Clinical Practice Improvement Project Report: NURS2006 Assignment
VerifiedAdded on 2023/05/28
|13
|5351
|360
Report
AI Summary
This Clinical Practice Improvement (CPI) project report, prepared as a supplementary assessment for NURS2006, focuses on reducing medication errors in acute wards through the implementation of Computerized Provider Order Entry (CPOE) training for nurses. The project, guided by SMART goals, aims to enhance nurses' knowledge and competence, leading to improved patient safety. The report provides a comprehensive background, emphasizing the significance of medication errors and their impact on patient outcomes, supported by relevant literature and evidence. It explores the relevance of clinical governance, outlining the four key pillars – professional development, clinical risk, consumer value, and clinical performance – in the context of preventing medication errors. The report details the key stakeholders, including physicians, IT personnel, hospital authorities, and nurses, and outlines the CPI tool, incorporating the PDSA cycle and PEPPA framework for effective project implementation and evaluation. The report also covers barriers to implementation and evaluation strategies, making it a valuable resource for understanding and addressing medication safety challenges in healthcare settings. The project also uses PEPPA framework for the improvement of the project.
NURS2006 SUPPLEMENTARY ASSESSMENT
Clinical Practice Improvement Project Report
Student Name, FAN and ID:
Project Aim:
Title- Provide training to nurses on the use of Computerized Provider Order Entry (CPOE) in acute
wards, for preventing and/or reducing rates of medication errors.
Aim- The aim of the project can be categorised in the form of SMART goals:
S- Provide CPOE training to nurses
M- Enhanced awareness and knowledge among nurses and subsequent reduction in medication
error rates
A- Increased nursing competence and enhanced patient safety
R- Nurses working in acute wards will be selected
T- One month of training
Background and Evidence that the issue is worth solving:
Medication errors refer to preventable and avoidable proceedings that are responsible for causing or
leading to unsuitable medication usage, and subsequent patient harm ,while administration of
medications are in control of healthcare professionals, or consumers (Cloete 2015). Medication
errors are commonly associated with professional practice that typically comprises of medicine
prescribing, communicating orders, product packaging, labeling, and nomenclature, dispensing,
compounding, distribution, monitoring, and use (Wittich, Burkle and Lanier 2014). Evidences also
elaborate on the fact that at times, such medication errors ensue as a consequence of systemic
problems, other than poor performance by doctors, nurses and other healthcare providers. Typically
medication errors affect only a solitary patient at a time, thus they are considered as isolated events,
and little attention is drawn the problems that ensue (Hayes et al. 2015).
Incidence of medication errors is a matter of growing concern owing to the fact that medication
errors account for 2-3% of hospital admissions in Australia. Additionally, improving medication
safety has been recognized as a key area of emphasis by the Australian Commission on Safety and
Quality in Health Care, facilitated by WHO regional campaign and Australian Government
Department of Health. Findings from literature also suggest that errors associated with wrong
administration of medication among hospitals occur in 9% cases, besides errors occurring in
discharge summary documentation, with rates of 2 error/patient (Roughead, Semple and Rosenfeld
NURS2006 Supplementary Assessment for Semester Two, 2018. 1
Clinical Practice Improvement Project Report
Student Name, FAN and ID:
Project Aim:
Title- Provide training to nurses on the use of Computerized Provider Order Entry (CPOE) in acute
wards, for preventing and/or reducing rates of medication errors.
Aim- The aim of the project can be categorised in the form of SMART goals:
S- Provide CPOE training to nurses
M- Enhanced awareness and knowledge among nurses and subsequent reduction in medication
error rates
A- Increased nursing competence and enhanced patient safety
R- Nurses working in acute wards will be selected
T- One month of training
Background and Evidence that the issue is worth solving:
Medication errors refer to preventable and avoidable proceedings that are responsible for causing or
leading to unsuitable medication usage, and subsequent patient harm ,while administration of
medications are in control of healthcare professionals, or consumers (Cloete 2015). Medication
errors are commonly associated with professional practice that typically comprises of medicine
prescribing, communicating orders, product packaging, labeling, and nomenclature, dispensing,
compounding, distribution, monitoring, and use (Wittich, Burkle and Lanier 2014). Evidences also
elaborate on the fact that at times, such medication errors ensue as a consequence of systemic
problems, other than poor performance by doctors, nurses and other healthcare providers. Typically
medication errors affect only a solitary patient at a time, thus they are considered as isolated events,
and little attention is drawn the problems that ensue (Hayes et al. 2015).
Incidence of medication errors is a matter of growing concern owing to the fact that medication
errors account for 2-3% of hospital admissions in Australia. Additionally, improving medication
safety has been recognized as a key area of emphasis by the Australian Commission on Safety and
Quality in Health Care, facilitated by WHO regional campaign and Australian Government
Department of Health. Findings from literature also suggest that errors associated with wrong
administration of medication among hospitals occur in 9% cases, besides errors occurring in
discharge summary documentation, with rates of 2 error/patient (Roughead, Semple and Rosenfeld
NURS2006 Supplementary Assessment for Semester Two, 2018. 1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
2016). Manias et al. (2014) opined that medication errors occurred at a rate of 6.58 cases/1000 bed
days, with the most common types of errors comprising of dose omission (n = 341, 12.4%), and
overdose (n = 579, 21.0%). Some of the chief contributing factors were identified to be
communication difficulties across clinical settings (n = 929, 33.7%), and lack of adherence to
procedures and polices (n = 617, 22.4%).
Keers et al. (2013) investigated the factors, which contribute to the onset of errors in medication
management and suggested that slips and breaks were the major testified unsafe deeds, followed by
knowledge-based errors and deliberate defilements. Furthermore, error-provoking circumstances
that influenced medication errors encompassed insufficient written message (prescriptions,
transcription, documentation), difficulties with drugs supply and storing (pharmacy provision errors
and stock management), workload, patient factors (obtainability, acuity), equipment problems
(access, functionality), fatigue and stress among staff, and distractions during medicine
administration. According to Lu et al. (2013) insufficient knowledge among nurses is one major
factor that leads to medication errors, which results in severe health consequences. This was also in
accordance with Sanghera et al. (2007) who elaborated on the fact that frequent interruptions
during drug administration and poor communication were some of the factors that led to such
errors. Moreover, organisational factors governing these errors were namely, absence of clarity for
checking drug administration, lack of feedback, and practice of administering drugs without
complete medication orders. In addition, the standard 6 also makes it imperative for all nurses to
deliver nursing practice in an appropriate and safe manner, with the aim of accomplishing their
agreed goals and responding to the needs of their service users (NMBA 2014). Besides, the nurses
are also accountable to the people seeking care services, for their actions, behaviours and decisions,
including documentation. This calls for the need of preventing and/or reducing incidence of
medication errors in healthcare settings.
Relevance of Clinical Governance to your project
Clinical governance refers to the framework that is used by the NHS organisations for remaining
accountable for bringing about continuous improvement in the quality of their services, and
fostering an environment where excellence in clinical care flourishes (Van Zwanenberg and Edwards
2018). In other words, clinical governance comprises of several procedures and principles that have
the primary objective of promoting patient safety, by reducing errors within healthcare settings. The
operations are typically controlled by governing bodies that adopt appropriate strategies for the
easy delivery of care services in a manner that enhances wellbeing of the patients. The four pillars of
clinical governance that are relevant to the realm of preventing medication errors by training the
nurses are as follows:
1. Professional development and management- This pillar encompasses conducting a
surveillance of the management of healthcare professionals and the changes that are
required to be made in the setting, for achieving the intended objectives. The CPI project will
NURS2006 Supplementary Assessment for Semester Two, 2018. 2
days, with the most common types of errors comprising of dose omission (n = 341, 12.4%), and
overdose (n = 579, 21.0%). Some of the chief contributing factors were identified to be
communication difficulties across clinical settings (n = 929, 33.7%), and lack of adherence to
procedures and polices (n = 617, 22.4%).
