CVD Health Promotion for Aboriginal & Torres Strait Islander People
VerifiedAdded on 2022/08/29
|10
|2850
|24
Report
AI Summary
This report presents a comprehensive needs assessment focusing on cardiovascular disease (CVD) health promotion within Aboriginal and Torres Strait Islander populations. It begins with an introduction highlighting the significant health disparities in life expectancy between Indigenous and non-Indigenous Australians, emphasizing the critical need for interventions. The report analyzes the health needs of the target population, including the high prevalence of ischemic heart failure, particularly among younger Indigenous Australians, and the associated risk factors. It examines health status, demographic and geographic distributions, social, environmental, and behavioral determinants, and the existing service needs. The assessment also explores workforce availability, efficiency, and effectiveness of current programs. Furthermore, it identifies opportunities, priorities, and options for improvement, culminating in specific recommendations for actions, such as recalibrating risk assessment tools and expanding access to healthcare. Stakeholder analysis is included to demonstrate the involvement of different groups. The report concludes by emphasizing the importance of funding and expanded programs to improve the quality of life for Aboriginal and Torres Strait Islanders.

Running Head: CVD HEALTH PROMOTION AMONGST ABORIGINAL & TORRES POPULATION
CVD HEALTH PROMOTION AMONGST ABORIGINAL & TORRES POPULATION
Name of the Student:
Name of the University:
Author Note:
CVD HEALTH PROMOTION AMONGST ABORIGINAL & TORRES POPULATION
Name of the Student:
Name of the University:
Author Note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1CVD HEALTH PROMOTION AMONGST ABORIGINAL & TORRES POPULATION
Introduction:
The new 10-year report of the Closing the Gap Program, aiming at decreasing the gap in life
expectancy between Aboriginals and Torres Strait Islanders and other Australians by 2031 (Jones), found
that somehow the lifespan with both Indigenous and non-Indigenous Australians increased between
2005–2007 and 2010–2012, but the difference did not significantly reduce, and is still about 10 years old.
The article below reflects on the need to encourage avoidance of cardiovascular disorders by Indigenous
and Torres Strait citizens (Woodruffe et al., 2015). The article also demonstrates the importance of the
particular demographic community and the support required to implement the management and
promotion system (Jones et al., 2018) to increase quality of life.
Discussion:
Analysis of health needs of target population:
Ischaemic heart failure is the main cause of death for Australian Aboriginal and Torres Strait
Islanders, with a population rate 1.8 times that of non-Indigenous Australians where the percentage for
young people is far higher. These stand at 12.0 percent of heart disease-triggered deaths in 30–39 year old
Aboriginal Australians, relative to 3.8 percent for non-Indigenous citizens in this age range. While the
statistic is observed to be very small in Indigenous communities, it is recommended to add 5 percent to
the calculated 5-year risk score in cultures with lower prevalence of cardiovascular risk factors and
disease, whereas in societies with high prevalence of cardiovascular risk factors and disease it is proposed
that 5 percent be added to the assessed 5-year risk amount. The data given by their population survey
findings from the Australian Aboriginal and Torres Strait Islander Health Study, taken into account the
incidence of coronary disease and the utilization of lipid-lowering medication among Indigenous
Australians. Investigators recorded that 4.7% of participants aged 25–34 without pre-existing coronary
illness were at elevated extreme risk of cardiovascular disease, greater than the percentage of high
Introduction:
The new 10-year report of the Closing the Gap Program, aiming at decreasing the gap in life
expectancy between Aboriginals and Torres Strait Islanders and other Australians by 2031 (Jones), found
that somehow the lifespan with both Indigenous and non-Indigenous Australians increased between
2005–2007 and 2010–2012, but the difference did not significantly reduce, and is still about 10 years old.
The article below reflects on the need to encourage avoidance of cardiovascular disorders by Indigenous
and Torres Strait citizens (Woodruffe et al., 2015). The article also demonstrates the importance of the
particular demographic community and the support required to implement the management and
promotion system (Jones et al., 2018) to increase quality of life.
Discussion:
Analysis of health needs of target population:
Ischaemic heart failure is the main cause of death for Australian Aboriginal and Torres Strait
Islanders, with a population rate 1.8 times that of non-Indigenous Australians where the percentage for
young people is far higher. These stand at 12.0 percent of heart disease-triggered deaths in 30–39 year old
Aboriginal Australians, relative to 3.8 percent for non-Indigenous citizens in this age range. While the
statistic is observed to be very small in Indigenous communities, it is recommended to add 5 percent to
the calculated 5-year risk score in cultures with lower prevalence of cardiovascular risk factors and
disease, whereas in societies with high prevalence of cardiovascular risk factors and disease it is proposed
that 5 percent be added to the assessed 5-year risk amount. The data given by their population survey
findings from the Australian Aboriginal and Torres Strait Islander Health Study, taken into account the
incidence of coronary disease and the utilization of lipid-lowering medication among Indigenous
Australians. Investigators recorded that 4.7% of participants aged 25–34 without pre-existing coronary
illness were at elevated extreme risk of cardiovascular disease, greater than the percentage of high
2CVD HEALTH PROMOTION AMONGST ABORIGINAL & TORRES POPULATION
absolute risk (4.0%) among non-Indigenous Australians aged 45–54 years. There was a recurrent
circulatory disease in 12 per cent of the Indigenous and Torres Strait Islander communities. Aboriginal
and Torres Strait Islander populations were 20 per cent more likely than non-Indigenous Australians to
report circulatory disease. Since 2001, indigenous Australians with a recurrent circulatory condition have
seen a significant increase.
