3804NRS Assignment: Community Health Nursing Essay
VerifiedAdded on 2022/08/12
|9
|2068
|34
Essay
AI Summary
This essay, prepared for a community health nursing course, analyzes the Inala community in Brisbane, Queensland, using 2016 census data. The student identifies key social determinants of health, including indigenous status, unemployment, and lower education levels, and their impact on the community. The essay highlights the high prevalence of diabetes among the indigenous population as a critical health issue. It proposes a health promotion program based on the Medicare Benefits Scheme, focusing on health assessments, care planning, and increased access to healthcare services, including staff training and cultural awareness. The evaluation of the program is also discussed, with performance indicators such as reduced diabetes incidence and improved referral rates. The student concludes by emphasizing the importance of addressing these social determinants to improve health outcomes in the Inala community. The essay adheres to the assignment brief, providing a detailed community health nursing assessment and suggesting evidence-based interventions.

Running head: COMMUNITY HEALTH NURSING
Importance Community Health Nursing Concept & Principles
Student Name
Student Number
Total Word Count: 1174
Importance Community Health Nursing Concept & Principles
Student Name
Student Number
Total Word Count: 1174
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
COMMUNITY HEALTH NURSING
Part A
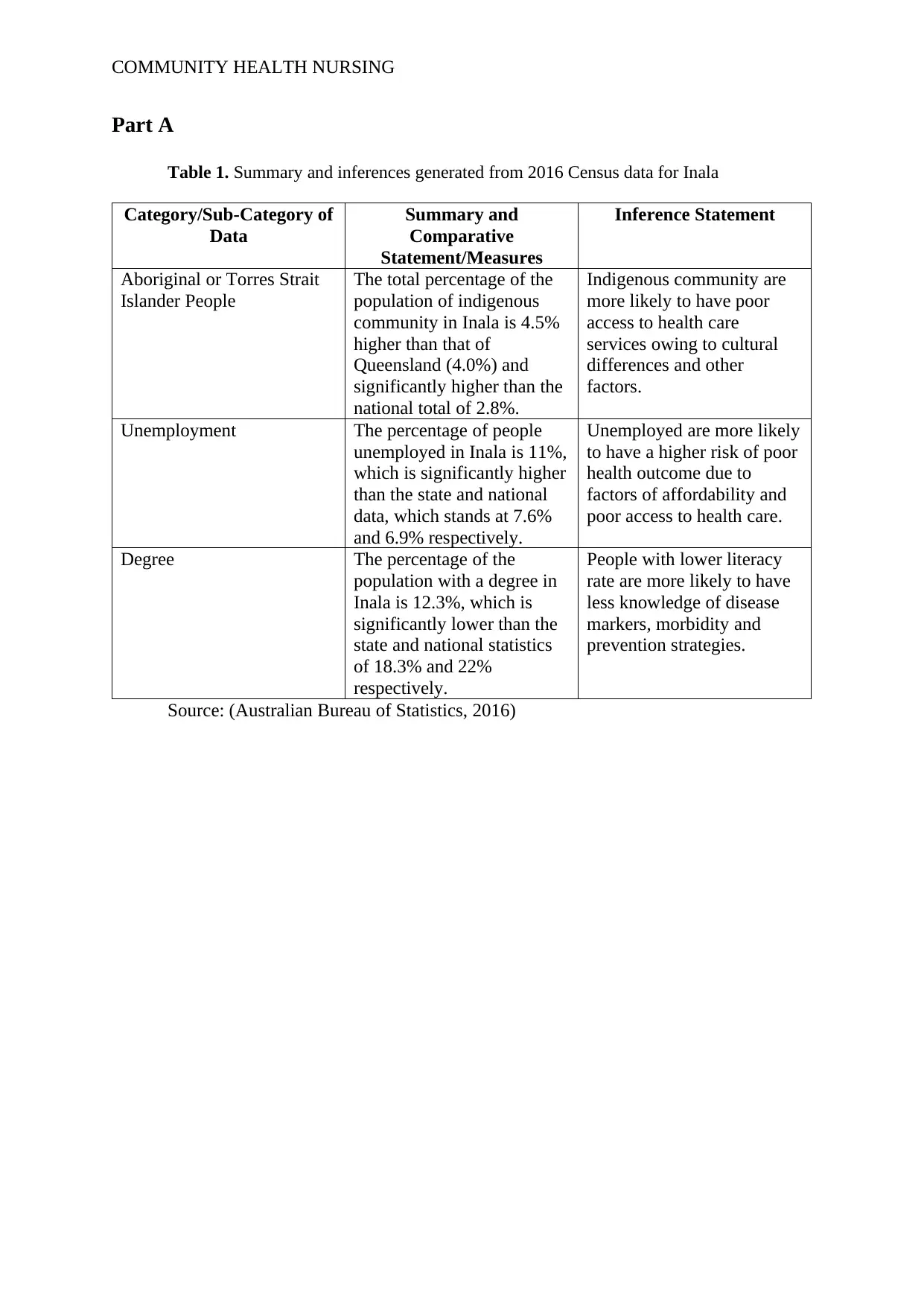
Table 1. Summary and inferences generated from 2016 Census data for Inala
Category/Sub-Category of
Data
Summary and
Comparative
Statement/Measures
Inference Statement
Aboriginal or Torres Strait
Islander People
The total percentage of the
population of indigenous
community in Inala is 4.5%
higher than that of
Queensland (4.0%) and
significantly higher than the
national total of 2.8%.
