Common Medical Condition Case study 2022
VerifiedAdded on 2022/08/12
|53
|7721
|10
AI Summary
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: LITERATURE REVIEW
LITERATURE REVIEW
Name of the Student:
Name of the University:
Author’s Note:
LITERATURE REVIEW
Name of the Student:
Name of the University:
Author’s Note:
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Is it necessary to give antipsychotics drugs to reduce delirium in the elderly
postoperative?
Introduction
Delirium is one of the common medical condition that is encountered in the world
because of which people consult psychiatrists. Liu et al. (2019) opined that delirium is a
disturbance of consciousness that leads to a reduction in concentration, change in cognitive
ability and perceptual disturbance. It can be predicted that 10 to 15% of mentally ill patients
are delirious and 30 to 50% of the acutely ill geriatric patient have this disorder at some point
in their lives (Wan and Chase 2017).
The phenomenon of postoperative delirium is mostly observed in elderly individuals
who have been a part of a surgical procedure recently (Sarpal et al. 2016). The prevalence of
experiencing delirium in elderly patients is high because of the decreasing capacity of the
individuals to comprehend the reason for delirium. Hence, for the appropriate treatment,
antipsychotic drugs are used which act as antidepressant drugs allowing the nervous system
to calm down as a result of which, the patient can be managed and controlled in an effective
manner (Sarpal et al. 2016). Therefore, the administration of antipsychotic drugs is important
for delirious patient is effective in nature.
The use of the medication among delirious patients is relatively a new aspect in my
mental health facility. It involves considering the impact of antipsychotic drugs on delirium
patients, especially among elderly post-operative patients, undergoing an operation. Hence, a
literature review has been conducted for gaining in-depth information in understanding its
effectiveness and efficacy level in managing the issues.
postoperative?
Introduction
Delirium is one of the common medical condition that is encountered in the world
because of which people consult psychiatrists. Liu et al. (2019) opined that delirium is a
disturbance of consciousness that leads to a reduction in concentration, change in cognitive
ability and perceptual disturbance. It can be predicted that 10 to 15% of mentally ill patients
are delirious and 30 to 50% of the acutely ill geriatric patient have this disorder at some point
in their lives (Wan and Chase 2017).
The phenomenon of postoperative delirium is mostly observed in elderly individuals
who have been a part of a surgical procedure recently (Sarpal et al. 2016). The prevalence of
experiencing delirium in elderly patients is high because of the decreasing capacity of the
individuals to comprehend the reason for delirium. Hence, for the appropriate treatment,
antipsychotic drugs are used which act as antidepressant drugs allowing the nervous system
to calm down as a result of which, the patient can be managed and controlled in an effective
manner (Sarpal et al. 2016). Therefore, the administration of antipsychotic drugs is important
for delirious patient is effective in nature.
The use of the medication among delirious patients is relatively a new aspect in my
mental health facility. It involves considering the impact of antipsychotic drugs on delirium
patients, especially among elderly post-operative patients, undergoing an operation. Hence, a
literature review has been conducted for gaining in-depth information in understanding its
effectiveness and efficacy level in managing the issues.
Method
For conducting the literature review, an electronic search was undertaken in various
databases such as ProQuest Health and Medical Complete, Cumulative Index to Nursing and
Allied Health Literature (CINAHL) and Cochrane database were used. The search items that
have been used were ‘delirium’ ‘antipsychotic drug’, ‘post-operative delirium’, ‘haloperidol’,
‘model of care’, ‘pharmacologic management’ and ‘drug therapy’. For ensuring that the
literature was significant to the current practice, inclusion criteria were not included that
involve journal articles were peer-reviewed, were published after 2014, need to be in English
and the full text was available. The reference list of the articles was reviewed to seek for
addition and relevant information related to the subject topic. In addition to this, the selection
of the articles used for the review was based on the level of evidence hierarchy, includes
systematic studies, meta-analysis, and cohort studies, and randomised control trials.
Each of the literature was individually evaluated to understand the efficacy of the
antipsychotic drugs on the patients suffering from delirium and the population was adults.
This helps in understanding management strategies used among the patient population to
address the issues exhibited by the disorder upon the brain functioning as well as the
cognitive behaviour of patients.
Background
Older surgical patients often experience postoperative delirium (POD) and
postoperative cognitive dysfunction (POCD) growth afterwards. Medical characteristics
include impairment of memory, concentration disturbance and decreased environmental
awareness, resulting in increased morbidity, mortality and increased use of social, financial
support (Androsova et al. 2015). The ageing Western societies could expect the incidence of
POD and POCD to increase. Due to their societal burden, the underlying pathophysiological
For conducting the literature review, an electronic search was undertaken in various
databases such as ProQuest Health and Medical Complete, Cumulative Index to Nursing and
Allied Health Literature (CINAHL) and Cochrane database were used. The search items that
have been used were ‘delirium’ ‘antipsychotic drug’, ‘post-operative delirium’, ‘haloperidol’,
‘model of care’, ‘pharmacologic management’ and ‘drug therapy’. For ensuring that the
literature was significant to the current practice, inclusion criteria were not included that
involve journal articles were peer-reviewed, were published after 2014, need to be in English
and the full text was available. The reference list of the articles was reviewed to seek for
addition and relevant information related to the subject topic. In addition to this, the selection
of the articles used for the review was based on the level of evidence hierarchy, includes
systematic studies, meta-analysis, and cohort studies, and randomised control trials.
Each of the literature was individually evaluated to understand the efficacy of the
antipsychotic drugs on the patients suffering from delirium and the population was adults.
This helps in understanding management strategies used among the patient population to
address the issues exhibited by the disorder upon the brain functioning as well as the
cognitive behaviour of patients.
Background
Older surgical patients often experience postoperative delirium (POD) and
postoperative cognitive dysfunction (POCD) growth afterwards. Medical characteristics
include impairment of memory, concentration disturbance and decreased environmental
awareness, resulting in increased morbidity, mortality and increased use of social, financial
support (Androsova et al. 2015). The ageing Western societies could expect the incidence of
POD and POCD to increase. Due to their societal burden, the underlying pathophysiological
mechanisms were studied at the molecular level though with unsatisfactory little research
efforts. The multifactorial cause of delirium and its complex pathophysiology have made
prevention and treatment difficult. Pain, its opioid treatment and the inflammatory response
to injury in surgical patients are all possible risk factors for delirium. A significant
development for perioperative treatment would be a drug that both offers analgesia and
avoids delirium.
As per the 2013 Pain, Agitation and Delirium (PAD) Guidelines of the American
College of Critical Care Medicines, there is no symptomatic target management of the
disorder as there is a lack of compelling data. However, the guidelines state that atypical
antipsychotics can be used for reducing the time of delirium to a low level. Antipsychotic
drugs are found to block the dopamine D2 receptors that are present in the dopaminergic
pathways in the brain, thus, reducing the effect of dopamine. Rivière et al. (2019) opined that
the release of excess dopamine in the mesolimbic pathway is associated with psychotic
episodes. In the case of bipolar disorder and schizophrenia, there is decreased production of
dopamine in the prefrontal cortex and more production in other pathways in postoperative
patients.
Furthermore, antipsychotic has an antagonising effect on 5-HT2A receptors. The
different alleles of the receptors are observed to have associated with different mental
conditions such as psychosis, schizophrenia and depression. Fontaine et al. (2018) opined
that a higher concentration of the receptors particular in the cortical and subcortical areas in
the right caudate nucleus that was previously recorded.
Discussion
Identification of Delirium
efforts. The multifactorial cause of delirium and its complex pathophysiology have made
prevention and treatment difficult. Pain, its opioid treatment and the inflammatory response
to injury in surgical patients are all possible risk factors for delirium. A significant
development for perioperative treatment would be a drug that both offers analgesia and
avoids delirium.
As per the 2013 Pain, Agitation and Delirium (PAD) Guidelines of the American
College of Critical Care Medicines, there is no symptomatic target management of the
disorder as there is a lack of compelling data. However, the guidelines state that atypical
antipsychotics can be used for reducing the time of delirium to a low level. Antipsychotic
drugs are found to block the dopamine D2 receptors that are present in the dopaminergic
pathways in the brain, thus, reducing the effect of dopamine. Rivière et al. (2019) opined that
the release of excess dopamine in the mesolimbic pathway is associated with psychotic
episodes. In the case of bipolar disorder and schizophrenia, there is decreased production of
dopamine in the prefrontal cortex and more production in other pathways in postoperative
patients.
Furthermore, antipsychotic has an antagonising effect on 5-HT2A receptors. The
different alleles of the receptors are observed to have associated with different mental
conditions such as psychosis, schizophrenia and depression. Fontaine et al. (2018) opined
that a higher concentration of the receptors particular in the cortical and subcortical areas in
the right caudate nucleus that was previously recorded.
Discussion
Identification of Delirium
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Delirium is one of the primary cause of mortality and morbidity in hospitalised
elderly patients, those who have dementia. Marcantonio (2017) opined that this is a
vulnerable group because due to low immune system, they acquire various conditions such as
hospital-acquired infection, nutritional issue, pressure, immobility, increase cost of healthcare
services, more extended stay in hospital and long term care after discharge. According to the
study conducted by Oh et al. (2017), 10014 admissions in the acute medical unit indicated
that the prevalence of delirium was 24.6% among patients above the age of 65 years and
7.9% on dementia patients. The concern of the disorder needs to be treated in an effective
manner. From the discussion of Oberai et al. (2018), the advance in diagnosis includes brief
screening tools such as 3-Minute Diagnostic Assessment, 4A’s test and proxy-based
measurement. These supported in monitoring the response to treatment, risk stratification and
prevention of symptoms. This indicates that advances in the diagnosis process help in early
recognition and risk identification of delirium. In another study by Mulkey, Olson and Hardin
(2019), nurse prevention and intervention strategies were stated that have evidence of
practice and its effectiveness. The four intervention includes day and night routine, early
mobility, reducing sensory impairment and reorientation. The use of evidence-informed
management requires an individualised and multi-component approach for restoring the
physiological functions of patients. According to a specific study by Lam and Gandell
(2018), it was found that the nurse-led the care process in Britain and pre-operative
assessment was not the structure of Canadian pre-operative clinics among the high-risk
vascular patients. The evidence for reduced length of stay using assessment of the
preoperative comprehensive geriatric patient in the vascular surgical setting.
Risk factors and outcome
The use of systematic review that involves 26442 old patients with the help of semi-
quantitative analysis was conducted for evaluating the risk factors and outcomes of deliriums
elderly patients, those who have dementia. Marcantonio (2017) opined that this is a
vulnerable group because due to low immune system, they acquire various conditions such as
hospital-acquired infection, nutritional issue, pressure, immobility, increase cost of healthcare
services, more extended stay in hospital and long term care after discharge. According to the
study conducted by Oh et al. (2017), 10014 admissions in the acute medical unit indicated
that the prevalence of delirium was 24.6% among patients above the age of 65 years and
7.9% on dementia patients. The concern of the disorder needs to be treated in an effective
manner. From the discussion of Oberai et al. (2018), the advance in diagnosis includes brief
screening tools such as 3-Minute Diagnostic Assessment, 4A’s test and proxy-based
measurement. These supported in monitoring the response to treatment, risk stratification and
prevention of symptoms. This indicates that advances in the diagnosis process help in early
recognition and risk identification of delirium. In another study by Mulkey, Olson and Hardin
(2019), nurse prevention and intervention strategies were stated that have evidence of
practice and its effectiveness. The four intervention includes day and night routine, early
mobility, reducing sensory impairment and reorientation. The use of evidence-informed
management requires an individualised and multi-component approach for restoring the
physiological functions of patients. According to a specific study by Lam and Gandell
(2018), it was found that the nurse-led the care process in Britain and pre-operative
assessment was not the structure of Canadian pre-operative clinics among the high-risk
vascular patients. The evidence for reduced length of stay using assessment of the
preoperative comprehensive geriatric patient in the vascular surgical setting.
Risk factors and outcome
The use of systematic review that involves 26442 old patients with the help of semi-
quantitative analysis was conducted for evaluating the risk factors and outcomes of deliriums
subtype (Krewulak et al. 2020). The risk factors that are taken into consideration include age,
sex and APACHE-II score and outcome include mechanical ventilation, mortality, and length
of hospital stay, tube removal and delirium duration. However, due to different aspects of
both reporting and limitation in methodical quality has restricted the generalisation of the
result and the evidence for various subtype-specific risk factors or the outcomes thus, making
it inconsistent among the studies. Kim et al. (2018) noted the persistent episodes of delirium
is found to have a negative impact on the patients because of it. The differences in an
underlying chronic condition that accounts for the difference in the discharge duration and
condition between medical ill patients and patients undergoing surgical suffering from
delirium. However, the disorders are commonly superimposed on dementia as a result which,
the identification process is delayed resulting in no or delayed treatment (Mulkey et al. 2018).
This has a profound impact on the patient’s recovery process and do not validates the care
setting. Thus, the limitations of the study are it was unable to identify the reason because of
which, the training provided was not appropriately addressed even though the assessment
tools were found to be promising in nature.
Use of Antipsychotic Drugs for treating Delirium
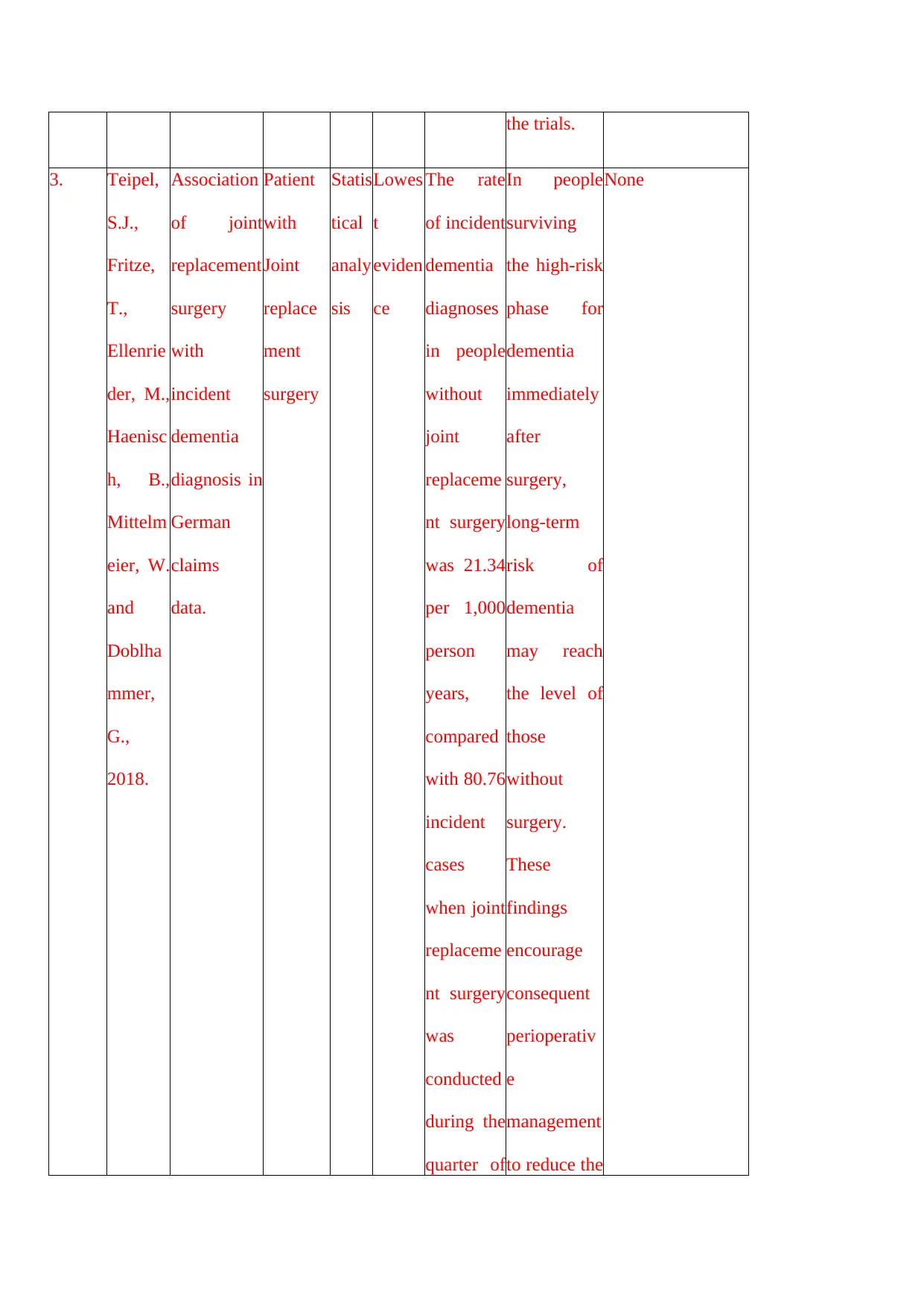
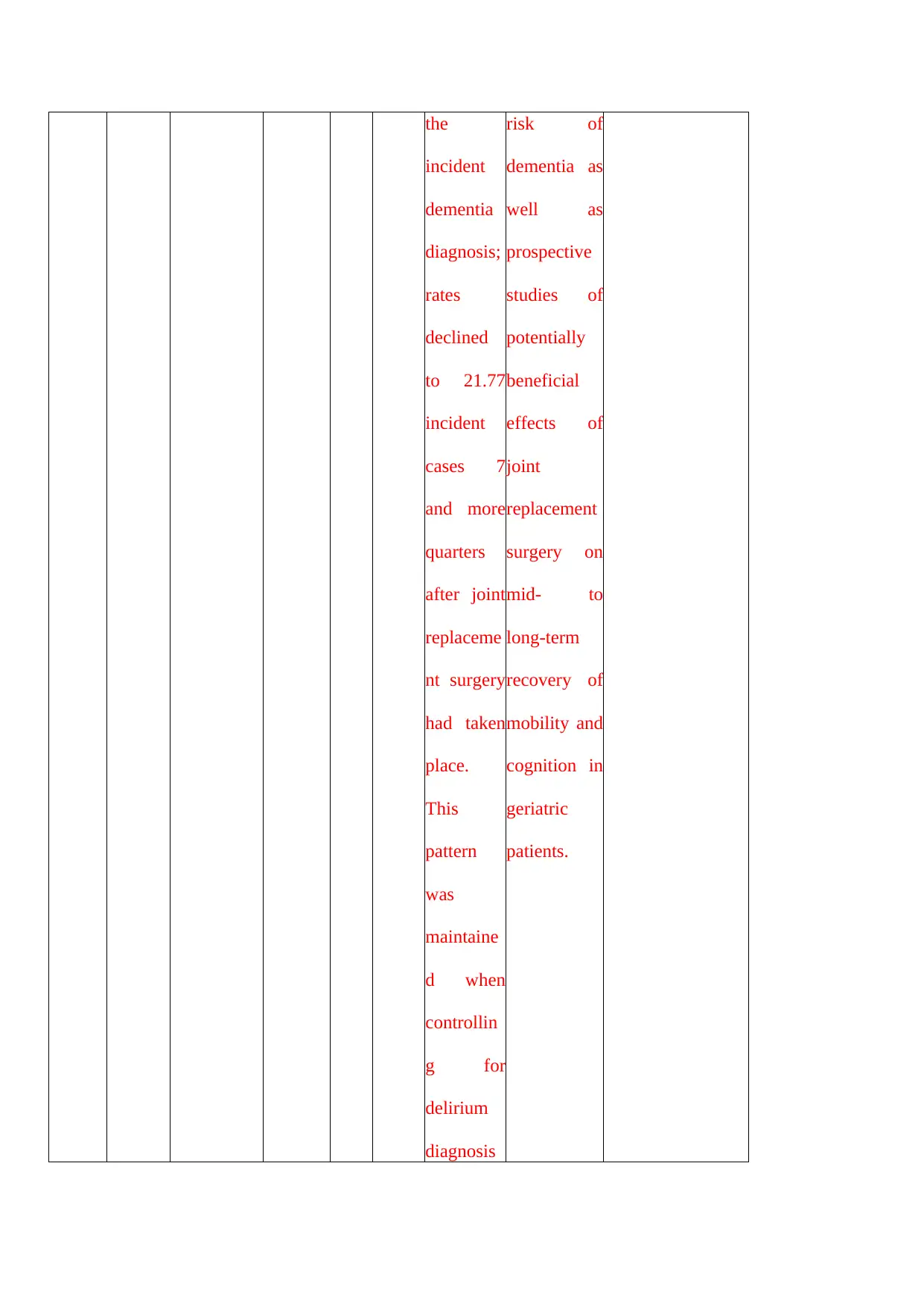
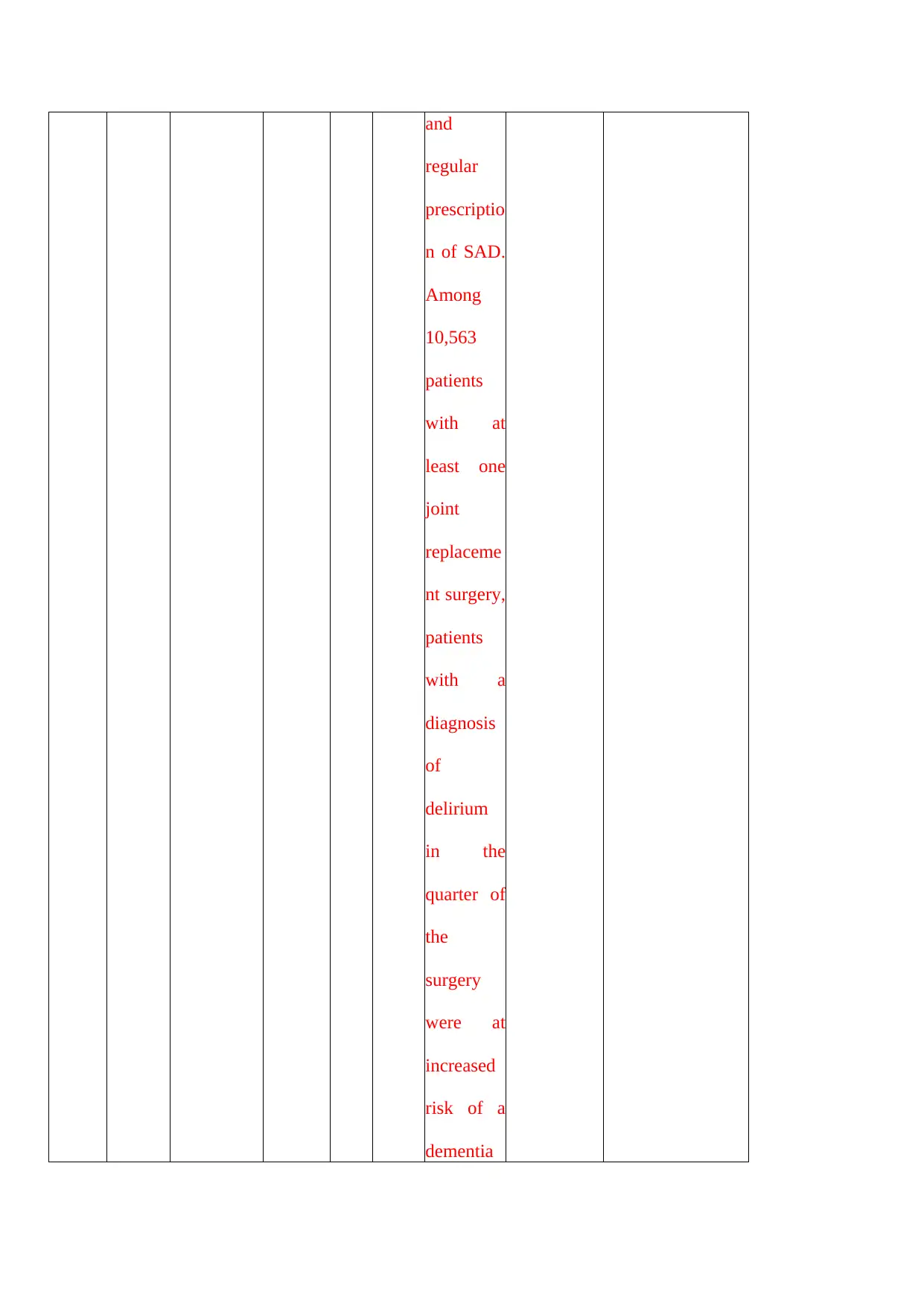
Teipel et al. (2018) noted that people that are at a high risk of dementia and
undergone surgery have a long-term risk. This may be involved in increasing the risk factor.