Health status:
Indigenous people are more likely to die from CVD than non-Indigenous residents, with
extremely high mortality risk levels for individuals in both young and middle ages. Coronary heart
disease (CHD), stroke (CBVD), and hypertension are the main medical conditions linked with increased
mortality among indigenous people. Such illnesses make up 76 percent of all cardiovascular deaths.
Rheumatic heart disease (RHD), now a rare cause of death in non-Aboriginal Australians, also causes
major deaths within the indigenous population, mainly due to the incidence of acute rheumatic fever
(ARF), especially in children. In 2010, CVD was the leading cause of death for indigenous populations,
responsible for 668 indigenous deaths (26 percent of all indigenous deaths). CHD and CBVD constituted
the two major popular causal factors of death from CVD. CHD accounted for 349 deaths among
indigenous peoples in 2010, 13 per cent of all fatalities and 52 per cent of cardiovascular fatalities among
indigenous peoples (also the leading cause of death for non-indigenous peoples). CHD mortality rates for
indigenous groups were almost twice as high as those for non-indigenous societies (179 deaths per
100,000, compared with 89 deaths per 100,000).
Demography and geography of population:
The Australian Statistics Bureau (ABS) reported the Indigenous and Torres Strait Islander
community at 30 June 2011, based on data gathered as part of the 2011 Community and Housing Survey,
to be 669,736 individuals. This is projected that the NSW population will be the highest (208,364
aboriginal people), followed by Qld (188,892), WA (88,277), and NT (68,901). The NT has the highest
absolute risk (4.0%) among non-Indigenous Australians aged 45–54 years. There was a recurrent
circulatory disease in 12 per cent of the Indigenous and Torres Strait Islander communities. Aboriginal
and Torres Strait Islander populations were 20 per cent more likely than non-Indigenous Australians to
report circulatory disease. Since 2001, indigenous Australians with a recurrent circulatory condition have
seen a significant increase.
Health status:
Indigenous people are more likely to die from CVD than non-Indigenous residents, with
extremely high mortality risk levels for individuals in both young and middle ages. Coronary heart
disease (CHD), stroke (CBVD), and hypertension are the main medical conditions linked with increased
mortality among indigenous people. Such illnesses make up 76 percent of all cardiovascular deaths.
Rheumatic heart disease (RHD), now a rare cause of death in non-Aboriginal Australians, also causes
major deaths within the indigenous population, mainly due to the incidence of acute rheumatic fever
(ARF), especially in children. In 2010, CVD was the leading cause of death for indigenous populations,
responsible for 668 indigenous deaths (26 percent of all indigenous deaths). CHD and CBVD constituted
the two major popular causal factors of death from CVD. CHD accounted for 349 deaths among
indigenous peoples in 2010, 13 per cent of all fatalities and 52 per cent of cardiovascular fatalities among
indigenous peoples (also the leading cause of death for non-indigenous peoples). CHD mortality rates for
indigenous groups were almost twice as high as those for non-indigenous societies (179 deaths per
100,000, compared with 89 deaths per 100,000).
Demography and geography of population:
The Australian Statistics Bureau (ABS) reported the Indigenous and Torres Strait Islander
community at 30 June 2011, based on data gathered as part of the 2011 Community and Housing Survey,
to be 669,736 individuals. This is projected that the NSW population will be the highest (208,364
aboriginal people), followed by Qld (188,892), WA (88,277), and NT (68,901). The NT has the highest
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3CVD HEALTH PROMOTION AMONGST ABORIGINAL & TORRES POPULATION
number of Indigenous people in the nation (29.8%) and the lowest in Vic (0.9%). The indigenous
community around Australia is far more scattered than the non-indigenous population is. Slightly over
half of the indigenous community resides in regions known as 'big cities' or 'core rural' zones, relative to
about nine-tenths of the non-indigenous people.
Social, environmental, and behavioral health determinants:
There are various triggers of CVD in indigenous people, but the disorder and its symptoms may
well be considerably reduced by modifying behavioural and biochemical risk factors, both of which are
influenced by mitigating factors such as the severe socioeconomic poverty experienced by indigenous
people. Often modifiable risk factors for CVD include smoking, alcohol, physical inactivity, eating,
overweight and obesity, diabetes, increased blood pressure and high blood cholesterol. These risk factors
are strongly associated with nearly 70 per cent of indigenous people's CVD load. Consumption of
nicotine is the key cause that contributes to overweight and obesity, elevated blood cholesterol, physical
inactivity and high blood pressure. For other Australians, a large percentage of the CVD strain is
attributed to the same risk factors, but the major causes are elevated blood pressure and high blood
cholesterol, followed by excessive inactivity, overweight and obesity, alcohol and inadequate
consumption of fruit and vegetables. Improvements in indigenous people's physical activity and nutrition
played a key role in the growth of CVD and diabetes, particularly in the second half of the 20th century,
as major modifiable risk factors for cardiovascular disease and other chronic conditions (Gubhajuet al.,
2019). Psychosocial problems and illnesses affecting indigenous people's behavioral and emotional well-
being are also considered to be main trigger factors for CVD and contribute to higher incidence. Financial
opportunities, natural infrastructure and socio-economic conditions have a significant effect on the well-
being of people, communities and culture as a whole. In addition, these effects are visible in measures
such as education, jobs, incomes, housing, resource exposure, social networks, land ties, discrimination
and incarceration. Indigenous populations experience significant disadvantage on all these tests.
number of Indigenous people in the nation (29.8%) and the lowest in Vic (0.9%). The indigenous
community around Australia is far more scattered than the non-indigenous population is. Slightly over
half of the indigenous community resides in regions known as 'big cities' or 'core rural' zones, relative to
about nine-tenths of the non-indigenous people.