Indigenous community are
more likely to have poor
access to health care
services owing to cultural
differences and other
factors.
Unemployment The percentage of people
unemployed in Inala is 11%,
which is significantly higher
than the state and national
data, which stands at 7.6%
and 6.9% respectively.
Unemployed are more likely
to have a higher risk of poor
health outcome due to
factors of affordability and
poor access to health care.
Degree The percentage of the
population with a degree in
Inala is 12.3%, which is
significantly lower than the
state and national statistics
of 18.3% and 22%
respectively.
People with lower literacy
rate are more likely to have
less knowledge of disease
markers, morbidity and
prevention strategies.
Source: (Australian Bureau of Statistics, 2016)
Part A
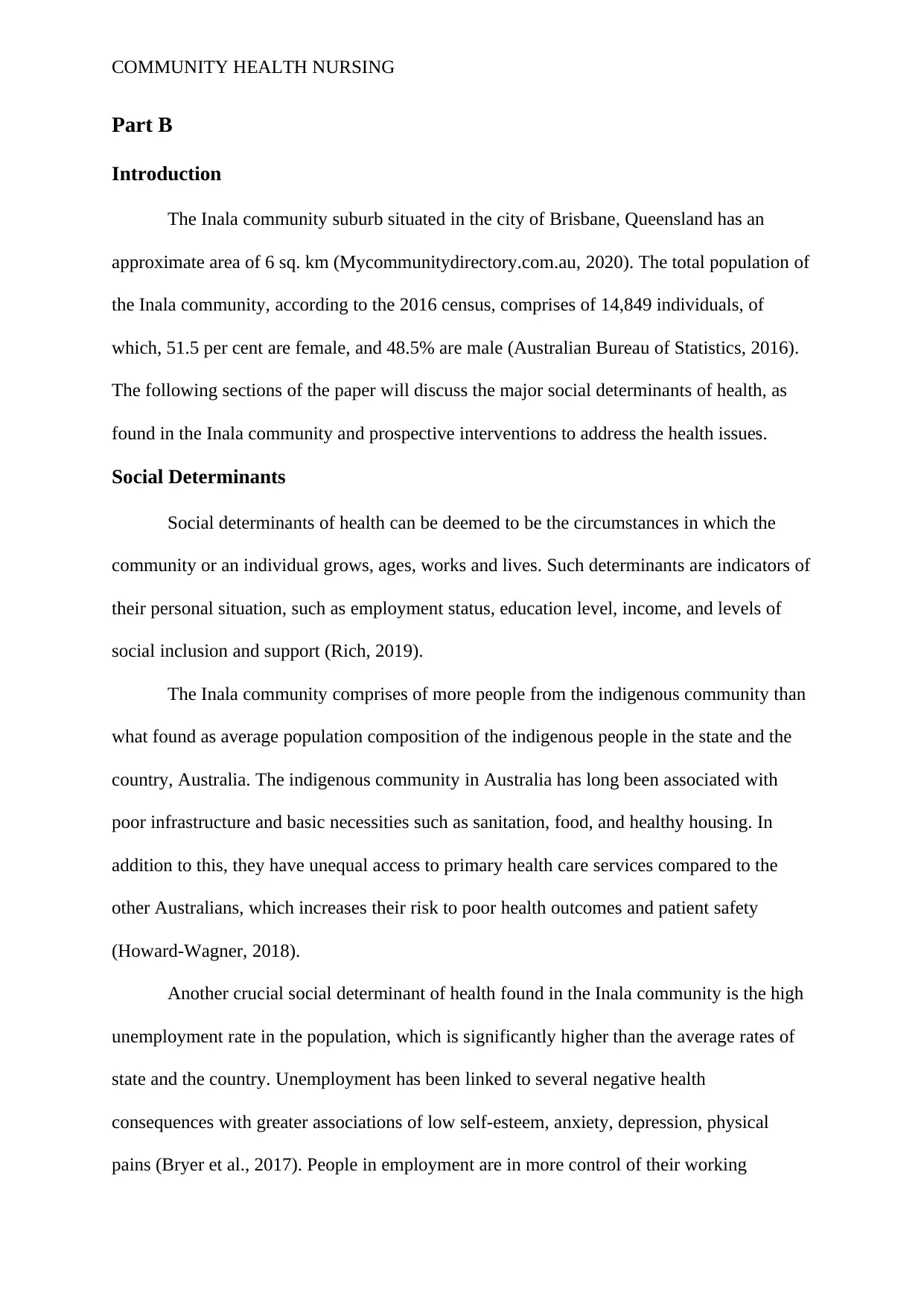
Table 1. Summary and inferences generated from 2016 Census data for Inala
Category/Sub-Category of
Data
Summary and
Comparative
Statement/Measures
Inference Statement
Aboriginal or Torres Strait
Islander People
The total percentage of the
population of indigenous
community in Inala is 4.5%
higher than that of
Queensland (4.0%) and
significantly higher than the
national total of 2.8%.