Keers et al. (2013) investigated the factors, which contribute to the onset of errors in medication
management and suggested that slips and breaks were the major testified unsafe deeds, followed by
knowledge-based errors and deliberate defilements. Furthermore, error-provoking circumstances
that influenced medication errors encompassed insufficient written message (prescriptions,
transcription, documentation), difficulties with drugs supply and storing (pharmacy provision errors
and stock management), workload, patient factors (obtainability, acuity), equipment problems
(access, functionality), fatigue and stress among staff, and distractions during medicine
administration. According to Lu et al. (2013) insufficient knowledge among nurses is one major
factor that leads to medication errors, which results in severe health consequences. This was also in
accordance with Sanghera et al. (2007) who elaborated on the fact that frequent interruptions
during drug administration and poor communication were some of the factors that led to such
errors. Moreover, organisational factors governing these errors were namely, absence of clarity for
checking drug administration, lack of feedback, and practice of administering drugs without
complete medication orders. In addition, the standard 6 also makes it imperative for all nurses to
deliver nursing practice in an appropriate and safe manner, with the aim of accomplishing their
agreed goals and responding to the needs of their service users (NMBA 2014). Besides, the nurses
are also accountable to the people seeking care services, for their actions, behaviours and decisions,
including documentation. This calls for the need of preventing and/or reducing incidence of
medication errors in healthcare settings.
Relevance of Clinical Governance to your project
Clinical governance refers to the framework that is used by the NHS organisations for remaining
accountable for bringing about continuous improvement in the quality of their services, and
fostering an environment where excellence in clinical care flourishes (Van Zwanenberg and Edwards
2018). In other words, clinical governance comprises of several procedures and principles that have
the primary objective of promoting patient safety, by reducing errors within healthcare settings. The
operations are typically controlled by governing bodies that adopt appropriate strategies for the
easy delivery of care services in a manner that enhances wellbeing of the patients. The four pillars of
clinical governance that are relevant to the realm of preventing medication errors by training the
nurses are as follows:
1. Professional development and management- This pillar encompasses conducting a
surveillance of the management of healthcare professionals and the changes that are
required to be made in the setting, for achieving the intended objectives. The CPI project will
NURS2006 Supplementary Assessment for Semester Two, 2018. 2
involve the adoption of reward and punishment strategies for the nursing staff working in
acute wards, who are found to successfully use CPOE and thus medication error, and those
who fail in doing so, respectively.
2. Clinical Risk- This pillar is precisely concerned with enhancing the safety and quality of
healthcare services delivered to patients, by recognising the opportunities and
circumstances that are responsible for putting the patients at risk of harm. In this case, the
pillar will assess the risk factors related with medication errors and the instances when they
can occur (Office of Safety and Quality in Healthcare 2016).
3. Consumer value- This pillar focuses on the need of increasing responsiveness to all
consumers. In this CPI tool, the pillar would place an emphasis on being more responsive to
monitor the wellbeing of the patients
4. Clinical performance and evaluation- This pillar is typically concerned with delivery of
services and also determines the efficiency of healthcare practitioners. This pillar will
determine whether the nurses have increased their knowledge on CPOE implementation
and are able to reduce rates of medication error.
Key Stakeholders:
Stakeholders refer to the individuals who are primarily affected by the actions, policies and
objectives of an organisation. The major stakeholders in this CPI tool are given below:
Physicians- The physicians will have the responsibility of electronically entering instructions,
which are vital for the treatment of patients. They will also educate the nurses with the help
of PowerPoint presentation, on the potential benefits of CPOE use, in relation to medication
errors, prevention of duplicate entries and billing.
IT personnel- They will provide hands-on training to the nurses on the usage of CPOE in an
efficient manner, and associated terminologies.
Hospital authorities- They will sanction adequate funds for the education program, and will
also provide remuneration to the IT personnel, for conducting the training sessions.
Nurses- They will be subjected to the training program that will focus on CPOE
implementation methods. The knowledge and awareness of the nurses will be analysed,
before and after implementation of the training program, with the aim of determining the
effectiveness of the program.
CPI Tool:
According to the NSW Health (2019), CPI signifies for Clinical Practice Improvement Training
Program. This training program helps the healthcare professionals to address any prevailing
healthcare problems which are negatively affecting the health and well-being of the patients. In
NURS2006 Supplementary Assessment for Semester Two, 2018. 3
acute wards, who are found to successfully use CPOE and thus medication error, and those
who fail in doing so, respectively.
2. Clinical Risk- This pillar is precisely concerned with enhancing the safety and quality of
healthcare services delivered to patients, by recognising the opportunities and
circumstances that are responsible for putting the patients at risk of harm. In this case, the
pillar will assess the risk factors related with medication errors and the instances when they
can occur (Office of Safety and Quality in Healthcare 2016).
3. Consumer value- This pillar focuses on the need of increasing responsiveness to all
consumers. In this CPI tool, the pillar would place an emphasis on being more responsive to
monitor the wellbeing of the patients
4. Clinical performance and evaluation- This pillar is typically concerned with delivery of
services and also determines the efficiency of healthcare practitioners. This pillar will
determine whether the nurses have increased their knowledge on CPOE implementation
and are able to reduce rates of medication error.
Key Stakeholders:
Stakeholders refer to the individuals who are primarily affected by the actions, policies and
objectives of an organisation. The major stakeholders in this CPI tool are given below:
Physicians- The physicians will have the responsibility of electronically entering instructions,
which are vital for the treatment of patients. They will also educate the nurses with the help
of PowerPoint presentation, on the potential benefits of CPOE use, in relation to medication
errors, prevention of duplicate entries and billing.
IT personnel- They will provide hands-on training to the nurses on the usage of CPOE in an
efficient manner, and associated terminologies.
Hospital authorities- They will sanction adequate funds for the education program, and will
also provide remuneration to the IT personnel, for conducting the training sessions.
Nurses- They will be subjected to the training program that will focus on CPOE
implementation methods. The knowledge and awareness of the nurses will be analysed,
before and after implementation of the training program, with the aim of determining the
effectiveness of the program.
CPI Tool:
According to the NSW Health (2019), CPI signifies for Clinical Practice Improvement Training
Program. This training program helps the healthcare professionals to address any prevailing
healthcare problems which are negatively affecting the health and well-being of the patients. In
NURS2006 Supplementary Assessment for Semester Two, 2018. 3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
order words, it can be said that the CPI tool helps in improving the overall quality of life and the
process of care (NSW Health 2019). The methodology once under the assistance of this training
program can be easily applied under numerous clinical settings. This ensures increase in the level of
patient’s safety and quality of care. The training also helps in improving the level of knowledge of
the healthcare professionals along with bringing proficiency in their skills.
PDSA is a CPI tool. PDSA is an abbreviated form of Plan, Do, Study and Act cycle. According
to the guidelines of the NSW Government (2018), the importance of PDSA is it helps to narrow down
the focus and can be easily implement over any small work field in order to bring continuous
improvement. Plan (P) helps in the identification of the principal measures of the project and the
tasks which are assigned against it along with the expected outcome. In relation to the chosen CPI
topi, the P is to introducing computerised physicians based order entry (CPOE) system under the
acute care settings and training the nurses to handle that system in order to decrease the chances of
the medication error. Do (D) stage deals with the subsequent implementation of the agreed plan
under pro-active approach in order to reduce targeted healthcare concern (NSW Health 2019). Here
target healthcare concern is medication errors under the acute care settings and the intervention
that will be implemented is introduction of CPOE and subsequent training of the nurses. The training
will be given under the acute care settings. Both hands on training and inter-active process through
power-point presentation will be undertaken. Study (S) signifies the study process which will be of
one month of the training session followed by review of the overall outcomes of the training process
like increase in the level of knowledge acquisition and skills of the nursing professionals. The review
will be done through MCQ in order to study the increase in the level of the knowledge of the nursing
professionals. The reduction in the medication error after training of the nursing professional will be
done through comparing the medication error data with the baseline data and the data after one
month of training. Act cycle (A) deals with development of the new standards of practice like skills in
using CPOE and it will be based o taking feedbacks from the nursing professionals in order to bring
refinement of the training process in the near future (NSW Health 2019).
PEPPA overview was developed to provide APN (Advanced Practice Nursing) researchers and
the healthcare professionals in order to guide and promote optimal development in the scope of
practice. Here P (population) is the first step of the framework which deals with the identification of
the priority population for the CPI program (Advance Practice Nursing 2019). The main population
that is selected for this CPI project include the nursing professionals who are working under the
acute care settings. This is because, the incident rate of the medication errors are higher among the
NURS2006 Supplementary Assessment for Semester Two, 2018. 4
process of care (NSW Health 2019). The methodology once under the assistance of this training
program can be easily applied under numerous clinical settings. This ensures increase in the level of
patient’s safety and quality of care. The training also helps in improving the level of knowledge of
the healthcare professionals along with bringing proficiency in their skills.
