Community Health Promotion Report: Health Promotion Strategies
VerifiedAdded on 2022/12/27
|7
|2200
|50
Report
AI Summary
This report provides a comprehensive analysis of obesity within the context of community health promotion. It begins by defining obesity, outlining Body Mass Index (BMI) categories, and detailing their associated risks of chronic diseases. The report then examines the impact of obesity on morbidity and mortality in Australian adults, highlighting the significant health burden. Furthermore, it explores how education level and family income influence obesity risk, underscoring the role of social determinants. The report identifies vulnerable subgroups in Australia with higher obesity rates, providing statistical comparisons to the general population. Finally, the report accesses and analyzes a research study, outlining its aim, design, intervention components, the role of nurses, primary outcomes, and weight loss results, thereby illustrating evidence-based approaches to obesity management. The report utilizes scholarly literature to support its arguments and findings, providing a well-rounded perspective on this critical public health issue.
Community Health
Promotion Report
Promotion Report
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Table of Contents
MAIN BODY...................................................................................................................................1
1. Defining obesity as well as outlining distinct categories of Body Mass Index along with the
ways each category related to risk level of chronic disease.........................................................1
2. Discussion of impact of obesity within Australia on morbidity and mortality in adults.........1
3. Explaining how education level as well as family income impacts towards risk of obesity...2
4. Identification and description of vulnerable sub-group of people in Australia in which
obesity rates are higher than general population of Australia and providing statistics in
percentage comparing rates of obesity within vulnerable subgroup of rates of obesity in
general population........................................................................................................................2
5. Accessing full text research and responding to questions:......................................................3
a. Outlining aim of study and study design..................................................................................3
b. Brief description of components of POWER+F as well as POWER+R arms of intervention 3
c. Describing role of nurses within delivering intervention.........................................................3
d. Describing primary outcome and how effectiveness of intervention was evaluated...............3
e. Outlining weight loss outcomes at 12 months on each group..................................................4
REFERENCES................................................................................................................................5
MAIN BODY...................................................................................................................................1
1. Defining obesity as well as outlining distinct categories of Body Mass Index along with the
ways each category related to risk level of chronic disease.........................................................1
2. Discussion of impact of obesity within Australia on morbidity and mortality in adults.........1
3. Explaining how education level as well as family income impacts towards risk of obesity...2
4. Identification and description of vulnerable sub-group of people in Australia in which
obesity rates are higher than general population of Australia and providing statistics in
percentage comparing rates of obesity within vulnerable subgroup of rates of obesity in
general population........................................................................................................................2
5. Accessing full text research and responding to questions:......................................................3
a. Outlining aim of study and study design..................................................................................3
b. Brief description of components of POWER+F as well as POWER+R arms of intervention 3
c. Describing role of nurses within delivering intervention.........................................................3
d. Describing primary outcome and how effectiveness of intervention was evaluated...............3
e. Outlining weight loss outcomes at 12 months on each group..................................................4
REFERENCES................................................................................................................................5
MAIN BODY
1. Defining obesity as well as outlining distinct categories of Body Mass Index along with the
ways each category related to risk level of chronic disease
The term obesity is said to abnormal or additional fat accumulation which reflect a risk to
health of an individual (Kumanyika, 2019). It is multifactorial which depends on genetic together
with behavioural factors.
