older people.17 Many drugs, psychotropic medications
and antihypertensive agents in particular, are related
to falls. The use of psychotropic medication should
be confined to patients who do not respond to non-
pharmacological intervention and the lowest dosage
should be prescribed. Periodic review of indications
and side-effectsshould be undertaken:gradual
withdrawal of psychotropic medication can reduce
rate of falls in community-dwelling elderly people.11
Nonethelessdrug withdrawalis a complicated
interventionthat should be implementedby an
experienced clinician after carefully weighing the
risks and benefits.A standardisedand explicit
medicinereview tool such as the Beers Criteria
for PotentiallyInappropriateMedicationUse in
Older Adults and STOPP (Screening Tool of Older
Person’spotentiallyinappropriatePrescriptions)
may be useful in reducing falls in older people but
the effectiveness of these approaches has not been
proven by RCTs.18,19 Although drug withdrawal
is beneficial, studies that include RCTs show that
many withdrawals (eg sleeping pills) are reversed
and patientsresumeprevioustherapy.Ongoing
monitoring is therefore essential.20
Foot and footwear
Foot and footwear problems are common but are
often ignored.Footwearinfluencesbalanceand
risk of falls. High-heeled shoes have been shown
to increasefalls in older people.Anti-slip shoe
devices effectively reduce outdoor falls in slippery
conditions.21 A systematic review recommends that
elderly individuals wear shoes with a low heel and
firm slip-resistant soles, both inside and outside the
home.22 Podiatrists, and prosthetics and orthotics
professionalscan give valuableadvice in this
respect. A recent RCT has shown that multifaceted
podiatry intervention with foot orthoses, footwear
advice, education, and foot and ankle exercises can
reduce the rate of falls in community-dwelling older
people.23
Vitamin D supplement
The benefit of vitamin D in falls/fractures extends
beyond improvedbone health. Vitamin D can
strengthen muscle and hence reduce falls. Meta-
analysis has shown that supplemental vitamin D at
a dose of 700 IU to 1000 IU a day reduces the risk of
falling among older individuals by 19%.24 The current
opinion is that in community-dwellingelderly,
vitamin D supplementation reduces the rate of falls
or risk of falling in a subgroup of people with low
vitamin D levels but its benefit is absent in people
without deficiency.11 In the institutionalised elderly,
vitamin D supplementationappearsto be more
effective in reducing falls and the recommendation
is to prescribe vitamin D with or without calcium
supplements to older people with low vitamin D
levels or those who are institutionalised.11 Despite
theserecommendations,most studieshave been
conducted in western countries that experience a
quite different duration and intensity of sunshine to
Hong Kong. Whether the benefit of vitamin D in fall
prevention applies equally to Hong Kong Chinese
populationis not known. Most public hospital
laboratories in Hong Kong do not have the means
to investigate vitamin D levels and clinicians are
required to send blood samples to private laboratories
for vitamin D level assay at a cost. Thus in the public
health sector,mass screeningof the elderlyfor
vitamin D deficiency prior to supplementation is
impractical. The pragmatic approach is to encourage
a healthy balanced diet that is rich in vitamin D. For
older people who are at risk of fall, especially those
in residential care home for the elderly (RCHE), a
dose of 800 IU of vitamin D3 per day with or without
calcium supplementation is recommended, provided
there is no contra-indication.11 The clinician should
also ask whether the older person is taking any over-
the-countervitamin D–containingdrugs before
commencing supplementation, as excess vitamin D
may result in hypercalcaemia.
Correction of vision
Poor visual acuity caused by presbyopia, cataract,
maculardegenerationor glaucoma,reductionin
depth perception and contrast sensitivity are risk
factors for falls.25 Maximising vision with cataract
surgery is effective in fall prevention. In a UK RCT
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
# Luk et al#
168 Hong Kong Med J⎥ Volume 21 Number 2⎥ April 2015⎥ www.hkmj.org
that compared fast-track (4 weeks) with routine-
queue(12 months)first eye cataractsurgery,a
significant reduction in fall and fracture rate in 1
year was observed in the fast-track group.26 Another
RCT by the same team showedthat fast-track
surgery (4 weeks) for the second eye in older people
also produced a tendency to fewer falls compared
with the routine queue (12 months) group.27 One
should beware, though, that correction of vision
may sometimes result in increased falls. One RCT
showed that vision assessment and intervention may
increase the risk of falls and fractures, possibly due
to poor adjustment to new spectacles.28 Multifocal
lenses may increase fall risk by reducing contrast
sensitivity and depth perception in the lower visual
field when mobilising.29 As such, older individuals
should wear single lens glasses,especiallywhen
performing outdoor activities.
Management of cardiovascular risk factors
Cardiovascularinvestigationsand interventions
are indicated for those with fall related to syncope
and orthostatichypotension.Neurally mediated
syndromes (carotid sinus hypersensitivity,
vasovagal syndrome, orthostatic hypotension,
postprandial hypotension), arrhythmias (sick sinus
syndrome,severeheart block, tachyarrhythmia),
and structuralcardiacdisease(valvularstenosis,
hypertrophicobstructivecardiomyopathy,atrial
myxoma, aortic dissection) are all risk factors for
falls because they cause either attacks of syncope or
transient hypotension (pre-syncope).30 Randomised
controlled trials in older patients have shown that
those with dual-chamber pacemaker implantation
for cardio-inhibitory carotid sinus hypersensitivity
had significantly fewer falls and fall-related
injuries.31,32It is beyond the scope of this article to
describe in detail the investigation and management
of individual cardiovascular conditions. Referrals to
cardiology colleagues are recommended for certain
conditions such as arrhythmias when appropriate.
