NSB 204 Mental Health: Assessment Task 2 - Holistic Assessment Report
VerifiedAdded on 2023/06/08
|19
|3790
|138
Report
AI Summary
This report presents a detailed mental health assessment of a 41-year-old accountant, Mary, diagnosed with depression. It includes a Mental Status Examination (MSE) outlining her appearance, behavior, speech, mood, thought content, perception, cognition, emotions, insight, and judgment. A clinical formulation table provides biological, psychological, and social factors influencing her condition, along with precipitating, predisposing, and perpetuating factors, and protective elements. The report details plans for nursing care, including establishing a therapeutic relationship, promoting self-worth, communication skills, patient-centered care, and evidence-based practices. It also covers clinical handover procedures. Part 2 delves into therapeutic engagement, emphasizing the therapeutic nurse-client relationship, cultural safety, and recovery-oriented nursing care. The report highlights the importance of trust, empathy, and professional boundaries in the therapeutic relationship. It also addresses the significance of cultural sensitivity and the implementation of recovery-oriented models to support the client's journey towards wellness, emphasizing self-determination and shared decision-making.
Running head: NSB 204 Mental Health: assessment Task 2.
MENTAL HEALTH DISORDER: Depression Case Scenario One.
STUDENT NAME:
STUDENT ID:
COURSE:
WORD COUNT: 1703
TUTOR NAME:
MENTAL HEALTH DISORDER: Depression Case Scenario One.
STUDENT NAME:
STUDENT ID:
COURSE:
WORD COUNT: 1703
TUTOR NAME:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NSB 204 Mental Health: assessment Task 2.
Part1: Holistic Assessment and Planning [903].
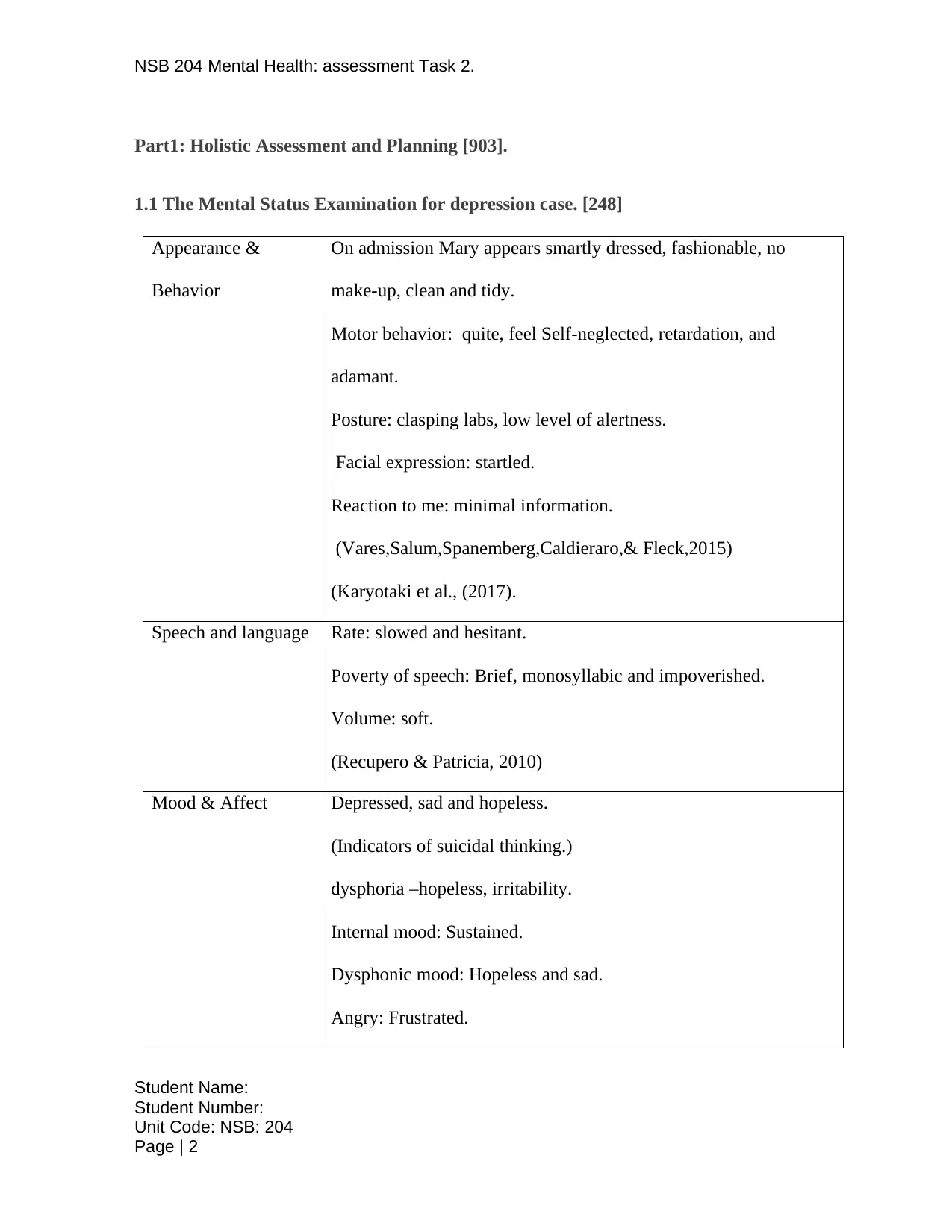
1.1 The Mental Status Examination for depression case. [248]
Appearance &
Behavior
On admission Mary appears smartly dressed, fashionable, no
make-up, clean and tidy.
Motor behavior: quite, feel Self-neglected, retardation, and
adamant.
Posture: clasping labs, low level of alertness.
Facial expression: startled.
Reaction to me: minimal information.
(Vares,Salum,Spanemberg,Caldieraro,& Fleck,2015)
(Karyotaki et al., (2017).
Speech and language Rate: slowed and hesitant.