Indigenous community are
more likely to have poor
access to health care
services owing to cultural
differences and other
factors.
Unemployment The percentage of people
unemployed in Inala is 11%,
which is significantly higher
than the state and national
data, which stands at 7.6%
and 6.9% respectively.
Unemployed are more likely
to have a higher risk of poor
health outcome due to
factors of affordability and
poor access to health care.
Degree The percentage of the
population with a degree in
Inala is 12.3%, which is
significantly lower than the
state and national statistics
of 18.3% and 22%
respectively.
People with lower literacy
rate are more likely to have
less knowledge of disease
markers, morbidity and
prevention strategies.
Source: (Australian Bureau of Statistics, 2016)
COMMUNITY HEALTH NURSING
Part B
Introduction
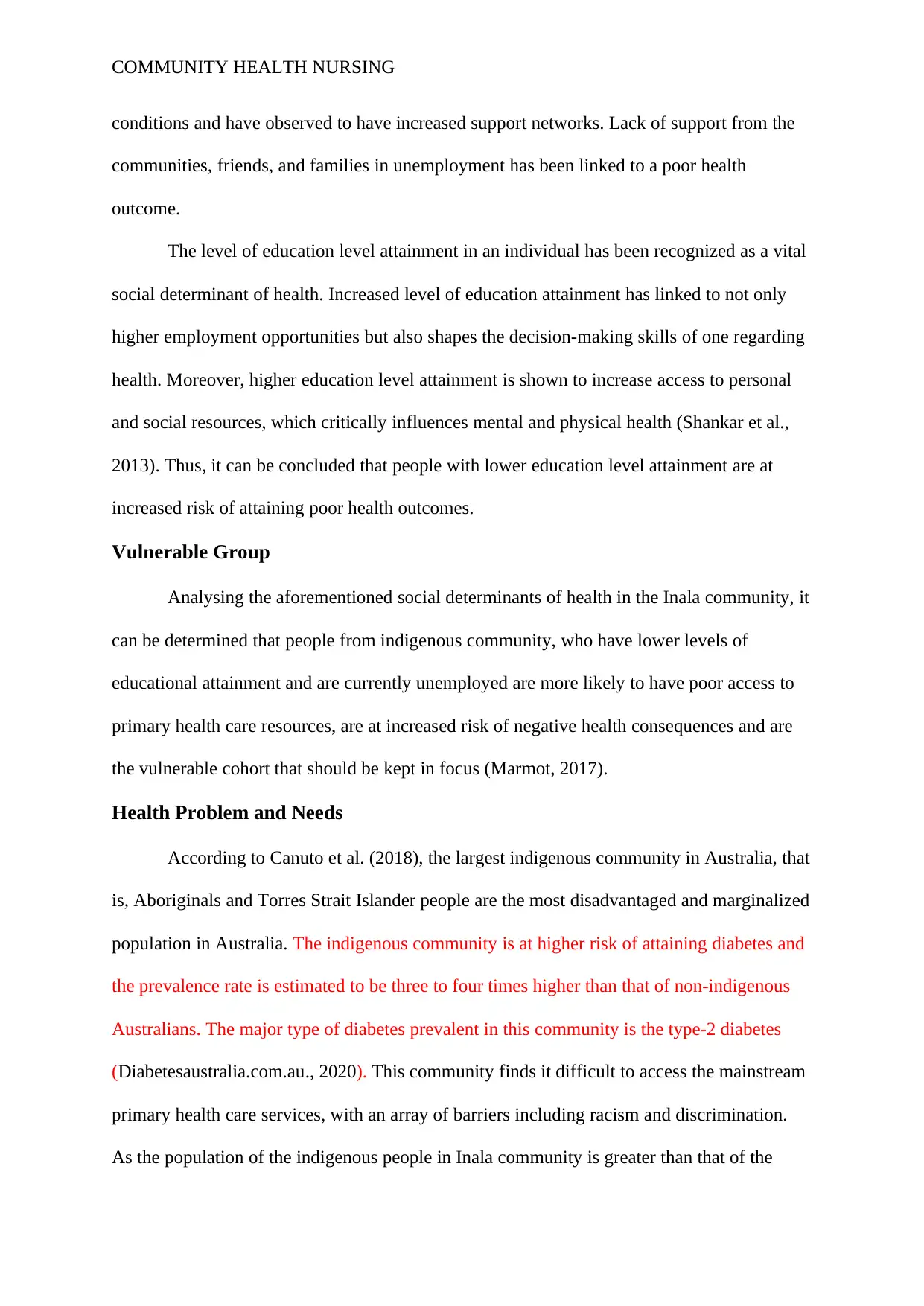
The Inala community suburb situated in the city of Brisbane, Queensland has an
approximate area of 6 sq. km (Mycommunitydirectory.com.au, 2020). The total population of
the Inala community, according to the 2016 census, comprises of 14,849 individuals, of
which, 51.5 per cent are female, and 48.5% are male (Australian Bureau of Statistics, 2016).
The following sections of the paper will discuss the major social determinants of health, as
found in the Inala community and prospective interventions to address the health issues.
Social Determinants
Social determinants of health can be deemed to be the circumstances in which the
community or an individual grows, ages, works and lives. Such determinants are indicators of
their personal situation, such as employment status, education level, income, and levels of
social inclusion and support (Rich, 2019).
The Inala community comprises of more people from the indigenous community than
what found as average population composition of the indigenous people in the state and the
country, Australia. The indigenous community in Australia has long been associated with
poor infrastructure and basic necessities such as sanitation, food, and healthy housing. In
addition to this, they have unequal access to primary health care services compared to the
other Australians, which increases their risk to poor health outcomes and patient safety
(Howard-Wagner, 2018).
Another crucial social determinant of health found in the Inala community is the high
