Cultural Safety: Personal Reflection on Values in Healthcare HSC230
VerifiedAdded on 2023/06/09
|8
|2277
|273
Report
AI Summary
This report provides a personal reflection on cultural safety in healthcare, emphasizing the importance of self-awareness regarding one's own cultural values, beliefs, and behaviors in delivering culturally sensitive care. The author explores values such as kindness, optimism, honesty, and compassion, and beliefs related to spirituality, patient-centered care, and the role of family. The reflection also covers behaviors like communication skills, emotional stability, and enthusiasm, highlighting their impact on providing safe and comprehensive care to individuals from diverse cultural backgrounds. The author identifies areas for further development, emphasizing the need for lifelong learning and enhanced cultural competency skills to provide better care in future practices. This document is available on Desklib, a platform offering a wide range of study resources for students.

Running head: CULTURAL SAFETY IN NURSING
CULTURAL SAFETY IN NURSING
Name of the Student
Name of the university
Author’s note
CULTURAL SAFETY IN NURSING
Name of the Student
Name of the university
Author’s note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1CULTURAL SAFETY IN NURSING
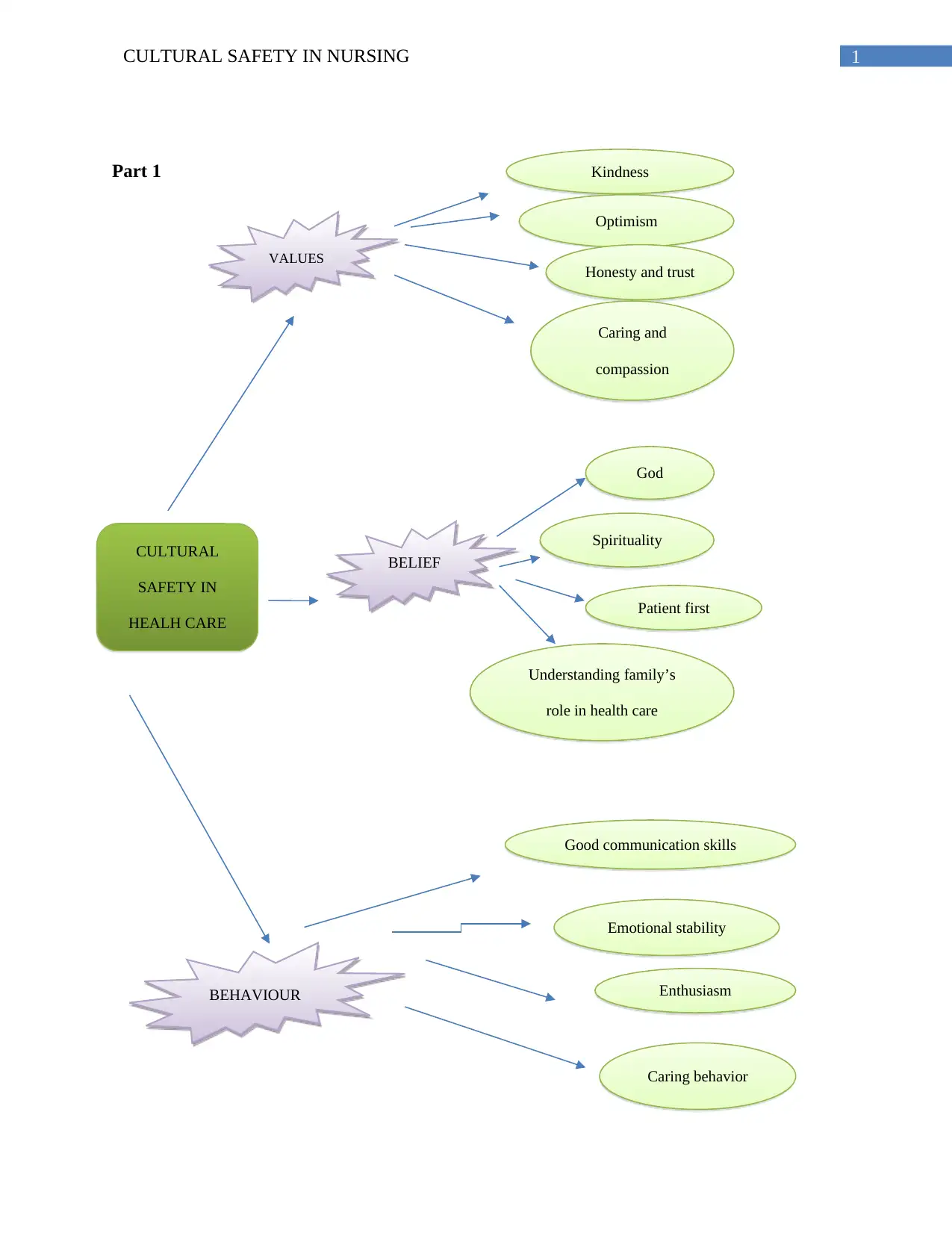
Part 1
VALUES
CULTURAL
SAFETY IN
HEALH CARE
Kindness
Optimism
Honesty and trust
Caring and
compassion
BELIEF
S
God
Spirituality
Patient first
Understanding family’s
role in health care
BEHAVIOUR
Good communication skills
Emotional stability
Enthusiasm
Caring behavior
Part 1
VALUES
CULTURAL
SAFETY IN
HEALH CARE
Kindness
Optimism
Honesty and trust
Caring and
compassion
BELIEF
S
God
Spirituality
Patient first
Understanding family’s
role in health care
BEHAVIOUR
Good communication skills
Emotional stability
Enthusiasm
Caring behavior

2CULTURAL SAFETY IN NURSING
Part 2 Reflection
Introduction
The diverse consumerism of the health care makes it essential to practice cultural safety
in health care. Self-realization of own culture, beliefs and values are necessary to understand and
accept the culture of others. In this reflective paper I would critically reflect upon my own
understanding about the cultural safety. I aim to incorporate the cultural safety in my nursing
practice by reflecting on my own culture, beliefs, values, attitudes and behavior and how they
impact the health services provided by me. In this paper I will also perform a self-assessment for
the self-judging and enhancing my professional practice.
Cultural safety
Cultural safety can be defined as an environment that is physically, socially, mentally and
emotionally safe for the people belonging to different cultural background. The concept of
cultural safety takes us above cultural awareness and acknowledgement of the differences
(Gerlach, 2012). Cultural awareness helps in practicing a care that is devoid of any inequalities
