Analyzing Dietary Intakes of Young Children Against AGHE Guidelines
VerifiedAdded on 2023/05/29
|9
|8394
|218
Report
AI Summary
This report analyzes the dietary intakes of 54 Australian children aged two to three years, comparing them against the Australian Guide to Healthy Eating (AGHE) and Nutrient Reference Values (NRVs). The study found that no child met all AGHE targets, with most consuming insufficient servings of breads/cereals, vegetables, and meat/alternatives, while meeting or exceeding dairy and fruit recommendations. Macronutrient intakes were generally within recommended ranges, but saturated fatty acid consumption was excessive. Children who met selected NRVs exhibited different dietary patterns compared to AGHE recommendations, consuming more fruit, dairy, and discretionary foods, but fewer breads/cereals and vegetables. The study concludes that children's dietary intakes do not align with AGHE guidelines, although adequate nutrient profiles can be achieved through varying dietary patterns, highlighting the need for further research with larger, representative samples. Additionally, a diet analysis table is included, comparing food group servings with the AGHE, identifying key nutrients, and calculating energy provided by each food group, as well as comparing it with a person's estimated energy requirements.
ORIGINAL RESEARCH
Disparities exist between the Australian Guide to
Healthy Eating and the dietary intakes of young
children aged two to three years
Li K CHAI,1 Lesley MACDONALD-WICKS,2 Alexis J HURE,3 Tracy L BURROWS,2
Michelle L BLUMFIELD,1 Roger SMITH3 and Clare E COLLINS1,2
1Priority Research Centre in PhysicalActivity and Nutrition 2School of Health Sciences, Faculty of Health and
Medicine and3Hunter Medical Research Institute and Schoolof Medicine and Public Health, The University of
Newcastle, Callaghan, New South Wales, Australia
Abstract
Aim: To compare dietary intakes of young children to the Australian Guide to Healthy Eating (AGHE) and Nutrient
Reference Values (NRVs).
Methods: Dietary intakes of 54 children (50% girls) aged two to three years (mean 2.7 years) from the Women and
Their Children’s Health (WATCH) study were reported by mothers using a validated 120-item food frequency
questionnaire. Daily consumption of AGHE food group servings, macronutrients, and micronutrients were compared
to the AGHE and NRVs using t-test with significance set at P < 0.05.
Results: No child achieved all AGHE targets, with the majority consuming less breads/cereals (1.9 vs 4.0 servings/
day), vegetables (1.3 vs 2.5), and meat/alternatives (0.7 vs 1.0), all P < 0.0001. Adequate servings were observed for
dairy (2.2 vs 1.5) and fruit (1.3 vs 1.0). Macronutrients were within recommended ranges, although 96% exceeded
saturated fatty acid recommendations. Children who met selected NRVs consumed more fruit (1.4 vs 1.0; P < 0.0086),
dairy (2.2 vs 1.5; P < 0.0001) and discretionary foods (2.6 vs ≤1.0; P < 0.0001) but less breads/cereals (2.0 vs 4.0;
P < 0.0001) and vegetables (1.3 vs 2.5; P < 0.0001) servings, compared to the AGHE recommended servings.
Conclusions: Child dietary intakes did not align with AGHE, while adequate nutrient profiles were achieved by
various dietary patterns. Future studies involving data from larger, representative samples of children are warranted.
Key words: Australian Guide to Healthy Eating, children, dietary intake; Nutrient Reference Values, nutritional
status.
Introduction
Childhood nutrition can have a lifelong impact on an indi-
vidual’s health.1–3 Current research indicates that dietary pat-
terns,including frequency,variety and amountof food
habituallyconsumed,track from childhood through to
adulthood.2–4 The early years, between ages of one and three,
are a time when eating patterns, skills, knowledge and atti-
tude towards food begin to develop.5,6 Healthy childhood
eating patterns are essentialfor the provision ofsufficient
energy and nutrients for growth,cognitive development,7
and to reduce the risk ofnutrition-related chronic disease
later in life.8
In Australia,a healthy dietis characterised by the con-
sumption of a variety of foods from the five core food groups,
which are: (i) bread/cereals, mostly wholegrain and/or high
fibre varieties;(ii) fruit;(iii) vegetables and legumes/beans;
(iv) dairy products,such as reduced-fat milk yoghurt,and
cheese; and (v) lean meats/alternatives, such as poultry, fish
eggs, nuts, and legumes, with additional allowances for low
intakes of unsaturated fat and discretionary foods (energy-
dense,nutrient-poor).9 These are operationalised as a rec-
ommended number of daily servings in the Australian Guide
to Healthy Eating (AGHE).9 The 2013 AGHE was developed
from a detailed evidence base in conjunction with a Food
Modelling System10,11to establish a range of virtual diets: the
Foundation Dietsand TotalDiets.This wasachieved by
L.K. Chai BNutrDiet (Hons) APD, Research Assistant
L. MacDonald-Wicks PhD GCTT AdvAPD, Senior Lecturer Nutrition
and Dietetics
A.J. Hure PhD AdvAPD, HMRI Public Health Postdoctoral Fellow
T.L. Burrows PhD APD, Lecturer in Nutrition and Dietetics
M.L. Blumfield PhD (Nutr&Diet) APD, Postdoctoral researcher
R. Smith PhD, Professor
C.E. Collins PhD (Nutr&Diet) AdvAPD FDAA, Professor in Nutrition
and Dietetics
Correspondence: C.E. Collins, School of Health Sciences, Faculty of
Health and Medicine, The University of Newcastle, Callaghan, NSW
2308, Australia. Email: Clare.Collins@newcastle.edu.au
Accepted April 2015
bs_bs_banner
Nutrition & Dietetics 2015; ••: ••–•• DOI: 10.1111/1747-0080.12203
© 2015 Dietitians Association of Australia 1
Disparities exist between the Australian Guide to
Healthy Eating and the dietary intakes of young
children aged two to three years
Li K CHAI,1 Lesley MACDONALD-WICKS,2 Alexis J HURE,3 Tracy L BURROWS,2
Michelle L BLUMFIELD,1 Roger SMITH3 and Clare E COLLINS1,2
1Priority Research Centre in PhysicalActivity and Nutrition 2School of Health Sciences, Faculty of Health and
Medicine and3Hunter Medical Research Institute and Schoolof Medicine and Public Health, The University of
Newcastle, Callaghan, New South Wales, Australia
Abstract
Aim: To compare dietary intakes of young children to the Australian Guide to Healthy Eating (AGHE) and Nutrient
Reference Values (NRVs).
Methods: Dietary intakes of 54 children (50% girls) aged two to three years (mean 2.7 years) from the Women and
Their Children’s Health (WATCH) study were reported by mothers using a validated 120-item food frequency
questionnaire. Daily consumption of AGHE food group servings, macronutrients, and micronutrients were compared
to the AGHE and NRVs using t-test with significance set at P < 0.05.
Results: No child achieved all AGHE targets, with the majority consuming less breads/cereals (1.9 vs 4.0 servings/
day), vegetables (1.3 vs 2.5), and meat/alternatives (0.7 vs 1.0), all P < 0.0001. Adequate servings were observed for
dairy (2.2 vs 1.5) and fruit (1.3 vs 1.0). Macronutrients were within recommended ranges, although 96% exceeded
saturated fatty acid recommendations. Children who met selected NRVs consumed more fruit (1.4 vs 1.0; P < 0.0086),
dairy (2.2 vs 1.5; P < 0.0001) and discretionary foods (2.6 vs ≤1.0; P < 0.0001) but less breads/cereals (2.0 vs 4.0;
P < 0.0001) and vegetables (1.3 vs 2.5; P < 0.0001) servings, compared to the AGHE recommended servings.
Conclusions: Child dietary intakes did not align with AGHE, while adequate nutrient profiles were achieved by
various dietary patterns. Future studies involving data from larger, representative samples of children are warranted.
Key words: Australian Guide to Healthy Eating, children, dietary intake; Nutrient Reference Values, nutritional
status.
Introduction
Childhood nutrition can have a lifelong impact on an indi-
vidual’s health.1–3 Current research indicates that dietary pat-
terns,including frequency,variety and amountof food
habituallyconsumed,track from childhood through to
adulthood.2–4 The early years, between ages of one and three,
are a time when eating patterns, skills, knowledge and atti-
tude towards food begin to develop.5,6 Healthy childhood
eating patterns are essentialfor the provision ofsufficient
energy and nutrients for growth,cognitive development,7
and to reduce the risk ofnutrition-related chronic disease
later in life.8
In Australia,a healthy dietis characterised by the con-
sumption of a variety of foods from the five core food groups,
which are: (i) bread/cereals, mostly wholegrain and/or high
fibre varieties;(ii) fruit;(iii) vegetables and legumes/beans;
(iv) dairy products,such as reduced-fat milk yoghurt,and
cheese; and (v) lean meats/alternatives, such as poultry, fish
eggs, nuts, and legumes, with additional allowances for low
intakes of unsaturated fat and discretionary foods (energy-
dense,nutrient-poor).9 These are operationalised as a rec-
ommended number of daily servings in the Australian Guide
to Healthy Eating (AGHE).9 The 2013 AGHE was developed
from a detailed evidence base in conjunction with a Food
Modelling System10,11to establish a range of virtual diets: the
Foundation Dietsand TotalDiets.This wasachieved by
L.K. Chai BNutrDiet (Hons) APD, Research Assistant
L. MacDonald-Wicks PhD GCTT AdvAPD, Senior Lecturer Nutrition
and Dietetics
A.J. Hure PhD AdvAPD, HMRI Public Health Postdoctoral Fellow
T.L. Burrows PhD APD, Lecturer in Nutrition and Dietetics
M.L. Blumfield PhD (Nutr&Diet) APD, Postdoctoral researcher
R. Smith PhD, Professor
C.E. Collins PhD (Nutr&Diet) AdvAPD FDAA, Professor in Nutrition
and Dietetics
Correspondence: C.E. Collins, School of Health Sciences, Faculty of
Health and Medicine, The University of Newcastle, Callaghan, NSW
2308, Australia. Email: Clare.Collins@newcastle.edu.au
Accepted April 2015
bs_bs_banner
Nutrition & Dietetics 2015; ••: ••–•• DOI: 10.1111/1747-0080.12203
© 2015 Dietitians Association of Australia 1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
converting the Nutrient Reference Values (NRVs) into com-
binations of types and amounts of foods within the core food
groups to meet the nutritional requirements of each age and
gendergroup,factoring in heightand physicalactivity
levels.11 The information was simplified into the AGHE,a
user-friendly food selection guide.9
NRVs outline the average nutrientrequirements needed
on a daily basisto meetphysiologicalfunction and to
prevent deficiency or chronic disease.12 NRVs for population
average intakes are termed ‘estimated average requirements’
(EARs) and ‘adequate intakes’(AIs).12 The EAR refers to the
everyday nutrient intake levelneeded to meet the require-
mentsof 50% of the healthypopulation in aspecific
life-stage and gender group.12 When an EAR cannot be deter-
mined, then an AI, which is the average daily nutrient intake
levelthatis likely to be sufficient,based on observed or
experimentally determined estimation of nutrient intake by
an apparently healthy cohort, is used.12 The Upper Level of
Intake (UL) refers to the maximum average daily nutrient
intake levellikely to have no adverse health effects to the
majority of individuals in the general population.12
No studieshave examined and compared the dietary
intakes of young Australian children aged two to three years
to the AGHE age-appropriate recommendationsthusfar.
This is because prior to 2013,there were no quantitative
dietary guidelines for children less than four years ofage,
limiting the comparison of dietary patterns in this age group
to age-appropriate standards.13 The 1995 National Nutrition
Survey (NNS),14 the 2007 Australian NationalChildren’s
Nutrition and PhysicalActivity Survey (ANCNPAS),15 the
Childhood Asthma Prevention Study (CAPS),16 and the 2010
Australian NationalInfantFeeding Survey:Indicator Results17
have allincluded young children,but were only able to
describe food and nutrientintakesin reference to older
children,rather than evaluating intakes based on compari-
son with age-appropriatenationalfood group serving
recommendations.
The aim of this study was to evaluate whether the dietary
intakes of a sample of Australian children aged two to three
years met:(i) the minimum recommended age-appropriate
daily food group servings in the AGHE, and (ii) the NRVs for
vitamin A, thiamin, folate, calcium, iron and zinc.
Methods
This is a secondary data analysis of child dietary intakes from
the Women and Their Children’s Health (WATCH) cohort.18
Pregnant women less than 18 gestational weeks were eligible
to participate in the WATCH study.18 Participants needed to
reside locally and be able to be present at the arranged study
visits at the John Hunter Hospital.18 Between June 2006 and
December 2007, 180 eligible participants were recruited to
the study through various approaches, such as via research
midwives at the John Hunter Hospital antenatal clinic, local
media coverage and by word ofmouth.18 The majority of
participants (n = 133,74% ofsample)remained enrolled
two years after study commencement, although not all par-
ticipants completed all components at study visits.18 Ethics
approvalfor the WATCH study wasobtained from the
Hunter New England Human Research Ethics Committee
and the University ofNewcastle Human Research Ethics
Committee.