Social, environmental, and behavioral health determinants:
There are various triggers of CVD in indigenous people, but the disorder and its symptoms may
well be considerably reduced by modifying behavioural and biochemical risk factors, both of which are
influenced by mitigating factors such as the severe socioeconomic poverty experienced by indigenous
people. Often modifiable risk factors for CVD include smoking, alcohol, physical inactivity, eating,
overweight and obesity, diabetes, increased blood pressure and high blood cholesterol. These risk factors
are strongly associated with nearly 70 per cent of indigenous people's CVD load. Consumption of
nicotine is the key cause that contributes to overweight and obesity, elevated blood cholesterol, physical
inactivity and high blood pressure. For other Australians, a large percentage of the CVD strain is
attributed to the same risk factors, but the major causes are elevated blood pressure and high blood
cholesterol, followed by excessive inactivity, overweight and obesity, alcohol and inadequate
consumption of fruit and vegetables. Improvements in indigenous people's physical activity and nutrition
played a key role in the growth of CVD and diabetes, particularly in the second half of the 20th century,
as major modifiable risk factors for cardiovascular disease and other chronic conditions (Gubhajuet al.,
2019). Psychosocial problems and illnesses affecting indigenous people's behavioral and emotional well-
being are also considered to be main trigger factors for CVD and contribute to higher incidence. Financial
opportunities, natural infrastructure and socio-economic conditions have a significant effect on the well-
being of people, communities and culture as a whole. In addition, these effects are visible in measures
such as education, jobs, incomes, housing, resource exposure, social networks, land ties, discrimination
and incarceration. Indigenous populations experience significant disadvantage on all these tests.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4CVD HEALTH PROMOTION AMONGST ABORIGINAL & TORRES POPULATION
Analysis of service needs:
In 2010, CVD was the leading cause of death for indigenous peoples, responsible for 668 deaths
of indigenous peoples (26% of all indigenous peoples 'deaths)[5]. CHD and CBVD represented the two
most severe causes of CVD death. For Indigenous males, fatalities from this disease were more frequent
than for Indigenous females, with a sex ratio of 2.1. In 2010, CHD was accounted for 349 indigenous
deaths, 13 per cent of all deaths and 52 per cent of cardiovascular deaths by indigenous citizens. CHD
mortality rates were almost twice as high for Aboriginal populations, than for non-Indigenous
communities. Most of the morbidity and mortality induced by CVD is preventable, both as regards the
early occurrence of the disease (primary prevention) and as regards the treatment and containment of
existing disease (secondary prevention and rehabilitation) (Woodruffe et al., 2015). CVD has attracted
substantial attention in Australia owing to the fairly preventable existence of the disease, and the
subsequent high degree of health risk and expense. This emphasis has contributed to advancements in
cardiovascular health in modern Australia but these innovations have not been completely incorporated
into indigenous cultures. This is illustrated by the continued elevated rates of prevalence, hospitalization,
and mortality in Aboriginal people with CVD.
Cardiovascular Risk Assessment Program for Aboriginal & Torres Islander
Traits:
Australia's total cardiovascular disease (CVD) risk evaluation algorithm(Paigea et al., 2019) first
determines which people follow the requirements for a scientifically defined elevated risk of CVD and,
among those that do not fulfill such requirements, the Framingham Risk Equation applies to predict an
individual's risk of CVD over the next 5 years. For Aboriginal and Torres Strait Islanders and non-
Indigenous Australians, the same risk calculation is used, but there is difference in inherent vulnerability
between the two groups, with the former facing a larger prevalence of cardiovascular risk factors.
Analysis of service needs:
In 2010, CVD was the leading cause of death for indigenous peoples, responsible for 668 deaths
of indigenous peoples (26% of all indigenous peoples 'deaths)[5]. CHD and CBVD represented the two
most severe causes of CVD death. For Indigenous males, fatalities from this disease were more frequent
than for Indigenous females, with a sex ratio of 2.1. In 2010, CHD was accounted for 349 indigenous
deaths, 13 per cent of all deaths and 52 per cent of cardiovascular deaths by indigenous citizens. CHD
mortality rates were almost twice as high for Aboriginal populations, than for non-Indigenous
communities. Most of the morbidity and mortality induced by CVD is preventable, both as regards the
early occurrence of the disease (primary prevention) and as regards the treatment and containment of
existing disease (secondary prevention and rehabilitation) (Woodruffe et al., 2015). CVD has attracted
substantial attention in Australia owing to the fairly preventable existence of the disease, and the
subsequent high degree of health risk and expense. This emphasis has contributed to advancements in
cardiovascular health in modern Australia but these innovations have not been completely incorporated
into indigenous cultures. This is illustrated by the continued elevated rates of prevalence, hospitalization,
and mortality in Aboriginal people with CVD.
