Assessment and Care Planning for COPD Patient (Nursing Assignment)
VerifiedAdded on 2023/04/21
|16
|4291
|73
Report
AI Summary
This assignment focuses on the holistic care of a 44-year-old man, Mr. Peter Newman, admitted to the hospital with an exacerbation of COPD. The report details a comprehensive nursing care plan, including patient assessment, nursing diagnoses, and interventions. It covers respiratory and neurological assessments, and addresses key nursing problems such as impaired gas exchange and risk of septic shock. The care plan includes specific goals, nursing interventions, and rationales, along with detailed patient education on smoking cessation, workplace safety, and pulmonary rehabilitation. The assignment also identifies the allied health team members essential for the patient's care, such as exercise physiologists, dieticians, occupational therapists, and counselors. The goal is to improve the patient's overall quality of life and manage his chronic condition effectively. The assignment emphasizes the application of the clinical reasoning cycle to develop and plan nursing care.
Description/Focus: Care of the person with a medical condition
Value: 40%
Due date: 1st April 2019 by 1300 ACST
Length: 1600 words
This assignment requires you to focus on the holistic care of a patient admitted to
hospital with an acute presentation of a chronic condition and to demonstrate your
ability to apply the clinical reasoning cycle to develop and plan nursing care.
Select one of the following case scenarios:
Mr. Peter Newman is a 44-year-old man admitted to the ward with infective
exacerbation of Chronic Obstructive Pulmonary Disease (COPD). Mr Newman is a heavy
smoker and social drinker. Mr Newman is a Fly-In-Fly-Out (FIFO) truck driver with a
remote mining company and is finding it difficult to meet work responsibilities due to
increasing breathlessness.
Mr Newman lives with his wife Marcy and 2 teenage children in a southern capital city and
works a 2 weeks on/2 weeks off roster.
Based on the information provided in the above case scenarios complete the following
tasks.
Use the learning provided martials to make this this assessment please.
Task 1. Consider the patient (200 words)
What will you consider when preparing the care plan for your chosen patient?
A nursing care plan comprises of several pertinent information related to patient diagnosis,
and the purpose of delivering treatment services, in addition to particular nursing orders, and a
comprehensive evaluation plan. While formulating a care plan for the patient Peter Newman, it must
be taken into consideration that Peter has been a heavy smoker and social drinker all throughout his
life. His smoking habits can be considered as a major risk factor that triggered the onset and
development of COPD symptoms. In addition, he is also a Fly-In-Fly-Out employee. This method of
employment focuses on providing job opportunities to people in remote locations by moving them
Value: 40%
Due date: 1st April 2019 by 1300 ACST
Length: 1600 words
This assignment requires you to focus on the holistic care of a patient admitted to
hospital with an acute presentation of a chronic condition and to demonstrate your
ability to apply the clinical reasoning cycle to develop and plan nursing care.
Select one of the following case scenarios:
Mr. Peter Newman is a 44-year-old man admitted to the ward with infective
exacerbation of Chronic Obstructive Pulmonary Disease (COPD). Mr Newman is a heavy
smoker and social drinker. Mr Newman is a Fly-In-Fly-Out (FIFO) truck driver with a
remote mining company and is finding it difficult to meet work responsibilities due to
increasing breathlessness.
Mr Newman lives with his wife Marcy and 2 teenage children in a southern capital city and
works a 2 weeks on/2 weeks off roster.
Based on the information provided in the above case scenarios complete the following
tasks.
Use the learning provided martials to make this this assessment please.
Task 1. Consider the patient (200 words)
What will you consider when preparing the care plan for your chosen patient?
A nursing care plan comprises of several pertinent information related to patient diagnosis,
and the purpose of delivering treatment services, in addition to particular nursing orders, and a
comprehensive evaluation plan. While formulating a care plan for the patient Peter Newman, it must
be taken into consideration that Peter has been a heavy smoker and social drinker all throughout his
life. His smoking habits can be considered as a major risk factor that triggered the onset and
development of COPD symptoms. In addition, he is also a Fly-In-Fly-Out employee. This method of
employment focuses on providing job opportunities to people in remote locations by moving them
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

to the work site temporarily. Peter is employed in a mining company that makes it
difficult for him to meet the job responsibilities. Recently he also reported breathing problems. He
currently resides with two teenage kids and his wife Marcy in the southern capital of the nation. His
work schedule also comprises of working continuously for two weeks, followed by taking a two week
leave. Hence, at the time of care plan formulation, his workplace circumstances, and family history,
social history must be considered, with the aim of lowering his likelihood of being exposed to factors
that might exacerbate his condition.
Task 2. Nursing assessments (300)
Nursing assessments involve the procedure of gathering vital information related to the
psychological, physiological, spiritual, and sociological status of patient, and is typically conducted by
a registered nurse (Giger, 2016). The primary objective of conducting a thorough and comprehensive
nursing assessment is to recognise pertinent health abnormalities that helps in prioritising necessary
medical interventions. The three nursing assessments that need to be conducted upon Peter include
(i) respiratory assessment, (ii) assessment of dyspnoea, and (iii) vital sign and/or neurological
assessment. The respiratory assessment will encompass an external evaluation of patient
ventilation, which in turn will comprise of observations of the respiration pattern, depth and rate. An
accurate assessment of the respiratory functioning will depend on identification of abdominal and
thoracic movements that generally gets affected in COPD (Des Jardins & Burton, 2019). Conducting
an assessment for dyspnoea will involve assessing the airway patency, while listening to the lungs of
the patient. This is vital since shortness of breath is a common manifestation of COPD due to
obstruction in the lungs. Furthermore, according to Perez et al. (2015) presence of a subjective
experience of discomfort in breathing that eventually consists of distinct sensations can also be
attributed to exposure to allergens, which is prevalent in this case (work in mining site). In addition,
conducting a vital signs assessment will provide a clear insight into the status of the life sustaining
functions of the patient’s body. The measurements related to heart rate, blood pressure, pulse
(heart rate), respiratory rate, and body temperature will help in determining whether COPD has
created an impact on the general physical status of Peter, thus providing necessary clues to the
disease (Villarroel et al., 2014). Neurological assessment will involve collection of subjective data,
mini-mental state examination, and use of the Glasgow Coma Scale. It is vital since COPD has been
found to exert a negative impact on thinking and memory. In addition, presence of low levels of
oxygen in bloodstream might also cause neural damage.
Task 3. Care planning. (500)
Use the provided care plan please. That someone else work, use that in your own wording
including evidence.
difficult for him to meet the job responsibilities. Recently he also reported breathing problems. He
currently resides with two teenage kids and his wife Marcy in the southern capital of the nation. His
work schedule also comprises of working continuously for two weeks, followed by taking a two week
leave. Hence, at the time of care plan formulation, his workplace circumstances, and family history,
social history must be considered, with the aim of lowering his likelihood of being exposed to factors
that might exacerbate his condition.
