DRIVING POST TRAUMATIC BRAIN INJURY: A NARRATIVE REVIEW.
VerifiedAdded on 2022/11/16
|13
|2869
|43
AI Summary
Current research into driving post Traumatic Brain Injuries, a narrative review.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

DRIVING POST TRAUMATIC BRAIN INJURY: A NARRATIVE REVIEW
DRIVING POST TRAUMATIC BRAIN INJURY: A NARRATIVE REVIEW
Name of the Student
Name of the University
Author’s Note
DRIVING POST TRAUMATIC BRAIN INJURY: A NARRATIVE REVIEW
Name of the Student
Name of the University
Author’s Note
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1DRIVING POST TRAUMATIC BRAIN INJURY: A NARRATIVE REVIEW
Executive Summary
Various parts of the brain helps in controlling and coordinating the skills required for on-road
driving. Following a traumatic injury to the brain, proper functionality required for the
correct execution of driving skills might be hampered. Proper assessment of the physical and
emotional recovery post traumatic brain injury along with a proper guided rehabilitation of
the driver is of utmost importance. Adequate reassessment of on-road driving and
interventions of occupational therapy has proven to be valuable for an increased prospect for
the return of the individual to driving along with constant support and care from the family
members and significant others to achieve independent driving and successful social
integration into the community. Therefore, detailed rehabilitation program with assessment of
driving skill on road and occupational therapy interventions are critical features for the
successful return of the individual post traumatic brain injury.
Executive Summary
Various parts of the brain helps in controlling and coordinating the skills required for on-road
driving. Following a traumatic injury to the brain, proper functionality required for the
correct execution of driving skills might be hampered. Proper assessment of the physical and
emotional recovery post traumatic brain injury along with a proper guided rehabilitation of
the driver is of utmost importance. Adequate reassessment of on-road driving and
interventions of occupational therapy has proven to be valuable for an increased prospect for
the return of the individual to driving along with constant support and care from the family
members and significant others to achieve independent driving and successful social
integration into the community. Therefore, detailed rehabilitation program with assessment of
driving skill on road and occupational therapy interventions are critical features for the
successful return of the individual post traumatic brain injury.
2DRIVING POST TRAUMATIC BRAIN INJURY: A NARRATIVE REVIEW
Table of Contents
Introduction................................................................................................................................3
Literature review........................................................................................................................4
Evaluation of articles..............................................................................................................4
Table of key findings.............................................................................................................6
Crucial bias.............................................................................................................................7
Assessment of the bias...........................................................................................................8
Discussion..................................................................................................................................8
Limitations.............................................................................................................................9
Implications of the study......................................................................................................10
Conclusion................................................................................................................................10
References................................................................................................................................11
Table of Contents
Introduction................................................................................................................................3
Literature review........................................................................................................................4
Evaluation of articles..............................................................................................................4
Table of key findings.............................................................................................................6
Crucial bias.............................................................................................................................7
Assessment of the bias...........................................................................................................8
Discussion..................................................................................................................................8
Limitations.............................................................................................................................9
Implications of the study......................................................................................................10
Conclusion................................................................................................................................10
References................................................................................................................................11
3DRIVING POST TRAUMATIC BRAIN INJURY: A NARRATIVE REVIEW
Introduction
Driving is a premium quality skill, developed by engaging various cognitive skills to
deliver an accurately determined process. Driving is based on a assorted set of cognition
functioning tasks namely information processing, comprehensive eye-hand-leg coordination,
memory processing, visuo-spatial perceptive skills, selective attention and concentration
skills along with navigational skills (Allen, Beck & Zanjani, 2019).
Different parts of the brain simultaneously work in achieving an integrated focus
leading to precise execution of driving. The dorso-lateral prefrontal cortex is the core center
for making decisive judgments whereas the parietal lobe concentrates on the integration of
the information gathered from all the senses along with visuo-spatial awareness. The occipital
lobe is responsible for the visual acuity whereas the temporal lobe comprising of the auditory
lobe is responsible for aural perception (Navarro, Osiurak & Reynaud, 2018). The cerebellum
coordinates the voluntary muscle actions and works to maintain balance and take rapid
decisions.
Head trauma leading to injury to the brain might cause significant problems which
might cause considerable physical, emotion and cognitive damages. The impact of the brain
injury might reflect on driving skills of the individual as driving requires immense control
and coordination of actions managed by various parts of the brain (Coleman et al., 2002).
This study aims at reviewing the researches on different factors and their implications on
driving, post a traumatic brain injury.
Introduction
Driving is a premium quality skill, developed by engaging various cognitive skills to
deliver an accurately determined process. Driving is based on a assorted set of cognition
functioning tasks namely information processing, comprehensive eye-hand-leg coordination,
memory processing, visuo-spatial perceptive skills, selective attention and concentration
skills along with navigational skills (Allen, Beck & Zanjani, 2019).
Different parts of the brain simultaneously work in achieving an integrated focus
leading to precise execution of driving. The dorso-lateral prefrontal cortex is the core center
for making decisive judgments whereas the parietal lobe concentrates on the integration of
the information gathered from all the senses along with visuo-spatial awareness. The occipital
lobe is responsible for the visual acuity whereas the temporal lobe comprising of the auditory
lobe is responsible for aural perception (Navarro, Osiurak & Reynaud, 2018). The cerebellum
coordinates the voluntary muscle actions and works to maintain balance and take rapid
decisions.
Head trauma leading to injury to the brain might cause significant problems which
might cause considerable physical, emotion and cognitive damages. The impact of the brain
injury might reflect on driving skills of the individual as driving requires immense control
and coordination of actions managed by various parts of the brain (Coleman et al., 2002).
