Cushing’s Syndrome - Assignnment
VerifiedAdded on 2021/05/31
|10
|2607
|42
AI Summary
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: CUSHING’S SYNDROME 1
Cushing’s Syndrome
Name
Institution
Cushing’s Syndrome
Name
Institution
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
CUSHING’S SYNDROME 2
Cushing’s Syndrome
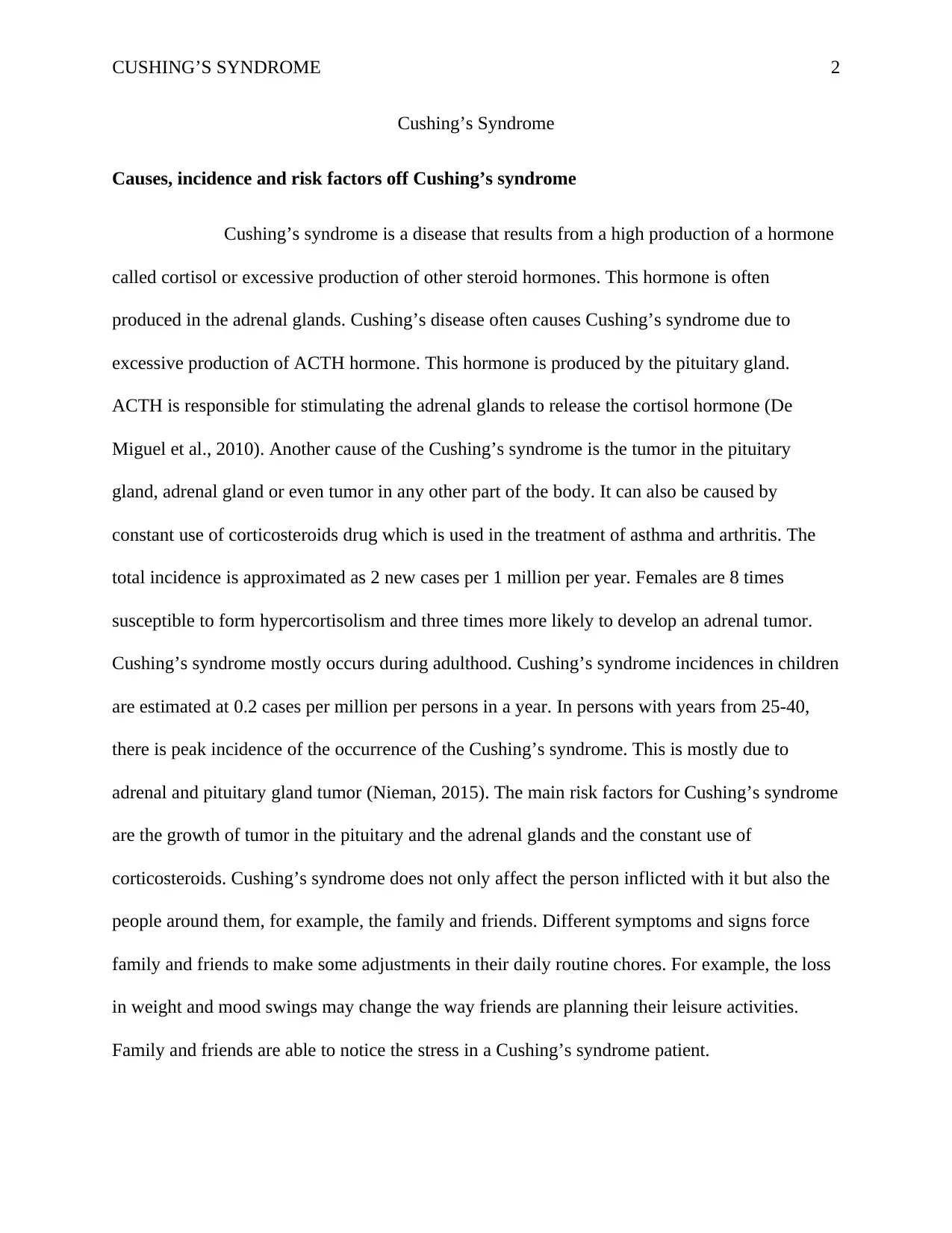
Causes, incidence and risk factors off Cushing’s syndrome
Cushing’s syndrome is a disease that results from a high production of a hormone
called cortisol or excessive production of other steroid hormones. This hormone is often
produced in the adrenal glands. Cushing’s disease often causes Cushing’s syndrome due to
excessive production of ACTH hormone. This hormone is produced by the pituitary gland.
ACTH is responsible for stimulating the adrenal glands to release the cortisol hormone (De
Miguel et al., 2010). Another cause of the Cushing’s syndrome is the tumor in the pituitary
gland, adrenal gland or even tumor in any other part of the body. It can also be caused by
constant use of corticosteroids drug which is used in the treatment of asthma and arthritis. The
total incidence is approximated as 2 new cases per 1 million per year. Females are 8 times
susceptible to form hypercortisolism and three times more likely to develop an adrenal tumor.
