Assessing Oxygen Therapy for Chronic Obstructive Pulmonary Disease
VerifiedAdded on 2023/06/15
|5
|931
|98
Report
AI Summary
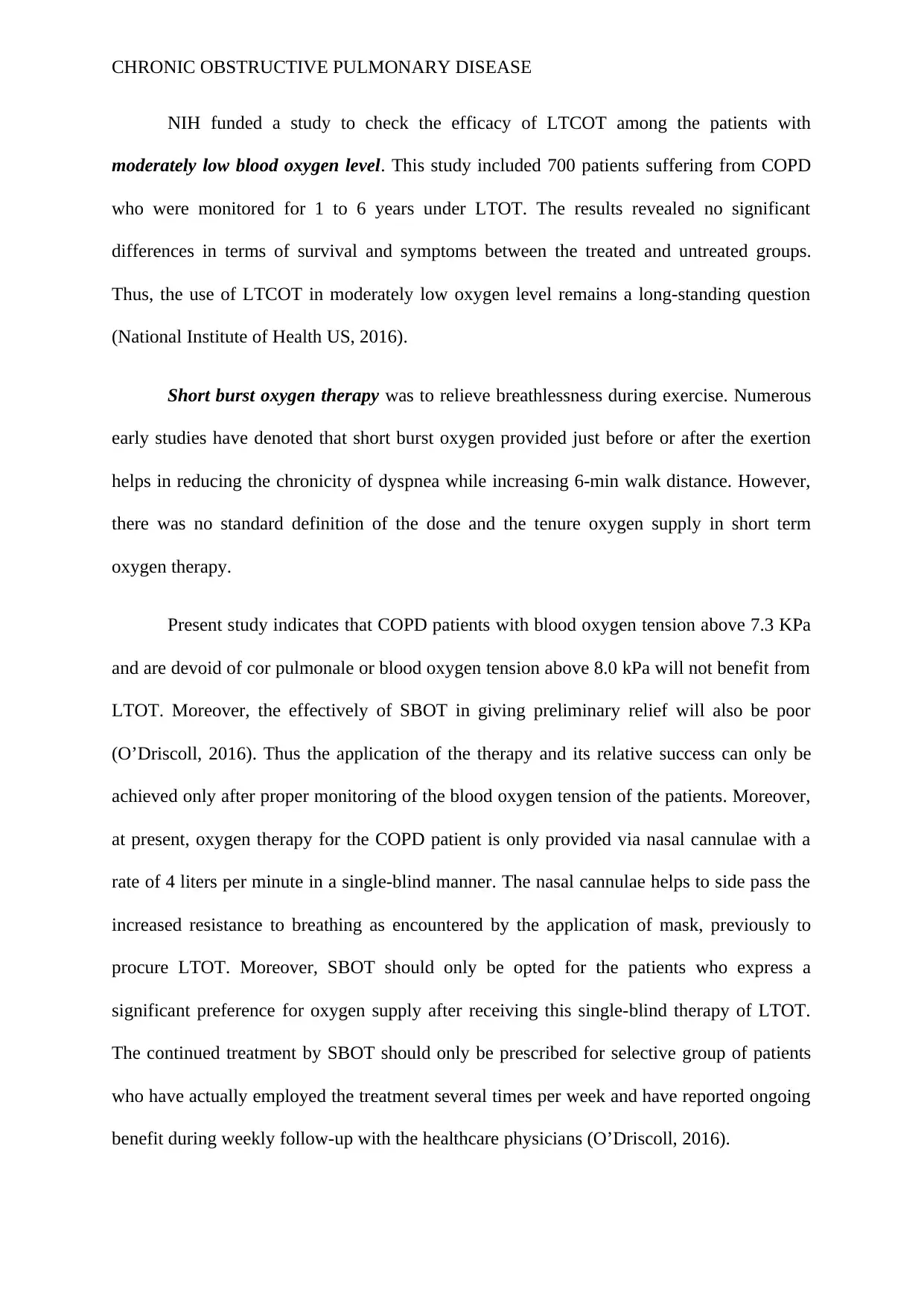
This report provides an overview of Chronic Obstructive Pulmonary Disease (COPD) and the use of long-term oxygen therapy (LTOT) in its management. It highlights that COPD is a leading cause of disability and mortality, damaging lung airways and causing breathlessness. LTOT is shown to increase life expectancy in patients with severe hypoxemia. The report references studies on the cost of LTOT, its impact on survival rates, exercise performance, and quality of life. A key study revealed no significant differences in survival or symptoms among COPD patients with moderately low blood oxygen levels treated with LTOT. Short burst oxygen therapy (SBOT) is also discussed for relieving breathlessness during exercise, emphasizing the need for proper monitoring of blood oxygen tension and selective prescription based on patient preference and reported benefits. The report concludes that the effectiveness of oxygen therapy depends on careful patient monitoring and individualized treatment plans.
1 out of 5








![[object Object]](/_next/static/media/star-bottom.7253800d.svg)