Task 2. Nursing assessments (300)
Nursing assessments involve the procedure of gathering vital information related to the
psychological, physiological, spiritual, and sociological status of patient, and is typically conducted by
a registered nurse (Giger, 2016). The primary objective of conducting a thorough and comprehensive
nursing assessment is to recognise pertinent health abnormalities that helps in prioritising necessary
medical interventions. The three nursing assessments that need to be conducted upon Peter include
(i) respiratory assessment, (ii) assessment of dyspnoea, and (iii) vital sign and/or neurological
assessment. The respiratory assessment will encompass an external evaluation of patient
ventilation, which in turn will comprise of observations of the respiration pattern, depth and rate. An
accurate assessment of the respiratory functioning will depend on identification of abdominal and
thoracic movements that generally gets affected in COPD (Des Jardins & Burton, 2019). Conducting
an assessment for dyspnoea will involve assessing the airway patency, while listening to the lungs of
the patient. This is vital since shortness of breath is a common manifestation of COPD due to
obstruction in the lungs. Furthermore, according to Perez et al. (2015) presence of a subjective
experience of discomfort in breathing that eventually consists of distinct sensations can also be
attributed to exposure to allergens, which is prevalent in this case (work in mining site). In addition,
conducting a vital signs assessment will provide a clear insight into the status of the life sustaining
functions of the patient’s body. The measurements related to heart rate, blood pressure, pulse
(heart rate), respiratory rate, and body temperature will help in determining whether COPD has
created an impact on the general physical status of Peter, thus providing necessary clues to the
disease (Villarroel et al., 2014). Neurological assessment will involve collection of subjective data,
mini-mental state examination, and use of the Glasgow Coma Scale. It is vital since COPD has been
found to exert a negative impact on thinking and memory. In addition, presence of low levels of
oxygen in bloodstream might also cause neural damage.
Task 3. Care planning. (500)