or bias. In the light of cultural safety a health care professional can improve care provision for
the patients, expose the social, political and the historical contexts of the health care, enable the
practitioners to eradicate discrimination, racism and prejudice and finally challenge the biased
power relations (Taylor & Guerin, 2010).
Self-perception about values
Over recent years we have been witnessing a downfall of the morale in health care, which
is often expressed as feelings of not being values. It is my culture and the upbringing that defines
my values. Some of the values that helps in providing a cultural safe care to the patients are
kindness, Optimism, caring and compassion, honesty and trust. Apart from the health care
provided these are some of the factors that enhance the patient care (Halligan, 2008).
Kindness is the basic element of the profession of nursing. Being kind requires a health
professional to remain vulnerable themselves while acknowledging the distress and the
vulnerability in the patient (Ellis & Rawson, 2015). Some times when we cannot offer any help
Part 2 Reflection
Introduction
The diverse consumerism of the health care makes it essential to practice cultural safety
in health care. Self-realization of own culture, beliefs and values are necessary to understand and
accept the culture of others. In this reflective paper I would critically reflect upon my own
understanding about the cultural safety. I aim to incorporate the cultural safety in my nursing
practice by reflecting on my own culture, beliefs, values, attitudes and behavior and how they
impact the health services provided by me. In this paper I will also perform a self-assessment for
the self-judging and enhancing my professional practice.
Cultural safety
Cultural safety can be defined as an environment that is physically, socially, mentally and
emotionally safe for the people belonging to different cultural background. The concept of
cultural safety takes us above cultural awareness and acknowledgement of the differences
(Gerlach, 2012). Cultural awareness helps in practicing a care that is devoid of any inequalities
or bias. In the light of cultural safety a health care professional can improve care provision for
the patients, expose the social, political and the historical contexts of the health care, enable the
practitioners to eradicate discrimination, racism and prejudice and finally challenge the biased
power relations (Taylor & Guerin, 2010).
Self-perception about values
Over recent years we have been witnessing a downfall of the morale in health care, which
is often expressed as feelings of not being values. It is my culture and the upbringing that defines
my values. Some of the values that helps in providing a cultural safe care to the patients are
kindness, Optimism, caring and compassion, honesty and trust. Apart from the health care
provided these are some of the factors that enhance the patient care (Halligan, 2008).
