Congestive Cardiac Failure
VerifiedAdded on 2023/04/08
|16
|2286
|223
AI Summary
This document provides information about congestive cardiac failure, including its causes, impacts, signs and symptoms, and a nursing care plan. It also mentions the availability of study material and assignments on Desklib.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: CONGESTIVE CARDIAC FAILURE
Congestive Cardiac Failure
Student’s name:
Institution:
Congestive Cardiac Failure
Student’s name:
Institution:
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.

CONGESTIVE CARDIAC FAILURE
2
1. Mrs. Sharon McKenzie is suffering from congestive cardiac failure which means that her
heart is unable to pump blood around the body efficiently.
Congestive cardiac failure is caused by conditions that damage the cardiac muscles such as;
Cardiomyopathy which results from side effects of drugs or infections associated with drug
taking, overworked cardiac which is brought about by blood pressure, hypertension, valve
diseases, kidney diseases or even defects that might be present in the heart from birth. Coronary
artery disease means the blood vessels supplying blood are either blocked or reduced flow of
blood which therefore damages the cardiac muscles. According to Michelucci, D’elios, Sticchi,
Pieragnoli, Ricciardi, Fatini, Prisco, (2016), heart attack results from sudden blockage of arteries
cause scars in the tissues hence reducing the effectiveness of blood pumping.
Congestive cardiac failure results in incidences and risks such as; Myocarditis which occur as
a result of inflammation of the heart muscle and leads to left sided heart failure,
hemochromatosis in which iron accumulates in the tissues, amyloidosis where organs in the body
accumulates deposits of abnormal proteins, obesity in which weight accumulates causing
difficulty in mobility, anemia in which red blood cells are deficient, hypothyroidism and
hyperthyroidism which result from under and over active thyroid gland respectively, smoking
which also increases the chances, heart arrhythmias which is abnormal heart rhythms which may
cause the heart to beat too faster or too slow, atria fibrillation which is described as an irregular
rapid heartbeat , lupus where the patient’s immune system attacks healthy cells and tissues,
emphysema where the patient experiences hardship when breathing and type 2 diabetes which
2
1. Mrs. Sharon McKenzie is suffering from congestive cardiac failure which means that her
heart is unable to pump blood around the body efficiently.
Congestive cardiac failure is caused by conditions that damage the cardiac muscles such as;
Cardiomyopathy which results from side effects of drugs or infections associated with drug
taking, overworked cardiac which is brought about by blood pressure, hypertension, valve
diseases, kidney diseases or even defects that might be present in the heart from birth. Coronary
artery disease means the blood vessels supplying blood are either blocked or reduced flow of
blood which therefore damages the cardiac muscles. According to Michelucci, D’elios, Sticchi,
Pieragnoli, Ricciardi, Fatini, Prisco, (2016), heart attack results from sudden blockage of arteries
cause scars in the tissues hence reducing the effectiveness of blood pumping.
Congestive cardiac failure results in incidences and risks such as; Myocarditis which occur as
a result of inflammation of the heart muscle and leads to left sided heart failure,
hemochromatosis in which iron accumulates in the tissues, amyloidosis where organs in the body
accumulates deposits of abnormal proteins, obesity in which weight accumulates causing
difficulty in mobility, anemia in which red blood cells are deficient, hypothyroidism and
hyperthyroidism which result from under and over active thyroid gland respectively, smoking
which also increases the chances, heart arrhythmias which is abnormal heart rhythms which may
cause the heart to beat too faster or too slow, atria fibrillation which is described as an irregular
rapid heartbeat , lupus where the patient’s immune system attacks healthy cells and tissues,
emphysema where the patient experiences hardship when breathing and type 2 diabetes which

CONGESTIVE CARDIAC FAILURE
3
also increases the chances of cardiac failure as noted by (Bartunek, Terzic, Behfar & Wijns,
2018).
Impacts of Congestive Cardiac Failure
Due to a considerable level of disability, she cannot attend to activities of daily living by
herself an aspect that makes her rely on people to help her hence may be a burden to family
members. Home based care requires the caregiver to study some fundamental principles of
managing the disease hence burdensome (Sims, Garcia, Mignatti, Colombo, Jones, Uriel, Jorde,
2010). A lot of money has to be spent on medication and specific foods to lower the risk of death
in managing the disease an aspect that leads to financial constraints especially in when there is a
single bread winner. Inability to work leads to lose of jobs which intern affects the income of the
family leading to extra struggles and even stress. In cases where all family members are working
and may not wish to forfeit their jobs, it calls for employment of a caregiver who may not turn
out to be as expected hence may traumatize the patient more an aspect that can lead to stress and
death if not realized and solved in time.