Standardised proceduresof data collection were used,
with detailed methodspublished elsewhere.18,19 Briefly,
anthropometry measurements and dietary intakes forthe
mothers and children were collected by qualified dietitians
at the annualstudy visit.18 Data on socio-economic status,
health and lifestyle variables were also obtained via a self-
reported questionnaire at the first study visit.18 Dietary data
of 57 children aged two to three years, including one set of
twins, were available for the current analysis.
The toddler version of the Australian Child and Adoles-
cent Eating Survey (ACAES) was used to evaluate the dietar
intake of children at age two or three years.20 The ACAES is
a 120-item semi-quantitative food frequency questionnaire
(FFQ) that was previouslyvalidated forenergyintake
using the gold-standard doubly labelled water method in
Australian children,21–24 including those aged two to three
years.20,22,23
Mothers were asked to complete the ACAES for
their child’s intake over the past six months as this reporting
period is designed to capture children’s usual eating habits.25
An individual response is required for each food item in the
ACAES, with varied frequency options ranging from ‘never’
to ‘four or more times per day’,18 and for some beverages up
to ‘seven or more glasses per day’.20 Toddler-specific portion
sizes were derived from the 2007 ANCNPAS15 unpublished
data purchased from the Australian SocialScience Data
Archive,Australian NationalUniversity.20 Additionalques-
tionsregarding food-related behavioursare described in
detail elsewhere.18 FFQs were included if they had less than
five missing responses,with three FFQs excluded for this
reason.
Raw data from the FFQ were entered into FoodWorks
Professional(Xyris Software,Brisbane,QLD, Australia)
based on AUSNUT 2007 to derive the amount (weight mass)
of daily food consumption and nutrient intakes. Food con-
sumption data were then exported into MicrosoftExcel
(MicrosoftCooperation,2010, Seattle,United States)
spreadsheets and categorised into food groups correspond-
ing to the core and discretionary groups of AGHE,9 which
has been published previously26 and reported in a number of
studies.22,27,28
Food portions were converted into a number of
servings based on the AGHE standard serving sizes.9 When
food items were not specified in the AGHE,standard por-
tions were derived based on similar energy values of other
food items in the same AGHE food group.For example,a
standard portion of cheese spread/cream cheese was deeme
to be 55 g as this amount provides a similar energy value to
the standard serving size of plain milk (250 mL), hard chees
(40 g) and ricotta cheese (120 g). To calculate consumption
of combination dishes, foods were broken into their compo-
nentingredientsand assigned into the appropriate food
groups.For example,the food item ‘beef/lamb pieces with
vegetables’was disaggregated into meat and vegetables food
groups in the weight ratio of 2:1. Foods that do not fit into
any of the core food groups were evaluated as ‘discretionary
L.K. Chai et al.
© 2015 Dietitians Association of Australia2
binations of types and amounts of foods within the core food
groups to meet the nutritional requirements of each age and
gendergroup,factoring in heightand physicalactivity
levels.11 The information was simplified into the AGHE,a
user-friendly food selection guide.9
NRVs outline the average nutrientrequirements needed
on a daily basisto meetphysiologicalfunction and to
prevent deficiency or chronic disease.12 NRVs for population
average intakes are termed ‘estimated average requirements’
(EARs) and ‘adequate intakes’(AIs).12 The EAR refers to the
everyday nutrient intake levelneeded to meet the require-
mentsof 50% of the healthypopulation in aspecific
life-stage and gender group.12 When an EAR cannot be deter-
mined, then an AI, which is the average daily nutrient intake
levelthatis likely to be sufficient,based on observed or
experimentally determined estimation of nutrient intake by
an apparently healthy cohort, is used.12 The Upper Level of
Intake (UL) refers to the maximum average daily nutrient
intake levellikely to have no adverse health effects to the
majority of individuals in the general population.12
No studieshave examined and compared the dietary
intakes of young Australian children aged two to three years
to the AGHE age-appropriate recommendationsthusfar.
This is because prior to 2013,there were no quantitative
dietary guidelines for children less than four years ofage,
limiting the comparison of dietary patterns in this age group
to age-appropriate standards.13 The 1995 National Nutrition
Survey (NNS),14 the 2007 Australian NationalChildren’s
Nutrition and PhysicalActivity Survey (ANCNPAS),15 the
Childhood Asthma Prevention Study (CAPS),16 and the 2010
Australian NationalInfantFeeding Survey:Indicator Results17
have allincluded young children,but were only able to
describe food and nutrientintakesin reference to older
children,rather than evaluating intakes based on compari-
son with age-appropriatenationalfood group serving
recommendations.
The aim of this study was to evaluate whether the dietary
intakes of a sample of Australian children aged two to three
years met:(i) the minimum recommended age-appropriate
daily food group servings in the AGHE, and (ii) the NRVs for
vitamin A, thiamin, folate, calcium, iron and zinc.
Methods
This is a secondary data analysis of child dietary intakes from
the Women and Their Children’s Health (WATCH) cohort.18
Pregnant women less than 18 gestational weeks were eligible
to participate in the WATCH study.18 Participants needed to
reside locally and be able to be present at the arranged study
visits at the John Hunter Hospital.18 Between June 2006 and
December 2007, 180 eligible participants were recruited to
the study through various approaches, such as via research
midwives at the John Hunter Hospital antenatal clinic, local
media coverage and by word ofmouth.18 The majority of
participants (n = 133,74% ofsample)remained enrolled
two years after study commencement, although not all par-
ticipants completed all components at study visits.18 Ethics
approvalfor the WATCH study wasobtained from the
Hunter New England Human Research Ethics Committee
and the University ofNewcastle Human Research Ethics
Committee.
Standardised proceduresof data collection were used,
with detailed methodspublished elsewhere.18,19 Briefly,
anthropometry measurements and dietary intakes forthe
mothers and children were collected by qualified dietitians
at the annualstudy visit.18 Data on socio-economic status,
health and lifestyle variables were also obtained via a self-
reported questionnaire at the first study visit.18 Dietary data
of 57 children aged two to three years, including one set of
twins, were available for the current analysis.
The toddler version of the Australian Child and Adoles-
cent Eating Survey (ACAES) was used to evaluate the dietar
intake of children at age two or three years.20 The ACAES is
a 120-item semi-quantitative food frequency questionnaire
(FFQ) that was previouslyvalidated forenergyintake
using the gold-standard doubly labelled water method in
Australian children,21–24 including those aged two to three
years.20,22,23
Mothers were asked to complete the ACAES for
their child’s intake over the past six months as this reporting
period is designed to capture children’s usual eating habits.25
An individual response is required for each food item in the
ACAES, with varied frequency options ranging from ‘never’
to ‘four or more times per day’,18 and for some beverages up
to ‘seven or more glasses per day’.20 Toddler-specific portion
sizes were derived from the 2007 ANCNPAS15 unpublished
data purchased from the Australian SocialScience Data
Archive,Australian NationalUniversity.20 Additionalques-
tionsregarding food-related behavioursare described in
detail elsewhere.18 FFQs were included if they had less than
five missing responses,with three FFQs excluded for this
reason.
Raw data from the FFQ were entered into FoodWorks
Professional(Xyris Software,Brisbane,QLD, Australia)
based on AUSNUT 2007 to derive the amount (weight mass)
of daily food consumption and nutrient intakes. Food con-
sumption data were then exported into MicrosoftExcel
(MicrosoftCooperation,2010, Seattle,United States)
spreadsheets and categorised into food groups correspond-
ing to the core and discretionary groups of AGHE,9 which
has been published previously26 and reported in a number of
studies.22,27,28
Food portions were converted into a number of
servings based on the AGHE standard serving sizes.9 When
food items were not specified in the AGHE,standard por-
tions were derived based on similar energy values of other
food items in the same AGHE food group.For example,a
standard portion of cheese spread/cream cheese was deeme
to be 55 g as this amount provides a similar energy value to
the standard serving size of plain milk (250 mL), hard chees
(40 g) and ricotta cheese (120 g). To calculate consumption
of combination dishes, foods were broken into their compo-
nentingredientsand assigned into the appropriate food
groups.For example,the food item ‘beef/lamb pieces with
vegetables’was disaggregated into meat and vegetables food
groups in the weight ratio of 2:1. Foods that do not fit into
any of the core food groups were evaluated as ‘discretionary
L.K. Chai et al.
© 2015 Dietitians Association of Australia2
foods’.9 Nutrient intake data were compared with the NRVs
to assess nutritional adequacy.
All data manipulation and statistical analyses was under-
taken using JMP (version 10,SAS Institute Inc.,Cary,NC,
1989–2007). Results were considered statistically significant
with P-values <0.05. Descriptive statistics were undertaken
to describe maternal and child characteristics by age groups.
Demographic characteristics of mothers (n = 53) were com-
pared to the baseline sample (n = 177) using t-tests.Body
mass index (BMI) z-scores for the children were calculated
using the LMS statistical method.29 Main outcome measures
included children’s daily consumption ofthe AGHE food
groups, macronutrients, and micronutrients; and the propor-
tion of children meeting recommendations as per the AGHE
and NRVs by age groups.The majority of dietary variables
were normally distributed (Shapiro–Wilk Goodness ofFit
tests).Differences between dietary intakes ofchildren and
the AGHE recommended numberof daily servingswere
assessed using t-tests. The initial analysis included the whole
sample and all nutrients. Individual mean daily macronutri-
ent and micronutrient intakes were compared to the EAR or
AI to assesswhetherthe children in thisstudy metthe
NRVs.12 Selected nutrients important for healthy growth and
development were investigated in the subsample (n = 47) in
addition to the number ofdaily servings from the AGHE
food groups to investigate differentaspects ofdiet.Daily
food groups and macronutrientintakes were assessed for
thosemeeting theEARs for vitamin A,thiamin,folate,
calcium, iron and zinc. These nutrients were selected as key
nutrients for health and were deemed as most important for
children’s development and health.30,31They also represent
both fat-soluble and water-soluble vitamins,in addition to
minerals.12
Results
The majority of the mothers were aged between 25 and 34
years old at the age of delivery (62%),married (68%) and
had attained post-year 12 educational qualifications (55%).
No significant difference was found between these maternal
characteristics compared to baseline data.Young children
(n = 54) in the current study were aged two to three years
(mean age 2.7 years) with equalnumbers of boys (n = 27)
and girls (n = 27).The group mean BMI ± standard devia-
tion (SD) was 16.4 kg/m2 ± 1.6.Using the LMS statistical
method,29 the mean z-scores ± SD for weight was 0.4 ± 1.1,
height 0.5 ± 1.1, and BMI 0.1 ± 1.0.
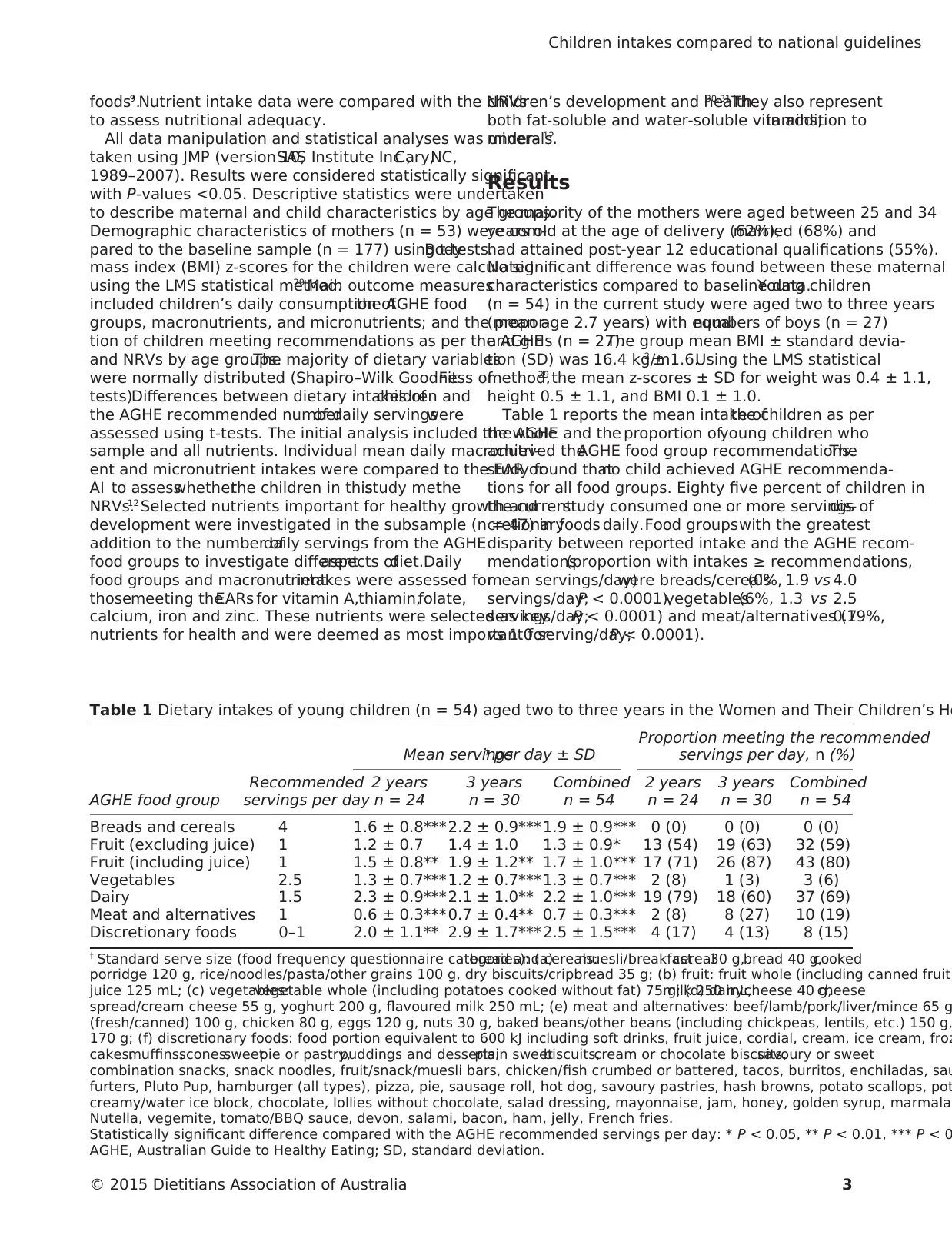
Table 1 reports the mean intake ofthe children as per
the AGHE and the proportion ofyoung children who
achieved theAGHE food group recommendations.The
study found thatno child achieved AGHE recommenda-
tions for all food groups. Eighty five percent of children in
the currentstudy consumed one or more servings ofdis-
cretionaryfoods daily.Food groupswith the greatest
disparity between reported intake and the AGHE recom-
mendations(proportion with intakes ≥ recommendations,
mean servings/day)were breads/cereals(0%, 1.9 vs 4.0
servings/day;P < 0.0001),vegetables(6%, 1.3 vs 2.5
servings/day;P < 0.0001) and meat/alternatives (19%,0.7
vs 1.0 serving/day;P < 0.0001).