unemployment rate in the population, which is significantly higher than the average rates of
state and the country. Unemployment has been linked to several negative health
consequences with greater associations of low self-esteem, anxiety, depression, physical
pains (Bryer et al., 2017). People in employment are in more control of their working
Part B
Introduction
The Inala community suburb situated in the city of Brisbane, Queensland has an
approximate area of 6 sq. km (Mycommunitydirectory.com.au, 2020). The total population of
the Inala community, according to the 2016 census, comprises of 14,849 individuals, of
which, 51.5 per cent are female, and 48.5% are male (Australian Bureau of Statistics, 2016).
The following sections of the paper will discuss the major social determinants of health, as
found in the Inala community and prospective interventions to address the health issues.
Social Determinants
Social determinants of health can be deemed to be the circumstances in which the
community or an individual grows, ages, works and lives. Such determinants are indicators of
their personal situation, such as employment status, education level, income, and levels of
social inclusion and support (Rich, 2019).
The Inala community comprises of more people from the indigenous community than
what found as average population composition of the indigenous people in the state and the
country, Australia. The indigenous community in Australia has long been associated with
poor infrastructure and basic necessities such as sanitation, food, and healthy housing. In
addition to this, they have unequal access to primary health care services compared to the
other Australians, which increases their risk to poor health outcomes and patient safety
(Howard-Wagner, 2018).
Another crucial social determinant of health found in the Inala community is the high
unemployment rate in the population, which is significantly higher than the average rates of
state and the country. Unemployment has been linked to several negative health
consequences with greater associations of low self-esteem, anxiety, depression, physical
pains (Bryer et al., 2017). People in employment are in more control of their working
COMMUNITY HEALTH NURSING
conditions and have observed to have increased support networks. Lack of support from the
communities, friends, and families in unemployment has been linked to a poor health
outcome.