The finding of the paper had stated that perioperative management could be used for reducing
the risk factors and can have benefits in joint replacement surgery that led to long-term
mobility and cognition among older populations. Scholtens et al. (2016) conducted a
preliminary study for evaluating the occurrence of delirium in older patients undergoing hip
replacement surgery and the impact of preoperative Cerebrospinal Fluid (CSF) Melatonin
concentration on the specified group of people. Melatonin is used for regulating the circadian
rhythm, and since delirium has a feature of disturbed rhythmic action of circadian thus, it was
sex and APACHE-II score and outcome include mechanical ventilation, mortality, and length
of hospital stay, tube removal and delirium duration. However, due to different aspects of
both reporting and limitation in methodical quality has restricted the generalisation of the
result and the evidence for various subtype-specific risk factors or the outcomes thus, making
it inconsistent among the studies. Kim et al. (2018) noted the persistent episodes of delirium
is found to have a negative impact on the patients because of it. The differences in an
underlying chronic condition that accounts for the difference in the discharge duration and
condition between medical ill patients and patients undergoing surgical suffering from
delirium. However, the disorders are commonly superimposed on dementia as a result which,
the identification process is delayed resulting in no or delayed treatment (Mulkey et al. 2018).
This has a profound impact on the patient’s recovery process and do not validates the care
setting. Thus, the limitations of the study are it was unable to identify the reason because of
which, the training provided was not appropriately addressed even though the assessment
tools were found to be promising in nature.
Use of Antipsychotic Drugs for treating Delirium
Teipel et al. (2018) noted that people that are at a high risk of dementia and
undergone surgery have a long-term risk. This may be involved in increasing the risk factor.
The finding of the paper had stated that perioperative management could be used for reducing
the risk factors and can have benefits in joint replacement surgery that led to long-term
mobility and cognition among older populations. Scholtens et al. (2016) conducted a
preliminary study for evaluating the occurrence of delirium in older patients undergoing hip
replacement surgery and the impact of preoperative Cerebrospinal Fluid (CSF) Melatonin
concentration on the specified group of people. Melatonin is used for regulating the circadian
rhythm, and since delirium has a feature of disturbed rhythmic action of circadian thus, it was
thought upon that this drug would be useful in treating the patients. A cohort study was
undertaken upon 67 patients with hip fracture than are above the age of 65 years and were
administered with spinal anaesthesia. From the study, it was concluded that there was no
significant impact of the drug on the patients in term of cognitive impairment or age. Thus, it
clearly indicated that this antipsychotic drug was not useful in case of treating delirium.
Delirium is considered to be one of the common and severe postoperative complications
among people who are older than 60 years and have a high risk of mortality and morbidity. In
another study, the use of subanaesthia ketamine is stated to be administered in case of
intraoperative surgery as a postoperative analgesic and there were some evidence that
suggested that this drug help in preventing the signs of deliriums. A Prevention of Delirium
and Complications Associated with Surgical Treatment (PODCAST) study conducted by
Avidan et al. (2017) was done that involve randomised trials among the adults with 60 years
who had undergone cardiac and non-cardiac surgery which was undertaken general
anaesthesia. From the result, it was interpreted that a single sub anaesthetic dose of ketamine
was not effective in decreasing the disorder among the target population after the surgery and
in severe case, it can be seen that it might cause harm to the patients by inducing negative
experience thus, causing traumatic effect on the patients' population. Therefore, the use of
antipsychotic drugs, specifically ketamine, was not found to be effective in treating delirium
in case of postoperative patients that are above the age of 60 years.
Pahwa, Qureshi and Cumbler (2019) have undertaken case study analysis that
particularly addresses the reason because of which people use antipsychotic drugs and why it
is not useful among delirium patients. With respect to the case, it was observed that the use of
haloperidol was used for reducing the severity and duration of the disorder as well as shorten
the duration of hospitalisation due to hip surgery. There is evidence that states that 10-30% of
the patients had received antipsychotic drugs during the hospital stay due to delirium.
undertaken upon 67 patients with hip fracture than are above the age of 65 years and were
administered with spinal anaesthesia. From the study, it was concluded that there was no
significant impact of the drug on the patients in term of cognitive impairment or age. Thus, it
clearly indicated that this antipsychotic drug was not useful in case of treating delirium.
Delirium is considered to be one of the common and severe postoperative complications
among people who are older than 60 years and have a high risk of mortality and morbidity. In
another study, the use of subanaesthia ketamine is stated to be administered in case of
intraoperative surgery as a postoperative analgesic and there were some evidence that
suggested that this drug help in preventing the signs of deliriums. A Prevention of Delirium
and Complications Associated with Surgical Treatment (PODCAST) study conducted by
Avidan et al. (2017) was done that involve randomised trials among the adults with 60 years
who had undergone cardiac and non-cardiac surgery which was undertaken general
anaesthesia. From the result, it was interpreted that a single sub anaesthetic dose of ketamine
was not effective in decreasing the disorder among the target population after the surgery and
in severe case, it can be seen that it might cause harm to the patients by inducing negative
experience thus, causing traumatic effect on the patients' population. Therefore, the use of
antipsychotic drugs, specifically ketamine, was not found to be effective in treating delirium
in case of postoperative patients that are above the age of 60 years.
Pahwa, Qureshi and Cumbler (2019) have undertaken case study analysis that
particularly addresses the reason because of which people use antipsychotic drugs and why it
is not useful among delirium patients. With respect to the case, it was observed that the use of
haloperidol was used for reducing the severity and duration of the disorder as well as shorten
the duration of hospitalisation due to hip surgery. There is evidence that states that 10-30% of
the patients had received antipsychotic drugs during the hospital stay due to delirium.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
However, the aspect of variability among the patterns of drugs was not understood that
resulted in conflicting results. A piece of evidence indicated that the fact that efficacy of these
drugs was not appropriate and there is an absence of persuasive evidence that indicated any
change in stay length in the hospital or the benefits of antipsychotic drugs in treating
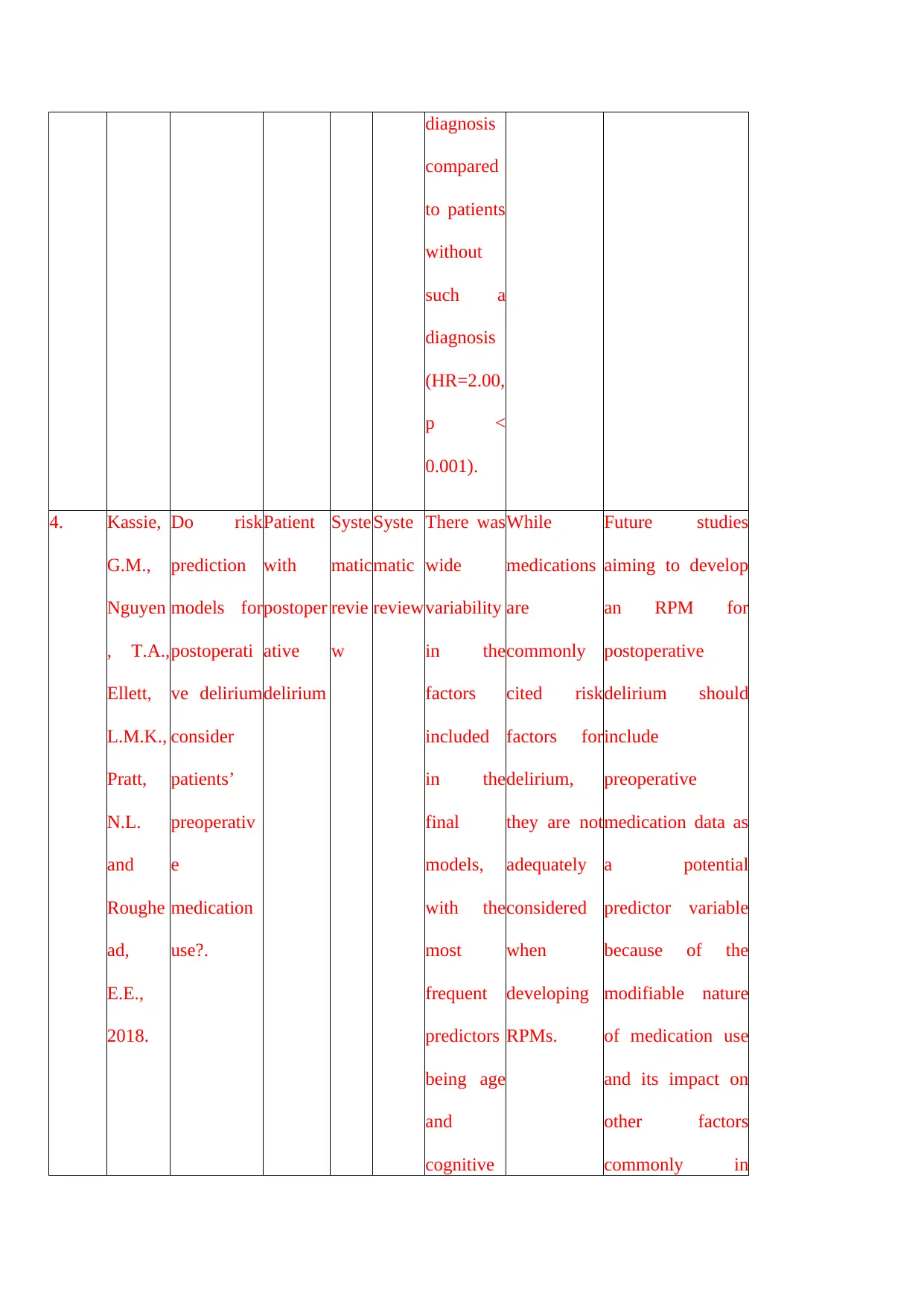
postoperative delirium. A study that was conducted by Kassie et al. (2018) stated that
medicines have the potential of risk factor in case of postoperative delirium. However, due to
inadequate evidence, the extent of the effectiveness of these drugs and the efficacy of the risk
prediction model (RPM) was not known. The use of systematic study was conducted that
supported in understanding the inclusion of preoperative medication in RPM for
postoperative delirium. It was found that even though the medications are commonly used,
however, these are not sufficiently considered in RPM; thus, there is a requirement of
developing an RPM in case of postoperative delirium for understanding the modifiable nature
as well as its impact on factors such as cognition. Tremblay and Gold (2016) had undertaken
a literature review for assessing the postoperative delirium (POD), which is found to be a
serious complication and caused a significant number of mortality and morbidity. In addition
to this, it also leads to various issues such as increases the cost of healthcare services, the
extension of the length of hospital stays; thus, there is a secondary complication after
postoperative delirium. The patient type and timing of the postoperative delirium are
observed to be associated with differential delirium outcome that suggested that fact that
targeted screening and use of interventional approaches are useful in handling the disorder.
From the extensive literature study, it was found that in 14 articles, evidence related to
reducing the incidence of postoperative delirium using pharmacological agent was found
where eight indicated the use of antipsychotic drugs, two with statins one with melatonin,
dexamethasone, gabapentin and diazepam respectively. As per the result, the issue of study
design, methods used and interpretation were found that has a negative impact on the
resulted in conflicting results. A piece of evidence indicated that the fact that efficacy of these
drugs was not appropriate and there is an absence of persuasive evidence that indicated any
change in stay length in the hospital or the benefits of antipsychotic drugs in treating
postoperative delirium. A study that was conducted by Kassie et al. (2018) stated that
medicines have the potential of risk factor in case of postoperative delirium. However, due to
inadequate evidence, the extent of the effectiveness of these drugs and the efficacy of the risk
prediction model (RPM) was not known. The use of systematic study was conducted that
supported in understanding the inclusion of preoperative medication in RPM for
postoperative delirium. It was found that even though the medications are commonly used,
however, these are not sufficiently considered in RPM; thus, there is a requirement of
developing an RPM in case of postoperative delirium for understanding the modifiable nature
as well as its impact on factors such as cognition. Tremblay and Gold (2016) had undertaken
a literature review for assessing the postoperative delirium (POD), which is found to be a
serious complication and caused a significant number of mortality and morbidity. In addition
to this, it also leads to various issues such as increases the cost of healthcare services, the
extension of the length of hospital stays; thus, there is a secondary complication after
postoperative delirium. The patient type and timing of the postoperative delirium are
observed to be associated with differential delirium outcome that suggested that fact that
targeted screening and use of interventional approaches are useful in handling the disorder.
From the extensive literature study, it was found that in 14 articles, evidence related to
reducing the incidence of postoperative delirium using pharmacological agent was found
where eight indicated the use of antipsychotic drugs, two with statins one with melatonin,
dexamethasone, gabapentin and diazepam respectively. As per the result, the issue of study
design, methods used and interpretation were found that has a negative impact on the
conclusion. This indicated that use of double-blinded randomised clinical trial needs to be
conducted for understanding the effectiveness of using pharmacological agents in reducing
POD. Oh et al. (2019) had initiated a study to understand the benefits and harms of the use
of psychotic drugs for reducing delirium where a systematic review was done. RCTs were
used for comparing the antipsychotic with placebo or other antipsychotic drugs, and it was
found that there was no difference in any of the variables in using antipsychotic drugs as
compared to placebo. The presence of different clinical characteristics pattern among the
older population of delirium were observed. This finding was relevant into the clinical care
with respect to acutely ill patients and proposed that there is the implication of different
pathways in the pathophysiology in delirium that need to be assessed for the development of
effective management of care. Haque, Naqvi and Dasgupta (2019) stated that due to POD,
there is a high rate of functional deaths. Thus, the use of Ondansetron, which is a serotonin
antagonist, could be used as a therapeutic option for the disorder. A systematic review using
valid and reliable database was used that included three RCTs that were selected in this case.
From the result, it was inferred that Ondansetron might be effective in case of treating or
preventing POD; however, the studies were not valid or reliable as it involves the poor
quality of studies which is responsible for making the conclusion more unsubstantiated in
nature. Therefore, the requirement of large RCTs will be required for understanding the
efficacy level of the drug in treating the disorder among adults’ especially old people that had
undergone cardiac or post-traumatic surgery in the ICU.