Cardiovascular Risk Assessment Program for Aboriginal & Torres Islander
Traits:
Australia's total cardiovascular disease (CVD) risk evaluation algorithm(Paigea et al., 2019) first
determines which people follow the requirements for a scientifically defined elevated risk of CVD and,
among those that do not fulfill such requirements, the Framingham Risk Equation applies to predict an
individual's risk of CVD over the next 5 years. For Aboriginal and Torres Strait Islanders and non-
Indigenous Australians, the same risk calculation is used, but there is difference in inherent vulnerability
between the two groups, with the former facing a larger prevalence of cardiovascular risk factors.
5CVD HEALTH PROMOTION AMONGST ABORIGINAL & TORRES POPULATION
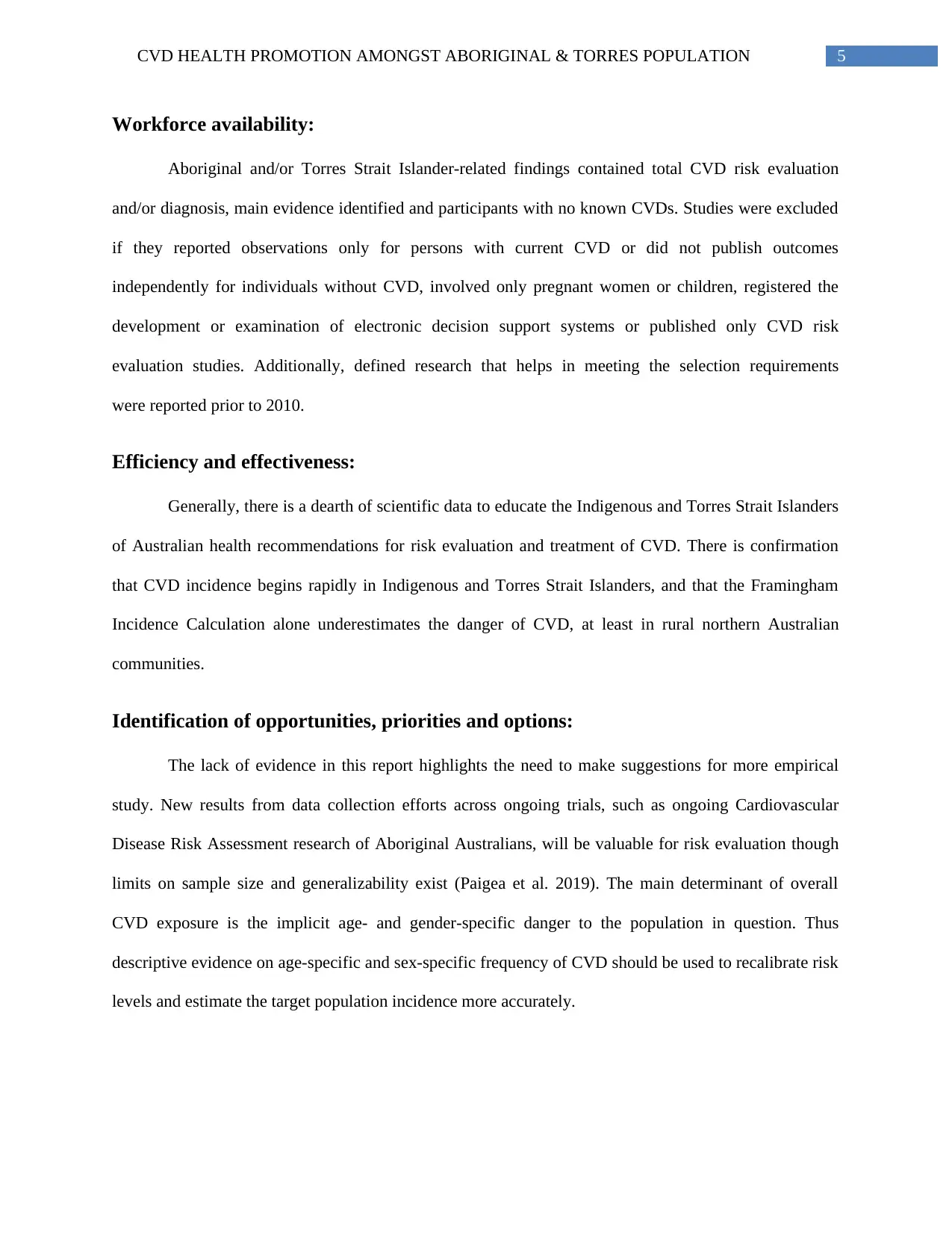
Workforce availability:
Aboriginal and/or Torres Strait Islander-related findings contained total CVD risk evaluation
and/or diagnosis, main evidence identified and participants with no known CVDs. Studies were excluded
if they reported observations only for persons with current CVD or did not publish outcomes
independently for individuals without CVD, involved only pregnant women or children, registered the
development or examination of electronic decision support systems or published only CVD risk
evaluation studies. Additionally, defined research that helps in meeting the selection requirements
were reported prior to 2010.