Table 1 Dietary intakes of young children (n = 54) aged two to three years in the Women and Their Children’s He
AGHE food group
Recommended
servings per day
Mean servings† per day ± SD
Proportion meeting the recommended
servings per day, n (%)
2 years 3 years Combined 2 years 3 years Combined
n = 24 n = 30 n = 54 n = 24 n = 30 n = 54
Breads and cereals 4 1.6 ± 0.8*** 2.2 ± 0.9***1.9 ± 0.9*** 0 (0) 0 (0) 0 (0)
Fruit (excluding juice) 1 1.2 ± 0.7 1.4 ± 1.0 1.3 ± 0.9* 13 (54) 19 (63) 32 (59)
Fruit (including juice) 1 1.5 ± 0.8** 1.9 ± 1.2** 1.7 ± 1.0*** 17 (71) 26 (87) 43 (80)
Vegetables 2.5 1.3 ± 0.7*** 1.2 ± 0.7***1.3 ± 0.7*** 2 (8) 1 (3) 3 (6)
Dairy 1.5 2.3 ± 0.9*** 2.1 ± 1.0** 2.2 ± 1.0*** 19 (79) 18 (60) 37 (69)
Meat and alternatives 1 0.6 ± 0.3*** 0.7 ± 0.4** 0.7 ± 0.3*** 2 (8) 8 (27) 10 (19)
Discretionary foods 0–1 2.0 ± 1.1** 2.9 ± 1.7*** 2.5 ± 1.5*** 4 (17) 4 (13) 8 (15)
† Standard serve size (food frequency questionnaire categories): (a)bread and cereals:muesli/breakfastcereal30 g,bread 40 g,cooked
porridge 120 g, rice/noodles/pasta/other grains 100 g, dry biscuits/cripbread 35 g; (b) fruit: fruit whole (including canned fruit)
juice 125 mL; (c) vegetables:vegetable whole (including potatoes cooked without fat) 75 g; (d) dairy:milk 250 mL,cheese 40 g,cheese
spread/cream cheese 55 g, yoghurt 200 g, flavoured milk 250 mL; (e) meat and alternatives: beef/lamb/pork/liver/mince 65 g
(fresh/canned) 100 g, chicken 80 g, eggs 120 g, nuts 30 g, baked beans/other beans (including chickpeas, lentils, etc.) 150 g,
170 g; (f) discretionary foods: food portion equivalent to 600 kJ including soft drinks, fruit juice, cordial, cream, ice cream, froz
cakes,muffins,scones,sweetpie or pastry,puddings and desserts,plain sweetbiscuits,cream or chocolate biscuits,savoury or sweet
combination snacks, snack noodles, fruit/snack/muesli bars, chicken/fish crumbed or battered, tacos, burritos, enchiladas, sau
furters, Pluto Pup, hamburger (all types), pizza, pie, sausage roll, hot dog, savoury pastries, hash browns, potato scallops, pot
creamy/water ice block, chocolate, lollies without chocolate, salad dressing, mayonnaise, jam, honey, golden syrup, marmalad
Nutella, vegemite, tomato/BBQ sauce, devon, salami, bacon, ham, jelly, French fries.
Statistically significant difference compared with the AGHE recommended servings per day: * P < 0.05, ** P < 0.01, *** P < 0
AGHE, Australian Guide to Healthy Eating; SD, standard deviation.
Children intakes compared to national guidelines
© 2015 Dietitians Association of Australia 3
to assess nutritional adequacy.
All data manipulation and statistical analyses was under-
taken using JMP (version 10,SAS Institute Inc.,Cary,NC,
1989–2007). Results were considered statistically significant
with P-values <0.05. Descriptive statistics were undertaken
to describe maternal and child characteristics by age groups.
Demographic characteristics of mothers (n = 53) were com-
pared to the baseline sample (n = 177) using t-tests.Body
mass index (BMI) z-scores for the children were calculated
using the LMS statistical method.29 Main outcome measures
included children’s daily consumption ofthe AGHE food
groups, macronutrients, and micronutrients; and the propor-
tion of children meeting recommendations as per the AGHE
and NRVs by age groups.The majority of dietary variables
were normally distributed (Shapiro–Wilk Goodness ofFit
tests).Differences between dietary intakes ofchildren and
the AGHE recommended numberof daily servingswere
assessed using t-tests. The initial analysis included the whole
sample and all nutrients. Individual mean daily macronutri-
ent and micronutrient intakes were compared to the EAR or
AI to assesswhetherthe children in thisstudy metthe
NRVs.12 Selected nutrients important for healthy growth and
development were investigated in the subsample (n = 47) in
addition to the number ofdaily servings from the AGHE
food groups to investigate differentaspects ofdiet.Daily
food groups and macronutrientintakes were assessed for
thosemeeting theEARs for vitamin A,thiamin,folate,
calcium, iron and zinc. These nutrients were selected as key
nutrients for health and were deemed as most important for
children’s development and health.30,31They also represent
both fat-soluble and water-soluble vitamins,in addition to
minerals.12
Results
The majority of the mothers were aged between 25 and 34
years old at the age of delivery (62%),married (68%) and
had attained post-year 12 educational qualifications (55%).
No significant difference was found between these maternal
characteristics compared to baseline data.Young children
(n = 54) in the current study were aged two to three years
(mean age 2.7 years) with equalnumbers of boys (n = 27)
and girls (n = 27).The group mean BMI ± standard devia-
tion (SD) was 16.4 kg/m2 ± 1.6.Using the LMS statistical
method,29 the mean z-scores ± SD for weight was 0.4 ± 1.1,
height 0.5 ± 1.1, and BMI 0.1 ± 1.0.
Table 1 reports the mean intake ofthe children as per
the AGHE and the proportion ofyoung children who
achieved theAGHE food group recommendations.The
study found thatno child achieved AGHE recommenda-
tions for all food groups. Eighty five percent of children in
the currentstudy consumed one or more servings ofdis-
cretionaryfoods daily.Food groupswith the greatest
disparity between reported intake and the AGHE recom-
mendations(proportion with intakes ≥ recommendations,
mean servings/day)were breads/cereals(0%, 1.9 vs 4.0
servings/day;P < 0.0001),vegetables(6%, 1.3 vs 2.5
servings/day;P < 0.0001) and meat/alternatives (19%,0.7
vs 1.0 serving/day;P < 0.0001).
Table 1 Dietary intakes of young children (n = 54) aged two to three years in the Women and Their Children’s He
AGHE food group
Recommended
servings per day
Mean servings† per day ± SD
Proportion meeting the recommended
servings per day, n (%)
2 years 3 years Combined 2 years 3 years Combined
n = 24 n = 30 n = 54 n = 24 n = 30 n = 54
Breads and cereals 4 1.6 ± 0.8*** 2.2 ± 0.9***1.9 ± 0.9*** 0 (0) 0 (0) 0 (0)
Fruit (excluding juice) 1 1.2 ± 0.7 1.4 ± 1.0 1.3 ± 0.9* 13 (54) 19 (63) 32 (59)
Fruit (including juice) 1 1.5 ± 0.8** 1.9 ± 1.2** 1.7 ± 1.0*** 17 (71) 26 (87) 43 (80)
Vegetables 2.5 1.3 ± 0.7*** 1.2 ± 0.7***1.3 ± 0.7*** 2 (8) 1 (3) 3 (6)
Dairy 1.5 2.3 ± 0.9*** 2.1 ± 1.0** 2.2 ± 1.0*** 19 (79) 18 (60) 37 (69)
Meat and alternatives 1 0.6 ± 0.3*** 0.7 ± 0.4** 0.7 ± 0.3*** 2 (8) 8 (27) 10 (19)
Discretionary foods 0–1 2.0 ± 1.1** 2.9 ± 1.7*** 2.5 ± 1.5*** 4 (17) 4 (13) 8 (15)
† Standard serve size (food frequency questionnaire categories): (a)bread and cereals:muesli/breakfastcereal30 g,bread 40 g,cooked
porridge 120 g, rice/noodles/pasta/other grains 100 g, dry biscuits/cripbread 35 g; (b) fruit: fruit whole (including canned fruit)
juice 125 mL; (c) vegetables:vegetable whole (including potatoes cooked without fat) 75 g; (d) dairy:milk 250 mL,cheese 40 g,cheese
spread/cream cheese 55 g, yoghurt 200 g, flavoured milk 250 mL; (e) meat and alternatives: beef/lamb/pork/liver/mince 65 g
(fresh/canned) 100 g, chicken 80 g, eggs 120 g, nuts 30 g, baked beans/other beans (including chickpeas, lentils, etc.) 150 g,
170 g; (f) discretionary foods: food portion equivalent to 600 kJ including soft drinks, fruit juice, cordial, cream, ice cream, froz
cakes,muffins,scones,sweetpie or pastry,puddings and desserts,plain sweetbiscuits,cream or chocolate biscuits,savoury or sweet
combination snacks, snack noodles, fruit/snack/muesli bars, chicken/fish crumbed or battered, tacos, burritos, enchiladas, sau
furters, Pluto Pup, hamburger (all types), pizza, pie, sausage roll, hot dog, savoury pastries, hash browns, potato scallops, pot
creamy/water ice block, chocolate, lollies without chocolate, salad dressing, mayonnaise, jam, honey, golden syrup, marmalad
Nutella, vegemite, tomato/BBQ sauce, devon, salami, bacon, ham, jelly, French fries.
Statistically significant difference compared with the AGHE recommended servings per day: * P < 0.05, ** P < 0.01, *** P < 0
AGHE, Australian Guide to Healthy Eating; SD, standard deviation.