Poverty of speech: Brief, monosyllabic and impoverished.
Volume: soft.
(Recupero & Patricia, 2010)
Mood & Affect Depressed, sad and hopeless.
(Indicators of suicidal thinking.)
dysphoria –hopeless, irritability.
Internal mood: Sustained.
Dysphonic mood: Hopeless and sad.
Angry: Frustrated.
Student Name:
Student Number:
Unit Code: NSB: 204
Page | 2
Part1: Holistic Assessment and Planning [903].
1.1 The Mental Status Examination for depression case. [248]
Appearance &
Behavior
On admission Mary appears smartly dressed, fashionable, no
make-up, clean and tidy.
Motor behavior: quite, feel Self-neglected, retardation, and
adamant.
Posture: clasping labs, low level of alertness.
Facial expression: startled.
Reaction to me: minimal information.
(Vares,Salum,Spanemberg,Caldieraro,& Fleck,2015)
(Karyotaki et al., (2017).
Speech and language Rate: slowed and hesitant.
Poverty of speech: Brief, monosyllabic and impoverished.
Volume: soft.
(Recupero & Patricia, 2010)
Mood & Affect Depressed, sad and hopeless.
(Indicators of suicidal thinking.)
dysphoria –hopeless, irritability.
Internal mood: Sustained.
Dysphonic mood: Hopeless and sad.
Angry: Frustrated.
Student Name:
Student Number:
Unit Code: NSB: 204
Page | 2
NSB 204 Mental Health: assessment Task 2.
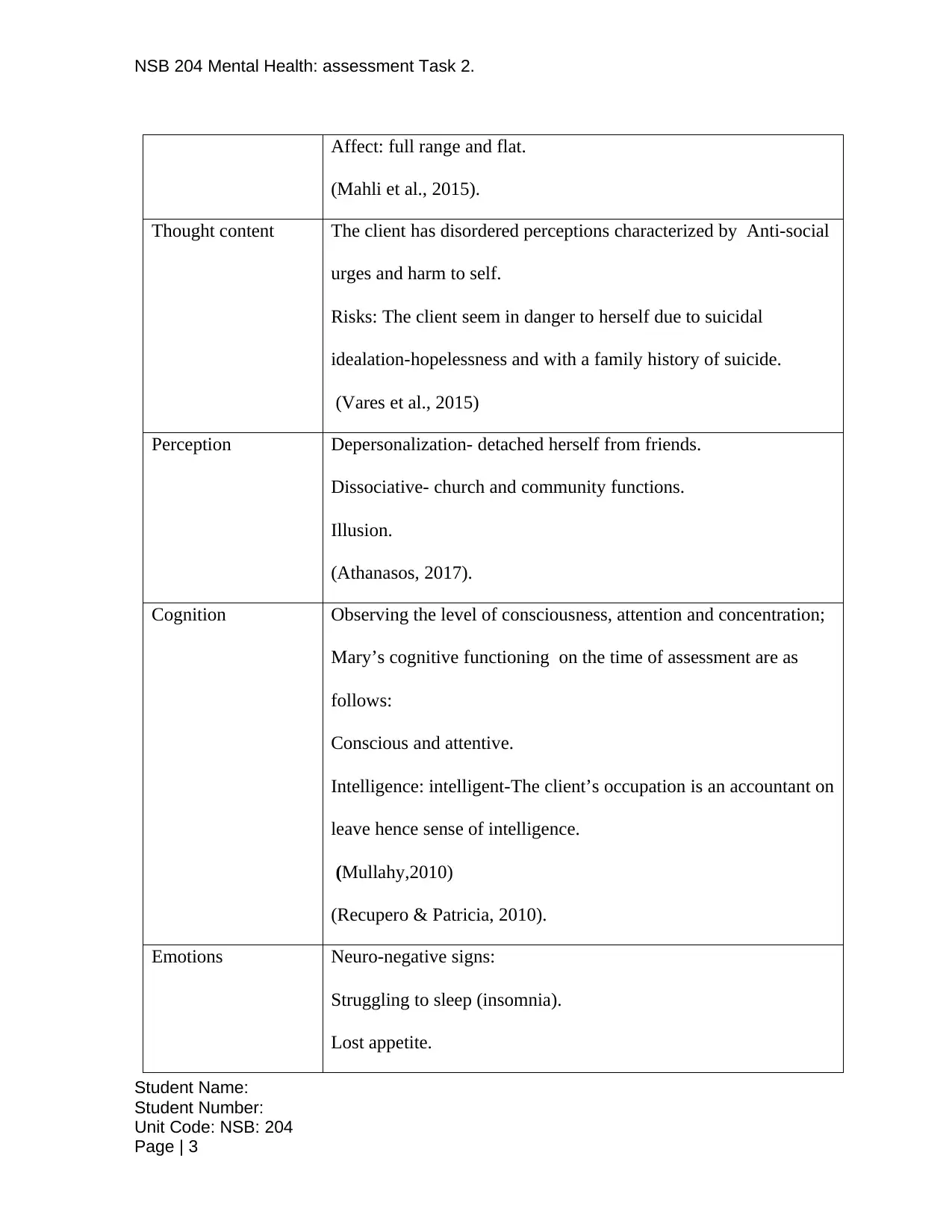
Affect: full range and flat.
(Mahli et al., 2015).
Thought content The client has disordered perceptions characterized by Anti-social
urges and harm to self.
Risks: The client seem in danger to herself due to suicidal
idealation-hopelessness and with a family history of suicide.
(Vares et al., 2015)
Perception Depersonalization- detached herself from friends.
Dissociative- church and community functions.
Illusion.
(Athanasos, 2017).
Cognition Observing the level of consciousness, attention and concentration;
Mary’s cognitive functioning on the time of assessment are as
follows:
Conscious and attentive.
Intelligence: intelligent-The client’s occupation is an accountant on
leave hence sense of intelligence.
