Cultural Safety in Nursing: Impact of Personal Culture on Care
VerifiedAdded on 2023/06/05
|8
|1677
|457
Essay
AI Summary
This essay provides a reflective analysis of cultural safety in nursing practice, examining the influence of personal values, beliefs, and behaviors on the quality of patient care within a multicultural healthcare environment. The author explores values such as freedom, family, learning, and competitiveness, as well as beliefs related to spirituality, morality, social interactions, and political views, and behaviors like meticulousness, communication, punctuality and exercise. The essay acknowledges the potential for personal biases to hinder culturally safe practices and emphasizes the importance of self-awareness, effective communication, and respect for diverse cultural perspectives in providing patient-centered care. The conclusion reiterates the significance of recognizing and addressing cultural differences to ensure equitable and safe healthcare services for all patients. Desklib offers similar solved assignments for students.
Running head: Cultural Safety 1
Cultural Safety
by
Course:
Tutor:
University:
Department:
Date:
Cultural Safety
by
Course:
Tutor:
University:
Department:
Date:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Cultural Safety 2
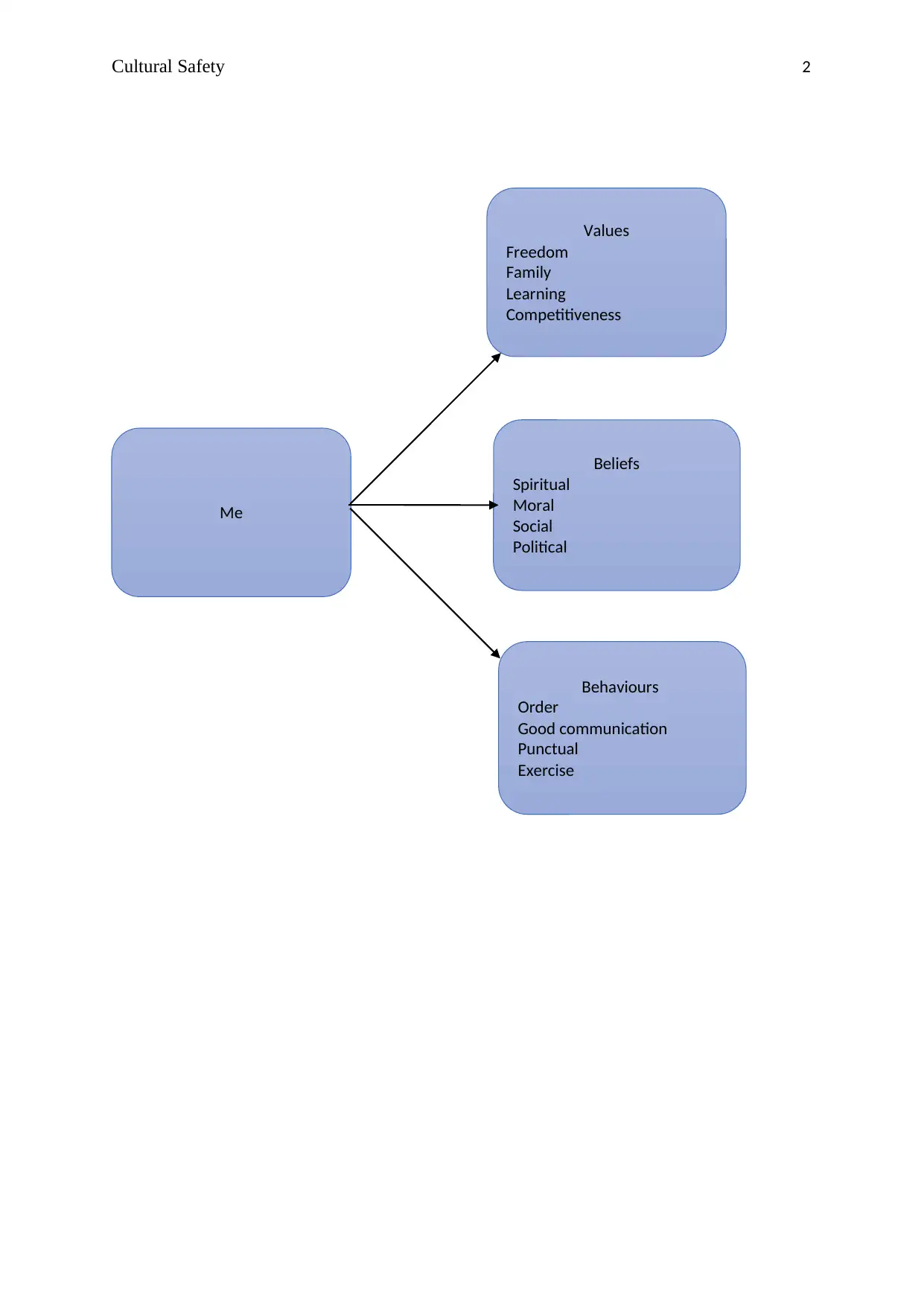
Values
Freedom
Family
Learning
Competitiveness
Beliefs
Spiritual
Moral
Social
Political
Behaviours
Order
Good communication
Punctual
Exercise
Me
Values
Freedom
Family
Learning
Competitiveness
Beliefs
Spiritual
Moral
Social
Political
Behaviours
Order
Good communication
Punctual
Exercise
Me
Cultural Safety 3
Introduction
My personal beliefs, values and behaviours affect clinical practice and the
quality of patient care. Similarly, pateints have values, beliefs and
behaviours which are likely to differ from mine. It is therefore important
that I understand that cultural differences can detract me from being a
culturally safe professional in a multicultural health care workplace
(Cherry & Jacob, 2016).
Values
Freedom
Freedom is a value that affects my nursing practice. Freedom involves
ones right to freely express their will without fear or favour. My value of
freedom contributes to a culturally safe environment because I allow
every client to speak for herself or himself. This is because I will not make
significant changes without involving the patients in decision making
process.
Family
Family involves my loved ones. Putting my family foremost is an issue that
I have always tried to maintain. Striking balance between family and work
remains an ongoing challenge for me. Life balance sustains engagement