2. Signs and symptoms of congestive cardiac failure
Congested lungs Buildup of fluid in the lungs leads to shortness of breath even when
resting in particular when lying down. A dry hacking cough may also
occur. This happens due to distension of blood vessels in the lungs as
a result of inappropriate blood pumping (Piotrowicz, Baranowski,
Piotrowska, Zieliński, and Piotrowicz (2012). Flooded alveoli occur as
3
also increases the chances of cardiac failure as noted by (Bartunek, Terzic, Behfar & Wijns,
2018).
Impacts of Congestive Cardiac Failure
Due to a considerable level of disability, she cannot attend to activities of daily living by
herself an aspect that makes her rely on people to help her hence may be a burden to family
members. Home based care requires the caregiver to study some fundamental principles of
managing the disease hence burdensome (Sims, Garcia, Mignatti, Colombo, Jones, Uriel, Jorde,
2010). A lot of money has to be spent on medication and specific foods to lower the risk of death
in managing the disease an aspect that leads to financial constraints especially in when there is a
single bread winner. Inability to work leads to lose of jobs which intern affects the income of the
family leading to extra struggles and even stress. In cases where all family members are working
and may not wish to forfeit their jobs, it calls for employment of a caregiver who may not turn
out to be as expected hence may traumatize the patient more an aspect that can lead to stress and
death if not realized and solved in time.
2. Signs and symptoms of congestive cardiac failure
Congested lungs Buildup of fluid in the lungs leads to shortness of breath even when
resting in particular when lying down. A dry hacking cough may also
occur. This happens due to distension of blood vessels in the lungs as
a result of inappropriate blood pumping (Piotrowicz, Baranowski,
Piotrowska, Zieliński, and Piotrowicz (2012). Flooded alveoli occur as
CONGESTIVE CARDIAC FAILURE
4
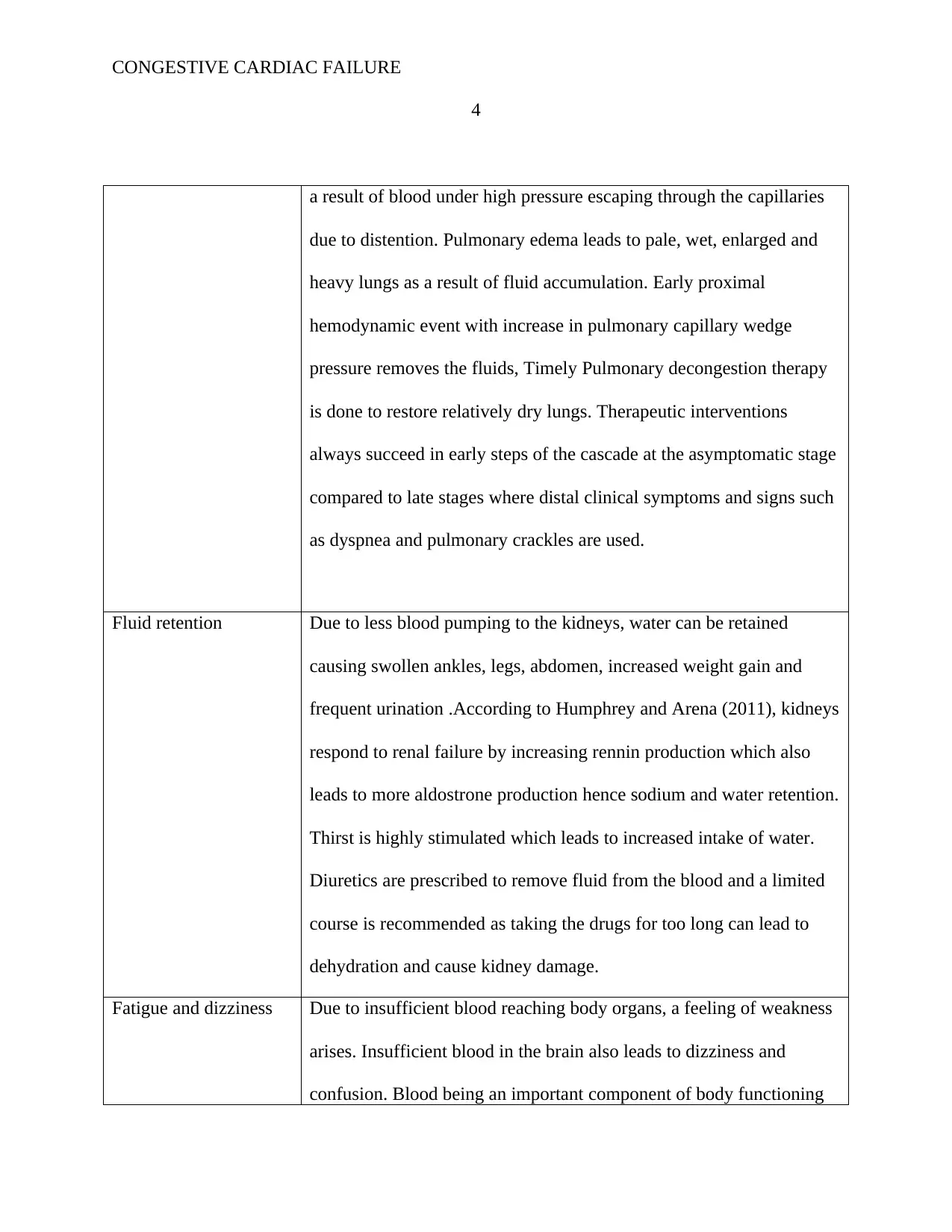
a result of blood under high pressure escaping through the capillaries
due to distention. Pulmonary edema leads to pale, wet, enlarged and
heavy lungs as a result of fluid accumulation. Early proximal
hemodynamic event with increase in pulmonary capillary wedge
pressure removes the fluids, Timely Pulmonary decongestion therapy
is done to restore relatively dry lungs. Therapeutic interventions
always succeed in early steps of the cascade at the asymptomatic stage
compared to late stages where distal clinical symptoms and signs such
as dyspnea and pulmonary crackles are used.
Fluid retention Due to less blood pumping to the kidneys, water can be retained
causing swollen ankles, legs, abdomen, increased weight gain and
frequent urination .According to Humphrey and Arena (2011), kidneys
respond to renal failure by increasing rennin production which also
leads to more aldostrone production hence sodium and water retention.
Thirst is highly stimulated which leads to increased intake of water.
Diuretics are prescribed to remove fluid from the blood and a limited
course is recommended as taking the drugs for too long can lead to
dehydration and cause kidney damage.