(Mullahy,2010)
(Recupero & Patricia, 2010).
Emotions Neuro-negative signs:
Struggling to sleep (insomnia).
Lost appetite.
Student Name:
Student Number:
Unit Code: NSB: 204
Page | 3
Affect: full range and flat.
(Mahli et al., 2015).
Thought content The client has disordered perceptions characterized by Anti-social
urges and harm to self.
Risks: The client seem in danger to herself due to suicidal
idealation-hopelessness and with a family history of suicide.
(Vares et al., 2015)
Perception Depersonalization- detached herself from friends.
Dissociative- church and community functions.
Illusion.
(Athanasos, 2017).
Cognition Observing the level of consciousness, attention and concentration;
Mary’s cognitive functioning on the time of assessment are as
follows:
Conscious and attentive.
Intelligence: intelligent-The client’s occupation is an accountant on
leave hence sense of intelligence.
(Mullahy,2010)
(Recupero & Patricia, 2010).
Emotions Neuro-negative signs:
Struggling to sleep (insomnia).
Lost appetite.
Student Name:
Student Number:
Unit Code: NSB: 204
Page | 3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
NSB 204 Mental Health: assessment Task 2.
(Silbersweig, 2015).
Insight and Judgment Insight: insight into her illness, aware of her surrounding and
responsibility.
Judgment: Impaired.
Risk assessment:
Vulnerable to suicide.
(Vares et al., 2015)
Table1: Showing Mental Status Examination of a depression case (Brannon&
Schetzer, 2011).
Student Name:
Student Number:
Unit Code: NSB: 204
Page | 4
(Silbersweig, 2015).
Insight and Judgment Insight: insight into her illness, aware of her surrounding and
responsibility.
Judgment: Impaired.
Risk assessment:
Vulnerable to suicide.
(Vares et al., 2015)
Table1: Showing Mental Status Examination of a depression case (Brannon&
Schetzer, 2011).
Student Name:
Student Number:
Unit Code: NSB: 204
Page | 4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NSB 204 Mental Health: assessment Task 2.
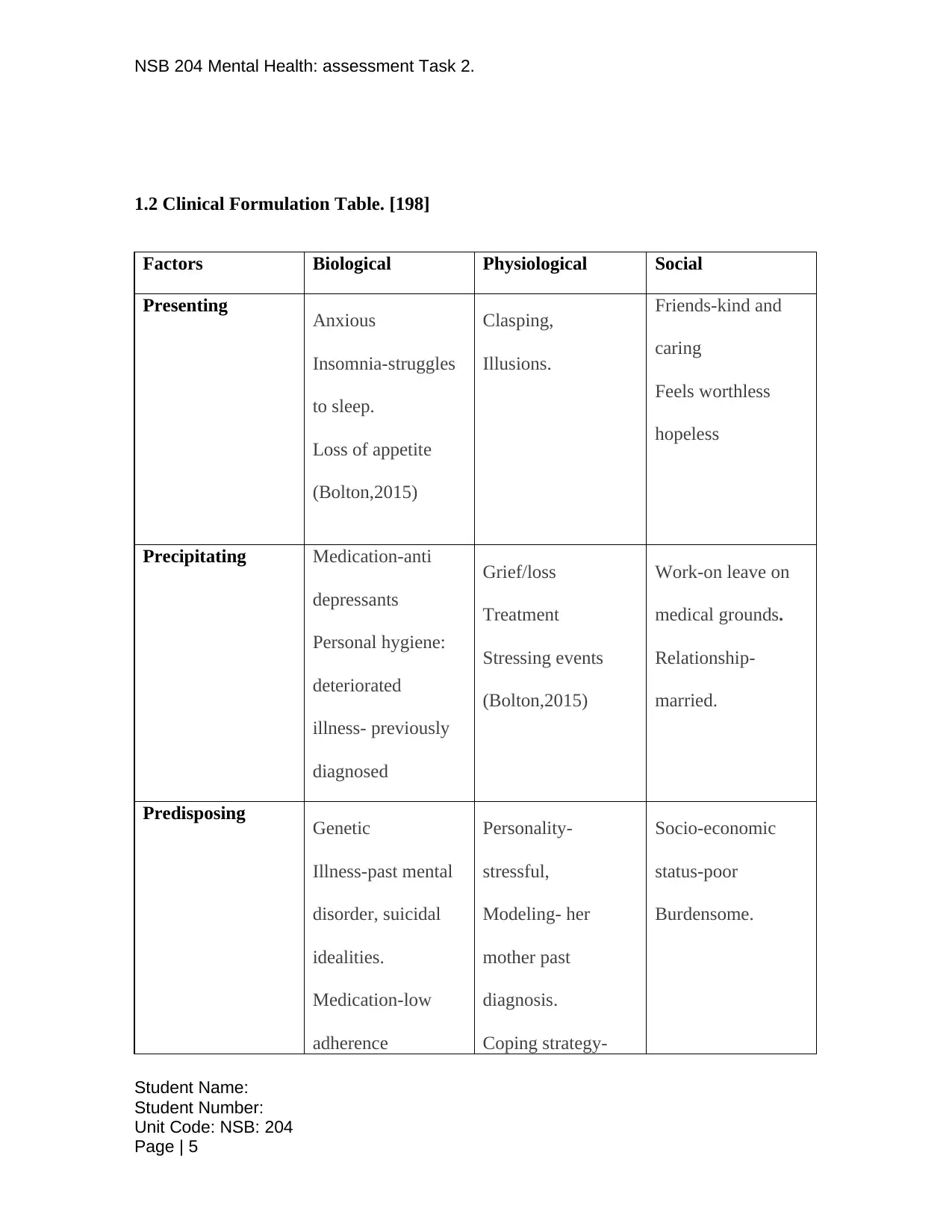
1.2 Clinical Formulation Table. [198]
Factors Biological Physiological Social
Presenting Anxious
Insomnia-struggles
to sleep.