Efficiency and effectiveness:
Generally, there is a dearth of scientific data to educate the Indigenous and Torres Strait Islanders
of Australian health recommendations for risk evaluation and treatment of CVD. There is confirmation
that CVD incidence begins rapidly in Indigenous and Torres Strait Islanders, and that the Framingham
Incidence Calculation alone underestimates the danger of CVD, at least in rural northern Australian
communities.
Identification of opportunities, priorities and options:
The lack of evidence in this report highlights the need to make suggestions for more empirical
study. New results from data collection efforts across ongoing trials, such as ongoing Cardiovascular
Disease Risk Assessment research of Aboriginal Australians, will be valuable for risk evaluation though
limits on sample size and generalizability exist (Paigea et al. 2019). The main determinant of overall
CVD exposure is the implicit age- and gender-specific danger to the population in question. Thus
descriptive evidence on age-specific and sex-specific frequency of CVD should be used to recalibrate risk
levels and estimate the target population incidence more accurately.
Workforce availability:
Aboriginal and/or Torres Strait Islander-related findings contained total CVD risk evaluation
and/or diagnosis, main evidence identified and participants with no known CVDs. Studies were excluded
if they reported observations only for persons with current CVD or did not publish outcomes
independently for individuals without CVD, involved only pregnant women or children, registered the
development or examination of electronic decision support systems or published only CVD risk
evaluation studies. Additionally, defined research that helps in meeting the selection requirements
were reported prior to 2010.
Efficiency and effectiveness:
Generally, there is a dearth of scientific data to educate the Indigenous and Torres Strait Islanders
of Australian health recommendations for risk evaluation and treatment of CVD. There is confirmation
that CVD incidence begins rapidly in Indigenous and Torres Strait Islanders, and that the Framingham
Incidence Calculation alone underestimates the danger of CVD, at least in rural northern Australian
communities.
Identification of opportunities, priorities and options:
The lack of evidence in this report highlights the need to make suggestions for more empirical
study. New results from data collection efforts across ongoing trials, such as ongoing Cardiovascular
Disease Risk Assessment research of Aboriginal Australians, will be valuable for risk evaluation though
limits on sample size and generalizability exist (Paigea et al. 2019). The main determinant of overall
CVD exposure is the implicit age- and gender-specific danger to the population in question. Thus
descriptive evidence on age-specific and sex-specific frequency of CVD should be used to recalibrate risk
levels and estimate the target population incidence more accurately.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6CVD HEALTH PROMOTION AMONGST ABORIGINAL & TORRES POPULATION
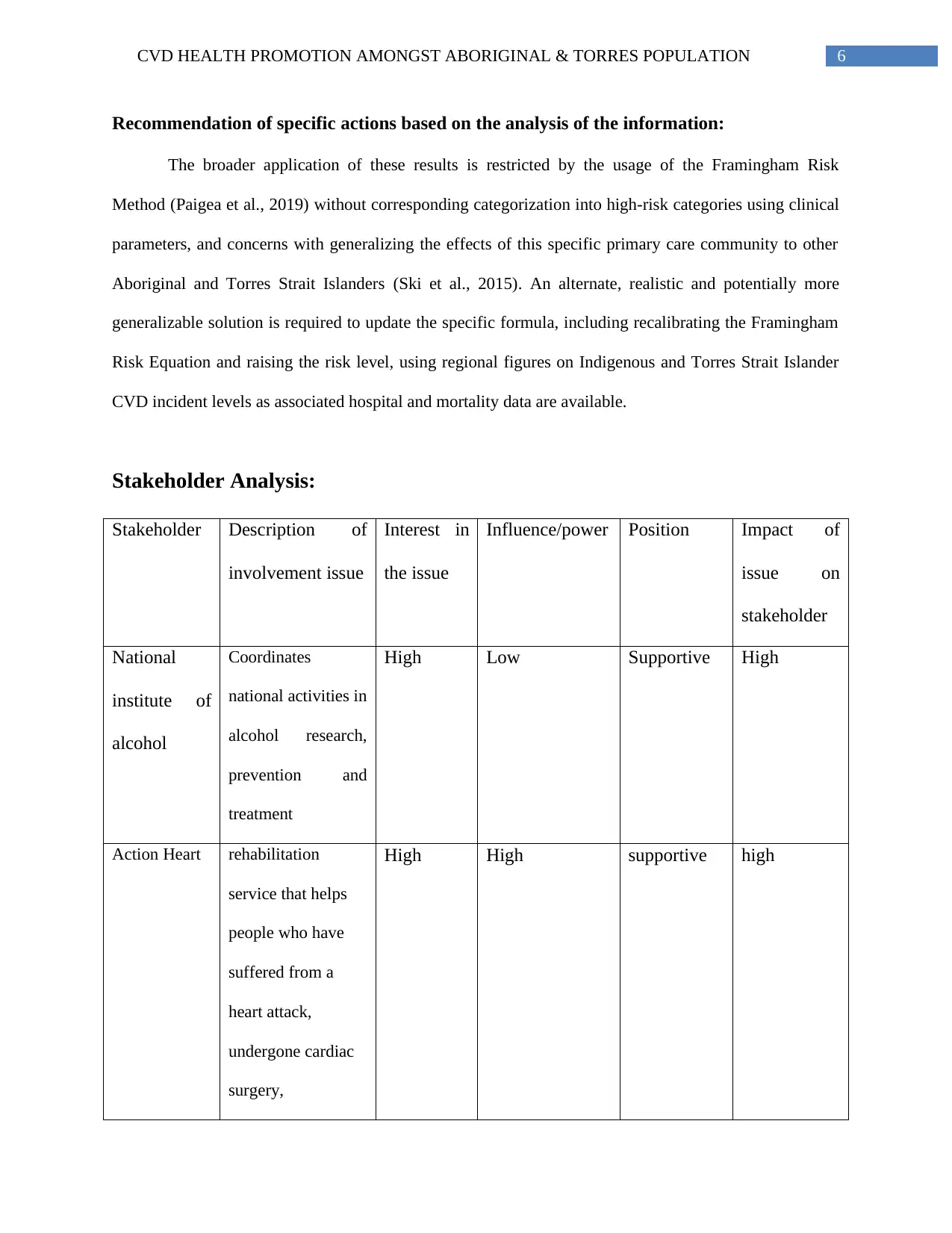
Recommendation of specific actions based on the analysis of the information:
The broader application of these results is restricted by the usage of the Framingham Risk
Method (Paigea et al., 2019) without corresponding categorization into high-risk categories using clinical
parameters, and concerns with generalizing the effects of this specific primary care community to other
Aboriginal and Torres Strait Islanders (Ski et al., 2015). An alternate, realistic and potentially more
generalizable solution is required to update the specific formula, including recalibrating the Framingham
Risk Equation and raising the risk level, using regional figures on Indigenous and Torres Strait Islander
CVD incident levels as associated hospital and mortality data are available.