Cushing’s syndrome mostly occurs during adulthood. Cushing’s syndrome incidences in children
are estimated at 0.2 cases per million per persons in a year. In persons with years from 25-40,
there is peak incidence of the occurrence of the Cushing’s syndrome. This is mostly due to
adrenal and pituitary gland tumor (Nieman, 2015). The main risk factors for Cushing’s syndrome
are the growth of tumor in the pituitary and the adrenal glands and the constant use of
corticosteroids. Cushing’s syndrome does not only affect the person inflicted with it but also the
people around them, for example, the family and friends. Different symptoms and signs force
family and friends to make some adjustments in their daily routine chores. For example, the loss
in weight and mood swings may change the way friends are planning their leisure activities.
Family and friends are able to notice the stress in a Cushing’s syndrome patient.
Cushing’s Syndrome
Causes, incidence and risk factors off Cushing’s syndrome
Cushing’s syndrome is a disease that results from a high production of a hormone
called cortisol or excessive production of other steroid hormones. This hormone is often
produced in the adrenal glands. Cushing’s disease often causes Cushing’s syndrome due to
excessive production of ACTH hormone. This hormone is produced by the pituitary gland.
ACTH is responsible for stimulating the adrenal glands to release the cortisol hormone (De
Miguel et al., 2010). Another cause of the Cushing’s syndrome is the tumor in the pituitary
gland, adrenal gland or even tumor in any other part of the body. It can also be caused by
constant use of corticosteroids drug which is used in the treatment of asthma and arthritis. The
total incidence is approximated as 2 new cases per 1 million per year. Females are 8 times
susceptible to form hypercortisolism and three times more likely to develop an adrenal tumor.
Cushing’s syndrome mostly occurs during adulthood. Cushing’s syndrome incidences in children
are estimated at 0.2 cases per million per persons in a year. In persons with years from 25-40,
there is peak incidence of the occurrence of the Cushing’s syndrome. This is mostly due to
adrenal and pituitary gland tumor (Nieman, 2015). The main risk factors for Cushing’s syndrome
are the growth of tumor in the pituitary and the adrenal glands and the constant use of
corticosteroids. Cushing’s syndrome does not only affect the person inflicted with it but also the
people around them, for example, the family and friends. Different symptoms and signs force
family and friends to make some adjustments in their daily routine chores. For example, the loss
in weight and mood swings may change the way friends are planning their leisure activities.
Family and friends are able to notice the stress in a Cushing’s syndrome patient.
CUSHING’S SYNDROME 3
The physical appearance of a patient with Cushing’s syndrome may even change. Change in
physical appearance may include loss of hair, gain in weight and probably the formation of acne
and skin infections on the skin (Nieman, 2015). This might make the patient feel like sidelining
themselves from family and friends. They will totally isolate themselves from them. Patients also
tend to be weak and are not always able to do some things, for example, walking through the
stairs. This limits them from having fun because they do not have enough energy to walk around
or even go shopping and go outdoors (Nieman, 2014). This, therefore, affects the family life of
the patient and how the patient relates to their partners.
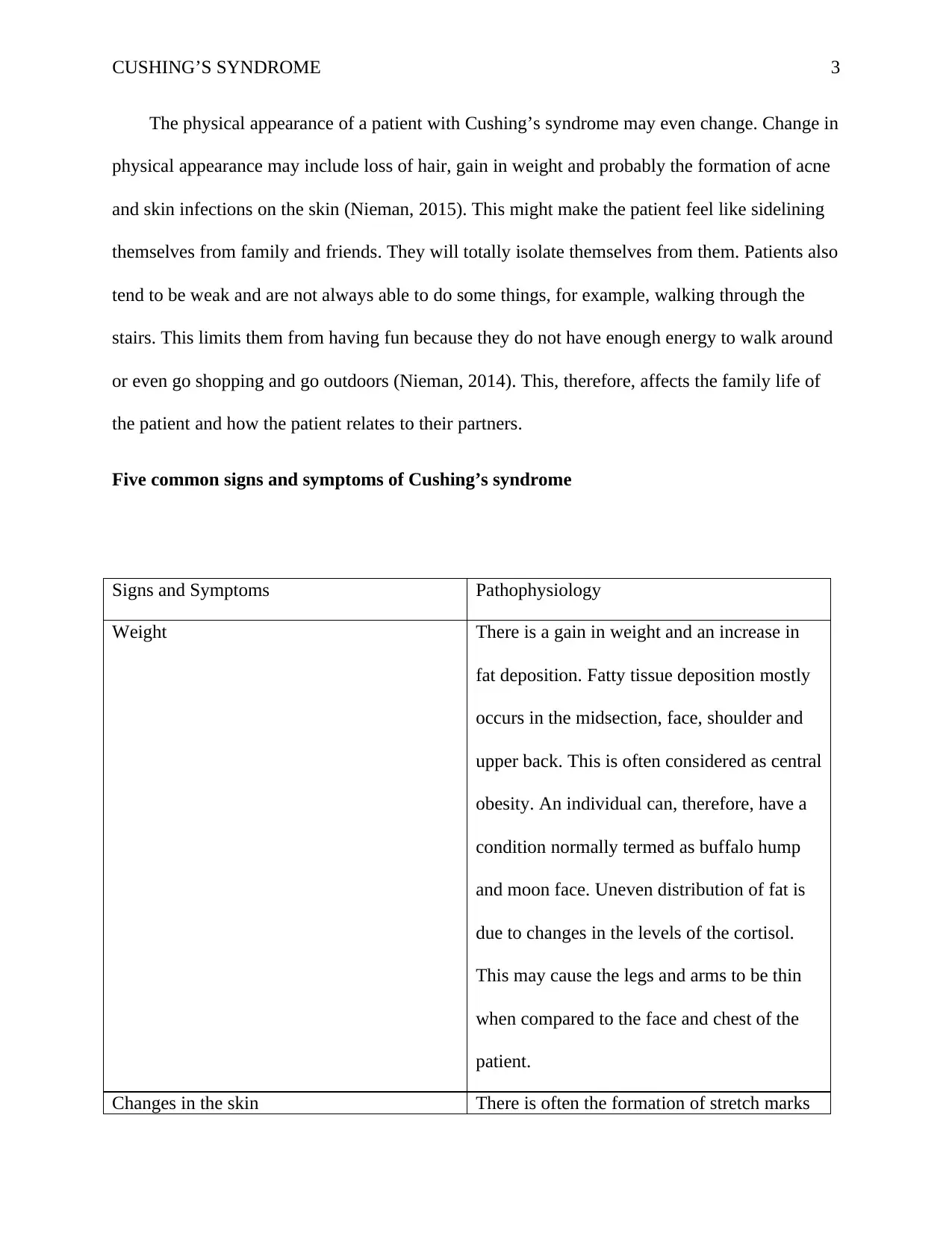
Five common signs and symptoms of Cushing’s syndrome