Loss of appetite
(Bolton,2015)
Clasping,
Illusions.
Friends-kind and
caring
Feels worthless
hopeless
Precipitating Medication-anti
depressants
Personal hygiene:
deteriorated
illness- previously
diagnosed
Grief/loss
Treatment
Stressing events
(Bolton,2015)
Work-on leave on
medical grounds.
Relationship-
married.
Predisposing Genetic
Illness-past mental
disorder, suicidal
idealities.
Medication-low
adherence
Personality-
stressful,
Modeling- her
mother past
diagnosis.
Coping strategy-
Socio-economic
status-poor
Burdensome.
Student Name:
Student Number:
Unit Code: NSB: 204
Page | 5
1.2 Clinical Formulation Table. [198]
Factors Biological Physiological Social
Presenting Anxious
Insomnia-struggles
to sleep.
Loss of appetite
(Bolton,2015)
Clasping,
Illusions.
Friends-kind and
caring
Feels worthless
hopeless
Precipitating Medication-anti
depressants
Personal hygiene:
deteriorated
illness- previously
diagnosed
Grief/loss
Treatment
Stressing events
(Bolton,2015)
Work-on leave on
medical grounds.
Relationship-
married.
Predisposing Genetic
Illness-past mental
disorder, suicidal
idealities.
Medication-low
adherence
Personality-
stressful,
Modeling- her
mother past
diagnosis.
Coping strategy-
Socio-economic
status-poor
Burdensome.
Student Name:
Student Number:
Unit Code: NSB: 204
Page | 5
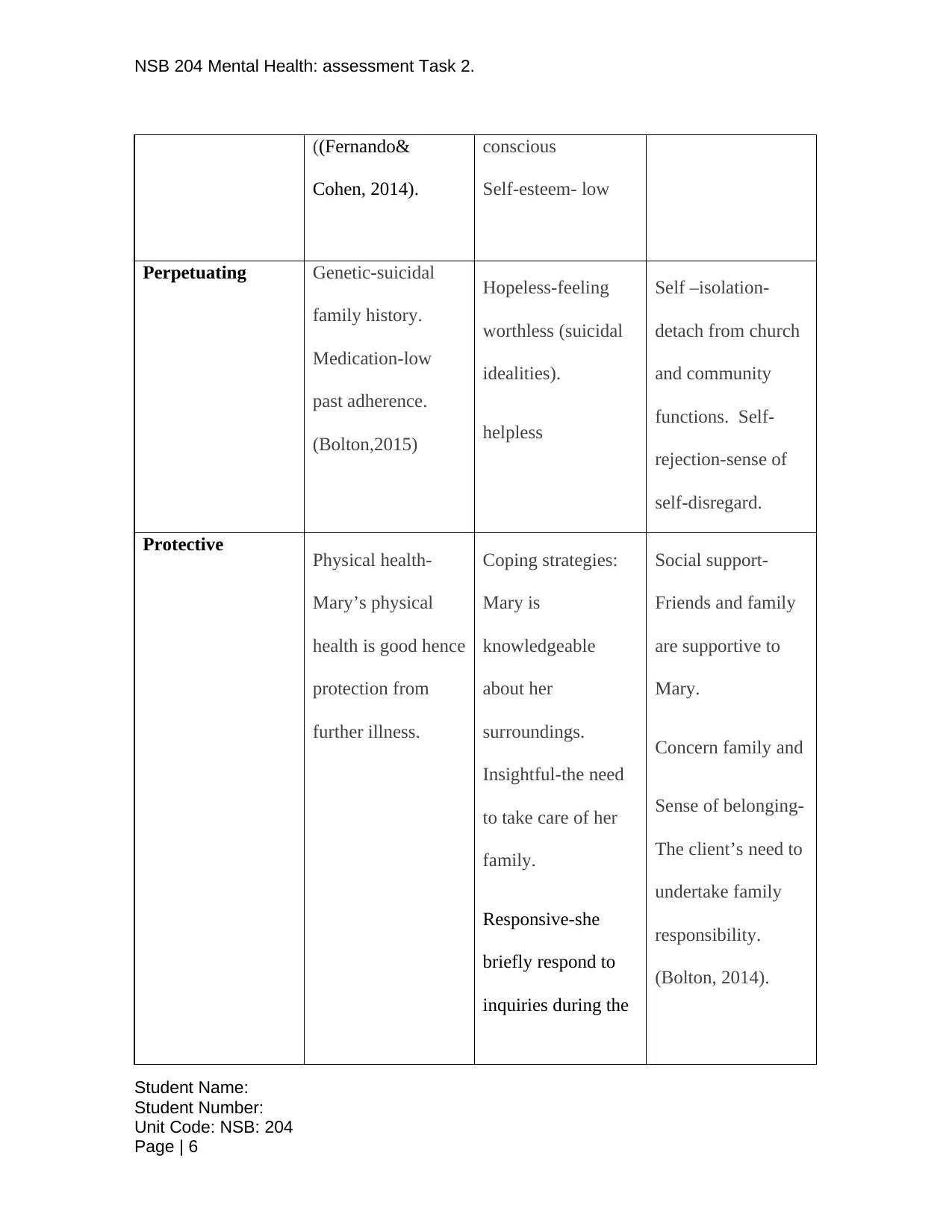
NSB 204 Mental Health: assessment Task 2.
((Fernando&
Cohen, 2014).
conscious
Self-esteem- low
Perpetuating Genetic-suicidal
family history.
Medication-low
past adherence.
(Bolton,2015)
Hopeless-feeling
worthless (suicidal
idealities).
helpless
Self –isolation-
detach from church
and community
functions. Self-
rejection-sense of
self-disregard.
Protective Physical health-
Mary’s physical
health is good hence
protection from
further illness.
Coping strategies:
Mary is
knowledgeable
about her
surroundings.
Insightful-the need
to take care of her
family.