Use the provided care plan please. That someone else work, use that in your own wording
including evidence.
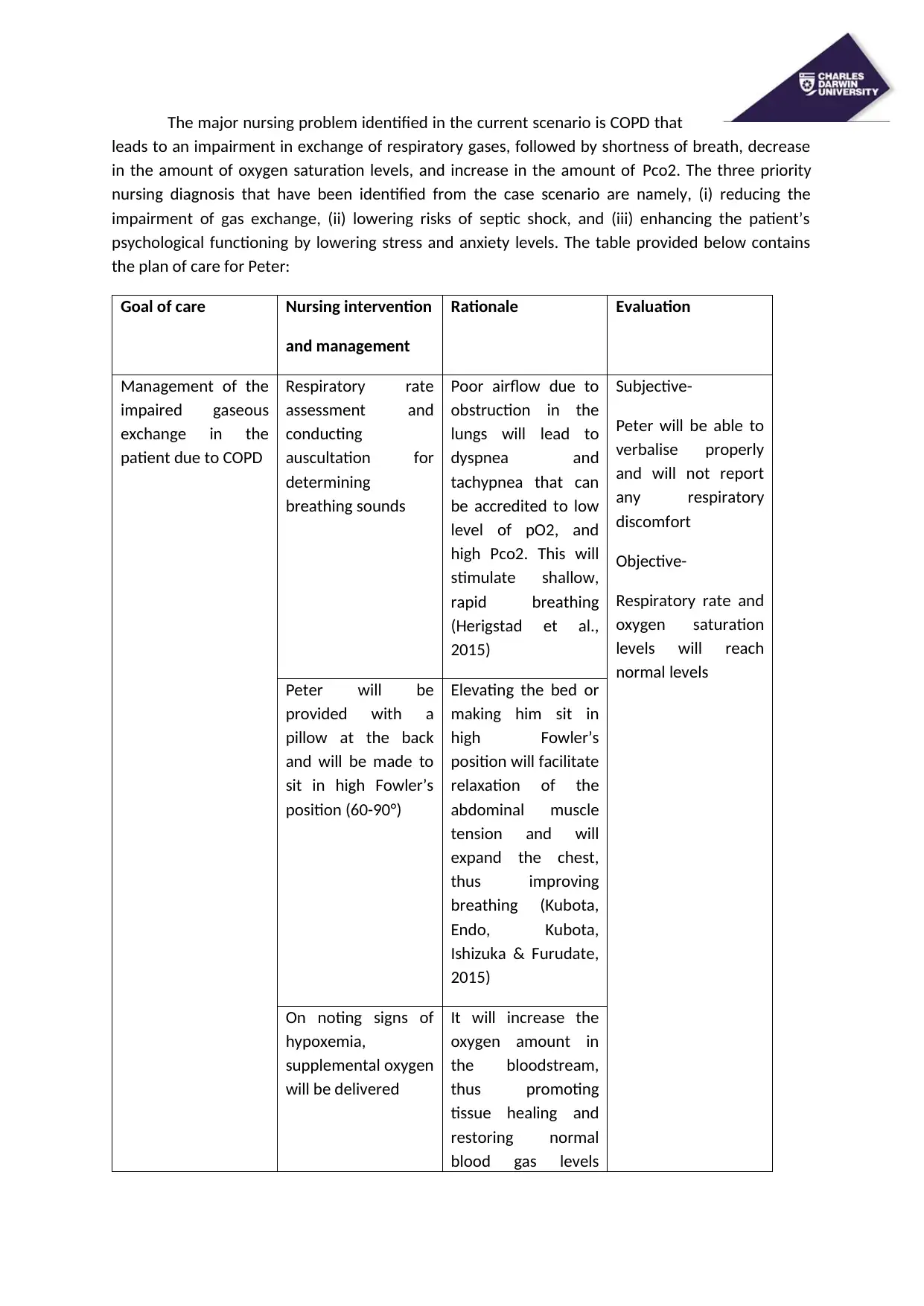
The major nursing problem identified in the current scenario is COPD that
leads to an impairment in exchange of respiratory gases, followed by shortness of breath, decrease
in the amount of oxygen saturation levels, and increase in the amount of Pco2. The three priority
nursing diagnosis that have been identified from the case scenario are namely, (i) reducing the
impairment of gas exchange, (ii) lowering risks of septic shock, and (iii) enhancing the patient’s
psychological functioning by lowering stress and anxiety levels. The table provided below contains
the plan of care for Peter:
Goal of care Nursing intervention
and management
Rationale Evaluation
Management of the
impaired gaseous
exchange in the
patient due to COPD
Respiratory rate
assessment and
conducting
auscultation for
determining
breathing sounds
Poor airflow due to
obstruction in the
lungs will lead to
dyspnea and
tachypnea that can
be accredited to low
level of pO2, and
high Pco2. This will
stimulate shallow,
rapid breathing
(Herigstad et al.,
2015)
Subjective-
Peter will be able to
verbalise properly
and will not report
any respiratory
discomfort
Objective-
Respiratory rate and
oxygen saturation
levels will reach
normal levels
Peter will be
provided with a
pillow at the back
and will be made to
sit in high Fowler’s
position (60-90°)
Elevating the bed or
making him sit in
high Fowler’s
position will facilitate
relaxation of the
abdominal muscle
tension and will
expand the chest,
thus improving
breathing (Kubota,
Endo, Kubota,
Ishizuka & Furudate,
2015)
On noting signs of
hypoxemia,
supplemental oxygen
will be delivered
It will increase the
oxygen amount in
the bloodstream,
thus promoting
tissue healing and
restoring normal
blood gas levels
leads to an impairment in exchange of respiratory gases, followed by shortness of breath, decrease
in the amount of oxygen saturation levels, and increase in the amount of Pco2. The three priority
nursing diagnosis that have been identified from the case scenario are namely, (i) reducing the
impairment of gas exchange, (ii) lowering risks of septic shock, and (iii) enhancing the patient’s