Signs and Symptoms Pathophysiology
Weight There is a gain in weight and an increase in
fat deposition. Fatty tissue deposition mostly
occurs in the midsection, face, shoulder and
upper back. This is often considered as central
obesity. An individual can, therefore, have a
condition normally termed as buffalo hump
and moon face. Uneven distribution of fat is
due to changes in the levels of the cortisol.
This may cause the legs and arms to be thin
when compared to the face and chest of the
patient.
Changes in the skin There is often the formation of stretch marks
The physical appearance of a patient with Cushing’s syndrome may even change. Change in
physical appearance may include loss of hair, gain in weight and probably the formation of acne
and skin infections on the skin (Nieman, 2015). This might make the patient feel like sidelining
themselves from family and friends. They will totally isolate themselves from them. Patients also
tend to be weak and are not always able to do some things, for example, walking through the
stairs. This limits them from having fun because they do not have enough energy to walk around
or even go shopping and go outdoors (Nieman, 2014). This, therefore, affects the family life of
the patient and how the patient relates to their partners.
Five common signs and symptoms of Cushing’s syndrome
Signs and Symptoms Pathophysiology
Weight There is a gain in weight and an increase in
fat deposition. Fatty tissue deposition mostly
occurs in the midsection, face, shoulder and
upper back. This is often considered as central
obesity. An individual can, therefore, have a
condition normally termed as buffalo hump
and moon face. Uneven distribution of fat is
due to changes in the levels of the cortisol.
This may cause the legs and arms to be thin
when compared to the face and chest of the
patient.
Changes in the skin There is often the formation of stretch marks
CUSHING’S SYNDROME 4
around the buttocks, thighs, arms and breasts.
There are purple and pinkish lines in the areas
where the skin has stretched. There may be
spots on the shoulders, chest and the face. It
also characterized by the darkening of the
neck. The ability of the skin to be healed is
reduced. When the insect bites an individual
with the syndrome, it takes longer to heal.
This is also caused by increased levels of
cortisol in the body. Skin proteins are often
broken down causing the blood vessels
weakening.
Bones and Muscles Bones and muscles of the patient often
weaken due to increasing levels of cortisol
hormone. This might cause bone fractures
because the density of bone is reduced. This
may also lead to osteoporosis.
Psychological Symptoms Patients with Cushing’s syndrome often feel
tired so easily. This is due to depression and
symptoms of psychology which includes
anxiety and sadness, anger and irritability and
finally the control over emotion is reduced.
Individuals always experience mood swings
around the buttocks, thighs, arms and breasts.
There are purple and pinkish lines in the areas
where the skin has stretched. There may be
spots on the shoulders, chest and the face. It
also characterized by the darkening of the
neck. The ability of the skin to be healed is
reduced. When the insect bites an individual
with the syndrome, it takes longer to heal.
This is also caused by increased levels of
cortisol in the body. Skin proteins are often
broken down causing the blood vessels
weakening.
Bones and Muscles Bones and muscles of the patient often
weaken due to increasing levels of cortisol
hormone. This might cause bone fractures
because the density of bone is reduced. This
may also lead to osteoporosis.