Responsive-she
briefly respond to
inquiries during the
Social support-
Friends and family
are supportive to
Mary.
Concern family and
Sense of belonging-
The client’s need to
undertake family
responsibility.
(Bolton, 2014).
Student Name:
Student Number:
Unit Code: NSB: 204
Page | 6
((Fernando&
Cohen, 2014).
conscious
Self-esteem- low
Perpetuating Genetic-suicidal
family history.
Medication-low
past adherence.
(Bolton,2015)
Hopeless-feeling
worthless (suicidal
idealities).
helpless
Self –isolation-
detach from church
and community
functions. Self-
rejection-sense of
self-disregard.
Protective Physical health-
Mary’s physical
health is good hence
protection from
further illness.
Coping strategies:
Mary is
knowledgeable
about her
surroundings.
Insightful-the need
to take care of her
family.
Responsive-she
briefly respond to
inquiries during the
Social support-
Friends and family
are supportive to
Mary.
Concern family and
Sense of belonging-
The client’s need to
undertake family
responsibility.
(Bolton, 2014).
Student Name:
Student Number:
Unit Code: NSB: 204
Page | 6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
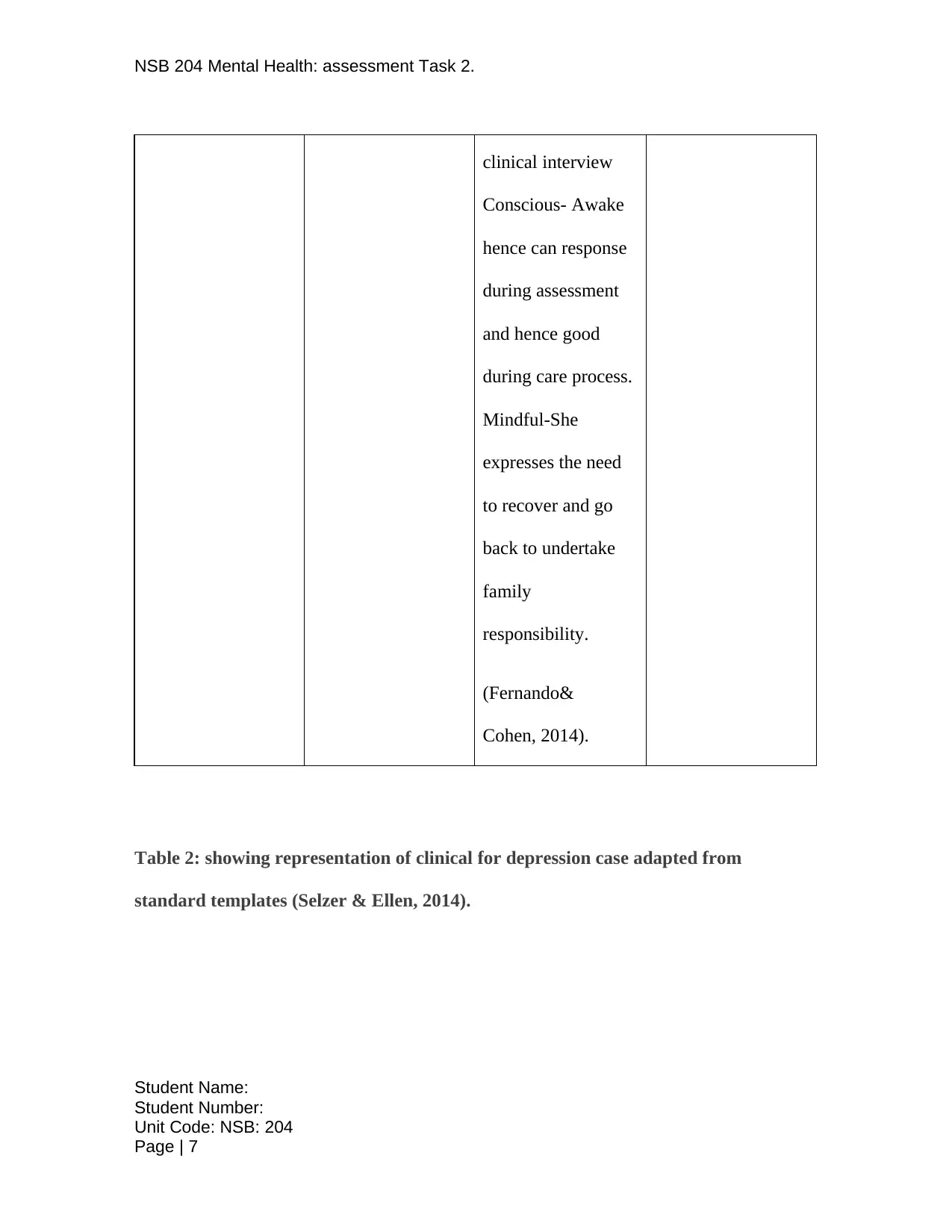
NSB 204 Mental Health: assessment Task 2.
clinical interview
Conscious- Awake
hence can response
during assessment
and hence good
during care process.
Mindful-She
expresses the need
to recover and go
back to undertake
family
responsibility.
(Fernando&
Cohen, 2014).
Table 2: showing representation of clinical for depression case adapted from
standard templates (Selzer & Ellen, 2014).
Student Name:
Student Number:
Unit Code: NSB: 204
Page | 7
clinical interview
Conscious- Awake
hence can response
during assessment
and hence good
during care process.
Mindful-She
expresses the need
to recover and go
back to undertake
family
responsibility.
(Fernando&
Cohen, 2014).
Table 2: showing representation of clinical for depression case adapted from
standard templates (Selzer & Ellen, 2014).
Student Name:
Student Number:
Unit Code: NSB: 204
Page | 7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NSB 204 Mental Health: assessment Task 2.
