University of Manchester Dentistry Dissertation: Myofascial Pain Study
VerifiedAdded on 2020/01/07
|16
|5260
|18
Thesis and Dissertation
AI Summary
This dissertation explores the effectiveness of Botulinum Toxin A (BTX-A) compared to occlusal appliance therapy (splint therapy) in relieving myofascial pain. It begins with a literature review encompassing the background of myofascial pain syndrome (MPS), its causes, symptoms, and prevalence, as well as the current treatment options, including BTX-A and splint therapy. The dissertation outlines a PICO framework, including study rationale, population (adults with myofascial pain), intervention (BTX-A), control (splint therapy), and outcome measures (pain intensity via VAS). A detailed search strategy is presented, including databases (Psych-INFO, MEDLINE, CINAHL), key search terms, Boolean operators, and inclusion/exclusion criteria. The study also includes a critical appraisal of key research papers related to the topic. Overall, the dissertation aims to determine the effectiveness of BTX-A compared to conventional splint therapy in treating myofascial pain through a randomized controlled clinical trial.
DISSERTATION ON DENTISTRY
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

TABLE OF CONTENTS
LITERATURE REVIEW.......................................................................................................................4
BACKGROUND..................................................................................................................................4
SEARCH STRATEGY....................................................................................................................5
Literature search strategy.............................................................................................................5
Databases.....................................................................................................................................5
Key search terms..........................................................................................................................6
Boolean operators........................................................................................................................6
Inclusion and exclusion criteria...................................................................................................6
CRITICAL APPRAISAL OF KEY RESEARCH PAPERS............................................................................7
Effectiveness of BTX- A in relieving myofascial pain...............................................................9
REFERENCES..............................................................................................................................10
LITERATURE REVIEW.......................................................................................................................4
BACKGROUND..................................................................................................................................4
SEARCH STRATEGY....................................................................................................................5
Literature search strategy.............................................................................................................5
Databases.....................................................................................................................................5
Key search terms..........................................................................................................................6
Boolean operators........................................................................................................................6
Inclusion and exclusion criteria...................................................................................................6
CRITICAL APPRAISAL OF KEY RESEARCH PAPERS............................................................................7
Effectiveness of BTX- A in relieving myofascial pain...............................................................9
REFERENCES..............................................................................................................................10
PICO FRAMEWORK
Research title study: Efficacy of BTX-A compared to occlusal appliance therapy in relieving
myofascial pain.
Study rationale: insert here.
Population: Adult patients aged between 18-60 years old, presenting with myofascial pain in a
secondary care setting.
Intervention: Treatment of myofascial pain using with BTX-A.
Control: Treatment of myofascial pain using conventional stabilization splint therapy
Outcome measure (primary):
The intensity of the myofascial pain will be assessed using a visual analogue scale (VAS)
at baseline and at the follow up appointments at 1 month and 3 months.
Outcome measure (secondary):
The intensity of Pain-free during maximal mouth opening.
The clinical findings will be monitored at baseline, 1 months and 3 months.
Aim and Objectives
Aim: To determine the effectiveness of BTX-A as compared to conventional splint therapy in
treating myofascial pain.
Objectives:
To undertake a randomised controlled clinical trial in a secondary care setting, to
compare the effectiveness of BTX- and conventional splint therapy in treating myofascial
pain.
To measure and analyse patients’ reported levels of pain before, during and after
treatment with BTX-A or with conventional splint therapy.
Research title study: Efficacy of BTX-A compared to occlusal appliance therapy in relieving
myofascial pain.
Study rationale: insert here.
Population: Adult patients aged between 18-60 years old, presenting with myofascial pain in a
secondary care setting.
Intervention: Treatment of myofascial pain using with BTX-A.
Control: Treatment of myofascial pain using conventional stabilization splint therapy
Outcome measure (primary):
The intensity of the myofascial pain will be assessed using a visual analogue scale (VAS)
at baseline and at the follow up appointments at 1 month and 3 months.
Outcome measure (secondary):
The intensity of Pain-free during maximal mouth opening.
The clinical findings will be monitored at baseline, 1 months and 3 months.
Aim and Objectives
Aim: To determine the effectiveness of BTX-A as compared to conventional splint therapy in
treating myofascial pain.
Objectives:
To undertake a randomised controlled clinical trial in a secondary care setting, to
compare the effectiveness of BTX- and conventional splint therapy in treating myofascial
pain.
To measure and analyse patients’ reported levels of pain before, during and after
treatment with BTX-A or with conventional splint therapy.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

LITERATURE REVIEW
INTRODUCTION
Myofascial pain syndrome, also called myofascial pain and dysfunction syndrome, occurs
in patients with a normal temporomandibular joint. The temporal mandibular joint is the synovial
joint that connects the jaw to the skull and these two joints are located just in front of each ear.
Myofascial pain syndrome is caused by tension, fatigue or spasm in the masticatory muscles
(Kim, Yun and Kim, 2016). It is also believed that MPD syndrome is a physical manifestation of
psychological stress. Its symptoms include bruxism, pain and tenderness in and around the
masticatory apparatus. Health care practitioners diagnose it based on historical records and
physical examination. The syndrome is one of the most common disorders that can affect the
temporomandibular region. It is most common among women and it also has a bimodal age
distribution in the early 20s and during menopause (Fortuna, Vaz and et.al., 2011).
It has been identified that up to 30% adults experience Myofascial pain at some point in
their lives; the condition is not usually serious and can be managed with the help of suitable care
and exercises (Sahai, Dowson, Khan and et.al., 2010). However, because of symptoms, patients
can lead to lower quality of life. At the same time, specialist treatment is required if the condition
is severe. Earaches and toothaches are directly associated with the masseter which is a trigger
point that radiates pain directly into the tooth. Thus, Myofascial pain syndrome is a failure of jaw
joint function that is mostly painful. This also limits the movement of the jaw and specific
problem arises during sleeping, eating and talking. Functional disturbances are common in
Myofascial pain (Bohluli, Motamedi and et.al., 2011).
BACKGROUND
Myofascial pain syndrome (MPS) is a chronic pain disorder. In this, a person feels the
pressure in sensitive points in muscles causes pain in seemingly unrelated parts of body. It can be
considered as referred pain (Myofascial Pain Syndrome (MPS), 2016). This occurs after a muscle
has been contracted repetitively. In normal context, everyone has experienced muscles tension
pain. In human body, a tough connective tissue layer i.e. fascia covers muscles and spread
uninterrupted through body. When this area injured, this tissues become tight and contract
INTRODUCTION
Myofascial pain syndrome, also called myofascial pain and dysfunction syndrome, occurs
in patients with a normal temporomandibular joint. The temporal mandibular joint is the synovial
joint that connects the jaw to the skull and these two joints are located just in front of each ear.