Management strategies for delirium
As per the study of Johnson et al. (2017), impatient geriatric patients that have
reversible conditions of delirium may continue to have antipsychotic medications after
hospital discharge. Thus, a retrospective chart review was conducted. It was observed that in
the healthcare system, most of the old population of patients with delirium are discharged
conducted for understanding the effectiveness of using pharmacological agents in reducing
POD. Oh et al. (2019) had initiated a study to understand the benefits and harms of the use
of psychotic drugs for reducing delirium where a systematic review was done. RCTs were
used for comparing the antipsychotic with placebo or other antipsychotic drugs, and it was
found that there was no difference in any of the variables in using antipsychotic drugs as
compared to placebo. The presence of different clinical characteristics pattern among the
older population of delirium were observed. This finding was relevant into the clinical care
with respect to acutely ill patients and proposed that there is the implication of different
pathways in the pathophysiology in delirium that need to be assessed for the development of
effective management of care. Haque, Naqvi and Dasgupta (2019) stated that due to POD,
there is a high rate of functional deaths. Thus, the use of Ondansetron, which is a serotonin
antagonist, could be used as a therapeutic option for the disorder. A systematic review using
valid and reliable database was used that included three RCTs that were selected in this case.
From the result, it was inferred that Ondansetron might be effective in case of treating or
preventing POD; however, the studies were not valid or reliable as it involves the poor
quality of studies which is responsible for making the conclusion more unsubstantiated in
nature. Therefore, the requirement of large RCTs will be required for understanding the
efficacy level of the drug in treating the disorder among adults’ especially old people that had
undergone cardiac or post-traumatic surgery in the ICU.
Management strategies for delirium
As per the study of Johnson et al. (2017), impatient geriatric patients that have
reversible conditions of delirium may continue to have antipsychotic medications after
hospital discharge. Thus, a retrospective chart review was conducted. It was observed that in
the healthcare system, most of the old population of patients with delirium are discharged
with a new antipsychotic drug where no instruction was outlined to the providers about
discontinuation management. As known, prolonged use of the drug have several negative
impacts and thus, require interventions that would help in offering more guidance related to
the antipsychotic medication at the transition of care. Finucane et al. (2020) stated that drug
therapy is one of the management for delirium. The use of RCTs for drug therapies in term of
dose by any route, which is a non-pharmacological approach. The studies had reported the
outcome that stated essential elements such as the symptoms of delirium such as agitation and
adverse events of the disorders. The drugs such as haloperidol, risperidone, olanzapine,
placebo, lorazepam and chlorpromazine. As per the study, it was not possible to combine the
data because of lack of similarity in them; as a result, low-quality evidence was observed that
stated drugs such as risperidone and haloperidol had worsened the symptoms of the disease
among terminally ill older patients that have mild to moderate delirium. Thus, further
research needs to be conducted for the determination of the negative impact of drug therapy
on the vulnerable population.
van den Boogaard et al. (2020) conducted a multinational cohort study that was
initiated in understanding the impact of sedation on delirium among critically illness people
where 1660 patients were assessed using Richmond Agitation-Sedation Scale along with
sedating medications. Logistic regression was used that aided in the analysis of the factors
that may potentially affect the level of sedation on the above-stated population. It was found
that the influence was dependent on the usage of the Intensive Care Delirium Screening
Checklist (ICDSU) or Confusion Assessment Method for the Intensive Care Unit (CAM-
ICU). In addition to this, ICU nurses were considered while assessing the level of sedation
among patients suffering from delirium. Thus, it was stated that future studies need to be
conducted that will help in comparing the CAM-ICU and the ICDSC in a simultaneous
manner to understand its effectiveness using a sample population and control group. Eeles et
discontinuation management. As known, prolonged use of the drug have several negative
impacts and thus, require interventions that would help in offering more guidance related to
the antipsychotic medication at the transition of care. Finucane et al. (2020) stated that drug
therapy is one of the management for delirium. The use of RCTs for drug therapies in term of
dose by any route, which is a non-pharmacological approach. The studies had reported the
outcome that stated essential elements such as the symptoms of delirium such as agitation and
adverse events of the disorders. The drugs such as haloperidol, risperidone, olanzapine,
placebo, lorazepam and chlorpromazine. As per the study, it was not possible to combine the
data because of lack of similarity in them; as a result, low-quality evidence was observed that
stated drugs such as risperidone and haloperidol had worsened the symptoms of the disease
among terminally ill older patients that have mild to moderate delirium. Thus, further
research needs to be conducted for the determination of the negative impact of drug therapy
on the vulnerable population.
van den Boogaard et al. (2020) conducted a multinational cohort study that was
initiated in understanding the impact of sedation on delirium among critically illness people
where 1660 patients were assessed using Richmond Agitation-Sedation Scale along with
sedating medications. Logistic regression was used that aided in the analysis of the factors
that may potentially affect the level of sedation on the above-stated population. It was found
that the influence was dependent on the usage of the Intensive Care Delirium Screening
Checklist (ICDSU) or Confusion Assessment Method for the Intensive Care Unit (CAM-
ICU). In addition to this, ICU nurses were considered while assessing the level of sedation
among patients suffering from delirium. Thus, it was stated that future studies need to be
conducted that will help in comparing the CAM-ICU and the ICDSC in a simultaneous
manner to understand its effectiveness using a sample population and control group. Eeles et
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.

al. (2020) opined that delirium is one of the major healthcare problems on a global scale and
have severe consequences where the use of sub-optimal management is a universal strategy.
The interval or gap found in the care process of the patients were observed to have
distinctiveness of the disorder as it affects oneself. The corruptive and violent behaviour of
the patient render harm to both selves as well as the external surrounding; thus, require
control over the symptoms, which place the individual at risk of mechanical dehumanisation
behaviour.
Conclusion
From the literature review, it was found that antipsychotic drugs are commonly used
among delirious patients. The most significant aspect of using this class of drug is because
there is less evidence that state the underlying factors and risks with respect to aetiology and
pathophysiology of the disease. Various other management plans have been developed with
respect to delirium among the older population and people suffering from critical illness;
however, the effectiveness of those care processes was not sufficient enough that would help
in limiting the use of antipsychotic drugs. The antipsychotic drugs do not have any evidence
related to its efficacy and effectiveness among the patient population. The focus was given on
postoperative delirium and the impact of antipsychotic drug in disorder, which was not
sufficiently addressed because of lack of evidence. The nursing practices were found to be in
conjunction with the identification and treatment of the disease among patient undergoing
surgeries. Due to lack of proper training related to the use of various assessment tools
available for early detection, the treatment process is hampered to a large extent. One of the
aspects that affect the care plan of postoperative delirium is due to lack of training and
shortage of skilled professional nurses; the condition is often mistaken with dementia. It is
responsible for delaying the process of care mainly that affect the use of antipsychotic drugs
among the specified target population in effectively treating the disorder.
have severe consequences where the use of sub-optimal management is a universal strategy.
The interval or gap found in the care process of the patients were observed to have
distinctiveness of the disorder as it affects oneself. The corruptive and violent behaviour of
the patient render harm to both selves as well as the external surrounding; thus, require
control over the symptoms, which place the individual at risk of mechanical dehumanisation
behaviour.
Conclusion
From the literature review, it was found that antipsychotic drugs are commonly used
among delirious patients. The most significant aspect of using this class of drug is because
there is less evidence that state the underlying factors and risks with respect to aetiology and
pathophysiology of the disease. Various other management plans have been developed with
respect to delirium among the older population and people suffering from critical illness;
however, the effectiveness of those care processes was not sufficient enough that would help
in limiting the use of antipsychotic drugs. The antipsychotic drugs do not have any evidence
related to its efficacy and effectiveness among the patient population. The focus was given on
postoperative delirium and the impact of antipsychotic drug in disorder, which was not
sufficiently addressed because of lack of evidence. The nursing practices were found to be in
conjunction with the identification and treatment of the disease among patient undergoing
surgeries. Due to lack of proper training related to the use of various assessment tools
available for early detection, the treatment process is hampered to a large extent. One of the
aspects that affect the care plan of postoperative delirium is due to lack of training and
shortage of skilled professional nurses; the condition is often mistaken with dementia. It is
responsible for delaying the process of care mainly that affect the use of antipsychotic drugs
among the specified target population in effectively treating the disorder.
References
Androsova, G., Krause, R., Winterer, G. and Schneider, R., 2015. Biomarkers of
postoperative delirium and cognitive dysfunction. Frontiers in aging neuroscience, 7, p.112.
Avidan, M.S., Maybrier, H.R., Abdallah, A.B., Jacobsohn, E., Vlisides, P.E., Pryor, K.O.,
Veselis, R.A., Grocott, H.P., Emmert, D.A., Rogers, E.M. and Downey, R.J., 2017.
Intraoperative ketamine for prevention of postoperative delirium or pain after major surgery
in older adults: an international, multicentre, double-blind, randomised clinical trial. The
Lancet, 390(10091), pp.267-275.
Eeles, E., England, R., Teodorczuk, A., Pandy, S., Pinsker, D. and Armstrong, A., 2020.
Delirium Management: Anything’s Possible. Canadian Journal on Aging/La Revue
canadienne du vieillissement, 39(1), pp.89-97.
Finucane, A.M., Jones, L., Leurent, B., Sampson, E.L., Stone, P., Tookman, A. and Candy,
B., 2020. Drug therapy for delirium in terminally ill adults. Cochrane Database of Systematic
Reviews, (1).
Fontaine, G.V., Mortensen, W., Guinto, K.M., Scott, D.M. and Miller III, R.R., 2018. Newly
initiated in-hospital antipsychotics continued at discharge in non-psychiatric
patients. Hospital pharmacy, 53(5), pp.308-315.
Haque, N., Naqvi, R.M. and Dasgupta, M., 2019. Efficacy of Ondansetron in the Prevention
or Treatment of Post-operative Delirium—a Systematic Review. Canadian Geriatrics
Journal, 22(1), p.1.
in diagnosis and treatment. Jama, 318(12), pp.1161-1174.
Androsova, G., Krause, R., Winterer, G. and Schneider, R., 2015. Biomarkers of
postoperative delirium and cognitive dysfunction. Frontiers in aging neuroscience, 7, p.112.
Avidan, M.S., Maybrier, H.R., Abdallah, A.B., Jacobsohn, E., Vlisides, P.E., Pryor, K.O.,
Veselis, R.A., Grocott, H.P., Emmert, D.A., Rogers, E.M. and Downey, R.J., 2017.
Intraoperative ketamine for prevention of postoperative delirium or pain after major surgery
in older adults: an international, multicentre, double-blind, randomised clinical trial. The
Lancet, 390(10091), pp.267-275.
Eeles, E., England, R., Teodorczuk, A., Pandy, S., Pinsker, D. and Armstrong, A., 2020.
Delirium Management: Anything’s Possible. Canadian Journal on Aging/La Revue
canadienne du vieillissement, 39(1), pp.89-97.
Finucane, A.M., Jones, L., Leurent, B., Sampson, E.L., Stone, P., Tookman, A. and Candy,
B., 2020. Drug therapy for delirium in terminally ill adults. Cochrane Database of Systematic
Reviews, (1).
Fontaine, G.V., Mortensen, W., Guinto, K.M., Scott, D.M. and Miller III, R.R., 2018. Newly
initiated in-hospital antipsychotics continued at discharge in non-psychiatric
patients. Hospital pharmacy, 53(5), pp.308-315.
Haque, N., Naqvi, R.M. and Dasgupta, M., 2019. Efficacy of Ondansetron in the Prevention
or Treatment of Post-operative Delirium—a Systematic Review. Canadian Geriatrics
Journal, 22(1), p.1.
in diagnosis and treatment. Jama, 318(12), pp.1161-1174.
Johnson, K.G., Fashoyin, A., Madden‐Fuentes, R., Muzyk, A.J., Gagliardi, J.P. and
Yanamadala, M., 2017. Discharge plans for geriatric inpatients with delirium: a plan to stop
antipsychotics?. Journal of the American Geriatrics Society, 65(10), pp.2278-2281.
Kassie, G.M., Nguyen, T.A., Ellett, L.M.K., Pratt, N.L. and Roughead, E.E., 2018. Do risk
prediction models for postoperative delirium consider patients’ preoperative medication
use?. Drugs & aging, 35(3), pp.213-222.
Kim, S., Kim, J.J., Oh, J., Park, J. and Park, J.Y., 2018. Delirium characteristics and
outcomes in medical and surgical lnpatients: A subgroup analysis. Journal of critical
care, 43, pp.156-162.
Krewulak, K.D., Stelfox, H.T., Ely, E.W. and Fiest, K.M., 2020. Risk factors and outcomes
among delirium subtypes in adult ICUs: A systematic review. Journal of Critical Care.
Lam, K. and Gandell, D., 2018. The Top Articles in Geriatrics 2016–2017. Canadian
Geriatrics Journal, 21(3), p.210.
Liu, Y., Li, X.J., Liang, Y. and Kang, Y., 2019. Pharmacological prevention of postoperative
delirium: a systematic review and meta-analysis of randomized controlled trials. Evidence-
Based Complementary and Alternative Medicine, 2019.
Marcantonio, E.R., 2017. Delirium in hospitalized older adults. New England Journal of
Medicine, 377(15), pp.1456-1466.
Marcantonio, E.R., 2017. Delirium in hospitalized older adults. New England Journal of
Medicine, 377(15), pp.1456-1466.
Mulkey, M.A., Olson, D.M. and Hardin, S.R., 2019. Top Four Evidence-Based Nursing
Interventions for Delirium. Medsurg Nursing, 28(6), pp.357-362.
Yanamadala, M., 2017. Discharge plans for geriatric inpatients with delirium: a plan to stop
antipsychotics?. Journal of the American Geriatrics Society, 65(10), pp.2278-2281.
Kassie, G.M., Nguyen, T.A., Ellett, L.M.K., Pratt, N.L. and Roughead, E.E., 2018. Do risk
prediction models for postoperative delirium consider patients’ preoperative medication
use?. Drugs & aging, 35(3), pp.213-222.
Kim, S., Kim, J.J., Oh, J., Park, J. and Park, J.Y., 2018. Delirium characteristics and
outcomes in medical and surgical lnpatients: A subgroup analysis. Journal of critical
care, 43, pp.156-162.
Krewulak, K.D., Stelfox, H.T., Ely, E.W. and Fiest, K.M., 2020. Risk factors and outcomes
among delirium subtypes in adult ICUs: A systematic review. Journal of Critical Care.
Lam, K. and Gandell, D., 2018. The Top Articles in Geriatrics 2016–2017. Canadian
Geriatrics Journal, 21(3), p.210.
Liu, Y., Li, X.J., Liang, Y. and Kang, Y., 2019. Pharmacological prevention of postoperative
delirium: a systematic review and meta-analysis of randomized controlled trials. Evidence-
Based Complementary and Alternative Medicine, 2019.
Marcantonio, E.R., 2017. Delirium in hospitalized older adults. New England Journal of
Medicine, 377(15), pp.1456-1466.
Marcantonio, E.R., 2017. Delirium in hospitalized older adults. New England Journal of
Medicine, 377(15), pp.1456-1466.
Mulkey, M.A., Olson, D.M. and Hardin, S.R., 2019. Top Four Evidence-Based Nursing
Interventions for Delirium. Medsurg Nursing, 28(6), pp.357-362.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Mulkey, M.A., Roberson, D.W., Everhart, D.E. and Hardin, S.R., 2018. Choosing the right
delirium assessment tool. Journal of Neuroscience Nursing, 50(6), pp.343-348.
Oberai, T., Laver, K., Crotty, M., Killington, M. and Jaarsma, R., 2018. Effectiveness of
multicomponent interventions on incidence of delirium in hospitalized older patients with hip
fracture: a systematic review. International psychogeriatrics, 30(4), pp.481-492.
Oh, E.S., Fong, T.G., Hshieh, T.T. and Inouye, S.K., 2017. Delirium in older persons:
advances in diagnosis and treatment. Jama, 318(12), pp.1161-1174.
Oh, E.S., Needham, D.M., Nikooie, R., Wilson, L.M., Zhang, A., Robinson, K.A. and
Neufeld, K.J., 2019. Antipsychotics for Preventing Delirium in Hospitalized Adults. Annals
of internal medicine, 171(7), pp.474-484.
Pahwa, A. K., Qureshi, I., and Cumbler, E. 2019. Things We Do For No Reason™: Use of
Antipsychotic Medications in Patients with Delirium. Journal of hospital medicine, 14(9),
p.565.
Rivière, J., van der Mast, R.C., Vandenberghe, J. and Van Den Eede, F., 2019. Efficacy and
tolerability of atypical antipsychotics in the treatment of delirium: a systematic review of the
literature. Psychosomatics, 60(1), pp.18-26.
Sarpal, D.K., Argyelan, M., Robinson, D.G., Szeszko, P.R., Karlsgodt, K.H., John, M.,
Weissman, N., Gallego, J.A., Kane, J.M., Lencz, T. and Malhotra, A.K., 2016. Baseline
striatal functional connectivity as a predictor of response to antipsychotic drug
treatment. American Journal of Psychiatry, 173(1), pp.69-77.
Scholtens, R.M., de Rooij, S.E., Vellekoop, A.E., Vrouenraets, B.C. and van Munster, B.C.,
2016. Preoperative CSF melatonin concentrations and the occurrence of delirium in older hip
fracture patients: a preliminary study. PloS one, 11(12).
delirium assessment tool. Journal of Neuroscience Nursing, 50(6), pp.343-348.
Oberai, T., Laver, K., Crotty, M., Killington, M. and Jaarsma, R., 2018. Effectiveness of
multicomponent interventions on incidence of delirium in hospitalized older patients with hip
fracture: a systematic review. International psychogeriatrics, 30(4), pp.481-492.
Oh, E.S., Fong, T.G., Hshieh, T.T. and Inouye, S.K., 2017. Delirium in older persons:
advances in diagnosis and treatment. Jama, 318(12), pp.1161-1174.
Oh, E.S., Needham, D.M., Nikooie, R., Wilson, L.M., Zhang, A., Robinson, K.A. and
Neufeld, K.J., 2019. Antipsychotics for Preventing Delirium in Hospitalized Adults. Annals
of internal medicine, 171(7), pp.474-484.
Pahwa, A. K., Qureshi, I., and Cumbler, E. 2019. Things We Do For No Reason™: Use of
Antipsychotic Medications in Patients with Delirium. Journal of hospital medicine, 14(9),
p.565.
Rivière, J., van der Mast, R.C., Vandenberghe, J. and Van Den Eede, F., 2019. Efficacy and
tolerability of atypical antipsychotics in the treatment of delirium: a systematic review of the
literature. Psychosomatics, 60(1), pp.18-26.
Sarpal, D.K., Argyelan, M., Robinson, D.G., Szeszko, P.R., Karlsgodt, K.H., John, M.,
Weissman, N., Gallego, J.A., Kane, J.M., Lencz, T. and Malhotra, A.K., 2016. Baseline
striatal functional connectivity as a predictor of response to antipsychotic drug
treatment. American Journal of Psychiatry, 173(1), pp.69-77.
Scholtens, R.M., de Rooij, S.E., Vellekoop, A.E., Vrouenraets, B.C. and van Munster, B.C.,
2016. Preoperative CSF melatonin concentrations and the occurrence of delirium in older hip
fracture patients: a preliminary study. PloS one, 11(12).
Tremblay, P. and Gold, S., 2016. Prevention of post-operative delirium in the elderly using
pharmacological agents. Canadian Geriatrics Journal, 19(3), p.113.
van den Boogaard, M., Wassenaar, A., van Haren, F.M., Slooter, A.J., Jorens, P.G., van der
Jagt, M., Simons, K.S., Egerod, I., Burry, L.D., Beishuizen, A. and Pickkers, P., 2020.
Influence of sedation on delirium recognition in critically ill patients: A multinational cohort
study. Australian Critical Care.