Other conditions such as postural hypotension can
usually be managed by a geriatrician.
Multifactorial intervention
A MFI programme is a set of interventions designed
to addressmultiple elementsof fall risk.33 The
elements of MFI usually include multi-component
exercises,medical assessmentand management
of falls, medication adjustment, vitamin D
supplementationif appropriate,environmental
modifications, and patient education. Since falls are
often multifactorial in nature, MFI (rather than a
singular approach) is more likely to be effective and
is therefore recommended. The intervention can take
the form of a general MFI or be an individualised
MFI with tailor-made interventions based on specific
individual needs.11 Most evidence to support MFI
efficacy is in community-dwelling older people. In a
community setting, general MFI can achieve a 24%
to 31% reduction in fall risk, while individualise
MFI may improve this figure to 27% to 41%.10 Multi-
factorial intervention may not be effective in fa
prevention in other settings, such as in the acciden
and emergency department.34 A recent Malaysian
RCT has just been completed to determine whether
MFI is appropriate in an Asian country; the results
are pending.35
Fracture reduction
Fall-related fractures can be reduced by improv
bone strength.Thus assessmentof bone health
should be performed in older people as part of the
comprehensive assessment. If indicated clinically
bone mineral density assessment can be undertake
in patients at risk of fragility fracture.36 In addition
to vitamin D and calcium supplementation, specific
pharmacological treatment should be considered
The World Health OrganizationFRAX (Fracture
Risk Assessment Tool) score can be used to gu
treatment by calculating the 10-year osteoporot
fracture rate.37 It is beyond the scope of this article to
describe in detail the management of bone fragility
Another means of fracture protection is the
use of hip protectors.38 Most hip protector designs
consist of two mechanically proven hard plastic cup
or soft pads placed or sewn to each side of a panty
Compliance with their use has been a problem
most studies though, and rates varying from 31
to 68% have been reported, reducing in particu
over time.39 One local study reported overall
compliance rates of 55% to 70% with an 82% relati
risk reductionof hip fracture.40 In Hong Kong,
the hot and humid weather makes wearing of
protectors uncomfortable for a prolonged period of
time. Nonetheless a small reduction in hip fracture
risk was reported in a systematic review when
protectors were used in a RCHE with risk ratio
0.82 (confidence interval, 0.67-1.00).41 No evidence
of such benefit was observed in a community settin
hence their use should probably be confined to the
RCHE setting.
Fall prevention in hospital and residentia
care home setting
Multifactorial interventionin hospital and the
RCHE has been shown in a systematic review t
reduce rate of falls.42 The effective components were
comprehensive assessment, staff education, assisti
devices, and reduction of medications.Older
patients or residents should be assessed individuall
to developindividualisedMFI treatmentplans.
However, the use of screening tools for risk of
is more controversial in the institutional setting
168 Hong Kong Med J⎥ Volume 21 Number 2⎥ April 2015⎥ www.hkmj.org
that compared fast-track (4 weeks) with routine-
queue(12 months)first eye cataractsurgery,a
significant reduction in fall and fracture rate in 1
year was observed in the fast-track group.26 Another
RCT by the same team showedthat fast-track
surgery (4 weeks) for the second eye in older people
also produced a tendency to fewer falls compared
with the routine queue (12 months) group.27 One
should beware, though, that correction of vision
may sometimes result in increased falls. One RCT
showed that vision assessment and intervention may
increase the risk of falls and fractures, possibly due
to poor adjustment to new spectacles.28 Multifocal
lenses may increase fall risk by reducing contrast
sensitivity and depth perception in the lower visual
field when mobilising.29 As such, older individuals
should wear single lens glasses,especiallywhen
performing outdoor activities.
Management of cardiovascular risk factors
Cardiovascularinvestigationsand interventions
are indicated for those with fall related to syncope
and orthostatichypotension.Neurally mediated
syndromes (carotid sinus hypersensitivity,
vasovagal syndrome, orthostatic hypotension,
postprandial hypotension), arrhythmias (sick sinus
syndrome,severeheart block, tachyarrhythmia),
and structuralcardiacdisease(valvularstenosis,
hypertrophicobstructivecardiomyopathy,atrial
myxoma, aortic dissection) are all risk factors for
falls because they cause either attacks of syncope or
transient hypotension (pre-syncope).30 Randomised
controlled trials in older patients have shown that
those with dual-chamber pacemaker implantation
for cardio-inhibitory carotid sinus hypersensitivity
had significantly fewer falls and fall-related
injuries.31,32It is beyond the scope of this article to
describe in detail the investigation and management
of individual cardiovascular conditions. Referrals to
cardiology colleagues are recommended for certain
conditions such as arrhythmias when appropriate.
Other conditions such as postural hypotension can
usually be managed by a geriatrician.