This study aims at reviewing the researches on different factors and their implications on
driving, post a traumatic brain injury.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4DRIVING POST TRAUMATIC BRAIN INJURY: A NARRATIVE REVIEW
Literature review
Evaluation of articles
Proper assessment of physical and emotional recovery is required for the individual
to return to driving after a traumatic brain injury (Hawley, 2001). The evaluation protocols
were bases on memory retention, occurrence of headaches, fatigability, problems with sleep,
dizziness, depressions aural problems, visual concerns, seizures, blank spells, balance issues
along with behavioral predicaments namely anger management, irritability, aggressions,
mood swings, behavioral changes and so on. Physical and emotional assessment with the help
of functional independence/functional assessment measuring tool (FIM+FAM) to review the
individual’s orientation, emotional status, judgment of safety and attention are crucial
(Hawley, 2001).
The individual has to deal with various barriers and requires adequate time for the
integration into community as it was before the traumatic brain injury (Rapport, Hanks &
Bryer, 2006). Research suggests that family members and relatives influence the individuals
to cease driving for safety reasons after traumatic brain injury which ends up curbing the
independence and confidence of the individual to some extent. Thus, counseling of the family
members is also required to overcome emotional and social barriers in order to maximize the
community integration and independence of the traumatic brain injury survivor (Rapport,
Hanks & Bryer, 2006).
The study encompasses articles on early neuropsychological diagnostic tests as the
medical correlates of returning to driving on road, after physical recovery from a traumatic
brain injury (Cullen, Krakowski & Taggart, 2014). The four neuropsychological tests used
for the assessment of neuropsychological functionality were the trail making A test, the trail
making B test, the digit span forward test and the digit span backward test which were all
Literature review
Evaluation of articles
Proper assessment of physical and emotional recovery is required for the individual
to return to driving after a traumatic brain injury (Hawley, 2001). The evaluation protocols
were bases on memory retention, occurrence of headaches, fatigability, problems with sleep,
dizziness, depressions aural problems, visual concerns, seizures, blank spells, balance issues
along with behavioral predicaments namely anger management, irritability, aggressions,
mood swings, behavioral changes and so on. Physical and emotional assessment with the help
of functional independence/functional assessment measuring tool (FIM+FAM) to review the
individual’s orientation, emotional status, judgment of safety and attention are crucial
(Hawley, 2001).
The individual has to deal with various barriers and requires adequate time for the
integration into community as it was before the traumatic brain injury (Rapport, Hanks &
Bryer, 2006). Research suggests that family members and relatives influence the individuals
to cease driving for safety reasons after traumatic brain injury which ends up curbing the
independence and confidence of the individual to some extent. Thus, counseling of the family
members is also required to overcome emotional and social barriers in order to maximize the
community integration and independence of the traumatic brain injury survivor (Rapport,
Hanks & Bryer, 2006).
The study encompasses articles on early neuropsychological diagnostic tests as the
medical correlates of returning to driving on road, after physical recovery from a traumatic
brain injury (Cullen, Krakowski & Taggart, 2014). The four neuropsychological tests used
for the assessment of neuropsychological functionality were the trail making A test, the trail
making B test, the digit span forward test and the digit span backward test which were all
5DRIVING POST TRAUMATIC BRAIN INJURY: A NARRATIVE REVIEW
examined during the rehabilitation program and were compared and analyzed against the
results of same test results of drivers and non-drivers (Cullen, Krakowski & Taggart, 2014).
Research is also based on the inclusion of variable parameters to predict the
performance of the individual, following a traumatic brain injury, as an on-road driver (Ross
et al., 2015). The variables which were assessed were the age of injury, Glasgow Coma Scale
Score, post traumatic amnesia duration, driving experience, reaction timing and physical
impairment. Duration of post traumatic amnesia was predicted to be a better judge of
assessment of driving compared to outcomes assessed by Glasgow Coma Scale score and the
post traumatic amnesia duration might aid physicians in determining the criteria of reference
for the occupational therapy on-road assessment of driving (Ross et al., 2015). Completion
of a defined route along with examination of lane changing maneuvers, parking, merging
with traffic, tactful negotiations with intersections, high and low density traffic handling,
management of distractions were evaluated to assess the individuals level of competency and
expertise before returning to independent on-road driving.
It also draws attention to various awareness protocols that should be followed for
proper on-road performance of driving after recovery from a traumatic brain injury (Gooden
et al., 2017). Drivers who had failed their on-road driving skill evaluation test overestimated
their ability to drive significantly. The cognitive functions including psychomotor analysis of
speed and attention to details were found to be intricately associated with the alertness during
driving, whereas the psychological aspect was related to the self-ratings of the driving ability.
The impaired awareness therefore must be addressed during the rehabilitation programs of
the driver with traumatic brain injury (Gooden et al., 2017).
Investigation also shows that individuals after physical recovery from a distressing
brain injury frequently miscalculates the risks after passing evaluation of driving procedural
examined during the rehabilitation program and were compared and analyzed against the
results of same test results of drivers and non-drivers (Cullen, Krakowski & Taggart, 2014).
Research is also based on the inclusion of variable parameters to predict the
performance of the individual, following a traumatic brain injury, as an on-road driver (Ross
et al., 2015). The variables which were assessed were the age of injury, Glasgow Coma Scale
Score, post traumatic amnesia duration, driving experience, reaction timing and physical
impairment. Duration of post traumatic amnesia was predicted to be a better judge of
assessment of driving compared to outcomes assessed by Glasgow Coma Scale score and the
post traumatic amnesia duration might aid physicians in determining the criteria of reference
for the occupational therapy on-road assessment of driving (Ross et al., 2015). Completion
of a defined route along with examination of lane changing maneuvers, parking, merging
with traffic, tactful negotiations with intersections, high and low density traffic handling,
management of distractions were evaluated to assess the individuals level of competency and
expertise before returning to independent on-road driving.