Myofascial pain syndrome is caused by tension, fatigue or spasm in the masticatory muscles
(Kim, Yun and Kim, 2016). It is also believed that MPD syndrome is a physical manifestation of
psychological stress. Its symptoms include bruxism, pain and tenderness in and around the
masticatory apparatus. Health care practitioners diagnose it based on historical records and
physical examination. The syndrome is one of the most common disorders that can affect the
temporomandibular region. It is most common among women and it also has a bimodal age
distribution in the early 20s and during menopause (Fortuna, Vaz and et.al., 2011).
It has been identified that up to 30% adults experience Myofascial pain at some point in
their lives; the condition is not usually serious and can be managed with the help of suitable care
and exercises (Sahai, Dowson, Khan and et.al., 2010). However, because of symptoms, patients
can lead to lower quality of life. At the same time, specialist treatment is required if the condition
is severe. Earaches and toothaches are directly associated with the masseter which is a trigger
point that radiates pain directly into the tooth. Thus, Myofascial pain syndrome is a failure of jaw
joint function that is mostly painful. This also limits the movement of the jaw and specific
problem arises during sleeping, eating and talking. Functional disturbances are common in
Myofascial pain (Bohluli, Motamedi and et.al., 2011).
BACKGROUND
Myofascial pain syndrome (MPS) is a chronic pain disorder. In this, a person feels the
pressure in sensitive points in muscles causes pain in seemingly unrelated parts of body. It can be
considered as referred pain (Myofascial Pain Syndrome (MPS), 2016). This occurs after a muscle
has been contracted repetitively. In normal context, everyone has experienced muscles tension
pain. In human body, a tough connective tissue layer i.e. fascia covers muscles and spread
uninterrupted through body. When this area injured, this tissues become tight and contract
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
putting painful pressure on nerves, organs, muscles or bones. That area can be referred as a
trigger point and there, person feels like a knot or band in the muscle. These points may not only
generate at the injured site but also in various other areas of the body. Generally, MPS develops
between ages 20 to 40 and is more common in women and those people who are having
sedentary lifestyles (Diseases and Conditions: Myofascial pain syndrome, 2016).
By considering its symptoms, the pain creates in muscles or fascia. At the time of
speaking, the following pain is steady, aching and deep. Along with this, another sings of MPS
are headaches, jaw pain, lower back pain, arm and leg pain, pelvic pain, depression, fatigue,
mood disturbances, anxiety etc. So, it is important to treat MPS pain and the available treatment
options are Botulinum Toxin A (BTX-A), splint therapy etc.BTX-A is a kind of protein that
produced by the bacterium Clostridium botulinum. It is a potent neurotoxin which eventually
inhibits muscle contractions. With the help of this, the issues related to BTX A can be treated.
On the other hand, in splint therapy, it allows the muscles and ligaments to relax. By this, ridding
the facial muscles of the tension and tightness can be minimized.
SEARCH STRATEGY
Literature search strategy
A literature search was conducted to identify literature relating to the treatment of
myofascial pain, specifically using splint therapies and BTX-A. Due to the relatively recent
introduction of BTX-A as a potential treatment for myofascial pain, the search was broaden to
consider wider uses for BTX-A and their relevance to this research question.
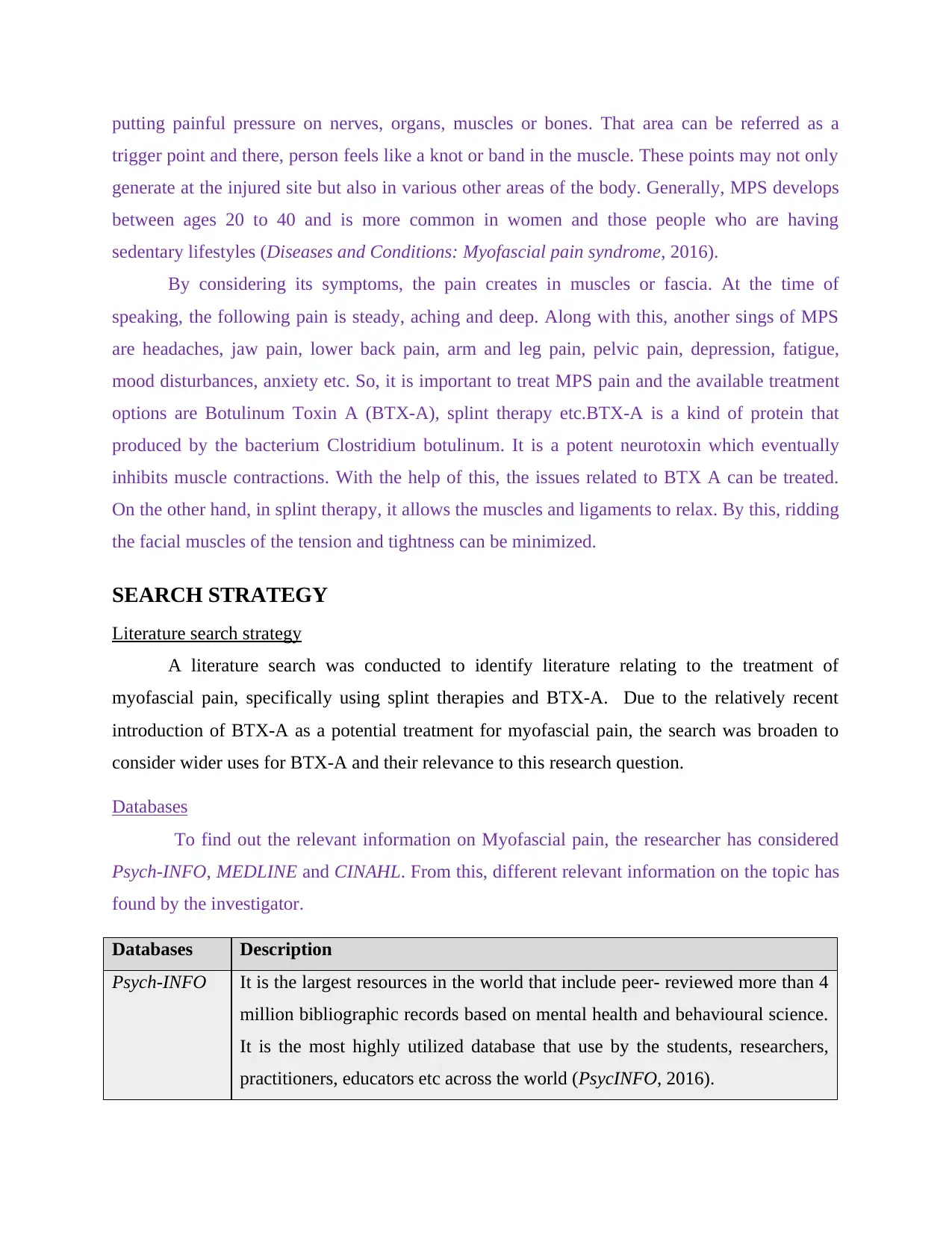
Databases
To find out the relevant information on Myofascial pain, the researcher has considered
Psych-INFO, MEDLINE and CINAHL. From this, different relevant information on the topic has
found by the investigator.