Multifactorial intervention
A MFI programme is a set of interventions designed
to addressmultiple elementsof fall risk.33 The
elements of MFI usually include multi-component
exercises,medical assessmentand management
of falls, medication adjustment, vitamin D
supplementationif appropriate,environmental
modifications, and patient education. Since falls are
often multifactorial in nature, MFI (rather than a
singular approach) is more likely to be effective and
is therefore recommended. The intervention can take
the form of a general MFI or be an individualised
MFI with tailor-made interventions based on specific
individual needs.11 Most evidence to support MFI
efficacy is in community-dwelling older people. In a
community setting, general MFI can achieve a 24%
to 31% reduction in fall risk, while individualise
MFI may improve this figure to 27% to 41%.10 Multi-
factorial intervention may not be effective in fa
prevention in other settings, such as in the acciden
and emergency department.34 A recent Malaysian
RCT has just been completed to determine whether
MFI is appropriate in an Asian country; the results
are pending.35
Fracture reduction
Fall-related fractures can be reduced by improv
bone strength.Thus assessmentof bone health
should be performed in older people as part of the
comprehensive assessment. If indicated clinically
bone mineral density assessment can be undertake
in patients at risk of fragility fracture.36 In addition
to vitamin D and calcium supplementation, specific
pharmacological treatment should be considered
The World Health OrganizationFRAX (Fracture
Risk Assessment Tool) score can be used to gu
treatment by calculating the 10-year osteoporot
fracture rate.37 It is beyond the scope of this article to
describe in detail the management of bone fragility
Another means of fracture protection is the
use of hip protectors.38 Most hip protector designs
consist of two mechanically proven hard plastic cup
or soft pads placed or sewn to each side of a panty
Compliance with their use has been a problem
most studies though, and rates varying from 31
to 68% have been reported, reducing in particu
over time.39 One local study reported overall
compliance rates of 55% to 70% with an 82% relati
risk reductionof hip fracture.40 In Hong Kong,
the hot and humid weather makes wearing of
protectors uncomfortable for a prolonged period of
time. Nonetheless a small reduction in hip fracture
risk was reported in a systematic review when
protectors were used in a RCHE with risk ratio
0.82 (confidence interval, 0.67-1.00).41 No evidence
of such benefit was observed in a community settin
hence their use should probably be confined to the
RCHE setting.
Fall prevention in hospital and residentia
care home setting
Multifactorial interventionin hospital and the
RCHE has been shown in a systematic review t
reduce rate of falls.42 The effective components were
comprehensive assessment, staff education, assisti
devices, and reduction of medications.Older
patients or residents should be assessed individuall
to developindividualisedMFI treatmentplans.
However, the use of screening tools for risk of
is more controversial in the institutional setting
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
# Falls prevention in the elderly#
169Hong Kong Med J⎥ Volume 21 Number 2⎥ April 2015⎥ www.hkmj.org
In Hong Kong, screening tools such as Morse Fall
Scale and STRATIFY are mandated in many hospital
wards, long-stay wards in particular, with the former
more commonly used.43,44 To date though, there is
no evidence to support their use in fall prevention
in an institutional setting. An experienced nurse’s
clinical judgement is just as effective.45 In addition,
a disadvantage of screening tools is that they predict
fall due to physiological factors, not incidental falls
(eg patient slipping or tripping) or unpredictable
physiologicalfalls (eg seizures,syncope).Other
risk factors for falls such as “impaired judgement in
patients with cognitive impairment” may also not be
included in traditional screening tools.46
Health care providers in hospitals or RCHEs
may employphysicalrestraintsto older patients
when they are at risk of falling or delirious although
evidencesuggeststhese are ineffective,not to
mentionundignified.47 Further,patientsmay fall
more frequently and sustain more serious injuries.
Restraintsincreasethe risk of delirium in the
hospital setting and the consequent immobilisation
precipitatesother problems such as pressure
sores, respiratorycomplications,and death via
strangulation and aspiration. Although some long-
stay hospitals and institutions in Hong Kong have
implementeda restraint reduction programme,
they remain commonly used in some institutional
settings.48
Vitamin D can be consideredfor all older
people who live in RCHEs where the prevalence of
deficiency is high. Other strategies for fall prevention
that havebeen used in institutionalsettingsare
a chair/bed alarm system,ultra-low beds, and
changing of the floor surface from vinyl to carpet.
Nevertheless the effectiveness of these methods has
not been proven through RCTs.49
Fall prevention in the cognitively impaired
older people
Although falls are common among the elderly, there
is insufficient evidence to recommend MFI or single
intervention for cognitively impaired older people
in community, hospital, and RCHE settings. The
elderly with dementia have often been excluded from
large-scale studies of falls. During training for fall
prevention, older patients may be required to learn
exercise skills and remember instructions; impaired
memory can affect the success of fall prevention.
Another report concludes that intervention for fall
prevention among cognitively impaired older people
in RCHEs is ineffective.50 Nonetheless some studies
have reported positive effects. A local retrospective
study showed that older people with dementia can
still benefit from rehabilitation.51 One meta-analysis
showed that strategies to prevent falls and fractures in
hospitals and RCHEs were not affected by cognitive
impairment.52 Another study demonstrated that the
number of falls in psychogeriatric RCHE residents
could be reduced by a targetedMFI.53 More
studies are required to determine the optimum fall
prevention strategies for older people with dementia.