Children intakes compared to national guidelines
© 2015 Dietitians Association of Australia 3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
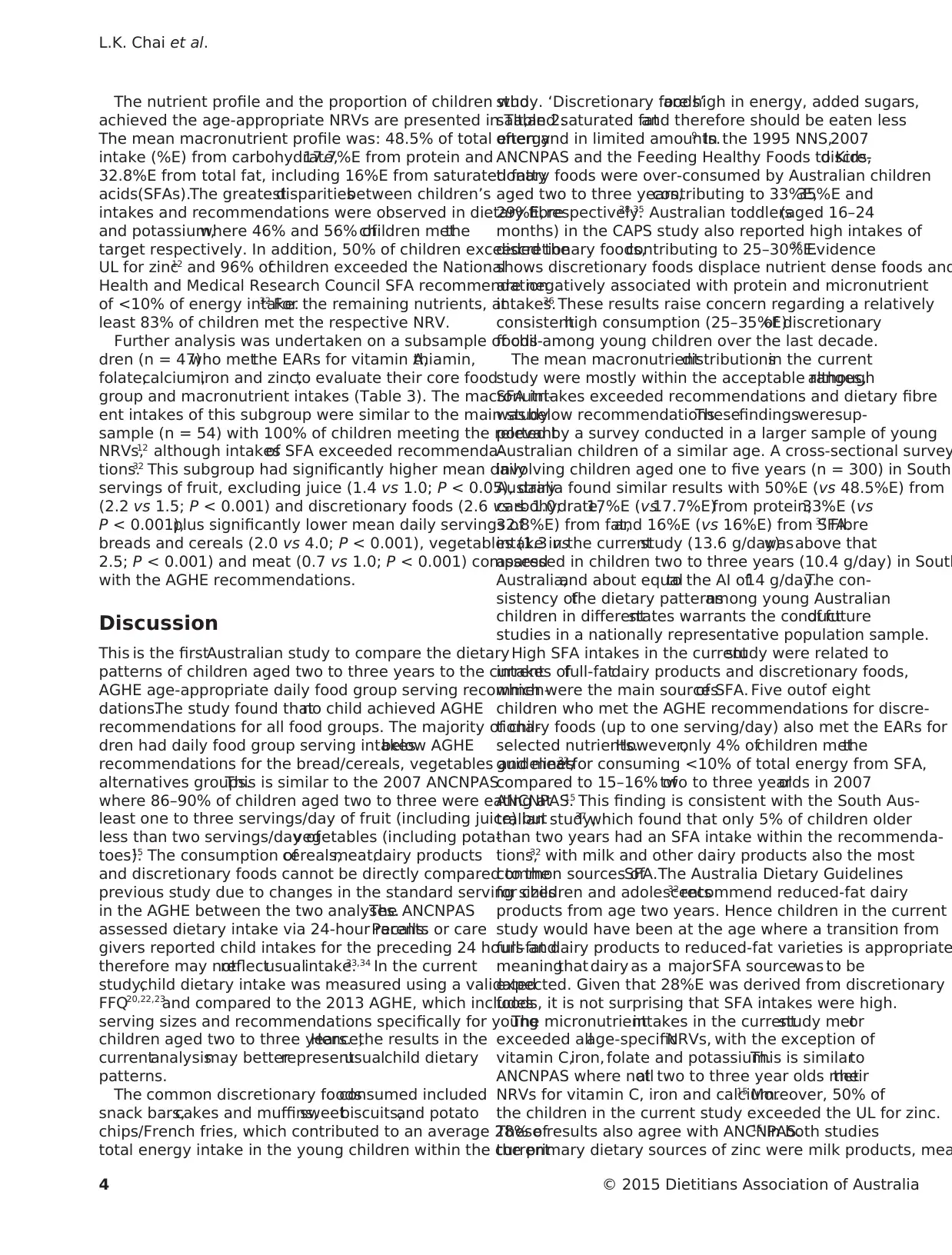
The nutrient profile and the proportion of children who
achieved the age-appropriate NRVs are presented in Table 2.
The mean macronutrient profile was: 48.5% of total energy
intake (%E) from carbohydrate,17.7%E from protein and
32.8%E from total fat, including 16%E from saturated fatty
acids(SFAs).The greatestdisparitiesbetween children’s
intakes and recommendations were observed in dietary fibre
and potassium,where 46% and 56% ofchildren metthe
target respectively. In addition, 50% of children exceeded the
UL for zinc12 and 96% ofchildren exceeded the National
Health and Medical Research Council SFA recommendation
of <10% of energy intake.32 For the remaining nutrients, at
least 83% of children met the respective NRV.
Further analysis was undertaken on a subsample of chil-
dren (n = 47)who metthe EARs for vitamin A,thiamin,
folate,calcium,iron and zinc,to evaluate their core food
group and macronutrient intakes (Table 3). The macronutri-
ent intakes of this subgroup were similar to the main study
sample (n = 54) with 100% of children meeting the relevant
NRVs,12 although intakesof SFA exceeded recommenda-
tions.32 This subgroup had significantly higher mean daily
servings of fruit, excluding juice (1.4 vs 1.0; P < 0.05), dairy
(2.2 vs 1.5; P < 0.001) and discretionary foods (2.6 vs ≤ 1.0;
P < 0.001),plus significantly lower mean daily servings of
breads and cereals (2.0 vs 4.0; P < 0.001), vegetables (1.3 vs
2.5; P < 0.001) and meat (0.7 vs 1.0; P < 0.001) compared
with the AGHE recommendations.
Discussion
This is the firstAustralian study to compare the dietary
patterns of children aged two to three years to the current
AGHE age-appropriate daily food group serving recommen-
dations.The study found thatno child achieved AGHE
recommendations for all food groups. The majority of chil-
dren had daily food group serving intakesbelow AGHE
recommendations for the bread/cereals, vegetables and meat/
alternatives groups.This is similar to the 2007 ANCNPAS
where 86–90% of children aged two to three were eating at
least one to three servings/day of fruit (including juice) but
less than two servings/day ofvegetables (including pota-
toes).15 The consumption ofcereals,meat,dairy products
and discretionary foods cannot be directly compared to the
previous study due to changes in the standard serving sizes
in the AGHE between the two analyses.The ANCNPAS
assessed dietary intake via 24-hour recalls.Parents or care
givers reported child intakes for the preceding 24 hours and
therefore may notreflectusualintake.33,34 In the current
study,child dietary intake was measured using a validated
FFQ20,22,23
and compared to the 2013 AGHE, which includes
serving sizes and recommendations specifically for young
children aged two to three years.Hence,the results in the
currentanalysismay betterrepresentusualchild dietary
patterns.
The common discretionary foodsconsumed included
snack bars,cakes and muffins,sweetbiscuits,and potato
chips/French fries, which contributed to an average 28% of
total energy intake in the young children within the current
study. ‘Discretionary foods’are high in energy, added sugars,
salt,and saturated fatand therefore should be eaten less
often and in limited amounts.9 In the 1995 NNS,2007
ANCNPAS and the Feeding Healthy Foods to Kids,discre-
tionary foods were over-consumed by Australian children
aged two to three years,contributing to 33%E,35%E and
29%E, respectively.28,35 Australian toddlers(aged 16–24
months) in the CAPS study also reported high intakes of
discretionary foods,contributing to 25–30%E.36 Evidence
shows discretionary foods displace nutrient dense foods and
are negatively associated with protein and micronutrient
intakes.36 These results raise concern regarding a relatively
consistenthigh consumption (25–35%E)of discretionary
foods among young children over the last decade.
The mean macronutrientdistributionsin the current
study were mostly within the acceptable ranges,although
SFA intakes exceeded recommendations and dietary fibre
was below recommendations.Thesefindingsweresup-
ported by a survey conducted in a larger sample of young
Australian children of a similar age. A cross-sectional survey
involving children aged one to five years (n = 300) in South
Australia found similar results with 50%E (vs 48.5%E) from
carbohydrate,17%E (vs17.7%E)from protein,33%E (vs
32.8%E) from fat,and 16%E (vs 16%E) from SFA.37 Fibre
intake in the currentstudy (13.6 g/day)wasabove that
assessed in children two to three years (10.4 g/day) in South
Australia,and about equalto the AI of14 g/day.The con-
sistency ofthe dietary patternsamong young Australian
children in differentstates warrants the conductof future
studies in a nationally representative population sample.
High SFA intakes in the currentstudy were related to
intakes offull-fatdairy products and discretionary foods,
which were the main sourcesof SFA. Five outof eight
children who met the AGHE recommendations for discre-
tionary foods (up to one serving/day) also met the EARs for
selected nutrients.However,only 4% ofchildren metthe
guidelines32 for consuming <10% of total energy from SFA,
compared to 15–16% oftwo to three yearolds in 2007
ANCNPAS.15 This finding is consistent with the South Aus-
tralian study,37 which found that only 5% of children older
than two years had an SFA intake within the recommenda-
tions,32 with milk and other dairy products also the most
common sources ofSFA.The Australia Dietary Guidelines
for children and adolescents32 recommend reduced-fat dairy
products from age two years. Hence children in the current
study would have been at the age where a transition from
full-fat dairy products to reduced-fat varieties is appropriate
meaningthat dairy as a majorSFA sourcewas to be
expected. Given that 28%E was derived from discretionary
foods, it is not surprising that SFA intakes were high.
The micronutrientintakes in the currentstudy metor
exceeded allage-specificNRVs, with the exception of
vitamin C,iron, folate and potassium.This is similarto
ANCNPAS where notall two to three year olds mettheir
NRVs for vitamin C, iron and calcium.15 Moreover, 50% of
the children in the current study exceeded the UL for zinc.
These results also agree with ANCNPAS.15 In both studies
the primary dietary sources of zinc were milk products, mea
L.K. Chai et al.
© 2015 Dietitians Association of Australia4
achieved the age-appropriate NRVs are presented in Table 2.
The mean macronutrient profile was: 48.5% of total energy
intake (%E) from carbohydrate,17.7%E from protein and
32.8%E from total fat, including 16%E from saturated fatty
acids(SFAs).The greatestdisparitiesbetween children’s
intakes and recommendations were observed in dietary fibre
and potassium,where 46% and 56% ofchildren metthe
target respectively. In addition, 50% of children exceeded the
UL for zinc12 and 96% ofchildren exceeded the National
Health and Medical Research Council SFA recommendation
of <10% of energy intake.32 For the remaining nutrients, at
least 83% of children met the respective NRV.
Further analysis was undertaken on a subsample of chil-
dren (n = 47)who metthe EARs for vitamin A,thiamin,
folate,calcium,iron and zinc,to evaluate their core food
group and macronutrient intakes (Table 3). The macronutri-
ent intakes of this subgroup were similar to the main study
sample (n = 54) with 100% of children meeting the relevant
NRVs,12 although intakesof SFA exceeded recommenda-
tions.32 This subgroup had significantly higher mean daily
servings of fruit, excluding juice (1.4 vs 1.0; P < 0.05), dairy
(2.2 vs 1.5; P < 0.001) and discretionary foods (2.6 vs ≤ 1.0;
P < 0.001),plus significantly lower mean daily servings of
breads and cereals (2.0 vs 4.0; P < 0.001), vegetables (1.3 vs
2.5; P < 0.001) and meat (0.7 vs 1.0; P < 0.001) compared
with the AGHE recommendations.
Discussion
This is the firstAustralian study to compare the dietary
patterns of children aged two to three years to the current
AGHE age-appropriate daily food group serving recommen-
dations.The study found thatno child achieved AGHE
recommendations for all food groups. The majority of chil-
dren had daily food group serving intakesbelow AGHE
recommendations for the bread/cereals, vegetables and meat/
alternatives groups.This is similar to the 2007 ANCNPAS
where 86–90% of children aged two to three were eating at
least one to three servings/day of fruit (including juice) but
less than two servings/day ofvegetables (including pota-
toes).15 The consumption ofcereals,meat,dairy products
and discretionary foods cannot be directly compared to the
previous study due to changes in the standard serving sizes
in the AGHE between the two analyses.The ANCNPAS
assessed dietary intake via 24-hour recalls.Parents or care
givers reported child intakes for the preceding 24 hours and
therefore may notreflectusualintake.33,34 In the current
study,child dietary intake was measured using a validated
FFQ20,22,23
and compared to the 2013 AGHE, which includes
serving sizes and recommendations specifically for young
children aged two to three years.Hence,the results in the
currentanalysismay betterrepresentusualchild dietary
patterns.
The common discretionary foodsconsumed included
snack bars,cakes and muffins,sweetbiscuits,and potato
chips/French fries, which contributed to an average 28% of
total energy intake in the young children within the current
study. ‘Discretionary foods’are high in energy, added sugars,
salt,and saturated fatand therefore should be eaten less
often and in limited amounts.9 In the 1995 NNS,2007
ANCNPAS and the Feeding Healthy Foods to Kids,discre-
tionary foods were over-consumed by Australian children
aged two to three years,contributing to 33%E,35%E and
29%E, respectively.28,35 Australian toddlers(aged 16–24
months) in the CAPS study also reported high intakes of
discretionary foods,contributing to 25–30%E.36 Evidence
shows discretionary foods displace nutrient dense foods and
are negatively associated with protein and micronutrient
intakes.36 These results raise concern regarding a relatively
consistenthigh consumption (25–35%E)of discretionary
foods among young children over the last decade.
The mean macronutrientdistributionsin the current
study were mostly within the acceptable ranges,although
SFA intakes exceeded recommendations and dietary fibre
was below recommendations.Thesefindingsweresup-
ported by a survey conducted in a larger sample of young
Australian children of a similar age. A cross-sectional survey
involving children aged one to five years (n = 300) in South
Australia found similar results with 50%E (vs 48.5%E) from
carbohydrate,17%E (vs17.7%E)from protein,33%E (vs
32.8%E) from fat,and 16%E (vs 16%E) from SFA.37 Fibre
intake in the currentstudy (13.6 g/day)wasabove that
assessed in children two to three years (10.4 g/day) in South
Australia,and about equalto the AI of14 g/day.The con-
sistency ofthe dietary patternsamong young Australian
children in differentstates warrants the conductof future
studies in a nationally representative population sample.
High SFA intakes in the currentstudy were related to
intakes offull-fatdairy products and discretionary foods,
which were the main sourcesof SFA. Five outof eight
children who met the AGHE recommendations for discre-
tionary foods (up to one serving/day) also met the EARs for
selected nutrients.However,only 4% ofchildren metthe
guidelines32 for consuming <10% of total energy from SFA,
compared to 15–16% oftwo to three yearolds in 2007
ANCNPAS.15 This finding is consistent with the South Aus-
tralian study,37 which found that only 5% of children older
than two years had an SFA intake within the recommenda-
tions,32 with milk and other dairy products also the most
common sources ofSFA.The Australia Dietary Guidelines
for children and adolescents32 recommend reduced-fat dairy
products from age two years. Hence children in the current
study would have been at the age where a transition from
full-fat dairy products to reduced-fat varieties is appropriate
meaningthat dairy as a majorSFA sourcewas to be
expected. Given that 28%E was derived from discretionary
foods, it is not surprising that SFA intakes were high.