It also draws attention to various awareness protocols that should be followed for
proper on-road performance of driving after recovery from a traumatic brain injury (Gooden
et al., 2017). Drivers who had failed their on-road driving skill evaluation test overestimated
their ability to drive significantly. The cognitive functions including psychomotor analysis of
speed and attention to details were found to be intricately associated with the alertness during
driving, whereas the psychological aspect was related to the self-ratings of the driving ability.
The impaired awareness therefore must be addressed during the rehabilitation programs of
the driver with traumatic brain injury (Gooden et al., 2017).
Investigation also shows that individuals after physical recovery from a distressing
brain injury frequently miscalculates the risks after passing evaluation of driving procedural
6DRIVING POST TRAUMATIC BRAIN INJURY: A NARRATIVE REVIEW
when compared to individuals after recovery from traumatic brain injury driving without any
driving evaluation test (McKerral et al., 2019). The individuals with successful driving
evaluation had the tendency of giving low scores while self assessment while the official
driving records reflected higher demerit points and significant higher occurrence of post-
rehabilitation accidents as compared to the group of post traumatic brain injury individuals
without any driving individuals (McKerral et al., 2019). Impaired awareness and wrong self
assessment during driving must be addressed during driver rehabilitation program.
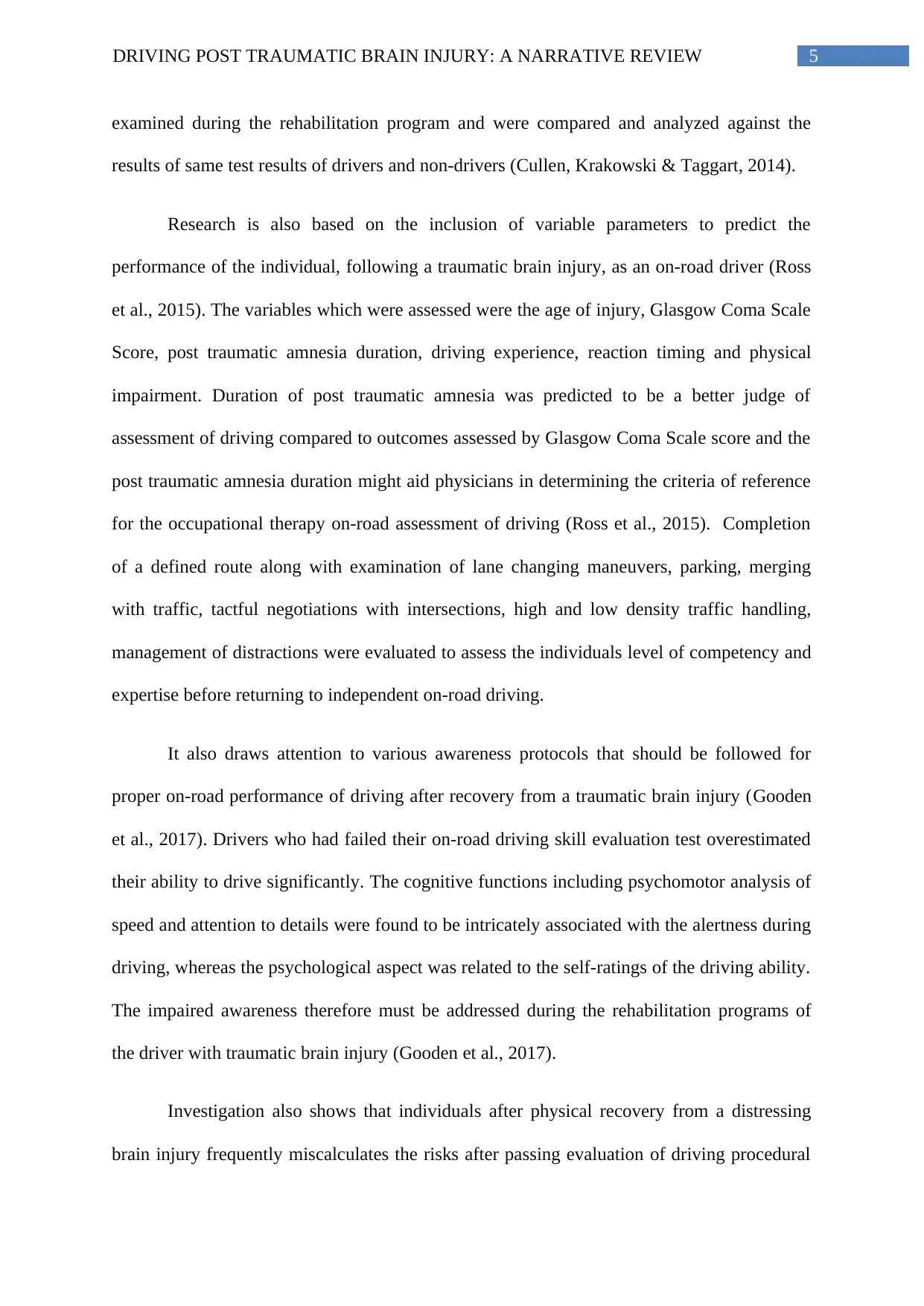
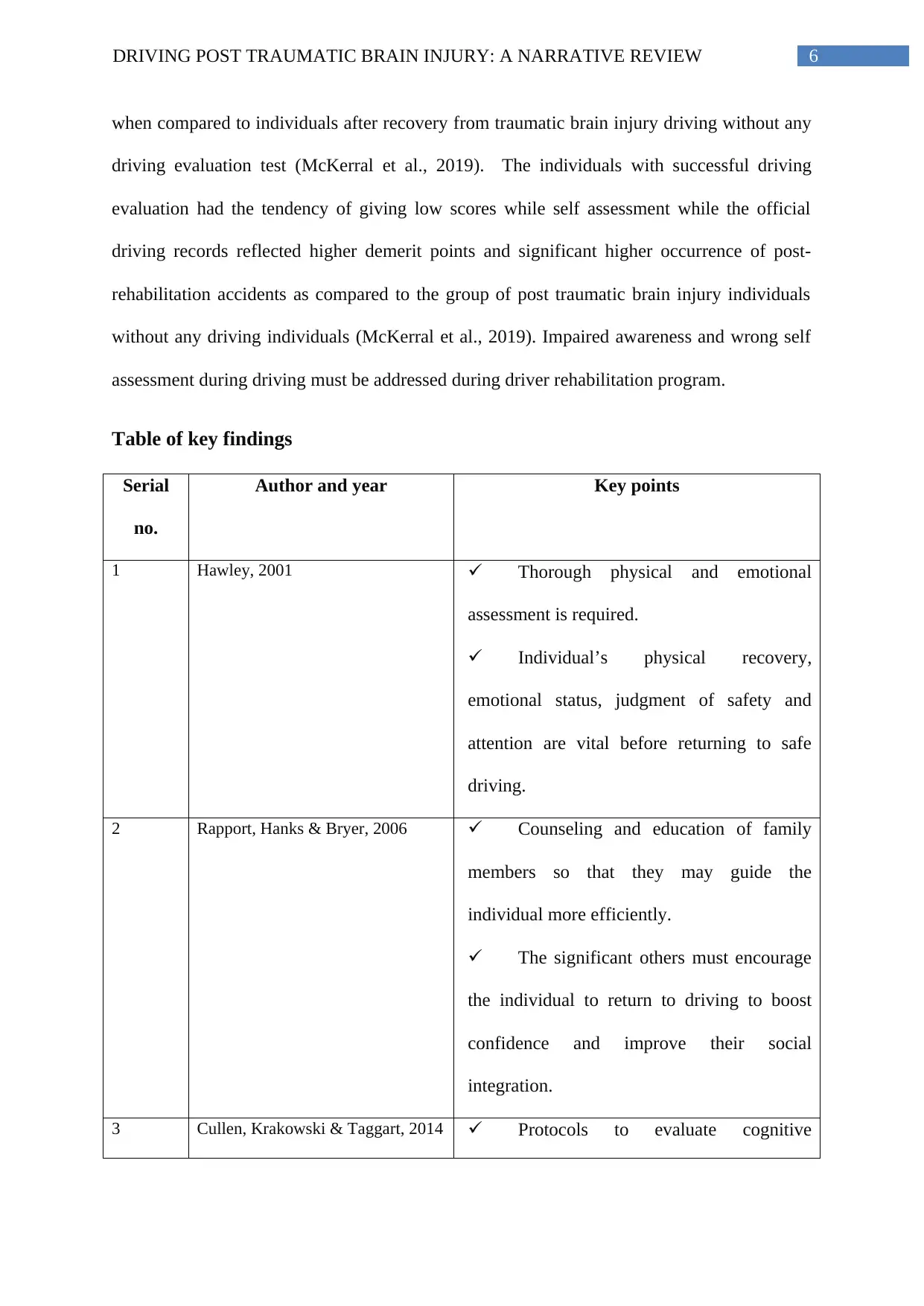
Table of key findings
Serial
no.