Wan, M. and Chase, J.M., 2017. Delirium in older adults: Diagnosis, prevention, and
treatment. British Columbia Medical Journal, 59(3).
pharmacological agents. Canadian Geriatrics Journal, 19(3), p.113.
van den Boogaard, M., Wassenaar, A., van Haren, F.M., Slooter, A.J., Jorens, P.G., van der
Jagt, M., Simons, K.S., Egerod, I., Burry, L.D., Beishuizen, A. and Pickkers, P., 2020.
Influence of sedation on delirium recognition in critically ill patients: A multinational cohort
study. Australian Critical Care.
Wan, M. and Chase, J.M., 2017. Delirium in older adults: Diagnosis, prevention, and
treatment. British Columbia Medical Journal, 59(3).
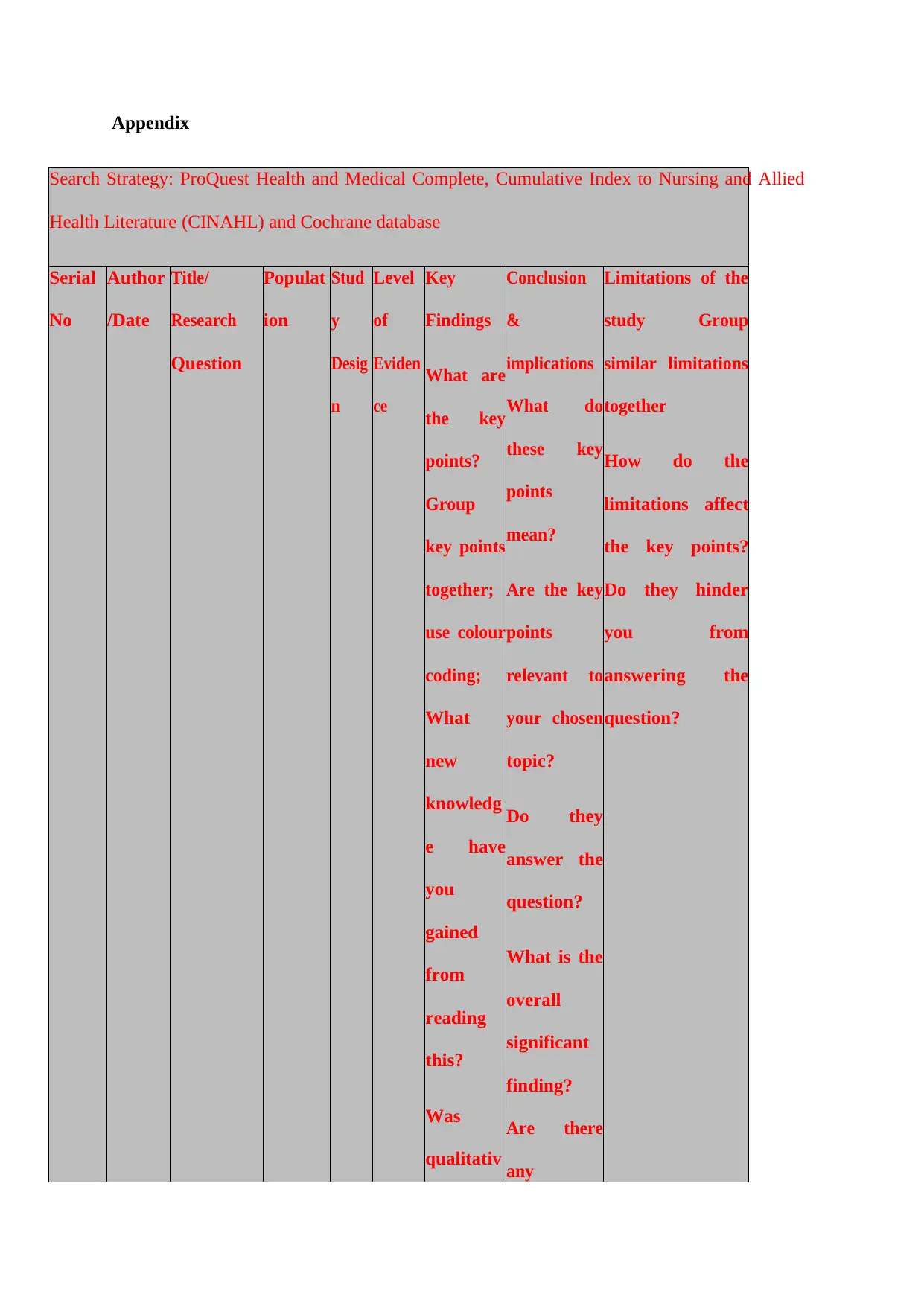
Appendix
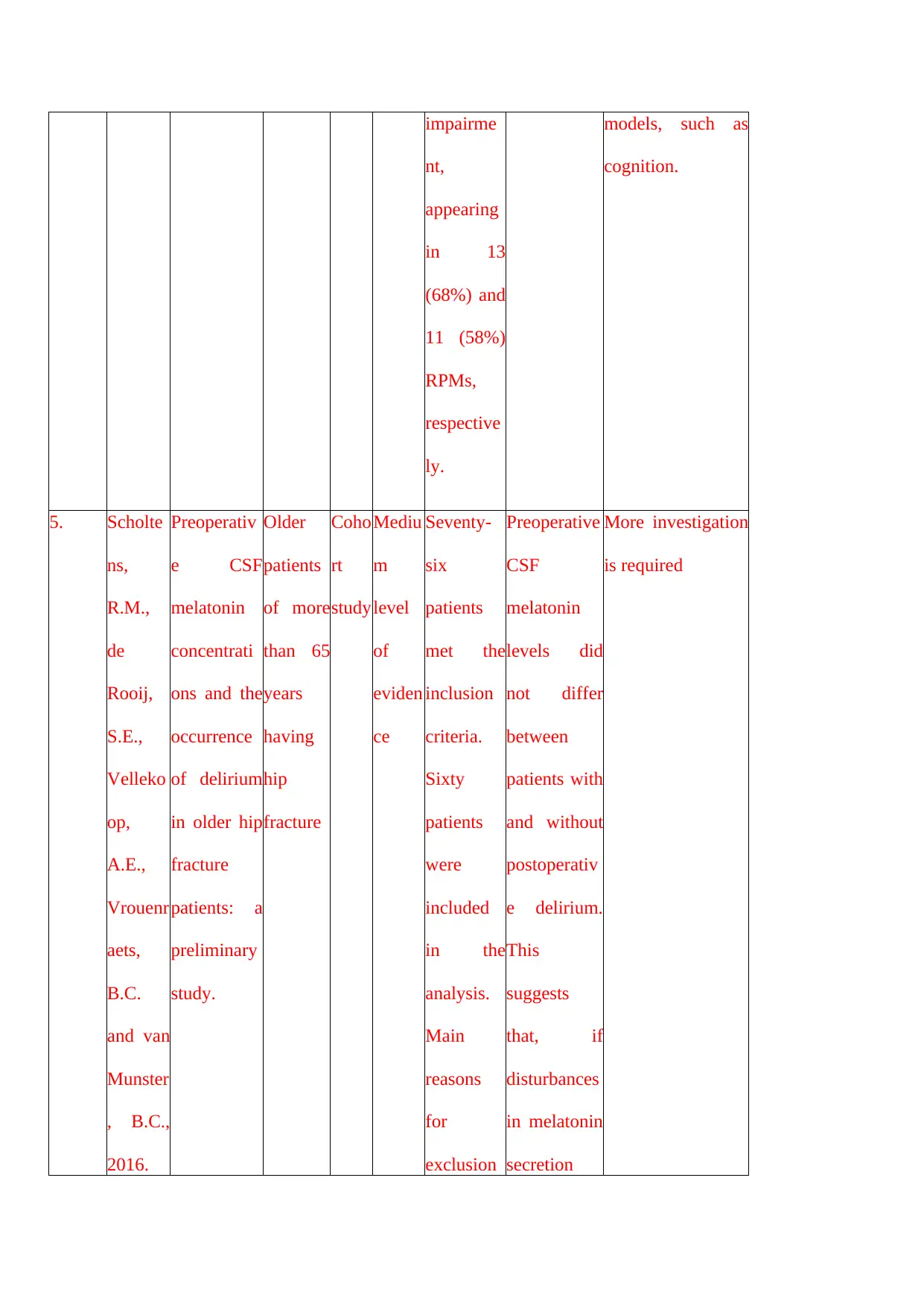
Search Strategy: ProQuest Health and Medical Complete, Cumulative Index to Nursing and Allied
Health Literature (CINAHL) and Cochrane database
Serial
No
Author
/Date
Title/
Research
Question
Populat
ion
Stud
y
Desig
n
Level
of
Eviden
ce
Key
Findings
What are
the key
points?
Group
key points
together;
use colour
coding;
What
new
knowledg
e have
you
gained
from
reading
this?
Was
qualitativ
Conclusion
&
implications
What do
these key
points
mean?
Are the key
points
relevant to
your chosen
topic?
Do they
answer the
question?
What is the
overall
significant
finding?
Are there
any
Limitations of the
study Group
similar limitations
together
How do the
limitations affect
the key points?
Do they hinder
you from
answering the
question?
Search Strategy: ProQuest Health and Medical Complete, Cumulative Index to Nursing and Allied
Health Literature (CINAHL) and Cochrane database
Serial
No
Author
/Date
Title/
Research
Question
Populat
ion
Stud
y
Desig
n
Level
of
Eviden
ce
Key
Findings
What are
the key
points?
Group
key points
together;
use colour
coding;
What
new
knowledg
e have
you
gained
from
reading
this?
Was
qualitativ
Conclusion
&
implications
What do
these key
points
mean?
Are the key
points
relevant to
your chosen
topic?
Do they
answer the
question?
What is the
overall
significant
finding?
Are there
any
Limitations of the
study Group
similar limitations
together
How do the
limitations affect
the key points?
Do they hinder
you from
answering the
question?
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
e or
quantitati
ve or
mixed
methods
used?
recommend
ations you
can
draw from
this paper?
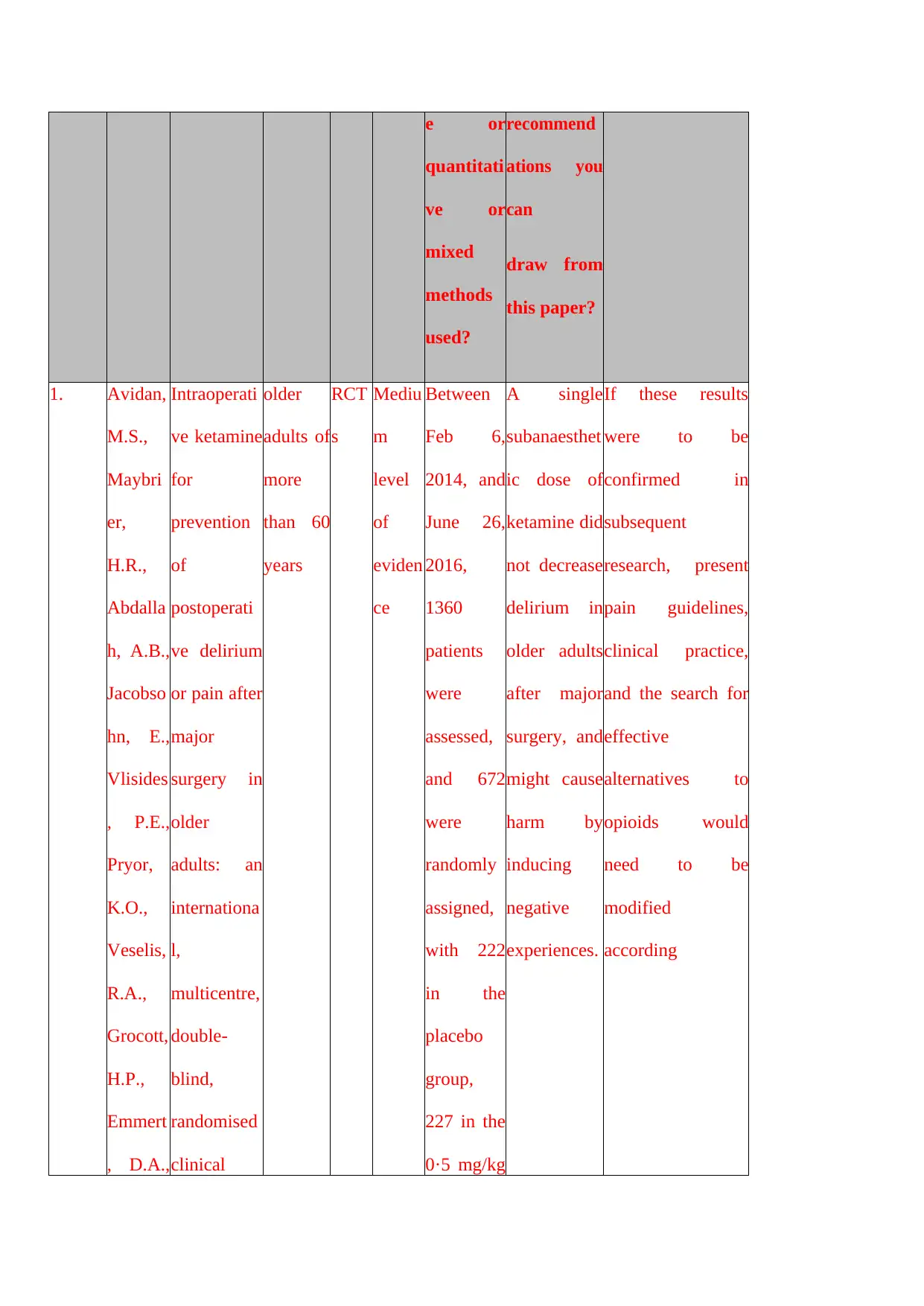
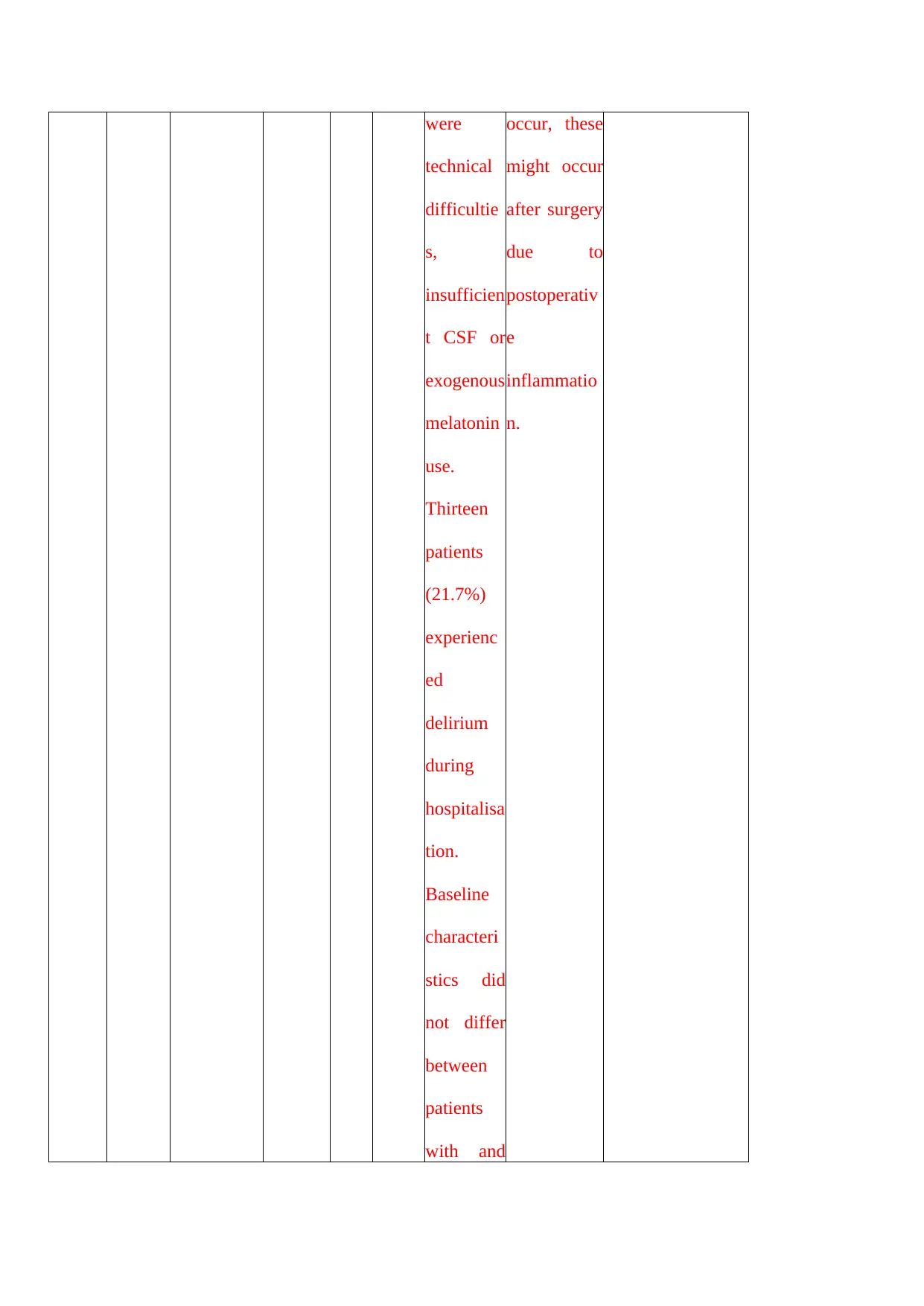
1. Avidan,
M.S.,
Maybri
er,
H.R.,
Abdalla
h, A.B.,
Jacobso
hn, E.,
Vlisides
, P.E.,
Pryor,
K.O.,
Veselis,
R.A.,
Grocott,
H.P.,
Emmert
, D.A.,
Intraoperati
ve ketamine
for
prevention
of
postoperati
ve delirium
or pain after
major
surgery in
older
adults: an
internationa
l,
multicentre,
double-
blind,
randomised
clinical
older
adults of
more
than 60
years
RCT
s
Mediu
m
level
of
eviden
ce
Between
Feb 6,
2014, and
June 26,
2016,
1360
patients
were
assessed,
and 672
were
randomly
assigned,
with 222
in the
placebo
group,
227 in the
0·5 mg/kg
A single
subanaesthet
ic dose of
ketamine did
not decrease
delirium in
older adults
after major
surgery, and
might cause
harm by
inducing
negative
experiences.
If these results
were to be
confirmed in
subsequent
research, present
pain guidelines,
clinical practice,
and the search for
effective
alternatives to
opioids would
need to be
modified
according
quantitati
ve or
mixed
methods
used?
recommend
ations you
can
draw from
this paper?
1. Avidan,
M.S.,
Maybri
er,
H.R.,
Abdalla
h, A.B.,
Jacobso
hn, E.,
Vlisides
, P.E.,
Pryor,
K.O.,
Veselis,
R.A.,
Grocott,
H.P.,
Emmert
, D.A.,
Intraoperati
ve ketamine
for
prevention
of
postoperati
ve delirium
or pain after
major
surgery in
older
adults: an
internationa
l,
multicentre,
double-
blind,
randomised
clinical
older
adults of
more
than 60
years
RCT
s
Mediu
m
level
of
eviden
ce
Between
Feb 6,
2014, and
June 26,
2016,
1360
patients
were
assessed,
and 672
were
randomly
assigned,
with 222
in the
placebo
group,
227 in the
0·5 mg/kg
A single
subanaesthet
ic dose of
ketamine did
not decrease
delirium in
older adults
after major
surgery, and
might cause
harm by
inducing
negative
experiences.