The micronutrientintakes in the currentstudy metor
exceeded allage-specificNRVs, with the exception of
vitamin C,iron, folate and potassium.This is similarto
ANCNPAS where notall two to three year olds mettheir
NRVs for vitamin C, iron and calcium.15 Moreover, 50% of
the children in the current study exceeded the UL for zinc.
These results also agree with ANCNPAS.15 In both studies
the primary dietary sources of zinc were milk products, mea
L.K. Chai et al.
© 2015 Dietitians Association of Australia4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
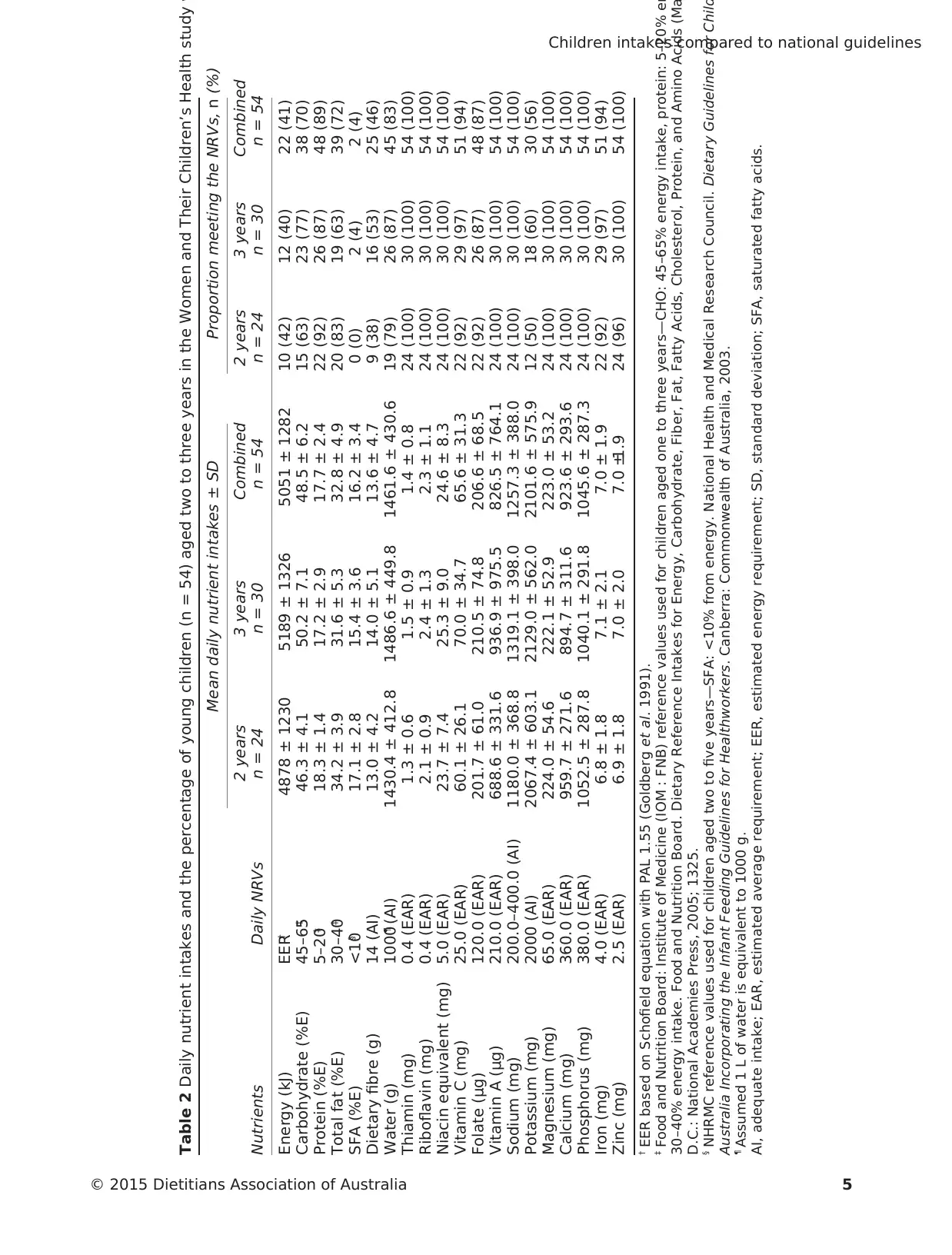
Table 2 Daily nutrient intakes and the percentage of young children (n = 54) aged two to three years in the Women and Their Children’s Health study w
Nutrients Daily NRVs
Mean daily nutrient intakes ± SD Proportion meeting the NRVs, n (%)
2 years
n = 24
3 years
n = 30
Combined 2 years 3 years Combined
n = 54 n = 24 n = 30 n = 54
Energy (kJ) EER† 4878 ± 1230 5189 ± 1326 5051 ± 1282 10 (42) 12 (40) 22 (41)
Carbohydrate (%E) 45–65‡ 46.3 ± 4.1 50.2 ± 7.1 48.5 ± 6.2 15 (63) 23 (77) 38 (70)
Protein (%E) 5–20‡ 18.3 ± 1.4 17.2 ± 2.9 17.7 ± 2.4 22 (92) 26 (87) 48 (89)
Total fat (%E) 30–40‡ 34.2 ± 3.9 31.6 ± 5.3 32.8 ± 4.9 20 (83) 19 (63) 39 (72)
SFA (%E) <10§ 17.1 ± 2.8 15.4 ± 3.6 16.2 ± 3.4 0 (0) 2 (4) 2 (4)
Dietary fibre (g) 14 (AI) 13.0 ± 4.2 14.0 ± 5.1 13.6 ± 4.7 9 (38) 16 (53) 25 (46)
Water (g) 1000¶ (AI) 1430.4 ± 412.8 1486.6 ± 449.8 1461.6 ± 430.6 19 (79) 26 (87) 45 (83)
Thiamin (mg) 0.4 (EAR) 1.3 ± 0.6 1.5 ± 0.9 1.4 ± 0.8 24 (100) 30 (100) 54 (100)
Riboflavin (mg) 0.4 (EAR) 2.1 ± 0.9 2.4 ± 1.3 2.3 ± 1.1 24 (100) 30 (100) 54 (100)
Niacin equivalent (mg) 5.0 (EAR) 23.7 ± 7.4 25.3 ± 9.0 24.6 ± 8.3 24 (100) 30 (100) 54 (100)
Vitamin C (mg) 25.0 (EAR) 60.1 ± 26.1 70.0 ± 34.7 65.6 ± 31.3 22 (92) 29 (97) 51 (94)
Folate (μg) 120.0 (EAR) 201.7 ± 61.0 210.5 ± 74.8 206.6 ± 68.5 22 (92) 26 (87) 48 (87)
Vitamin A (μg) 210.0 (EAR) 688.6 ± 331.6 936.9 ± 975.5 826.5 ± 764.1 24 (100) 30 (100) 54 (100)
Sodium (mg) 200.0–400.0 (AI) 1180.0 ± 368.8 1319.1 ± 398.0 1257.3 ± 388.0 24 (100) 30 (100) 54 (100)
Potassium (mg) 2000 (AI) 2067.4 ± 603.1 2129.0 ± 562.0 2101.6 ± 575.9 12 (50) 18 (60) 30 (56)
Magnesium (mg) 65.0 (EAR) 224.0 ± 54.6 222.1 ± 52.9 223.0 ± 53.2 24 (100) 30 (100) 54 (100)
Calcium (mg) 360.0 (EAR) 959.7 ± 271.6 894.7 ± 311.6 923.6 ± 293.6 24 (100) 30 (100) 54 (100)
Phosphorus (mg) 380.0 (EAR) 1052.5 ± 287.8 1040.1 ± 291.8 1045.6 ± 287.3 24 (100) 30 (100) 54 (100)
Iron (mg) 4.0 (EAR) 6.8 ± 1.8 7.1 ± 2.1 7.0 ± 1.9 22 (92) 29 (97) 51 (94)
Zinc (mg) 2.5 (EAR) 6.9 ± 1.8 7.0 ± 2.0 7.0 ±1.9 24 (96) 30 (100) 54 (100)
† EER based on Schofield equation with PAL 1.55 (Goldberg et al. 1991).
‡ Food and Nutrition Board: Institute of Medicine (IOM : FNB) reference values used for children aged one to three years—CHO: 45–65% energy intake, protein: 5–20% en
30–40% energy intake. Food and Nutrition Board. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Ma
D.C.: National Academies Press, 2005; 1325.
§ NHRMC reference values used for children aged two to five years—SFA: <10% from energy. National Health and Medical Research Council. Dietary Guidelines for Child
Australia Incorporating the Infant Feeding Guidelines for Healthworkers. Canberra: Commonwealth of Australia, 2003.
¶ Assumed 1 L of water is equivalent to 1000 g.
AI, adequate intake; EAR, estimated average requirement; EER, estimated energy requirement; SD, standard deviation; SFA, saturated fatty acids.
Children intakes compared to national guidelines
© 2015 Dietitians Association of Australia 5
Nutrients Daily NRVs
Mean daily nutrient intakes ± SD Proportion meeting the NRVs, n (%)
2 years
n = 24
3 years
n = 30
Combined 2 years 3 years Combined
n = 54 n = 24 n = 30 n = 54
Energy (kJ) EER† 4878 ± 1230 5189 ± 1326 5051 ± 1282 10 (42) 12 (40) 22 (41)
Carbohydrate (%E) 45–65‡ 46.3 ± 4.1 50.2 ± 7.1 48.5 ± 6.2 15 (63) 23 (77) 38 (70)
Protein (%E) 5–20‡ 18.3 ± 1.4 17.2 ± 2.9 17.7 ± 2.4 22 (92) 26 (87) 48 (89)
Total fat (%E) 30–40‡ 34.2 ± 3.9 31.6 ± 5.3 32.8 ± 4.9 20 (83) 19 (63) 39 (72)
SFA (%E) <10§ 17.1 ± 2.8 15.4 ± 3.6 16.2 ± 3.4 0 (0) 2 (4) 2 (4)
Dietary fibre (g) 14 (AI) 13.0 ± 4.2 14.0 ± 5.1 13.6 ± 4.7 9 (38) 16 (53) 25 (46)
Water (g) 1000¶ (AI) 1430.4 ± 412.8 1486.6 ± 449.8 1461.6 ± 430.6 19 (79) 26 (87) 45 (83)
Thiamin (mg) 0.4 (EAR) 1.3 ± 0.6 1.5 ± 0.9 1.4 ± 0.8 24 (100) 30 (100) 54 (100)
Riboflavin (mg) 0.4 (EAR) 2.1 ± 0.9 2.4 ± 1.3 2.3 ± 1.1 24 (100) 30 (100) 54 (100)
Niacin equivalent (mg) 5.0 (EAR) 23.7 ± 7.4 25.3 ± 9.0 24.6 ± 8.3 24 (100) 30 (100) 54 (100)
Vitamin C (mg) 25.0 (EAR) 60.1 ± 26.1 70.0 ± 34.7 65.6 ± 31.3 22 (92) 29 (97) 51 (94)
Folate (μg) 120.0 (EAR) 201.7 ± 61.0 210.5 ± 74.8 206.6 ± 68.5 22 (92) 26 (87) 48 (87)
Vitamin A (μg) 210.0 (EAR) 688.6 ± 331.6 936.9 ± 975.5 826.5 ± 764.1 24 (100) 30 (100) 54 (100)
Sodium (mg) 200.0–400.0 (AI) 1180.0 ± 368.8 1319.1 ± 398.0 1257.3 ± 388.0 24 (100) 30 (100) 54 (100)
Potassium (mg) 2000 (AI) 2067.4 ± 603.1 2129.0 ± 562.0 2101.6 ± 575.9 12 (50) 18 (60) 30 (56)
Magnesium (mg) 65.0 (EAR) 224.0 ± 54.6 222.1 ± 52.9 223.0 ± 53.2 24 (100) 30 (100) 54 (100)
Calcium (mg) 360.0 (EAR) 959.7 ± 271.6 894.7 ± 311.6 923.6 ± 293.6 24 (100) 30 (100) 54 (100)
Phosphorus (mg) 380.0 (EAR) 1052.5 ± 287.8 1040.1 ± 291.8 1045.6 ± 287.3 24 (100) 30 (100) 54 (100)
Iron (mg) 4.0 (EAR) 6.8 ± 1.8 7.1 ± 2.1 7.0 ± 1.9 22 (92) 29 (97) 51 (94)
Zinc (mg) 2.5 (EAR) 6.9 ± 1.8 7.0 ± 2.0 7.0 ±1.9 24 (96) 30 (100) 54 (100)
† EER based on Schofield equation with PAL 1.55 (Goldberg et al. 1991).