Kindness is the basic element of the profession of nursing. Being kind requires a health
professional to remain vulnerable themselves while acknowledging the distress and the
vulnerability in the patient (Ellis & Rawson, 2015). Some times when we cannot offer any help
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3CULTURAL SAFETY IN NURSING
to a person’s distress. Especially in case of palliative care patients, it the kindness that allows the
patient to be as they are, accepting their feelings and providing companionship to them. Kind and
caring gestures like using words of empathy, gentle patting on shoulder, warm hugs for children
can sometimes work wonders (Peate, 2012).
Although the origin of the word compassion is firmly linked with religious ideologies of
19th century, however in health care it is the provision of emotional and spiritual care for the
patients for making their health care experience more comfortable, especially when the treatment
has failed (Peate, 2012). Some of the factors that I follow to provide a compassionate care to the
patient is to communicate compassionately with the patient, showing advocacy and respecting
the dignity of the patients. I realize that as a nurse I am faced with stress and burnouts but at the
same time I also understand that I should keep the priorities of the patient in the frontline and
hence their health should not be compromised due to me.
Optimism and positivity is another value that has helped me to handle crisis with
resilience, to view difficult times as a challenge (Stagman-Tyrer, 2014). I believe that this value
of a person symbolizes the proclivity of the person to achieve his/her goal. A nurse is faced with
several adverse situations related to the care of the linguistically or culturally different people,
and multiplying responsibilities each day. In order to cope up with this they have to remain
optimistic in face of the difficulties (Stagman-Tyrer, 2014).
Honesty and trust are two related terms. It is the honesty of a person helps to build a
relationship of trust with the client. Trust helps to build a positive relationship with the client as
it creates the scope for openness with the patient and the family members involved in the care
(Straughair, 2012). I have realized that with the increased complexities of the consumerism in
health care, the patients have become vulnerable and are seeking for answers. Hence I always try
to keep a transparency regarding the disclosure of the health care and remain honest and
accountable to my practices. I realize that I need to work more on establishing rapport with the
patients so that I can build the credibility that I truly understand the value of the patients.
Beliefs
While I was working with an aboriginal patient I understood how spirituality and mental
wellbeing affects the physical health of a patient. Hence one of my beliefs is spirituality.
to a person’s distress. Especially in case of palliative care patients, it the kindness that allows the
patient to be as they are, accepting their feelings and providing companionship to them. Kind and
caring gestures like using words of empathy, gentle patting on shoulder, warm hugs for children
can sometimes work wonders (Peate, 2012).
Although the origin of the word compassion is firmly linked with religious ideologies of
19th century, however in health care it is the provision of emotional and spiritual care for the
patients for making their health care experience more comfortable, especially when the treatment
has failed (Peate, 2012). Some of the factors that I follow to provide a compassionate care to the
patient is to communicate compassionately with the patient, showing advocacy and respecting
the dignity of the patients. I realize that as a nurse I am faced with stress and burnouts but at the
same time I also understand that I should keep the priorities of the patient in the frontline and
hence their health should not be compromised due to me.
Optimism and positivity is another value that has helped me to handle crisis with
resilience, to view difficult times as a challenge (Stagman-Tyrer, 2014). I believe that this value
of a person symbolizes the proclivity of the person to achieve his/her goal. A nurse is faced with
several adverse situations related to the care of the linguistically or culturally different people,
and multiplying responsibilities each day. In order to cope up with this they have to remain
optimistic in face of the difficulties (Stagman-Tyrer, 2014).
Honesty and trust are two related terms. It is the honesty of a person helps to build a
relationship of trust with the client. Trust helps to build a positive relationship with the client as
it creates the scope for openness with the patient and the family members involved in the care
(Straughair, 2012). I have realized that with the increased complexities of the consumerism in
health care, the patients have become vulnerable and are seeking for answers. Hence I always try
to keep a transparency regarding the disclosure of the health care and remain honest and
accountable to my practices. I realize that I need to work more on establishing rapport with the
patients so that I can build the credibility that I truly understand the value of the patients.