psychological functioning by lowering stress and anxiety levels. The table provided below contains
the plan of care for Peter:
Goal of care Nursing intervention
and management
Rationale Evaluation
Management of the
impaired gaseous
exchange in the
patient due to COPD
Respiratory rate
assessment and
conducting
auscultation for
determining
breathing sounds
Poor airflow due to
obstruction in the
lungs will lead to
dyspnea and
tachypnea that can
be accredited to low
level of pO2, and
high Pco2. This will
stimulate shallow,
rapid breathing
(Herigstad et al.,
2015)
Subjective-
Peter will be able to
verbalise properly
and will not report
any respiratory
discomfort
Objective-
Respiratory rate and
oxygen saturation
levels will reach
normal levels
Peter will be
provided with a
pillow at the back
and will be made to
sit in high Fowler’s
position (60-90°)
Elevating the bed or
making him sit in
high Fowler’s
position will facilitate
relaxation of the
abdominal muscle
tension and will
expand the chest,
thus improving
breathing (Kubota,
Endo, Kubota,
Ishizuka & Furudate,
2015)
On noting signs of
hypoxemia,
supplemental oxygen
will be delivered
It will increase the
oxygen amount in
the bloodstream,
thus promoting
tissue healing and
restoring normal
blood gas levels
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
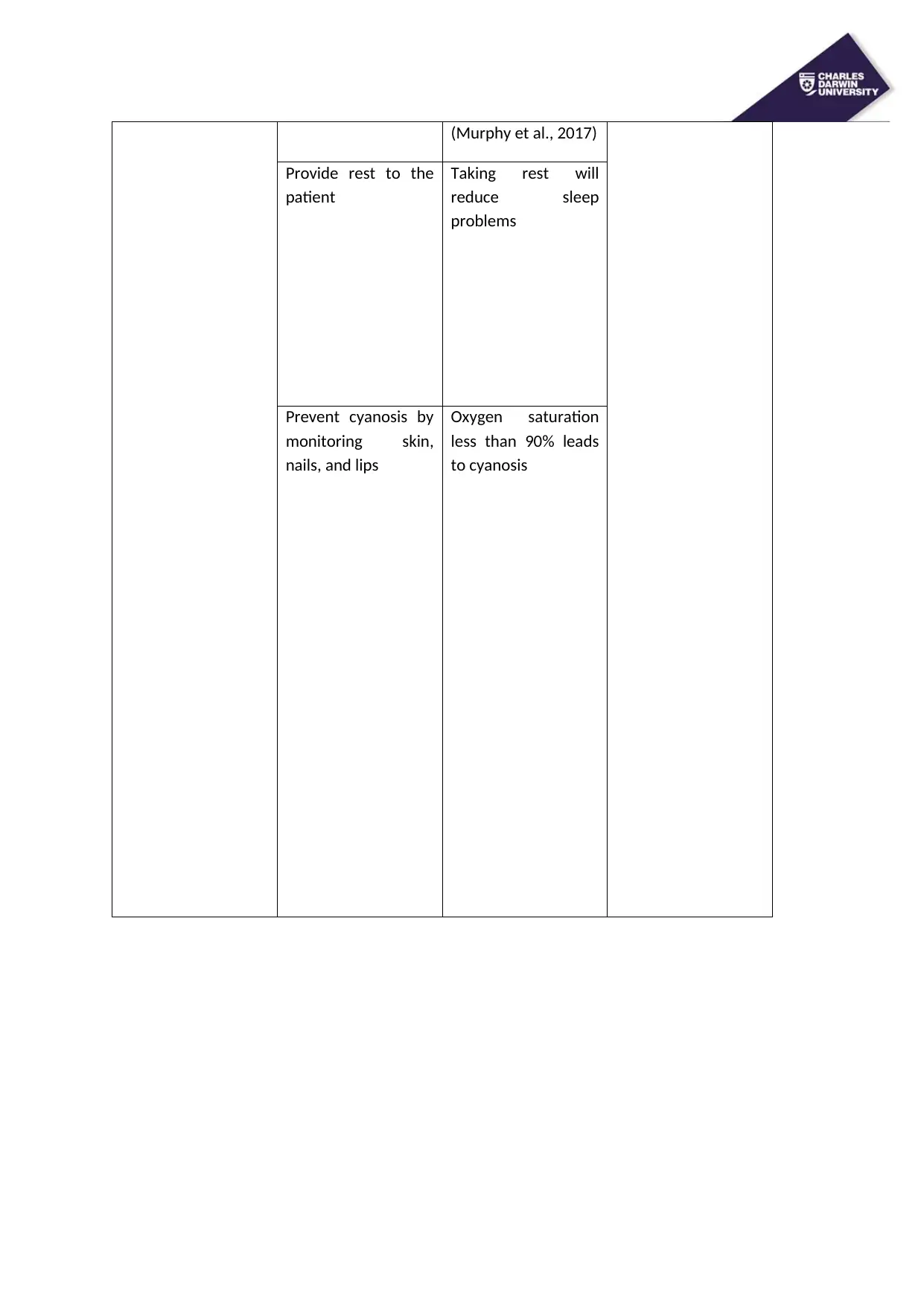
(Murphy et al., 2017)
Provide rest to the
patient
Taking rest will
reduce sleep
problems
Prevent cyanosis by
monitoring skin,
nails, and lips
Oxygen saturation
less than 90% leads
to cyanosis
Provide rest to the
patient
Taking rest will
reduce sleep
problems
Prevent cyanosis by
monitoring skin,
nails, and lips
Oxygen saturation
less than 90% leads
to cyanosis
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
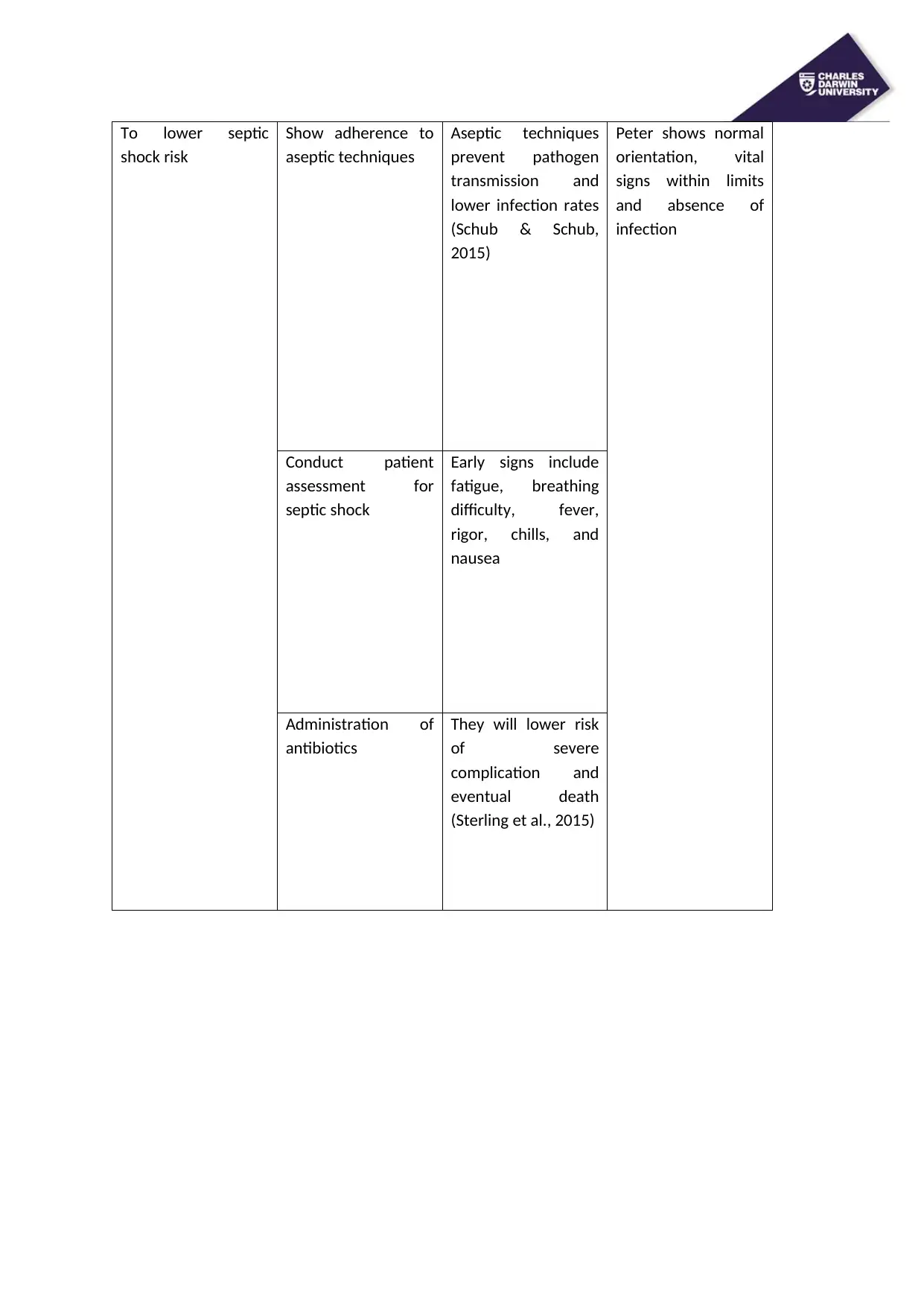
To lower septic
shock risk
Show adherence to
aseptic techniques
Aseptic techniques
prevent pathogen
transmission and
lower infection rates
(Schub & Schub,
2015)
Peter shows normal
orientation, vital
signs within limits
and absence of
infection
Conduct patient
assessment for
septic shock
Early signs include
fatigue, breathing
difficulty, fever,
rigor, chills, and
nausea
Administration of
antibiotics
They will lower risk
of severe
complication and
eventual death