Author and year Key points
1 Hawley, 2001 Thorough physical and emotional
assessment is required.
Individual’s physical recovery,
emotional status, judgment of safety and
attention are vital before returning to safe
driving.
2 Rapport, Hanks & Bryer, 2006 Counseling and education of family
members so that they may guide the
individual more efficiently.
The significant others must encourage
the individual to return to driving to boost
confidence and improve their social
integration.
3 Cullen, Krakowski & Taggart, 2014 Protocols to evaluate cognitive
when compared to individuals after recovery from traumatic brain injury driving without any
driving evaluation test (McKerral et al., 2019). The individuals with successful driving
evaluation had the tendency of giving low scores while self assessment while the official
driving records reflected higher demerit points and significant higher occurrence of post-
rehabilitation accidents as compared to the group of post traumatic brain injury individuals
without any driving individuals (McKerral et al., 2019). Impaired awareness and wrong self
assessment during driving must be addressed during driver rehabilitation program.
Table of key findings
Serial
no.
Author and year Key points
1 Hawley, 2001 Thorough physical and emotional
assessment is required.
Individual’s physical recovery,
emotional status, judgment of safety and
attention are vital before returning to safe
driving.
2 Rapport, Hanks & Bryer, 2006 Counseling and education of family
members so that they may guide the
individual more efficiently.
The significant others must encourage
the individual to return to driving to boost
confidence and improve their social
integration.