Conclusion
Evidence-basedinterventions include multi-
component group or home-based exercises, Tai Chi,
environmentalmodifications,medicationreview,
management of foot and footwear problems, vitamin
D supplementation, and addressing cardiovascular
problems. If possible, these are best implemented
in the form of MFI. Bone health enhancement for
RCHE and appropriatecommunitypatientsand
prescription of hip protectors for RCHE patients
are also recommended.A MFI programmemay
also be useful in the hospital and RCHE setting. Use
of physical restraints is not recommended for fall
prevention. More high-quality studies are required
to examine fall prevention for older people with
cognitive impairment. Modern technology for fall
prevention, such as movement alarms and sensor
technology, should also be further explored.
References
1. Willeboordse F, Hugtenburg JG, van Dijk L, et al. Opti-
Med: the effectiveness of optimised clinical medication
reviews in older people with ‘geriatric giants’ in general
practice; study protocol of a cluster randomised controlled
trial. BMC Geriatr 2014;14:116.
2. Nevitt MC, CummingsSR, Hudes ES. Risk factors
for injurious falls: a prospectivestudy. J Gerontol
1991;46:M164-70.
3. Chu LW, Chi I, Chiu AY. Falls and fall-related injuries in
community-dwelling elderly persons in Hong Kong: a study
on risk factors, functional decline, and health services
utilization after falls. Hong Kong Med J 2007;13(Suppl
1):S8-12.
4. Chu LW, Chi I, Chiu AY. Incidence and predictors of falls in
the Chinese elderly. Ann Acad Med Singapore 2005;34:60-
72.
5. Luk JK, Chiu PK, Chu LW. Factors affecting
institutionalization in older Hong Kong Chinese patients
after recovery from acute medical problems. Arch Gerontol
Geriatr 2009;49:e110-4.
6. Chu LW, Chiu AY. Chi I. Falls and subsequent health
service utilization in community-dwelling Chinese older
adults. Arch Gerontol Geriatr 2008;46:125-35.
7. Hill AM, Hoffmann T, Hill K, et al. Measuring falls events
in acute hospitals—acomparisonof three reporting
methods to identify missing data in the hospital reporting
system. J Am Geriatr Soc 2010;58:1347-52.
8. Chan DK. Chan’s practical geriatrics. 2nd ed. Brookvale,
NSW: BA Printing & Publishing Services; 2009.
9. Luk JK, Or KH, Woo J. Using the comprehensive geriatric
assessmenttechniqueto assesselderlypatients.Hong
Kong Med J 2000;6:93-8.
10. Podsiadlo D, Richardson S. The timed “Up & Go”: a test
of basic functional mobility for frail elderly persons. J Am
Geriatr Soc 1991;39:142-8.
169Hong Kong Med J⎥ Volume 21 Number 2⎥ April 2015⎥ www.hkmj.org
In Hong Kong, screening tools such as Morse Fall
Scale and STRATIFY are mandated in many hospital
wards, long-stay wards in particular, with the former
more commonly used.43,44 To date though, there is
no evidence to support their use in fall prevention
in an institutional setting. An experienced nurse’s
clinical judgement is just as effective.45 In addition,
a disadvantage of screening tools is that they predict
fall due to physiological factors, not incidental falls
(eg patient slipping or tripping) or unpredictable
physiologicalfalls (eg seizures,syncope).Other
risk factors for falls such as “impaired judgement in
patients with cognitive impairment” may also not be
included in traditional screening tools.46
Health care providers in hospitals or RCHEs
may employphysicalrestraintsto older patients
when they are at risk of falling or delirious although
evidencesuggeststhese are ineffective,not to
mentionundignified.47 Further,patientsmay fall
more frequently and sustain more serious injuries.
Restraintsincreasethe risk of delirium in the
hospital setting and the consequent immobilisation
precipitatesother problems such as pressure
sores, respiratorycomplications,and death via
strangulation and aspiration. Although some long-
stay hospitals and institutions in Hong Kong have
implementeda restraint reduction programme,
they remain commonly used in some institutional
settings.48
Vitamin D can be consideredfor all older
people who live in RCHEs where the prevalence of
deficiency is high. Other strategies for fall prevention
that havebeen used in institutionalsettingsare
a chair/bed alarm system,ultra-low beds, and
changing of the floor surface from vinyl to carpet.
Nevertheless the effectiveness of these methods has
not been proven through RCTs.49
Fall prevention in the cognitively impaired
older people
Although falls are common among the elderly, there
is insufficient evidence to recommend MFI or single
intervention for cognitively impaired older people
in community, hospital, and RCHE settings. The
elderly with dementia have often been excluded from
large-scale studies of falls. During training for fall
prevention, older patients may be required to learn
exercise skills and remember instructions; impaired
memory can affect the success of fall prevention.
Another report concludes that intervention for fall
prevention among cognitively impaired older people
in RCHEs is ineffective.50 Nonetheless some studies
have reported positive effects. A local retrospective
study showed that older people with dementia can
still benefit from rehabilitation.51 One meta-analysis
showed that strategies to prevent falls and fractures in
hospitals and RCHEs were not affected by cognitive
impairment.52 Another study demonstrated that the
number of falls in psychogeriatric RCHE residents
could be reduced by a targetedMFI.53 More
studies are required to determine the optimum fall
prevention strategies for older people with dementia.