Databases Description
Psych-INFO It is the largest resources in the world that include peer- reviewed more than 4
million bibliographic records based on mental health and behavioural science.
It is the most highly utilized database that use by the students, researchers,
practitioners, educators etc across the world (PsycINFO, 2016).
trigger point and there, person feels like a knot or band in the muscle. These points may not only
generate at the injured site but also in various other areas of the body. Generally, MPS develops
between ages 20 to 40 and is more common in women and those people who are having
sedentary lifestyles (Diseases and Conditions: Myofascial pain syndrome, 2016).
By considering its symptoms, the pain creates in muscles or fascia. At the time of
speaking, the following pain is steady, aching and deep. Along with this, another sings of MPS
are headaches, jaw pain, lower back pain, arm and leg pain, pelvic pain, depression, fatigue,
mood disturbances, anxiety etc. So, it is important to treat MPS pain and the available treatment
options are Botulinum Toxin A (BTX-A), splint therapy etc.BTX-A is a kind of protein that
produced by the bacterium Clostridium botulinum. It is a potent neurotoxin which eventually
inhibits muscle contractions. With the help of this, the issues related to BTX A can be treated.
On the other hand, in splint therapy, it allows the muscles and ligaments to relax. By this, ridding
the facial muscles of the tension and tightness can be minimized.
SEARCH STRATEGY
Literature search strategy
A literature search was conducted to identify literature relating to the treatment of
myofascial pain, specifically using splint therapies and BTX-A. Due to the relatively recent
introduction of BTX-A as a potential treatment for myofascial pain, the search was broaden to
consider wider uses for BTX-A and their relevance to this research question.
Databases
To find out the relevant information on Myofascial pain, the researcher has considered
Psych-INFO, MEDLINE and CINAHL. From this, different relevant information on the topic has
found by the investigator.
Databases Description
Psych-INFO It is the largest resources in the world that include peer- reviewed more than 4
million bibliographic records based on mental health and behavioural science.
It is the most highly utilized database that use by the students, researchers,
practitioners, educators etc across the world (PsycINFO, 2016).
MEDLINE It is a bibliographic database that comprises academic journals covering on a
wide range of topics such as nursing, health care, medicines and dentistry
(Medline, 2016).
CINAHL This is an index of journals relating to nursing, biomedicine, healthcare and
allied health (CINAHL Database, 2016).
To search the literature review on the similar topic, the researcher has been used perch
engine such as EBSCOhost. It is an electronic journal host and encloses journals of large number
of different publishers across the world. The following search engine allows the scholar to search
for articles from the vast collection of journals (Riesenberg, Leisch and Cunningham, 2010).
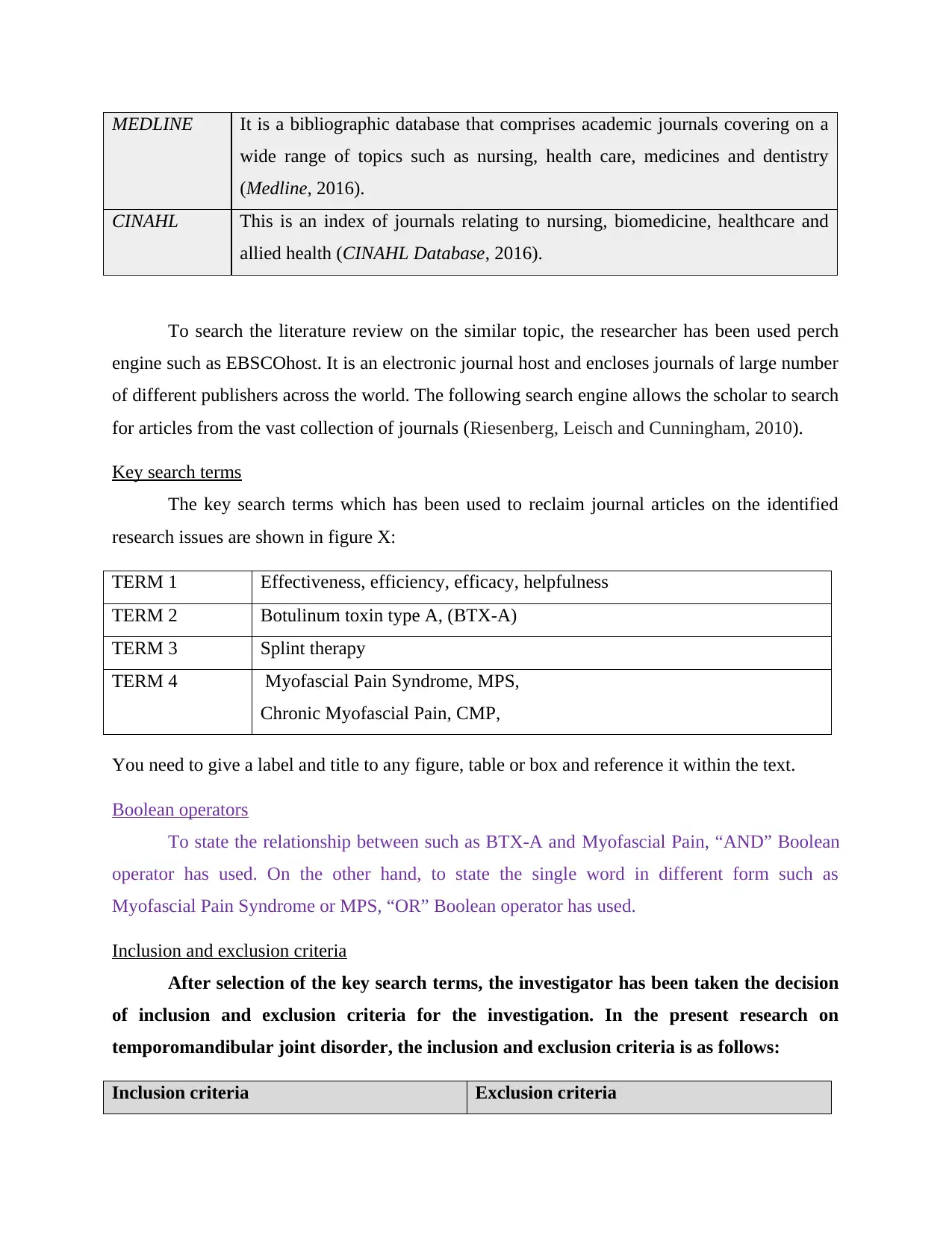
Key search terms
The key search terms which has been used to reclaim journal articles on the identified
research issues are shown in figure X:
TERM 1 Effectiveness, efficiency, efficacy, helpfulness
TERM 2 Botulinum toxin type A, (BTX-A)
TERM 3 Splint therapy
TERM 4 Myofascial Pain Syndrome, MPS,
Chronic Myofascial Pain, CMP,
You need to give a label and title to any figure, table or box and reference it within the text.