If these results
were to be
confirmed in
subsequent
research, present
pain guidelines,
clinical practice,
and the search for
effective
alternatives to
opioids would
need to be
modified
according
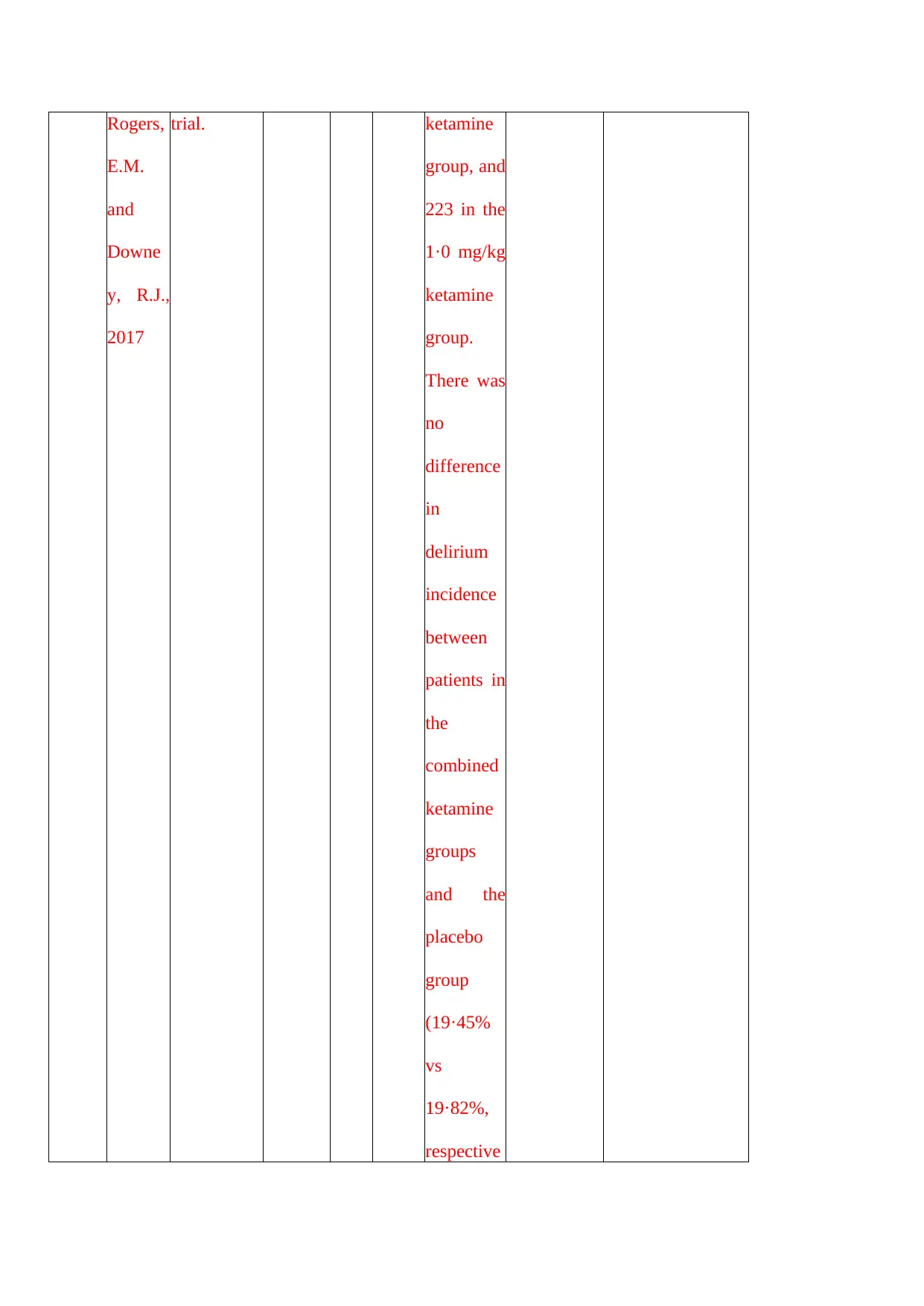
Rogers,
E.M.
and
Downe
y, R.J.,
2017
trial. ketamine
group, and
223 in the
1·0 mg/kg
ketamine
group.
There was
no
difference
in
delirium
incidence
between
patients in
the
combined
ketamine
groups
and the
placebo
group
(19·45%
vs
19·82%,
respective
E.M.
and
Downe
y, R.J.,
2017
trial. ketamine
group, and
223 in the
1·0 mg/kg
ketamine
group.
There was
no
difference
in
delirium
incidence
between
patients in
the
combined
ketamine
groups
and the
placebo
group
(19·45%
vs
19·82%,
respective
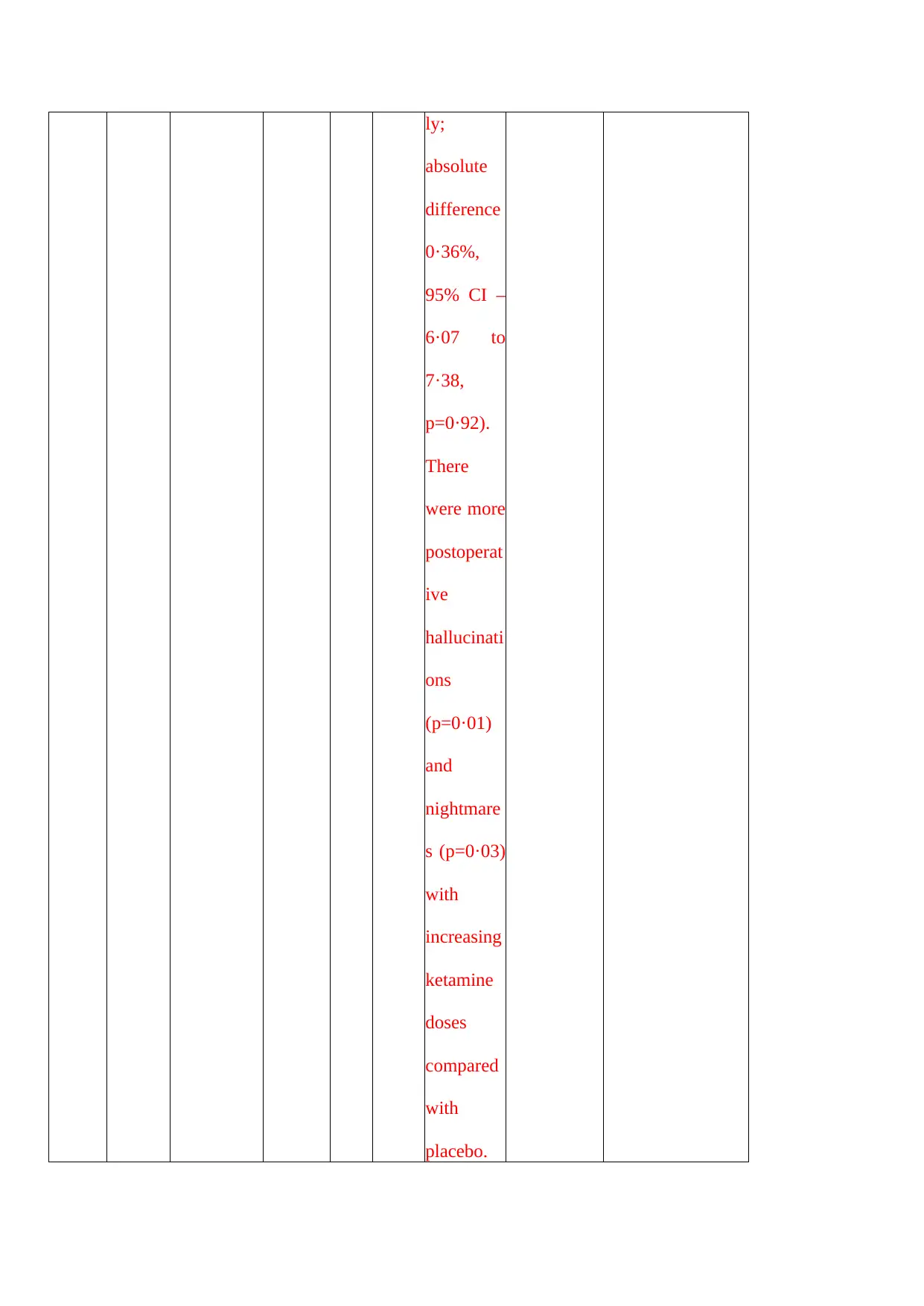
ly;
absolute
difference
0·36%,
95% CI –
6·07 to
7·38,
p=0·92).
There
were more
postoperat
ive
hallucinati
ons
(p=0·01)
and
nightmare
s (p=0·03)
with
increasing
ketamine
doses
compared
with
placebo.
absolute
difference
0·36%,
95% CI –
6·07 to
7·38,
p=0·92).
There
were more
postoperat
ive
hallucinati
ons
(p=0·01)
and
nightmare
s (p=0·03)
with
increasing
ketamine
doses
compared
with
placebo.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
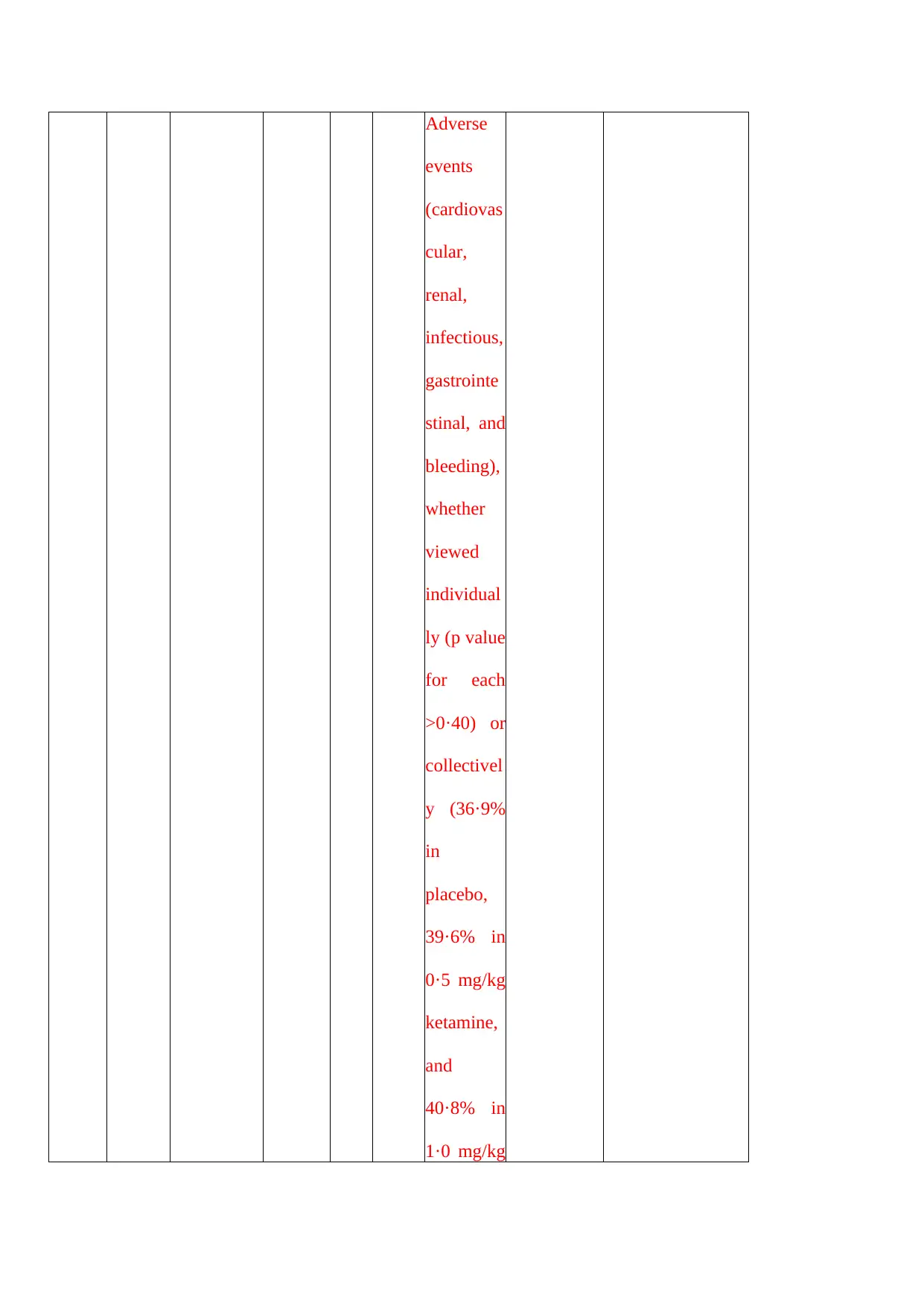
Adverse
events
(cardiovas
cular,
renal,
infectious,
gastrointe
stinal, and
bleeding),
whether
viewed
individual
ly (p value
for each
>0·40) or
collectivel
y (36·9%
in
placebo,
39·6% in
0·5 mg/kg
ketamine,
and
40·8% in
1·0 mg/kg
events
(cardiovas
cular,
renal,
infectious,
gastrointe
stinal, and
bleeding),
whether
viewed
individual
ly (p value
for each
>0·40) or
collectivel
y (36·9%
in
placebo,
39·6% in
0·5 mg/kg
ketamine,
and
40·8% in
1·0 mg/kg
ketamine
groups,
p=0·69),
did not
differ
significant
ly across
groups.
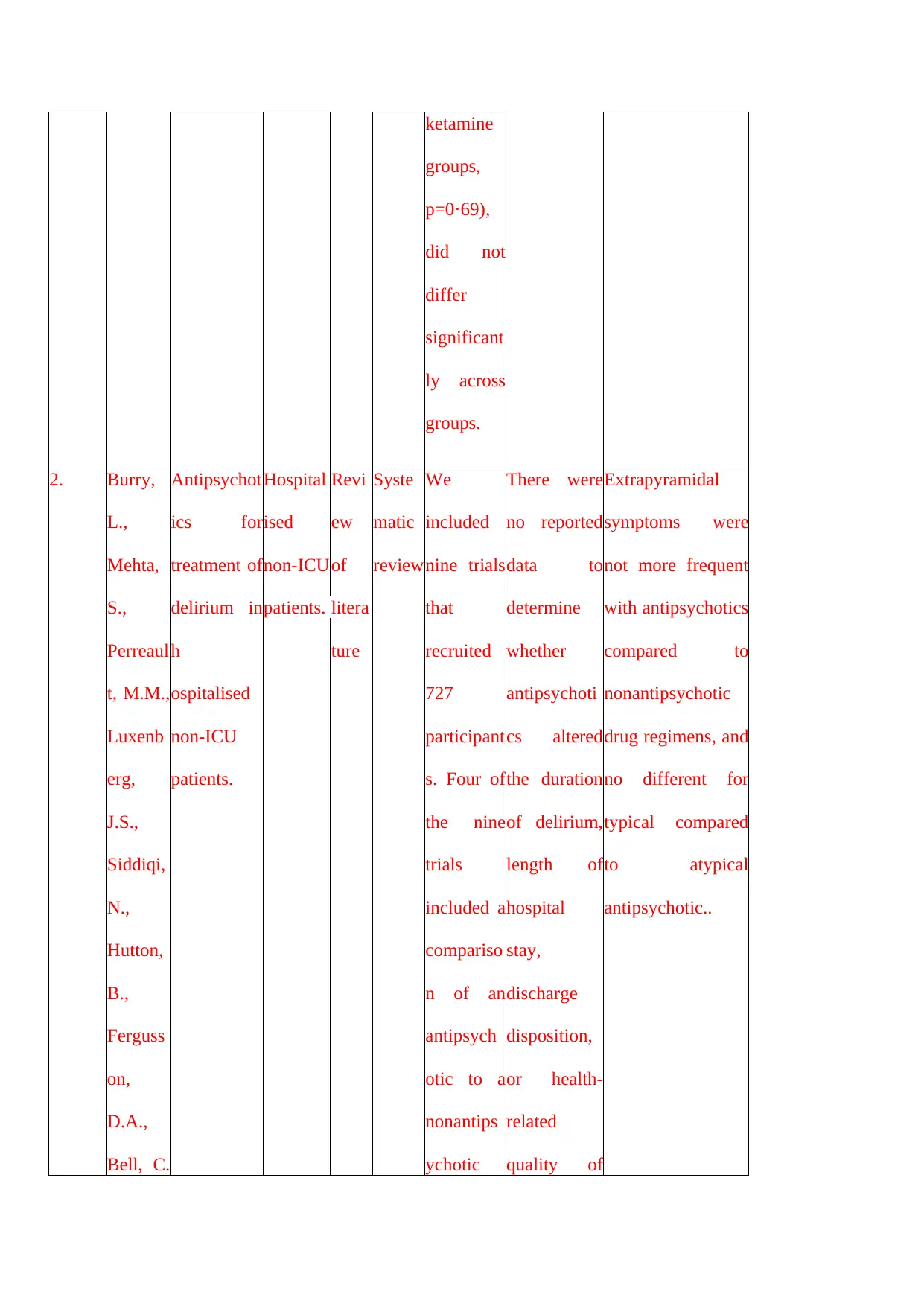
2. Burry,
L.,
Mehta,
S.,
Perreaul
t, M.M.,
Luxenb
erg,
J.S.,
Siddiqi,
N.,
Hutton,
B.,
Ferguss
on,
D.A.,
Bell, C.
Antipsychot
ics for
treatment of
delirium in
h
ospitalised
non‐ICU
patients.
Hospital
ised
non‐ICU
patients.
Revi
ew
of
litera
ture
Syste
matic
review
We
included
nine trials
that
recruited
727
participant
s. Four of
the nine
trials
included a
compariso
n of an
antipsych
otic to a
nonantips
ychotic
There were
no reported
data to
determine
whether
antipsychoti
cs altered
the duration
of delirium,
length of
hospital
stay,
discharge
disposition,
or health‐
related
quality of
Extrapyramidal
symptoms were
not more frequent
with antipsychotics
compared to
nonantipsychotic
drug regimens, and
no different for
typical compared
to atypical
antipsychotic..
groups,
p=0·69),
did not
differ
significant
ly across
groups.
2. Burry,
L.,
Mehta,
S.,
Perreaul
t, M.M.,
Luxenb
erg,
J.S.,
Siddiqi,
N.,
Hutton,
B.,
Ferguss
on,
D.A.,
Bell, C.
Antipsychot
ics for
treatment of
delirium in
h
ospitalised
non‐ICU
patients.
Hospital
ised
non‐ICU
patients.
Revi
ew
of
litera
ture
Syste
matic
review
We
included
nine trials
that
recruited
727
participant
s. Four of
the nine
trials
included a
compariso
n of an
antipsych
otic to a
nonantips
ychotic
There were
no reported
data to
determine
whether
antipsychoti
cs altered
the duration
of delirium,
length of
hospital
stay,
discharge
disposition,
or health‐
related
quality of
Extrapyramidal
symptoms were
not more frequent
with antipsychotics
compared to
nonantipsychotic
drug regimens, and
no different for
typical compared
to atypical
antipsychotic..
