Effect of Circuit Resistance Training on Glycemic Control of Females with Diabetes Type II
VerifiedAdded on 2022/12/20
|5
|3183
|59
AI Summary
This study examines the effects of circuit resistance training (CRT) on glycemic control of females with Type II diabetes. Results show significant changes in glycosylated hemoglobin (HbA1c) and subcutaneous fat in the CRT group. The study concludes that CRT can be recommended for patients with diabetes Type II.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
International Journal of Preventive Medicine
Effect of Circuit Resistance Training on Glycemic Control of
Females with Diabetes Type II
Ramin Shabani, Marzieh Nazari, Setila Dalili1, Afagh Hassanzadeh Rad1
Department of Exercise Physiology, Islamic Azad University, Rasht Branch, Rasht, Guilan, Iran,1Pediatrics Growth Disorders Research Center, 17 Shahrivar
Hospital, School of Medicine, Guilan University of Medical Sciences, Rasht, Guilan, Iran
ABSTRACT
Background: We aimed to assess effects of circuit resistance training (CRT) on glycemic control
of females with Type II diabetes.
Methods: Twenty obese and overweight females with diabetes Type II were randomly selected in
two groups (circuit resistance exercise and control). CRT performed in 3 days/week for 3 months,
and the serum and body parameters were assessed. Data were analyzed by Mann–Whitney
U‑test and Wilcoxon Signed‑Rank test in SPSS version 19.
Results: Mean age in the CRT and control group was 50.2 ± 4.89 years and 51.3 ± 6.63 years,
respectively. Results showed significant changes in glycosylated hemoglobin (HbA 1c) and
subcutaneous fat were noted in the CRT group (P = 0.04, P = 0.002, respectively). Also, findings
indicated higher HbA 1c in CRT group after intervention in comparison with controls and results
showed a significant difference (P = 0.04).
Conclusions: According to the positive effect of CRT, it seems that can be recommended for
patients with diabetes Type II.
Keywords:Body composition, circuit resistance training, diabetes Type II, glycemic control
Copyright: © 2015 Shabani R. This is an open‑access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricte
distribution, and reproduction in any medium, provided the original author and source are credited.
Short Communication Open Access
Access this article online
Quick Response Code:
Website: www.ijpvmjournal.net/www.ijpm.ir
DOI:
10.4103/2008-7802.154923
to control blood sugar may induce serious complication
such as heart and kidney diseases,stroke, nervous
damages, blindness and poor quality of life.[6]
However,appropriatelevel of physical activity can
manage Type II diabetes[7] and resistance training has
been recentlydocumentedto be a safe and officious
therapeutic mean for the treatment of various chronic
diseases for obese individuals during elderly.[1] Improved
glycemic control can note the positive effect of physica
activity and glycosylatedhemoglobin (HbA1c
) can
be applied to measurelong‑term(120 days) control.
Sufficient glucose control is indicated as <7.0% HbA1c
value.[7] Although, previous studies that assessed resistance
exercise with combined resistance and aerobic exercise
sessions, showed significant reductions in HbA1c
.[8‑10] In
contrast, Geirsdottir et al. did not experience favorable
changesin fastingglucoseor HbA1c in patientswith
INTRODUCTION
Diabetesand obesityare global epidemicdiseases.[1‑3]
Currently,The World Health Organizationestimated
that in 2030, half of people living with diabetes will be
Asian.[4] According to the previous investigation in Iran,
about 2 million adults (7.7%) aged 25–64 yearshad
diabetes and among whom one‑half were undiagnosed.
Also, 4.4 million had impaired fasting glucose.[5] Inability
Correspondence to:
Asst Prof. Setila Dalili, Pediatric Growth Disorder Research Center, 17 Shahrivar Hospital, Shahid Siadati Street, Rasht, Guila
E‑mail: setiladalili1346@yahoo.com
How to cite this article: Shabani R, Nazari M, Dalili S, Rad AH. Effect of circuit resistance training on glycemic control of
diabetes Type II. Int J Prev Med 2015;6:34.
[Downloaded free from http://www.ijpvmjournal.net on Saturday, April 11, 2015, IP: 176.102.237.61] || Click here to download free Android application for this journa
Effect of Circuit Resistance Training on Glycemic Control of
Females with Diabetes Type II
Ramin Shabani, Marzieh Nazari, Setila Dalili1, Afagh Hassanzadeh Rad1
Department of Exercise Physiology, Islamic Azad University, Rasht Branch, Rasht, Guilan, Iran,1Pediatrics Growth Disorders Research Center, 17 Shahrivar
Hospital, School of Medicine, Guilan University of Medical Sciences, Rasht, Guilan, Iran
ABSTRACT
Background: We aimed to assess effects of circuit resistance training (CRT) on glycemic control
of females with Type II diabetes.
Methods: Twenty obese and overweight females with diabetes Type II were randomly selected in
two groups (circuit resistance exercise and control). CRT performed in 3 days/week for 3 months,
and the serum and body parameters were assessed. Data were analyzed by Mann–Whitney
U‑test and Wilcoxon Signed‑Rank test in SPSS version 19.