Conclusion
Evidence-basedinterventions include multi-
component group or home-based exercises, Tai Chi,
environmentalmodifications,medicationreview,
management of foot and footwear problems, vitamin
D supplementation, and addressing cardiovascular
problems. If possible, these are best implemented
in the form of MFI. Bone health enhancement for
RCHE and appropriatecommunitypatientsand
prescription of hip protectors for RCHE patients
are also recommended.A MFI programmemay
also be useful in the hospital and RCHE setting. Use
of physical restraints is not recommended for fall
prevention. More high-quality studies are required
to examine fall prevention for older people with
cognitive impairment. Modern technology for fall
prevention, such as movement alarms and sensor
technology, should also be further explored.
References
1. Willeboordse F, Hugtenburg JG, van Dijk L, et al. Opti-
Med: the effectiveness of optimised clinical medication
reviews in older people with ‘geriatric giants’ in general
practice; study protocol of a cluster randomised controlled
trial. BMC Geriatr 2014;14:116.
2. Nevitt MC, CummingsSR, Hudes ES. Risk factors
for injurious falls: a prospectivestudy. J Gerontol
1991;46:M164-70.
3. Chu LW, Chi I, Chiu AY. Falls and fall-related injuries in
community-dwelling elderly persons in Hong Kong: a study
on risk factors, functional decline, and health services
utilization after falls. Hong Kong Med J 2007;13(Suppl
1):S8-12.
4. Chu LW, Chi I, Chiu AY. Incidence and predictors of falls in
the Chinese elderly. Ann Acad Med Singapore 2005;34:60-
72.
5. Luk JK, Chiu PK, Chu LW. Factors affecting
institutionalization in older Hong Kong Chinese patients
after recovery from acute medical problems. Arch Gerontol
Geriatr 2009;49:e110-4.
6. Chu LW, Chiu AY. Chi I. Falls and subsequent health
service utilization in community-dwelling Chinese older
adults. Arch Gerontol Geriatr 2008;46:125-35.
7. Hill AM, Hoffmann T, Hill K, et al. Measuring falls events
in acute hospitals—acomparisonof three reporting
methods to identify missing data in the hospital reporting
system. J Am Geriatr Soc 2010;58:1347-52.
8. Chan DK. Chan’s practical geriatrics. 2nd ed. Brookvale,
NSW: BA Printing & Publishing Services; 2009.
9. Luk JK, Or KH, Woo J. Using the comprehensive geriatric
assessmenttechniqueto assesselderlypatients.Hong
Kong Med J 2000;6:93-8.
10. Podsiadlo D, Richardson S. The timed “Up & Go”: a test
of basic functional mobility for frail elderly persons. J Am
Geriatr Soc 1991;39:142-8.
# Luk et al#
170 Hong Kong Med J⎥ Volume 21 Number 2⎥ April 2015⎥ www.hkmj.org
11. GillespieLD, Robertson MC, Gillespie WJ, et al.
Interventionsfor preventingfalls in older people
living in the community. Cochrane Database Syst Rev
2012;(9):CD007146.
12. El-KhouryF, CassouB, CharlesMA, Dargent-Molina
P. The effect of fall prevention exercise programmes on
fall induced injuries in community dwelling older adults:
systematicreview and meta-analysisof randomised
controlled trials. BMJ 2013;347:f6234.
13. Gardner MM, Robertson MC, Campbell AJ. Exercise in
preventing falls and fall related injuries in older people: a
review of randomised controlled trials. Br J Sports Med
2000;34:7-17.
14. Wolf SL, Barnhart HX, Kutner NG, McNeely E, Coogler
C, Xu T; Atlanta FICSIT Group. Selected as the best paper
in the 1990s: Reducing frailty and falls in older persons: an
investigation of tai chi and computerized balance training.
J Am Geriatr Soc 2003;51:1794-803.
15. Hackney ME, Wolf SL. Impact of Tai Chi Chu’an practice
on balance and mobility in older adults: an integrative
review of 20 yearsof research.J Geriatr Phys Ther
2014;37:127-35.
16. Woo J, Hong A, Lau E, Lynn H. A randomised controlled
trial of Tai Chi and resistance exercise on bone health,
muscle strength and balance in community-living elderly
people. Age Ageing 2007;36:262-8.
17. HammondT, Wilson A. Polypharmacyand falls in
the elderly:a literaturereview.Nurs Midwifery Stud
2013;2:171-5.
18. de Vries OJ, Peeters G, Elders P, et al. The elimination
half-life of benzodiazepines and fall risk: two prospective
observational studies. Age Ageing 2013;42:764-70.
19. Fick DM, Cooper JW, Wade WE, Waller JL, Maclean JR,
BeersMH. Updatingthe Beerscriteriafor potentially
inappropriatemedicationuse in older adults:results
of a US consensus panel of experts. Arch Intern Med
2003;163:2716-24.
20. CampbellAJ, RobertsonMC, Gardner MM, Norton
RN, Buchner DM. Psychotropic medication withdrawal
and a home-based exercise program to prevent falls: a
randomized, controlled trial. J Am Geriatr Soc 1999;47:850-
3.
21. McKiernan FE. A simple gait-stabilizing device reduces
outdoor falls and nonseriousinjurious falls in fall-
prone older people during the winter. J Am Geriatr Soc
2005;53:943-7.
22. Menant JC, Steele JR, Menz HB, Munro BJ, Lord SR.
Optimizing footwear for older people at risk of falls. J
Rehabil Res Dev 2008;45:1167-81.