Boolean operators
To state the relationship between such as BTX-A and Myofascial Pain, “AND” Boolean
operator has used. On the other hand, to state the single word in different form such as
Myofascial Pain Syndrome or MPS, “OR” Boolean operator has used.
Inclusion and exclusion criteria
After selection of the key search terms, the investigator has been taken the decision
of inclusion and exclusion criteria for the investigation. In the present research on
temporomandibular joint disorder, the inclusion and exclusion criteria is as follows:
Inclusion criteria Exclusion criteria
wide range of topics such as nursing, health care, medicines and dentistry
(Medline, 2016).
CINAHL This is an index of journals relating to nursing, biomedicine, healthcare and
allied health (CINAHL Database, 2016).
To search the literature review on the similar topic, the researcher has been used perch
engine such as EBSCOhost. It is an electronic journal host and encloses journals of large number
of different publishers across the world. The following search engine allows the scholar to search
for articles from the vast collection of journals (Riesenberg, Leisch and Cunningham, 2010).
Key search terms
The key search terms which has been used to reclaim journal articles on the identified
research issues are shown in figure X:
TERM 1 Effectiveness, efficiency, efficacy, helpfulness
TERM 2 Botulinum toxin type A, (BTX-A)
TERM 3 Splint therapy
TERM 4 Myofascial Pain Syndrome, MPS,
Chronic Myofascial Pain, CMP,
You need to give a label and title to any figure, table or box and reference it within the text.
Boolean operators
To state the relationship between such as BTX-A and Myofascial Pain, “AND” Boolean
operator has used. On the other hand, to state the single word in different form such as
Myofascial Pain Syndrome or MPS, “OR” Boolean operator has used.
Inclusion and exclusion criteria
After selection of the key search terms, the investigator has been taken the decision
of inclusion and exclusion criteria for the investigation. In the present research on
temporomandibular joint disorder, the inclusion and exclusion criteria is as follows:
Inclusion criteria Exclusion criteria
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
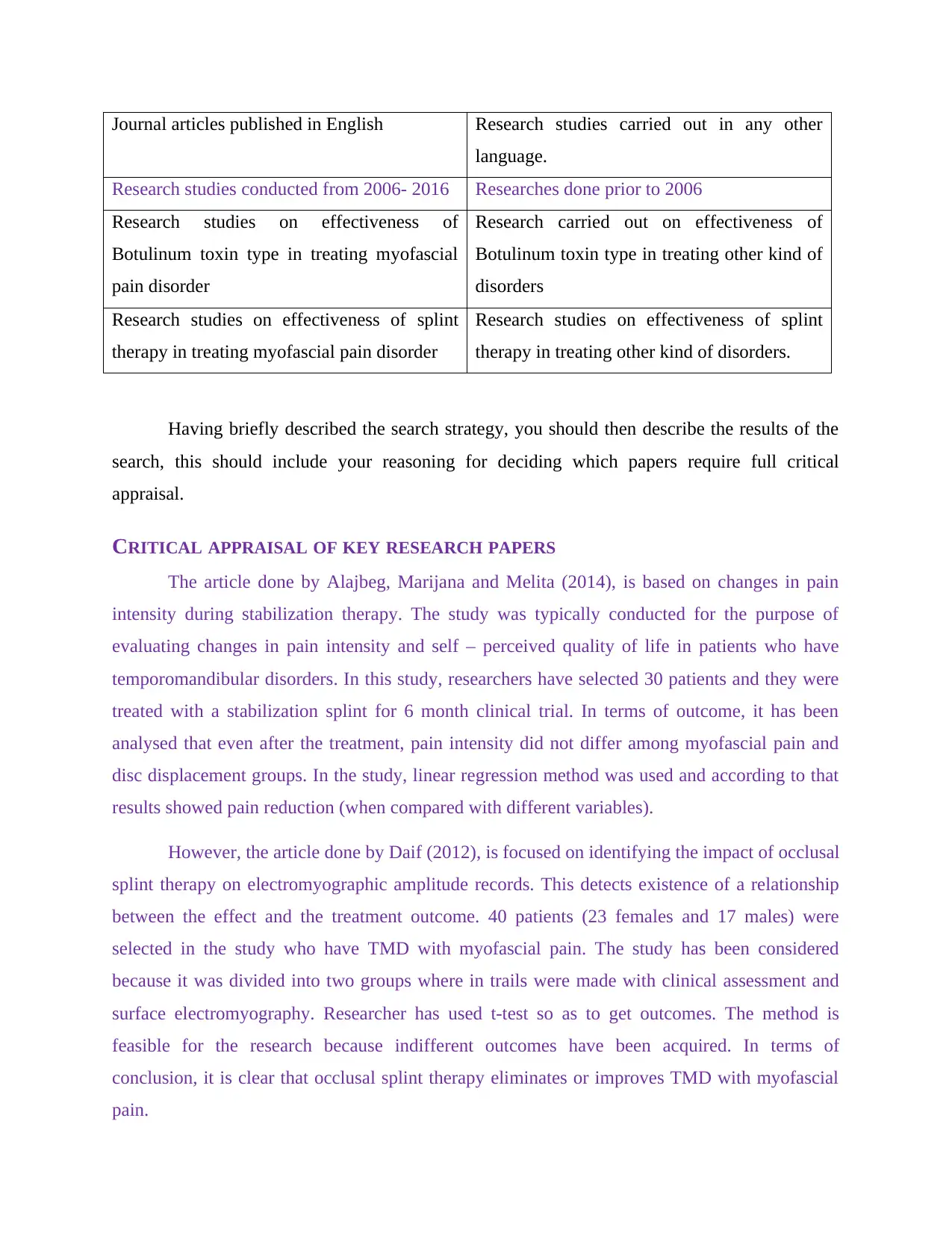
Journal articles published in English Research studies carried out in any other
language.