Psychological Symptoms Patients with Cushing’s syndrome often feel
tired so easily. This is due to depression and
symptoms of psychology which includes
anxiety and sadness, anger and irritability and
finally the control over emotion is reduced.
Individuals always experience mood swings
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
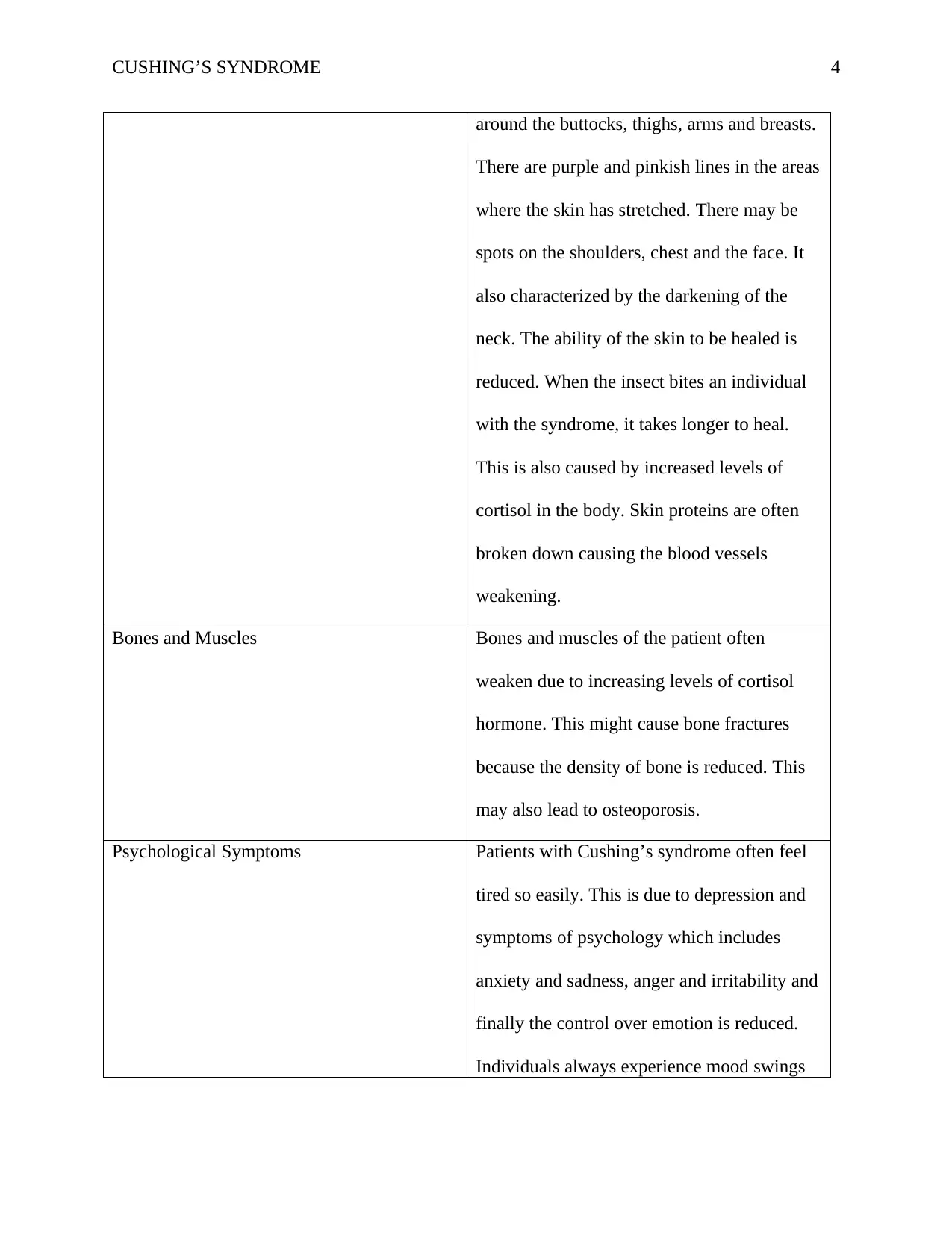
CUSHING’S SYNDROME 5
and experience difficulty in controlling their
emotions. Due to this, individuals are prone to
crying and laughing at odd moments.
High blood pressure There are high chances of blood pressure for
individuals with ectopic Cushing’s syndrome.
This is often referred to as hypertension.
When there is high blood pressure then the
more severe are the symptodiagnosisms felt.
This arises due to increased secretion of
glucocorticoids. The reduction in blood
pressure is often due to a reduction in the
cortisol hormone. When the levels of cortisol
are increased then blood pressure increases.
Effects of cortisol always increase on both
type 1 and type 2.
(Mazziotti et al, 2011). (Nieman, 2015)
Classes of drugs used for patients with Cushing’s syndrome
Steroidogenesis Inhibitors
This is the types of drugs that used in controlling the cortisol production. This is
done by decreasing the production of steroid hormone by the adrenal glands. It achieves this by
inhibiting one or more enzyme that aid in steroid synthesis. Inhibitors of steroidogenesis can be
used mostly for blocking the production of cortisol either completely or partially (Fleseriu et al.,
2012). The doses of steroidogenesis inhibitors are often adjusted so that the normal cortisol level
and experience difficulty in controlling their
emotions. Due to this, individuals are prone to
crying and laughing at odd moments.