PDSA is a CPI tool. PDSA is an abbreviated form of Plan, Do, Study and Act cycle. According
to the guidelines of the NSW Government (2018), the importance of PDSA is it helps to narrow down
the focus and can be easily implement over any small work field in order to bring continuous
improvement. Plan (P) helps in the identification of the principal measures of the project and the
tasks which are assigned against it along with the expected outcome. In relation to the chosen CPI
topi, the P is to introducing computerised physicians based order entry (CPOE) system under the
acute care settings and training the nurses to handle that system in order to decrease the chances of
the medication error. Do (D) stage deals with the subsequent implementation of the agreed plan
under pro-active approach in order to reduce targeted healthcare concern (NSW Health 2019). Here
target healthcare concern is medication errors under the acute care settings and the intervention
that will be implemented is introduction of CPOE and subsequent training of the nurses. The training
will be given under the acute care settings. Both hands on training and inter-active process through
power-point presentation will be undertaken. Study (S) signifies the study process which will be of
one month of the training session followed by review of the overall outcomes of the training process
like increase in the level of knowledge acquisition and skills of the nursing professionals. The review
will be done through MCQ in order to study the increase in the level of the knowledge of the nursing
professionals. The reduction in the medication error after training of the nursing professional will be
done through comparing the medication error data with the baseline data and the data after one
month of training. Act cycle (A) deals with development of the new standards of practice like skills in
using CPOE and it will be based o taking feedbacks from the nursing professionals in order to bring
refinement of the training process in the near future (NSW Health 2019).
PEPPA overview was developed to provide APN (Advanced Practice Nursing) researchers and
the healthcare professionals in order to guide and promote optimal development in the scope of
practice. Here P (population) is the first step of the framework which deals with the identification of
the priority population for the CPI program (Advance Practice Nursing 2019). The main population
that is selected for this CPI project include the nursing professionals who are working under the
acute care settings. This is because, the incident rate of the medication errors are higher among the
NURS2006 Supplementary Assessment for Semester Two, 2018. 4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
nursing professionals as they are mainly engaged in providing medication to the patients
(Christensen and Lundh 2016). The second step of PEPPA framework is identification of the
stakeholders and the recruitment of the participants. The main stakeholders of this CPI program for
the management of the medication errors include the nursing professionals (the trainee), the
physicians (who will place the order in the CPOE), and the information technology (IT) professionals
who will provide training in the domain of operation of the CPOE and the hospital funding authority.
The selection and the participants will be done under the acute care settings. The third step of
PEPPA includes determination of the new care model for meeting the patient health needs via taking
opinions from the different stakeholders. The fourth step deals with identification of the priority
problems and improvement of the model of care (Advance Practice Nursing, 2019). Here the main
priority problems is increase in the medication error under the acute care settings and thereby
increasing the overall cost of care, increase in patient’s mortality and length of stay at the hospital
(Christensen and Lundh 2016). The model of care is implementation of the CPOE. Step five deals
with defining new model of care and the role of the nursing professionals followed by the sixth step
of the plan implementation and seventh step of the initiation of the nursing professionals’ role in the
implementation of the plan. The implementation of the plan can be done after the success
completion of the program (Advance Practice Nursing 2019).
Summary of proposed intervention:
The plan for the reduction of the medical error under the acute care settings is illustrated below
1. Selecting the target population upon which the training will be conducted: The nursing
professionals under the acute care settings
2. Designing the training guidelines and training modules by the physicians
3. Installation of the CPOE under the acute settings under the funding granted by the hospital
authority
4. Educating nursing professionals about the mechanisms and the importance of COPE and how it
can reduce the medication error. The educational program will also help the nurses to educate the
consequences of the medication error. Training will be provided by the healthcare physicians
5. This will be followed by hands-on training to operate the CPOE by the IT professionals
6. After one month of training MCQ test will be conducted in order to gauge the level of education
among the nursing professionals about the tutorial taught in the programs
7. The reduction in the medication error will be accessed by comparison the data before the
NURS2006 Supplementary Assessment for Semester Two, 2018. 5
(Christensen and Lundh 2016). The second step of PEPPA framework is identification of the
stakeholders and the recruitment of the participants. The main stakeholders of this CPI program for
the management of the medication errors include the nursing professionals (the trainee), the
physicians (who will place the order in the CPOE), and the information technology (IT) professionals
who will provide training in the domain of operation of the CPOE and the hospital funding authority.
The selection and the participants will be done under the acute care settings. The third step of
PEPPA includes determination of the new care model for meeting the patient health needs via taking
opinions from the different stakeholders. The fourth step deals with identification of the priority
problems and improvement of the model of care (Advance Practice Nursing, 2019). Here the main
priority problems is increase in the medication error under the acute care settings and thereby
increasing the overall cost of care, increase in patient’s mortality and length of stay at the hospital
(Christensen and Lundh 2016). The model of care is implementation of the CPOE. Step five deals
with defining new model of care and the role of the nursing professionals followed by the sixth step
of the plan implementation and seventh step of the initiation of the nursing professionals’ role in the
implementation of the plan. The implementation of the plan can be done after the success
completion of the program (Advance Practice Nursing 2019).
Summary of proposed intervention:
The plan for the reduction of the medical error under the acute care settings is illustrated below
1. Selecting the target population upon which the training will be conducted: The nursing
professionals under the acute care settings
2. Designing the training guidelines and training modules by the physicians
3. Installation of the CPOE under the acute settings under the funding granted by the hospital
authority
4. Educating nursing professionals about the mechanisms and the importance of COPE and how it
can reduce the medication error. The educational program will also help the nurses to educate the
consequences of the medication error. Training will be provided by the healthcare physicians
5. This will be followed by hands-on training to operate the CPOE by the IT professionals
6. After one month of training MCQ test will be conducted in order to gauge the level of education
among the nursing professionals about the tutorial taught in the programs
7. The reduction in the medication error will be accessed by comparison the data before the
NURS2006 Supplementary Assessment for Semester Two, 2018. 5
initiation of the training and after the successful completion of the training
8. Taking feedbacks form the nursing professionals in order to improve the future training programs
According to Feleke et al. (2015) the medication errors or the drug error mainly occurs in any of the
three different steps of use of the medication starting from prescribing of medicines, dispensing and
administration. However, Alsulami, Conroy and Choonara (2013) are of the opinion that the
medication error is the single most avoidable cause behind the patient’s harm. Feleke et al. (2015)
stated highest reported cases of medication errors occur during the medication administration.
Keers et al. (2013) investigated the factors which contributed the onset of the medication errors and
highlighted that medication errors occur either for lack of knowledge, lack of proper attention or
deliberate errors. According to Lu et al. (2013) other chances of the medication errors occur due to
inability to encrypt the handwriting of the doctors, increase in the job pressure due to poor nurse:
patient ration and equipment problems. The medication errors lead to severe health consequences
like increased rate of mortality and morbidity, increase in health complications, increase length of
stay at the hospital and increased medication cost. Feleke et al. (2015) highlighted that the main
defaulters behind increased rate of the medication errors under the acute care settings are the
nursing professionals. This is because, the duty of medication administration are mainly opted to the
nurses and since they spent the majority of their duty time by monitoring the patients, the level of
medication errors are high among them. The nurses cannot solely be blamed for the increased rate
of reported cases of the medication errors. The cross-sectional study conducted by Salam et al.
(2018) revealed that increased job demands and social stressors increase the chance of the
medication error. Social stressor include imbalance in the work-life balance, dealing with difficult
colleagues and patients, challenging duty hours (working in the night shifts or doing round the clock
shift for 24 hours, working in the weekends or national holidays), poor revenue earning in the job,
lack of proper professional growth in the nursing profession. All these social stressors increase
compassion fatigue and overall frustration, which hamper the mental peace of mind and thereby
increasing the vulnerability of medication error (Salam et al. 2018). Dolansky et al. (2013)
highlighted the importance of giving hands-on training and face-to-face interactive settings are
helpful in reducing the knowledge based medication errors among the nursing professionals.