Research studies conducted from 2006- 2016 Researches done prior to 2006
Research studies on effectiveness of
Botulinum toxin type in treating myofascial
pain disorder
Research carried out on effectiveness of
Botulinum toxin type in treating other kind of
disorders
Research studies on effectiveness of splint
therapy in treating myofascial pain disorder
Research studies on effectiveness of splint
therapy in treating other kind of disorders.
Having briefly described the search strategy, you should then describe the results of the
search, this should include your reasoning for deciding which papers require full critical
appraisal.
CRITICAL APPRAISAL OF KEY RESEARCH PAPERS
The article done by Alajbeg, Marijana and Melita (2014), is based on changes in pain
intensity during stabilization therapy. The study was typically conducted for the purpose of
evaluating changes in pain intensity and self – perceived quality of life in patients who have
temporomandibular disorders. In this study, researchers have selected 30 patients and they were
treated with a stabilization splint for 6 month clinical trial. In terms of outcome, it has been
analysed that even after the treatment, pain intensity did not differ among myofascial pain and
disc displacement groups. In the study, linear regression method was used and according to that
results showed pain reduction (when compared with different variables).
However, the article done by Daif (2012), is focused on identifying the impact of occlusal
splint therapy on electromyographic amplitude records. This detects existence of a relationship
between the effect and the treatment outcome. 40 patients (23 females and 17 males) were
selected in the study who have TMD with myofascial pain. The study has been considered
because it was divided into two groups where in trails were made with clinical assessment and
surface electromyography. Researcher has used t-test so as to get outcomes. The method is
feasible for the research because indifferent outcomes have been acquired. In terms of
conclusion, it is clear that occlusal splint therapy eliminates or improves TMD with myofascial
pain.
language.
Research studies conducted from 2006- 2016 Researches done prior to 2006
Research studies on effectiveness of
Botulinum toxin type in treating myofascial
pain disorder
Research carried out on effectiveness of
Botulinum toxin type in treating other kind of
disorders
Research studies on effectiveness of splint
therapy in treating myofascial pain disorder
Research studies on effectiveness of splint
therapy in treating other kind of disorders.
Having briefly described the search strategy, you should then describe the results of the
search, this should include your reasoning for deciding which papers require full critical
appraisal.
CRITICAL APPRAISAL OF KEY RESEARCH PAPERS
The article done by Alajbeg, Marijana and Melita (2014), is based on changes in pain
intensity during stabilization therapy. The study was typically conducted for the purpose of
evaluating changes in pain intensity and self – perceived quality of life in patients who have
temporomandibular disorders. In this study, researchers have selected 30 patients and they were
treated with a stabilization splint for 6 month clinical trial. In terms of outcome, it has been
analysed that even after the treatment, pain intensity did not differ among myofascial pain and
disc displacement groups. In the study, linear regression method was used and according to that
results showed pain reduction (when compared with different variables).
However, the article done by Daif (2012), is focused on identifying the impact of occlusal
splint therapy on electromyographic amplitude records. This detects existence of a relationship
between the effect and the treatment outcome. 40 patients (23 females and 17 males) were
selected in the study who have TMD with myofascial pain. The study has been considered
because it was divided into two groups where in trails were made with clinical assessment and
surface electromyography. Researcher has used t-test so as to get outcomes. The method is
feasible for the research because indifferent outcomes have been acquired. In terms of
conclusion, it is clear that occlusal splint therapy eliminates or improves TMD with myofascial
pain.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Further, the article done by Turp, Komine and Hugger (2004), is being selected to
provide evidence of stabilization splints for the masticatory muscle pain. In the research, a
systematic search was conducted in different electronic database which depicts the feasibility of
the research methodologies. On the basis of current study, researchers said that most of the
patients with masticatory pain can be treated through stabilization splint.The research work
seems to be less important for the present study because it was conducted before 12 years and
due to changes in technologies, several new aspects have been brought in medical science.
Moreover, the research done by Al- Ani MZ, Gray and Glenny (2004), is also selected for
the present work as it is based on identifying the effectiveness of stabilization splint therapy in
reducing the symptoms in patients with dysfunction syndrome. Cochrane library and EMBASE
both the databases have been selected in the study for collecting information about the subject
matter. Randomised and quasi- randomised controlled trails were compared concurrently with
occlusal appliances. In terms of conclusion, author summed up that there is insufficient evidence
against the use of stabilization splint therapy for the treatment of temporomandibular pain
dysfunction syndrome.
Apart from these articles, study of Zaid Al-Ani, Gray and Davies (2005), has been
considered for the present research work because it is based on the effectiveness of stabilization
splint therapy in reducing the symptoms in patients who have myofascial pain. The theory has
also showed the difference between stabilization splint vs. non- occluding splints and as per the
results it has been identified that there is no statistically difference in both the methods. Various
measures were adopted in the study for the purpose of assessing the outcomes of treatment.
Further, standardization of methods were also used to measures the outcomes of the treatment of
myofascial pain.
The research work done by Santana-Moraa and Santana Penin (2009), stated the
difference in electromyographic activity that is recorded at the time of clenching with chronic
unilateral temporomandibular disorders as compared to control subjects. Integrated surface EMG
have been used over a 1 a contraction. In this, the anterior temporalis and masseter muscles were
evaluated bilaterally at the time when subjects performed maximum voluntary clenching.