‡ Food and Nutrition Board: Institute of Medicine (IOM : FNB) reference values used for children aged one to three years—CHO: 45–65% energy intake, protein: 5–20% en
30–40% energy intake. Food and Nutrition Board. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Ma
D.C.: National Academies Press, 2005; 1325.
§ NHRMC reference values used for children aged two to five years—SFA: <10% from energy. National Health and Medical Research Council. Dietary Guidelines for Child
Australia Incorporating the Infant Feeding Guidelines for Healthworkers. Canberra: Commonwealth of Australia, 2003.
¶ Assumed 1 L of water is equivalent to 1000 g.
AI, adequate intake; EAR, estimated average requirement; EER, estimated energy requirement; SD, standard deviation; SFA, saturated fatty acids.
Children intakes compared to national guidelines
© 2015 Dietitians Association of Australia 5
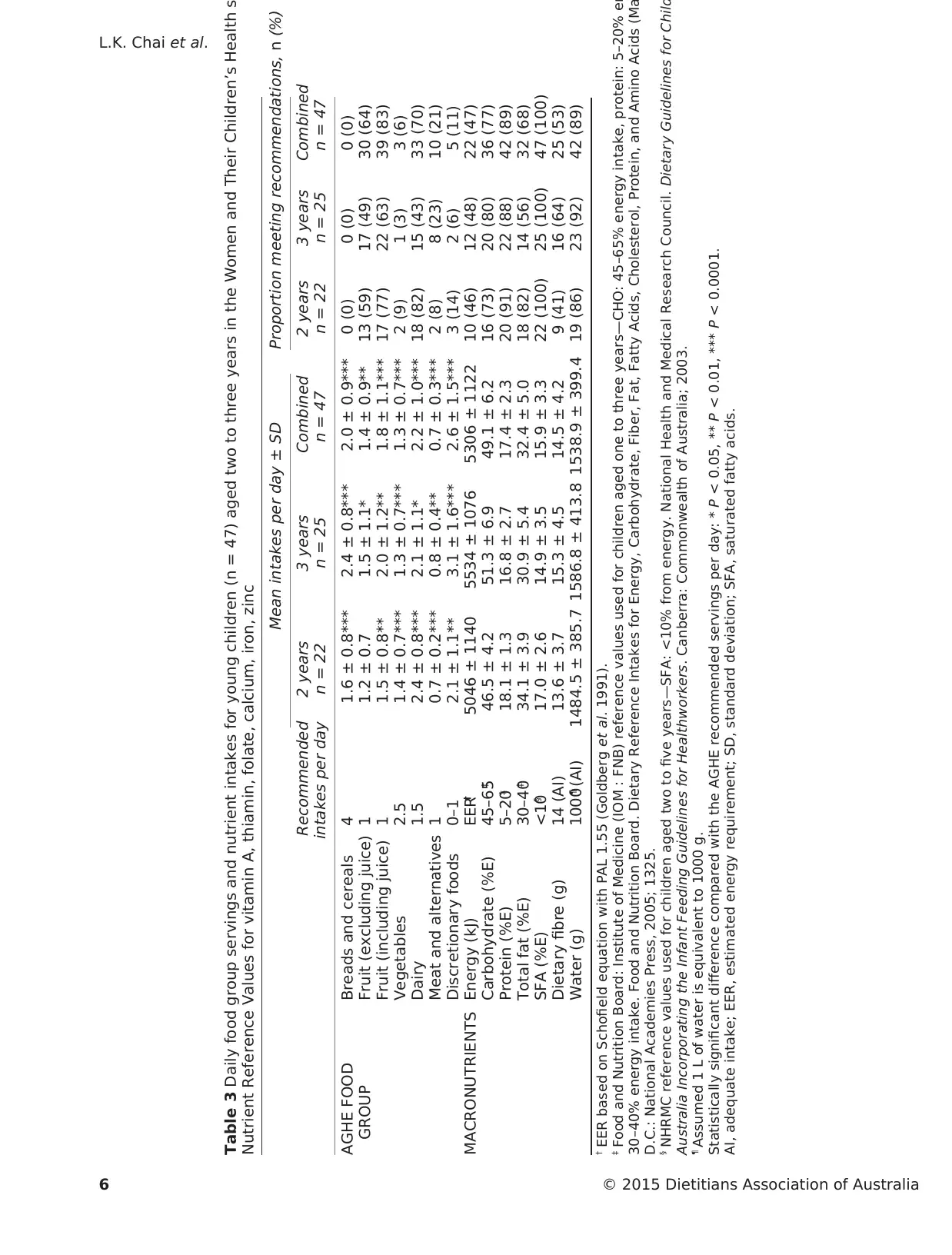
Table 3 Daily food group servings and nutrient intakes for young children (n = 47) aged two to three years in the Women and Their Children’s Health st
Nutrient Reference Values for vitamin A, thiamin, folate, calcium, iron, zinc
Recommended
intakes per day
Mean intakes per day ± SD Proportion meeting recommendations, n (%)
2 years 3 years Combined 2 years 3 years Combined
n = 22 n = 25 n = 47 n = 22 n = 25 n = 47
AGHE FOOD
GROUP
Breads and cereals 4 1.6 ± 0.8*** 2.4 ± 0.8*** 2.0 ± 0.9*** 0 (0) 0 (0) 0 (0)
Fruit (excluding juice) 1 1.2 ± 0.7 1.5 ± 1.1* 1.4 ± 0.9** 13 (59) 17 (49) 30 (64)
Fruit (including juice) 1 1.5 ± 0.8** 2.0 ± 1.2** 1.8 ± 1.1*** 17 (77) 22 (63) 39 (83)
Vegetables 2.5 1.4 ± 0.7*** 1.3 ± 0.7*** 1.3 ± 0.7*** 2 (9) 1 (3) 3 (6)
Dairy 1.5 2.4 ± 0.8*** 2.1 ± 1.1* 2.2 ± 1.0*** 18 (82) 15 (43) 33 (70)
Meat and alternatives 1 0.7 ± 0.2*** 0.8 ± 0.4** 0.7 ± 0.3*** 2 (8) 8 (23) 10 (21)
Discretionary foods 0–1 2.1 ± 1.1** 3.1 ± 1.6*** 2.6 ± 1.5*** 3 (14) 2 (6) 5 (11)
MACRONUTRIENTS Energy (kJ) EER† 5046 ± 1140 5534 ± 1076 5306 ± 1122 10 (46) 12 (48) 22 (47)
Carbohydrate (%E) 45–65‡ 46.5 ± 4.2 51.3 ± 6.9 49.1 ± 6.2 16 (73) 20 (80) 36 (77)
Protein (%E) 5–20‡ 18.1 ± 1.3 16.8 ± 2.7 17.4 ± 2.3 20 (91) 22 (88) 42 (89)
Total fat (%E) 30–40‡ 34.1 ± 3.9 30.9 ± 5.4 32.4 ± 5.0 18 (82) 14 (56) 32 (68)
SFA (%E) <10§ 17.0 ± 2.6 14.9 ± 3.5 15.9 ± 3.3 22 (100) 25 (100) 47 (100)
Dietary fibre (g) 14 (AI) 13.6 ± 3.7 15.3 ± 4.5 14.5 ± 4.2 9 (41) 16 (64) 25 (53)
Water (g) 1000¶ (AI) 1484.5 ± 385.7 1586.8 ± 413.8 1538.9 ± 399.4 19 (86) 23 (92) 42 (89)
† EER based on Schofield equation with PAL 1.55 (Goldberg et al. 1991).
‡ Food and Nutrition Board: Institute of Medicine (IOM : FNB) reference values used for children aged one to three years—CHO: 45–65% energy intake, protein: 5–20% en
30–40% energy intake. Food and Nutrition Board. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Ma
D.C.: National Academies Press, 2005; 1325.
§ NHRMC reference values used for children aged two to five years—SFA: <10% from energy. National Health and Medical Research Council. Dietary Guidelines for Child
Australia Incorporating the Infant Feeding Guidelines for Healthworkers. Canberra: Commonwealth of Australia; 2003.
¶ Assumed 1 L of water is equivalent to 1000 g.
Statistically significant difference compared with the AGHE recommended servings per day: * P < 0.05, ** P < 0.01, *** P < 0.0001.
AI, adequate intake; EER, estimated energy requirement; SD, standard deviation; SFA, saturated fatty acids.
L.K. Chai et al.
© 2015 Dietitians Association of Australia6
Nutrient Reference Values for vitamin A, thiamin, folate, calcium, iron, zinc
Recommended
intakes per day
Mean intakes per day ± SD Proportion meeting recommendations, n (%)
2 years 3 years Combined 2 years 3 years Combined
n = 22 n = 25 n = 47 n = 22 n = 25 n = 47
AGHE FOOD
GROUP
Breads and cereals 4 1.6 ± 0.8*** 2.4 ± 0.8*** 2.0 ± 0.9*** 0 (0) 0 (0) 0 (0)
Fruit (excluding juice) 1 1.2 ± 0.7 1.5 ± 1.1* 1.4 ± 0.9** 13 (59) 17 (49) 30 (64)
Fruit (including juice) 1 1.5 ± 0.8** 2.0 ± 1.2** 1.8 ± 1.1*** 17 (77) 22 (63) 39 (83)
Vegetables 2.5 1.4 ± 0.7*** 1.3 ± 0.7*** 1.3 ± 0.7*** 2 (9) 1 (3) 3 (6)
Dairy 1.5 2.4 ± 0.8*** 2.1 ± 1.1* 2.2 ± 1.0*** 18 (82) 15 (43) 33 (70)
Meat and alternatives 1 0.7 ± 0.2*** 0.8 ± 0.4** 0.7 ± 0.3*** 2 (8) 8 (23) 10 (21)
Discretionary foods 0–1 2.1 ± 1.1** 3.1 ± 1.6*** 2.6 ± 1.5*** 3 (14) 2 (6) 5 (11)
MACRONUTRIENTS Energy (kJ) EER† 5046 ± 1140 5534 ± 1076 5306 ± 1122 10 (46) 12 (48) 22 (47)
Carbohydrate (%E) 45–65‡ 46.5 ± 4.2 51.3 ± 6.9 49.1 ± 6.2 16 (73) 20 (80) 36 (77)
Protein (%E) 5–20‡ 18.1 ± 1.3 16.8 ± 2.7 17.4 ± 2.3 20 (91) 22 (88) 42 (89)
Total fat (%E) 30–40‡ 34.1 ± 3.9 30.9 ± 5.4 32.4 ± 5.0 18 (82) 14 (56) 32 (68)
SFA (%E) <10§ 17.0 ± 2.6 14.9 ± 3.5 15.9 ± 3.3 22 (100) 25 (100) 47 (100)
Dietary fibre (g) 14 (AI) 13.6 ± 3.7 15.3 ± 4.5 14.5 ± 4.2 9 (41) 16 (64) 25 (53)
Water (g) 1000¶ (AI) 1484.5 ± 385.7 1586.8 ± 413.8 1538.9 ± 399.4 19 (86) 23 (92) 42 (89)
† EER based on Schofield equation with PAL 1.55 (Goldberg et al. 1991).
‡ Food and Nutrition Board: Institute of Medicine (IOM : FNB) reference values used for children aged one to three years—CHO: 45–65% energy intake, protein: 5–20% en
30–40% energy intake. Food and Nutrition Board. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Ma
D.C.: National Academies Press, 2005; 1325.
§ NHRMC reference values used for children aged two to five years—SFA: <10% from energy. National Health and Medical Research Council. Dietary Guidelines for Child
Australia Incorporating the Infant Feeding Guidelines for Healthworkers. Canberra: Commonwealth of Australia; 2003.
¶ Assumed 1 L of water is equivalent to 1000 g.
Statistically significant difference compared with the AGHE recommended servings per day: * P < 0.05, ** P < 0.01, *** P < 0.0001.
AI, adequate intake; EER, estimated energy requirement; SD, standard deviation; SFA, saturated fatty acids.
L.K. Chai et al.
© 2015 Dietitians Association of Australia6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
and poultry, and cereal products. It is possible that children
in this age group are atrisk of excessive zinc intakes.38
However, these findings need to be interpreted with caution
given thatadverse effects secondary to high dietary zinc
intakes have not been reported in Australia.Therefore our
study supports Rangan and Samman’s conclusions that the
currentUL for the two- to three-years age group may be
underestimated and should be reviewed.38
Further analyses were undertaken to assess whether the
eating patterns ofchildren who met the NRVs for vitamin
A, thiamin,folate,calcium,iron and zinc were similar or
differentfrom the eating pattern suggested by the AGHE.
The majority of children in this study met the NRV targets
by followinga patternthat deviatedfrom the age-
appropriaterecommendations.This demonstratedthat
young children could meet the NRVs for selected nutrients
by consuming a significantly greater number of daily serv-
ingsof fruit (excluding juice)and dairy,in combination
with significantly lowermean daily servingsof breads/
cereals,vegetables and meat/alternatives compared to the
AGHE.Implications ofthese findings indicate that model-
ling of food group patterns to inform future refinements of
the AGHE could considerthis approach.Potentially this
would lead to incorporation of even greater diversity in the
distribution of food group servings, within optimal nutrient
intake ranges.