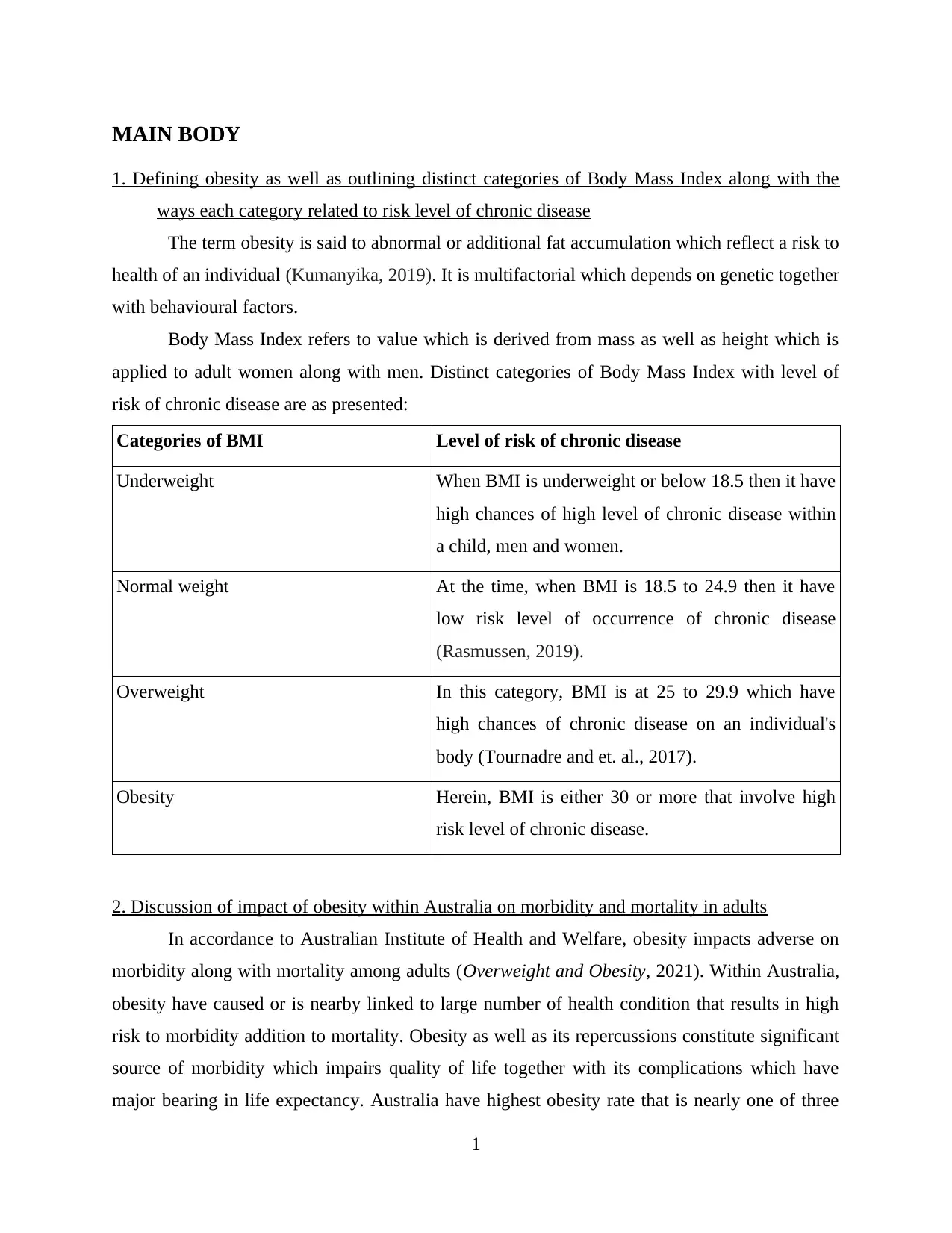
Body Mass Index refers to value which is derived from mass as well as height which is
applied to adult women along with men. Distinct categories of Body Mass Index with level of
risk of chronic disease are as presented:
Categories of BMI Level of risk of chronic disease
Underweight When BMI is underweight or below 18.5 then it have
high chances of high level of chronic disease within
a child, men and women.
Normal weight At the time, when BMI is 18.5 to 24.9 then it have
low risk level of occurrence of chronic disease
(Rasmussen, 2019).
Overweight In this category, BMI is at 25 to 29.9 which have
high chances of chronic disease on an individual's
body (Tournadre and et. al., 2017).
Obesity Herein, BMI is either 30 or more that involve high
risk level of chronic disease.
2. Discussion of impact of obesity within Australia on morbidity and mortality in adults
In accordance to Australian Institute of Health and Welfare, obesity impacts adverse on
morbidity along with mortality among adults (Overweight and Obesity, 2021). Within Australia,
obesity have caused or is nearby linked to large number of health condition that results in high
risk to morbidity addition to mortality. Obesity as well as its repercussions constitute significant
source of morbidity which impairs quality of life together with its complications which have
major bearing in life expectancy. Australia have highest obesity rate that is nearly one of three
1
1. Defining obesity as well as outlining distinct categories of Body Mass Index along with the
ways each category related to risk level of chronic disease
The term obesity is said to abnormal or additional fat accumulation which reflect a risk to
health of an individual (Kumanyika, 2019). It is multifactorial which depends on genetic together
with behavioural factors.