with nursing practice and fosters one’s ability to provide quality
healthcare services (Schluter, Turner, Huntington, Bain, & McClure, 2011).
My cultural value of a family will make me a more culturally safe expert in
a multicultural healthcare environment because I will involve the family
members of the patient in decision making and updating them on the key
progress of their patient.
Learning
I believe that learning is very important because it creates awareness and
improves the knowledge and skills necessary to address any diversity in
cultural background. It is through learning that communication skills are
Introduction
My personal beliefs, values and behaviours affect clinical practice and the
quality of patient care. Similarly, pateints have values, beliefs and
behaviours which are likely to differ from mine. It is therefore important
that I understand that cultural differences can detract me from being a
culturally safe professional in a multicultural health care workplace
(Cherry & Jacob, 2016).
Values
Freedom
Freedom is a value that affects my nursing practice. Freedom involves
ones right to freely express their will without fear or favour. My value of
freedom contributes to a culturally safe environment because I allow
every client to speak for herself or himself. This is because I will not make
significant changes without involving the patients in decision making
process.
Family
Family involves my loved ones. Putting my family foremost is an issue that
I have always tried to maintain. Striking balance between family and work
remains an ongoing challenge for me. Life balance sustains engagement
with nursing practice and fosters one’s ability to provide quality
healthcare services (Schluter, Turner, Huntington, Bain, & McClure, 2011).
My cultural value of a family will make me a more culturally safe expert in
a multicultural healthcare environment because I will involve the family
members of the patient in decision making and updating them on the key
progress of their patient.
Learning
I believe that learning is very important because it creates awareness and
improves the knowledge and skills necessary to address any diversity in
cultural background. It is through learning that communication skills are
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Cultural Safety 4
learnt and improved. As a result there is improve communication between
the patient and the nurse (Kourkouta & Papathanasiou, 2014). Learning
promotes a culturally safe professional care in the work environment.
Furthermore, I will use different communication symbols to convey the
right message in a multicultural context.