Findings from the presentstudy are similar to those of
nationally representative studies ofAmerican and Belgian
children where a large proportion did notmeetnational
recommendations for food group servings.39,40Sixty percent
and 93% ofAmerican children aged 1–18 years did not
consume the recommended number of servings of fruit and
vegetables,respectively.39 The majority (>50%) ofyounger
Belgian children aged three to seven years did not meet the
recommended number of servings of fruits,vegetables and
dairy products.40
The current study has a few limitations and, in particular,
the small sample size. Hence, results from this study may not
be representative ofother populations and ethnicities and
should be interpreted with caution. The study, although not
population-based,is the firstAustralian study to examine
associations between dietary patterns of children aged two to
three years compared to the revised 2013 AGHE.9 While the
FFQ data were proxy-reported by mothers with a possibility
of reporting bias as parents were unable to observe child
intake at preschoolor day care,the ACAES has been vali-
dated for total energy intake18 in preschool age children and
micronutrient intakes in children above five years.20,21While
FFQs are able to capture usualintake over a longer time
frame,25 and reliable for estimating micronutrient intakes in
infants and preschool children,41 it is acknowledged that the
ACAES has notbeen validated atthe food group level.In
addition, it must be acknowledged that for younger children
the six months reporting period of the FFQ may not accu-
rately reflecttheirusualintake overthattime.A further
limitation is that not all EARs and AIs were considered in the
subsample analysis and hence results should be interpreted
with caution.
In conclusion, the dietary patterns of Australian children
aged two to three in the current study do not align with the
recommended daily servings in the AGHE.Children who
achieved the NRVs for nutrients importantfor health and
development consumed more fruit, dairy and discretionary
servings than current recommendations.Further studies in
larger nationally representative population samples should
be undertaken to evaluate whetherthe currentfindings
apply. Findings from larger cohorts may help to inform the
future modelling of food patterns to incorporate even greater
diversity in the distribution offood group servings while
optimising nutrient intakes.
Funding source
The WATCH study received funding from the University of
Newcastle, the Newcastle Permanent Charitable Foundation
and the John Hunter HospitalCharitable Trust.The study
sponsors were not involved in research design, implementa-
tion or publication.
Conflict of interest
The authors declare that they have no competing interests.
Authorship
LKC, LMW,AJH, MLB, TLB and CEC contributed to the
methodologicaldesign ofthe study;LKC performed data
analysisand prepared the manuscript.LKC, LMW, TLB,
AJH, MLB,RS and CEC contributed to the revision ofthe
manuscriptand tables.AJH, CEC and RS established the
originalWATCH cohortand MLB contributed to the data
collection. This study was undertaken as a part requirement
for the degreeof Bachelorof Nutrition and Dietetics
(Honours) at the University of Newcastle (LKC),Australia.
All authors contributed to reviewing, editing and approving
the final version of the manuscript.
References
1 Lynch J,Smith GD.A life course approach to chronic disease
epidemiology. Annu Rev Public Health 2005; 26: 1–35.
2 Kaikkonen JE, Mikkila V, Magnussen CG, Juonala M, Viikari JS,
Raitakari OT. Does childhood nutrition influence adult cardio-
vascular disease risk?—insights from the Young Finns Study.
Ann Med 2013; 45: 120–28.
3 Jaaskelainen P,Magnussen CG,Pahkala K et al.Childhood
nutrition in predicting metabolic syndrome in adults:the car-
diovascular risk in Young Finns Study. Diabetes Care 2012; 35:
1937–43.
4 Togo P, Osler M, Sorensen T, Heitmann B. Food intake patterns
and body mass index iobservationalstudies.Int J Obes Relat
Metab Disord 2001; 25: 1741–51.
5 HorodynskiMA, StommelM. Nutrition education aimed at
toddlers:an intervention study.Pediatr Nurs 2005;31 (364):
367–72.
6 Birch LL, Doub AE. Learning to eat: birth to age 2 y. Am J Clin
Nutr 2014; 99: 723S–8S.
Children intakes compared to national guidelines
© 2015 Dietitians Association of Australia 7
in this age group are atrisk of excessive zinc intakes.38
However, these findings need to be interpreted with caution
given thatadverse effects secondary to high dietary zinc
intakes have not been reported in Australia.Therefore our
study supports Rangan and Samman’s conclusions that the
currentUL for the two- to three-years age group may be
underestimated and should be reviewed.38
Further analyses were undertaken to assess whether the
eating patterns ofchildren who met the NRVs for vitamin
A, thiamin,folate,calcium,iron and zinc were similar or
differentfrom the eating pattern suggested by the AGHE.
The majority of children in this study met the NRV targets
by followinga patternthat deviatedfrom the age-
appropriaterecommendations.This demonstratedthat
young children could meet the NRVs for selected nutrients
by consuming a significantly greater number of daily serv-
ingsof fruit (excluding juice)and dairy,in combination
with significantly lowermean daily servingsof breads/
cereals,vegetables and meat/alternatives compared to the
AGHE.Implications ofthese findings indicate that model-
ling of food group patterns to inform future refinements of
the AGHE could considerthis approach.Potentially this
would lead to incorporation of even greater diversity in the
distribution of food group servings, within optimal nutrient
intake ranges.
Findings from the presentstudy are similar to those of
nationally representative studies ofAmerican and Belgian
children where a large proportion did notmeetnational
recommendations for food group servings.39,40Sixty percent
and 93% ofAmerican children aged 1–18 years did not
consume the recommended number of servings of fruit and
vegetables,respectively.39 The majority (>50%) ofyounger
Belgian children aged three to seven years did not meet the
recommended number of servings of fruits,vegetables and
dairy products.40
The current study has a few limitations and, in particular,
the small sample size. Hence, results from this study may not
be representative ofother populations and ethnicities and
should be interpreted with caution. The study, although not
population-based,is the firstAustralian study to examine
associations between dietary patterns of children aged two to
three years compared to the revised 2013 AGHE.9 While the
FFQ data were proxy-reported by mothers with a possibility
of reporting bias as parents were unable to observe child
intake at preschoolor day care,the ACAES has been vali-
dated for total energy intake18 in preschool age children and
micronutrient intakes in children above five years.20,21While
FFQs are able to capture usualintake over a longer time
frame,25 and reliable for estimating micronutrient intakes in
infants and preschool children,41 it is acknowledged that the
ACAES has notbeen validated atthe food group level.In
addition, it must be acknowledged that for younger children
the six months reporting period of the FFQ may not accu-
rately reflecttheirusualintake overthattime.A further
limitation is that not all EARs and AIs were considered in the
subsample analysis and hence results should be interpreted
with caution.
In conclusion, the dietary patterns of Australian children
aged two to three in the current study do not align with the
recommended daily servings in the AGHE.Children who
achieved the NRVs for nutrients importantfor health and
development consumed more fruit, dairy and discretionary
servings than current recommendations.Further studies in
larger nationally representative population samples should
be undertaken to evaluate whetherthe currentfindings
apply. Findings from larger cohorts may help to inform the
future modelling of food patterns to incorporate even greater
diversity in the distribution offood group servings while
optimising nutrient intakes.
Funding source
The WATCH study received funding from the University of
Newcastle, the Newcastle Permanent Charitable Foundation
and the John Hunter HospitalCharitable Trust.The study
sponsors were not involved in research design, implementa-
tion or publication.
Conflict of interest
The authors declare that they have no competing interests.
Authorship
LKC, LMW,AJH, MLB, TLB and CEC contributed to the
methodologicaldesign ofthe study;LKC performed data
analysisand prepared the manuscript.LKC, LMW, TLB,
AJH, MLB,RS and CEC contributed to the revision ofthe
manuscriptand tables.AJH, CEC and RS established the
originalWATCH cohortand MLB contributed to the data
collection. This study was undertaken as a part requirement
for the degreeof Bachelorof Nutrition and Dietetics
(Honours) at the University of Newcastle (LKC),Australia.
All authors contributed to reviewing, editing and approving
the final version of the manuscript.
References
1 Lynch J,Smith GD.A life course approach to chronic disease
epidemiology. Annu Rev Public Health 2005; 26: 1–35.
2 Kaikkonen JE, Mikkila V, Magnussen CG, Juonala M, Viikari JS,
Raitakari OT. Does childhood nutrition influence adult cardio-
vascular disease risk?—insights from the Young Finns Study.
Ann Med 2013; 45: 120–28.
3 Jaaskelainen P,Magnussen CG,Pahkala K et al.Childhood
nutrition in predicting metabolic syndrome in adults:the car-
diovascular risk in Young Finns Study. Diabetes Care 2012; 35:
1937–43.
4 Togo P, Osler M, Sorensen T, Heitmann B. Food intake patterns
and body mass index iobservationalstudies.Int J Obes Relat
Metab Disord 2001; 25: 1741–51.
5 HorodynskiMA, StommelM. Nutrition education aimed at
toddlers:an intervention study.Pediatr Nurs 2005;31 (364):
367–72.
6 Birch LL, Doub AE. Learning to eat: birth to age 2 y. Am J Clin
Nutr 2014; 99: 723S–8S.
Children intakes compared to national guidelines
© 2015 Dietitians Association of Australia 7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7 Queensland Health. A Healthy Start in Life:A Nutrition Manual
for Health Professionals. Brisbane: Queensland Health, 2008.
8 Queensland Public Health Forum.EatWellQueensland 2002–
2012:Smart Eating for a Healthier State.Brisbane:Queensland
Public Health Forum, 2002.
9 NationalHealth and MedicalResearch Council.Eat for Health
Australian Dietary GuidelinesSummary.Canberra:Common-
wealth of Australia, 2013. (Available from: http://
www.eatforhealth.gov.au/sites/default/files/files/the_guidelines/
n55a_australian_dietary_guidelines_summary_131014.pdf,
accessed 2 June 2015).
10 Cashel K, Jeffreson S. The Core Food Groups: The Scientific Basis
for DevelopingNutrition Education Tools.Canberra:National
Health and Medical Research Council, 1994.
11 NationalHealth and MedicalResearch Council.A Modelling
System to Inform the Revision ofthe Australian Guide to Healthy
Eating. Canberra: Commonwealth of Australia, 2011. (Available
from: https://www.eatforhealth.gov.au/sites/default/files/files/
public_consultation/n55a_dietary_guidelines_food_modelling
_111216.pdf, accessed 20 January 2015).
12 National Health and Medical Research Council. Nutrient Refer-
ence Values for Australia and New Zealand Including Recommended
Dietary Intakes.Canberra:NHMRC;, 2006.(Available from:
https://www.nrv.gov.au/nutrients-energy-calculation/nutrients
-energy-calc-result-1421754458, accessed 20 January 2015).
13 Kellett E, Smith A, Schmerlaib Y. The Australian Guide to Healthy
Eating—Background Information for Consumers.Canberra:Aus-
tralian GovernmentDepartmentof Health and Ageing,1998.
(Availablefrom: http://www.fairfieldcity.nsw.gov.au/upload/
pkmhl46337/AustGuidetoHealtyEating.pdf,accessed 20
January 2015).
14 Maclennan W,PodgerA. NationalNutrition Survey Nutrient
Intakesand PhysicalMeasurement1995.Canberra:Australian
Bureau of Statistics, 1998. (Available from: http://www.abs.gov
.au/ausstats/abs@.nsf/Lookup/95E87FE64B144FA3CA2568A9
001393C0, accessed 10 November 2014).
15 Australian Government Department of Health and Ageing. 2007
Australian NationalChildren’sNutrition and PhysicalActivity
Survey Main Findings.Canberra:Commonwealth ofAustralia,
2008. (Available from: http://www.health.gov.au/internet/main/
publishing.nsf/Content/8F4516D5FAC0700ACA257BF0001E0
109/$File/childrens-nut-phys-survey.pdf,accessed 20 January
2015).
16 Webb K, Rutishauser I, Knezevic N. Foods, nutrients and por-
tions consumed by a sample of Australian children aged 16–24
months. Nutr Diet 2008; 65: 56–65.
17 AIHW. 2010 Australian National Infant Feeding Survey: Indicator
Results.Canberra:AIHW, 2011.(Available from:http://www
.aihw.gov.au/publication-detail/?id=10737420927,accessed 10
November 2014).
18 Hure AJ, Collins CE, Giles WB, Wright IM, Smith R. Protocol for
the Women and TheirChildren’s Health (WATCH)study:a
cohort of pregnancy and beyond. J Epidemiol 2012; 22: 267–75.
19 Hure AJ, Collins C, Giles WB, Paul J, Smith R. Greater maternal
weightgain during pregnancy predicts a large butlean fetal
phenotype:a prospective cohortstudy.Matern Child Health J
2012; 17: 1374–84.
20 Collins CE,Burrows TL,Truby H et al.Comparison of energy
intake in toddlers assessed by food frequency questionnaire and
total energy expenditure measured by the doubly labeled water
method. J Acad Nutr Diet 2013; 113: 459–63.
21 Watson JF,CollinsCE, SibbrittDW, Dibley MJ,Garg ML.
Reproducibility and comparative validity ofa food frequency
questionnaire for children and adolescents. Int J Behav Nutr Phy
Act 2009; 6: 62. doi: 10.1186/1479-5868-6-62.