Results: Mean age in the CRT and control group was 50.2 ± 4.89 years and 51.3 ± 6.63 years,
respectively. Results showed significant changes in glycosylated hemoglobin (HbA 1c) and
subcutaneous fat were noted in the CRT group (P = 0.04, P = 0.002, respectively). Also, findings
indicated higher HbA 1c in CRT group after intervention in comparison with controls and results
showed a significant difference (P = 0.04).
Conclusions: According to the positive effect of CRT, it seems that can be recommended for
patients with diabetes Type II.
Keywords:Body composition, circuit resistance training, diabetes Type II, glycemic control
Copyright: © 2015 Shabani R. This is an open‑access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricte
distribution, and reproduction in any medium, provided the original author and source are credited.
Short Communication Open Access
Access this article online
Quick Response Code:
Website: www.ijpvmjournal.net/www.ijpm.ir
DOI:
10.4103/2008-7802.154923
to control blood sugar may induce serious complication
such as heart and kidney diseases,stroke, nervous
damages, blindness and poor quality of life.[6]
However,appropriatelevel of physical activity can
manage Type II diabetes[7] and resistance training has
been recentlydocumentedto be a safe and officious
therapeutic mean for the treatment of various chronic
diseases for obese individuals during elderly.[1] Improved
glycemic control can note the positive effect of physica
activity and glycosylatedhemoglobin (HbA1c
) can
be applied to measurelong‑term(120 days) control.
Sufficient glucose control is indicated as <7.0% HbA1c
value.[7] Although, previous studies that assessed resistance
exercise with combined resistance and aerobic exercise
sessions, showed significant reductions in HbA1c
.[8‑10] In
contrast, Geirsdottir et al. did not experience favorable
changesin fastingglucoseor HbA1c in patientswith
INTRODUCTION
Diabetesand obesityare global epidemicdiseases.[1‑3]
Currently,The World Health Organizationestimated
that in 2030, half of people living with diabetes will be
Asian.[4] According to the previous investigation in Iran,
about 2 million adults (7.7%) aged 25–64 yearshad
diabetes and among whom one‑half were undiagnosed.
Also, 4.4 million had impaired fasting glucose.[5] Inability
Correspondence to:
Asst Prof. Setila Dalili, Pediatric Growth Disorder Research Center, 17 Shahrivar Hospital, Shahid Siadati Street, Rasht, Guila
E‑mail: setiladalili1346@yahoo.com
How to cite this article: Shabani R, Nazari M, Dalili S, Rad AH. Effect of circuit resistance training on glycemic control of
diabetes Type II. Int J Prev Med 2015;6:34.
[Downloaded free from http://www.ijpvmjournal.net on Saturday, April 11, 2015, IP: 176.102.237.61] || Click here to download free Android application for this journa
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
International Journal of Preventive Medicine 2015, 6:34 http://www.ijpvmjournal.net/content/6/1/34
diabetes Type II.[11] Therefore, there is no consensus on
the effect of circuit resistance training (CRT) in females
with Type II diabetes. The aim of the present study was
to examine the effects of CRT with moderate intensity
and frequencyon glycemiccontrol of female with
Type II diabetes.
METHODS
Subjects
This study was conductedon obeseand overweight
femaleswith diabetesType II attendedin Ansari
Hospital, Roudsar.Informed consent was obtained,
and 20 participants were randomly divided into CRT
and control groups.First group underwent1‑month
dietitianregimenand 2 monthsCRT for 3 months.
Dietary intake was individually prescribed by 3‑day recall
technique.The Human Studies Review Committee
at Islamic Azad University, Rasht (679, 30 April 2014)
approved the study.
Measurements body composition
The height, body weight, and waist circumference
were measured at the enrollment and during the study.
Standard calibrated scale and stadiometer were used to
determine weight and height. Body mass index (BMI)
was calculated by dividing body weight (kg) by the square
of the height (m2). Caliper measuredsubcutaneous
fat in three areas (arm, super iliac and thigh). Waist
circumferencewas measuredat the midpoint of the
lowest rib and the iliac. Hip circumference was taken at
the maximum circumference of the hip. Also, waist to
hip ratio (WHR) was measured.
Laboratory tests
At the beginning and end of the study, the patients’
blood glycemic tests of the brachial vein were collected
after 12 h fasting. Baseline blood glycemic tests
including HbA1c and fasting blood glucose (FBS) (mg/dl)
were measured. FBS and HbA1c were obtained by Pars
Azmoon enzyme kits (Iran) and Biosystem auto‑analyzer
devices (Spanish), respectively.