Authors also defined that the unilateral reduction in temporalis can be regarded as a specific
protective functional adaptation of the neuromuscular system.
provide evidence of stabilization splints for the masticatory muscle pain. In the research, a
systematic search was conducted in different electronic database which depicts the feasibility of
the research methodologies. On the basis of current study, researchers said that most of the
patients with masticatory pain can be treated through stabilization splint.The research work
seems to be less important for the present study because it was conducted before 12 years and
due to changes in technologies, several new aspects have been brought in medical science.
Moreover, the research done by Al- Ani MZ, Gray and Glenny (2004), is also selected for
the present work as it is based on identifying the effectiveness of stabilization splint therapy in
reducing the symptoms in patients with dysfunction syndrome. Cochrane library and EMBASE
both the databases have been selected in the study for collecting information about the subject
matter. Randomised and quasi- randomised controlled trails were compared concurrently with
occlusal appliances. In terms of conclusion, author summed up that there is insufficient evidence
against the use of stabilization splint therapy for the treatment of temporomandibular pain
dysfunction syndrome.
Apart from these articles, study of Zaid Al-Ani, Gray and Davies (2005), has been
considered for the present research work because it is based on the effectiveness of stabilization
splint therapy in reducing the symptoms in patients who have myofascial pain. The theory has
also showed the difference between stabilization splint vs. non- occluding splints and as per the
results it has been identified that there is no statistically difference in both the methods. Various
measures were adopted in the study for the purpose of assessing the outcomes of treatment.
Further, standardization of methods were also used to measures the outcomes of the treatment of
myofascial pain.
The research work done by Santana-Moraa and Santana Penin (2009), stated the
difference in electromyographic activity that is recorded at the time of clenching with chronic
unilateral temporomandibular disorders as compared to control subjects. Integrated surface EMG
have been used over a 1 a contraction. In this, the anterior temporalis and masseter muscles were
evaluated bilaterally at the time when subjects performed maximum voluntary clenching.
Authors also defined that the unilateral reduction in temporalis can be regarded as a specific
protective functional adaptation of the neuromuscular system.
Additionally, the article of Katyayan, Shah and Patel (2013), is also considered which
was done for finding out the efficacy of appliance therapy on temporomandibular disorder
related facial pain and for such purpose a randomized controlled study is being selected. The
study has also assessed the efficacy of stabilization splint therapy; hence for that purpose sample
of 80 consecutive patients were diagnosed. Splint group and control group are the two major
groups that were selected at the initial stage of the study. t-test has been used in the study for the
purpose of finding out the level of significance.
Similarly, the study carried out by Glaros, Glass and Brockman (1997), is also utilized in
the study which tested the hypothesis that EMG activity is significantly greater for
temporomandibular disorder patients (who have myofascial pain)as compared to non-pain
control subjects. In this respect, 40 TMD patients were diagnosed and 54 non- pain control
subjects were examined. Results showed that TMD group has higher activity set for all the
examined participants.
Effectiveness of BTX- A in relieving myofascial pain
As per the study of Kerscher, Roll, Becker and Wigger-Alberti, 2012, “Botulinum toxin
type A (BTX-A) is a 150 kDa protein produced by the bacterium Clostridium botulinum”
(Kerscher, Roll, Becker and Wigger-Alberti, 2012). The following toxin is internalized into
presynapticcholinergic nerve terminals where it releases the neurotransmitter acetylcholine
which restraining the contraction of muscles. By considering the muscle relaxant properties,
BTX-A uses to treat variety of muscular conditions and it includes spasticity, cervical dystonia
and blepharospasm. In this context, Ernberg, Hedenberg-Magnusson, List, and Svensson, 2011
has stated that “the first effectiveness of BTX-A in treating temporomandibular joint disorder is
decompression of entrapped nerves in patient” (Ernberg, Hedenberg-Magnusson, List, and
Svensson, 2011).
With the help of this, it becomes easy to relaxation to muscles by deep massage. It also
helps in increasing the motion and stretching of muscles at the time of treating
temporomandibular joint disorder. In order to correct postural asymmetries and to stabilize the
musculature, BTX-A is design to strengthen and supporting co-contracting muscles. The
following treatment has effective in terms of breaking the cycle of pain, to attain neuromuscular
re-education and improve the working of joints masticatory muscles (Nigam and Nigam, 2010).
was done for finding out the efficacy of appliance therapy on temporomandibular disorder
related facial pain and for such purpose a randomized controlled study is being selected. The
study has also assessed the efficacy of stabilization splint therapy; hence for that purpose sample
of 80 consecutive patients were diagnosed. Splint group and control group are the two major
groups that were selected at the initial stage of the study. t-test has been used in the study for the
purpose of finding out the level of significance.
Similarly, the study carried out by Glaros, Glass and Brockman (1997), is also utilized in
the study which tested the hypothesis that EMG activity is significantly greater for
temporomandibular disorder patients (who have myofascial pain)as compared to non-pain
control subjects. In this respect, 40 TMD patients were diagnosed and 54 non- pain control
subjects were examined. Results showed that TMD group has higher activity set for all the
examined participants.
Effectiveness of BTX- A in relieving myofascial pain
As per the study of Kerscher, Roll, Becker and Wigger-Alberti, 2012, “Botulinum toxin
type A (BTX-A) is a 150 kDa protein produced by the bacterium Clostridium botulinum”
(Kerscher, Roll, Becker and Wigger-Alberti, 2012). The following toxin is internalized into
presynapticcholinergic nerve terminals where it releases the neurotransmitter acetylcholine
which restraining the contraction of muscles. By considering the muscle relaxant properties,
BTX-A uses to treat variety of muscular conditions and it includes spasticity, cervical dystonia
and blepharospasm. In this context, Ernberg, Hedenberg-Magnusson, List, and Svensson, 2011
has stated that “the first effectiveness of BTX-A in treating temporomandibular joint disorder is
decompression of entrapped nerves in patient” (Ernberg, Hedenberg-Magnusson, List, and
Svensson, 2011).