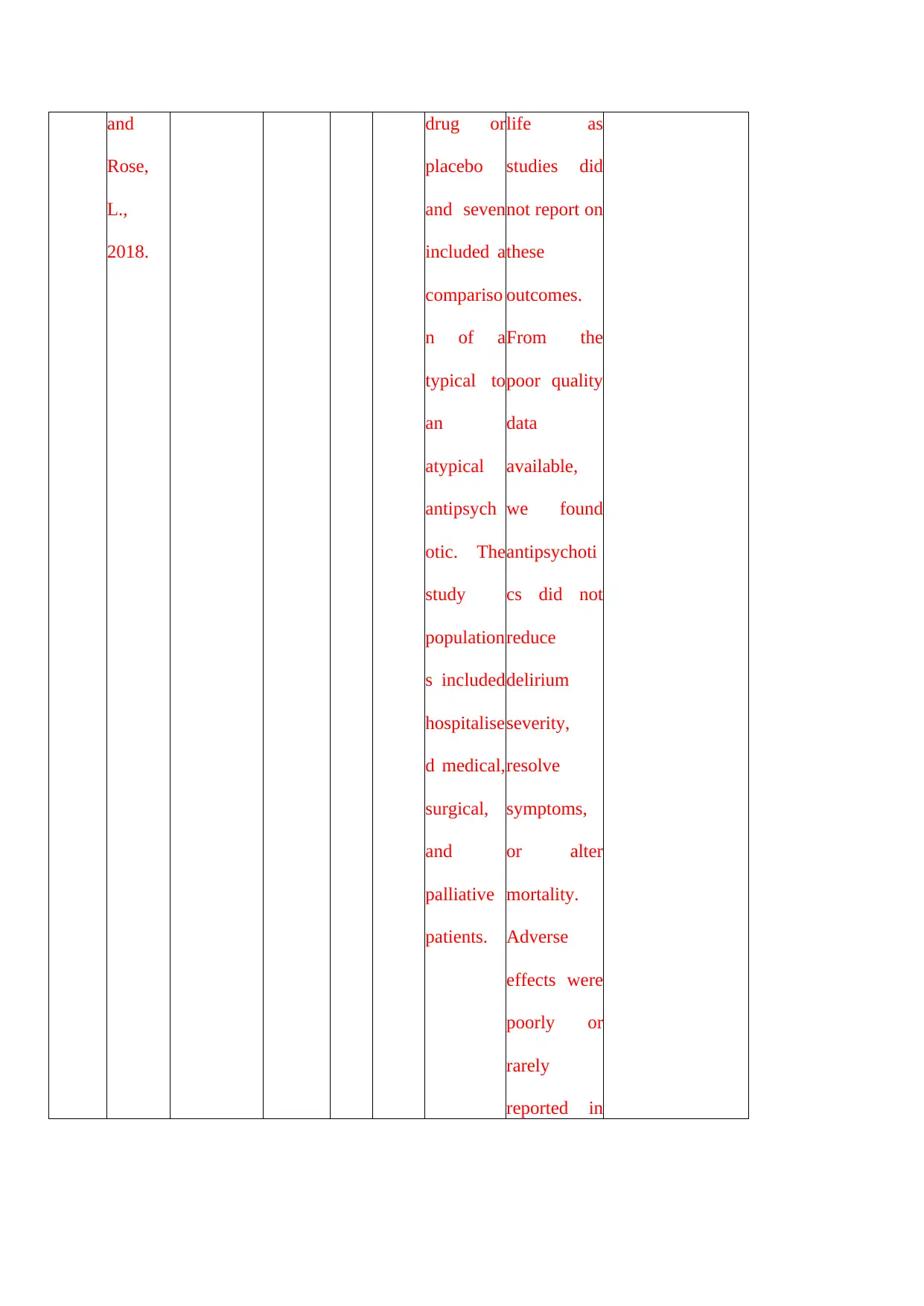
and
Rose,
L.,
2018.
drug or
placebo
and seven
included a
compariso
n of a
typical to
an
atypical
antipsych
otic. The
study
population
s included
hospitalise
d medical,
surgical,
and
palliative
patients.
life as
studies did
not report on
these
outcomes.
From the
poor quality
data
available,
we found
antipsychoti
cs did not
reduce
delirium
severity,
resolve
symptoms,
or alter
mortality.
Adverse
effects were
poorly or
rarely
reported in
Rose,
L.,
2018.
drug or
placebo
and seven
included a
compariso
n of a
typical to
an
atypical
antipsych
otic. The
study
population
s included
hospitalise
d medical,
surgical,
and
palliative
patients.
life as
studies did
not report on
these
outcomes.
From the
poor quality
data
available,
we found
antipsychoti
cs did not
reduce
delirium
severity,
resolve
symptoms,
or alter
mortality.
Adverse
effects were
poorly or
rarely
reported in
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
the trials.
3. Teipel,
S.J.,
Fritze,
T.,
Ellenrie
der, M.,
Haenisc
h, B.,
Mittelm
eier, W.
and
Doblha
mmer,
G.,
2018.
Association
of joint
replacement
surgery
with
incident
dementia
diagnosis in
German
claims
data.
Patient
with
Joint
replace
ment
surgery
Statis
tical
analy
sis
Lowes
t
eviden
ce
The rate
of incident
dementia
diagnoses
in people
without
joint
replaceme
nt surgery
was 21.34
per 1,000
person
years,
compared
with 80.76
incident
cases
when joint
replaceme
nt surgery
was
conducted
during the
quarter of
In people
surviving
the high-risk
phase for
dementia
immediately
after
surgery,
long-term
risk of
dementia
may reach
the level of
those
without
surgery.
These
findings
encourage
consequent
perioperativ
e
management
to reduce the
None
3. Teipel,
S.J.,
Fritze,
T.,
Ellenrie
der, M.,
Haenisc
h, B.,
Mittelm
eier, W.
and
Doblha
mmer,
G.,
2018.
Association
of joint
replacement
surgery
with
incident
dementia
diagnosis in
German
claims
data.
Patient
with
Joint
replace
ment
surgery
Statis
tical
analy
sis
Lowes
t
eviden
ce
The rate
of incident
dementia
diagnoses
in people
without
joint
replaceme
nt surgery
was 21.34
per 1,000
person
years,
compared
with 80.76
incident
cases
when joint
replaceme
nt surgery
was
conducted
during the
quarter of
In people
surviving
the high-risk
phase for
dementia
immediately
after
surgery,
long-term
risk of
dementia
may reach
the level of
those
without
surgery.
These
findings
encourage
consequent
perioperativ
e
management
to reduce the
None
the
incident
dementia
diagnosis;
rates
declined
to 21.77
incident
cases 7
and more
quarters
after joint
replaceme
nt surgery
had taken
place.
This
pattern
was
maintaine
d when
controllin
g for
delirium
diagnosis
risk of
dementia as
well as
prospective
studies of
potentially
beneficial
effects of
joint
replacement
surgery on
mid- to
long-term
recovery of
mobility and
cognition in
geriatric
patients.
incident
dementia
diagnosis;
rates
declined
to 21.77
incident
cases 7
and more
quarters
after joint
replaceme
nt surgery
had taken
place.
This
pattern
was
maintaine
d when
controllin
g for
delirium
diagnosis
risk of
dementia as
well as
prospective
studies of
potentially
beneficial
effects of
joint
replacement
surgery on
mid- to
long-term
recovery of
mobility and
cognition in
geriatric
patients.
and
regular
prescriptio
n of SAD.
Among
10,563
patients
with at
least one
joint
replaceme
nt surgery,
patients
with a
diagnosis
of
delirium
in the
quarter of
the
surgery
were at
increased
risk of a
dementia
regular
prescriptio
n of SAD.
Among
10,563
patients
with at
least one
joint
replaceme
nt surgery,
patients
with a
diagnosis
of
delirium
in the
quarter of
the
surgery
were at
increased
risk of a
dementia
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
diagnosis
compared
to patients
without
such a
diagnosis
(HR=2.00,
p <
0.001).
4. Kassie,
G.M.,
Nguyen
, T.A.,
Ellett,
L.M.K.,
Pratt,
N.L.
and
Roughe
ad,
E.E.,
2018.
Do risk
prediction
models for
postoperati
ve delirium
consider
patients’
preoperativ
e
medication
use?.
Patient
with
postoper
ative
delirium
Syste
matic
revie
w
Syste
matic
review
There was
wide
variability
in the
factors
included
in the
final
models,
with the
most
frequent
predictors
being age
and
cognitive
While
medications
are
commonly
cited risk
factors for
delirium,
they are not
adequately
considered
when
developing
RPMs.
Future studies
aiming to develop
an RPM for
postoperative
delirium should
include
preoperative
medication data as
a potential
predictor variable
because of the
modifiable nature
of medication use
and its impact on
other factors
commonly in
compared
to patients
without
such a
diagnosis
(HR=2.00,
p <
0.001).
4. Kassie,
G.M.,
Nguyen
, T.A.,
Ellett,
L.M.K.,
Pratt,
N.L.
and
Roughe
ad,
E.E.,
2018.
Do risk
prediction
models for
postoperati
ve delirium
consider
patients’
preoperativ
e
medication
use?.
Patient
with
postoper
ative
delirium
Syste
matic
revie
w
Syste
matic
review
There was
wide
variability
in the
factors
included
in the
final
models,
with the
most
frequent
predictors
being age
and
cognitive
While
medications
are
commonly
cited risk
factors for
delirium,
they are not
adequately
considered
when
developing
RPMs.
Future studies
aiming to develop
an RPM for
postoperative
delirium should
include
preoperative
medication data as
a potential
predictor variable
because of the
modifiable nature
of medication use
and its impact on
other factors
commonly in
impairme
nt,
appearing
in 13
(68%) and
11 (58%)
RPMs,
respective
ly.
models, such as
cognition.
5. Scholte
ns,
R.M.,
de
Rooij,
S.E.,
Velleko
op,
A.E.,
Vrouenr
aets,
B.C.
and van
Munster
, B.C.,
2016.
Preoperativ
e CSF
melatonin
concentrati
ons and the
occurrence
of delirium
in older hip
fracture
patients: a
preliminary
study.
Older
patients
of more
than 65
years
having
hip
fracture
Coho
rt
study
Mediu
m
level
of
eviden
ce
Seventy-
six
patients
met the
inclusion
criteria.
Sixty
patients
were
included
in the
analysis.
Main
reasons
for
exclusion
Preoperative
CSF
melatonin
levels did
not differ
between
patients with
and without
postoperativ
e delirium.
This
suggests
that, if
disturbances
in melatonin
secretion
More investigation
is required
nt,
appearing
in 13
(68%) and
11 (58%)
RPMs,
respective
ly.
models, such as
cognition.
5. Scholte
ns,
R.M.,
de
Rooij,
S.E.,
Velleko
op,
A.E.,
Vrouenr
aets,
B.C.
and van
Munster
, B.C.,
2016.
Preoperativ
e CSF
melatonin
concentrati
ons and the
occurrence
of delirium
in older hip
fracture
patients: a
preliminary
study.
Older
patients
of more
than 65
years
having
hip
fracture
Coho
rt
study
Mediu
m
level
of
eviden
ce
Seventy-
six
patients
met the
inclusion
criteria.
Sixty
patients
were
included
in the
analysis.
Main
reasons
for
exclusion
Preoperative
CSF
melatonin
levels did
not differ
between
patients with
and without
postoperativ
e delirium.
This
suggests
that, if
disturbances
in melatonin
secretion
More investigation
is required
were
technical
difficultie
s,
insufficien
t CSF or
exogenous
melatonin
use.
Thirteen
patients
(21.7%)
experienc
ed
delirium
during
hospitalisa
tion.
Baseline
characteri
stics did
not differ
between
patients
with and
occur, these
might occur
after surgery
due to
postoperativ
e
inflammatio
n.
technical
difficultie
s,
insufficien
t CSF or
exogenous
melatonin
use.
Thirteen
patients
(21.7%)
experienc
ed
delirium
during
hospitalisa
tion.
Baseline
characteri
stics did
not differ
between
patients
with and
occur, these
might occur
after surgery
due to
postoperativ
e
inflammatio
n.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
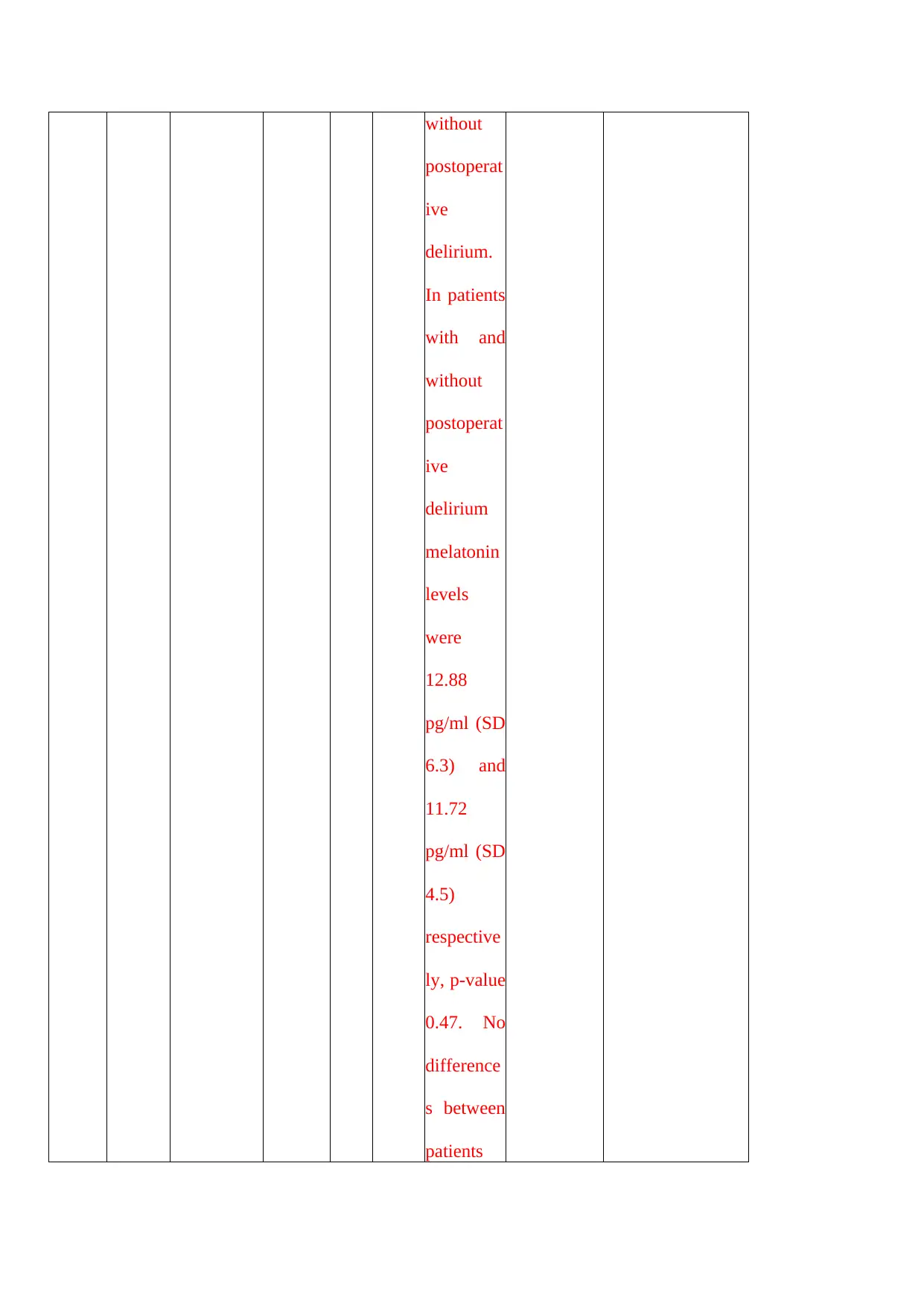
without
postoperat
ive
delirium.
In patients
with and
without
postoperat
ive
delirium
melatonin
levels
were
12.88
pg/ml (SD
6.3) and
11.72
pg/ml (SD
4.5)
respective
ly, p-value
0.47. No
difference
s between
patients
postoperat
ive
delirium.
In patients
with and
without
postoperat
ive
delirium
melatonin
levels
were
12.88
pg/ml (SD
6.3) and
11.72
pg/ml (SD
4.5)
respective
ly, p-value
0.47. No
difference
s between
patients
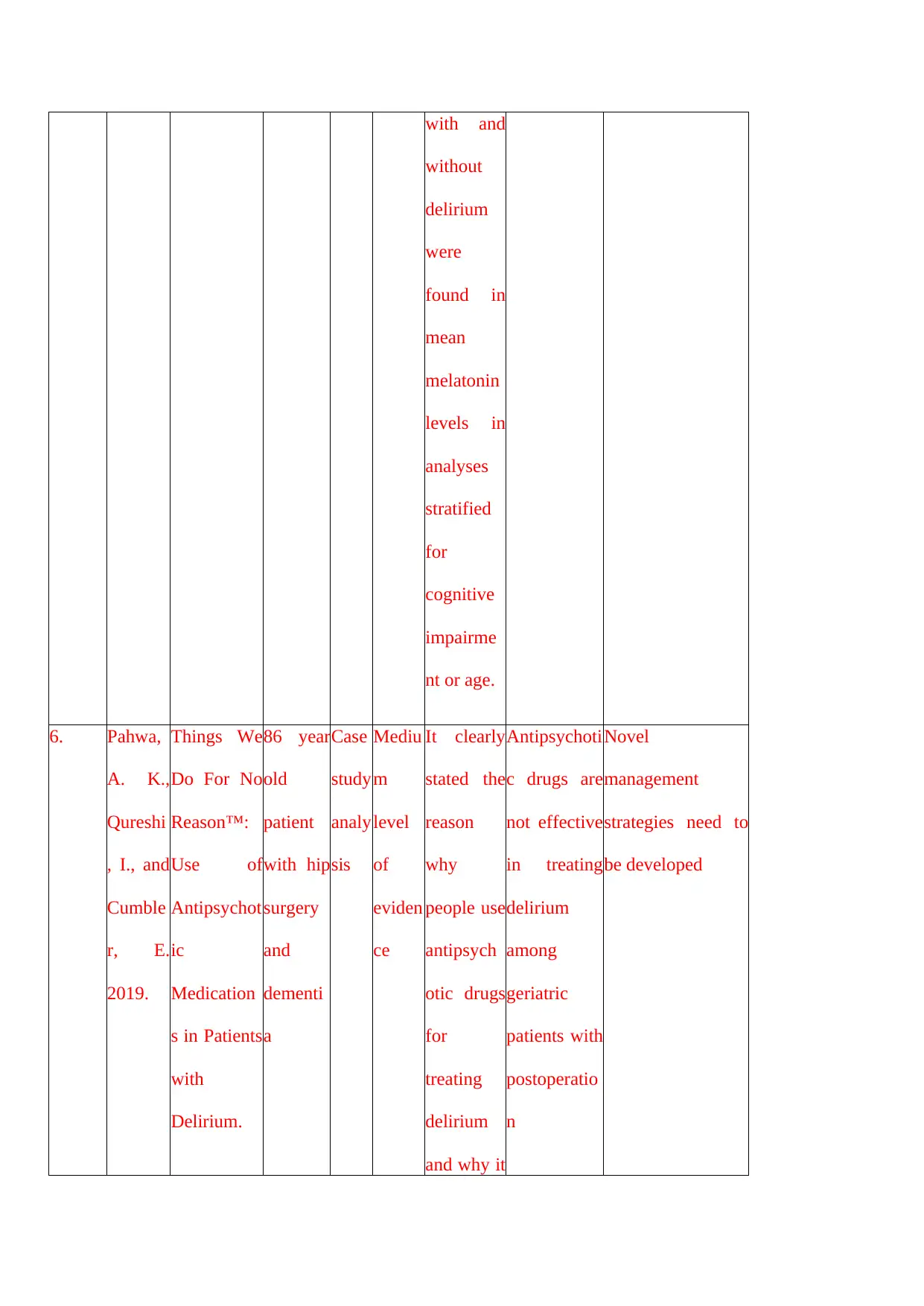
with and
without
delirium
were
found in
mean
melatonin
levels in
analyses
stratified
for
cognitive
impairme
nt or age.