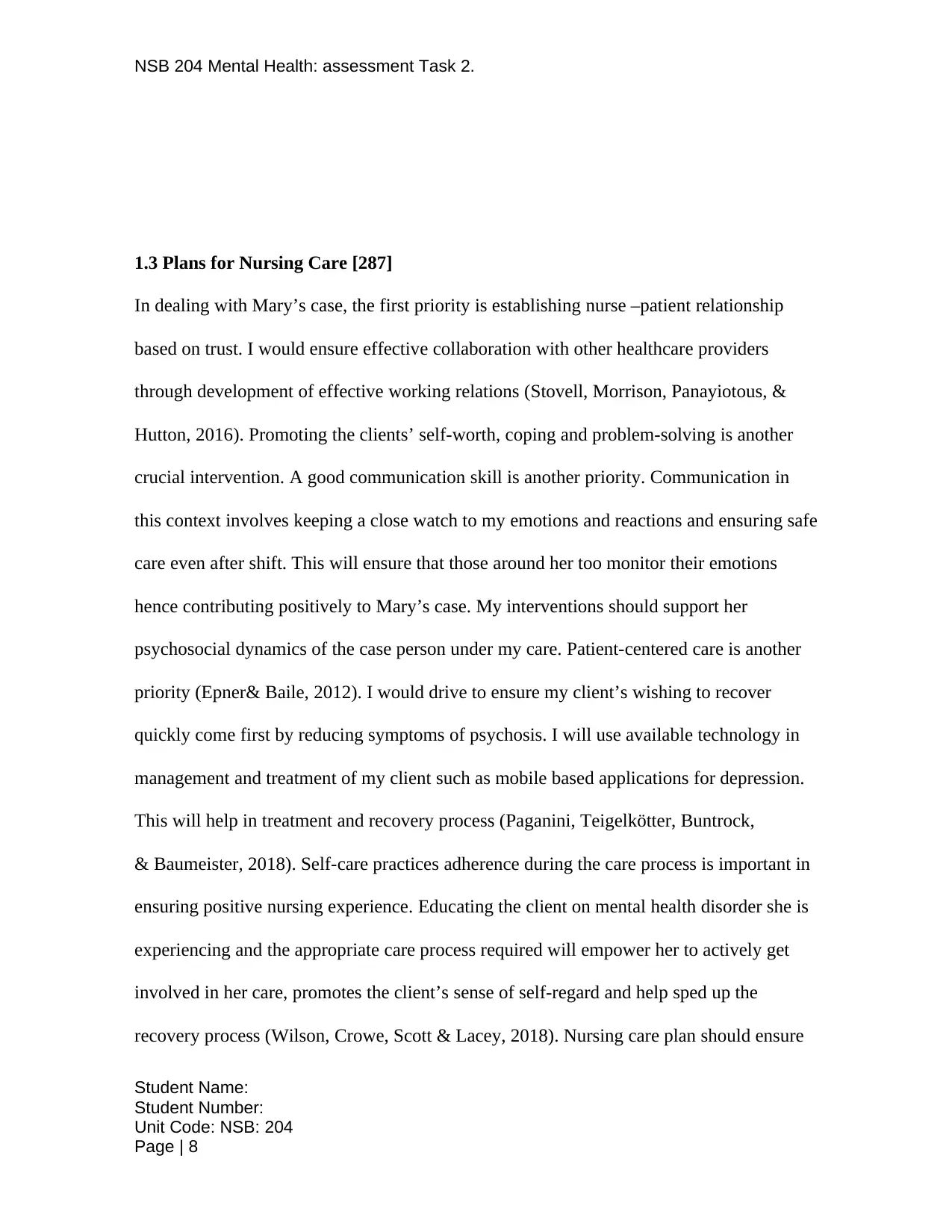
1.3 Plans for Nursing Care [287]
In dealing with Mary’s case, the first priority is establishing nurse –patient relationship
based on trust. I would ensure effective collaboration with other healthcare providers
through development of effective working relations (Stovell, Morrison, Panayiotous, &
Hutton, 2016). Promoting the clients’ self-worth, coping and problem-solving is another
crucial intervention. A good communication skill is another priority. Communication in
this context involves keeping a close watch to my emotions and reactions and ensuring safe
care even after shift. This will ensure that those around her too monitor their emotions
hence contributing positively to Mary’s case. My interventions should support her
psychosocial dynamics of the case person under my care. Patient-centered care is another
priority (Epner& Baile, 2012). I would drive to ensure my client’s wishing to recover
quickly come first by reducing symptoms of psychosis. I will use available technology in
management and treatment of my client such as mobile based applications for depression.
This will help in treatment and recovery process (Paganini, Teigelkötter, Buntrock,
& Baumeister, 2018). Self-care practices adherence during the care process is important in
ensuring positive nursing experience. Educating the client on mental health disorder she is
experiencing and the appropriate care process required will empower her to actively get
involved in her care, promotes the client’s sense of self-regard and help sped up the
recovery process (Wilson, Crowe, Scott & Lacey, 2018). Nursing care plan should ensure
Student Name:
Student Number:
Unit Code: NSB: 204
Page | 8
1.3 Plans for Nursing Care [287]
In dealing with Mary’s case, the first priority is establishing nurse –patient relationship
based on trust. I would ensure effective collaboration with other healthcare providers
through development of effective working relations (Stovell, Morrison, Panayiotous, &
Hutton, 2016). Promoting the clients’ self-worth, coping and problem-solving is another
crucial intervention. A good communication skill is another priority. Communication in
this context involves keeping a close watch to my emotions and reactions and ensuring safe
care even after shift. This will ensure that those around her too monitor their emotions
hence contributing positively to Mary’s case. My interventions should support her
psychosocial dynamics of the case person under my care. Patient-centered care is another
priority (Epner& Baile, 2012). I would drive to ensure my client’s wishing to recover
quickly come first by reducing symptoms of psychosis. I will use available technology in
management and treatment of my client such as mobile based applications for depression.