23. Spink MJ, Menz HB, Fotoohabadi MR, et al. Effectiveness
of a multifaceted podiatry intervention to prevent falls in
community dwelling older people with disabling foot pain:
randomised controlled trial. BMJ 2011;342:d3411.
24. Bischoff-Ferrari HA, Dawson-Hughes B, Staehelin HB, et
al. Fall prevention with supplemental and active forms of
vitamin D: a meta-analysis of randomised controlled trials.
BMJ 2009;339:b3692.
25. Lord SR. Visual risk factors for falls in older people. Age
Ageing 2006;35 Suppl 2:ii42-ii45.
26. Harwood RH, Foss AJ, Osborn F, Gregson RM, Zaman A,
Masud T. Falls and health status in elderly women following
first eye cataract surgery: a randomised controlled trial. Br
J Ophthalmol 2005;89:53-9.
27. Foss AJ, Harwood RH, Osborn F, Gregson RM, Zaman A,
Masud T. Falls and health status in elderly women follow
second eye cataract surgery: a randomised controlled tri
Age Ageing 2006;35:66-71.
28. Cumming RG, Ivers R, Clemson L, et al. Improving vision
to prevent falls in frail older people: a randomized trial. J
Am Geriatr Soc 2007;55:175-81.
29. Lord SR, Dayhew J, Howland A. Multifocal glasses impair
edge-contrastsensitivityand depth perceptionand
increase the risk of falls in older people. J Am Geriatr Soc
2002;50:1760-6.
30. Brian JC, Potter JF. Cardiovascular causes of falls. Age an
Ageing 2001;30 Suppl 4:19-24.
31. Ryan DJ, Nick S, Colette SM, Roseanne K. Carotid s
syndrome, should we pace? A multicentre, randomise
control trial (Safepace 2). Heart 2010;96:347-51.
32. Kenny RA, Richardson DA, Steen N, Bexton RS, Shaw FE
Bond J. Carotid sinus syndrome: a modifiable risk fa
for nonaccidental falls in older adults (SAFE PACE). J Am
Coll Cardiol 2001;38:1491-6.
33. Day LM. Fall prevention programs for community-dwellin
older people should primarily target a multifactorial
intervention rather than exercise as a single intervention
J Am Geriatr Soc 2013;61:284-5; discussion 285-6.
34. RussellMA, Hill KD, Day LM, et al. A randomized
controlled trial of a multifactorialfalls prevention
interventionfor older fallerspresentingto emergency
departments. J Am Geriatr Soc 2010;58:2265-74.
35. Tan PJ, Khoo EM, Chinna K, Hill KD, Poi PJ, Tan MP. An
individually-tailored multifactorial intervention program
for older fallers in a middle-income developing count
Malaysian Falls Assessmentand InterventionTrial
(MyFAIT). BMC Geriatr 2014;14:78.
36. Osteoporosis Society of Hong Kong (OSHK). 2013 OSHK
Guideline for Clinical Management of Postmenopausa
Osteoporosisin Hong Kong. Hong Kong Med J
2013;19(Supplement 2):S1-40.
37. Michieli R, Carraro AM. General Practitioner and FRAX(®
(computer-basedalgorithm).Clin Cases Miner Bone
Metab 2014;11:120-2.
38. GillespieWJ, GillespieLD, ParkerMJ. Hip protectors
for preventing hip fractures in older people. Cochran
Database Syst Rev 2010;(10):CD001255.
39. Sawka AM, Boulos P, Beattie K, et al. Do hip prote
decreasethe risk of hip fracturein institutionaland
community-dwellingelderly?A systematicreview and
meta-analysis of randomized controlled trials. Osteoporo
Int 2005;16:1461-74.
40. Woo J, Sum C, Yiu HH, Ip K, Chung L, Ho L. Efficacy of a
specially designed hip protector for hip fracture preventio
and compliance with use in elderly Hong Kong Chine
Clin Rehabil 2003;17:203-5.
41. Santesso N, Carrasco-Labra A, Brignardello-Petersen
Hip protectors for preventing hip fractures in older peopl
Cochrane Database Syst Rev 2014;(3):CD001255.
42. CameronID, Gillespie LD, Robertson MC, et al.
Interventions for preventing falls in older people in c
facilitiesand hospitals.CochraneDatabaseSyst Rev
2012;(12):CD005465.
43. Morse JM, Morse R, Tylko S. Development of a scal
identify the fall-prone patient. Can J Aging 1989;8:366-77
44. Oliver D, Britton M, Seed P, Martin FC, Hopper AH.
Developmentand evaluationof evidencebased risk
170 Hong Kong Med J⎥ Volume 21 Number 2⎥ April 2015⎥ www.hkmj.org
11. GillespieLD, Robertson MC, Gillespie WJ, et al.
Interventionsfor preventingfalls in older people
living in the community. Cochrane Database Syst Rev
2012;(9):CD007146.
12. El-KhouryF, CassouB, CharlesMA, Dargent-Molina
P. The effect of fall prevention exercise programmes on
fall induced injuries in community dwelling older adults:
systematicreview and meta-analysisof randomised
controlled trials. BMJ 2013;347:f6234.
13. Gardner MM, Robertson MC, Campbell AJ. Exercise in
preventing falls and fall related injuries in older people: a
review of randomised controlled trials. Br J Sports Med
2000;34:7-17.