Competitiveness
I believe in fair competition and rewarding based on merit, however, this
belief can easily detract me from being a culturally safe professional in a
multicultural health care environment. It is easy to offer quality services to
the most competitive or the most aggressive only because not all patients
have the same ability. According to Gurses, Carayon, and Wall (2009)
patients or caregivers that are not aggressive in seeking for healthcare
services, especially in pressured workplaces, are likely to be treated last
or receive low-quality services.
Beliefs
Spiritual
My commitment to spirituality is likely to make me become bias to those
who are of a different faith or atheists. This is because spirituality is very
central in my life and it’s believed that one can receive healing by
exercising his or her spirituality. Additionally, my spirituality is closely
connected to my cultural identity and those who expressly go contrary to
my spiritual tenets are likely to be side-lined (Kirmayer, Brass, &
Valaskakis, 2009). However, to become a culturally safe professional in
discharging my duties, I will try to avoid making mention of my spiritual
inclinations when conversing with the client
Moral
I believe that morality is closely tied to health and wellbeing (Hardy et al.,
2013). This belief is likely to detract me from being a culturally safe expert
in a multicultural healthcare environment because once I perceive a
patient to be immoral then I may end up becoming judgemental.
learnt and improved. As a result there is improve communication between
the patient and the nurse (Kourkouta & Papathanasiou, 2014). Learning
promotes a culturally safe professional care in the work environment.
Furthermore, I will use different communication symbols to convey the
right message in a multicultural context.
Competitiveness
I believe in fair competition and rewarding based on merit, however, this
belief can easily detract me from being a culturally safe professional in a
multicultural health care environment. It is easy to offer quality services to
the most competitive or the most aggressive only because not all patients
have the same ability. According to Gurses, Carayon, and Wall (2009)
patients or caregivers that are not aggressive in seeking for healthcare
services, especially in pressured workplaces, are likely to be treated last
or receive low-quality services.
Beliefs
Spiritual
My commitment to spirituality is likely to make me become bias to those
who are of a different faith or atheists. This is because spirituality is very
central in my life and it’s believed that one can receive healing by
exercising his or her spirituality. Additionally, my spirituality is closely
connected to my cultural identity and those who expressly go contrary to
my spiritual tenets are likely to be side-lined (Kirmayer, Brass, &
Valaskakis, 2009). However, to become a culturally safe professional in
discharging my duties, I will try to avoid making mention of my spiritual
inclinations when conversing with the client
Moral
I believe that morality is closely tied to health and wellbeing (Hardy et al.,
2013). This belief is likely to detract me from being a culturally safe expert
in a multicultural healthcare environment because once I perceive a
patient to be immoral then I may end up becoming judgemental.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Cultural Safety 5
However, I would ensure that my communication strategies support a
culturally safe practice by asking questions that are relevant to the
patient diagnosis only.
Social
I am a very social nurse and can easily mingle with clients from diverse
cultural backgrounds thus making it possible for me to become a
culturally safe expert in a multicultural health care environment. I do not,
therefore, segregate people based on culture. Douglas et al. (2011)
observed that the healthcare sector is a multicultural health care
environment that requires social skills in order to offer quality healthcare
services. I will use communication skills such as active listening and body
movements that are generally acceptable across cultures to foster a
culturally safe practice.
Political
I am not neutral when it comes to politics. This is likely to prevent me
from being a culturally safe expert in a multicultural healthcare setting in
which different people have different views and are of different political
view (Douglas et al., 2011). The most appropriate communication skills to
foster a culturally safe practice in such a case is to remain focused during
our conversation so as to avoid any political statements that may detract
me from achieving cultural safety at the workplace.
Behaviours
Meticulous
Since I was a child, I have always liked everything to be in order. Even in a
hospital setting, I would like the client or patient to do things in a
meticulous way, however, this is likely to hinder me from being a
culturally safe professional at work. In a multicultural setting, things are
viewed differently and I may find it difficult to get people to become
meticulous as I expect (Douglas et al., 2011).