This will help in treatment and recovery process (Paganini, Teigelkötter, Buntrock,
& Baumeister, 2018). Self-care practices adherence during the care process is important in
ensuring positive nursing experience. Educating the client on mental health disorder she is
experiencing and the appropriate care process required will empower her to actively get
involved in her care, promotes the client’s sense of self-regard and help sped up the
recovery process (Wilson, Crowe, Scott & Lacey, 2018). Nursing care plan should ensure
Student Name:
Student Number:
Unit Code: NSB: 204
Page | 8
NSB 204 Mental Health: assessment Task 2.
quality care, patient centered, informed care and recovery oriented. Evidence based nursing
care is important practice hence I will ensure that all the client ’s information within my
cope are available and a safe handover issued when my shift ends (Kathol, Perez, Cohen,
2010). My client will acknowledge for the quality service and satisfaction.
1.4 Clinical Handover [160].
Quality clinical handover is crucial for ensuring flow of information to other team
responsible for the patient when my shift ends (Jason, Siefferman et al. 2012). Mental
illness patient management requires clinical handover like other illness diagnosed by
physicians (Malla, 2015).Safe handover ensures patient safety (Merten, 2017). The
synthesized results for my case would be as follow:
Mary is 41years old accountant. Her symptoms on admission are; quiet and brief, fells
worthless and hopeless. She has a history of depressive mental disorder and genetically
vulnerable to mental illness. Insomnia and loss of appetite has been reported. Currently,
she is on leave and feels burdensome. Her physical health is good with history of low
adherence to medication. She seems suicidal due to self-rejection and hopelessness with a
family history of suicide under similar circumstances. Her coping strategies are good
physical health and responsibility to her family. She speaks less often hence feels agitated
when talked to.
Student Name:
Student Number:
Unit Code: NSB: 204
Page | 9
quality care, patient centered, informed care and recovery oriented. Evidence based nursing
care is important practice hence I will ensure that all the client ’s information within my
cope are available and a safe handover issued when my shift ends (Kathol, Perez, Cohen,
2010). My client will acknowledge for the quality service and satisfaction.
1.4 Clinical Handover [160].
Quality clinical handover is crucial for ensuring flow of information to other team
responsible for the patient when my shift ends (Jason, Siefferman et al. 2012). Mental
illness patient management requires clinical handover like other illness diagnosed by
physicians (Malla, 2015).Safe handover ensures patient safety (Merten, 2017). The
synthesized results for my case would be as follow:
Mary is 41years old accountant. Her symptoms on admission are; quiet and brief, fells
worthless and hopeless. She has a history of depressive mental disorder and genetically
vulnerable to mental illness. Insomnia and loss of appetite has been reported. Currently,
she is on leave and feels burdensome. Her physical health is good with history of low
adherence to medication. She seems suicidal due to self-rejection and hopelessness with a
family history of suicide under similar circumstances. Her coping strategies are good
physical health and responsibility to her family. She speaks less often hence feels agitated
when talked to.
Student Name:
Student Number:
Unit Code: NSB: 204
Page | 9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
NSB 204 Mental Health: assessment Task 2.
Part 2.0 Therapeutic engagement and clinical Interpretation [800]
2.1 The Therapeutic Relationship [249]
A therapeutic nurse-client relationship is based on mutual trust and respect (Unhjem,
Vatne, & Hem, 2018). The client have faith in me as a her case manager, requiring that I
become sensitive of her care, nurturing her and assisting with her physical, emotional, and
spiritual needs. A caring relationship develops when we come together with my client,
resulting in harmony and healing (Unhjem et al.,2018).The strategy I would use to
establish good relationship with my patient is communicating effectively, being empathic
and identify with her case. This will be important part of interacting with Mary and
ensuring provision of care in a way that enable her involvement in her car to achieve
wellness with respect to professional boundaries (Valente, 2017).I will introduce myself to
the patient and use her name whenever I talk to her. During provision of care for mental
illness privacy of the patient is important. Professional code of conducts and boundaries
adherence underpinned by the standards of practice (Australian College of Mental Health
Nurses, 2010). I would also create awareness on my client on her state of health and
professionally make her develop interest on her care process and recovery (Crane &
Ward,2016). I would implement self-care strategies to mitigate the effects of the work, and
to have sustainable working experience with my client (Hunter, 2016). Therapeutic
relationship with my client will be an invaluable tool throughout the care and recovery
process. It will also be important during follow-up with the client.
Student Name:
Student Number:
Unit Code: NSB: 204
Page | 10
Part 2.0 Therapeutic engagement and clinical Interpretation [800]
2.1 The Therapeutic Relationship [249]
A therapeutic nurse-client relationship is based on mutual trust and respect (Unhjem,
Vatne, & Hem, 2018). The client have faith in me as a her case manager, requiring that I
become sensitive of her care, nurturing her and assisting with her physical, emotional, and
spiritual needs. A caring relationship develops when we come together with my client,
resulting in harmony and healing (Unhjem et al.,2018).The strategy I would use to
establish good relationship with my patient is communicating effectively, being empathic
and identify with her case. This will be important part of interacting with Mary and
ensuring provision of care in a way that enable her involvement in her car to achieve
wellness with respect to professional boundaries (Valente, 2017).I will introduce myself to
the patient and use her name whenever I talk to her. During provision of care for mental
illness privacy of the patient is important. Professional code of conducts and boundaries
adherence underpinned by the standards of practice (Australian College of Mental Health
Nurses, 2010). I would also create awareness on my client on her state of health and
professionally make her develop interest on her care process and recovery (Crane &
Ward,2016). I would implement self-care strategies to mitigate the effects of the work, and
to have sustainable working experience with my client (Hunter, 2016). Therapeutic
relationship with my client will be an invaluable tool throughout the care and recovery
process. It will also be important during follow-up with the client.
Student Name:
Student Number:
Unit Code: NSB: 204
Page | 10
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NSB 204 Mental Health: assessment Task 2.