Barriers to implementation:
The main barriers in implementing the program are lack of motivation and enthusiasm of the nursing
students to take diligent part in the training session. The study conducted by Park and Choi (2015)
NURS2006 Supplementary Assessment for Semester Two, 2018. 6
8. Taking feedbacks form the nursing professionals in order to improve the future training programs
According to Feleke et al. (2015) the medication errors or the drug error mainly occurs in any of the
three different steps of use of the medication starting from prescribing of medicines, dispensing and
administration. However, Alsulami, Conroy and Choonara (2013) are of the opinion that the
medication error is the single most avoidable cause behind the patient’s harm. Feleke et al. (2015)
stated highest reported cases of medication errors occur during the medication administration.
Keers et al. (2013) investigated the factors which contributed the onset of the medication errors and
highlighted that medication errors occur either for lack of knowledge, lack of proper attention or
deliberate errors. According to Lu et al. (2013) other chances of the medication errors occur due to
inability to encrypt the handwriting of the doctors, increase in the job pressure due to poor nurse:
patient ration and equipment problems. The medication errors lead to severe health consequences
like increased rate of mortality and morbidity, increase in health complications, increase length of
stay at the hospital and increased medication cost. Feleke et al. (2015) highlighted that the main
defaulters behind increased rate of the medication errors under the acute care settings are the
nursing professionals. This is because, the duty of medication administration are mainly opted to the
nurses and since they spent the majority of their duty time by monitoring the patients, the level of
medication errors are high among them. The nurses cannot solely be blamed for the increased rate
of reported cases of the medication errors. The cross-sectional study conducted by Salam et al.
(2018) revealed that increased job demands and social stressors increase the chance of the
medication error. Social stressor include imbalance in the work-life balance, dealing with difficult
colleagues and patients, challenging duty hours (working in the night shifts or doing round the clock
shift for 24 hours, working in the weekends or national holidays), poor revenue earning in the job,
lack of proper professional growth in the nursing profession. All these social stressors increase
compassion fatigue and overall frustration, which hamper the mental peace of mind and thereby
increasing the vulnerability of medication error (Salam et al. 2018). Dolansky et al. (2013)
highlighted the importance of giving hands-on training and face-to-face interactive settings are
helpful in reducing the knowledge based medication errors among the nursing professionals.
Barriers to implementation:
The main barriers in implementing the program are lack of motivation and enthusiasm of the nursing
students to take diligent part in the training session. The study conducted by Park and Choi (2015)
NURS2006 Supplementary Assessment for Semester Two, 2018. 6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
highlighted that there is a co-relation between the self-esteem, satisfaction and career motivation
among the nursing student. Attending COPE based training will act as career motivation and thereby
helping to decrease the nursing absentees in the training sessions. The meta-analysis conducted by
Oh, Jeon and Koh (2015) stated that simulation-based learning process have a positive-impact on the
self-efficacy and learning motivation and these effect the knowledge and clinical skill acquisition.
This CPI program will follow the simulation based learning design where the power-point
presentation will be designed based on the artificial representation of the real world process in
order to gain educational goals.
In order to increase the nursing footfall in the training session, proper rewards and recognition are
importance. Henry (2014) is of the opinion that rewards and recognition will help to motivate the
nurse to participate actively in the training session. The rewards might come in form of financial
incentives after the successful completion of the training. The assurance of the financial incentives
during the onset of the training session will help to handle the resistance. However, the overall cost
might increase and same is required to be granted and sponsored by the main funding authority.
Evaluation of the project:
The evaluation of the successful outcome of the project can be done by comparing the baseline data
of the medication error before the implementation of the therapy plan and comparing the data after
implementation of the therapy plan. The reporting of the medication error can be done by a number
of ways like review of chart, claiming the data, incident type reporting, voluntary reporting,
examination of administrative data and computer monitoring and direct observation (Mansouri et al.
2013). The reporting of the medication error data will be done in this case by administrative data
examination. One of the advantage of this reporting system include, the process is disposable and
retroactive data and can be standardised easily. The evaluation will be done routinely based on
statistical analysis (Mansouri et al. 2013). Other process that can be used for the reporting and the
examination of the data include computer monitoring. One of the advantage of this approach is it is
a multi-data source integration and it also helps in real time reporting. However, there are certain
disadvantages of this approach and this includes inserted errors and poor software moreover the
overall process is costly (Mansouri et al. 2013).
Evaluation of the level of knowledge of the nurses will be done by the conduction of computerised
MCQ test where against each correct answer “1” mark will be assigned and “0” for negative answer.
There will be no negative marking. The questions will be based on the lectures and the study
NURS2006 Supplementary Assessment for Semester Two, 2018. 7
among the nursing student. Attending COPE based training will act as career motivation and thereby
helping to decrease the nursing absentees in the training sessions. The meta-analysis conducted by
Oh, Jeon and Koh (2015) stated that simulation-based learning process have a positive-impact on the
self-efficacy and learning motivation and these effect the knowledge and clinical skill acquisition.
This CPI program will follow the simulation based learning design where the power-point
presentation will be designed based on the artificial representation of the real world process in
order to gain educational goals.
In order to increase the nursing footfall in the training session, proper rewards and recognition are
importance. Henry (2014) is of the opinion that rewards and recognition will help to motivate the
nurse to participate actively in the training session. The rewards might come in form of financial
incentives after the successful completion of the training. The assurance of the financial incentives
during the onset of the training session will help to handle the resistance. However, the overall cost
might increase and same is required to be granted and sponsored by the main funding authority.
Evaluation of the project:
The evaluation of the successful outcome of the project can be done by comparing the baseline data
of the medication error before the implementation of the therapy plan and comparing the data after
implementation of the therapy plan. The reporting of the medication error can be done by a number
of ways like review of chart, claiming the data, incident type reporting, voluntary reporting,
examination of administrative data and computer monitoring and direct observation (Mansouri et al.
2013). The reporting of the medication error data will be done in this case by administrative data
examination. One of the advantage of this reporting system include, the process is disposable and
retroactive data and can be standardised easily. The evaluation will be done routinely based on
statistical analysis (Mansouri et al. 2013). Other process that can be used for the reporting and the
examination of the data include computer monitoring. One of the advantage of this approach is it is
a multi-data source integration and it also helps in real time reporting. However, there are certain
disadvantages of this approach and this includes inserted errors and poor software moreover the
overall process is costly (Mansouri et al. 2013).
Evaluation of the level of knowledge of the nurses will be done by the conduction of computerised
MCQ test where against each correct answer “1” mark will be assigned and “0” for negative answer.
There will be no negative marking. The questions will be based on the lectures and the study
NURS2006 Supplementary Assessment for Semester Two, 2018. 7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
material taught in the inter-active classes.
According to the Medication Safety in Australia, Government of Australia (2013), about 20 to 30% of
cases of the hospital admission is Australia occurs due to the medication errors and the percentage
is high among the older adults. Medication errors lead to adverse drug reactions which further
increases the severity of the health conditions. The statistics highlighted by the government of
Australia under the Australian Commission on Safety and Quality in Health Care stated that proper
training of the nursing professionals can help to reduce the chances of the medication errors and the
adverse drug reactions by 50%.
NURS2006 Supplementary Assessment for Semester Two, 2018. 8
According to the Medication Safety in Australia, Government of Australia (2013), about 20 to 30% of
cases of the hospital admission is Australia occurs due to the medication errors and the percentage
is high among the older adults. Medication errors lead to adverse drug reactions which further
increases the severity of the health conditions. The statistics highlighted by the government of
Australia under the Australian Commission on Safety and Quality in Health Care stated that proper
training of the nursing professionals can help to reduce the chances of the medication errors and the
adverse drug reactions by 50%.