Stakeholder Analysis:
Stakeholder Description of
involvement issue
Interest in
the issue
Influence/power Position Impact of
issue on
stakeholder
National
institute of
alcohol
Coordinates
national activities in
alcohol research,
prevention and
treatment
High Low Supportive High
Action Heart rehabilitation
service that helps
people who have
suffered from a
heart attack,
undergone cardiac
surgery,
High High supportive high
Recommendation of specific actions based on the analysis of the information:
The broader application of these results is restricted by the usage of the Framingham Risk
Method (Paigea et al., 2019) without corresponding categorization into high-risk categories using clinical
parameters, and concerns with generalizing the effects of this specific primary care community to other
Aboriginal and Torres Strait Islanders (Ski et al., 2015). An alternate, realistic and potentially more
generalizable solution is required to update the specific formula, including recalibrating the Framingham
Risk Equation and raising the risk level, using regional figures on Indigenous and Torres Strait Islander
CVD incident levels as associated hospital and mortality data are available.
Stakeholder Analysis:
Stakeholder Description of
involvement issue
Interest in
the issue
Influence/power Position Impact of
issue on
stakeholder
National
institute of
alcohol
Coordinates
national activities in
alcohol research,
prevention and
treatment
High Low Supportive High
Action Heart rehabilitation
service that helps
people who have
suffered from a
heart attack,
undergone cardiac
surgery,
High High supportive high
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
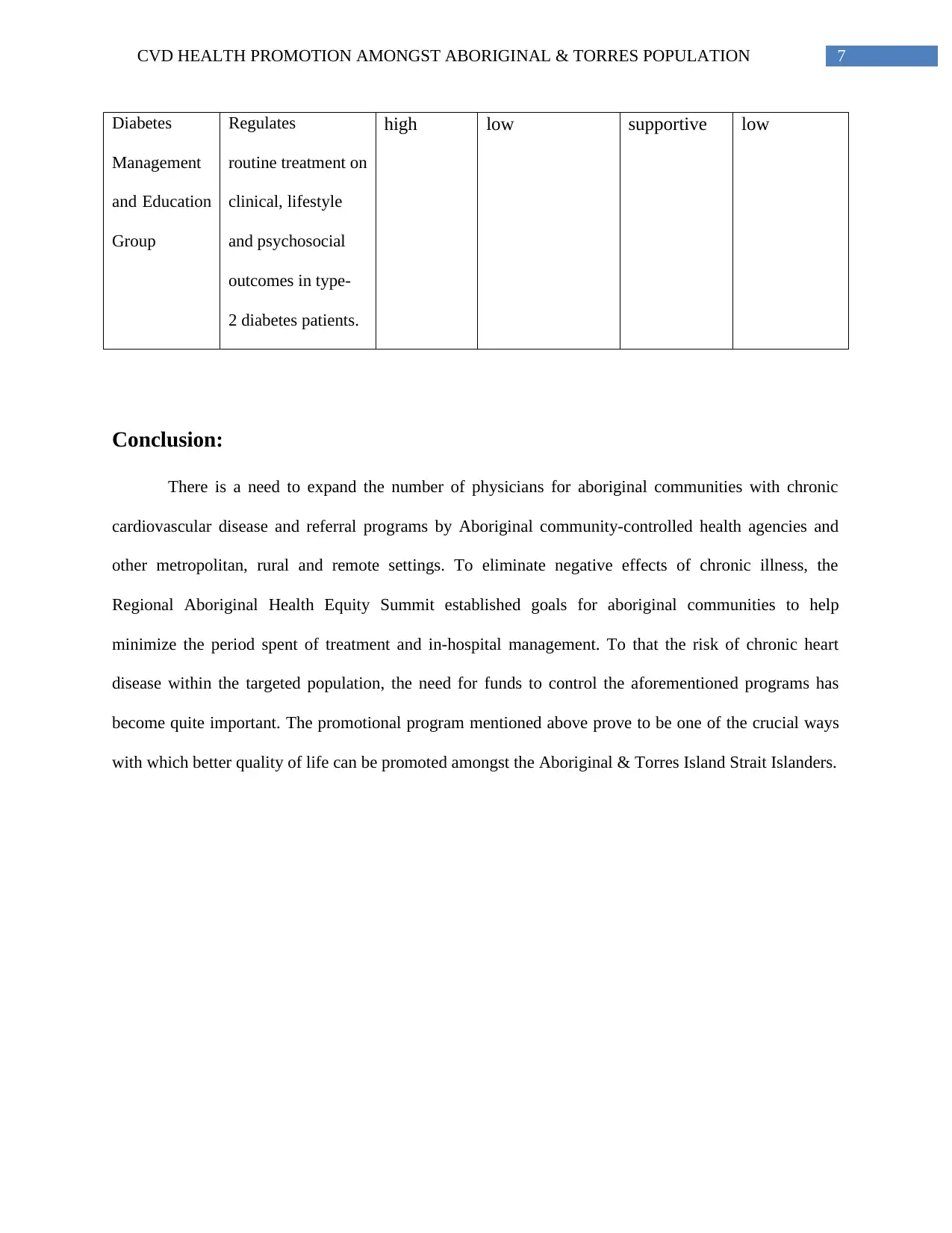
7CVD HEALTH PROMOTION AMONGST ABORIGINAL & TORRES POPULATION
Diabetes
Management
and Education
Group
Regulates
routine treatment on
clinical, lifestyle
and psychosocial
outcomes in type-
2 diabetes patients.
high low supportive low
Conclusion:
There is a need to expand the number of physicians for aboriginal communities with chronic
cardiovascular disease and referral programs by Aboriginal community-controlled health agencies and
other metropolitan, rural and remote settings. To eliminate negative effects of chronic illness, the
Regional Aboriginal Health Equity Summit established goals for aboriginal communities to help
minimize the period spent of treatment and in-hospital management. To that the risk of chronic heart
disease within the targeted population, the need for funds to control the aforementioned programs has
become quite important. The promotional program mentioned above prove to be one of the crucial ways
with which better quality of life can be promoted amongst the Aboriginal & Torres Island Strait Islanders.
Diabetes
Management
and Education
Group
Regulates
routine treatment on