Body Mass Index refers to value which is derived from mass as well as height which is
applied to adult women along with men. Distinct categories of Body Mass Index with level of
risk of chronic disease are as presented:
Categories of BMI Level of risk of chronic disease
Underweight When BMI is underweight or below 18.5 then it have
high chances of high level of chronic disease within
a child, men and women.
Normal weight At the time, when BMI is 18.5 to 24.9 then it have
low risk level of occurrence of chronic disease
(Rasmussen, 2019).
Overweight In this category, BMI is at 25 to 29.9 which have
high chances of chronic disease on an individual's
body (Tournadre and et. al., 2017).
Obesity Herein, BMI is either 30 or more that involve high
risk level of chronic disease.
2. Discussion of impact of obesity within Australia on morbidity and mortality in adults
In accordance to Australian Institute of Health and Welfare, obesity impacts adverse on
morbidity along with mortality among adults (Overweight and Obesity, 2021). Within Australia,
obesity have caused or is nearby linked to large number of health condition that results in high
risk to morbidity addition to mortality. Obesity as well as its repercussions constitute significant
source of morbidity which impairs quality of life together with its complications which have
major bearing in life expectancy. Australia have highest obesity rate that is nearly one of three
1
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

adults are facing obese. It is found that 40 per cent of Australian as well as 50 per cent of PCVD
mortality is concerned with overweight among adults.
Being overweight results in negative impacts on morbidity as it enhances related illnesses
including type 2 diabetes, osteoarthritis, cardiovascular disease and certain kinds of cancer. At
least 140 adult Australians die everyday from obesity associated disease which amounts to
approx 50000 people a year (de Siqueira and et. al., 2020). Furthermore, obesity is seen as to
have wider impact on people that are men aged over 75 along with women aged among 60 to 75
years. In other words, within Australia obesity impacts widely on morbidity along with mortality
among adults as it is linked with poorer mental health results as well as reduced quality of life.
3. Explaining how education level as well as family income impacts towards risk of obesity
Education level have huge implications on risk of obesity as an educated person takes
care of self and control their body fat. Positive effect of level of education on obesity is
determined to be attributed towards wider access to information about health as well as improves
ability for handling lifestyle choices (Park, Chooand Chang, 2019). For instance, with rise in
education level, rate of obesity among population of Australia drops. It is seen that people who
do not finish their school have high obesity level at 35.5 percent that is followed by school
graduates and college graduate. Education about physical activities results in enhancing total
energy expenditure among people which assist them to stay in balance or lose weight as more as
they do not eat for the purpose of compensating additional calories they burn. Health education
programs plays key role in improving knowledge among people about ways to manage their
weight and reduce risk of obesity.
Among men, particularly in Australia, obesity prevalence are similar at all levels of
income. In contrary. Non Hispanic along with Mexican American men with high income have
high level of obese in contrary to low income. At same time, it is seen that high income people
have less risk of obesity as they spend on healthy eating including dietary food and others that
plays great role in managing obese among them (D’Innocenzo, Biagi and Lanari, 2019). On an
average, rate of obesity enhances with income level, flatten out along with decrease gain for high
income population. Till 1990s, relationship among level of income and high adult obesity rate
was not observable. However, after this, correlation among obesity rate and that of household
income have grown steadily. For example, in the decade after 2004, obesity enhanced to one
percent on average within top wealthiest nations.
2
mortality is concerned with overweight among adults.
Being overweight results in negative impacts on morbidity as it enhances related illnesses
including type 2 diabetes, osteoarthritis, cardiovascular disease and certain kinds of cancer. At
least 140 adult Australians die everyday from obesity associated disease which amounts to
approx 50000 people a year (de Siqueira and et. al., 2020). Furthermore, obesity is seen as to
have wider impact on people that are men aged over 75 along with women aged among 60 to 75
years. In other words, within Australia obesity impacts widely on morbidity along with mortality
among adults as it is linked with poorer mental health results as well as reduced quality of life.