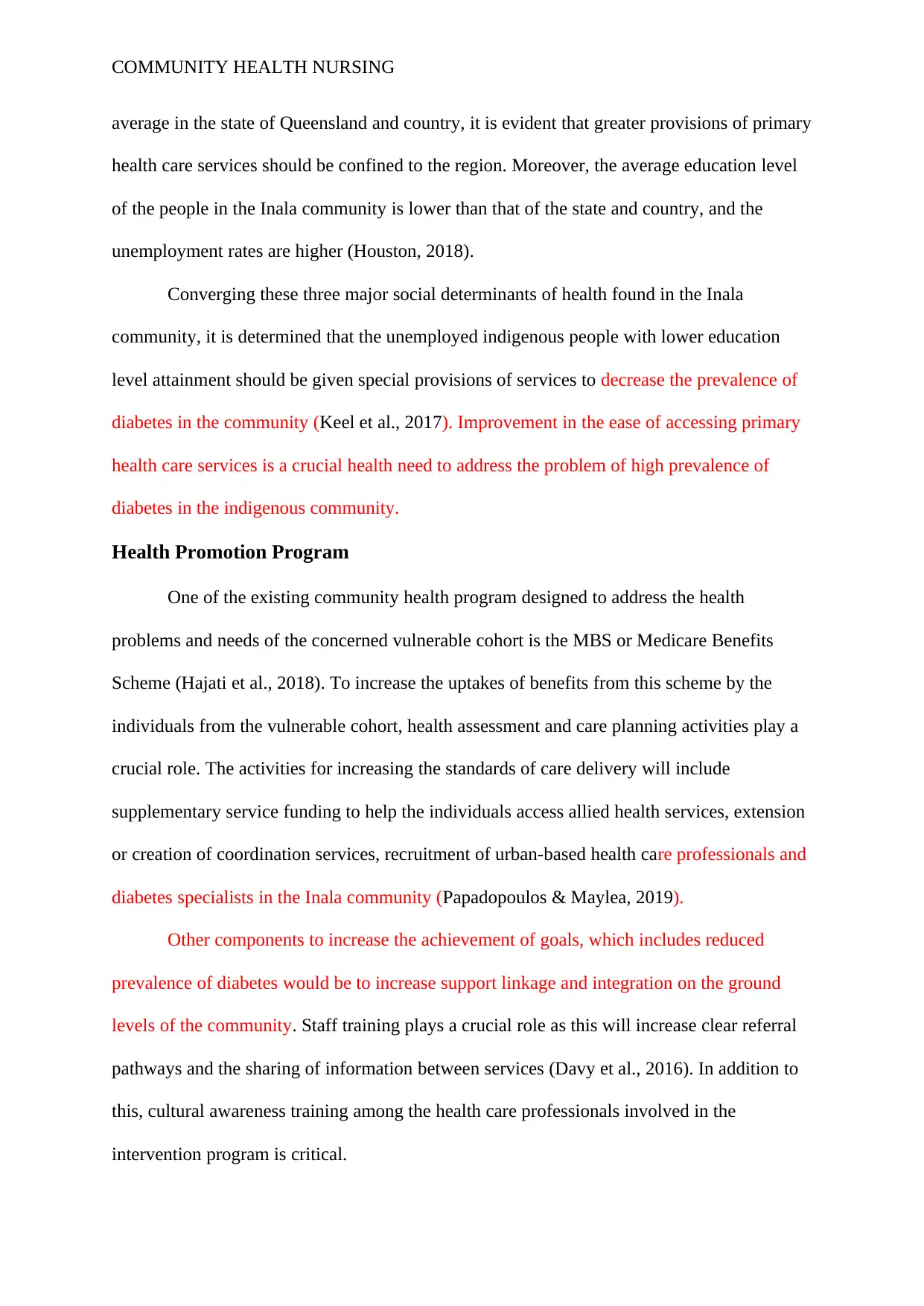
The level of education level attainment in an individual has been recognized as a vital
social determinant of health. Increased level of education attainment has linked to not only
higher employment opportunities but also shapes the decision-making skills of one regarding
health. Moreover, higher education level attainment is shown to increase access to personal
and social resources, which critically influences mental and physical health (Shankar et al.,
2013). Thus, it can be concluded that people with lower education level attainment are at
increased risk of attaining poor health outcomes.
Vulnerable Group
Analysing the aforementioned social determinants of health in the Inala community, it
can be determined that people from indigenous community, who have lower levels of
educational attainment and are currently unemployed are more likely to have poor access to
primary health care resources, are at increased risk of negative health consequences and are
the vulnerable cohort that should be kept in focus (Marmot, 2017).
Health Problem and Needs
According to Canuto et al. (2018), the largest indigenous community in Australia, that
is, Aboriginals and Torres Strait Islander people are the most disadvantaged and marginalized
population in Australia. The indigenous community is at higher risk of attaining diabetes and
the prevalence rate is estimated to be three to four times higher than that of non-indigenous
Australians. The major type of diabetes prevalent in this community is the type-2 diabetes
(Diabetesaustralia.com.au., 2020). This community finds it difficult to access the mainstream
primary health care services, with an array of barriers including racism and discrimination.