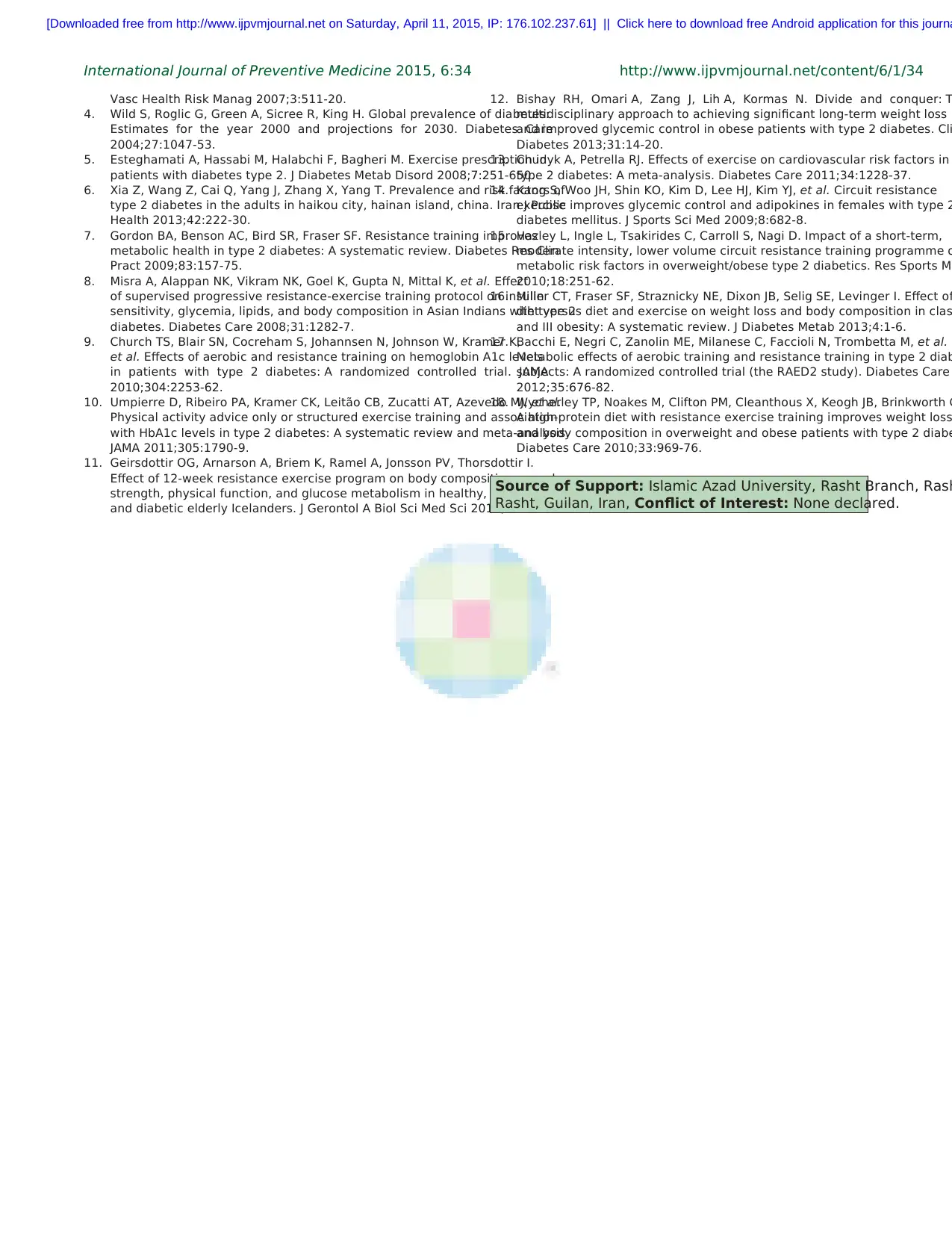
Circuit resistance training protocol
As the one‑repetitionmaximum (1‑RM) adjusted
the exerciseintensity,an individualizedCRT was
designed for each participant. After 1‑month regimen,
the CRT protocol was initiated 3 days/weekfor
2 months [Table 1]. The training consisted of 10 min
warm up and 10 min cooling. During first 1–3 weeks,
participants involved in six stations with 40–50% 1‑RM
intensity. Then, for remaining period (4–8 weeks), eight
stations with the 50–65% 1‑RM (16, 27) were indicated.
1–2 sets and 2–3 sets were noted for the first 3 weeks and
remaining 5 weeks, respectively. This program included
eight different exercises with 8–12 repetition in each set
and 3 min rest between sets. Exercises included benc
press, seated row, lateral pull down, biceps forward, front
thigh, back thigh, leg press and rowing [Table 1].
Statistical analysis
The normality of the data was indicated by
Kolmogorov–Smirnovtest. Descriptivestatisticssuch
as mean ± standard deviation was used, and data we
analyzedby Mann–WhitneyU‑test, Wilcoxon Signed
Rank‑test and Chi‑square in SPSS version 19 (SPCC
Inc., Chicago, IL, USA). P < 0.05 was considered as
statistically significant.
RESULTS
Twenty obese and overweight patients included in this
study. Mean age in the CRT and control group were
50.2 ± 4.89 years and 51.3 ± 6.63 years, respectivel
In the CRT group, significant changes in HbA1c and
subcutaneous fat were noted after intervention (P = 0.04,
P = 0.002, respectively) [Table 2].