NURS2006 Supplementary Assessment for Semester Two, 2018. 8
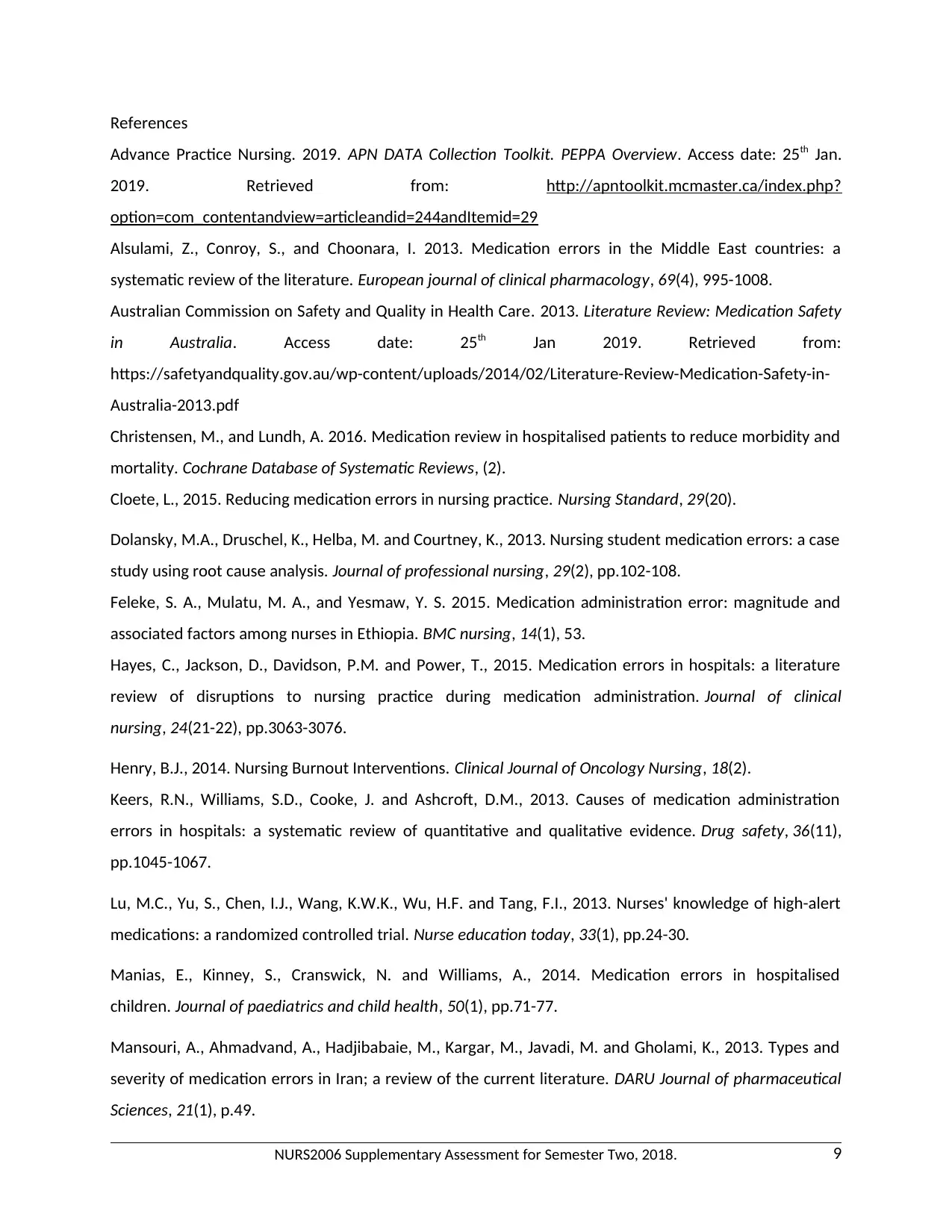
References
Advance Practice Nursing. 2019. APN DATA Collection Toolkit. PEPPA Overview. Access date: 25th Jan.
2019. Retrieved from: http://apntoolkit.mcmaster.ca/index.php?
option=com_contentandview=articleandid=244andItemid=29
Alsulami, Z., Conroy, S., and Choonara, I. 2013. Medication errors in the Middle East countries: a
systematic review of the literature. European journal of clinical pharmacology, 69(4), 995-1008.
Australian Commission on Safety and Quality in Health Care. 2013. Literature Review: Medication Safety
in Australia. Access date: 25th Jan 2019. Retrieved from:
https://safetyandquality.gov.au/wp-content/uploads/2014/02/Literature-Review-Medication-Safety-in-
Australia-2013.pdf
Christensen, M., and Lundh, A. 2016. Medication review in hospitalised patients to reduce morbidity and
mortality. Cochrane Database of Systematic Reviews, (2).
Cloete, L., 2015. Reducing medication errors in nursing practice. Nursing Standard, 29(20).
Dolansky, M.A., Druschel, K., Helba, M. and Courtney, K., 2013. Nursing student medication errors: a case
study using root cause analysis. Journal of professional nursing, 29(2), pp.102-108.
Feleke, S. A., Mulatu, M. A., and Yesmaw, Y. S. 2015. Medication administration error: magnitude and
associated factors among nurses in Ethiopia. BMC nursing, 14(1), 53.
Hayes, C., Jackson, D., Davidson, P.M. and Power, T., 2015. Medication errors in hospitals: a literature
review of disruptions to nursing practice during medication administration. Journal of clinical
nursing, 24(21-22), pp.3063-3076.
Henry, B.J., 2014. Nursing Burnout Interventions. Clinical Journal of Oncology Nursing, 18(2).
Keers, R.N., Williams, S.D., Cooke, J. and Ashcroft, D.M., 2013. Causes of medication administration
errors in hospitals: a systematic review of quantitative and qualitative evidence. Drug safety, 36(11),
pp.1045-1067.
Lu, M.C., Yu, S., Chen, I.J., Wang, K.W.K., Wu, H.F. and Tang, F.I., 2013. Nurses' knowledge of high-alert
medications: a randomized controlled trial. Nurse education today, 33(1), pp.24-30.
Manias, E., Kinney, S., Cranswick, N. and Williams, A., 2014. Medication errors in hospitalised
children. Journal of paediatrics and child health, 50(1), pp.71-77.
Mansouri, A., Ahmadvand, A., Hadjibabaie, M., Kargar, M., Javadi, M. and Gholami, K., 2013. Types and
severity of medication errors in Iran; a review of the current literature. DARU Journal of pharmaceutical
Sciences, 21(1), p.49.
NURS2006 Supplementary Assessment for Semester Two, 2018. 9
Advance Practice Nursing. 2019. APN DATA Collection Toolkit. PEPPA Overview. Access date: 25th Jan.
2019. Retrieved from: http://apntoolkit.mcmaster.ca/index.php?
option=com_contentandview=articleandid=244andItemid=29
Alsulami, Z., Conroy, S., and Choonara, I. 2013. Medication errors in the Middle East countries: a
systematic review of the literature. European journal of clinical pharmacology, 69(4), 995-1008.
Australian Commission on Safety and Quality in Health Care. 2013. Literature Review: Medication Safety
in Australia. Access date: 25th Jan 2019. Retrieved from:
https://safetyandquality.gov.au/wp-content/uploads/2014/02/Literature-Review-Medication-Safety-in-
Australia-2013.pdf
Christensen, M., and Lundh, A. 2016. Medication review in hospitalised patients to reduce morbidity and
mortality. Cochrane Database of Systematic Reviews, (2).
Cloete, L., 2015. Reducing medication errors in nursing practice. Nursing Standard, 29(20).
Dolansky, M.A., Druschel, K., Helba, M. and Courtney, K., 2013. Nursing student medication errors: a case
study using root cause analysis. Journal of professional nursing, 29(2), pp.102-108.
Feleke, S. A., Mulatu, M. A., and Yesmaw, Y. S. 2015. Medication administration error: magnitude and
associated factors among nurses in Ethiopia. BMC nursing, 14(1), 53.
Hayes, C., Jackson, D., Davidson, P.M. and Power, T., 2015. Medication errors in hospitals: a literature
review of disruptions to nursing practice during medication administration. Journal of clinical
nursing, 24(21-22), pp.3063-3076.
Henry, B.J., 2014. Nursing Burnout Interventions. Clinical Journal of Oncology Nursing, 18(2).
Keers, R.N., Williams, S.D., Cooke, J. and Ashcroft, D.M., 2013. Causes of medication administration
errors in hospitals: a systematic review of quantitative and qualitative evidence. Drug safety, 36(11),
pp.1045-1067.
Lu, M.C., Yu, S., Chen, I.J., Wang, K.W.K., Wu, H.F. and Tang, F.I., 2013. Nurses' knowledge of high-alert
medications: a randomized controlled trial. Nurse education today, 33(1), pp.24-30.