With the help of this, it becomes easy to relaxation to muscles by deep massage. It also
helps in increasing the motion and stretching of muscles at the time of treating
temporomandibular joint disorder. In order to correct postural asymmetries and to stabilize the
musculature, BTX-A is design to strengthen and supporting co-contracting muscles. The
following treatment has effective in terms of breaking the cycle of pain, to attain neuromuscular
re-education and improve the working of joints masticatory muscles (Nigam and Nigam, 2010).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
On the other hand, Wolf, Milton, Reiss and et.al., 2012 has asserted that “the most
important effectiveness of BTX-A at the time of treatment of temporomandibular joint disorder
is it increases the blood flow to the muscle and release of never fibers” (Wolf, Milton, Reiss and
et.al., 2012). The following toxin brings the reduction in muscle tone pain because of the
occurrence of myofascial pain syndrome. This enhances the blood circulation in the painful area
and releases nerve fibers in that area that is compressed by abnormally contracting muscle. It
shows some instant effect in terms of direct liberate of endogenous endorphins from the inserting
the needle of injection. BTX-A brings a modification in the sense of balance of peripheral and
central neurotransmitters (Kim, Yun and Kim, 2016).
From the investigation of Fortuna, Vaz and et.al., 2011, it has found that “BTX-A is
effective in reducing muscle spasticity over the large area as compare to cover by the injection”
(Fortuna, Vaz and et.al., 2011). The following observation can be explained by the facts that
ACh is released by both gamma and alpha motor neurons. These both have involved in the
muscle contractions in terms of either voluntary or involuntary basis. Gamma motor neurons
innervate the intrafusal fibers of the muscle spindles. BTX-A causes atrophy of the intrafusal
fibers and extrafusal fibers where alpha motor neurons are situated. The following toxin satisfies
the output from the muscle spindle to the central nervous system. In addition to this, Sahai,
Dowson, Khan and et.al., 2010 has explored from their research that “BTX-A reduces the spindle
afferent discharge in the human jaw muscle spindle” (Sahai, Dowson, Khan and et.al., 2010). It
has brought the reduction of overall muscles contraction at the time of movement of jaws. Along
with this, it has reduced the excess muscle contractions that are responsible for the pain.
Effectiveness of Conventional splint therapy in treating myofascial pain
As per the views of Turp, Komine and Hugger, (2004), Occlusal splint therapy has better
long term results in reducing the symptoms of MPDS. It terms of results, it leads to better patient
compliance with fewer side effects and it is also more cost effective than pharmacotherapy.
Thus, this is the reason it is highly recommended for the treatment of patients with MPDS.
Consequently, several therapies and some conservative surgeries are available for repositioning
of the mandible; however patients suffering with TMD dysfunction are suggested to go for
occlusal splint therapy. It is chosen in the orofacial region for various reasons. In this respect,
soft splints are recommended to patients with TMD and they can be made for maxillary arches
important effectiveness of BTX-A at the time of treatment of temporomandibular joint disorder
is it increases the blood flow to the muscle and release of never fibers” (Wolf, Milton, Reiss and
et.al., 2012). The following toxin brings the reduction in muscle tone pain because of the
occurrence of myofascial pain syndrome. This enhances the blood circulation in the painful area
and releases nerve fibers in that area that is compressed by abnormally contracting muscle. It
shows some instant effect in terms of direct liberate of endogenous endorphins from the inserting
the needle of injection. BTX-A brings a modification in the sense of balance of peripheral and
central neurotransmitters (Kim, Yun and Kim, 2016).
From the investigation of Fortuna, Vaz and et.al., 2011, it has found that “BTX-A is
effective in reducing muscle spasticity over the large area as compare to cover by the injection”
(Fortuna, Vaz and et.al., 2011). The following observation can be explained by the facts that
ACh is released by both gamma and alpha motor neurons. These both have involved in the
muscle contractions in terms of either voluntary or involuntary basis. Gamma motor neurons
innervate the intrafusal fibers of the muscle spindles. BTX-A causes atrophy of the intrafusal
fibers and extrafusal fibers where alpha motor neurons are situated. The following toxin satisfies
the output from the muscle spindle to the central nervous system. In addition to this, Sahai,
Dowson, Khan and et.al., 2010 has explored from their research that “BTX-A reduces the spindle
afferent discharge in the human jaw muscle spindle” (Sahai, Dowson, Khan and et.al., 2010). It
has brought the reduction of overall muscles contraction at the time of movement of jaws. Along
with this, it has reduced the excess muscle contractions that are responsible for the pain.
Effectiveness of Conventional splint therapy in treating myofascial pain
As per the views of Turp, Komine and Hugger, (2004), Occlusal splint therapy has better
long term results in reducing the symptoms of MPDS. It terms of results, it leads to better patient
compliance with fewer side effects and it is also more cost effective than pharmacotherapy.
Thus, this is the reason it is highly recommended for the treatment of patients with MPDS.
Consequently, several therapies and some conservative surgeries are available for repositioning
of the mandible; however patients suffering with TMD dysfunction are suggested to go for
occlusal splint therapy. It is chosen in the orofacial region for various reasons. In this respect,
soft splints are recommended to patients with TMD and they can be made for maxillary arches
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
since that is easy to construct. It is often inserted immediately at the initial examination. From
the research study of various authors, it has been analyzed that a high degree of patient
acceptance has been reported with soft splints. Since, it has resilient material; therefore it assists
in distributing the heavy load that occurs during parafunctional activity.
Thus, it is clear that the conventional soft occlusal splint therapy is a much safer and
effective mode of a conservative line of therapy as compared to long term pharmacotherapy in
patients who have myofascial pain dysfunction syndrome. The degree of pain decreases up to
some extent and it helps in improving sleep, efficiency at work, social activities. The
stabilization splint (SS) is one basic category of occlusal splint. The stabilization splint is a hard
acrylic splint that provides a temporary and removable ideal occlusion which assists in releasing
the degree of TMD pain. Appropriate management of an occlusion by the use of splint therapy
reduces abnormal muscle activity and at the same time it produces neuromuscular balance.
However, Kim, Yun and Kim, (2016), argued that stabilization splint therapy may be beneficial
for reducing severity in pain at rest and on palpation and depression when compared to other
treatments.
There are several treatment available for patients with this disorder, which may be
conservative or invasive, and researcher has highlighted a few points in this respect. Treatment
for TMD is not standardized due to the different etiologies and the distinct structures that might
be affected (Santana-Moraa and Santana Penin, 2009). A wide variety of drug classes have been
described for chronic orofacial pain, ranging from short-term treatment with Non-Steroidal Anti-
Inflammatory Drugs (NSAIDs) and muscle relaxants for pain of muscular origin to long-term
administration of antidepressants for less well-characterized pain. This reduction was significant
only when the post-installation data for the OS were compared to the initial and post-counseling
data. The objective of any treatment modality for myofascial pain is to minimize or eliminate the
symptom as well as to reestablish muscular function (Katyayan, Shah and Patel, 2013). Along
with this, the myorelaxant occlusal splints may improve the pain and the amplitude of the
mandibular movement significantly; hence that is applied to numerous cases. Thus, it is
considered as an effective treatment for patients who are suffering myofascial pain with
Dislocated Disks.