3 Cullen, Krakowski & Taggart, 2014 Protocols to evaluate cognitive
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
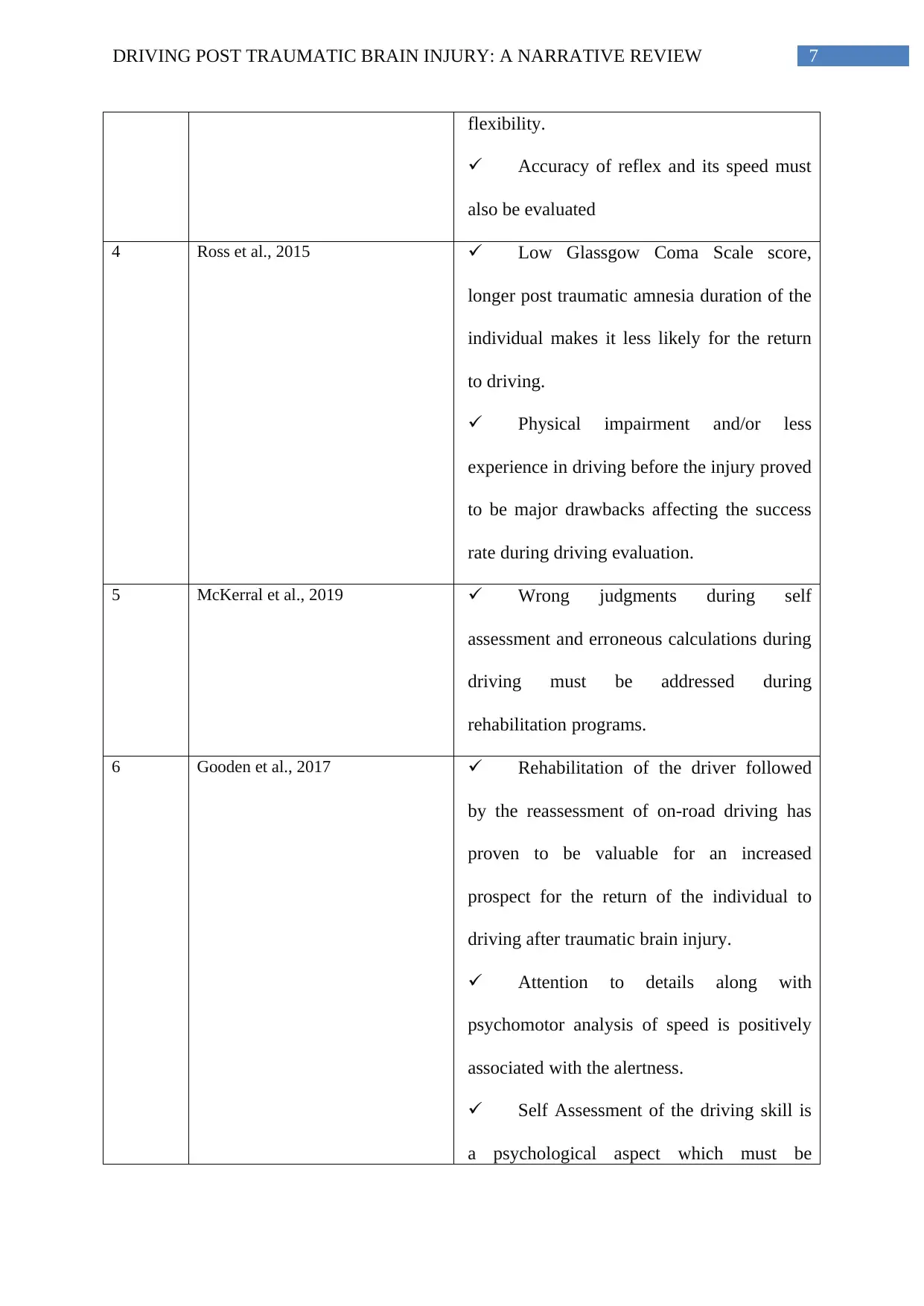
7DRIVING POST TRAUMATIC BRAIN INJURY: A NARRATIVE REVIEW
flexibility.
Accuracy of reflex and its speed must
also be evaluated
4 Ross et al., 2015 Low Glassgow Coma Scale score,
longer post traumatic amnesia duration of the
individual makes it less likely for the return
to driving.
Physical impairment and/or less
experience in driving before the injury proved
to be major drawbacks affecting the success
rate during driving evaluation.
5 McKerral et al., 2019 Wrong judgments during self
assessment and erroneous calculations during
driving must be addressed during
rehabilitation programs.
6 Gooden et al., 2017 Rehabilitation of the driver followed
by the reassessment of on-road driving has
proven to be valuable for an increased
prospect for the return of the individual to
driving after traumatic brain injury.
Attention to details along with
psychomotor analysis of speed is positively
associated with the alertness.
Self Assessment of the driving skill is
a psychological aspect which must be
flexibility.
Accuracy of reflex and its speed must
also be evaluated
4 Ross et al., 2015 Low Glassgow Coma Scale score,
longer post traumatic amnesia duration of the
individual makes it less likely for the return
to driving.
Physical impairment and/or less
experience in driving before the injury proved
to be major drawbacks affecting the success
rate during driving evaluation.
5 McKerral et al., 2019 Wrong judgments during self
assessment and erroneous calculations during
driving must be addressed during
rehabilitation programs.
6 Gooden et al., 2017 Rehabilitation of the driver followed
by the reassessment of on-road driving has
proven to be valuable for an increased
prospect for the return of the individual to
driving after traumatic brain injury.
Attention to details along with
psychomotor analysis of speed is positively
associated with the alertness.
Self Assessment of the driving skill is
a psychological aspect which must be
8DRIVING POST TRAUMATIC BRAIN INJURY: A NARRATIVE REVIEW
evaluated before on-road driving.