14. Wolf SL, Barnhart HX, Kutner NG, McNeely E, Coogler
C, Xu T; Atlanta FICSIT Group. Selected as the best paper
in the 1990s: Reducing frailty and falls in older persons: an
investigation of tai chi and computerized balance training.
J Am Geriatr Soc 2003;51:1794-803.
15. Hackney ME, Wolf SL. Impact of Tai Chi Chu’an practice
on balance and mobility in older adults: an integrative
review of 20 yearsof research.J Geriatr Phys Ther
2014;37:127-35.
16. Woo J, Hong A, Lau E, Lynn H. A randomised controlled
trial of Tai Chi and resistance exercise on bone health,
muscle strength and balance in community-living elderly
people. Age Ageing 2007;36:262-8.
17. HammondT, Wilson A. Polypharmacyand falls in
the elderly:a literaturereview.Nurs Midwifery Stud
2013;2:171-5.
18. de Vries OJ, Peeters G, Elders P, et al. The elimination
half-life of benzodiazepines and fall risk: two prospective
observational studies. Age Ageing 2013;42:764-70.
19. Fick DM, Cooper JW, Wade WE, Waller JL, Maclean JR,
BeersMH. Updatingthe Beerscriteriafor potentially
inappropriatemedicationuse in older adults:results
of a US consensus panel of experts. Arch Intern Med
2003;163:2716-24.
20. CampbellAJ, RobertsonMC, Gardner MM, Norton
RN, Buchner DM. Psychotropic medication withdrawal
and a home-based exercise program to prevent falls: a
randomized, controlled trial. J Am Geriatr Soc 1999;47:850-
3.
21. McKiernan FE. A simple gait-stabilizing device reduces
outdoor falls and nonseriousinjurious falls in fall-
prone older people during the winter. J Am Geriatr Soc
2005;53:943-7.
22. Menant JC, Steele JR, Menz HB, Munro BJ, Lord SR.
Optimizing footwear for older people at risk of falls. J
Rehabil Res Dev 2008;45:1167-81.
23. Spink MJ, Menz HB, Fotoohabadi MR, et al. Effectiveness
of a multifaceted podiatry intervention to prevent falls in
community dwelling older people with disabling foot pain:
randomised controlled trial. BMJ 2011;342:d3411.
24. Bischoff-Ferrari HA, Dawson-Hughes B, Staehelin HB, et
al. Fall prevention with supplemental and active forms of
vitamin D: a meta-analysis of randomised controlled trials.
BMJ 2009;339:b3692.
25. Lord SR. Visual risk factors for falls in older people. Age
Ageing 2006;35 Suppl 2:ii42-ii45.
26. Harwood RH, Foss AJ, Osborn F, Gregson RM, Zaman A,
Masud T. Falls and health status in elderly women following
first eye cataract surgery: a randomised controlled trial. Br
J Ophthalmol 2005;89:53-9.
27. Foss AJ, Harwood RH, Osborn F, Gregson RM, Zaman A,
Masud T. Falls and health status in elderly women follow
second eye cataract surgery: a randomised controlled tri
Age Ageing 2006;35:66-71.
28. Cumming RG, Ivers R, Clemson L, et al. Improving vision
to prevent falls in frail older people: a randomized trial. J
Am Geriatr Soc 2007;55:175-81.
29. Lord SR, Dayhew J, Howland A. Multifocal glasses impair
edge-contrastsensitivityand depth perceptionand
increase the risk of falls in older people. J Am Geriatr Soc
2002;50:1760-6.
30. Brian JC, Potter JF. Cardiovascular causes of falls. Age an
Ageing 2001;30 Suppl 4:19-24.
31. Ryan DJ, Nick S, Colette SM, Roseanne K. Carotid s
syndrome, should we pace? A multicentre, randomise
control trial (Safepace 2). Heart 2010;96:347-51.
32. Kenny RA, Richardson DA, Steen N, Bexton RS, Shaw FE
Bond J. Carotid sinus syndrome: a modifiable risk fa
for nonaccidental falls in older adults (SAFE PACE). J Am
Coll Cardiol 2001;38:1491-6.
33. Day LM. Fall prevention programs for community-dwellin
older people should primarily target a multifactorial
intervention rather than exercise as a single intervention
J Am Geriatr Soc 2013;61:284-5; discussion 285-6.
34. RussellMA, Hill KD, Day LM, et al. A randomized
controlled trial of a multifactorialfalls prevention
interventionfor older fallerspresentingto emergency
departments. J Am Geriatr Soc 2010;58:2265-74.
35. Tan PJ, Khoo EM, Chinna K, Hill KD, Poi PJ, Tan MP. An
individually-tailored multifactorial intervention program
for older fallers in a middle-income developing count
Malaysian Falls Assessmentand InterventionTrial
(MyFAIT). BMC Geriatr 2014;14:78.
36. Osteoporosis Society of Hong Kong (OSHK). 2013 OSHK
Guideline for Clinical Management of Postmenopausa
Osteoporosisin Hong Kong. Hong Kong Med J
2013;19(Supplement 2):S1-40.
37. Michieli R, Carraro AM. General Practitioner and FRAX(®
(computer-basedalgorithm).Clin Cases Miner Bone
Metab 2014;11:120-2.
38. GillespieWJ, GillespieLD, ParkerMJ. Hip protectors
for preventing hip fractures in older people. Cochran
Database Syst Rev 2010;(10):CD001255.