Discussion
the research study of various authors, it has been analyzed that a high degree of patient
acceptance has been reported with soft splints. Since, it has resilient material; therefore it assists
in distributing the heavy load that occurs during parafunctional activity.
Thus, it is clear that the conventional soft occlusal splint therapy is a much safer and
effective mode of a conservative line of therapy as compared to long term pharmacotherapy in
patients who have myofascial pain dysfunction syndrome. The degree of pain decreases up to
some extent and it helps in improving sleep, efficiency at work, social activities. The
stabilization splint (SS) is one basic category of occlusal splint. The stabilization splint is a hard
acrylic splint that provides a temporary and removable ideal occlusion which assists in releasing
the degree of TMD pain. Appropriate management of an occlusion by the use of splint therapy
reduces abnormal muscle activity and at the same time it produces neuromuscular balance.
However, Kim, Yun and Kim, (2016), argued that stabilization splint therapy may be beneficial
for reducing severity in pain at rest and on palpation and depression when compared to other
treatments.
There are several treatment available for patients with this disorder, which may be
conservative or invasive, and researcher has highlighted a few points in this respect. Treatment
for TMD is not standardized due to the different etiologies and the distinct structures that might
be affected (Santana-Moraa and Santana Penin, 2009). A wide variety of drug classes have been
described for chronic orofacial pain, ranging from short-term treatment with Non-Steroidal Anti-
Inflammatory Drugs (NSAIDs) and muscle relaxants for pain of muscular origin to long-term
administration of antidepressants for less well-characterized pain. This reduction was significant
only when the post-installation data for the OS were compared to the initial and post-counseling
data. The objective of any treatment modality for myofascial pain is to minimize or eliminate the
symptom as well as to reestablish muscular function (Katyayan, Shah and Patel, 2013). Along
with this, the myorelaxant occlusal splints may improve the pain and the amplitude of the
mandibular movement significantly; hence that is applied to numerous cases. Thus, it is
considered as an effective treatment for patients who are suffering myofascial pain with
Dislocated Disks.
Discussion
Henceforth, concluding the entire discussion it can be said that with the help of
stabilization therapy, the intensity and level of pain can be identified. As per the results of
different researches, it can be said that the electromyography activity of the two muscles during
maximal biting was not markedly changed after the muscle relaxation splint is being used. The
results also showed that changes observed in electromyographic activity of the involved and non-
involved sides were insignificant as well (Seifeldin and Elhayes, 2015). In the above section,
research work of different authors and scholars have been discussed which clearly depicts that
splint therapy is somewhere more helpful in reducing the intensity of pain. Several research
studies have also stated that myorelazant occlusal splints are also useful to improve the pain
level. Furthermore, it also changes the amplitude of the mandibular movement.
For the purpose of correcting postural asymmetries and also to stabilize musculature
BTX-A can be given. This can also underpin and support co-contracting muscles. This is also
useful in terms of breaking the intensity of pain. At the same time, it could also improve the
working of joints masticatory muscles (Raphael and et.al., 2013). The research studies also
contends that providing appropriate treatment of temporomandibular joint disorder can increase
the blood flow to the muscle and it can also release the fibers. Following this procedure could
bring reduction in muscle tone pain due to the availability of myofascial pain syndrome.
However, this also enhances the blood circulation in the painful area and releases nerve fibers in
those areas which are compressed by abnormal contracting muscle.
Reviewing other research work, it has been identified that Occlusal Splint therapy is
highly effective for MPDS pain and it can also reduce the symptoms on higher extent. According
to clinical research, several other therapies are also available for repositioning of the mandible;
but when the intensity of pain is higher, patients are suggested to use occlusal therapy. Similarly,
soft splints are also recommended to the patients which are made up of maxillary arches and
which can be easily be constructed in the affected area. Soft splints are more acceptable by the
patients as compared to other surgeries (Park and Bae, 2013). The problem is based on different
etiologies and different structures; thus sometimes treatment for TMD is insufficient through
hard and soft splints. The chief aim of any treatment for myofascial pain is to eliminate the
symptom for the purpose of establishing muscular function.
Summary
stabilization therapy, the intensity and level of pain can be identified. As per the results of
different researches, it can be said that the electromyography activity of the two muscles during
maximal biting was not markedly changed after the muscle relaxation splint is being used. The
results also showed that changes observed in electromyographic activity of the involved and non-
involved sides were insignificant as well (Seifeldin and Elhayes, 2015). In the above section,
research work of different authors and scholars have been discussed which clearly depicts that
splint therapy is somewhere more helpful in reducing the intensity of pain. Several research
studies have also stated that myorelazant occlusal splints are also useful to improve the pain
level. Furthermore, it also changes the amplitude of the mandibular movement.
For the purpose of correcting postural asymmetries and also to stabilize musculature
BTX-A can be given. This can also underpin and support co-contracting muscles. This is also
useful in terms of breaking the intensity of pain. At the same time, it could also improve the
working of joints masticatory muscles (Raphael and et.al., 2013). The research studies also
contends that providing appropriate treatment of temporomandibular joint disorder can increase
the blood flow to the muscle and it can also release the fibers. Following this procedure could
bring reduction in muscle tone pain due to the availability of myofascial pain syndrome.
However, this also enhances the blood circulation in the painful area and releases nerve fibers in
those areas which are compressed by abnormal contracting muscle.
Reviewing other research work, it has been identified that Occlusal Splint therapy is
highly effective for MPDS pain and it can also reduce the symptoms on higher extent. According
to clinical research, several other therapies are also available for repositioning of the mandible;
but when the intensity of pain is higher, patients are suggested to use occlusal therapy. Similarly,
soft splints are also recommended to the patients which are made up of maxillary arches and
which can be easily be constructed in the affected area. Soft splints are more acceptable by the
patients as compared to other surgeries (Park and Bae, 2013). The problem is based on different
etiologies and different structures; thus sometimes treatment for TMD is insufficient through
hard and soft splints. The chief aim of any treatment for myofascial pain is to eliminate the
symptom for the purpose of establishing muscular function.
Summary
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 16
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.