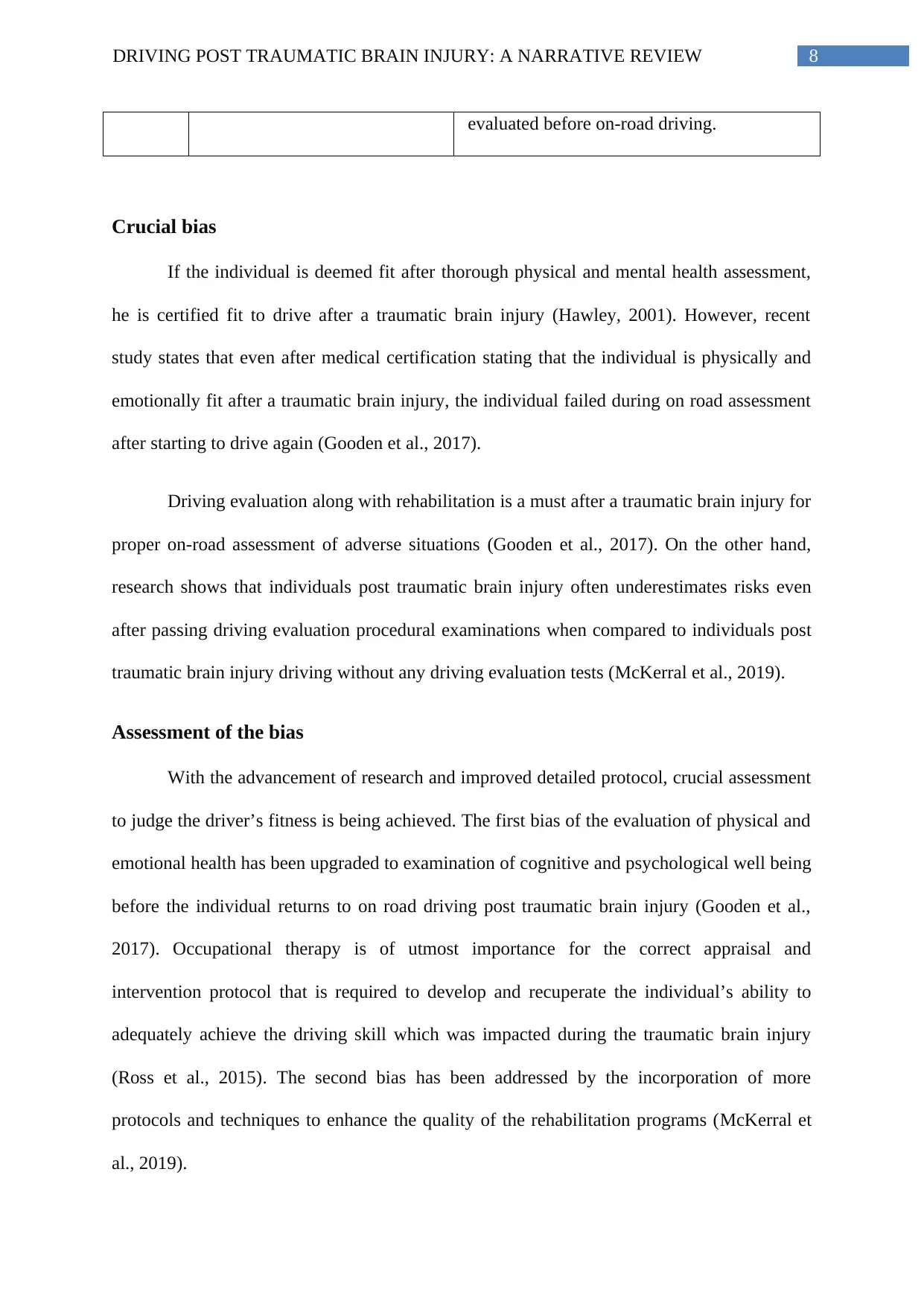
Crucial bias
If the individual is deemed fit after thorough physical and mental health assessment,
he is certified fit to drive after a traumatic brain injury (Hawley, 2001). However, recent
study states that even after medical certification stating that the individual is physically and
emotionally fit after a traumatic brain injury, the individual failed during on road assessment
after starting to drive again (Gooden et al., 2017).
Driving evaluation along with rehabilitation is a must after a traumatic brain injury for
proper on-road assessment of adverse situations (Gooden et al., 2017). On the other hand,
research shows that individuals post traumatic brain injury often underestimates risks even
after passing driving evaluation procedural examinations when compared to individuals post
traumatic brain injury driving without any driving evaluation tests (McKerral et al., 2019).
Assessment of the bias
With the advancement of research and improved detailed protocol, crucial assessment
to judge the driver’s fitness is being achieved. The first bias of the evaluation of physical and
emotional health has been upgraded to examination of cognitive and psychological well being
before the individual returns to on road driving post traumatic brain injury (Gooden et al.,
2017). Occupational therapy is of utmost importance for the correct appraisal and
intervention protocol that is required to develop and recuperate the individual’s ability to
adequately achieve the driving skill which was impacted during the traumatic brain injury
(Ross et al., 2015). The second bias has been addressed by the incorporation of more
protocols and techniques to enhance the quality of the rehabilitation programs (McKerral et
al., 2019).
evaluated before on-road driving.
Crucial bias
If the individual is deemed fit after thorough physical and mental health assessment,
he is certified fit to drive after a traumatic brain injury (Hawley, 2001). However, recent
study states that even after medical certification stating that the individual is physically and
emotionally fit after a traumatic brain injury, the individual failed during on road assessment
after starting to drive again (Gooden et al., 2017).
Driving evaluation along with rehabilitation is a must after a traumatic brain injury for
proper on-road assessment of adverse situations (Gooden et al., 2017). On the other hand,
research shows that individuals post traumatic brain injury often underestimates risks even
after passing driving evaluation procedural examinations when compared to individuals post
traumatic brain injury driving without any driving evaluation tests (McKerral et al., 2019).