As the population of the indigenous people in Inala community is greater than that of the
conditions and have observed to have increased support networks. Lack of support from the
communities, friends, and families in unemployment has been linked to a poor health
outcome.
The level of education level attainment in an individual has been recognized as a vital
social determinant of health. Increased level of education attainment has linked to not only
higher employment opportunities but also shapes the decision-making skills of one regarding
health. Moreover, higher education level attainment is shown to increase access to personal
and social resources, which critically influences mental and physical health (Shankar et al.,
2013). Thus, it can be concluded that people with lower education level attainment are at
increased risk of attaining poor health outcomes.
Vulnerable Group
Analysing the aforementioned social determinants of health in the Inala community, it
can be determined that people from indigenous community, who have lower levels of
educational attainment and are currently unemployed are more likely to have poor access to
primary health care resources, are at increased risk of negative health consequences and are
the vulnerable cohort that should be kept in focus (Marmot, 2017).
Health Problem and Needs
According to Canuto et al. (2018), the largest indigenous community in Australia, that
is, Aboriginals and Torres Strait Islander people are the most disadvantaged and marginalized
population in Australia. The indigenous community is at higher risk of attaining diabetes and
the prevalence rate is estimated to be three to four times higher than that of non-indigenous
Australians. The major type of diabetes prevalent in this community is the type-2 diabetes
(Diabetesaustralia.com.au., 2020). This community finds it difficult to access the mainstream
primary health care services, with an array of barriers including racism and discrimination.
As the population of the indigenous people in Inala community is greater than that of the
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
COMMUNITY HEALTH NURSING
average in the state of Queensland and country, it is evident that greater provisions of primary
health care services should be confined to the region. Moreover, the average education level
of the people in the Inala community is lower than that of the state and country, and the
unemployment rates are higher (Houston, 2018).
Converging these three major social determinants of health found in the Inala
community, it is determined that the unemployed indigenous people with lower education
level attainment should be given special provisions of services to decrease the prevalence of
diabetes in the community (Keel et al., 2017). Improvement in the ease of accessing primary
health care services is a crucial health need to address the problem of high prevalence of
diabetes in the indigenous community.
Health Promotion Program
One of the existing community health program designed to address the health
problems and needs of the concerned vulnerable cohort is the MBS or Medicare Benefits
Scheme (Hajati et al., 2018). To increase the uptakes of benefits from this scheme by the
individuals from the vulnerable cohort, health assessment and care planning activities play a
crucial role. The activities for increasing the standards of care delivery will include
supplementary service funding to help the individuals access allied health services, extension
or creation of coordination services, recruitment of urban-based health care professionals and
diabetes specialists in the Inala community (Papadopoulos & Maylea, 2019).
Other components to increase the achievement of goals, which includes reduced
prevalence of diabetes would be to increase support linkage and integration on the ground
levels of the community. Staff training plays a crucial role as this will increase clear referral
pathways and the sharing of information between services (Davy et al., 2016). In addition to
this, cultural awareness training among the health care professionals involved in the
intervention program is critical.
average in the state of Queensland and country, it is evident that greater provisions of primary
health care services should be confined to the region. Moreover, the average education level
of the people in the Inala community is lower than that of the state and country, and the
unemployment rates are higher (Houston, 2018).
Converging these three major social determinants of health found in the Inala
community, it is determined that the unemployed indigenous people with lower education
level attainment should be given special provisions of services to decrease the prevalence of
diabetes in the community (Keel et al., 2017). Improvement in the ease of accessing primary
health care services is a crucial health need to address the problem of high prevalence of
diabetes in the indigenous community.
Health Promotion Program
One of the existing community health program designed to address the health
problems and needs of the concerned vulnerable cohort is the MBS or Medicare Benefits
Scheme (Hajati et al., 2018). To increase the uptakes of benefits from this scheme by the
individuals from the vulnerable cohort, health assessment and care planning activities play a
crucial role. The activities for increasing the standards of care delivery will include
supplementary service funding to help the individuals access allied health services, extension
or creation of coordination services, recruitment of urban-based health care professionals and
diabetes specialists in the Inala community (Papadopoulos & Maylea, 2019).
Other components to increase the achievement of goals, which includes reduced
prevalence of diabetes would be to increase support linkage and integration on the ground
levels of the community. Staff training plays a crucial role as this will increase clear referral
pathways and the sharing of information between services (Davy et al., 2016). In addition to
this, cultural awareness training among the health care professionals involved in the
intervention program is critical.