Although, findings indicatedhigher HbA1c in CRT
group after intervention and results showed a significant
differencein two groups (P = 0.04) [Table 3].
However, there was no significantdifference between
groupsregardingweight,BMI, WHR and FBS after
intervention (P > 0.05).
DISCUSSION
This study demonstrated that a supervised CRT program
was safe and well tolerated by obese and overweight
patientswith Type II diabetes.Although we found
CRT involving eight upper and lower body exercises led
to significantreductionsin HbA1c and Subcutaneous
fat, BMI, body weight, and the WHR did not change
significantly(P ≤ 0.05) which was inconsistentwith
Bishay et al. and Chudyk and Petrella They showed CRT
as an effective tool for improving body composition.[12,13]
In addition, Kang et al. reported that 12 weeks CRT
and aerobicexerciseeffectivelyincreasedglucoseuse
and reduced the amount of insulin required.[14] Hazley
et al. noted that 50–60% of 1‑RM CRT for 8 weeks, can
reduce waist circumference and WHR significantly, with
no associated changes in the control group.
CONCLUSIONS
The resistancetrainingprogramhad little impact on
metabolic risk factors in diabetics Type II.[15] However,
some studies observedno effect. In a systematic
review by Miller et al. which examined the combined
effectsof diet versusdiet and exercise,the majority
[Downloaded free from http://www.ijpvmjournal.net on Saturday, April 11, 2015, IP: 176.102.237.61] || Click here to download free Android application for this journa
diabetes Type II.[11] Therefore, there is no consensus on
the effect of circuit resistance training (CRT) in females
with Type II diabetes. The aim of the present study was
to examine the effects of CRT with moderate intensity
and frequencyon glycemiccontrol of female with
Type II diabetes.
METHODS
Subjects
This study was conductedon obeseand overweight
femaleswith diabetesType II attendedin Ansari
Hospital, Roudsar.Informed consent was obtained,
and 20 participants were randomly divided into CRT
and control groups.First group underwent1‑month
dietitianregimenand 2 monthsCRT for 3 months.
Dietary intake was individually prescribed by 3‑day recall
technique.The Human Studies Review Committee
at Islamic Azad University, Rasht (679, 30 April 2014)
approved the study.
Measurements body composition
The height, body weight, and waist circumference
were measured at the enrollment and during the study.
Standard calibrated scale and stadiometer were used to
determine weight and height. Body mass index (BMI)
was calculated by dividing body weight (kg) by the square
of the height (m2). Caliper measuredsubcutaneous
fat in three areas (arm, super iliac and thigh). Waist
circumferencewas measuredat the midpoint of the
lowest rib and the iliac. Hip circumference was taken at
the maximum circumference of the hip. Also, waist to
hip ratio (WHR) was measured.
Laboratory tests
At the beginning and end of the study, the patients’
blood glycemic tests of the brachial vein were collected
after 12 h fasting. Baseline blood glycemic tests
including HbA1c and fasting blood glucose (FBS) (mg/dl)
were measured. FBS and HbA1c were obtained by Pars
Azmoon enzyme kits (Iran) and Biosystem auto‑analyzer
devices (Spanish), respectively.
Circuit resistance training protocol
As the one‑repetitionmaximum (1‑RM) adjusted
the exerciseintensity,an individualizedCRT was
designed for each participant. After 1‑month regimen,
the CRT protocol was initiated 3 days/weekfor
2 months [Table 1]. The training consisted of 10 min
warm up and 10 min cooling. During first 1–3 weeks,
participants involved in six stations with 40–50% 1‑RM
intensity. Then, for remaining period (4–8 weeks), eight
stations with the 50–65% 1‑RM (16, 27) were indicated.
1–2 sets and 2–3 sets were noted for the first 3 weeks and
remaining 5 weeks, respectively. This program included
eight different exercises with 8–12 repetition in each set
and 3 min rest between sets. Exercises included benc
press, seated row, lateral pull down, biceps forward, front
thigh, back thigh, leg press and rowing [Table 1].
Statistical analysis
The normality of the data was indicated by
Kolmogorov–Smirnovtest. Descriptivestatisticssuch
as mean ± standard deviation was used, and data we
analyzedby Mann–WhitneyU‑test, Wilcoxon Signed
Rank‑test and Chi‑square in SPSS version 19 (SPCC
Inc., Chicago, IL, USA). P < 0.05 was considered as
statistically significant.
RESULTS
Twenty obese and overweight patients included in this
study. Mean age in the CRT and control group were
50.2 ± 4.89 years and 51.3 ± 6.63 years, respectivel
In the CRT group, significant changes in HbA1c and
subcutaneous fat were noted after intervention (P = 0.04,
P = 0.002, respectively) [Table 2].
Although, findings indicatedhigher HbA1c in CRT
group after intervention and results showed a significant
differencein two groups (P = 0.04) [Table 3].