Assessment of the bias
With the advancement of research and improved detailed protocol, crucial assessment
to judge the driver’s fitness is being achieved. The first bias of the evaluation of physical and
emotional health has been upgraded to examination of cognitive and psychological well being
before the individual returns to on road driving post traumatic brain injury (Gooden et al.,
2017). Occupational therapy is of utmost importance for the correct appraisal and
intervention protocol that is required to develop and recuperate the individual’s ability to
adequately achieve the driving skill which was impacted during the traumatic brain injury
(Ross et al., 2015). The second bias has been addressed by the incorporation of more
protocols and techniques to enhance the quality of the rehabilitation programs (McKerral et
al., 2019).
9DRIVING POST TRAUMATIC BRAIN INJURY: A NARRATIVE REVIEW
Discussion
Driving being a fine skill, aspects of which are controlled by various sections of the
brain, traumatic brain injury impacts the efficiency of the driving ability and the precise skills
required for the proper execution along with competent performance. A comprehensive
physical and emotional estimation is required before the individual returns to driving
following an injury to the head (Hawley, 2001). The protocols to evaluate the cognitive
flexibility and the reflex speed are imperative before the individual returns to on-road driving,
(Cullen, Krakowski & Taggart, 2014). High score on the Glassgow Coma Scale along with
short interval of post traumatic amnesia are good signs for the individual’s successful
accomplishment of on road driving whereas physical impairment and/or less experience in
driving before the injury proved to be major drawbacks affecting the rate of achievement
during driving evaluation (Ross et al., 2015).
Rehabilitation of the driver followed by the reassessment of on-road driving has
proven to be valuable for an increased prospect for the return of the individual to driving after
traumatic brain injury (Ross et al., 2015). The family members along with the significant
others must be educated so that they may provide better support and make community
integration easier for the individual after a traumatic brain injury as all these factors influence
independent driving (Rapport, Hanks & Bryer, 2006). The individuals who had failed in their
on-road assessment evaluation extensively overestimated their skills at on-road driving
(Gooden et al., 2017). The reduced self awareness during driving could be attributed to the
impairment of their cognitive function and should be addressed and focused on during the
rehabilitation programs so that miscalculations during driving can be reduced (McKerral et
al., 2019).
Discussion
Driving being a fine skill, aspects of which are controlled by various sections of the
brain, traumatic brain injury impacts the efficiency of the driving ability and the precise skills
required for the proper execution along with competent performance. A comprehensive
physical and emotional estimation is required before the individual returns to driving
following an injury to the head (Hawley, 2001). The protocols to evaluate the cognitive
flexibility and the reflex speed are imperative before the individual returns to on-road driving,
(Cullen, Krakowski & Taggart, 2014). High score on the Glassgow Coma Scale along with
short interval of post traumatic amnesia are good signs for the individual’s successful
accomplishment of on road driving whereas physical impairment and/or less experience in
driving before the injury proved to be major drawbacks affecting the rate of achievement
during driving evaluation (Ross et al., 2015).
Rehabilitation of the driver followed by the reassessment of on-road driving has
proven to be valuable for an increased prospect for the return of the individual to driving after
traumatic brain injury (Ross et al., 2015). The family members along with the significant
others must be educated so that they may provide better support and make community
integration easier for the individual after a traumatic brain injury as all these factors influence
independent driving (Rapport, Hanks & Bryer, 2006). The individuals who had failed in their
on-road assessment evaluation extensively overestimated their skills at on-road driving
(Gooden et al., 2017). The reduced self awareness during driving could be attributed to the
impairment of their cognitive function and should be addressed and focused on during the
rehabilitation programs so that miscalculations during driving can be reduced (McKerral et
al., 2019).
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
10DRIVING POST TRAUMATIC BRAIN INJURY: A NARRATIVE REVIEW
Limitations
The main limitations of the studies incorporated in this review as follows.
1. The sample sizes taken for the research are relatively small
2. The sample data collected are primarily from urban samples
3. The predominant urban samples have lead to a generalization of the findings which
must be revisited before implying any policy that might impact the entire population.
Thus these findings must be replicated with a bigger sample size and including urban,
suburban and rural populations if possible.
Implications of the study
Extensive physical and psychological analysis followed by rehabilitation which
carefully assesses the cognitive and qualitative skills of driving are required before the
individual with traumatic brain injury can return to independent safe on-road driving. The
study implies the importance occupational therapy and its significance in the correct analysis
and judgment along with introducing various intervention protocols that is mandatory to
develop and restoration of the ability of the individual to effectively achieve the driving skill
which was hampered during the traumatic brain injury.
Conclusion
Therefore, in conclusion it can be noted that the modus operandi to evaluate the
physical capability and emotional outcomes along with cognitive flexibility and the reflex
speed are imperative before the individual returns to on-road driving. High Glassgow Coma
Scale score with a small period of post traumatic amnesia are good indicators suggesting high
possibility of the individual’s return to on-road driving whereas physical impairment and/or
less experience in driving before the might lower the chances of successful return to driving
Limitations
The main limitations of the studies incorporated in this review as follows.
1. The sample sizes taken for the research are relatively small
2. The sample data collected are primarily from urban samples
3. The predominant urban samples have lead to a generalization of the findings which
must be revisited before implying any policy that might impact the entire population.
Thus these findings must be replicated with a bigger sample size and including urban,
suburban and rural populations if possible.
Implications of the study
Extensive physical and psychological analysis followed by rehabilitation which
carefully assesses the cognitive and qualitative skills of driving are required before the
individual with traumatic brain injury can return to independent safe on-road driving. The
study implies the importance occupational therapy and its significance in the correct analysis
and judgment along with introducing various intervention protocols that is mandatory to
develop and restoration of the ability of the individual to effectively achieve the driving skill
which was hampered during the traumatic brain injury.