COMMUNITY HEALTH NURSING
Evaluation and monitoring of the programme indicators are crucial to determine the
efficiency of the program. A decrease in the diabetes incidence, morbidity, increase in
diabetic health education, higher rates of competent referrals is few of the performance
indicator to adjudge the success of the program (Porterfield et al., 2018).
Conclusion
The above paper analysed the demographics of the Inala community and compared
the statistics with their corresponding state and national level data. The major social
determinants of health recognized in this community are indigenous status, unemployment
rates and lower education level. It is reported that the indigenous community are at high risk
of attaining diabetes. To address this health impact of these social determinants of health, a
health promotion plan comprising of several components and health activities will be
implemented to increase the uptake of benefits of the Medicare Benefits Scheme specially
designed for the concerned vulnerable cohort.
Evaluation and monitoring of the programme indicators are crucial to determine the
efficiency of the program. A decrease in the diabetes incidence, morbidity, increase in
diabetic health education, higher rates of competent referrals is few of the performance
indicator to adjudge the success of the program (Porterfield et al., 2018).
Conclusion
The above paper analysed the demographics of the Inala community and compared
the statistics with their corresponding state and national level data. The major social
determinants of health recognized in this community are indigenous status, unemployment
rates and lower education level. It is reported that the indigenous community are at high risk
of attaining diabetes. To address this health impact of these social determinants of health, a
health promotion plan comprising of several components and health activities will be
implemented to increase the uptake of benefits of the Medicare Benefits Scheme specially
designed for the concerned vulnerable cohort.
COMMUNITY HEALTH NURSING
References
Australian Bureau of Statistics (2016). Abs.gov.au. 2016 Census. 1 March 2020
https://www.abs.gov.au/websitedbs/censushome.nsf/home/2016
Bryer, M., Torres Stone, R. A., Kostova, Z., & Logan, D. G. (2017). There's More to Young
Adult Unemployment Than Mental Health: What Else to Look For. Psychiatry
Information in Brief, 14(7), 1.
Canuto, K., Brown, A., Wittert, G., & Harfield, S. (2018). Understanding the utilization of
primary health care services by Indigenous men: a systematic review. BMC public
health, 18(1), 1198. 10.1186/s12889-018-6093-2
Davy, C., Harfield, S., McArthur, A., Munn, Z., & Brown, A. (2016). Access to primary
health care services for Indigenous peoples: a framework synthesis. International
journal for equity in health, 15(1), 163. https://doi.org/10.1186/s12939-016-0450-5
Diabetesaustralia.com.au. Aboriginal & Torres Strait Islander people.
(2020). Diabetesaustralia.com.au. Retrieved 4 March 2020, from
https://www.diabetesaustralia.com.au/aboriginal-and-torres-strait-islanders
Hajati, F., Atlantis, E., Bell, K. J., & Girosi, F. (2018). Patterns and trends of potentially
inappropriate high-density lipoprotein cholesterol testing in Australian adults at high
risk of cardiovascular disease from 2008 to 2014: analysis of linked individual patient
data from the Australian Medicare Benefits Schedule and Pharmaceutical Benefits
Scheme. BMJ open, 8(3), e019041.
Houston, A. G. (2018). Exploring the cultural appropriateness and usefulness of an mHealth
program for optimal infant feeding in an urban Aboriginal and Torres Strait Islander
Health Service: Growing healthy at Inala (Doctoral dissertation).
References
Australian Bureau of Statistics (2016). Abs.gov.au. 2016 Census. 1 March 2020
https://www.abs.gov.au/websitedbs/censushome.nsf/home/2016
Bryer, M., Torres Stone, R. A., Kostova, Z., & Logan, D. G. (2017). There's More to Young
Adult Unemployment Than Mental Health: What Else to Look For. Psychiatry
Information in Brief, 14(7), 1.
Canuto, K., Brown, A., Wittert, G., & Harfield, S. (2018). Understanding the utilization of
primary health care services by Indigenous men: a systematic review. BMC public
health, 18(1), 1198. 10.1186/s12889-018-6093-2
Davy, C., Harfield, S., McArthur, A., Munn, Z., & Brown, A. (2016). Access to primary
health care services for Indigenous peoples: a framework synthesis. International
journal for equity in health, 15(1), 163. https://doi.org/10.1186/s12939-016-0450-5
Diabetesaustralia.com.au. Aboriginal & Torres Strait Islander people.
(2020). Diabetesaustralia.com.au. Retrieved 4 March 2020, from
https://www.diabetesaustralia.com.au/aboriginal-and-torres-strait-islanders
Hajati, F., Atlantis, E., Bell, K. J., & Girosi, F. (2018). Patterns and trends of potentially
inappropriate high-density lipoprotein cholesterol testing in Australian adults at high
risk of cardiovascular disease from 2008 to 2014: analysis of linked individual patient
data from the Australian Medicare Benefits Schedule and Pharmaceutical Benefits
Scheme. BMJ open, 8(3), e019041.