However, there was no significantdifference between
groupsregardingweight,BMI, WHR and FBS after
intervention (P > 0.05).
DISCUSSION
This study demonstrated that a supervised CRT program
was safe and well tolerated by obese and overweight
patientswith Type II diabetes.Although we found
CRT involving eight upper and lower body exercises led
to significantreductionsin HbA1c and Subcutaneous
fat, BMI, body weight, and the WHR did not change
significantly(P ≤ 0.05) which was inconsistentwith
Bishay et al. and Chudyk and Petrella They showed CRT
as an effective tool for improving body composition.[12,13]
In addition, Kang et al. reported that 12 weeks CRT
and aerobicexerciseeffectivelyincreasedglucoseuse
and reduced the amount of insulin required.[14] Hazley
et al. noted that 50–60% of 1‑RM CRT for 8 weeks, can
reduce waist circumference and WHR significantly, with
no associated changes in the control group.
CONCLUSIONS
The resistancetrainingprogramhad little impact on
metabolic risk factors in diabetics Type II.[15] However,
some studies observedno effect. In a systematic
review by Miller et al. which examined the combined
effectsof diet versusdiet and exercise,the majority
[Downloaded free from http://www.ijpvmjournal.net on Saturday, April 11, 2015, IP: 176.102.237.61] || Click here to download free Android application for this journa

International Journal of Preventive Medicine 2015, 6:34 http://www.ijpvmjournal.net/content/6/1/34
of studies mentioned no significant difference in
body compositionwhen exercisewas added to diet
restriction.[16] Furthermore, Misra et al. assessed effect of
12 weeks progressive resistance‑exercise training on body
composition in patients with Type II diabetes. Resistance
training produced an increase in fat‑free mass and diabetic
patientsneededmore resistancetraining to improve
muscle mass as they got older. It seems that resistance
training reduces subcutaneous fat and probably it causes
increased muscle fiber that might be due to some factors
such as frequency, duration and intensity of exercise.[8]
Church et al. Showed that the effect of resistance
exerciseon glycemiccontrol in individualsassociated
with a 0.57% decline in absolute HbA1c as compared with
control.[9] Also, another study assessed resistance training
and aerobic training in females aged between 40 and
70 years in two groups. They indicated improvement in
HbA1c in both groups after 4 months.[17] Another study
showedthat 12 weeksprogressivemoderate‑intensity
resistance exercise resulted in significant improvements
in glycaemia in Indians with Type II diabetes.[18] This
showed that the effectiveness of resistance training on
improving HbA1c in diabetes patients appeared to differ
accordingto the intensity,frequency,and durationof
training. As a result, CRT had a positive effect on HbA1c
in females with diabetics Type II. It seems that plasma
membrane GLUT4 was increased in skeletal muscle from
individual with Type II diabetes in response to an acut
exercise. Also, lower resting plasma membrane GLUT4
content in insulin resistant subjects have been observe
in some studies.[1]
ACKNOWLEDGEMENTS
We appreciatepatientsparticipatingin this study and the
staff of Diabetes Unit in Ansari Hospital of Roudsar for their
cooperation. This study was financially supported by Islamic
Azad University, Rasht Branch.
Received: 12 Nov 14 Accepted: 23 Feb 15
Published: 10 Apr 15
REFERENCES
1. Arora E, Shenoy S, Sandhu JS. Effects of resistance training on metabolic
profile of adults with type 2 diabetes. Indian J Med Res 2009;129:515‑9.
2. Eakin EG, Reeves MM, Lawler SP, Oldenburg B, Del Mar C, Wilkie K,
et al. The Logan Healthy Living Program: A cluster randomized trial of a
telephone‑delivered physical activity and dietary behavior intervention fo
primary care patients with type 2 diabetes or hypertension from a socially
disadvantaged community – Rationale, design and recruitment. Contemp
Clin Trials 2008;29:439‑54.