clinical, lifestyle
and psychosocial
outcomes in type-
2 diabetes patients.
high low supportive low
Conclusion:
There is a need to expand the number of physicians for aboriginal communities with chronic
cardiovascular disease and referral programs by Aboriginal community-controlled health agencies and
other metropolitan, rural and remote settings. To eliminate negative effects of chronic illness, the
Regional Aboriginal Health Equity Summit established goals for aboriginal communities to help
minimize the period spent of treatment and in-hospital management. To that the risk of chronic heart
disease within the targeted population, the need for funds to control the aforementioned programs has
become quite important. The promotional program mentioned above prove to be one of the crucial ways
with which better quality of life can be promoted amongst the Aboriginal & Torres Island Strait Islanders.
8CVD HEALTH PROMOTION AMONGST ABORIGINAL & TORRES POPULATION
References:
Brown, A., & Kritharides, L. (2017). Overcoming cardiovascular disease in Indigenous
Australians. Medical Journal of Australia, 206(1), 10-12.
Gibson, O., Lisy, K., Davy, C., Aromataris, E., Kite, E., Lockwood, C., ... & Brown, A. (2015). Enablers
and barriers to the implementation of primary health care interventions for Indigenous people
with chronic diseases: a systematic review. Implementation Science, 10(1), 71.
Gubhaju, L., Banks, E., MacNiven, R., McNamara, B. J., Joshy, G., Bauman, A., & Eades, S. J. (2015).
Physical functional limitations among Aboriginal and non-Aboriginal older adults: associations
with socio-demographic factors and health. PloS one, 10(9).
Gubhaju, L., Banks, E., Ward, J., D’Este, C., Ivers, R., Roseby, R., ... & Hotu, C. (2019). ‘Next
Generation Youth Well-being Study:’understanding the health and social well-being trajectories
of Australian Aboriginal adolescents aged 10–24 years: study protocol. BMJ open, 9(3), e028734.
Helms, A., Gilhotra, R., Preston, S., Saireddy, R., Starmer, G., & Sutcliffe, S. (2020). P188 Aboriginal
and Torres Strait Australians have significantly
Jones, R. The epidemiology of Aboriginal and Torres Strait Islander culture, health and wellbeing.
(Jones)
Jones, R., Thurber, K. A., Wright, A., Chapman, J., Donohoe, P., Davis, V., & Lovett, R. (2018).
Associations between participation in a ranger program and health and wellbeing outcomes
among aboriginal and torres strait islander people in Central Australia: a proof of concept
study. International journal of environmental research and public health, 15(7), 1478.
Paigea, E., Jenkinsa, L. O. D., Agostinoa, J., Penningsc, S., Waded, V., Lovetta, R., ... & Banksa, E.
(2019). Aboriginal and Torres Strait Islander absolute cardiovascular risk assessment and
management: systematic review of evidence to inform national guidelines.