Houston, A. G. (2018). Exploring the cultural appropriateness and usefulness of an mHealth
program for optimal infant feeding in an urban Aboriginal and Torres Strait Islander
Health Service: Growing healthy at Inala (Doctoral dissertation).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
COMMUNITY HEALTH NURSING
Howard-Wagner, D. (2018). Governance of indigenous policy in the neo-liberal age:
indigenous disadvantage and the intersecting of paternalism and neo-liberalism as a
racial project. Ethnic and Racial Studies, 41(7), 1332-1351.
Keel, S., Foreman, J., Xie, J., Van Wijngaarden, P., Taylor, H. R., & Dirani, M. (2017). The
prevalence of self-reported diabetes in the Australian national eye health
survey. PLoS One, 12(1).
Marmot, M. G. (2017). Dignity, social investment and the Indigenous health gap. Medical
Journal of Australia, 207(1), 20-21.
Mycommunitydirectory.com.au. (2020). About Inala Community - My Community Directory.
[online] 1 Mar. 2020
https://www.mycommunitydirectory.com.au/About/Suburb/Queensland/Inala
Papadopoulos, A., & Maylea, C. (2019). Medicare Funded Mental Health Social Work:
Better Access to What?. Australian Social Work, 1-13.
Porterfield, D., Jacobs, S., Farrell, K., Yarnoff, B., Strazza, K., Elkins, W., ... & AB Peterson,
G. (2018). Evaluation of the Medicaid Coverage for the National Diabetes Prevention
Program Demonstration Project.
Rich, M. (2019). Teaching Social Determinants of Health. In Health Disparities (pp. 221-
236). Springer, Cham.
Shankar, J., Ip, E., Khalema, E., Couture, J., Tan, S., Zulla, R. T., & Lam, G. (2013).
Education as a social determinant of health: issues facing indigenous and visible
minority students in postsecondary education in western Canada. International
journal of environmental research and public health, 10(9), 3908-3929.
10.3390/ijerph10093908
Www1.health.gov.au. (2020). [online] 1 March 2020,
https://www1.health.gov.au/internet/main/publishing.nsf/Content/09AEEA5F377AEB
Howard-Wagner, D. (2018). Governance of indigenous policy in the neo-liberal age:
indigenous disadvantage and the intersecting of paternalism and neo-liberalism as a
racial project. Ethnic and Racial Studies, 41(7), 1332-1351.
Keel, S., Foreman, J., Xie, J., Van Wijngaarden, P., Taylor, H. R., & Dirani, M. (2017). The
prevalence of self-reported diabetes in the Australian national eye health
survey. PLoS One, 12(1).
Marmot, M. G. (2017). Dignity, social investment and the Indigenous health gap. Medical
Journal of Australia, 207(1), 20-21.
Mycommunitydirectory.com.au. (2020). About Inala Community - My Community Directory.
[online] 1 Mar. 2020
https://www.mycommunitydirectory.com.au/About/Suburb/Queensland/Inala
Papadopoulos, A., & Maylea, C. (2019). Medicare Funded Mental Health Social Work:
Better Access to What?. Australian Social Work, 1-13.
Porterfield, D., Jacobs, S., Farrell, K., Yarnoff, B., Strazza, K., Elkins, W., ... & AB Peterson,
G. (2018). Evaluation of the Medicaid Coverage for the National Diabetes Prevention
Program Demonstration Project.
Rich, M. (2019). Teaching Social Determinants of Health. In Health Disparities (pp. 221-
236). Springer, Cham.
Shankar, J., Ip, E., Khalema, E., Couture, J., Tan, S., Zulla, R. T., & Lam, G. (2013).
Education as a social determinant of health: issues facing indigenous and visible
minority students in postsecondary education in western Canada. International
journal of environmental research and public health, 10(9), 3908-3929.
10.3390/ijerph10093908
Www1.health.gov.au. (2020). [online] 1 March 2020,
https://www1.health.gov.au/internet/main/publishing.nsf/Content/09AEEA5F377AEB

COMMUNITY HEALTH NURSING
B5CA257F1C00159135/$File/Indigenous%20Australians%20Health%20Programme
%20Guidelines.pdf [Accessed 1 Mar. 2020].
B5CA257F1C00159135/$File/Indigenous%20Australians%20Health%20Programme
%20Guidelines.pdf [Accessed 1 Mar. 2020].
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