High blood pressure There are high chances of blood pressure for
individuals with ectopic Cushing’s syndrome.
This is often referred to as hypertension.
When there is high blood pressure then the
more severe are the symptodiagnosisms felt.
This arises due to increased secretion of
glucocorticoids. The reduction in blood
pressure is often due to a reduction in the
cortisol hormone. When the levels of cortisol
are increased then blood pressure increases.
Effects of cortisol always increase on both
type 1 and type 2.
(Mazziotti et al, 2011). (Nieman, 2015)
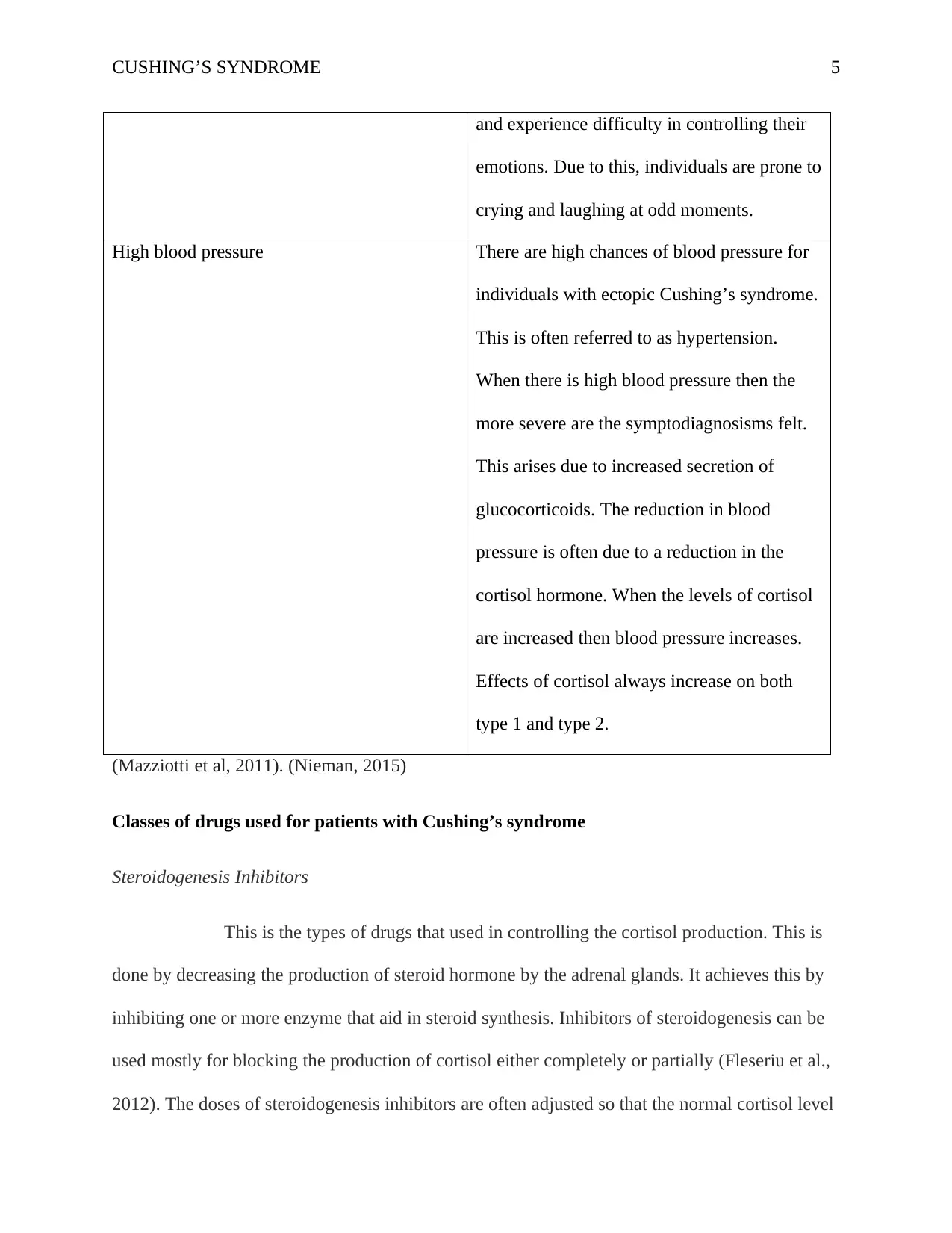
Classes of drugs used for patients with Cushing’s syndrome
Steroidogenesis Inhibitors
This is the types of drugs that used in controlling the cortisol production. This is
done by decreasing the production of steroid hormone by the adrenal glands. It achieves this by
inhibiting one or more enzyme that aid in steroid synthesis. Inhibitors of steroidogenesis can be
used mostly for blocking the production of cortisol either completely or partially (Fleseriu et al.,
2012). The doses of steroidogenesis inhibitors are often adjusted so that the normal cortisol level
CUSHING’S SYNDROME 6
of urine diagnosis. This is done when the partial blockade is required. Whenever complete
blockade is needed, doses of steroidogenesis is given such that complete inhibition of the
synthesis of cortisol and glucocorticoids is achieved. After this, the physiologic needs are
replaced. Examples of steroidogenesis inhibitors include fluconazole aminoglutethimide,
mitotane, ketoconazole, metyrapone and etomidate. KTZ and metyrapone are mostly used
because they have good properties of inhibiting the various pathways of steroids, therefore,
reducing the synthesis of cortisol (Feelders et al., 2010). Mitotane action, on the other hand, is
prolonged upon use. KTZ acts as an antifungal agent blocking multiple steps of the synthesis.