6. Pahwa,
A. K.,
Qureshi
, I., and
Cumble
r, E.
2019.
Things We
Do For No
Reason™:
Use of
Antipsychot
ic
Medication
s in Patients
with
Delirium.
86 year
old
patient
with hip
surgery
and
dementi
a
Case
study
analy
sis
Mediu
m
level
of
eviden
ce
It clearly
stated the
reason
why
people use
antipsych
otic drugs
for
treating
delirium
and why it
Antipsychoti
c drugs are
not effective
in treating
delirium
among
geriatric
patients with
postoperatio
n
Novel
management
strategies need to
be developed
without
delirium
were
found in
mean
melatonin
levels in
analyses
stratified
for
cognitive
impairme
nt or age.
6. Pahwa,
A. K.,
Qureshi
, I., and
Cumble
r, E.
2019.
Things We
Do For No
Reason™:
Use of
Antipsychot
ic
Medication
s in Patients
with
Delirium.
86 year
old
patient
with hip
surgery
and
dementi
a
Case
study
analy
sis
Mediu
m
level
of
eviden
ce
It clearly
stated the
reason
why
people use
antipsych
otic drugs
for
treating
delirium
and why it
Antipsychoti
c drugs are
not effective
in treating
delirium
among
geriatric
patients with
postoperatio
n
Novel
management
strategies need to
be developed
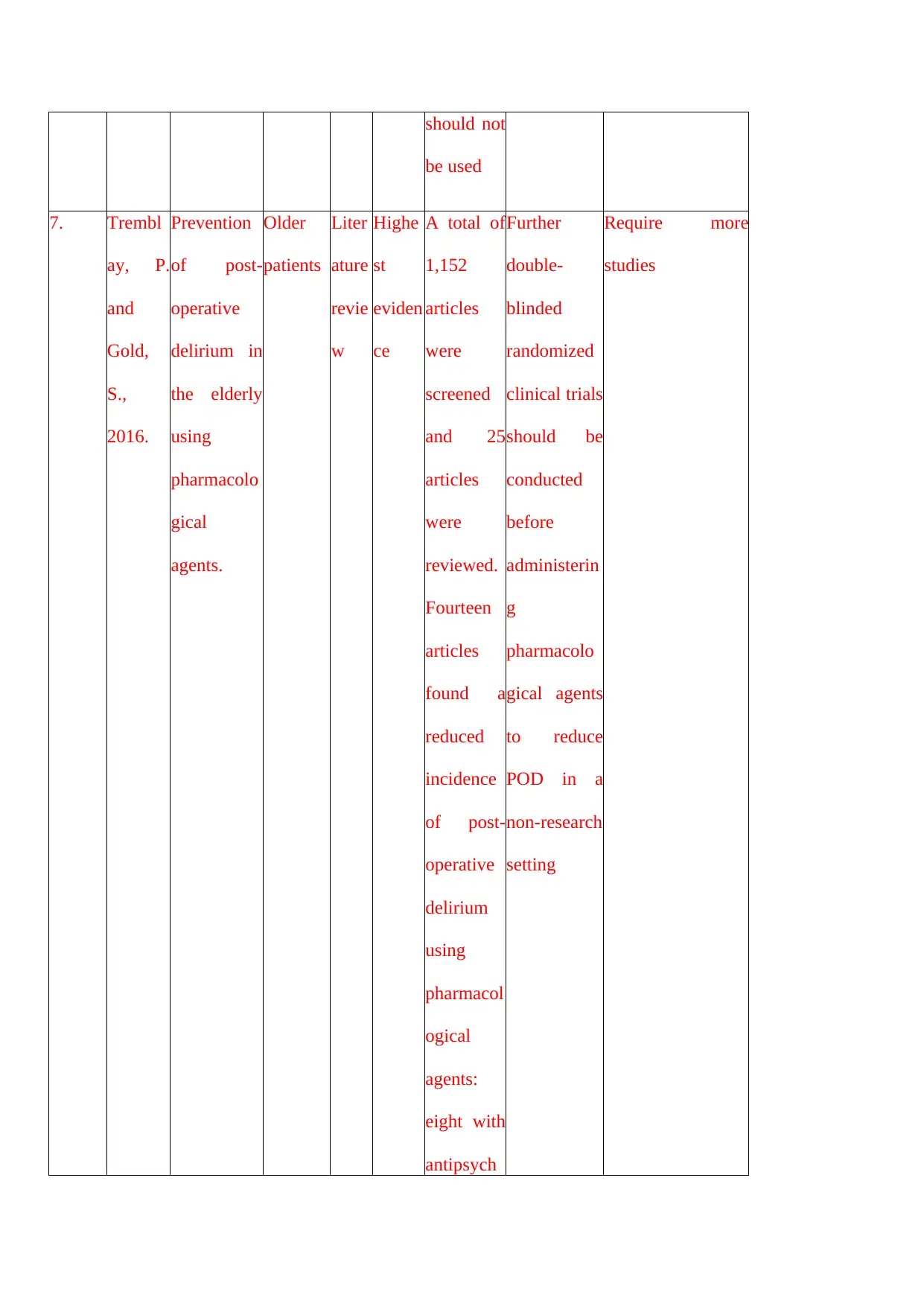
should not
be used
7. Trembl
ay, P.
and
Gold,
S.,
2016.
Prevention
of post-
operative
delirium in
the elderly
using
pharmacolo
gical
agents.
Older
patients
Liter
ature
revie
w
Highe
st
eviden
ce
A total of
1,152
articles
were
screened
and 25
articles
were
reviewed.
Fourteen
articles
found a
reduced
incidence
of post-
operative
delirium
using
pharmacol
ogical
agents:
eight with
antipsych
Further
double-
blinded
randomized
clinical trials
should be
conducted
before
administerin
g
pharmacolo
gical agents
to reduce
POD in a
non-research
setting
Require more
studies
be used
7. Trembl
ay, P.
and
Gold,
S.,
2016.
Prevention
of post-
operative
delirium in
the elderly
using
pharmacolo
gical
agents.
Older
patients
Liter
ature
revie
w
Highe
st
eviden
ce
A total of
1,152
articles
were
screened
and 25
articles
were
reviewed.
Fourteen
articles
found a
reduced
incidence
of post-
operative
delirium
using
pharmacol
ogical
agents:
eight with
antipsych
Further
double-
blinded
randomized
clinical trials
should be
conducted
before
administerin
g
pharmacolo
gical agents
to reduce
POD in a
non-research
setting
Require more
studies
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
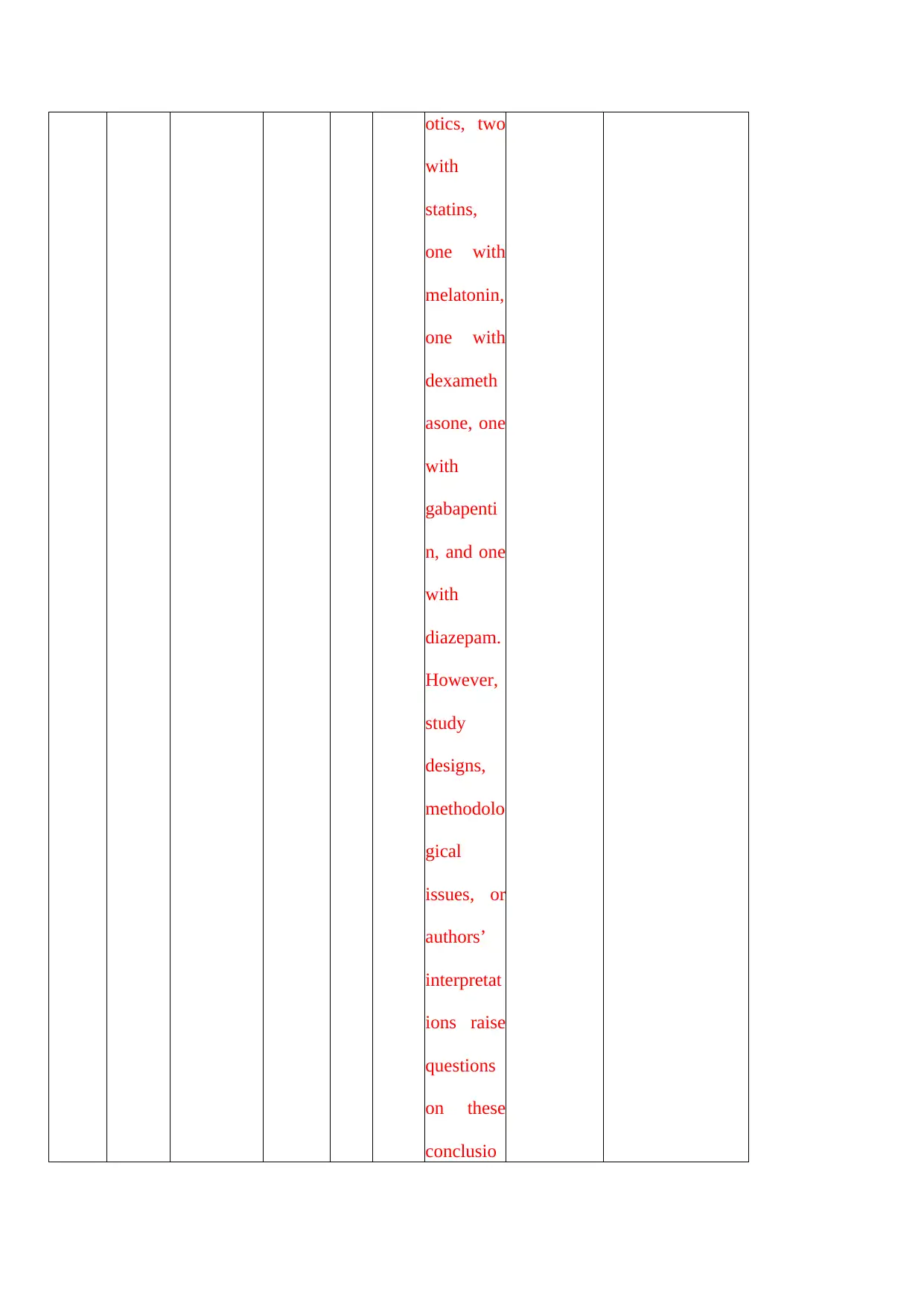
otics, two
with
statins,
one with
melatonin,
one with
dexameth
asone, one
with
gabapenti
n, and one
with
diazepam.
However,
study
designs,
methodolo
gical
issues, or
authors’
interpretat
ions raise
questions
on these
conclusio
with
statins,
one with
melatonin,
one with
dexameth
asone, one
with
gabapenti
n, and one
with
diazepam.
However,
study
designs,
methodolo
gical
issues, or
authors’
interpretat
ions raise
questions
on these
conclusio
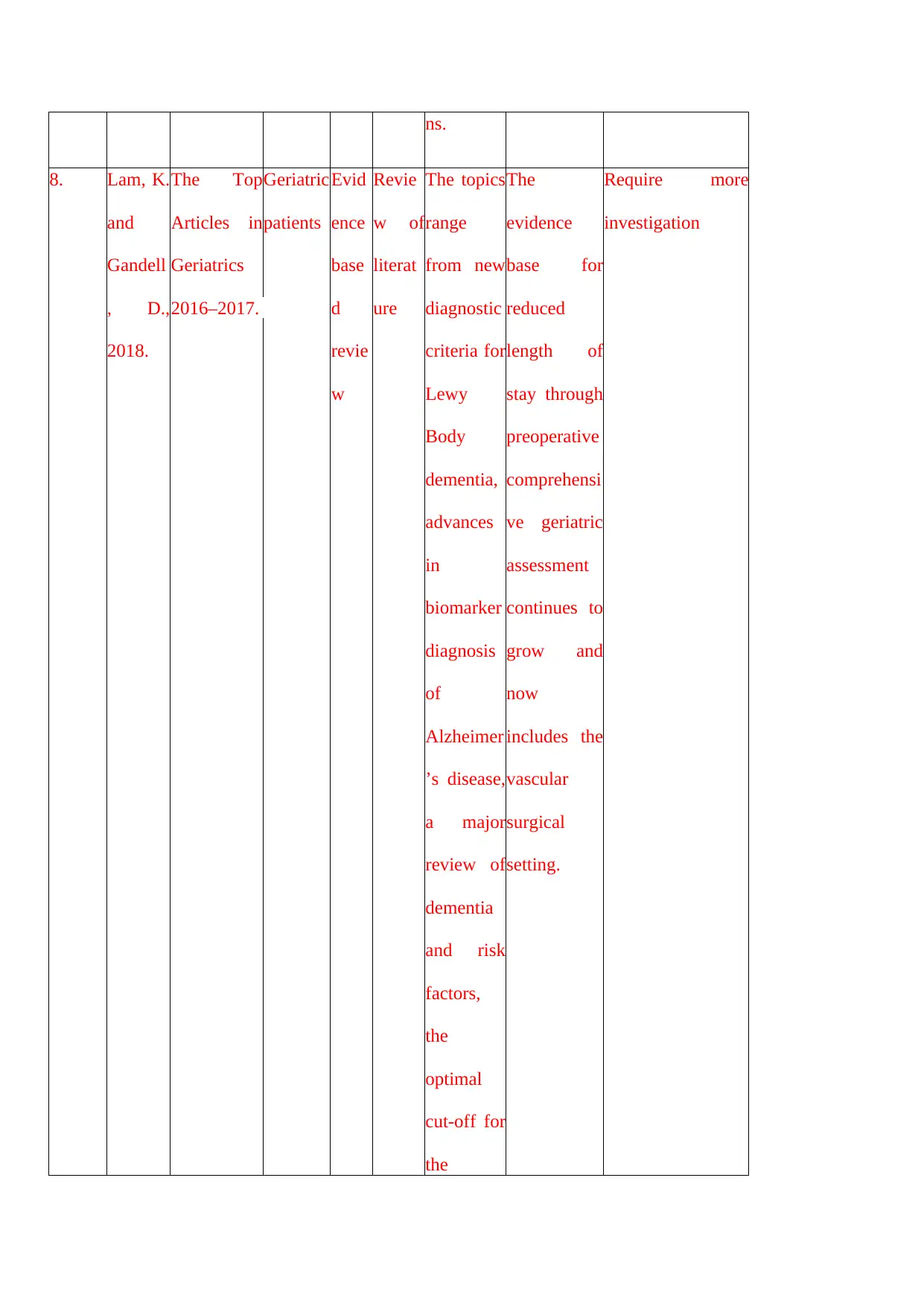
ns.
8. Lam, K.
and
Gandell
, D.,
2018.
The Top
Articles in
Geriatrics
2016–2017.
Geriatric
patients
Evid
ence
base
d
revie
w
Revie
w of
literat
ure
The topics
range
from new
diagnostic
criteria for
Lewy
Body
dementia,
advances
in
biomarker
diagnosis
of
Alzheimer
’s disease,
a major
review of
dementia
and risk
factors,
the
optimal
cut-off for
the
The
evidence
base for
reduced
length of
stay through
preoperative
comprehensi
ve geriatric
assessment
continues to
grow and
now
includes the
vascular
surgical
setting.
Require more
investigation
8. Lam, K.
and
Gandell
, D.,
2018.
The Top
Articles in
Geriatrics
2016–2017.
Geriatric
patients
Evid
ence
base
d
revie
w
Revie
w of
literat
ure
The topics
range
from new
diagnostic
criteria for
Lewy
Body
dementia,
advances
in
biomarker
diagnosis
of
Alzheimer
’s disease,
a major
review of
dementia
and risk
factors,
the
optimal
cut-off for
the
The
evidence
base for
reduced
length of
stay through
preoperative
comprehensi
ve geriatric
assessment
continues to
grow and
now
includes the
vascular
surgical
setting.