2.2 Cultural Safety [213]
Provision of culturally safe care by reflecting on my own practice is a critical aspect of
cultural safety practice. Working with the client present reflection on how my own beliefs
and values may influence my relationship with the client (Koshy, Limb, Gundogan,
Whitehurst, & Jafree, 2017). It is worthwhile to incorporate cultural factors that
positively affect my client (Walker, St.Pierre-Hansen, Cromarty, Kelly, & Minty, 2010).
Understanding my client’s culture is a step in championing culturally safe care. The issue
worth identifying is stigmatization in relation to mental illness (Rossler, 2016). I will
focus on recognizing and responding professionally to my client’s deterioration in her
mental state with reference to culturally safe care provision good practices (Australian
Commission on Safety and Quality in Health Care, 2017). I will enlighten my client and
her family and those around her on positive cultural practices that impact on her care. I will
work together with the other team to discourage any form of labeling on my client in her
social cycles and create awareness to reduce its impact on my client’s mental health.
Maintaining my client’s autonomy and dignity during the care process and high level of
privacy is an important practice.
2.3 Recovery-Oriented Nursing Care [322.]
Recovery is an individual process that cannot be controlled but can be supported and
facilitated at individual, organization and system levels (Schon, Svedberg & Rosenberg,
Student Name:
Student Number:
Unit Code: NSB: 204
Page | 11
2.2 Cultural Safety [213]
Provision of culturally safe care by reflecting on my own practice is a critical aspect of
cultural safety practice. Working with the client present reflection on how my own beliefs
and values may influence my relationship with the client (Koshy, Limb, Gundogan,
Whitehurst, & Jafree, 2017). It is worthwhile to incorporate cultural factors that
positively affect my client (Walker, St.Pierre-Hansen, Cromarty, Kelly, & Minty, 2010).
Understanding my client’s culture is a step in championing culturally safe care. The issue
worth identifying is stigmatization in relation to mental illness (Rossler, 2016). I will
focus on recognizing and responding professionally to my client’s deterioration in her
mental state with reference to culturally safe care provision good practices (Australian
Commission on Safety and Quality in Health Care, 2017). I will enlighten my client and
her family and those around her on positive cultural practices that impact on her care. I will
work together with the other team to discourage any form of labeling on my client in her
social cycles and create awareness to reduce its impact on my client’s mental health.
Maintaining my client’s autonomy and dignity during the care process and high level of
privacy is an important practice.
2.3 Recovery-Oriented Nursing Care [322.]
Recovery is an individual process that cannot be controlled but can be supported and
facilitated at individual, organization and system levels (Schon, Svedberg & Rosenberg,
Student Name:
Student Number:
Unit Code: NSB: 204
Page | 11
NSB 204 Mental Health: assessment Task 2.
2015).It is evident that persons with serious mental health illness can recover to normal. As
literature searches reveals the need for understanding process of recovery, the case person
under my care will be supported in recovery through clinical interventions outlined earlier.
Recovery process of my client needs support from all healthcare team in the continuum of
care. Providing safe care, maintaining favorable nurse-client relationship, patient-centre
care and evidence base care will speed up recovery process. A guiding principle to
recovery that emphasize on hope and a strong belief that develops enhancing environment
for quick recovery is my central focus (Jacob, 2015). I will use both traditional and
recovery models to ensure my client recovers quickly from the mental illness (Snow,
Meadus, Marie, Budden, Kirby, Reid, 2014). The traditional model on mental health care
focuses on diagnosis, compliance, the eradication of symptoms and illness and reducing
risk while recovery model focuses on the client’s lived experience, choices and self-
determination on achieving dreams and on encouraging positive risk-taking (Snow et al.,
2014). Understanding the client’s lived experience with shared decision making make her
the expert in her own care and make it possible to tame behaviors such as low adherence to
medication that may undermine recovery process. The practice of my professionalism the
case will be based on dignity and respect for the patient under my care. It will recognize
the possibility of recovery and wellness, self-determination and self-management of mental
health and also helps families to understand and support their loved one (Cavanaugh,
2014).The recovery approach acknowledges that individual expectations about themselves
have a strong influence on behavior and outcomes hence worth applying in respect to my
client. Using this model in the care process will ensure quick recovery for my client.
Student Name:
Student Number:
Unit Code: NSB: 204
Page | 12
2015).It is evident that persons with serious mental health illness can recover to normal. As
literature searches reveals the need for understanding process of recovery, the case person
under my care will be supported in recovery through clinical interventions outlined earlier.
Recovery process of my client needs support from all healthcare team in the continuum of
care. Providing safe care, maintaining favorable nurse-client relationship, patient-centre
care and evidence base care will speed up recovery process. A guiding principle to
recovery that emphasize on hope and a strong belief that develops enhancing environment
for quick recovery is my central focus (Jacob, 2015). I will use both traditional and
recovery models to ensure my client recovers quickly from the mental illness (Snow,
Meadus, Marie, Budden, Kirby, Reid, 2014). The traditional model on mental health care
focuses on diagnosis, compliance, the eradication of symptoms and illness and reducing
risk while recovery model focuses on the client’s lived experience, choices and self-
determination on achieving dreams and on encouraging positive risk-taking (Snow et al.,
2014). Understanding the client’s lived experience with shared decision making make her
the expert in her own care and make it possible to tame behaviors such as low adherence to
medication that may undermine recovery process. The practice of my professionalism the
case will be based on dignity and respect for the patient under my care. It will recognize
the possibility of recovery and wellness, self-determination and self-management of mental
health and also helps families to understand and support their loved one (Cavanaugh,
2014).The recovery approach acknowledges that individual expectations about themselves
have a strong influence on behavior and outcomes hence worth applying in respect to my
client. Using this model in the care process will ensure quick recovery for my client.
Student Name:
Student Number:
Unit Code: NSB: 204
Page | 12
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 19
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