Conclusion
Therefore, in conclusion it can be noted that the modus operandi to evaluate the
physical capability and emotional outcomes along with cognitive flexibility and the reflex
speed are imperative before the individual returns to on-road driving. High Glassgow Coma
Scale score with a small period of post traumatic amnesia are good indicators suggesting high
possibility of the individual’s return to on-road driving whereas physical impairment and/or
less experience in driving before the might lower the chances of successful return to driving
11DRIVING POST TRAUMATIC BRAIN INJURY: A NARRATIVE REVIEW
post traumatic brain injury. Proper guided rehabilitation of the driver followed by the
reassessment of on-road driving has proven to be valuable for an increased prospect for the
return of the individual to driving along with constant support and care from the family
members and significant others to achieve independent driving and successful social
integration into the community. Thus, interventions of occupational therapy and detailed
rehabilitation program with assessment of driving skill on road are vital key points for the
successful return of the individual post traumatic brain injury.
References
Ross, P. E., Ponsford, J. L., Di Stefano, M., & Spitz, G. (2015). Predictors of on-road driver
performance following traumatic brain injury. Archives of physical medicine and
rehabilitation, 96(3), 440-446.
McKerral, M., Moreno, A., Delhomme, P., & Gélinas, I. (2019). Driving Behaviors 2–3
Years After Traumatic Brain Injury Rehabilitation: A Multicenter Case-Control
Study. Frontiers in neurology, 10.
Cullen, N., Krakowski, A., & Taggart, C. (2014). Early neuropsychological tests as correlates
of return to driving after traumatic brain injury. Brain injury, 28(1), 38-43.
Rapport, L. J., Hanks, R. A., & Bryer, R. C. (2006). Barriers to driving and community
integration after traumatic brain injury. The Journal of head trauma rehabilitation, 21(1), 34-
44.
Hawley, C. A. (2001). Return to driving after head injury. Journal of Neurology,
Neurosurgery & Psychiatry, 70(6), 761-766.
post traumatic brain injury. Proper guided rehabilitation of the driver followed by the
reassessment of on-road driving has proven to be valuable for an increased prospect for the
return of the individual to driving along with constant support and care from the family
members and significant others to achieve independent driving and successful social
integration into the community. Thus, interventions of occupational therapy and detailed
rehabilitation program with assessment of driving skill on road are vital key points for the
successful return of the individual post traumatic brain injury.
References
Ross, P. E., Ponsford, J. L., Di Stefano, M., & Spitz, G. (2015). Predictors of on-road driver
performance following traumatic brain injury. Archives of physical medicine and
rehabilitation, 96(3), 440-446.
McKerral, M., Moreno, A., Delhomme, P., & Gélinas, I. (2019). Driving Behaviors 2–3
Years After Traumatic Brain Injury Rehabilitation: A Multicenter Case-Control
Study. Frontiers in neurology, 10.
Cullen, N., Krakowski, A., & Taggart, C. (2014). Early neuropsychological tests as correlates
of return to driving after traumatic brain injury. Brain injury, 28(1), 38-43.
Rapport, L. J., Hanks, R. A., & Bryer, R. C. (2006). Barriers to driving and community
integration after traumatic brain injury. The Journal of head trauma rehabilitation, 21(1), 34-
44.
Hawley, C. A. (2001). Return to driving after head injury. Journal of Neurology,
Neurosurgery & Psychiatry, 70(6), 761-766.
12DRIVING POST TRAUMATIC BRAIN INJURY: A NARRATIVE REVIEW
Gooden, J. R., Ponsford, J. L., Charlton, J. L., Ross, P. E., Marshall, S., Gagnon, S., ... &
Stolwyk, R. J. (2017). Self-awareness and self-ratings of on-road driving performance after
traumatic brain injury. Journal of head trauma rehabilitation, 32(1), E50-E59.
Allen, H. K., Beck, K. H., & Zanjani, F. (2019). Driving concerns among older adults:
Associations with driving skill, behaviors, and experiences. Traffic injury prevention, 20(1),
45-51.
Coleman, R. D., Rapport, L. J., Ergh, T. C., Hanks, R. A., Ricker, J. H., & Millis, S. R.
(2002). Predictors of driving outcome after traumatic brain injury. Archives of Physical
Medicine and Rehabilitation, 83(10), 1415-1422.
Navarro, J., Osiurak, F., & Reynaud, E. (2018). Neuroergonomics of car driving: A critical
meta-analysis of neuroimaging data on the human brain behind the wheel. Neuroscience &
Biobehavioral Reviews.
Gooden, J. R., Ponsford, J. L., Charlton, J. L., Ross, P. E., Marshall, S., Gagnon, S., ... &
Stolwyk, R. J. (2017). Self-awareness and self-ratings of on-road driving performance after
traumatic brain injury. Journal of head trauma rehabilitation, 32(1), E50-E59.
Allen, H. K., Beck, K. H., & Zanjani, F. (2019). Driving concerns among older adults:
Associations with driving skill, behaviors, and experiences. Traffic injury prevention, 20(1),
45-51.
Coleman, R. D., Rapport, L. J., Ergh, T. C., Hanks, R. A., Ricker, J. H., & Millis, S. R.
(2002). Predictors of driving outcome after traumatic brain injury. Archives of Physical
Medicine and Rehabilitation, 83(10), 1415-1422.
Navarro, J., Osiurak, F., & Reynaud, E. (2018). Neuroergonomics of car driving: A critical
meta-analysis of neuroimaging data on the human brain behind the wheel. Neuroscience &
Biobehavioral Reviews.
1 out of 13
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.