Glucocorticoid receptor antagonist mifepristone
This works differently from other medications as it helps in blocking the action of
cortisol on the body instead of decreasing the amount of cortisol produced (Fleseriu et al, 2012).
The physical appearance of the patients is often achieved when these drugs are used. There is
also a blood sugar improvement when used. Side effects of mifepristone are significantly high.
Mifepristone antagonizes the negative feedback of pituitary glucocorticoids (Fleseriu &
Petersenn, 2012). The drugs are mostly absorbed immediately into the body and are administered
only once on a daily basis because it has a long life span in the body. It always blocks the
progesterone hormone in the female, therefore, altering the menstrual cycle. Individuals using
the drug often have a high level of cortisol because it does not lower its levels. It helps in the
improvement of blood levels and blood sugar in the body and aids in the loss of weight. It is
therefore not advisable for patients planning to have children. This drug has many adverse
effects on the patient, for example, nausea, muscle discomfort and loss of appetite (Fleseriu et al,
2012).
Nursing care strategies.
of urine diagnosis. This is done when the partial blockade is required. Whenever complete
blockade is needed, doses of steroidogenesis is given such that complete inhibition of the
synthesis of cortisol and glucocorticoids is achieved. After this, the physiologic needs are
replaced. Examples of steroidogenesis inhibitors include fluconazole aminoglutethimide,
mitotane, ketoconazole, metyrapone and etomidate. KTZ and metyrapone are mostly used
because they have good properties of inhibiting the various pathways of steroids, therefore,
reducing the synthesis of cortisol (Feelders et al., 2010). Mitotane action, on the other hand, is
prolonged upon use. KTZ acts as an antifungal agent blocking multiple steps of the synthesis.
Glucocorticoid receptor antagonist mifepristone
This works differently from other medications as it helps in blocking the action of
cortisol on the body instead of decreasing the amount of cortisol produced (Fleseriu et al, 2012).
The physical appearance of the patients is often achieved when these drugs are used. There is
also a blood sugar improvement when used. Side effects of mifepristone are significantly high.
Mifepristone antagonizes the negative feedback of pituitary glucocorticoids (Fleseriu &
Petersenn, 2012). The drugs are mostly absorbed immediately into the body and are administered
only once on a daily basis because it has a long life span in the body. It always blocks the
progesterone hormone in the female, therefore, altering the menstrual cycle. Individuals using
the drug often have a high level of cortisol because it does not lower its levels. It helps in the
improvement of blood levels and blood sugar in the body and aids in the loss of weight. It is
therefore not advisable for patients planning to have children. This drug has many adverse
effects on the patient, for example, nausea, muscle discomfort and loss of appetite (Fleseriu et al,
2012).
Nursing care strategies.
CUSHING’S SYNDROME 7
A nurse should try as much as possible to be close to a patient with Cushing’s
syndrome. The first thing I will do is to assess the patient. This helps in focusing on the effects of
the body with the high concentration of cortex upon exposure to aldosterone and cortisol levels.
In this step, the nurse should focus on the health history of the patient (Tritos et al., 2011). This
involves the level of activity of the patient and patient’s capability to do their own activities. The
other things to be assessed is the physical appearance of the patient. The observation of the skin
is considered, for example, bruising, infection or even edema. Thereafter, the nurse should assess
the mental functionality of the patient for example mood swings, depression level and
environmental awareness.
The second thing is the diagnosis according to the patient assessment data. The major
diagnosis includes a risk of injury which is related to weakness (Juszczak & Grossman, 2012).
This may result from the environment compromising with the individual’s health. In this, the
skin of the individual is frequently checked especially for bruises. The feces also are also
assessed for occult blood to check whether gastrointestinal bleeding has begun. The client is also
prepared for evaluation of the bone density. Another diagnosis is the risk to infection (Juszczak
& Grossman, 2012). It this, the patient is diagnosed if he is at an increased risk of being infected
with pathogenic infections. The patient is then advised by the nurse on how to maintain hygiene
for example hand washing. Another thing a nurse diagnosis is body image disturbance. This
involves the physical appearance of the patient and patient’s activity level. Another diagnosis is
the disturbed thought processes which include the mood swings of the patient (Juszczak &
Grossman, 2012).