References:
Brown, A., & Kritharides, L. (2017). Overcoming cardiovascular disease in Indigenous
Australians. Medical Journal of Australia, 206(1), 10-12.
Gibson, O., Lisy, K., Davy, C., Aromataris, E., Kite, E., Lockwood, C., ... & Brown, A. (2015). Enablers
and barriers to the implementation of primary health care interventions for Indigenous people
with chronic diseases: a systematic review. Implementation Science, 10(1), 71.
Gubhaju, L., Banks, E., MacNiven, R., McNamara, B. J., Joshy, G., Bauman, A., & Eades, S. J. (2015).
Physical functional limitations among Aboriginal and non-Aboriginal older adults: associations
with socio-demographic factors and health. PloS one, 10(9).
Gubhaju, L., Banks, E., Ward, J., D’Este, C., Ivers, R., Roseby, R., ... & Hotu, C. (2019). ‘Next
Generation Youth Well-being Study:’understanding the health and social well-being trajectories
of Australian Aboriginal adolescents aged 10–24 years: study protocol. BMJ open, 9(3), e028734.
Helms, A., Gilhotra, R., Preston, S., Saireddy, R., Starmer, G., & Sutcliffe, S. (2020). P188 Aboriginal
and Torres Strait Australians have significantly
Jones, R. The epidemiology of Aboriginal and Torres Strait Islander culture, health and wellbeing.
(Jones)
Jones, R., Thurber, K. A., Wright, A., Chapman, J., Donohoe, P., Davis, V., & Lovett, R. (2018).
Associations between participation in a ranger program and health and wellbeing outcomes
among aboriginal and torres strait islander people in Central Australia: a proof of concept
study. International journal of environmental research and public health, 15(7), 1478.
Paigea, E., Jenkinsa, L. O. D., Agostinoa, J., Penningsc, S., Waded, V., Lovetta, R., ... & Banksa, E.
(2019). Aboriginal and Torres Strait Islander absolute cardiovascular risk assessment and
management: systematic review of evidence to inform national guidelines.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9CVD HEALTH PROMOTION AMONGST ABORIGINAL & TORRES POPULATION
Rice, K., Te Hiwi, B., Zwarenstein, M., Lavallee, B., Barre, D. E., & Harris, S. B. (2016). Best practices
for the prevention and Management of Diabetes and Obesity-Related Chronic Disease among
indigenous peoples in Canada: a review. Canadian journal of diabetes, 40(3), 216-225.
Sahle, B. W., Owen, A. J., Mutowo, M. P., Krum, H., & Reid, C. M. (2016). Prevalence of heart failure in
Australia: a systematic review. BMC cardiovascular disorders, 16(1), 32.
Ski, C. F., Vale, M. J., Bennett, G. R., Chalmers, V. L., McFarlane, K., Jelinek, V. M., ... & Thompson,
D. R. (2015). Improving access and equity in reducing cardiovascular risk: the Queensland
Health model. Medical Journal of Australia, 202(3), 148-152.
Woodruffe, S., Neubeck, L., Clark, R. A., Gray, K., Ferry, C., Finan, J., ... & Briffa, T. G. (2015).
Australian Cardiovascular Health and Rehabilitation Association (ACRA) core components of
cardiovascular disease secondary prevention and cardiac rehabilitation 2014. Heart, Lung and
Circulation, 24(5), 430-441.
Woodruffe, S., Neubeck, L., Clark, R. A., Gray, K., Ferry, C., Finan, J., ... & Briffa, T. G. (2015).
Australian Cardiovascular Health and Rehabilitation Association (ACRA) core components of
cardiovascular disease secondary prevention and cardiac rehabilitation 2014. Heart, Lung and
Circulation, 24(5), 430-441.
Rice, K., Te Hiwi, B., Zwarenstein, M., Lavallee, B., Barre, D. E., & Harris, S. B. (2016). Best practices
for the prevention and Management of Diabetes and Obesity-Related Chronic Disease among
indigenous peoples in Canada: a review. Canadian journal of diabetes, 40(3), 216-225.
Sahle, B. W., Owen, A. J., Mutowo, M. P., Krum, H., & Reid, C. M. (2016). Prevalence of heart failure in
Australia: a systematic review. BMC cardiovascular disorders, 16(1), 32.
Ski, C. F., Vale, M. J., Bennett, G. R., Chalmers, V. L., McFarlane, K., Jelinek, V. M., ... & Thompson,
D. R. (2015). Improving access and equity in reducing cardiovascular risk: the Queensland
Health model. Medical Journal of Australia, 202(3), 148-152.
Woodruffe, S., Neubeck, L., Clark, R. A., Gray, K., Ferry, C., Finan, J., ... & Briffa, T. G. (2015).
Australian Cardiovascular Health and Rehabilitation Association (ACRA) core components of
cardiovascular disease secondary prevention and cardiac rehabilitation 2014. Heart, Lung and
Circulation, 24(5), 430-441.
Woodruffe, S., Neubeck, L., Clark, R. A., Gray, K., Ferry, C., Finan, J., ... & Briffa, T. G. (2015).
Australian Cardiovascular Health and Rehabilitation Association (ACRA) core components of
cardiovascular disease secondary prevention and cardiac rehabilitation 2014. Heart, Lung and
Circulation, 24(5), 430-441.
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