Fatigue and dizziness Due to insufficient blood reaching body organs, a feeling of weakness
arises. Insufficient blood in the brain also leads to dizziness and
confusion. Blood being an important component of body functioning
4
a result of blood under high pressure escaping through the capillaries
due to distention. Pulmonary edema leads to pale, wet, enlarged and
heavy lungs as a result of fluid accumulation. Early proximal
hemodynamic event with increase in pulmonary capillary wedge
pressure removes the fluids, Timely Pulmonary decongestion therapy
is done to restore relatively dry lungs. Therapeutic interventions
always succeed in early steps of the cascade at the asymptomatic stage
compared to late stages where distal clinical symptoms and signs such
as dyspnea and pulmonary crackles are used.
Fluid retention Due to less blood pumping to the kidneys, water can be retained
causing swollen ankles, legs, abdomen, increased weight gain and
frequent urination .According to Humphrey and Arena (2011), kidneys
respond to renal failure by increasing rennin production which also
leads to more aldostrone production hence sodium and water retention.
Thirst is highly stimulated which leads to increased intake of water.
Diuretics are prescribed to remove fluid from the blood and a limited
course is recommended as taking the drugs for too long can lead to
dehydration and cause kidney damage.
Fatigue and dizziness Due to insufficient blood reaching body organs, a feeling of weakness
arises. Insufficient blood in the brain also leads to dizziness and
confusion. Blood being an important component of body functioning
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.

CONGESTIVE CARDIAC FAILURE
5
leads to wearing and tearing of muscles if not appropriately pumped.
Since blood carries oxygen to the brain, reduction in the amount of
blood pumped to it means reduced amount of oxygen hence confusion.
Regular exercises are recommended to exercise body muscles (Richer,
Domergue, Gervais, Fornes, Trabold, & Giudicelli, 2013). Plenty of
rest and avoiding mentally taxing activities and alcohol is also
recommended. Acetaminophen is recommended to manage associated
headaches.
3. Phamacodynamics and Pharmacokinetics of Aldosterone Antagonists
Aldosterone antagonists are diuretics or “water pills” namely Spironolactone (Aldactone) and
Eplerenone (Inspra) which can also be called aldosterone receptor blockers. As connoted by
Roche, Pichot, Da Costa, Isaaz, Costes, Dall’Acqua, Barthélémy (2015), the drugs in this class
help the kidneys to produce more urine and the more the patient urinates the more excess salt and
water is flushed out of the body an aspect that makes it easier for the heart to pump blood. The
diuretics also ease the workload of an overworked heart which leads to easy and effective
pumping. Blood pressure which is associated with the disease is also lowered by the use of the
receptor blockers and it is kept at reasonable or rather normal levels. Shortness of breath which
is as a result of lungs congestion or blocked air ways, is also relieved. Swelling and bloating in
the lower abdomen, legs and ankles is reduced to a greater extent. The diuretics also lead to
5
leads to wearing and tearing of muscles if not appropriately pumped.