3. Iqbal N. The burden of type 2 diabetes: Strategies to prevent or delay ons
Table 3: Comparison of changes in body composition and
laboratory results after intervention period
Variable CRT (n=10) control (n=10) Pvalue
Weight (kg) 75.7±11.3 74.6±11.8 0.4
BMI (kg) 31.3±4.8 30.3±4.8 0.5
Subcutaneous fat (mm)31.02±4.6 29.68±2.62 0.001*
Waist‑hip ratio 0.89±0.07 0.88±0.06 0.052
HbA1c, mg/dl 7.6±1.7 6.1±1.1 0.04*
FBS, mg/dl 158±41.1 26.1±158.6 0.2
Significant difference of P≤0.05*
Table 1. Timeline of intervention
Duration
(week)
Time line (in minute) workout Training frequency
(Day/W)
Intensity
descriptionWarm‑up Resistance exerciseCool down Seated resting
1st and 3nd week 10 30‑35 10 1‑2 3 40‑50% 1RM
1‑2 set, 8 reps*
6 stations
4st and 8nd week 10 40‑45 10 2‑3 3 50‑65% 1RM
2‑3 set, 10‑12 reps
8 stations
Reps – Repetitions*
Table 2. Body composition and laboratory results at the initiation and their changes during interven
groups
CRT (n=10) Pvalue Control (n=10) Pvalue
Pre Post Wilcoxon test Pre Post Wilcoxon test
Weight (kg) 75.5±10.16 74.6±11.8 0.4 74.6±11.8 75.7±11.3 0.8
BMI (kg/m2) 30.16±3.6 31.3±4.8 0.4 30.5±4.8 30.3±4.8 0.8
Subcutaneous fat (mm) 32.8±47.3 29.68±2.62 0.002* 31.66±4.4 31.02±4.6 0.2
Waist‑hip ratio 0.86±0.05 0.88±0.06 0.052 0.88±0.07 0.89±0.07 0.07
HbA1c, mg/dl 7.1±1.1 6.1±1.1 0.02* 7.8±1.7 7.6±1.7 0.1
FBS, mg/dl 159.6±52.2 158.6±26.1 0.3 158.6±48.4 158±41.1 0.1
*Significant difference of P≤0.05
[Downloaded free from http://www.ijpvmjournal.net on Saturday, April 11, 2015, IP: 176.102.237.61] || Click here to download free Android application for this journa
of studies mentioned no significant difference in
body compositionwhen exercisewas added to diet
restriction.[16] Furthermore, Misra et al. assessed effect of
12 weeks progressive resistance‑exercise training on body
composition in patients with Type II diabetes. Resistance
training produced an increase in fat‑free mass and diabetic
patientsneededmore resistancetraining to improve
muscle mass as they got older. It seems that resistance
training reduces subcutaneous fat and probably it causes
increased muscle fiber that might be due to some factors
such as frequency, duration and intensity of exercise.[8]
Church et al. Showed that the effect of resistance
exerciseon glycemiccontrol in individualsassociated
with a 0.57% decline in absolute HbA1c as compared with
control.[9] Also, another study assessed resistance training
and aerobic training in females aged between 40 and
70 years in two groups. They indicated improvement in
HbA1c in both groups after 4 months.[17] Another study
showedthat 12 weeksprogressivemoderate‑intensity
resistance exercise resulted in significant improvements
in glycaemia in Indians with Type II diabetes.[18] This
showed that the effectiveness of resistance training on
improving HbA1c in diabetes patients appeared to differ
accordingto the intensity,frequency,and durationof
training. As a result, CRT had a positive effect on HbA1c
in females with diabetics Type II. It seems that plasma
membrane GLUT4 was increased in skeletal muscle from
individual with Type II diabetes in response to an acut
exercise. Also, lower resting plasma membrane GLUT4
content in insulin resistant subjects have been observe
in some studies.[1]
ACKNOWLEDGEMENTS
We appreciatepatientsparticipatingin this study and the
staff of Diabetes Unit in Ansari Hospital of Roudsar for their
cooperation. This study was financially supported by Islamic
Azad University, Rasht Branch.
Received: 12 Nov 14 Accepted: 23 Feb 15
Published: 10 Apr 15
REFERENCES
1. Arora E, Shenoy S, Sandhu JS. Effects of resistance training on metabolic
profile of adults with type 2 diabetes. Indian J Med Res 2009;129:515‑9.
2. Eakin EG, Reeves MM, Lawler SP, Oldenburg B, Del Mar C, Wilkie K,
et al. The Logan Healthy Living Program: A cluster randomized trial of a
telephone‑delivered physical activity and dietary behavior intervention fo
primary care patients with type 2 diabetes or hypertension from a socially
disadvantaged community – Rationale, design and recruitment. Contemp
Clin Trials 2008;29:439‑54.
3. Iqbal N. The burden of type 2 diabetes: Strategies to prevent or delay ons
Table 3: Comparison of changes in body composition and
laboratory results after intervention period
Variable CRT (n=10) control (n=10) Pvalue
Weight (kg) 75.7±11.3 74.6±11.8 0.4
BMI (kg) 31.3±4.8 30.3±4.8 0.5
Subcutaneous fat (mm)31.02±4.6 29.68±2.62 0.001*
Waist‑hip ratio 0.89±0.07 0.88±0.06 0.052
HbA1c, mg/dl 7.6±1.7 6.1±1.1 0.04*
FBS, mg/dl 158±41.1 26.1±158.6 0.2
Significant difference of P≤0.05*
Table 1. Timeline of intervention
Duration
(week)
Time line (in minute) workout Training frequency
(Day/W)
Intensity
descriptionWarm‑up Resistance exerciseCool down Seated resting
1st and 3nd week 10 30‑35 10 1‑2 3 40‑50% 1RM
1‑2 set, 8 reps*
6 stations
4st and 8nd week 10 40‑45 10 2‑3 3 50‑65% 1RM
2‑3 set, 10‑12 reps
8 stations
Reps – Repetitions*
Table 2. Body composition and laboratory results at the initiation and their changes during interven
groups
CRT (n=10) Pvalue Control (n=10) Pvalue
Pre Post Wilcoxon test Pre Post Wilcoxon test
Weight (kg) 75.5±10.16 74.6±11.8 0.4 74.6±11.8 75.7±11.3 0.8
BMI (kg/m2) 30.16±3.6 31.3±4.8 0.4 30.5±4.8 30.3±4.8 0.8
Subcutaneous fat (mm) 32.8±47.3 29.68±2.62 0.002* 31.66±4.4 31.02±4.6 0.2
Waist‑hip ratio 0.86±0.05 0.88±0.06 0.052 0.88±0.07 0.89±0.07 0.07
HbA1c, mg/dl 7.1±1.1 6.1±1.1 0.02* 7.8±1.7 7.6±1.7 0.1
FBS, mg/dl 159.6±52.2 158.6±26.1 0.3 158.6±48.4 158±41.1 0.1
*Significant difference of P≤0.05
[Downloaded free from http://www.ijpvmjournal.net on Saturday, April 11, 2015, IP: 176.102.237.61] || Click here to download free Android application for this journa
International Journal of Preventive Medicine 2015, 6:34 http://www.ijpvmjournal.net/content/6/1/34
Vasc Health Risk Manag 2007;3:511‑20.
4. Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes:
Estimates for the year 2000 and projections for 2030. Diabetes Care
2004;27:1047‑53.
5. Esteghamati A, Hassabi M, Halabchi F, Bagheri M. Exercise prescription in
patients with diabetes type 2. J Diabetes Metab Disord 2008;7:251‑650.
6. Xia Z, Wang Z, Cai Q, Yang J, Zhang X, Yang T. Prevalence and risk factors of
type 2 diabetes in the adults in haikou city, hainan island, china. Iran J Public
Health 2013;42:222‑30.
7. Gordon BA, Benson AC, Bird SR, Fraser SF. Resistance training improves
metabolic health in type 2 diabetes: A systematic review. Diabetes Res Clin
Pract 2009;83:157‑75.
8. Misra A, Alappan NK, Vikram NK, Goel K, Gupta N, Mittal K, et al. Effect
of supervised progressive resistance‑exercise training protocol on insulin
sensitivity, glycemia, lipids, and body composition in Asian Indians with type 2
diabetes. Diabetes Care 2008;31:1282‑7.
9. Church TS, Blair SN, Cocreham S, Johannsen N, Johnson W, Kramer K,
et al. Effects of aerobic and resistance training on hemoglobin A1c levels
in patients with type 2 diabetes: A randomized controlled trial. JAMA
2010;304:2253‑62.
10. Umpierre D, Ribeiro PA, Kramer CK, Leitão CB, Zucatti AT, Azevedo MJ, et al.
Physical activity advice only or structured exercise training and association
with HbA1c levels in type 2 diabetes: A systematic review and meta‑analysis.
JAMA 2011;305:1790‑9.
11. Geirsdottir OG, Arnarson A, Briem K, Ramel A, Jonsson PV, Thorsdottir I.
Effect of 12‑week resistance exercise program on body composition, muscle
strength, physical function, and glucose metabolism in healthy, insulin‑resistant,
and diabetic elderly Icelanders. J Gerontol A Biol Sci Med Sci 2012;67:1259‑65.
12. Bishay RH, Omari A, Zang J, Lih A, Kormas N. Divide and conquer: T
multidisciplinary approach to achieving significant long‑term weight loss
and improved glycemic control in obese patients with type 2 diabetes. Cli
Diabetes 2013;31:14‑20.
13. Chudyk A, Petrella RJ. Effects of exercise on cardiovascular risk factors in
type 2 diabetes: A meta‑analysis. Diabetes Care 2011;34:1228‑37.
14. Kang S, Woo JH, Shin KO, Kim D, Lee HJ, Kim YJ, et al. Circuit resistance
exercise improves glycemic control and adipokines in females with type 2
diabetes mellitus. J Sports Sci Med 2009;8:682‑8.
15. Hazley L, Ingle L, Tsakirides C, Carroll S, Nagi D. Impact of a short‑term,
moderate intensity, lower volume circuit resistance training programme o
metabolic risk factors in overweight/obese type 2 diabetics. Res Sports Me
2010;18:251‑62.
16. Miller CT, Fraser SF, Straznicky NE, Dixon JB, Selig SE, Levinger I. Effect of
diet versus diet and exercise on weight loss and body composition in clas
and III obesity: A systematic review. J Diabetes Metab 2013;4:1‑6.
17. Bacchi E, Negri C, Zanolin ME, Milanese C, Faccioli N, Trombetta M, et al.
Metabolic effects of aerobic training and resistance training in type 2 diab
subjects: A randomized controlled trial (the RAED2 study). Diabetes Care
2012;35:676‑82.
18. Wycherley TP, Noakes M, Clifton PM, Cleanthous X, Keogh JB, Brinkworth G
A high‑protein diet with resistance exercise training improves weight loss
and body composition in overweight and obese patients with type 2 diabe
Diabetes Care 2010;33:969‑76.