(Sterling et al., 2015)
shock risk
Show adherence to
aseptic techniques
Aseptic techniques
prevent pathogen
transmission and
lower infection rates
(Schub & Schub,
2015)
Peter shows normal
orientation, vital
signs within limits
and absence of
infection
Conduct patient
assessment for
septic shock
Early signs include
fatigue, breathing
difficulty, fever,
rigor, chills, and
nausea
Administration of
antibiotics
They will lower risk
of severe
complication and
eventual death
(Sterling et al., 2015)
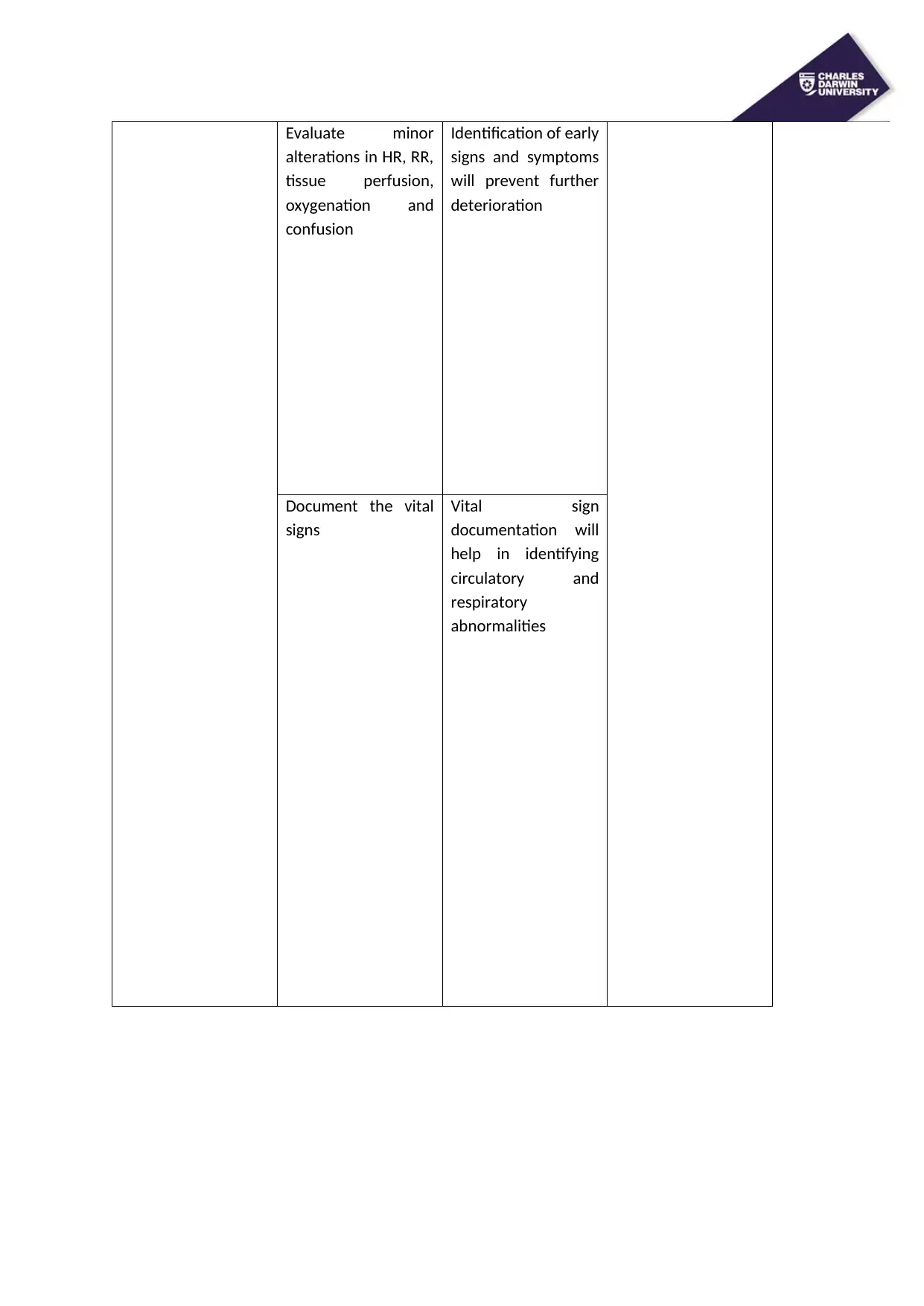
Evaluate minor
alterations in HR, RR,
tissue perfusion,
oxygenation and
confusion
Identification of early
signs and symptoms
will prevent further
deterioration
Document the vital
signs
Vital sign
documentation will
help in identifying
circulatory and
respiratory
abnormalities
alterations in HR, RR,
tissue perfusion,
oxygenation and
confusion
Identification of early
signs and symptoms
will prevent further
deterioration
Document the vital
signs
Vital sign
documentation will
help in identifying
circulatory and
respiratory
abnormalities
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
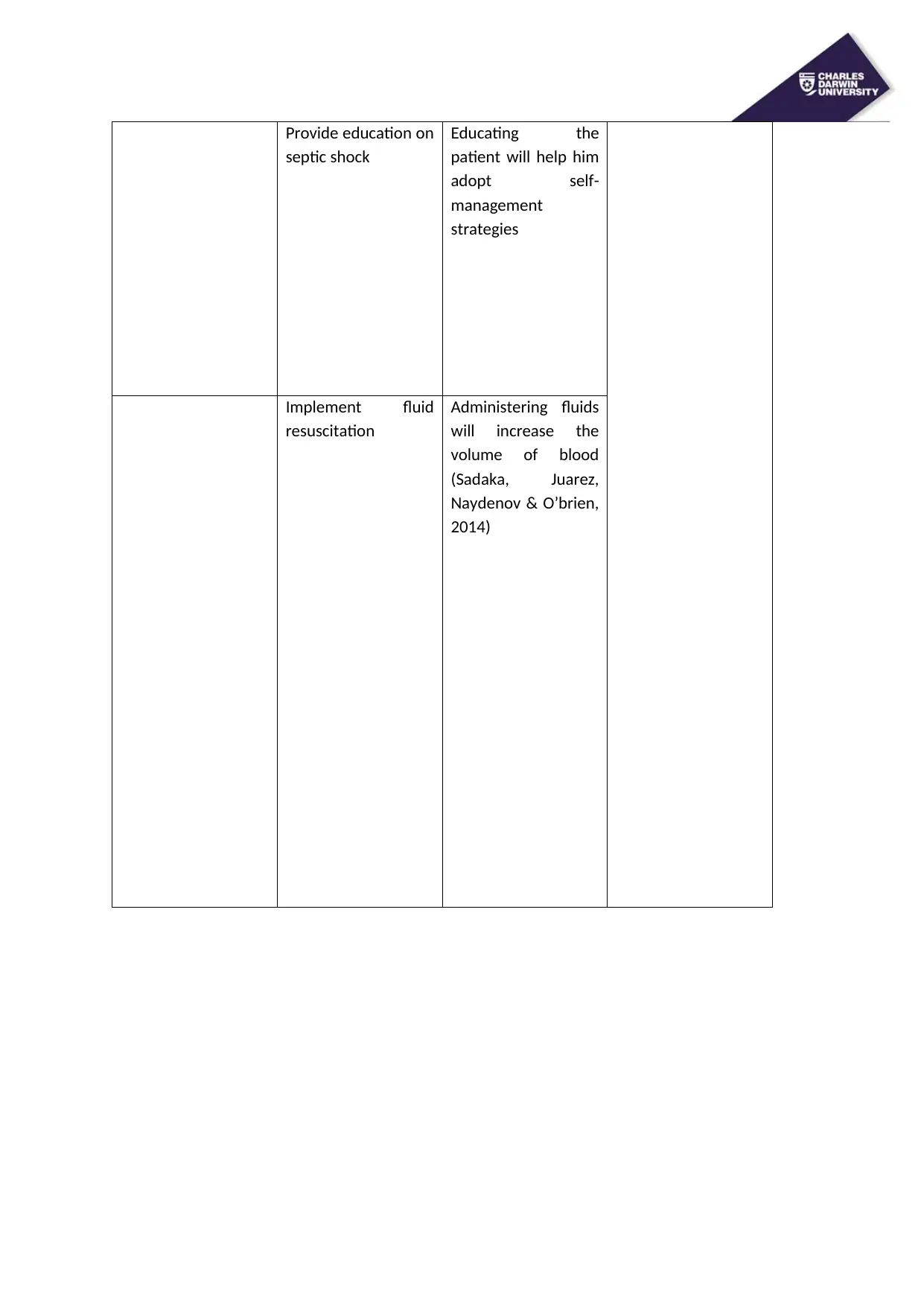
Provide education on
septic shock
Educating the
patient will help him
adopt self-
management
strategies
Implement fluid
resuscitation
Administering fluids
will increase the
volume of blood
(Sadaka, Juarez,
Naydenov & O’brien,
2014)
septic shock
Educating the
patient will help him
adopt self-
management
strategies
Implement fluid
resuscitation
Administering fluids
will increase the
volume of blood
(Sadaka, Juarez,
Naydenov & O’brien,
2014)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
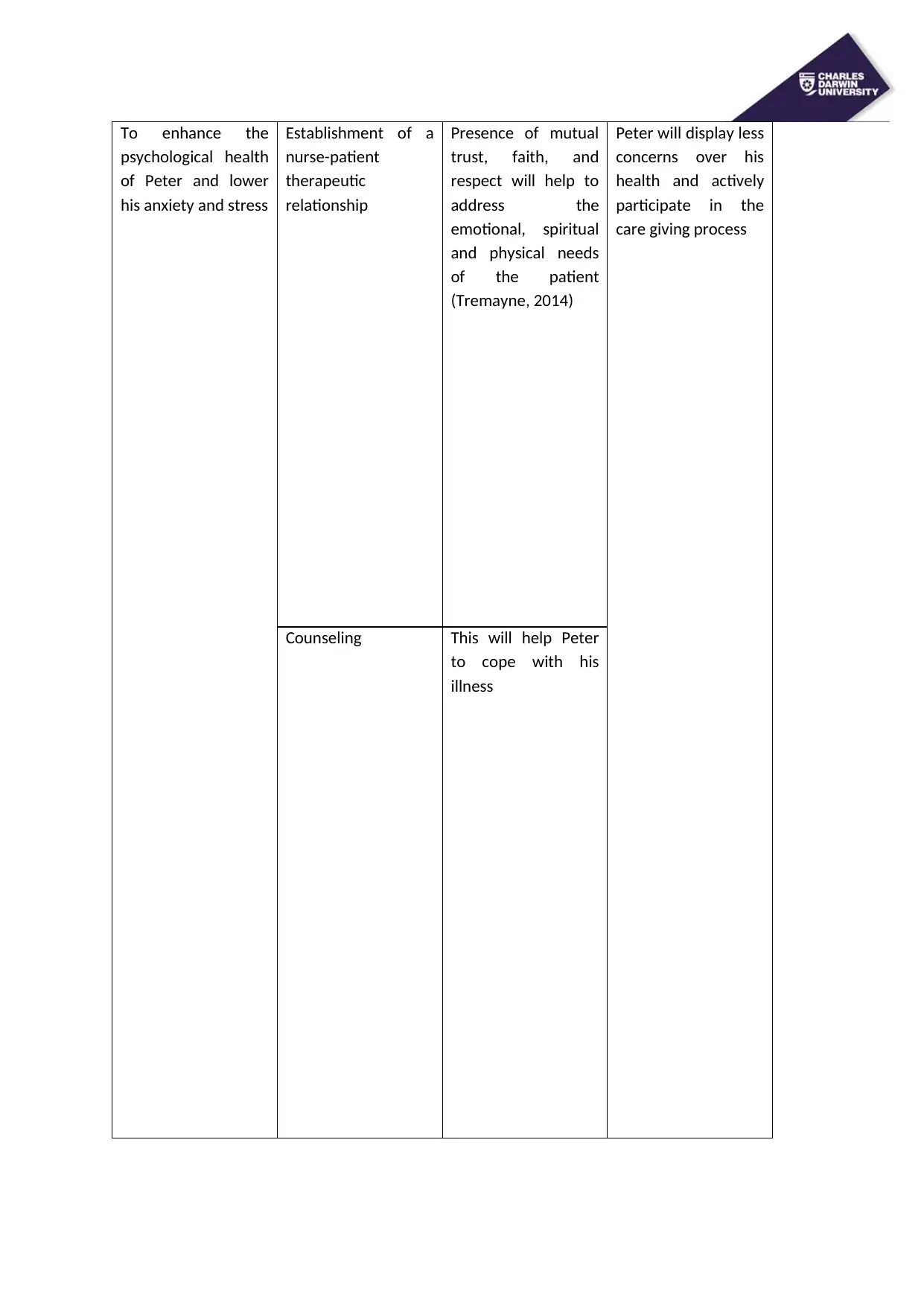
To enhance the
psychological health
of Peter and lower
his anxiety and stress
Establishment of a
nurse-patient
therapeutic
relationship
Presence of mutual
trust, faith, and
respect will help to
address the
emotional, spiritual
and physical needs
of the patient
(Tremayne, 2014)
Peter will display less
concerns over his
health and actively
participate in the
care giving process
Counseling This will help Peter
to cope with his
illness
psychological health
of Peter and lower
his anxiety and stress
Establishment of a
nurse-patient
therapeutic
relationship
Presence of mutual