3. Explaining how education level as well as family income impacts towards risk of obesity
Education level have huge implications on risk of obesity as an educated person takes
care of self and control their body fat. Positive effect of level of education on obesity is
determined to be attributed towards wider access to information about health as well as improves
ability for handling lifestyle choices (Park, Chooand Chang, 2019). For instance, with rise in
education level, rate of obesity among population of Australia drops. It is seen that people who
do not finish their school have high obesity level at 35.5 percent that is followed by school
graduates and college graduate. Education about physical activities results in enhancing total
energy expenditure among people which assist them to stay in balance or lose weight as more as
they do not eat for the purpose of compensating additional calories they burn. Health education
programs plays key role in improving knowledge among people about ways to manage their
weight and reduce risk of obesity.
Among men, particularly in Australia, obesity prevalence are similar at all levels of
income. In contrary. Non Hispanic along with Mexican American men with high income have
high level of obese in contrary to low income. At same time, it is seen that high income people
have less risk of obesity as they spend on healthy eating including dietary food and others that
plays great role in managing obese among them (D’Innocenzo, Biagi and Lanari, 2019). On an
average, rate of obesity enhances with income level, flatten out along with decrease gain for high
income population. Till 1990s, relationship among level of income and high adult obesity rate
was not observable. However, after this, correlation among obesity rate and that of household
income have grown steadily. For example, in the decade after 2004, obesity enhanced to one
percent on average within top wealthiest nations.
2
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4. Identification and description of vulnerable sub-group of people in Australia in which obesity
rates are higher than general population of Australia and providing statistics in percentage
comparing rates of obesity within vulnerable subgroup of rates of obesity in general
population
Vulnerable sub-group refers to groups of population which faces higher risk of social
exclusion, violence, poverty as well as discrimination against general population (Gefen, 2017).
Low socio-economic status population is vulnerable sub group in Australia among which
there is high obesity level. In the year 2019 and 20, one of four low economic status people were
overweight. Because of high prevalence along with adverse consequences, obesity within the
subgroup continues to be wider than general population (Jankauskiene and Baceviciene, 2019).
In contrary, it is analysed that in 2019-20, around 2 in 3 Australians that are aged 18 or more
were overweight which was near to 67 per cent. Of all, children and adolescent that are aged 2 to
17 were obese and 8.2% were facing obesity that belong to general population. It is also
determined that obesity is wider common within older groups as 16% adults between 18 to 24
were obese in comparison to 41% adults among 65 to 74 years.
5. Accessing full text research and responding to questions:
a. Outlining aim of study and study design
Aim of the study conducted by Little and Et. Al. (2016) is to estimate effectiveness along
with cost effectiveness associated to an internet based behavioural intervention that is POWER+
combined with brief practice nurse support within primary care. The study design of the research
is randomised controlled trial through which participants are randomly assigned to conduct the
study.
b. Brief description of components of POWER+F as well as POWER+R arms of intervention
POWeR+F is described as web based intervention as well as face to face nurse support in
which nurses contact over some months (Timofeeva, Ofial and Mayr, 2018). Key component of
POWeR+F arm of intervention is web based technology along with support of nurse. Likewise
POWeR+R is a session, weight management and web based intervention which last to six
months.
3
rates are higher than general population of Australia and providing statistics in percentage
comparing rates of obesity within vulnerable subgroup of rates of obesity in general
population
Vulnerable sub-group refers to groups of population which faces higher risk of social
exclusion, violence, poverty as well as discrimination against general population (Gefen, 2017).
Low socio-economic status population is vulnerable sub group in Australia among which
there is high obesity level. In the year 2019 and 20, one of four low economic status people were
overweight. Because of high prevalence along with adverse consequences, obesity within the
subgroup continues to be wider than general population (Jankauskiene and Baceviciene, 2019).
In contrary, it is analysed that in 2019-20, around 2 in 3 Australians that are aged 18 or more
were overweight which was near to 67 per cent. Of all, children and adolescent that are aged 2 to
17 were obese and 8.2% were facing obesity that belong to general population. It is also
determined that obesity is wider common within older groups as 16% adults between 18 to 24
were obese in comparison to 41% adults among 65 to 74 years.