Beliefs
While I was working with an aboriginal patient I understood how spirituality and mental
wellbeing affects the physical health of a patient. Hence one of my beliefs is spirituality.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4CULTURAL SAFETY IN NURSING
Previously I had a very vague notion regarding the role of the spirituality, which is common in
the health care practice of the aboriginals (Connell Meehan, 2012). I have understood that the
aboriginal’s connectedness with the land, kingship and spirit contribute to their mental
wellbeing. The spiritual dimension of care seeks a meaningful explanation of illness that
considers, family, person and the community issue and it is the spirituality that enables a person
to perceive his/her life in a different way (Mitchell & Golden, 2012). I have learnt that certain
spiritual practices such as meditation can be beneficial for the treatment of chronic pain,
depression, hostility, insomnia, anxiety and premenstrual problem, although it should be kept in
mind that spiritual beliefs of certain patients or the caregivers can directly contradict medical
science.
Another belief that helps me to deliver a patient centered cares, is to keep the interest of
the patient at the first place (Salimi & Azimpour, 2013). Being a health care professional I have
always believed on going an extra mile for the wellbeing of the patient, for example, while
working on a pediatric patient, I often used to gift goodies to children at the time of discharge or
often had to work extra time in case of some emergency conditions. As a nurse it is natural to
work beyond the comfort zone or time, aiming to abide by the ethical principle of beneficence.
This ethical principle requires the health care professionals to provide maximum benefits to the
patient.
My third belief is to understand the role of the families in providing a culturally safe
care. Family plays a crucial role in the decision making process as it is the family that shaped up
the personality , behaviors or the health care habits of a person. Hence I have believed that a
culturally safe caregiving is not possible, unless I communicate with the families to facilitate a
shared decision making.
The final belief on which I will be reflecting is my belief in god. It is this belief that has
led me to believe that every religion, race and ethnicities are equal in the eyes of god, so we
don’t have the right to discriminate human beings. It is this belief that has helped me to believe
in patient’s autonomy, that every patient has the right to decide or express their opinions.
Previously I had a very vague notion regarding the role of the spirituality, which is common in
the health care practice of the aboriginals (Connell Meehan, 2012). I have understood that the
aboriginal’s connectedness with the land, kingship and spirit contribute to their mental
wellbeing. The spiritual dimension of care seeks a meaningful explanation of illness that
considers, family, person and the community issue and it is the spirituality that enables a person
to perceive his/her life in a different way (Mitchell & Golden, 2012). I have learnt that certain
spiritual practices such as meditation can be beneficial for the treatment of chronic pain,
depression, hostility, insomnia, anxiety and premenstrual problem, although it should be kept in
mind that spiritual beliefs of certain patients or the caregivers can directly contradict medical
science.
Another belief that helps me to deliver a patient centered cares, is to keep the interest of
the patient at the first place (Salimi & Azimpour, 2013). Being a health care professional I have
always believed on going an extra mile for the wellbeing of the patient, for example, while
working on a pediatric patient, I often used to gift goodies to children at the time of discharge or
often had to work extra time in case of some emergency conditions. As a nurse it is natural to
work beyond the comfort zone or time, aiming to abide by the ethical principle of beneficence.
This ethical principle requires the health care professionals to provide maximum benefits to the
patient.
My third belief is to understand the role of the families in providing a culturally safe
care. Family plays a crucial role in the decision making process as it is the family that shaped up
the personality , behaviors or the health care habits of a person. Hence I have believed that a
culturally safe caregiving is not possible, unless I communicate with the families to facilitate a
shared decision making.
The final belief on which I will be reflecting is my belief in god. It is this belief that has
led me to believe that every religion, race and ethnicities are equal in the eyes of god, so we
don’t have the right to discriminate human beings. It is this belief that has helped me to believe
in patient’s autonomy, that every patient has the right to decide or express their opinions.
5CULTURAL SAFETY IN NURSING
Behavior
Behavior determines the way, how the care is being conducted to the patient. My culture
and my family have helped me to incorporate these behaviors- good communication skills,
emotional stability, enthusiastic and caring behavior. Communication skills are a primary skill
required in nursing where one needs to communicate with patients, patient’s family and the peers
(Manias, 2015). Although I always remain mindful about asking consent before touching the
patient before any physical examination but it cannot be expected to obtain a consent before
giving a compassionate hug or a friendly pat, but any kind of touching without consent can be
considered to be an act of disrespect in many cultures. Apart from verbal communication, non-
verbal communication is also important in providing care to geriatric or the pediatric patient
(Taylor et al., 2013). I make it sure that my facial expressions are of empathy and the patients
feel that they are being cared for, yet I sometimes realize that I can work more in understanding
the non-verbal expression of the patients, such as facial grimacing due to pain.