However, I would ensure that my communication strategies support a
culturally safe practice by asking questions that are relevant to the
patient diagnosis only.
Social
I am a very social nurse and can easily mingle with clients from diverse
cultural backgrounds thus making it possible for me to become a
culturally safe expert in a multicultural health care environment. I do not,
therefore, segregate people based on culture. Douglas et al. (2011)
observed that the healthcare sector is a multicultural health care
environment that requires social skills in order to offer quality healthcare
services. I will use communication skills such as active listening and body
movements that are generally acceptable across cultures to foster a
culturally safe practice.
Political
I am not neutral when it comes to politics. This is likely to prevent me
from being a culturally safe expert in a multicultural healthcare setting in
which different people have different views and are of different political
view (Douglas et al., 2011). The most appropriate communication skills to
foster a culturally safe practice in such a case is to remain focused during
our conversation so as to avoid any political statements that may detract
me from achieving cultural safety at the workplace.
Behaviours
Meticulous
Since I was a child, I have always liked everything to be in order. Even in a
hospital setting, I would like the client or patient to do things in a
meticulous way, however, this is likely to hinder me from being a
culturally safe professional at work. In a multicultural setting, things are
viewed differently and I may find it difficult to get people to become
meticulous as I expect (Douglas et al., 2011).
Cultural Safety 6
Good communication
I have learnt good communication skills right from the time I was in
elementary school and these skills are likely to contribute to cultural
safety at work. Studies have emphasized the need for effective
communication skills in a multicultural healthcare environment for patient
centred care (Kourkouta & Papathanasiou, 2014). My good communication
skills such as active listening, the use of therapeutic touch and silence will
support the culturally safe practice because, despite the different cultures,
these skills can be utilised to develop a good rapport and support
culturally safe practices
Punctual
I am always punctual and therefore grow impatient when people are
behind schedule. This behaviour is likely to prevent me from becoming a
culturally safe expert in a multicultural health care setting. For instance,
when patients do not take appointments, it’s likely to hinder me from
keeping a culturally safe practice. I would, however, apply my
communication skills such as empathy (Kourkouta & Papathanasiou,
2014) to try to accommodate every patient
Exercise
The healthcare providers are expected to provide preventive education on
the value of exercise in the prevention and management of chronic
illnesses. Socio-economic, health status and cultural factors determine the
client’s interest and ability to participate in exercise (Chodzko-Zajko et al.,
2009). However, exercise might detract me from cultural safety because
other cultures have different beliefs in the causes of diseases, and thus
their approach to preventive care will also differ widely.
Conclusion
Values, beliefs and behaviours are inherent to my cultural identity, though
they are likely to be different from those of the client. It is not culturally
safe to segregate patients on the basis of differences in culture.
Good communication
I have learnt good communication skills right from the time I was in
elementary school and these skills are likely to contribute to cultural
safety at work. Studies have emphasized the need for effective
communication skills in a multicultural healthcare environment for patient
centred care (Kourkouta & Papathanasiou, 2014). My good communication
skills such as active listening, the use of therapeutic touch and silence will
support the culturally safe practice because, despite the different cultures,
these skills can be utilised to develop a good rapport and support
culturally safe practices
Punctual
I am always punctual and therefore grow impatient when people are
behind schedule. This behaviour is likely to prevent me from becoming a
culturally safe expert in a multicultural health care setting. For instance,
when patients do not take appointments, it’s likely to hinder me from
keeping a culturally safe practice. I would, however, apply my
communication skills such as empathy (Kourkouta & Papathanasiou,
2014) to try to accommodate every patient
Exercise
The healthcare providers are expected to provide preventive education on
the value of exercise in the prevention and management of chronic
illnesses. Socio-economic, health status and cultural factors determine the
client’s interest and ability to participate in exercise (Chodzko-Zajko et al.,
2009). However, exercise might detract me from cultural safety because
other cultures have different beliefs in the causes of diseases, and thus
their approach to preventive care will also differ widely.