Manias, E., Kinney, S., Cranswick, N. and Williams, A., 2014. Medication errors in hospitalised
children. Journal of paediatrics and child health, 50(1), pp.71-77.
Mansouri, A., Ahmadvand, A., Hadjibabaie, M., Kargar, M., Javadi, M. and Gholami, K., 2013. Types and
severity of medication errors in Iran; a review of the current literature. DARU Journal of pharmaceutical
Sciences, 21(1), p.49.
NURS2006 Supplementary Assessment for Semester Two, 2018. 9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
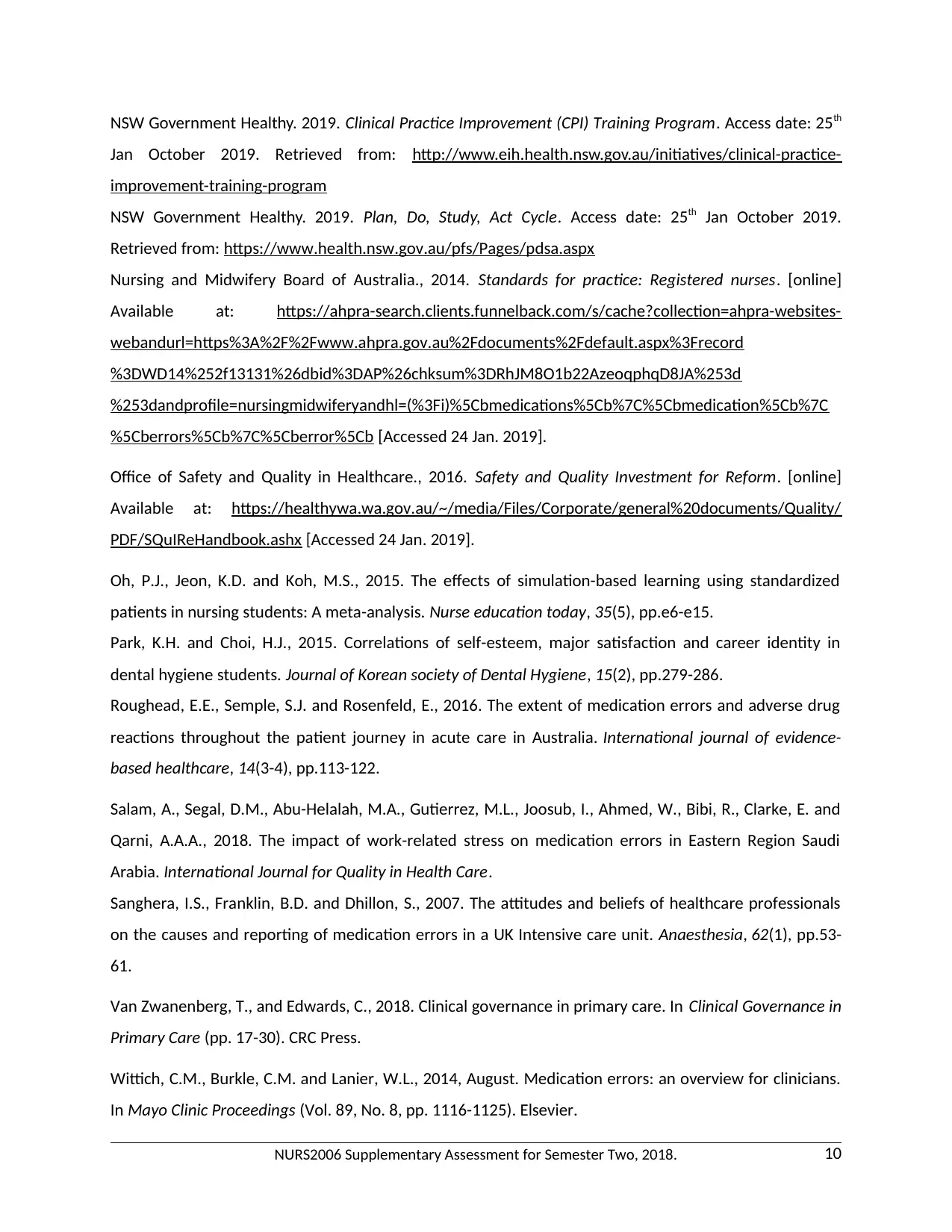
NSW Government Healthy. 2019. Clinical Practice Improvement (CPI) Training Program. Access date: 25th
Jan October 2019. Retrieved from: http://www.eih.health.nsw.gov.au/initiatives/clinical-practice-
improvement-training-program
NSW Government Healthy. 2019. Plan, Do, Study, Act Cycle. Access date: 25th Jan October 2019.
Retrieved from: https://www.health.nsw.gov.au/pfs/Pages/pdsa.aspx
Nursing and Midwifery Board of Australia., 2014. Standards for practice: Registered nurses. [online]
Available at: https://ahpra-search.clients.funnelback.com/s/cache?collection=ahpra-websites-
webandurl=https%3A%2F%2Fwww.ahpra.gov.au%2Fdocuments%2Fdefault.aspx%3Frecord
%3DWD14%252f13131%26dbid%3DAP%26chksum%3DRhJM8O1b22AzeoqphqD8JA%253d
%253dandprofile=nursingmidwiferyandhl=(%3Fi)%5Cbmedications%5Cb%7C%5Cbmedication%5Cb%7C
%5Cberrors%5Cb%7C%5Cberror%5Cb [Accessed 24 Jan. 2019].
Office of Safety and Quality in Healthcare., 2016. Safety and Quality Investment for Reform. [online]
Available at: https://healthywa.wa.gov.au/~/media/Files/Corporate/general%20documents/Quality/
PDF/SQuIReHandbook.ashx [Accessed 24 Jan. 2019].
Oh, P.J., Jeon, K.D. and Koh, M.S., 2015. The effects of simulation-based learning using standardized
patients in nursing students: A meta-analysis. Nurse education today, 35(5), pp.e6-e15.
Park, K.H. and Choi, H.J., 2015. Correlations of self-esteem, major satisfaction and career identity in
dental hygiene students. Journal of Korean society of Dental Hygiene, 15(2), pp.279-286.
Roughead, E.E., Semple, S.J. and Rosenfeld, E., 2016. The extent of medication errors and adverse drug
reactions throughout the patient journey in acute care in Australia. International journal of evidence-
based healthcare, 14(3-4), pp.113-122.
Salam, A., Segal, D.M., Abu-Helalah, M.A., Gutierrez, M.L., Joosub, I., Ahmed, W., Bibi, R., Clarke, E. and
Qarni, A.A.A., 2018. The impact of work-related stress on medication errors in Eastern Region Saudi
Arabia. International Journal for Quality in Health Care.
Sanghera, I.S., Franklin, B.D. and Dhillon, S., 2007. The attitudes and beliefs of healthcare professionals
on the causes and reporting of medication errors in a UK Intensive care unit. Anaesthesia, 62(1), pp.53-
61.
Van Zwanenberg, T., and Edwards, C., 2018. Clinical governance in primary care. In Clinical Governance in
Primary Care (pp. 17-30). CRC Press.
Wittich, C.M., Burkle, C.M. and Lanier, W.L., 2014, August. Medication errors: an overview for clinicians.
In Mayo Clinic Proceedings (Vol. 89, No. 8, pp. 1116-1125). Elsevier.
NURS2006 Supplementary Assessment for Semester Two, 2018. 10
Jan October 2019. Retrieved from: http://www.eih.health.nsw.gov.au/initiatives/clinical-practice-
improvement-training-program
NSW Government Healthy. 2019. Plan, Do, Study, Act Cycle. Access date: 25th Jan October 2019.
Retrieved from: https://www.health.nsw.gov.au/pfs/Pages/pdsa.aspx
Nursing and Midwifery Board of Australia., 2014. Standards for practice: Registered nurses. [online]
Available at: https://ahpra-search.clients.funnelback.com/s/cache?collection=ahpra-websites-
webandurl=https%3A%2F%2Fwww.ahpra.gov.au%2Fdocuments%2Fdefault.aspx%3Frecord
%3DWD14%252f13131%26dbid%3DAP%26chksum%3DRhJM8O1b22AzeoqphqD8JA%253d
%253dandprofile=nursingmidwiferyandhl=(%3Fi)%5Cbmedications%5Cb%7C%5Cbmedication%5Cb%7C
%5Cberrors%5Cb%7C%5Cberror%5Cb [Accessed 24 Jan. 2019].