In spite of having good communication skills, I believe that I should assimilate more in
others culture to communicate to them effectively. I have noticed that individuals with emotional
stability are less likely to face stress or burnout or exhibit strong emotional responses in stressful
conditions. I will need to work on my emotional stability to work in stressful conditions. My
enthusiastic behavior has helped me lot to reach out and get involved in conversation with people
with different cultural background. Being enthusiastic to leaning about a culture has helped me
out to accept and assimilate in other culture and I truly enjoy to explore about other cultures. My
love for people pushes to me to know about their culture and provide care to them. However I
wish to indulge in lifelong learning and thrive to develop my personal and professional skills in
nursing.
Conclusion
In conclusion it can be said that cultural safety is the key to provide a safe and
comprehensive care to person irrespective of their race, ethnicities and cultures. Each of the
beliefs and the values that have been discussed have helped me to polish my concepts about
cultural safety and can be possibly used by some to achieve cultural sensitiveness. I believe that,
I need to thrive more on my competency skills, which requires a lifelong learning. However I
Behavior
Behavior determines the way, how the care is being conducted to the patient. My culture
and my family have helped me to incorporate these behaviors- good communication skills,
emotional stability, enthusiastic and caring behavior. Communication skills are a primary skill
required in nursing where one needs to communicate with patients, patient’s family and the peers
(Manias, 2015). Although I always remain mindful about asking consent before touching the
patient before any physical examination but it cannot be expected to obtain a consent before
giving a compassionate hug or a friendly pat, but any kind of touching without consent can be
considered to be an act of disrespect in many cultures. Apart from verbal communication, non-
verbal communication is also important in providing care to geriatric or the pediatric patient
(Taylor et al., 2013). I make it sure that my facial expressions are of empathy and the patients
feel that they are being cared for, yet I sometimes realize that I can work more in understanding
the non-verbal expression of the patients, such as facial grimacing due to pain.
In spite of having good communication skills, I believe that I should assimilate more in
others culture to communicate to them effectively. I have noticed that individuals with emotional
stability are less likely to face stress or burnout or exhibit strong emotional responses in stressful
conditions. I will need to work on my emotional stability to work in stressful conditions. My
enthusiastic behavior has helped me lot to reach out and get involved in conversation with people
with different cultural background. Being enthusiastic to leaning about a culture has helped me
out to accept and assimilate in other culture and I truly enjoy to explore about other cultures. My
love for people pushes to me to know about their culture and provide care to them. However I
wish to indulge in lifelong learning and thrive to develop my personal and professional skills in
nursing.
Conclusion
In conclusion it can be said that cultural safety is the key to provide a safe and
comprehensive care to person irrespective of their race, ethnicities and cultures. Each of the
beliefs and the values that have been discussed have helped me to polish my concepts about
cultural safety and can be possibly used by some to achieve cultural sensitiveness. I believe that,
I need to thrive more on my competency skills, which requires a lifelong learning. However I
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6CULTURAL SAFETY IN NURSING
hope to enhance my cultural competency skills and devote myself to the care of people in future
practices.
References
Connell Meehan, T. (2012). Spirituality and spiritual care from a Careful Nursing perspective.
Journal of Nursing Management, 20(8), 990-1001.https://doi.org/10.1111/j.1365-
2834.2012.01462.x
Ellis, J. M., & Rawson, H. (2015). Nurses' and personal care assistants' role in improving the
relocation of older people into nursing homes. Journal of Clinical Nursing, 24(13-14),
2005-2013.https://doi.org/10.1111/jocn.12798
Gerlach, A. J. (2012). A critical reflection on the concept of cultural safety. Canadian Journal of
Occupational Therapy, 79(3), 151-158.https://doi.org/10.2182/cjot.2012.79.3.4
Halligan, A. (2008). The importance of values in healthcare. Journal of the Royal Society of
Medicine, 101(10), 480–481. http://doi.org/10.1258/jrsm.08k019
Manias, E. (2015). Communication relating to family members' involvement and understandings
about patients' medication management in hospital. Health Expectations, 18(5), 850-866.
doi:10.1111/hex.12057
Mitchell, P., & Golden, R. (2012). Core principles & values of effective team-based health care.