22 Burrows T,Berthon B,Garg ML,Collins CE.A comparative
validation ofa child food frequency questionnaire using red
blood cellmembrane fatty acids.Eur J Clin Nutr 2012;66:
825–29.
23 Burrows T, Truby H, Morgan P, Callister R, Davies P, Collins C.
A comparison and validation of child versus parent reporting of
children’s energy intake using food frequency questionnaires
versus food records: who’s an accurate reporter? Clin Nutr 2013
32: 613–18.
24 BurrowsTL, Warren JM,ColyvasK, Garg ML,CollinsCE.
Validation of parental report of overweight children’s fruit and
vegetable intake using plasma carotenoids.Obesity 2009;17:
162–68.
25 WillettW. ed.NutritionalEpidemiology,2nd edn.New York:
Oxford University Press, 1998.
26 Burrows T, Warren JM, Baur LA, Collins CE. Impact of a child
obesity intervention on dietary intake and behaviors. Int J Obes
(Lond) 2008; 32: 1481–88.
27 Burrows T,Collins C,Warren JM.Long term changes in food
consumption trendsin overweightchildren enrolled in the
HIKCUPS intervention.J Pediatr GastroenterolNutr 2011;53:
543–47.
28 Duncanson K,Burrows T,Collins C.Effect ofa low-intensity
parent-focused nutrition intervention on dietary intake of 2- to
5-year olds. J Pediatr Gastroenterol Nutr 2013; 57: 728–34.
29 Cole T,Pan H.LMS growth computer program.2.12 ed.Cam-
bridge: Medical Research Council, 2002.
30 Nicklas TA.Calcium intake trends and health consequences
from childhood through adulthood.J Am CollNutr 2003;22:
340–56.
31 Maggini S, Wenzlaff S, Hornig D. Essential role of vitamin C and
Zinc in child immunity and health.J Int Med Res 2010;38:
386–414.
32 National Health and Medical Research Council. Dietary Guide-
lines for Children and Adolescents in Australia Incorporating the
InfantFeedingGuidelinesfor Healthworkers.Canberra:Com-
monwealth ofAustralia,2003.(Available from:http://www
.nhmrc.gov.au/_files_nhmrc/publications/attachments/n34.pdf,
accessed 20 January 2015).
33 Montgomery C, Reilly JJ, Jackson DM et al. Validation of energy
intake by 24-hour multiple pass recall:comparison with total
energy expenditure in children aged 5–7 years. Br J Nutr 2005;
93: 671–76.
34 Reilly JJ, Montgomery C, Jackson D, MacRitchie J, Armstrong J.
Energy intake by multiple pass 24 h recalland totalenergy
expenditure:a comparison in a representative sample of3–4-
year-olds. Br J Nutr 2001; 86: 601–5.
35 Rangan AM,RandallD, Hector DJ,Gill TP, Webb KL.Con-
sumption of ‘extra’foods by Australian children: types, quanti-
ties and contribution to energy and nutrient intakes. Eur J Clin
Nutr 2008; 62: 356–64.
36 Webb KL,Lahti-KoskiM, Rutishauser I et al.Consumption of
‘extra’ foods (energy-dense, nutrient poor) among children age
16–24 months from western Sydney,Australia.Public Health
Nutr 2006; 9: 1035–44.
37 Zhou SJ, Gibson RA, Gibson RS, Makrides M. Nutrient intakes
and status ofpreschoolchildren in Adelaide,South Australia.
Med J Aust 2012; 196: 696–700.
38 Rangan AM,Samman S.Zinc intake and its dietary sources:
results of the 2007 Australian National Children’s Nutrition and
Physical Activity Survey. Nutrients 2012; 4: 611–24.
L.K. Chai et al.
© 2015 Dietitians Association of Australia8
for Health Professionals. Brisbane: Queensland Health, 2008.
8 Queensland Public Health Forum.EatWellQueensland 2002–
2012:Smart Eating for a Healthier State.Brisbane:Queensland
Public Health Forum, 2002.
9 NationalHealth and MedicalResearch Council.Eat for Health
Australian Dietary GuidelinesSummary.Canberra:Common-
wealth of Australia, 2013. (Available from: http://
www.eatforhealth.gov.au/sites/default/files/files/the_guidelines/
n55a_australian_dietary_guidelines_summary_131014.pdf,
accessed 2 June 2015).
10 Cashel K, Jeffreson S. The Core Food Groups: The Scientific Basis
for DevelopingNutrition Education Tools.Canberra:National
Health and Medical Research Council, 1994.
11 NationalHealth and MedicalResearch Council.A Modelling
System to Inform the Revision ofthe Australian Guide to Healthy
Eating. Canberra: Commonwealth of Australia, 2011. (Available
from: https://www.eatforhealth.gov.au/sites/default/files/files/
public_consultation/n55a_dietary_guidelines_food_modelling
_111216.pdf, accessed 20 January 2015).
12 National Health and Medical Research Council. Nutrient Refer-
ence Values for Australia and New Zealand Including Recommended
Dietary Intakes.Canberra:NHMRC;, 2006.(Available from:
https://www.nrv.gov.au/nutrients-energy-calculation/nutrients
-energy-calc-result-1421754458, accessed 20 January 2015).
13 Kellett E, Smith A, Schmerlaib Y. The Australian Guide to Healthy
Eating—Background Information for Consumers.Canberra:Aus-
tralian GovernmentDepartmentof Health and Ageing,1998.
(Availablefrom: http://www.fairfieldcity.nsw.gov.au/upload/
pkmhl46337/AustGuidetoHealtyEating.pdf,accessed 20
January 2015).
14 Maclennan W,PodgerA. NationalNutrition Survey Nutrient
Intakesand PhysicalMeasurement1995.Canberra:Australian
Bureau of Statistics, 1998. (Available from: http://www.abs.gov
.au/ausstats/abs@.nsf/Lookup/95E87FE64B144FA3CA2568A9
001393C0, accessed 10 November 2014).
15 Australian Government Department of Health and Ageing. 2007
Australian NationalChildren’sNutrition and PhysicalActivity
Survey Main Findings.Canberra:Commonwealth ofAustralia,
2008. (Available from: http://www.health.gov.au/internet/main/
publishing.nsf/Content/8F4516D5FAC0700ACA257BF0001E0
109/$File/childrens-nut-phys-survey.pdf,accessed 20 January
2015).
16 Webb K, Rutishauser I, Knezevic N. Foods, nutrients and por-
tions consumed by a sample of Australian children aged 16–24
months. Nutr Diet 2008; 65: 56–65.
17 AIHW. 2010 Australian National Infant Feeding Survey: Indicator
Results.Canberra:AIHW, 2011.(Available from:http://www
.aihw.gov.au/publication-detail/?id=10737420927,accessed 10
November 2014).
18 Hure AJ, Collins CE, Giles WB, Wright IM, Smith R. Protocol for
the Women and TheirChildren’s Health (WATCH)study:a
cohort of pregnancy and beyond. J Epidemiol 2012; 22: 267–75.
19 Hure AJ, Collins C, Giles WB, Paul J, Smith R. Greater maternal
weightgain during pregnancy predicts a large butlean fetal
phenotype:a prospective cohortstudy.Matern Child Health J
2012; 17: 1374–84.
20 Collins CE,Burrows TL,Truby H et al.Comparison of energy
intake in toddlers assessed by food frequency questionnaire and
total energy expenditure measured by the doubly labeled water
method. J Acad Nutr Diet 2013; 113: 459–63.
21 Watson JF,CollinsCE, SibbrittDW, Dibley MJ,Garg ML.
Reproducibility and comparative validity ofa food frequency
questionnaire for children and adolescents. Int J Behav Nutr Phy
Act 2009; 6: 62. doi: 10.1186/1479-5868-6-62.
22 Burrows T,Berthon B,Garg ML,Collins CE.A comparative
validation ofa child food frequency questionnaire using red
blood cellmembrane fatty acids.Eur J Clin Nutr 2012;66:
825–29.
23 Burrows T, Truby H, Morgan P, Callister R, Davies P, Collins C.
A comparison and validation of child versus parent reporting of
children’s energy intake using food frequency questionnaires
versus food records: who’s an accurate reporter? Clin Nutr 2013
32: 613–18.
24 BurrowsTL, Warren JM,ColyvasK, Garg ML,CollinsCE.
Validation of parental report of overweight children’s fruit and
vegetable intake using plasma carotenoids.Obesity 2009;17:
162–68.
25 WillettW. ed.NutritionalEpidemiology,2nd edn.New York:
Oxford University Press, 1998.
26 Burrows T, Warren JM, Baur LA, Collins CE. Impact of a child
obesity intervention on dietary intake and behaviors. Int J Obes
(Lond) 2008; 32: 1481–88.
27 Burrows T,Collins C,Warren JM.Long term changes in food
consumption trendsin overweightchildren enrolled in the
HIKCUPS intervention.J Pediatr GastroenterolNutr 2011;53:
543–47.
28 Duncanson K,Burrows T,Collins C.Effect ofa low-intensity
parent-focused nutrition intervention on dietary intake of 2- to
5-year olds. J Pediatr Gastroenterol Nutr 2013; 57: 728–34.
29 Cole T,Pan H.LMS growth computer program.2.12 ed.Cam-
bridge: Medical Research Council, 2002.
30 Nicklas TA.Calcium intake trends and health consequences
from childhood through adulthood.J Am CollNutr 2003;22:
340–56.
31 Maggini S, Wenzlaff S, Hornig D. Essential role of vitamin C and
Zinc in child immunity and health.J Int Med Res 2010;38:
386–414.
32 National Health and Medical Research Council. Dietary Guide-
lines for Children and Adolescents in Australia Incorporating the
InfantFeedingGuidelinesfor Healthworkers.Canberra:Com-
monwealth ofAustralia,2003.(Available from:http://www
.nhmrc.gov.au/_files_nhmrc/publications/attachments/n34.pdf,
accessed 20 January 2015).
33 Montgomery C, Reilly JJ, Jackson DM et al. Validation of energy
intake by 24-hour multiple pass recall:comparison with total
energy expenditure in children aged 5–7 years. Br J Nutr 2005;
93: 671–76.
34 Reilly JJ, Montgomery C, Jackson D, MacRitchie J, Armstrong J.
Energy intake by multiple pass 24 h recalland totalenergy
expenditure:a comparison in a representative sample of3–4-
year-olds. Br J Nutr 2001; 86: 601–5.
35 Rangan AM,RandallD, Hector DJ,Gill TP, Webb KL.Con-
sumption of ‘extra’foods by Australian children: types, quanti-
ties and contribution to energy and nutrient intakes. Eur J Clin
Nutr 2008; 62: 356–64.
36 Webb KL,Lahti-KoskiM, Rutishauser I et al.Consumption of
‘extra’ foods (energy-dense, nutrient poor) among children age
16–24 months from western Sydney,Australia.Public Health
Nutr 2006; 9: 1035–44.
37 Zhou SJ, Gibson RA, Gibson RS, Makrides M. Nutrient intakes
and status ofpreschoolchildren in Adelaide,South Australia.
Med J Aust 2012; 196: 696–700.
38 Rangan AM,Samman S.Zinc intake and its dietary sources:
results of the 2007 Australian National Children’s Nutrition and
Physical Activity Survey. Nutrients 2012; 4: 611–24.
L.K. Chai et al.
© 2015 Dietitians Association of Australia8
39 Kim SA, Moore LV, Galuska D et al. Vital signs: fruit and veg-
etableintakeamongchildren—United States,2003–2010.
MMWR MorbMortalWkly Rep 2014;63: 671–76.(Avail-
able from: http://www.cdc.gov/mmwr/pdf/wk/mm6331.pdf,
accessed 20 January 2015).
40 HuybrechtsI, MatthysC, Vereecken C et al.Food intakes
by preschoolchildren in Flanderscompared with dietary
guidelines.Int J Environ ResPublicHealth2008;5: 243–
57.
41 Roman-Vinas B,Ortiz-AndrellucchiA, Mendez M et al.Is the
food frequency questionnaire suitable to assess micronutrient
intake adequacy for infants,children and adolescents? Matern
Child Nutr 2010; 6: 112–21.
Children intakes compared to national guidelines
© 2015 Dietitians Association of Australia 9
etableintakeamongchildren—United States,2003–2010.
MMWR MorbMortalWkly Rep 2014;63: 671–76.(Avail-
able from: http://www.cdc.gov/mmwr/pdf/wk/mm6331.pdf,
accessed 20 January 2015).
40 HuybrechtsI, MatthysC, Vereecken C et al.Food intakes
by preschoolchildren in Flanderscompared with dietary
guidelines.Int J Environ ResPublicHealth2008;5: 243–
57.
41 Roman-Vinas B,Ortiz-AndrellucchiA, Mendez M et al.Is the
food frequency questionnaire suitable to assess micronutrient
intake adequacy for infants,children and adolescents? Matern
Child Nutr 2010; 6: 112–21.
Children intakes compared to national guidelines
© 2015 Dietitians Association of Australia 9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.