Since blood carries oxygen to the brain, reduction in the amount of
blood pumped to it means reduced amount of oxygen hence confusion.
Regular exercises are recommended to exercise body muscles (Richer,
Domergue, Gervais, Fornes, Trabold, & Giudicelli, 2013). Plenty of
rest and avoiding mentally taxing activities and alcohol is also
recommended. Acetaminophen is recommended to manage associated
headaches.
3. Phamacodynamics and Pharmacokinetics of Aldosterone Antagonists
Aldosterone antagonists are diuretics or “water pills” namely Spironolactone (Aldactone) and
Eplerenone (Inspra) which can also be called aldosterone receptor blockers. As connoted by
Roche, Pichot, Da Costa, Isaaz, Costes, Dall’Acqua, Barthélémy (2015), the drugs in this class
help the kidneys to produce more urine and the more the patient urinates the more excess salt and
water is flushed out of the body an aspect that makes it easier for the heart to pump blood. The
diuretics also ease the workload of an overworked heart which leads to easy and effective
pumping. Blood pressure which is associated with the disease is also lowered by the use of the
receptor blockers and it is kept at reasonable or rather normal levels. Shortness of breath which
is as a result of lungs congestion or blocked air ways, is also relieved. Swelling and bloating in
the lower abdomen, legs and ankles is reduced to a greater extent. The diuretics also lead to

CONGESTIVE CARDIAC FAILURE
6
frequent urination hence healthcare providers always advice patients to take drugs six hours
before bedtime to avoid waking up at night.
Determination of plasma concentration of the diuretics is chromatographically characterized
with one to two dihydro-spirorenone and the patient is advised accordingly. Plasma levels of
drugs and metabolic action is determined to ensure the patient is fully aware on the appropriate
intake of the drugs without unnecessary harm to self. Aldosterone receptor antagonists
antagonize the aldosterone hormone in the body and prevent sympathetic activation of
parasympathetic inhibition, and myocardial remodeling which may occur (Miller, Hemauer,
Smith, Stickland, & Dempsey, 2016). In congestive cardiac failure with reduced ejection
fraction, may be considered in patients who are symptomatic despite optimal doses of
angiotensin-converting enzyme inhibitors and beta blockers, but it should not be used in the
management of patients with preserved ejection fraction without other cormorbidities.
Aldestrone antagonists may be considered as an add-on in patients with inadequate control of
blood pressure or in patients with primary hyperaldosteronism.
4. Nursing Care Plan
Condition Assessment Diagnosis Goals and
plans
Nursing Interventions Evaluation
Acute
pain
Difficulty
in
breathing
The patient
is
experiencin
The
patients
pain will
Assess the
pain using a
pain rating
The patient will be
relieved of the
pain.
6
frequent urination hence healthcare providers always advice patients to take drugs six hours
before bedtime to avoid waking up at night.
Determination of plasma concentration of the diuretics is chromatographically characterized
with one to two dihydro-spirorenone and the patient is advised accordingly. Plasma levels of
drugs and metabolic action is determined to ensure the patient is fully aware on the appropriate
intake of the drugs without unnecessary harm to self. Aldosterone receptor antagonists
antagonize the aldosterone hormone in the body and prevent sympathetic activation of
parasympathetic inhibition, and myocardial remodeling which may occur (Miller, Hemauer,
Smith, Stickland, & Dempsey, 2016). In congestive cardiac failure with reduced ejection
fraction, may be considered in patients who are symptomatic despite optimal doses of
angiotensin-converting enzyme inhibitors and beta blockers, but it should not be used in the
management of patients with preserved ejection fraction without other cormorbidities.
Aldestrone antagonists may be considered as an add-on in patients with inadequate control of
blood pressure or in patients with primary hyperaldosteronism.
4. Nursing Care Plan
Condition Assessment Diagnosis Goals and
plans
Nursing Interventions Evaluation
Acute
pain
Difficulty
in
breathing
The patient
is
experiencin
The
patients
pain will
Assess the
pain using a
pain rating
The patient will be
relieved of the
pain.