5. Accessing full text research and responding to questions:
a. Outlining aim of study and study design
Aim of the study conducted by Little and Et. Al. (2016) is to estimate effectiveness along
with cost effectiveness associated to an internet based behavioural intervention that is POWER+
combined with brief practice nurse support within primary care. The study design of the research
is randomised controlled trial through which participants are randomly assigned to conduct the
study.
b. Brief description of components of POWER+F as well as POWER+R arms of intervention
POWeR+F is described as web based intervention as well as face to face nurse support in
which nurses contact over some months (Timofeeva, Ofial and Mayr, 2018). Key component of
POWeR+F arm of intervention is web based technology along with support of nurse. Likewise
POWeR+R is a session, weight management and web based intervention which last to six
months.
3
c. Describing role of nurses within delivering intervention
Key role of nurse in delivering intervention is to provide proper care for managing
obesity with primary care (Černelič-Bizjak, 2019). At same time, other objective is to protect as
well as promote health among working population. Nurses also have role to control infection,
provide mobility therapy, provide sleep pattern control and managing diet in delivering effective
intervention. More than this, nurses have role to deliver intervention for the purpose of
improving results of health and feel engaged together with rewarded through success of patients
in enhancing their physical practices.
d. Describing primary outcome and how effectiveness of intervention was evaluated
Primary outcome is that weight loss could be maintained among certain people through
using novel written material with occasional brief nurse follow-up. Effectiveness of intervention
was evaluated by maintaining proper record of weight reductions with the help of web based
behavioural program.
e. Outlining weight loss outcomes at 12 months on each group
Weight loss averaged on 12 months was recorded in 666 or 81% participants. It is
analysed that control group have lost around 3 kg in 12 months which is calculated by the
formula crude mean weight is baseline 104.38 kg [SD 21.11; n=270). Primary imputed analysis
have showed that patients with POWeR+ Group have attained additional weight reduction of 1.5
kg. Moreover, patients with POWeR+R Group have accomplished 1.3 kg. With this, it can be
said that around 21% patients within control group have maintained clinically important weight
reduction at month 12 in contrary to 29% patients in POWeR+F group.
4
Key role of nurse in delivering intervention is to provide proper care for managing
obesity with primary care (Černelič-Bizjak, 2019). At same time, other objective is to protect as
well as promote health among working population. Nurses also have role to control infection,
provide mobility therapy, provide sleep pattern control and managing diet in delivering effective
intervention. More than this, nurses have role to deliver intervention for the purpose of
improving results of health and feel engaged together with rewarded through success of patients
in enhancing their physical practices.
d. Describing primary outcome and how effectiveness of intervention was evaluated
Primary outcome is that weight loss could be maintained among certain people through
using novel written material with occasional brief nurse follow-up. Effectiveness of intervention
was evaluated by maintaining proper record of weight reductions with the help of web based
behavioural program.
e. Outlining weight loss outcomes at 12 months on each group
Weight loss averaged on 12 months was recorded in 666 or 81% participants. It is
analysed that control group have lost around 3 kg in 12 months which is calculated by the
formula crude mean weight is baseline 104.38 kg [SD 21.11; n=270). Primary imputed analysis
have showed that patients with POWeR+ Group have attained additional weight reduction of 1.5
kg. Moreover, patients with POWeR+R Group have accomplished 1.3 kg. With this, it can be
said that around 21% patients within control group have maintained clinically important weight
reduction at month 12 in contrary to 29% patients in POWeR+F group.
4
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
REFERENCES
Books and Journals:
Černelič-Bizjak, M., 2019. Changes in body image during a 6-month lifestyle behaviour
intervention in a sample of overweight and obese individuals. Journal of bodywork and
movement therapies. 23(3). pp.515-520.
D’Innocenzo, S., Biagi, C. and Lanari, M., 2019. Obesity and the mediterranean diet: a review of
evidence of the role and sustainability of the mediterranean diet. Nutrients. 11(6). p.1306.
de Siqueira, J. V. V. and et. al., 2020. Impact of obesity on hospitalizations and mortality, due to
COVID-19: a systematic review. Obesity research & clinical practice.
Gefen, A., 2017. Why is the heel particularly vulnerable to pressure ulcers?. British Journal of
Nursing. 26(Sup20). pp.S62-S74.
Jankauskiene, R. and Baceviciene, M., 2019. Body image concerns and body weight
overestimation do not promote healthy behaviour: Evidence from adolescents in
Lithuania. International journal of environmental research and public health. 16(5).
p.864.