National Academy of
Sciences.http://thuvienso.thanglong.edu.vn/handle/DHTL_123456789/3976
hope to enhance my cultural competency skills and devote myself to the care of people in future
practices.
References
Connell Meehan, T. (2012). Spirituality and spiritual care from a Careful Nursing perspective.
Journal of Nursing Management, 20(8), 990-1001.https://doi.org/10.1111/j.1365-
2834.2012.01462.x
Ellis, J. M., & Rawson, H. (2015). Nurses' and personal care assistants' role in improving the
relocation of older people into nursing homes. Journal of Clinical Nursing, 24(13-14),
2005-2013.https://doi.org/10.1111/jocn.12798
Gerlach, A. J. (2012). A critical reflection on the concept of cultural safety. Canadian Journal of
Occupational Therapy, 79(3), 151-158.https://doi.org/10.2182/cjot.2012.79.3.4
Halligan, A. (2008). The importance of values in healthcare. Journal of the Royal Society of
Medicine, 101(10), 480–481. http://doi.org/10.1258/jrsm.08k019
Manias, E. (2015). Communication relating to family members' involvement and understandings
about patients' medication management in hospital. Health Expectations, 18(5), 850-866.
doi:10.1111/hex.12057
Mitchell, P., & Golden, R. (2012). Core principles & values of effective team-based health care.
National Academy of
Sciences.http://thuvienso.thanglong.edu.vn/handle/DHTL_123456789/3976
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7CULTURAL SAFETY IN NURSING
Peate, I. (2012). Kindness, caring and compassion. Australian Nursing and Midwifery Journal,
19(7), 16.
Salimi, S., &Azimpour, A. (2013). Determinants of Nurses’ Caring Behaviors (DNCB):
Preliminary Validation of a Scale. Journal of Caring Sciences, 2(4), 269–278.
http://doi.org/10.5681/jcs.2013.032
Stagman-Tyrer, D. (2014). Resiliency and the nurse leader: The importance of equanimity,
optimism, and perseverance. Nursing management, 45(6), 46-50. doi:
10.1097/01.NUMA.0000449763.99370.7f
Straughair, C. (2012). Exploring compassion: implications for contemporary nursing. Part 1.
British Journal of Nursing, 21(3), 160-164.https://doi.org/10.12968/bjon.2012.21.3.160
Taylor, K. A., Lindeman, M. A., Stothers, K., Piper, K., &Kuipers, P. (2012). Intercultural
communications in remote Aboriginal Australian communities: What works in dementia
education and management?.Health Sociology Review, 21(2),
208-219./doi/abs/10.5172/hesr.2012.21.2.208
Taylor, K., & Guerin, P. (2010). Health care and Indigenous Australians: Cultural safety in
practice(2nd ed., pp. 9-23) South Yarra: Palgrave Macmillan.
https://books.google.co.in/books/about/Health_Care_and_Indigenous_Australians.html?
id=T9XZpdz2HKQC&redir_esc=y
Peate, I. (2012). Kindness, caring and compassion. Australian Nursing and Midwifery Journal,
19(7), 16.
Salimi, S., &Azimpour, A. (2013). Determinants of Nurses’ Caring Behaviors (DNCB):
Preliminary Validation of a Scale. Journal of Caring Sciences, 2(4), 269–278.
http://doi.org/10.5681/jcs.2013.032
Stagman-Tyrer, D. (2014). Resiliency and the nurse leader: The importance of equanimity,
optimism, and perseverance. Nursing management, 45(6), 46-50. doi:
10.1097/01.NUMA.0000449763.99370.7f
Straughair, C. (2012). Exploring compassion: implications for contemporary nursing. Part 1.
British Journal of Nursing, 21(3), 160-164.https://doi.org/10.12968/bjon.2012.21.3.160
Taylor, K. A., Lindeman, M. A., Stothers, K., Piper, K., &Kuipers, P. (2012). Intercultural
communications in remote Aboriginal Australian communities: What works in dementia
education and management?.Health Sociology Review, 21(2),
208-219./doi/abs/10.5172/hesr.2012.21.2.208
Taylor, K., & Guerin, P. (2010). Health care and Indigenous Australians: Cultural safety in
practice(2nd ed., pp. 9-23) South Yarra: Palgrave Macmillan.
https://books.google.co.in/books/about/Health_Care_and_Indigenous_Australians.html?
id=T9XZpdz2HKQC&redir_esc=y
1 out of 8
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