CONGESTIVE CARDIAC FAILURE
7
Chest pain
Restlessnes
s
g acute pain
in the chest
be reduced
and patient
will
demonstrat
e activities
that will
prevent
pain re
occurrence.
scale
Administer
vasodilators as
ordered
Assess the
response to
medication
Provide
comfort
measures
Establish a
quiet
environment
(Feiereisen,
Delagardelle,
Vaillant,
Lasar, &
Beissel, 2017)
Elevate head
of the bead
Monitor pulse
and blood
7
Chest pain
Restlessnes
s
g acute pain
in the chest
be reduced
and patient
will
demonstrat
e activities
that will
prevent
pain re
occurrence.
scale
Administer
vasodilators as
ordered
Assess the
response to
medication
Provide
comfort
measures
Establish a
quiet
environment
(Feiereisen,
Delagardelle,
Vaillant,
Lasar, &
Beissel, 2017)
Elevate head
of the bead
Monitor pulse
and blood
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

CONGESTIVE CARDIAC FAILURE
8
pressure
Teach the
patient
relaxation
techniques
Decreased
cardiac
output
Pale
conjunctiva
Irregular
pulse
rhythm
General
body
weakness
The patients
cardiac
output has
decreased
After 3-4
hours the
patient will
participate
in activities
that will
reduce
cardiac
workload
Assess
abnormal lung
sounds
Monitor the
blood pressure
Assess the
level of
consciousness
Monitor
laboratory
results
(Feiereisen,
Delagardelle,
Vaillant,
Lasar, &
After the
interventions, the
patient shall
participate in
activities that
reduce the
workload of the
cardiac.
8
pressure
Teach the
patient
relaxation
techniques
Decreased
cardiac
output
Pale
conjunctiva
Irregular
pulse
rhythm
General
body
weakness
The patients
cardiac
output has
decreased
After 3-4
hours the
patient will
participate
in activities
that will
reduce
cardiac
workload
Assess
abnormal lung
sounds
Monitor the
blood pressure
Assess the
level of
consciousness
Monitor
laboratory
results
(Feiereisen,
Delagardelle,
Vaillant,
Lasar, &
After the
interventions, the
patient shall
participate in
activities that
reduce the
workload of the
cardiac.

CONGESTIVE CARDIAC FAILURE
9
Beissel, 2017)
Assess body
temperature
Monitor
oxygen
saturation
Administer
cardiac
glycoside
agents
Encourage
periods of rest
Excess
fluid
volume
Difficulty
in
breathing
Crackles
Edema of
extremities
Change in
mental
Excessive
Fluid
volume
related
to decrease
d cardiac
output and
sodium and
water
Adequate
fluid
balance
will be
realized
since the
patient will
demonstrat
e behaviors
Establishing a
good rapport
with the
patient
Assessing
patients
general
condition
Monitor fluid
The excess fluid
volume will reduce
since the diuretic
therapy will help to
eradicate fluids.
The restriction of
fluid and sodium
intake also reduces
the chances of fluid
9
Beissel, 2017)
Assess body
temperature
Monitor
oxygen
saturation
Administer
cardiac
glycoside
agents
Encourage
periods of rest
Excess
fluid
volume
Difficulty
in
breathing
Crackles
Edema of
extremities
Change in
mental
Excessive
Fluid
volume
related
to decrease
d cardiac
output and
sodium and
water
Adequate
fluid
balance
will be
realized
since the
patient will
demonstrat
e behaviors
Establishing a
good rapport
with the
patient
Assessing
patients
general
condition
Monitor fluid
The excess fluid
volume will reduce
since the diuretic
therapy will help to
eradicate fluids.
The restriction of
fluid and sodium
intake also reduces
the chances of fluid

CONGESTIVE CARDIAC FAILURE
10
status
Anxiety
retention that will
resolve the
excess
fluid
volume.
Edema and
breathing
sounds will
decrease.
intake and
output every 4
hours
Monitor and
record any
health
improvements
Weigh patient
daily and
compare with
previous
weight
Determine
breathing
sounds
Follow low
sodium diet
and fluid
restriction
Evaluate urine
output in
relation to
accumulation.
(Kravari,Vasileiadi
s, Gerovasili,
Karatzanos,
Tasoulis, Kalligras,
Nanas, 2010).
10
status
Anxiety
retention that will
resolve the
excess
fluid
volume.
Edema and
breathing
sounds will
decrease.
intake and
output every 4
hours
Monitor and
record any
health
improvements
Weigh patient
daily and
compare with
previous
weight
Determine
breathing
sounds
Follow low
sodium diet
and fluid
restriction
Evaluate urine
output in
relation to
accumulation.
(Kravari,Vasileiadi
s, Gerovasili,
Karatzanos,
Tasoulis, Kalligras,
Nanas, 2010).
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.