Kumanyika, S. K., 2019. Unraveling common threads in obesity risk among racial/ethnic
minority and migrant populations. Public health. 172. pp.125-134.
Little, P. and Et. Al., 2016) An internet-based intervention with brief nurse support to manage
obesity in primary care (POWeR+): a pragmatic, parallel-group, randomised controlled
trial. The Lancet Diabetes & Endocrinology, 4(10), 821-828. doi:10.1016/S2213-
8587(16)30099-7.
Park, S., Choo, J. and Chang, S. O., 2019. Healthy eating for obese children from
socioeconomically disadvantaged families: Its ecological factors and strategies. Journal
of Transcultural Nursing. 30(3). pp.268-279.
Rasmussen, N., 2019. Downsizing obesity: On Ancel Keys, the origins of BMI, and the neglect
of excess weight as a health hazard in the United States from the 1950s to 1970s. Journal
of the History of the Behavioral Sciences. 55(4). pp.299-318.
Timofeeva, D. S., Ofial, A. R. and Mayr, H., 2018. Kinetics of electrophilic fluorinations of
enamines and carbanions: comparison of the fluorinating power of N–F reagents. Journal
of the American Chemical Society. 140(36). pp.11474-11486.
Tournadre, A. and et. al., 2017. Changes in body composition and metabolic profile during
interleukin 6 inhibition in rheumatoid arthritis. Journal of cachexia, sarcopenia and
muscle. 8(4). pp.639-646
Online:
Overweight and Obesity. 2021. [Online]. Available through: <https://www.aihw.gov.au/reports-
data/behaviours-risk-factors/overweight-obesity/overview>
5
Books and Journals:
Černelič-Bizjak, M., 2019. Changes in body image during a 6-month lifestyle behaviour
intervention in a sample of overweight and obese individuals. Journal of bodywork and
movement therapies. 23(3). pp.515-520.
D’Innocenzo, S., Biagi, C. and Lanari, M., 2019. Obesity and the mediterranean diet: a review of
evidence of the role and sustainability of the mediterranean diet. Nutrients. 11(6). p.1306.
de Siqueira, J. V. V. and et. al., 2020. Impact of obesity on hospitalizations and mortality, due to
COVID-19: a systematic review. Obesity research & clinical practice.
Gefen, A., 2017. Why is the heel particularly vulnerable to pressure ulcers?. British Journal of
Nursing. 26(Sup20). pp.S62-S74.
Jankauskiene, R. and Baceviciene, M., 2019. Body image concerns and body weight
overestimation do not promote healthy behaviour: Evidence from adolescents in
Lithuania. International journal of environmental research and public health. 16(5).
p.864.
Kumanyika, S. K., 2019. Unraveling common threads in obesity risk among racial/ethnic
minority and migrant populations. Public health. 172. pp.125-134.
Little, P. and Et. Al., 2016) An internet-based intervention with brief nurse support to manage
obesity in primary care (POWeR+): a pragmatic, parallel-group, randomised controlled
trial. The Lancet Diabetes & Endocrinology, 4(10), 821-828. doi:10.1016/S2213-
8587(16)30099-7.
Park, S., Choo, J. and Chang, S. O., 2019. Healthy eating for obese children from
socioeconomically disadvantaged families: Its ecological factors and strategies. Journal
of Transcultural Nursing. 30(3). pp.268-279.
Rasmussen, N., 2019. Downsizing obesity: On Ancel Keys, the origins of BMI, and the neglect
of excess weight as a health hazard in the United States from the 1950s to 1970s. Journal
of the History of the Behavioral Sciences. 55(4). pp.299-318.
Timofeeva, D. S., Ofial, A. R. and Mayr, H., 2018. Kinetics of electrophilic fluorinations of
enamines and carbanions: comparison of the fluorinating power of N–F reagents. Journal
of the American Chemical Society. 140(36). pp.11474-11486.
Tournadre, A. and et. al., 2017. Changes in body composition and metabolic profile during
interleukin 6 inhibition in rheumatoid arthritis. Journal of cachexia, sarcopenia and
muscle. 8(4). pp.639-646
Online:
Overweight and Obesity. 2021. [Online]. Available through: <https://www.aihw.gov.au/reports-
data/behaviours-risk-factors/overweight-obesity/overview>
5
1 out of 7