Source of Support: Islamic Azad University, Rasht Branch, Rash
Rasht, Guilan, Iran, Conflict of Interest: None declared.
[Downloaded free from http://www.ijpvmjournal.net on Saturday, April 11, 2015, IP: 176.102.237.61] || Click here to download free Android application for this journa
Vasc Health Risk Manag 2007;3:511‑20.
4. Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes:
Estimates for the year 2000 and projections for 2030. Diabetes Care
2004;27:1047‑53.
5. Esteghamati A, Hassabi M, Halabchi F, Bagheri M. Exercise prescription in
patients with diabetes type 2. J Diabetes Metab Disord 2008;7:251‑650.
6. Xia Z, Wang Z, Cai Q, Yang J, Zhang X, Yang T. Prevalence and risk factors of
type 2 diabetes in the adults in haikou city, hainan island, china. Iran J Public
Health 2013;42:222‑30.
7. Gordon BA, Benson AC, Bird SR, Fraser SF. Resistance training improves
metabolic health in type 2 diabetes: A systematic review. Diabetes Res Clin
Pract 2009;83:157‑75.
8. Misra A, Alappan NK, Vikram NK, Goel K, Gupta N, Mittal K, et al. Effect
of supervised progressive resistance‑exercise training protocol on insulin
sensitivity, glycemia, lipids, and body composition in Asian Indians with type 2
diabetes. Diabetes Care 2008;31:1282‑7.
9. Church TS, Blair SN, Cocreham S, Johannsen N, Johnson W, Kramer K,
et al. Effects of aerobic and resistance training on hemoglobin A1c levels
in patients with type 2 diabetes: A randomized controlled trial. JAMA
2010;304:2253‑62.
10. Umpierre D, Ribeiro PA, Kramer CK, Leitão CB, Zucatti AT, Azevedo MJ, et al.
Physical activity advice only or structured exercise training and association
with HbA1c levels in type 2 diabetes: A systematic review and meta‑analysis.
JAMA 2011;305:1790‑9.
11. Geirsdottir OG, Arnarson A, Briem K, Ramel A, Jonsson PV, Thorsdottir I.
Effect of 12‑week resistance exercise program on body composition, muscle
strength, physical function, and glucose metabolism in healthy, insulin‑resistant,
and diabetic elderly Icelanders. J Gerontol A Biol Sci Med Sci 2012;67:1259‑65.
12. Bishay RH, Omari A, Zang J, Lih A, Kormas N. Divide and conquer: T
multidisciplinary approach to achieving significant long‑term weight loss
and improved glycemic control in obese patients with type 2 diabetes. Cli
Diabetes 2013;31:14‑20.
13. Chudyk A, Petrella RJ. Effects of exercise on cardiovascular risk factors in
type 2 diabetes: A meta‑analysis. Diabetes Care 2011;34:1228‑37.
14. Kang S, Woo JH, Shin KO, Kim D, Lee HJ, Kim YJ, et al. Circuit resistance
exercise improves glycemic control and adipokines in females with type 2
diabetes mellitus. J Sports Sci Med 2009;8:682‑8.
15. Hazley L, Ingle L, Tsakirides C, Carroll S, Nagi D. Impact of a short‑term,
moderate intensity, lower volume circuit resistance training programme o
metabolic risk factors in overweight/obese type 2 diabetics. Res Sports Me
2010;18:251‑62.
16. Miller CT, Fraser SF, Straznicky NE, Dixon JB, Selig SE, Levinger I. Effect of
diet versus diet and exercise on weight loss and body composition in clas
and III obesity: A systematic review. J Diabetes Metab 2013;4:1‑6.
17. Bacchi E, Negri C, Zanolin ME, Milanese C, Faccioli N, Trombetta M, et al.
Metabolic effects of aerobic training and resistance training in type 2 diab
subjects: A randomized controlled trial (the RAED2 study). Diabetes Care
2012;35:676‑82.
18. Wycherley TP, Noakes M, Clifton PM, Cleanthous X, Keogh JB, Brinkworth G
A high‑protein diet with resistance exercise training improves weight loss
and body composition in overweight and obese patients with type 2 diabe
Diabetes Care 2010;33:969‑76.
Source of Support: Islamic Azad University, Rasht Branch, Rash
Rasht, Guilan, Iran, Conflict of Interest: None declared.
[Downloaded free from http://www.ijpvmjournal.net on Saturday, April 11, 2015, IP: 176.102.237.61] || Click here to download free Android application for this journa
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Copyright of International Journal of Preventive Medicine is the property of Medknow
Publications & Media Pvt. Ltd. and its content may not be copied or emailed to multiple sites
or posted to a listserv without the copyright holder's express written permission. However,
users may print, download, or email articles for individual use.
Publications & Media Pvt. Ltd. and its content may not be copied or emailed to multiple sites
or posted to a listserv without the copyright holder's express written permission. However,
users may print, download, or email articles for individual use.
1 out of 5
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.