Office of Safety and Quality in Healthcare., 2016. Safety and Quality Investment for Reform. [online]
Available at: https://healthywa.wa.gov.au/~/media/Files/Corporate/general%20documents/Quality/
PDF/SQuIReHandbook.ashx [Accessed 24 Jan. 2019].
Oh, P.J., Jeon, K.D. and Koh, M.S., 2015. The effects of simulation-based learning using standardized
patients in nursing students: A meta-analysis. Nurse education today, 35(5), pp.e6-e15.
Park, K.H. and Choi, H.J., 2015. Correlations of self-esteem, major satisfaction and career identity in
dental hygiene students. Journal of Korean society of Dental Hygiene, 15(2), pp.279-286.
Roughead, E.E., Semple, S.J. and Rosenfeld, E., 2016. The extent of medication errors and adverse drug
reactions throughout the patient journey in acute care in Australia. International journal of evidence-
based healthcare, 14(3-4), pp.113-122.
Salam, A., Segal, D.M., Abu-Helalah, M.A., Gutierrez, M.L., Joosub, I., Ahmed, W., Bibi, R., Clarke, E. and
Qarni, A.A.A., 2018. The impact of work-related stress on medication errors in Eastern Region Saudi
Arabia. International Journal for Quality in Health Care.
Sanghera, I.S., Franklin, B.D. and Dhillon, S., 2007. The attitudes and beliefs of healthcare professionals
on the causes and reporting of medication errors in a UK Intensive care unit. Anaesthesia, 62(1), pp.53-
61.
Van Zwanenberg, T., and Edwards, C., 2018. Clinical governance in primary care. In Clinical Governance in
Primary Care (pp. 17-30). CRC Press.
Wittich, C.M., Burkle, C.M. and Lanier, W.L., 2014, August. Medication errors: an overview for clinicians.
In Mayo Clinic Proceedings (Vol. 89, No. 8, pp. 1116-1125). Elsevier.
NURS2006 Supplementary Assessment for Semester Two, 2018. 10
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
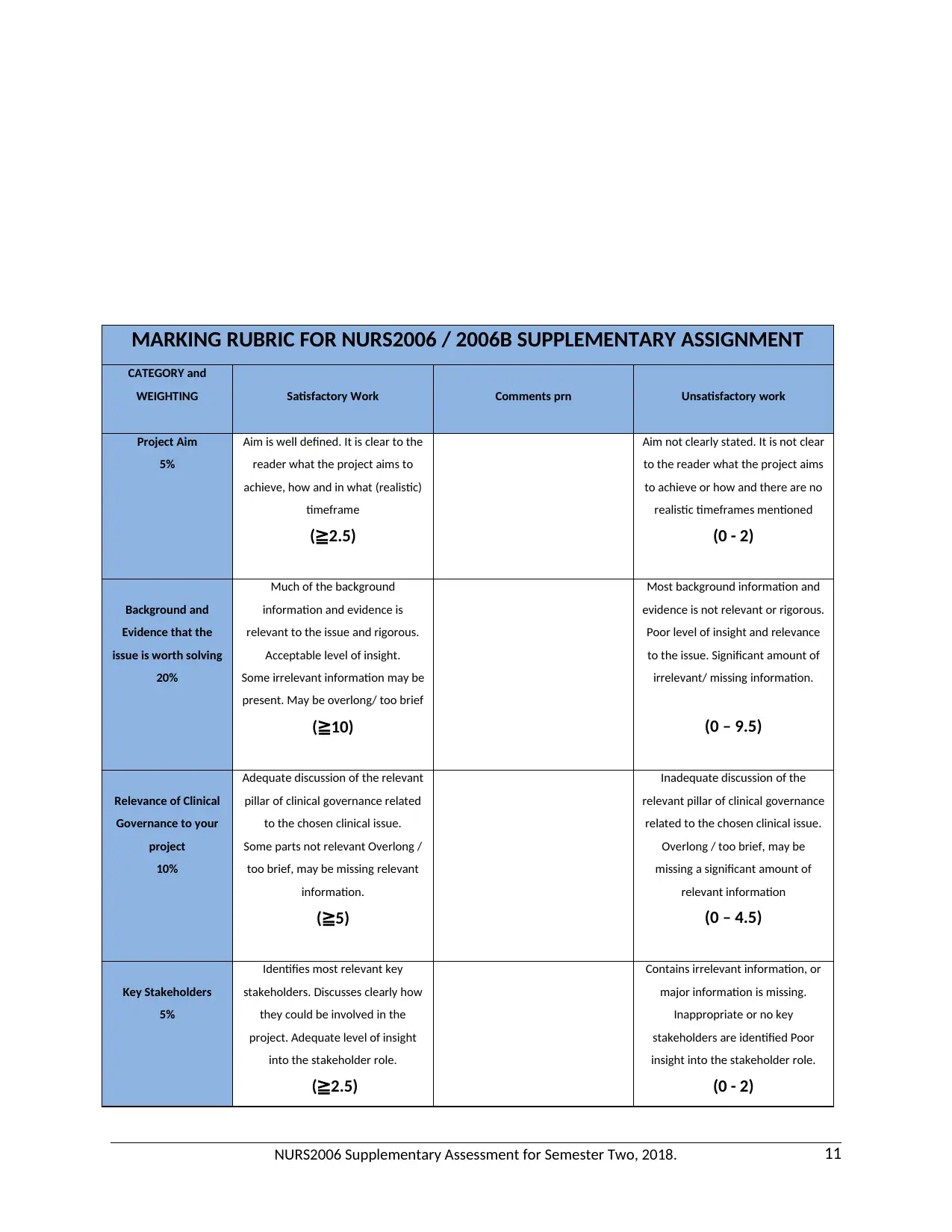
MARKING RUBRIC FOR NURS2006 / 2006B SUPPLEMENTARY ASSIGNMENT
CATEGORY and
WEIGHTING Satisfactory Work Comments prn Unsatisfactory work
Project Aim
5%
Aim is well defined. It is clear to the
reader what the project aims to
achieve, how and in what (realistic)
timeframe
(≧2.5)
Aim not clearly stated. It is not clear
to the reader what the project aims
to achieve or how and there are no
realistic timeframes mentioned
(0 - 2)
Background and
Evidence that the
issue is worth solving
20%
Much of the background
information and evidence is
relevant to the issue and rigorous.
Acceptable level of insight.
Some irrelevant information may be
present. May be overlong/ too brief
(≧10)
Most background information and
evidence is not relevant or rigorous.
Poor level of insight and relevance
to the issue. Significant amount of
irrelevant/ missing information.
(0 – 9.5)
Relevance of Clinical
Governance to your
project
10%
Adequate discussion of the relevant
pillar of clinical governance related
to the chosen clinical issue.
Some parts not relevant Overlong /
too brief, may be missing relevant
information.
(≧5)
Inadequate discussion of the
relevant pillar of clinical governance
related to the chosen clinical issue.
Overlong / too brief, may be
missing a significant amount of
relevant information
(0 – 4.5)
Key Stakeholders
5%
Identifies most relevant key
stakeholders. Discusses clearly how
they could be involved in the
project. Adequate level of insight
into the stakeholder role.
(≧2.5)
Contains irrelevant information, or
major information is missing.
Inappropriate or no key
stakeholders are identified Poor
insight into the stakeholder role.
(0 - 2)
NURS2006 Supplementary Assessment for Semester Two, 2018. 11
CATEGORY and
WEIGHTING Satisfactory Work Comments prn Unsatisfactory work
Project Aim
5%
Aim is well defined. It is clear to the
reader what the project aims to
achieve, how and in what (realistic)
timeframe
(≧2.5)
Aim not clearly stated. It is not clear
to the reader what the project aims
to achieve or how and there are no
realistic timeframes mentioned
(0 - 2)
Background and
Evidence that the
issue is worth solving
20%
Much of the background
information and evidence is
relevant to the issue and rigorous.
Acceptable level of insight.
Some irrelevant information may be
present. May be overlong/ too brief
(≧10)
Most background information and
evidence is not relevant or rigorous.
Poor level of insight and relevance
to the issue. Significant amount of
irrelevant/ missing information.