Conclusion
Values, beliefs and behaviours are inherent to my cultural identity, though
they are likely to be different from those of the client. It is not culturally
safe to segregate patients on the basis of differences in culture.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Cultural Safety 7
References
Cherry, B., & Jacob, S. R. (2016). Contemporary nursing: Issues, trends,
& managemen (7th ed.). Chatswood, NSW: Elsevier Health Sciences.
Chodzko-Zajko, W. J., Proctor, D. N., Singh, M. A. F., Minson, C. T., Nigg,
C. R., Salem, G. J., & Skinner, J. S. (2009). Exercise and physical
activity for older adults. Medicine & science in sports &
exercise, 41(7), 1510-1530.
Douglas, M. K., Pierce, J. U., Rosenkoetter, M., Pacquiao, D., Callister, L.
C., Hattar-Pollara, M., ... & Purnell, L. (2011). Standards of practice
for culturally competent nursing care: 2011 update. Journal of
Transcultural Nursing, 22(4), 317-333.
Gurses, A. P., Carayon, P., & Wall, M. (2009). Impact of performance
obstacles on intensive care nurses' workload, perceived quality and
safety of care, and quality of working life. Health services
research, 44(2p1), 422-443.
Hardy, S. A., Francis, S. W., Zamboanga, B. L., Kim, S. Y., Anderson, S.
G., & Forthun, L. F. (2013). The roles of identity formation and moral
identity in college student mental health, health‐risk behaviors, and
psychological well‐being. Journal of Clinical Psychology, 69(4), 364-
382.
Kirmayer, L. J., Brass, G. M., & Valaskakis, G. G. (2009). Conclusion:
Healing/invention/tradition. Healing traditions: The mental health of
aboriginal peoples in Canada, 26, 440-472.
Kourkouta, L., & Papathanasiou, I. V. (2014). Communication in nursing
practice. Materia socio-medica, 26(1), 65-70.
Schluter, P. J., Turner, C., Huntington, A. D., Bain, C. J., & McClure, R. J.
References
Cherry, B., & Jacob, S. R. (2016). Contemporary nursing: Issues, trends,
& managemen (7th ed.). Chatswood, NSW: Elsevier Health Sciences.
Chodzko-Zajko, W. J., Proctor, D. N., Singh, M. A. F., Minson, C. T., Nigg,
C. R., Salem, G. J., & Skinner, J. S. (2009). Exercise and physical
activity for older adults. Medicine & science in sports &
exercise, 41(7), 1510-1530.
Douglas, M. K., Pierce, J. U., Rosenkoetter, M., Pacquiao, D., Callister, L.
C., Hattar-Pollara, M., ... & Purnell, L. (2011). Standards of practice
for culturally competent nursing care: 2011 update. Journal of
Transcultural Nursing, 22(4), 317-333.
Gurses, A. P., Carayon, P., & Wall, M. (2009). Impact of performance
obstacles on intensive care nurses' workload, perceived quality and
safety of care, and quality of working life. Health services
research, 44(2p1), 422-443.
Hardy, S. A., Francis, S. W., Zamboanga, B. L., Kim, S. Y., Anderson, S.
G., & Forthun, L. F. (2013). The roles of identity formation and moral
identity in college student mental health, health‐risk behaviors, and
psychological well‐being. Journal of Clinical Psychology, 69(4), 364-
382.
Kirmayer, L. J., Brass, G. M., & Valaskakis, G. G. (2009). Conclusion:
Healing/invention/tradition. Healing traditions: The mental health of
aboriginal peoples in Canada, 26, 440-472.
Kourkouta, L., & Papathanasiou, I. V. (2014). Communication in nursing
practice. Materia socio-medica, 26(1), 65-70.
Schluter, P. J., Turner, C., Huntington, A. D., Bain, C. J., & McClure, R. J.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Cultural Safety 8
(2011). Work/life balance and health: the Nurses and Midwives e‐
cohort study. International Nursing Review, 58(1), 28-36.
(2011). Work/life balance and health: the Nurses and Midwives e‐
cohort study. International Nursing Review, 58(1), 28-36.
1 out of 8
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