CONGESTIVE CARDIAC FAILURE
11
diuretics
therapy
Ineffectiv
e
breathing
pattern
General
body
weakness
Frothy
sputum
Productive
cough
Pursed lip
breathing
Ineffective
breathing
pattern
which is
related to
fatigue and
decreased
lung
expansion
and
pulmonary
congestion
which are
secondary
to
congestive
cardiac
The
patients
respiratory
system will
be
functioning
without
causing by
any chance
any
unnecessar
y fatigue.
Establish good
rapport with
the patient
Inspect the
breathing
system to
establish the
effectiveness
of the
prescribed
drugs
Assess the
emotional
responses of
the patient to
treatment
Measure tidal
volume and
Proper breathing
pattern will be
restored since the
patient will be able
to comply with the
guidelines given on
medication
(Benazon, Foster,
& Coyne, 2014).
11
diuretics
therapy
Ineffectiv
e
breathing
pattern
General
body
weakness
Frothy
sputum
Productive
cough
Pursed lip
breathing
Ineffective
breathing
pattern
which is
related to
fatigue and
decreased
lung
expansion
and
pulmonary
congestion
which are
secondary
to
congestive
cardiac
The
patients
respiratory
system will
be
functioning
without
causing by
any chance
any
unnecessar
y fatigue.
Establish good
rapport with
the patient
Inspect the
breathing
system to
establish the
effectiveness
of the
prescribed
drugs
Assess the
emotional
responses of
the patient to
treatment
Measure tidal
volume and
Proper breathing
pattern will be
restored since the
patient will be able
to comply with the
guidelines given on
medication
(Benazon, Foster,
& Coyne, 2014).

CONGESTIVE CARDIAC FAILURE
12
failure vital capacity
Position
patient in
optimal body
alignment for
proper
breathing
Assist the
patient to use
relaxation
technique to
improve
breathing.
Activity
intoleranc
e
Limited
range of
motion
Abnormal
pulse rate
and rhythm
Imbalance
in the
supply and
demand of
oxygen
The patient
will be able
to tolerate
activities at
the end of
the
medication
Monitor and
record vital
signs
Assess the
general
condition of
the patient
Encourage
Balanced supply
and demand of
oxygen will enable
the patient to
tolerate normal
activities. (Meyer,
Schwaibold, Hajric,
Westbrook, Ebfeld,
12
failure vital capacity
Position
patient in
optimal body
alignment for
proper
breathing
Assist the
patient to use
relaxation
technique to
improve
breathing.
Activity
intoleranc
e
Limited
range of
motion
Abnormal
pulse rate
and rhythm
Imbalance
in the
supply and
demand of
oxygen
The patient
will be able
to tolerate
activities at
the end of
the
medication
Monitor and
record vital
signs
Assess the
general
condition of
the patient
Encourage
Balanced supply
and demand of
oxygen will enable
the patient to
tolerate normal
activities. (Meyer,
Schwaibold, Hajric,
Westbrook, Ebfeld,

CONGESTIVE CARDIAC FAILURE
13
Weakness
adequate bed
rest
Adjust the
daily activities
of the patient
Leyk, & Roskamm,
2018).
References
Bartunek, J., Terzic, A., Behfar, A., & Wijns, W. (2018). Clinical Experience With Regenerative
Therapy in Heart Failure. Canadian Modern Language Review, 122(10), 1344–1346.
https://doi.org/10.1161/CIRCRESAHA.118.312753
Benazon, N. R., Foster, M. D., & Coyne, J. C. (2014). Expressed emotion, adaptation, and
patient survival among couples coping with chronic heart failure. Journal of Family
Psychology, 20(2), 328–334. https://doi.org/10.1037/0893-3200.20.2.328
13
Weakness
adequate bed
rest
Adjust the
daily activities
of the patient
Leyk, & Roskamm,
2018).
References
Bartunek, J., Terzic, A., Behfar, A., & Wijns, W. (2018). Clinical Experience With Regenerative
Therapy in Heart Failure. Canadian Modern Language Review, 122(10), 1344–1346.
https://doi.org/10.1161/CIRCRESAHA.118.312753
Benazon, N. R., Foster, M. D., & Coyne, J. C. (2014). Expressed emotion, adaptation, and
patient survival among couples coping with chronic heart failure. Journal of Family
Psychology, 20(2), 328–334. https://doi.org/10.1037/0893-3200.20.2.328
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

CONGESTIVE CARDIAC FAILURE
14
Feiereisen, P., Delagardelle, C., Vaillant, M., Lasar, Y., & Beissel, J. (2017). Is Strength
Training the More Efficient Training Modality in Chronic Heart Failure? Medicine &
Science in Sports & Exercise, 39(11), 1910–1917. Retrieved from
http://search.ebscohost.com/login.aspx?direct=true&db=s3h&AN=SPHS-
1067792&site=ehost-live
Humphrey, R., & Arena, R. (2011). Surgical Innovations for Chronic Heart Failure in the
Context of Cardiopulmonary Rehabilitation. Physical Therapy, 80(1), 61–69. Retrieved
from http://search.ebscohost.com/login.aspx?