The third step is the nurse planning and goals. The nurse tries to reduce what he had
diagnosed. For example, decreasing the risk of injury, decreasing the infection risk, increasing
A nurse should try as much as possible to be close to a patient with Cushing’s
syndrome. The first thing I will do is to assess the patient. This helps in focusing on the effects of
the body with the high concentration of cortex upon exposure to aldosterone and cortisol levels.
In this step, the nurse should focus on the health history of the patient (Tritos et al., 2011). This
involves the level of activity of the patient and patient’s capability to do their own activities. The
other things to be assessed is the physical appearance of the patient. The observation of the skin
is considered, for example, bruising, infection or even edema. Thereafter, the nurse should assess
the mental functionality of the patient for example mood swings, depression level and
environmental awareness.
The second thing is the diagnosis according to the patient assessment data. The major
diagnosis includes a risk of injury which is related to weakness (Juszczak & Grossman, 2012).
This may result from the environment compromising with the individual’s health. In this, the
skin of the individual is frequently checked especially for bruises. The feces also are also
assessed for occult blood to check whether gastrointestinal bleeding has begun. The client is also
prepared for evaluation of the bone density. Another diagnosis is the risk to infection (Juszczak
& Grossman, 2012). It this, the patient is diagnosed if he is at an increased risk of being infected
with pathogenic infections. The patient is then advised by the nurse on how to maintain hygiene
for example hand washing. Another thing a nurse diagnosis is body image disturbance. This
involves the physical appearance of the patient and patient’s activity level. Another diagnosis is
the disturbed thought processes which include the mood swings of the patient (Juszczak &
Grossman, 2012).
The third step is the nurse planning and goals. The nurse tries to reduce what he had
diagnosed. For example, decreasing the risk of injury, decreasing the infection risk, increasing
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CUSHING’S SYNDROME 8
self-care activities ability, body image improvement, mental function improvement, and skin
integrity improvement (Tiemensma et al., 2011). In order to decrease injury risk, the nurse
provides an environment where bones and injuries to the tissues s very minimal. The nurse also
assists a weak patient to avoid falls and collision with the furniture (Tiemensma et al., 2010).
The nurse should advise the patient to eat food rich in vitamin D and calcium to reduce the risk
of wasting muscles. When preparing the patient for surgery, glucose levels and blood stools
should be monitored. This is because diabetes mellitus is one of the common problems
(Tiemensma et al., 2011). When improving skin integrity, meticulous skin care should be used to
avoid a fragile skin. The nurse should also talk with the patient about the cause of emotional
stress and help them deal depression and mood swings. The nurse should also encourage the
patients to verbalize their emotions and thoughts. Before discharging the patient family and the
patient should be taught home care guidelines, for example, modifying the diet. the diet should
be rich in calcium and vitamins. The patient is also told to monitor the blood pressure levels,
weight and their sugar levels. The nurse should also encourage the patient to follow up
appointments.
References
self-care activities ability, body image improvement, mental function improvement, and skin
integrity improvement (Tiemensma et al., 2011). In order to decrease injury risk, the nurse
provides an environment where bones and injuries to the tissues s very minimal. The nurse also
assists a weak patient to avoid falls and collision with the furniture (Tiemensma et al., 2010).
The nurse should advise the patient to eat food rich in vitamin D and calcium to reduce the risk
of wasting muscles. When preparing the patient for surgery, glucose levels and blood stools
should be monitored. This is because diabetes mellitus is one of the common problems
(Tiemensma et al., 2011). When improving skin integrity, meticulous skin care should be used to
avoid a fragile skin. The nurse should also talk with the patient about the cause of emotional
stress and help them deal depression and mood swings. The nurse should also encourage the
patients to verbalize their emotions and thoughts. Before discharging the patient family and the
patient should be taught home care guidelines, for example, modifying the diet. the diet should
be rich in calcium and vitamins. The patient is also told to monitor the blood pressure levels,
weight and their sugar levels. The nurse should also encourage the patient to follow up
appointments.
References
CUSHING’S SYNDROME 9
De Miguel, V., Redal, M. A., Viale, M. L., Kahan, M., Glerean, M., Beskow, A., & Fainstein
Day, P. (2010). Aberrant expression of glucagon receptors in adrenal glands of a patient
with Cushing’s syndrome and ACTH-independent macronodular adrenal
hyperplasia. Medicina (B Aires), 70(3), 254-256.
Feelders, R. A., Hofland, L. J., & De Herder, W. W. (2010). Medical treatment of Cushing’s
syndrome: adrenal-blocking drugs and ketaconazole. Neuroendocrinology, 92(Suppl. 1),
111-115.
Fleseriu, M., & Petersenn, S. (2012). Medical management of Cushing’s disease: what is the
future?. Pituitary, 15(3), 330-341.
Fleseriu, M., Biller, B. M., Findling, J. W., Molitch, M. E., Schteingart, D. E., Gross, C., ... &
SEISMIC Study Investigators include. (2012). Mifepristone, a glucocorticoid receptor
antagonist, produces clinical and metabolic benefits in patients with Cushing's
syndrome. The Journal of Clinical Endocrinology & Metabolism, 97(6), 2039-
2049.Valassi, E., Crespo, I., Gich, I., Rodríguez, J., & Webb, S. M. (2012). A reappraisal
of the medical therapy with steroidogenesis inhibitors in Cushing's syndrome. Clinical
endocrinology, 77(5), 735-742.