trust, faith, and
respect will help to
address the
emotional, spiritual
and physical needs
of the patient
(Tremayne, 2014)
Peter will display less
concerns over his
health and actively
participate in the
care giving process
Counseling This will help Peter
to cope with his
illness
Involving his wife
and teenage kids in
the care process
Involving family
members will help to
meet the needs of
the patient (Coyne,
2015)
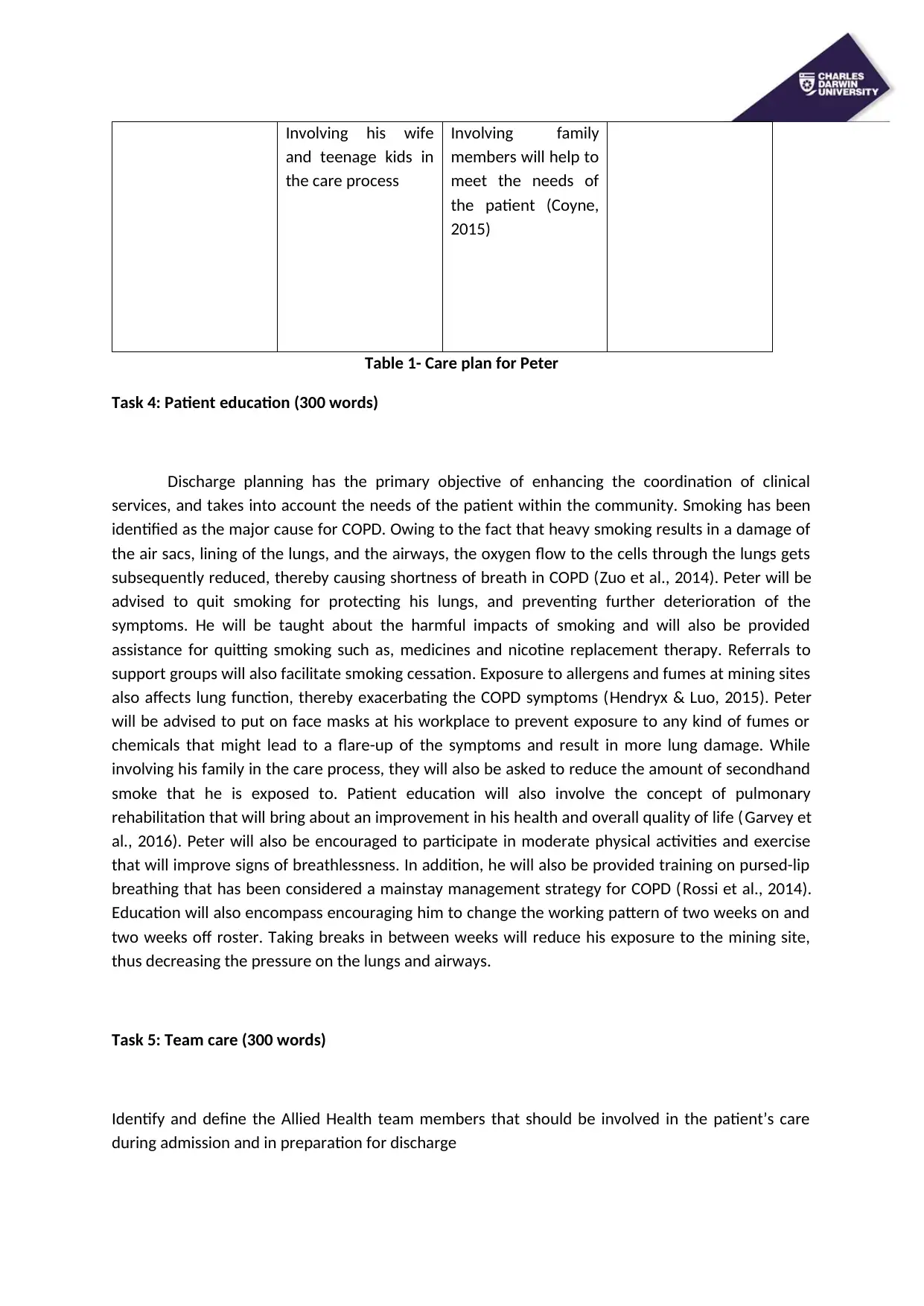
Table 1- Care plan for Peter
Task 4: Patient education (300 words)
Discharge planning has the primary objective of enhancing the coordination of clinical
services, and takes into account the needs of the patient within the community. Smoking has been
identified as the major cause for COPD. Owing to the fact that heavy smoking results in a damage of
the air sacs, lining of the lungs, and the airways, the oxygen flow to the cells through the lungs gets
subsequently reduced, thereby causing shortness of breath in COPD (Zuo et al., 2014). Peter will be
advised to quit smoking for protecting his lungs, and preventing further deterioration of the
symptoms. He will be taught about the harmful impacts of smoking and will also be provided
assistance for quitting smoking such as, medicines and nicotine replacement therapy. Referrals to
support groups will also facilitate smoking cessation. Exposure to allergens and fumes at mining sites
also affects lung function, thereby exacerbating the COPD symptoms (Hendryx & Luo, 2015). Peter
will be advised to put on face masks at his workplace to prevent exposure to any kind of fumes or
chemicals that might lead to a flare-up of the symptoms and result in more lung damage. While
involving his family in the care process, they will also be asked to reduce the amount of secondhand
smoke that he is exposed to. Patient education will also involve the concept of pulmonary
rehabilitation that will bring about an improvement in his health and overall quality of life (Garvey et
al., 2016). Peter will also be encouraged to participate in moderate physical activities and exercise
that will improve signs of breathlessness. In addition, he will also be provided training on pursed-lip
breathing that has been considered a mainstay management strategy for COPD (Rossi et al., 2014).