direct=true&db=s3h&AN=2724533&site=ehost-live
Kravari, M., Vasileiadis, I., Gerovasili, V., Karatzanos, E., Tasoulis, A., Kalligras, K., … Nanas,
S. (2010). Effects of a 3-month rehabilitation program on muscle oxygenation in
congestive heart failure patients as assessed by NIRS. International Journal of Industrial
Ergonomics, 40(2), 212–217. https://doi.org/10.1016/j.ergon.2009.03.006
Meyer, K., Schwaibold, M., Hajric, R., Westbrook, S., Ebfeld, D., Leyk, D., & Roskamm, H.
(2018). Delayed VO2 kinetics during ramp exercise: a criterion for cardiopulmonary
exercise capacity in chronic heart failure. / Retards au niveau de la cinetique de la VO2
pendant le ramp test pour determiner par l ’ exercice la capacite cardiopulmonaire chez
des patients souffrant d ’ insuffisance cardiaque chronique. Medicine & Science in Sports
& Exercise, 30(5), 643–648. Retrieved from http://search.ebscohost.com/login.aspx?
direct=true&db=s3h&AN=SPH463445&site=ehost-live
Michelucci, A., D’elios, M. M., Sticchi, E., Pieragnoli, P., Ricciardi, G., Fatini, C., … Prisco, D.
(2016). Autoantibodies against β1-Adrenergic Receptors: Response to Cardiac
14
Feiereisen, P., Delagardelle, C., Vaillant, M., Lasar, Y., & Beissel, J. (2017). Is Strength
Training the More Efficient Training Modality in Chronic Heart Failure? Medicine &
Science in Sports & Exercise, 39(11), 1910–1917. Retrieved from
http://search.ebscohost.com/login.aspx?direct=true&db=s3h&AN=SPHS-
1067792&site=ehost-live
Humphrey, R., & Arena, R. (2011). Surgical Innovations for Chronic Heart Failure in the
Context of Cardiopulmonary Rehabilitation. Physical Therapy, 80(1), 61–69. Retrieved
from http://search.ebscohost.com/login.aspx?
direct=true&db=s3h&AN=2724533&site=ehost-live
Kravari, M., Vasileiadis, I., Gerovasili, V., Karatzanos, E., Tasoulis, A., Kalligras, K., … Nanas,
S. (2010). Effects of a 3-month rehabilitation program on muscle oxygenation in
congestive heart failure patients as assessed by NIRS. International Journal of Industrial
Ergonomics, 40(2), 212–217. https://doi.org/10.1016/j.ergon.2009.03.006
Meyer, K., Schwaibold, M., Hajric, R., Westbrook, S., Ebfeld, D., Leyk, D., & Roskamm, H.
(2018). Delayed VO2 kinetics during ramp exercise: a criterion for cardiopulmonary
exercise capacity in chronic heart failure. / Retards au niveau de la cinetique de la VO2
pendant le ramp test pour determiner par l ’ exercice la capacite cardiopulmonaire chez
des patients souffrant d ’ insuffisance cardiaque chronique. Medicine & Science in Sports
& Exercise, 30(5), 643–648. Retrieved from http://search.ebscohost.com/login.aspx?
direct=true&db=s3h&AN=SPH463445&site=ehost-live
Michelucci, A., D’elios, M. M., Sticchi, E., Pieragnoli, P., Ricciardi, G., Fatini, C., … Prisco, D.
(2016). Autoantibodies against β1-Adrenergic Receptors: Response to Cardiac

CONGESTIVE CARDIAC FAILURE
15
Resynchronization Therapy and Renal Function. Pacing & Clinical Electrophysiology,
39(1), 65–72. Retrieved from http://search.ebscohost.com/login.aspx?
direct=true&db=s3h&AN=112131093&site=ehost-live
Miller, J. D., Hemauer, S. J., Smith, C. A., Stickland, M. K., & Dempsey, J. A. (2016).
Expiratory threshold loading impairs cardiovascular function in health and chronic heart
failure during submaximal exercise. Journal of Applied Physiology, 101(1), 213–227.