Juszczak, A., & Grossman, A. (2012). The investigation of Cushing syndrome: essentials in
optimizing appropriate diagnosis and management. Annals of Saudi medicine, 32(5), 455.
Mazziotti, G., Gazzaruso, C., & Giustina, A. (2011). Diabetes in Cushing syndrome: basic and
clinical aspects. Trends in Endocrinology & Metabolism, 22(12), 499-506.
De Miguel, V., Redal, M. A., Viale, M. L., Kahan, M., Glerean, M., Beskow, A., & Fainstein
Day, P. (2010). Aberrant expression of glucagon receptors in adrenal glands of a patient
with Cushing’s syndrome and ACTH-independent macronodular adrenal
hyperplasia. Medicina (B Aires), 70(3), 254-256.
Feelders, R. A., Hofland, L. J., & De Herder, W. W. (2010). Medical treatment of Cushing’s
syndrome: adrenal-blocking drugs and ketaconazole. Neuroendocrinology, 92(Suppl. 1),
111-115.
Fleseriu, M., & Petersenn, S. (2012). Medical management of Cushing’s disease: what is the
future?. Pituitary, 15(3), 330-341.
Fleseriu, M., Biller, B. M., Findling, J. W., Molitch, M. E., Schteingart, D. E., Gross, C., ... &
SEISMIC Study Investigators include. (2012). Mifepristone, a glucocorticoid receptor
antagonist, produces clinical and metabolic benefits in patients with Cushing's
syndrome. The Journal of Clinical Endocrinology & Metabolism, 97(6), 2039-
2049.Valassi, E., Crespo, I., Gich, I., Rodríguez, J., & Webb, S. M. (2012). A reappraisal
of the medical therapy with steroidogenesis inhibitors in Cushing's syndrome. Clinical
endocrinology, 77(5), 735-742.
Juszczak, A., & Grossman, A. (2012). The investigation of Cushing syndrome: essentials in
optimizing appropriate diagnosis and management. Annals of Saudi medicine, 32(5), 455.
Mazziotti, G., Gazzaruso, C., & Giustina, A. (2011). Diabetes in Cushing syndrome: basic and
clinical aspects. Trends in Endocrinology & Metabolism, 22(12), 499-506.
CUSHING’S SYNDROME 10
Nieman, L. (2014). Epidemiology and clinical manifestations of Cushing’s
syndrome. UpToDate. Waltham (MA): Available at: http://www. uptodate.
com/contents/epidemiology-and-clinical-manifestations-of-cushings-syndrome.
Nieman, L. K. (2015). Cushing's syndrome: update on signs, symptoms and biochemical
screening. European journal of endocrinology, 173(4), M33-M38.
Tiemensma, J., Kaptein, A. A., Pereira, A. M., Smit, J. W., Romijn, J. A., & Biermasz, N. R.
(2011). Coping strategies in patients after treatment for functioning or nonfunctioning
pituitary adenomas. The Journal of Clinical Endocrinology & Metabolism, 96(4), 964-
971.
Tiemensma, J., Kokshoorn, N. E., Biermasz, N. R., Keijser, B. J. S., Wassenaar, M. J.,
Middelkoop, H. A., ... & Romijn, J. A. (2010). Subtle cognitive impairments in patients
with long-term cure of Cushing’s disease. The Journal of Clinical Endocrinology &
Metabolism, 95(6), 2699-2714.
Tritos, N. A., Biller, B. M., & Swearingen, B. (2011). Management of Cushing disease. Nature
Reviews Endocrinology, 7(5), 279.
Nieman, L. (2014). Epidemiology and clinical manifestations of Cushing’s
syndrome. UpToDate. Waltham (MA): Available at: http://www. uptodate.
com/contents/epidemiology-and-clinical-manifestations-of-cushings-syndrome.
Nieman, L. K. (2015). Cushing's syndrome: update on signs, symptoms and biochemical
screening. European journal of endocrinology, 173(4), M33-M38.
Tiemensma, J., Kaptein, A. A., Pereira, A. M., Smit, J. W., Romijn, J. A., & Biermasz, N. R.
(2011). Coping strategies in patients after treatment for functioning or nonfunctioning
pituitary adenomas. The Journal of Clinical Endocrinology & Metabolism, 96(4), 964-
971.
Tiemensma, J., Kokshoorn, N. E., Biermasz, N. R., Keijser, B. J. S., Wassenaar, M. J.,
Middelkoop, H. A., ... & Romijn, J. A. (2010). Subtle cognitive impairments in patients
with long-term cure of Cushing’s disease. The Journal of Clinical Endocrinology &
Metabolism, 95(6), 2699-2714.
Tritos, N. A., Biller, B. M., & Swearingen, B. (2011). Management of Cushing disease. Nature
Reviews Endocrinology, 7(5), 279.
1 out of 10
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.