Education will also encompass encouraging him to change the working pattern of two weeks on and
two weeks off roster. Taking breaks in between weeks will reduce his exposure to the mining site,
thus decreasing the pressure on the lungs and airways.
Task 5: Team care (300 words)
Identify and define the Allied Health team members that should be involved in the patient’s care
during admission and in preparation for discharge
and teenage kids in
the care process
Involving family
members will help to
meet the needs of
the patient (Coyne,
2015)
Table 1- Care plan for Peter
Task 4: Patient education (300 words)
Discharge planning has the primary objective of enhancing the coordination of clinical
services, and takes into account the needs of the patient within the community. Smoking has been
identified as the major cause for COPD. Owing to the fact that heavy smoking results in a damage of
the air sacs, lining of the lungs, and the airways, the oxygen flow to the cells through the lungs gets
subsequently reduced, thereby causing shortness of breath in COPD (Zuo et al., 2014). Peter will be
advised to quit smoking for protecting his lungs, and preventing further deterioration of the
symptoms. He will be taught about the harmful impacts of smoking and will also be provided
assistance for quitting smoking such as, medicines and nicotine replacement therapy. Referrals to
support groups will also facilitate smoking cessation. Exposure to allergens and fumes at mining sites
also affects lung function, thereby exacerbating the COPD symptoms (Hendryx & Luo, 2015). Peter
will be advised to put on face masks at his workplace to prevent exposure to any kind of fumes or
chemicals that might lead to a flare-up of the symptoms and result in more lung damage. While
involving his family in the care process, they will also be asked to reduce the amount of secondhand
smoke that he is exposed to. Patient education will also involve the concept of pulmonary
rehabilitation that will bring about an improvement in his health and overall quality of life (Garvey et
al., 2016). Peter will also be encouraged to participate in moderate physical activities and exercise
that will improve signs of breathlessness. In addition, he will also be provided training on pursed-lip
breathing that has been considered a mainstay management strategy for COPD (Rossi et al., 2014).
Education will also encompass encouraging him to change the working pattern of two weeks on and
two weeks off roster. Taking breaks in between weeks will reduce his exposure to the mining site,
thus decreasing the pressure on the lungs and airways.
Task 5: Team care (300 words)
Identify and define the Allied Health team members that should be involved in the patient’s care
during admission and in preparation for discharge
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Allied Health team members typically comprise of
chiropractors, occupational therapists, exercise physiologists, osteopaths, orthoptists, prosthetists,
podiatrists, psychologists, sonographers, hospital pharmacists, and social workers. An exercise
physiologist will play an important role in this case scenario since they will help the patient
understand the benefits of participation in exercise activities, thus facilitating Peter to gain optimal
fitness, and increasing the quality of life. This allied health professional will be involved in assessing
exertional oxygen, while encouraging Peter to show adherence to exercise rehabilitation, which in
turn will improve arm movement and enhance pulmonary capacity and function. A dietician will also
play an important role during care delivery and discharge planning since breathing needs a conscious
effort among most patients. Owing to the fact that a poor diet will prevent the patient from
compensating for increased energy demands, thus resulting in subsequent loss in weight (Nordén et
al., 2015). There is mounting evidence for the association between continuous smoking and
deficiency of serum vitamin C levels (Zendedel et al., 2015). Having adequate nutrition will prevent
malnutrition and also enhance the pulmonary status of the patient. Hence, a dietician will
recommend the daily intake of food and drinks to Peter in order to meet his energy needs and avoid
weight loss. An occupational therapist will also be involved in educating and monitoring Peter in
techniques of energy conservation by prioritisation and conscious planning (Corhay, Dang, Van
Cauwenberge & Louis, 2014). The therapist will teach Peter ways to maintain balance between rest
and activity, and usage of alternate breathing techniques. Peter will also be provided training on
body positioning, adjusting tempo, and breathing techniques. A counsellor will also be involved in
the care giving process and will provide much needed psychosocial support to Peter for handling the
consequences of COPD, and the alteration in participation abilities, and activities. Counselling will
also prove beneficial in encouraging Peter for smoking cessation (Marques et al., 2015).
Referencing: Reminder marks are allocated for academic integrity. See
the marking criteria below for more details. Breaches of
academic integrity will be lodged on the University system
and may have serious consequences for students.
CDU APA 6th referencing style is to be used for both in-text
citations and end of assessment references.
All resources must be dated between 2010 and 2018
There must be at least 15 peer-reviewed journal articles
and/or evidence based practice guidelines cited in your
assignment. Do not use any health facility or local health
service policies or procedures
Only 1 current Australian medication textbook and 1 current
Australian medical surgical nursing textbook to be referenced
Assessment This assessment will be marked against the following
chiropractors, occupational therapists, exercise physiologists, osteopaths, orthoptists, prosthetists,
podiatrists, psychologists, sonographers, hospital pharmacists, and social workers. An exercise
physiologist will play an important role in this case scenario since they will help the patient
understand the benefits of participation in exercise activities, thus facilitating Peter to gain optimal
fitness, and increasing the quality of life. This allied health professional will be involved in assessing
exertional oxygen, while encouraging Peter to show adherence to exercise rehabilitation, which in
turn will improve arm movement and enhance pulmonary capacity and function. A dietician will also
play an important role during care delivery and discharge planning since breathing needs a conscious
effort among most patients. Owing to the fact that a poor diet will prevent the patient from
compensating for increased energy demands, thus resulting in subsequent loss in weight (Nordén et
al., 2015). There is mounting evidence for the association between continuous smoking and
deficiency of serum vitamin C levels (Zendedel et al., 2015). Having adequate nutrition will prevent
malnutrition and also enhance the pulmonary status of the patient. Hence, a dietician will
recommend the daily intake of food and drinks to Peter in order to meet his energy needs and avoid
weight loss. An occupational therapist will also be involved in educating and monitoring Peter in
techniques of energy conservation by prioritisation and conscious planning (Corhay, Dang, Van
Cauwenberge & Louis, 2014). The therapist will teach Peter ways to maintain balance between rest
and activity, and usage of alternate breathing techniques. Peter will also be provided training on
body positioning, adjusting tempo, and breathing techniques. A counsellor will also be involved in
the care giving process and will provide much needed psychosocial support to Peter for handling the
consequences of COPD, and the alteration in participation abilities, and activities. Counselling will
also prove beneficial in encouraging Peter for smoking cessation (Marques et al., 2015).
Referencing: Reminder marks are allocated for academic integrity. See
the marking criteria below for more details. Breaches of
academic integrity will be lodged on the University system
and may have serious consequences for students.
CDU APA 6th referencing style is to be used for both in-text
citations and end of assessment references.