Retrieved from http://search.ebscohost.com/login.aspx?
direct=true&db=s3h&AN=21628096&site=ehost-live
Piotrowicz, E., Baranowski, R., Piotrowska, M., Zieliński, T., & Piotrowicz, R. (2012). Variable
Effects of Physical Training of Heart Rate Variability, Heart Rate Recovery, and Heart
Rate Turbulence in Chronic Heart Failure. Pacing & Clinical Electrophysiology, 32,
S113–S115. Retrieved from http://search.ebscohost.com/login.aspx?
direct=true&db=s3h&AN=36606737&site=ehost-live
Richer, C., Domergue, V., Gervais, M., Fornes, P., Trabold, F., & Giudicelli, J.-F. (2013).
Coronary Dilatation Reserve in Experimental Hypertension and Chronic Heart Failure:
Effects of Blockade of the Renin–Angiotensin System. Clinical & Experimental
Pharmacology & Physiology, 28(12), 997–1001. Retrieved from
http://search.ebscohost.com/login.aspx?direct=true&db=s3h&AN=5740004&site=ehost-
live
Roche, F., Pichot, V., Da Costa, A., Isaaz, K., Costes, F., Dall’Acqua, T., … Barthélémy, J.-C.
(2015). Chronotropic incompetence response to exercise in congestive heart failure,
relationship with the cardiac autonomic status. Clinical Physiology, 21(3), 335–342.
15
Resynchronization Therapy and Renal Function. Pacing & Clinical Electrophysiology,
39(1), 65–72. Retrieved from http://search.ebscohost.com/login.aspx?
direct=true&db=s3h&AN=112131093&site=ehost-live
Miller, J. D., Hemauer, S. J., Smith, C. A., Stickland, M. K., & Dempsey, J. A. (2016).
Expiratory threshold loading impairs cardiovascular function in health and chronic heart
failure during submaximal exercise. Journal of Applied Physiology, 101(1), 213–227.
Retrieved from http://search.ebscohost.com/login.aspx?
direct=true&db=s3h&AN=21628096&site=ehost-live
Piotrowicz, E., Baranowski, R., Piotrowska, M., Zieliński, T., & Piotrowicz, R. (2012). Variable
Effects of Physical Training of Heart Rate Variability, Heart Rate Recovery, and Heart
Rate Turbulence in Chronic Heart Failure. Pacing & Clinical Electrophysiology, 32,
S113–S115. Retrieved from http://search.ebscohost.com/login.aspx?
direct=true&db=s3h&AN=36606737&site=ehost-live
Richer, C., Domergue, V., Gervais, M., Fornes, P., Trabold, F., & Giudicelli, J.-F. (2013).
Coronary Dilatation Reserve in Experimental Hypertension and Chronic Heart Failure:
Effects of Blockade of the Renin–Angiotensin System. Clinical & Experimental
Pharmacology & Physiology, 28(12), 997–1001. Retrieved from
http://search.ebscohost.com/login.aspx?direct=true&db=s3h&AN=5740004&site=ehost-
live
Roche, F., Pichot, V., Da Costa, A., Isaaz, K., Costes, F., Dall’Acqua, T., … Barthélémy, J.-C.
(2015). Chronotropic incompetence response to exercise in congestive heart failure,
relationship with the cardiac autonomic status. Clinical Physiology, 21(3), 335–342.

CONGESTIVE CARDIAC FAILURE
16
Retrieved from http://search.ebscohost.com/login.aspx?
direct=true&db=s3h&AN=4534969&site=ehost-live
Sims, D. B., Garcia, L. I., Mignatti, A., Colombo, P. C., Jones, M., Uriel, N., … Jorde, U. P.
(2010). Utilization of Defibrillators and Resynchronization Therapy at the Time of
Evaluation at a Heart Failure and Cardiac Transplantation Center. Pacing & Clinical
Electrophysiology, 33(8), 988–993. Retrieved from
http://search.ebscohost.com/login.aspx?
direct=true&db=s3h&AN=52670506&site=ehost-live
16
Retrieved from http://search.ebscohost.com/login.aspx?
direct=true&db=s3h&AN=4534969&site=ehost-live
Sims, D. B., Garcia, L. I., Mignatti, A., Colombo, P. C., Jones, M., Uriel, N., … Jorde, U. P.
(2010). Utilization of Defibrillators and Resynchronization Therapy at the Time of
Evaluation at a Heart Failure and Cardiac Transplantation Center. Pacing & Clinical
Electrophysiology, 33(8), 988–993. Retrieved from
http://search.ebscohost.com/login.aspx?
direct=true&db=s3h&AN=52670506&site=ehost-live
1 out of 16
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