39. Sawka AM, Boulos P, Beattie K, et al. Do hip prote
decreasethe risk of hip fracturein institutionaland
community-dwellingelderly?A systematicreview and
meta-analysis of randomized controlled trials. Osteoporo
Int 2005;16:1461-74.
40. Woo J, Sum C, Yiu HH, Ip K, Chung L, Ho L. Efficacy of a
specially designed hip protector for hip fracture preventio
and compliance with use in elderly Hong Kong Chine
Clin Rehabil 2003;17:203-5.
41. Santesso N, Carrasco-Labra A, Brignardello-Petersen
Hip protectors for preventing hip fractures in older peopl
Cochrane Database Syst Rev 2014;(3):CD001255.
42. CameronID, Gillespie LD, Robertson MC, et al.
Interventions for preventing falls in older people in c
facilitiesand hospitals.CochraneDatabaseSyst Rev
2012;(12):CD005465.
43. Morse JM, Morse R, Tylko S. Development of a scal
identify the fall-prone patient. Can J Aging 1989;8:366-77
44. Oliver D, Britton M, Seed P, Martin FC, Hopper AH.
Developmentand evaluationof evidencebased risk
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
# Falls prevention in the elderly#
171Hong Kong Med J⎥ Volume 21 Number 2⎥ April 2015⎥ www.hkmj.org
assessmenttool (STRATIFY) to predict which elderly
inpatients will fall: case-control and cohort studies. BMJ
1997;315:1049-53.
45. Meyer G, Köpke S, Haastert B, Mühlhauser I. Comparison
of a fall risk assessmenttool with nurses’judgement
alone: a cluster-randomised controlled trial. Age Ageing
2009;38:417-23.
46. ChanDK, Diu E, Loh F. Pilot study into impaired
judgement,self-toiletingbehaviourin fallersand non-
fallers. Eur J Ageing 2013;10:257-60.
47. Australian Commission on Safety and Quality in Healthcare.
Preventing falls and harm from falls in older people. Best
practice guidelines for Australian hospitals and residential
aged care facilities. In: Canberra (Australia): Australian
Commission on Safety and Quality in Healthcare; 2009.
48. Kwok T, Bai X, Chui MY, et al. Effect of physical restraint
reduction on older patients’ hospital length of stay. J Am
Med Dir Assoc 2012;13:645-50.
49. Becker C, Rapp K. Fall prevention in nursing homes. Clin
Geriatr Med 2010;26:693-704.
50. JensenLE, Padilla R. Effectivenessof interventionsto
prevent falls in people with Alzheimer’s disease and related
dementias. Am J Occup Ther 2011;65:532-40.
51. Luk JK, Chiu PK, Chu LW. Rehabilitation of older Chinese
patients with different cognitive functions: how do they
differ in outcome? Arch Phys Med Rehabil 2008;89:1714-9.
52. OliverD, ConnellyJB, Victor CR, et al. Strategiesto
prevent falls and fractures in hospitals and care homes
and effect of cognitive impairment: systematic review and
meta-analyses. BMJ 2007;334:82.
53. NeyensJC, Dijcks BP, Twisk J, et al. A multifactorial
intervention for the prevention of falls in psychogeriatric
nursing home patients,a randomisedcontrolledtrial
(RCT). Age Ageing 2009;38:194-9.
171Hong Kong Med J⎥ Volume 21 Number 2⎥ April 2015⎥ www.hkmj.org
assessmenttool (STRATIFY) to predict which elderly
inpatients will fall: case-control and cohort studies. BMJ
1997;315:1049-53.
45. Meyer G, Köpke S, Haastert B, Mühlhauser I. Comparison
of a fall risk assessmenttool with nurses’judgement
alone: a cluster-randomised controlled trial. Age Ageing
2009;38:417-23.
46. ChanDK, Diu E, Loh F. Pilot study into impaired
judgement,self-toiletingbehaviourin fallersand non-
fallers. Eur J Ageing 2013;10:257-60.
47. Australian Commission on Safety and Quality in Healthcare.
Preventing falls and harm from falls in older people. Best
practice guidelines for Australian hospitals and residential
aged care facilities. In: Canberra (Australia): Australian
Commission on Safety and Quality in Healthcare; 2009.
48. Kwok T, Bai X, Chui MY, et al. Effect of physical restraint
reduction on older patients’ hospital length of stay. J Am
Med Dir Assoc 2012;13:645-50.
49. Becker C, Rapp K. Fall prevention in nursing homes. Clin
Geriatr Med 2010;26:693-704.
50. JensenLE, Padilla R. Effectivenessof interventionsto
prevent falls in people with Alzheimer’s disease and related
dementias. Am J Occup Ther 2011;65:532-40.
51. Luk JK, Chiu PK, Chu LW. Rehabilitation of older Chinese
patients with different cognitive functions: how do they
differ in outcome? Arch Phys Med Rehabil 2008;89:1714-9.
52. OliverD, ConnellyJB, Victor CR, et al. Strategiesto
prevent falls and fractures in hospitals and care homes
and effect of cognitive impairment: systematic review and
meta-analyses. BMJ 2007;334:82.
53. NeyensJC, Dijcks BP, Twisk J, et al. A multifactorial
intervention for the prevention of falls in psychogeriatric
nursing home patients,a randomisedcontrolledtrial
(RCT). Age Ageing 2009;38:194-9.
1 out of 7
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