All resources must be dated between 2010 and 2018
There must be at least 15 peer-reviewed journal articles
and/or evidence based practice guidelines cited in your
assignment. Do not use any health facility or local health
service policies or procedures
Only 1 current Australian medication textbook and 1 current
Australian medical surgical nursing textbook to be referenced
Assessment This assessment will be marked against the following
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

criteria: criteria:
Ability to interpret and address topic
Written expression
Using the literature effectively
Structure, logical sequencing & flow of information
CDU APA referencing
Please refer to the marking rubric attached to your
assignment task above
Ability to interpret and address topic
Written expression
Using the literature effectively
Structure, logical sequencing & flow of information
CDU APA referencing
Please refer to the marking rubric attached to your
assignment task above
References
Corhay, J. L., Dang, D. N., Van Cauwenberge, H., & Louis, R. (2014). Pulmonary rehabilitation and
COPD: providing patients a good environment for optimizing therapy. International journal
of chronic obstructive pulmonary disease, 9, 27. doi: 10.2147/COPD.S52012
Coyne, I. (2015). Families and health care professionals' perspectives and expectations of family‐ ‐
centred care: hidden expectations and unclear roles. Health expectations, 18(5), 796-808.
https://doi.org/10.1111/hex.12104
Des Jardins, T., & Burton, G. G. (2019). Clinical manifestations and assessment of respiratory disease.
Mosby. https://books.google.co.in/books?
hl=en&lr=&id=cdiCDwAAQBAJ&oi=fnd&pg=PP1&dq=respiratory+assessment&ots=Co0UEzb
XfN&sig=ve3N4871gTNbwvUkVIyxZiuJAPI#v=onepage&q=respiratory
%20assessment&f=false
Garvey, C., Bayles, M. P., Hamm, L. F., Hill, K., Holland, A., Limberg, T. M., & Spruit, M. A. (2016).
Pulmonary rehabilitation exercise prescription in chronic obstructive pulmonary disease:
review of selected guidelines. Journal of cardiopulmonary rehabilitation and
prevention, 36(2), 75-83. https://doi.org/10.1097/HCR.0000000000000171
Giger, J. N. (2016). Transcultural nursing: Assessment and intervention. Elsevier Health Sciences.
Retrieved from https://books.google.co.in/books?
hl=en&lr=&id=XCWKCwAAQBAJ&oi=fnd&pg=PP1&dq=nursing+assessment&ots=Ub4dBiESw
J&sig=-bERHkF1D0uIdrwESIO2aLW_1T4#v=onepage&q=nursing%20assessment&f=false
Hendryx, M., & Luo, J. (2015). An examination of the effects of mountaintop removal coal mining on
respiratory symptoms and COPD using propensity scores. International journal of
environmental health research, 25(3), 265-276.
https://doi.org/10.1080/09603123.2014.938027
Herigstad, M., Hayen, A., Evans, E., Hardinge, F. M., Davies, R. J., Wiech, K., & Pattinson, K. T. (2015).
Dyspnea-related cues engage the prefrontal cortex: evidence from functional brain imaging
in COPD. Chest, 148(4), 953-961. https://doi.org/10.1378/chest.15-0416
Kubota, S., Endo, Y., Kubota, M., Ishizuka, Y., & Furudate, T. (2015). Effects of trunk posture in
Fowler's position on hemodynamics. Autonomic Neuroscience, 189, 56-59.
https://doi.org/10.1016/j.autneu.2015.01.002
Marques, A., Jácome, C., Cruz, J., Gabriel, R., Brooks, D., & Figueiredo, D. (2015). Family-based
psychosocial support and education as part of pulmonary rehabilitation in COPD: a
randomized controlled trial. Chest, 147(3), 662-672. https://doi.org/10.1378/chest.14-1488
Murphy, P. B., Rehal, S., Arbane, G., Bourke, S., Calverley, P. M., Crook, A. M., ... & Hurst, J. R. (2017).
Effect of home noninvasive ventilation with oxygen therapy vs oxygen therapy alone on
hospital readmission or death after an acute COPD exacerbation: a randomized clinical
trial. Jama, 317(21), 2177-2186. doi:10.1001/jama.2017.4451
Corhay, J. L., Dang, D. N., Van Cauwenberge, H., & Louis, R. (2014). Pulmonary rehabilitation and
COPD: providing patients a good environment for optimizing therapy. International journal
of chronic obstructive pulmonary disease, 9, 27. doi: 10.2147/COPD.S52012
Coyne, I. (2015). Families and health care professionals' perspectives and expectations of family‐ ‐
centred care: hidden expectations and unclear roles. Health expectations, 18(5), 796-808.
https://doi.org/10.1111/hex.12104
Des Jardins, T., & Burton, G. G. (2019). Clinical manifestations and assessment of respiratory disease.
Mosby. https://books.google.co.in/books?
hl=en&lr=&id=cdiCDwAAQBAJ&oi=fnd&pg=PP1&dq=respiratory+assessment&ots=Co0UEzb
XfN&sig=ve3N4871gTNbwvUkVIyxZiuJAPI#v=onepage&q=respiratory
%20assessment&f=false
Garvey, C., Bayles, M. P., Hamm, L. F., Hill, K., Holland, A., Limberg, T. M., & Spruit, M. A. (2016).
Pulmonary rehabilitation exercise prescription in chronic obstructive pulmonary disease:
review of selected guidelines. Journal of cardiopulmonary rehabilitation and
prevention, 36(2), 75-83. https://doi.org/10.1097/HCR.0000000000000171
Giger, J. N. (2016). Transcultural nursing: Assessment and intervention. Elsevier Health Sciences.
Retrieved from https://books.google.co.in/books?
hl=en&lr=&id=XCWKCwAAQBAJ&oi=fnd&pg=PP1&dq=nursing+assessment&ots=Ub4dBiESw
J&sig=-bERHkF1D0uIdrwESIO2aLW_1T4#v=onepage&q=nursing%20assessment&f=false
Hendryx, M., & Luo, J. (2015). An examination of the effects of mountaintop removal coal mining on
respiratory symptoms and COPD using propensity scores. International journal of
environmental health research, 25(3), 265-276.
https://doi.org/10.1080/09603123.2014.938027
Herigstad, M., Hayen, A., Evans, E., Hardinge, F. M., Davies, R. J., Wiech, K., & Pattinson, K. T. (2015).
Dyspnea-related cues engage the prefrontal cortex: evidence from functional brain imaging
in COPD. Chest, 148(4), 953-961. https://doi.org/10.1378/chest.15-0416
Kubota, S., Endo, Y., Kubota, M., Ishizuka, Y., & Furudate, T. (2015). Effects of trunk posture in
Fowler's position on hemodynamics. Autonomic Neuroscience, 189, 56-59.
https://doi.org/10.1016/j.autneu.2015.01.002
Marques, A., Jácome, C., Cruz, J., Gabriel, R., Brooks, D., & Figueiredo, D. (2015). Family-based
psychosocial support and education as part of pulmonary rehabilitation in COPD: a
randomized controlled trial. Chest, 147(3), 662-672. https://doi.org/10.1378/chest.14-1488
Murphy, P. B., Rehal, S., Arbane, G., Bourke, S., Calverley, P. M., Crook, A. M., ... & Hurst, J. R. (2017).
Effect of home noninvasive ventilation with oxygen therapy vs oxygen therapy alone on
hospital readmission or death after an acute COPD exacerbation: a randomized clinical
trial. Jama, 317(21), 2177-2186. doi:10.1001/jama.2017.4451
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 16
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