(0 – 9.5)
Relevance of Clinical
Governance to your
project
10%
Adequate discussion of the relevant
pillar of clinical governance related
to the chosen clinical issue.
Some parts not relevant Overlong /
too brief, may be missing relevant
information.
(≧5)
Inadequate discussion of the
relevant pillar of clinical governance
related to the chosen clinical issue.
Overlong / too brief, may be
missing a significant amount of
relevant information
(0 – 4.5)
Key Stakeholders
5%
Identifies most relevant key
stakeholders. Discusses clearly how
they could be involved in the
project. Adequate level of insight
into the stakeholder role.
(≧2.5)
Contains irrelevant information, or
major information is missing.
Inappropriate or no key
stakeholders are identified Poor
insight into the stakeholder role.
(0 - 2)
NURS2006 Supplementary Assessment for Semester Two, 2018. 11
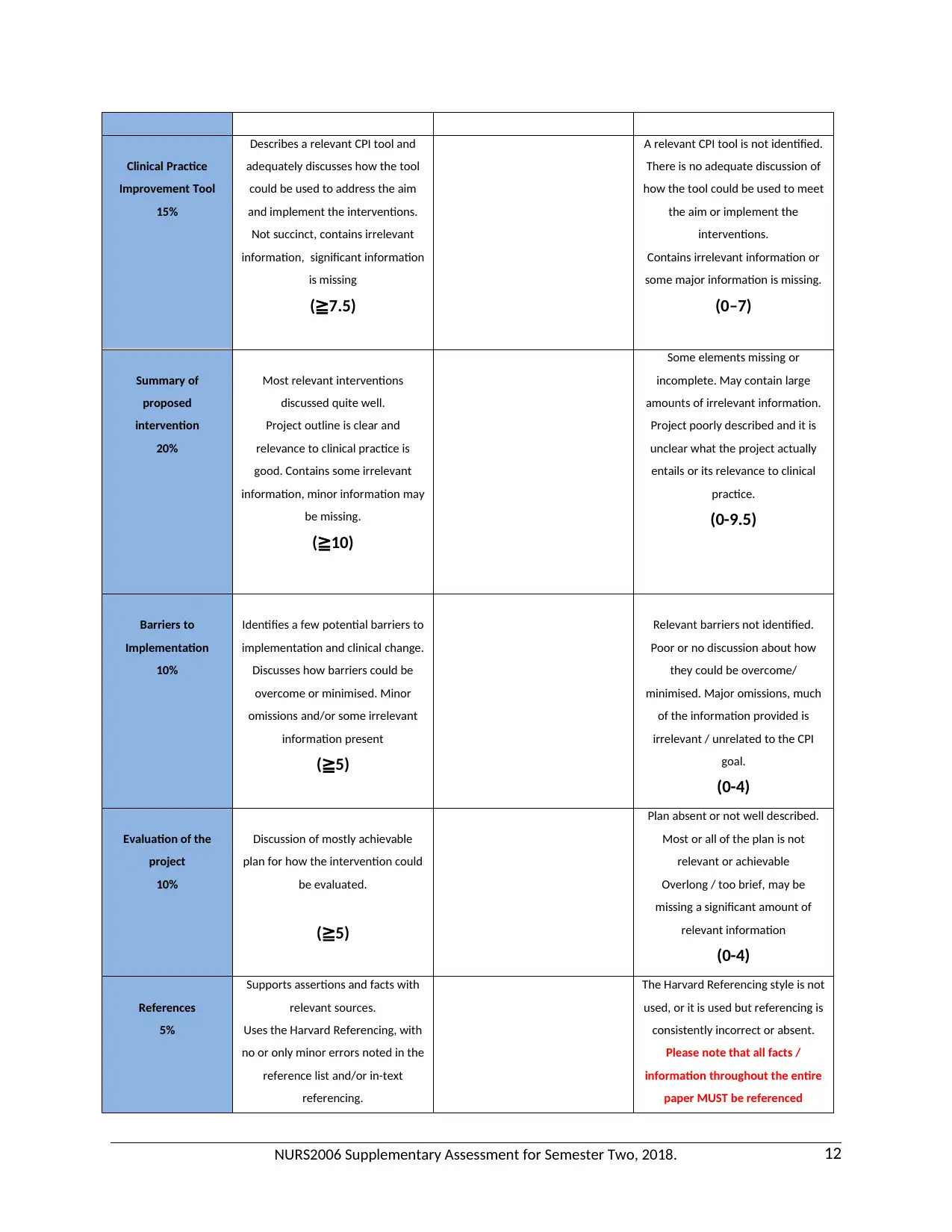
Clinical Practice
Improvement Tool
15%
Describes a relevant CPI tool and
adequately discusses how the tool
could be used to address the aim
and implement the interventions.
Not succinct, contains irrelevant
information, significant information
is missing
(≧7.5)
A relevant CPI tool is not identified.
There is no adequate discussion of
how the tool could be used to meet
the aim or implement the
interventions.
Contains irrelevant information or
some major information is missing.
(0–7)
Summary of
proposed
intervention
20%
Most relevant interventions
discussed quite well.
Project outline is clear and
relevance to clinical practice is
good. Contains some irrelevant
information, minor information may
be missing.
(≧10)
Some elements missing or
incomplete. May contain large
amounts of irrelevant information.
Project poorly described and it is
unclear what the project actually
entails or its relevance to clinical
practice.
(0-9.5)
Barriers to
Implementation
10%
Identifies a few potential barriers to
implementation and clinical change.
Discusses how barriers could be
overcome or minimised. Minor
omissions and/or some irrelevant
information present
(≧5)
Relevant barriers not identified.
Poor or no discussion about how
they could be overcome/
minimised. Major omissions, much
of the information provided is
irrelevant / unrelated to the CPI
goal.
(0-4)
Evaluation of the
project
10%
Discussion of mostly achievable
plan for how the intervention could
be evaluated.
(≧5)
Plan absent or not well described.
Most or all of the plan is not
relevant or achievable
Overlong / too brief, may be
missing a significant amount of
relevant information
(0-4)
References
5%
Supports assertions and facts with
relevant sources.
Uses the Harvard Referencing, with
no or only minor errors noted in the
reference list and/or in-text
referencing.
The Harvard Referencing style is not
used, or it is used but referencing is
consistently incorrect or absent.
Please note that all facts /
information throughout the entire
paper MUST be referenced
NURS2006 Supplementary Assessment for Semester Two, 2018. 12
Improvement Tool
15%
Describes a relevant CPI tool and
adequately discusses how the tool
could be used to address the aim
and implement the interventions.
Not succinct, contains irrelevant
information, significant information
is missing
(≧7.5)
A relevant CPI tool is not identified.
There is no adequate discussion of
how the tool could be used to meet
the aim or implement the
interventions.
Contains irrelevant information or
some major information is missing.
(0–7)
Summary of
proposed
intervention
20%
Most relevant interventions
discussed quite well.
Project outline is clear and
relevance to clinical practice is
good. Contains some irrelevant
information, minor information may
be missing.
(≧10)
Some elements missing or
incomplete. May contain large
amounts of irrelevant information.
Project poorly described and it is
unclear what the project actually
entails or its relevance to clinical
practice.
(0-9.5)
Barriers to
Implementation
10%
Identifies a few potential barriers to
implementation and clinical change.
Discusses how barriers could be
overcome or minimised. Minor
omissions and/or some irrelevant
information present
(≧5)
Relevant barriers not identified.
Poor or no discussion about how
they could be overcome/
minimised. Major omissions, much
of the information provided is
irrelevant / unrelated to the CPI
goal.
(0-4)
Evaluation of the
project
10%
Discussion of mostly achievable
plan for how the intervention could
be evaluated.
(≧5)
Plan absent or not well described.
Most or all of the plan is not
relevant or achievable
Overlong / too brief, may be
missing a significant amount of
relevant information
(0-4)
References
5%
Supports assertions and facts with
relevant sources.
Uses the Harvard Referencing, with
no or only minor errors noted in the
reference list and/or in-text
referencing.
The Harvard Referencing style is not
used, or it is used but referencing is
consistently incorrect or absent.
Please note that all facts /
information throughout the entire
paper MUST be referenced
NURS2006 Supplementary Assessment for Semester Two, 2018. 12
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 13
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