Require more
investigation
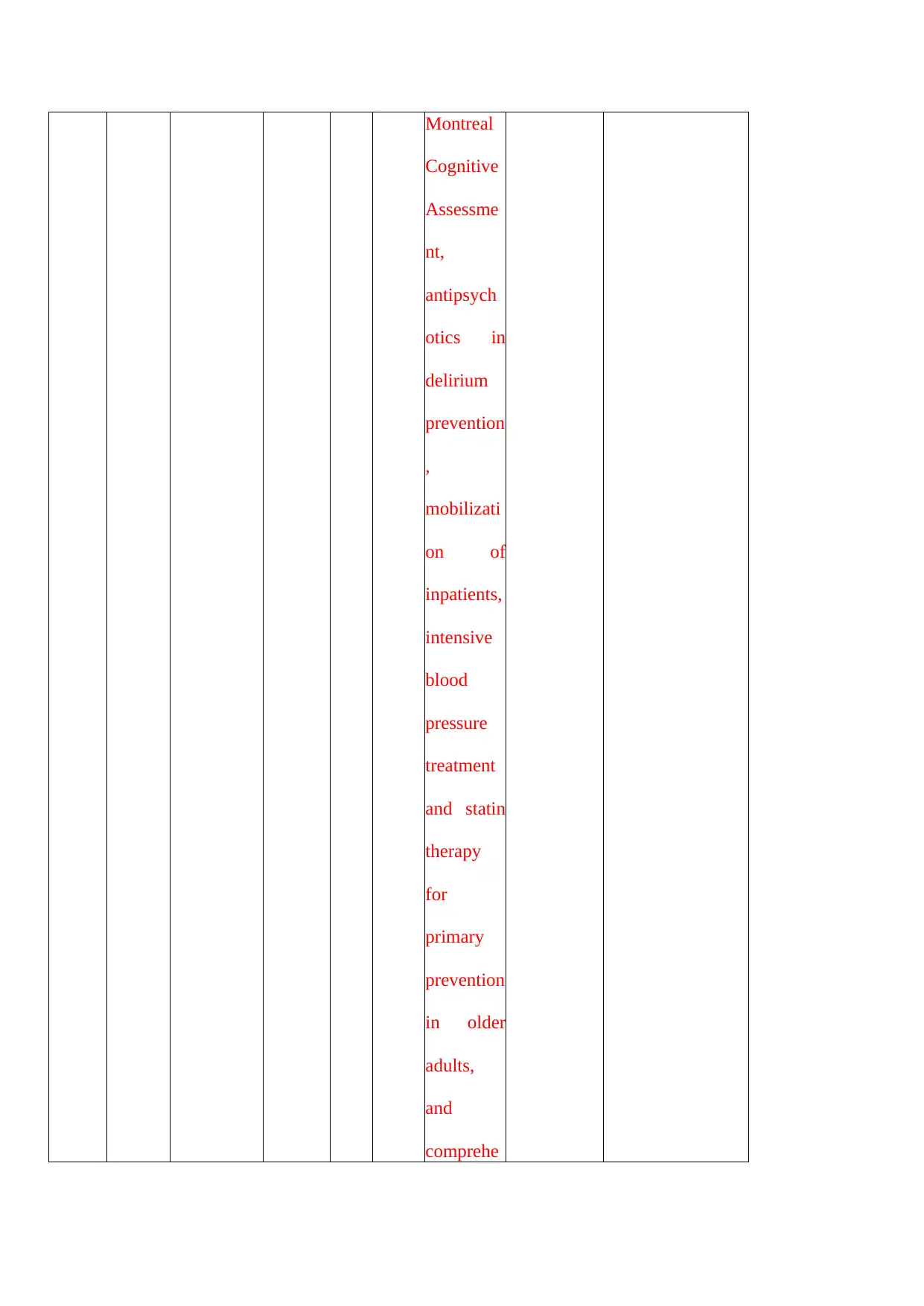
Montreal
Cognitive
Assessme
nt,
antipsych
otics in
delirium
prevention
,
mobilizati
on of
inpatients,
intensive
blood
pressure
treatment
and statin
therapy
for
primary
prevention
in older
adults,
and
comprehe
Cognitive
Assessme
nt,
antipsych
otics in
delirium
prevention
,
mobilizati
on of
inpatients,
intensive
blood
pressure
treatment
and statin
therapy
for
primary
prevention
in older
adults,
and
comprehe
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
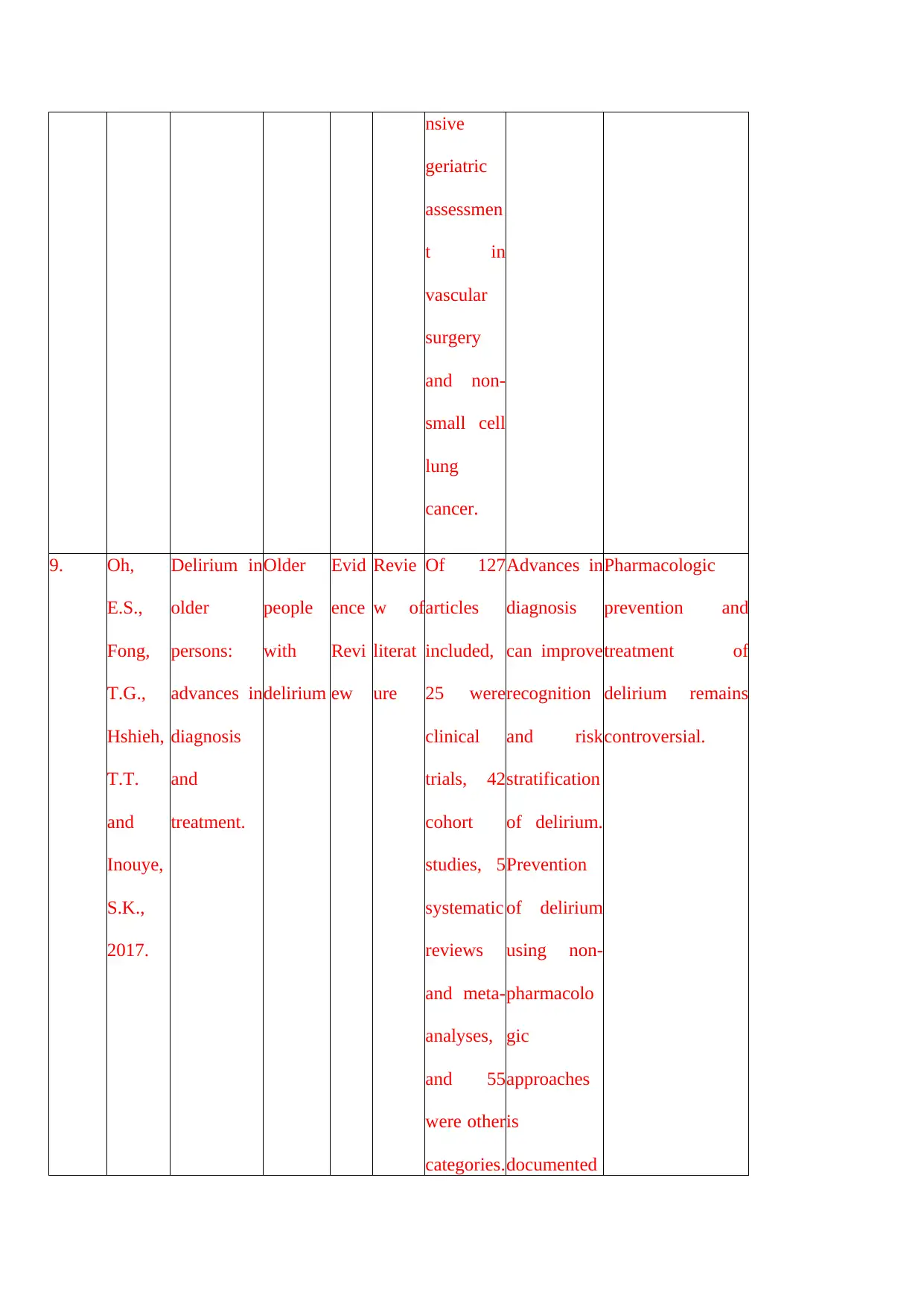
nsive
geriatric
assessmen
t in
vascular
surgery
and non-
small cell
lung
cancer.
9. Oh,
E.S.,
Fong,
T.G.,
Hshieh,
T.T.
and
Inouye,
S.K.,
2017.
Delirium in
older
persons:
advances in
diagnosis
and
treatment.
Older
people
with
delirium
Evid
ence
Revi
ew
Revie
w of
literat
ure
Of 127
articles
included,
25 were
clinical
trials, 42
cohort
studies, 5
systematic
reviews
and meta-
analyses,
and 55
were other
categories.
Advances in
diagnosis
can improve
recognition
and risk
stratification
of delirium.
Prevention
of delirium
using non-
pharmacolo
gic
approaches
is
documented
Pharmacologic
prevention and
treatment of
delirium remains
controversial.
geriatric
assessmen
t in
vascular
surgery
and non-
small cell
lung
cancer.
9. Oh,
E.S.,
Fong,
T.G.,
Hshieh,
T.T.
and
Inouye,
S.K.,
2017.
Delirium in
older
persons:
advances in
diagnosis
and
treatment.
Older
people
with
delirium
Evid
ence
Revi
ew
Revie
w of
literat
ure
Of 127
articles
included,
25 were
clinical
trials, 42
cohort
studies, 5
systematic
reviews
and meta-
analyses,
and 55
were other
categories.
Advances in
diagnosis
can improve
recognition
and risk
stratification
of delirium.
Prevention
of delirium
using non-
pharmacolo
gic
approaches
is
documented
Pharmacologic
prevention and
treatment of
delirium remains
controversial.
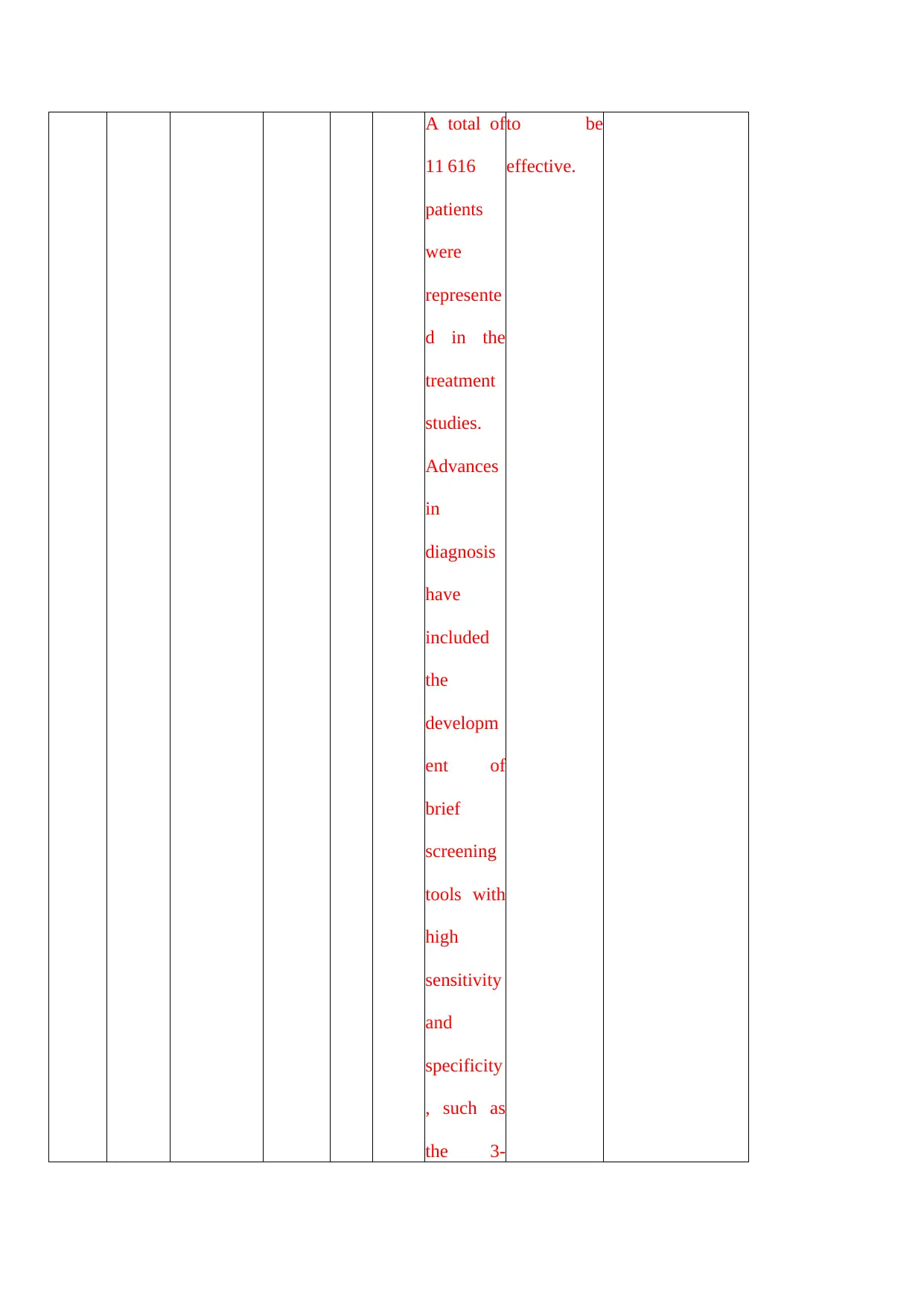
A total of
11 616
patients
were
represente
d in the
treatment
studies.
Advances
in
diagnosis
have
included
the
developm
ent of
brief
screening
tools with
high
sensitivity
and
specificity
, such as
the 3-
to be
effective.
11 616
patients
were
represente
d in the
treatment
studies.
Advances
in
diagnosis
have
included
the
developm
ent of
brief
screening
tools with
high
sensitivity
and
specificity
, such as
the 3-
to be
effective.
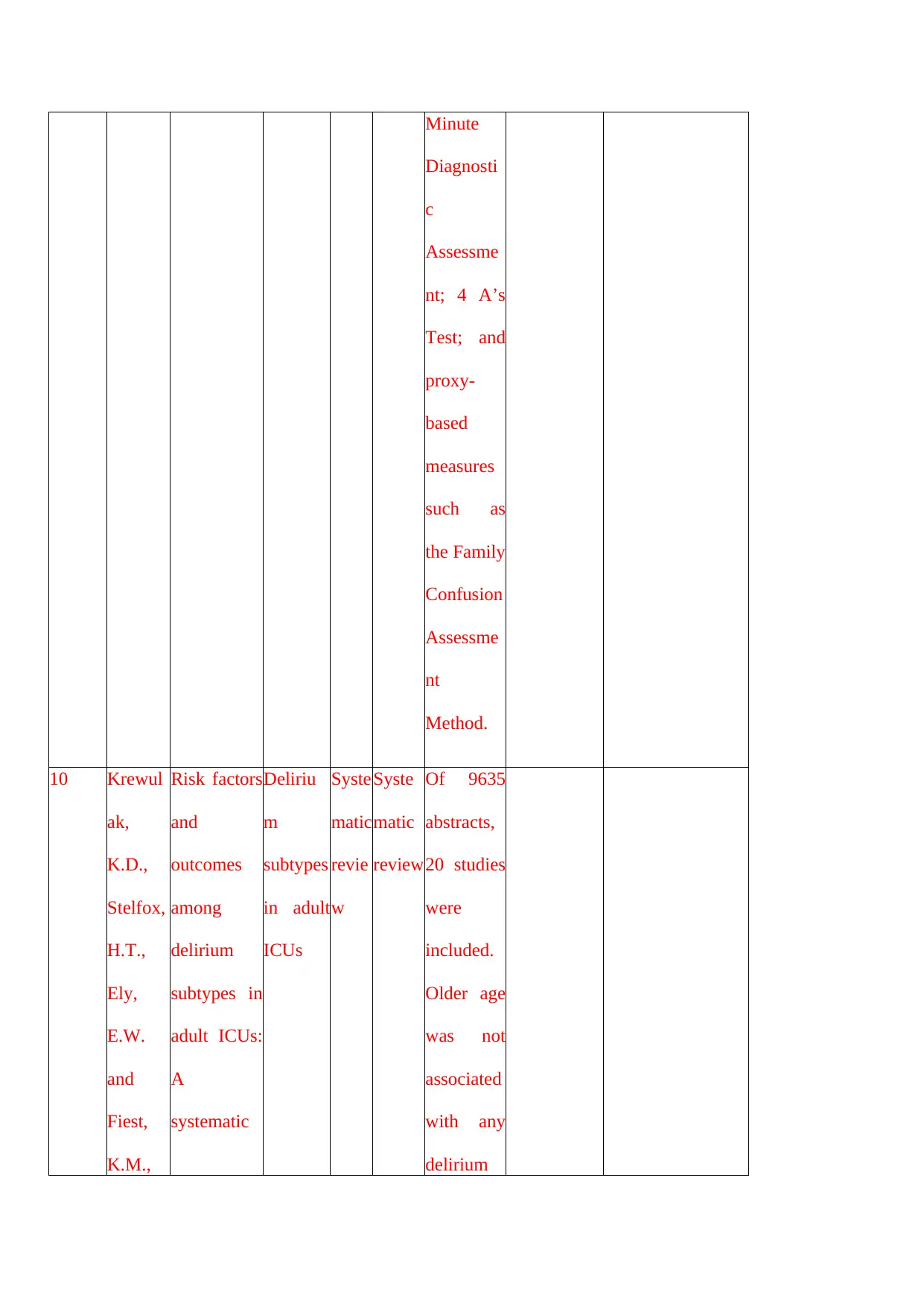
Minute
Diagnosti
c
Assessme
nt; 4 A’s
Test; and
proxy-
based
measures
such as
the Family
Confusion
Assessme
nt
Method.
10 Krewul
ak,
K.D.,
Stelfox,
H.T.,
Ely,
E.W.
and
Fiest,
K.M.,
Risk factors
and
outcomes
among
delirium
subtypes in
adult ICUs:
A
systematic
Deliriu
m
subtypes
in adult
ICUs
Syste
matic
revie
w
Syste
matic
review
Of 9635
abstracts,
20 studies
were
included.
Older age
was not
associated
with any
delirium
Diagnosti
c
Assessme
nt; 4 A’s
Test; and
proxy-
based
measures
such as
the Family
Confusion
Assessme
nt
Method.
10 Krewul
ak,
K.D.,
Stelfox,
H.T.,
Ely,
E.W.
and
Fiest,
K.M.,
Risk factors
and
outcomes
among
delirium
subtypes in
adult ICUs:
A
systematic
Deliriu
m
subtypes
in adult
ICUs
Syste
matic
revie
w
Syste
matic
review
Of 9635
abstracts,
20 studies
were
included.
Older age
was not
associated
with any
delirium
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
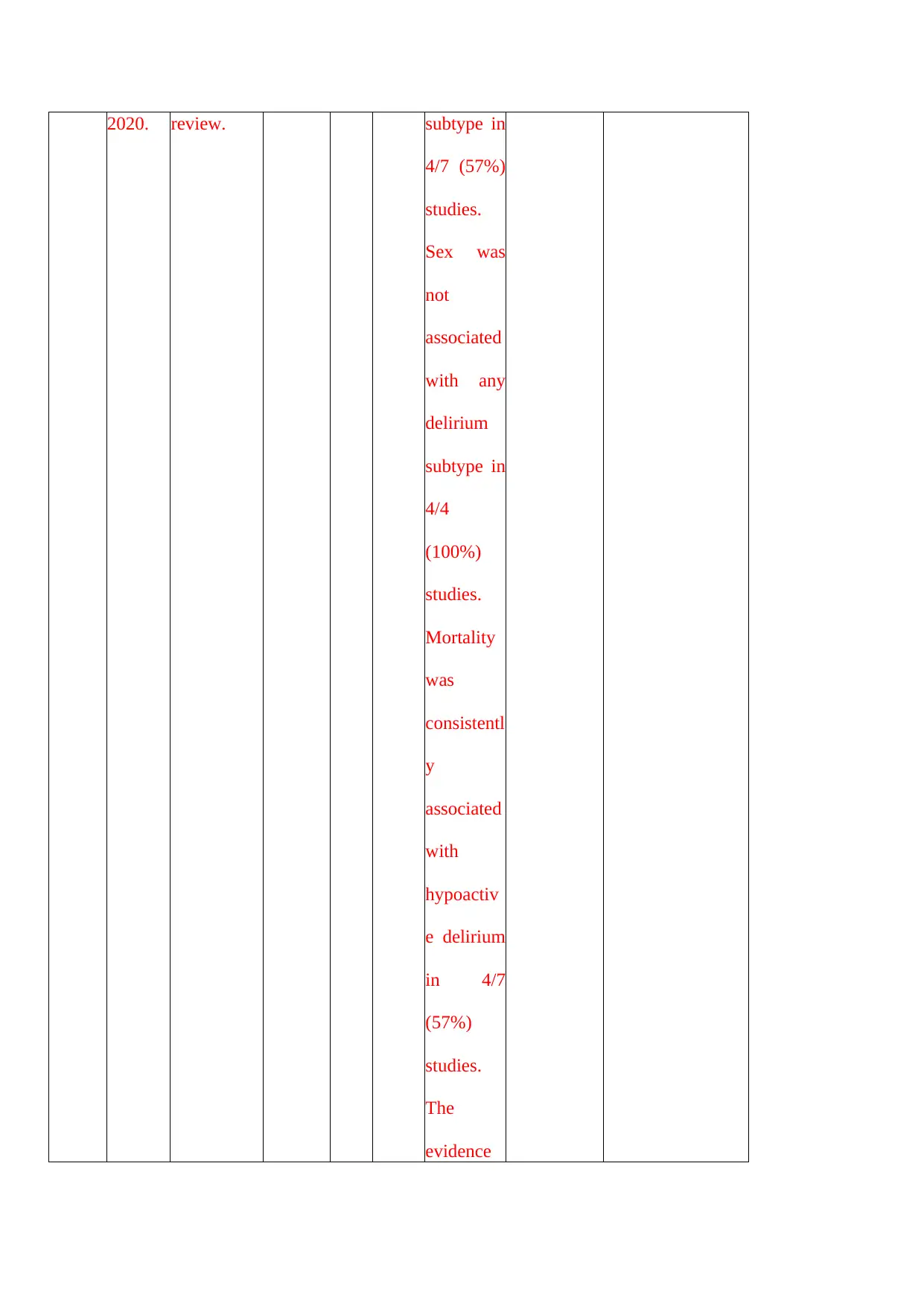
2020. review. subtype in
4/7 (57%)
studies.
Sex was
not
associated
with any
delirium
subtype in
4/4
(100%)
studies.
Mortality
was
consistentl
y
associated
with
hypoactiv
e delirium
in 4/7
(57%)
studies.
The
evidence
4/7 (57%)
studies.
Sex was
not
associated
with any
delirium
subtype in
4/4
(100%)
studies.
Mortality
was
consistentl
y
associated
with
hypoactiv
e delirium
in 4/7
(57%)
studies.
The
evidence
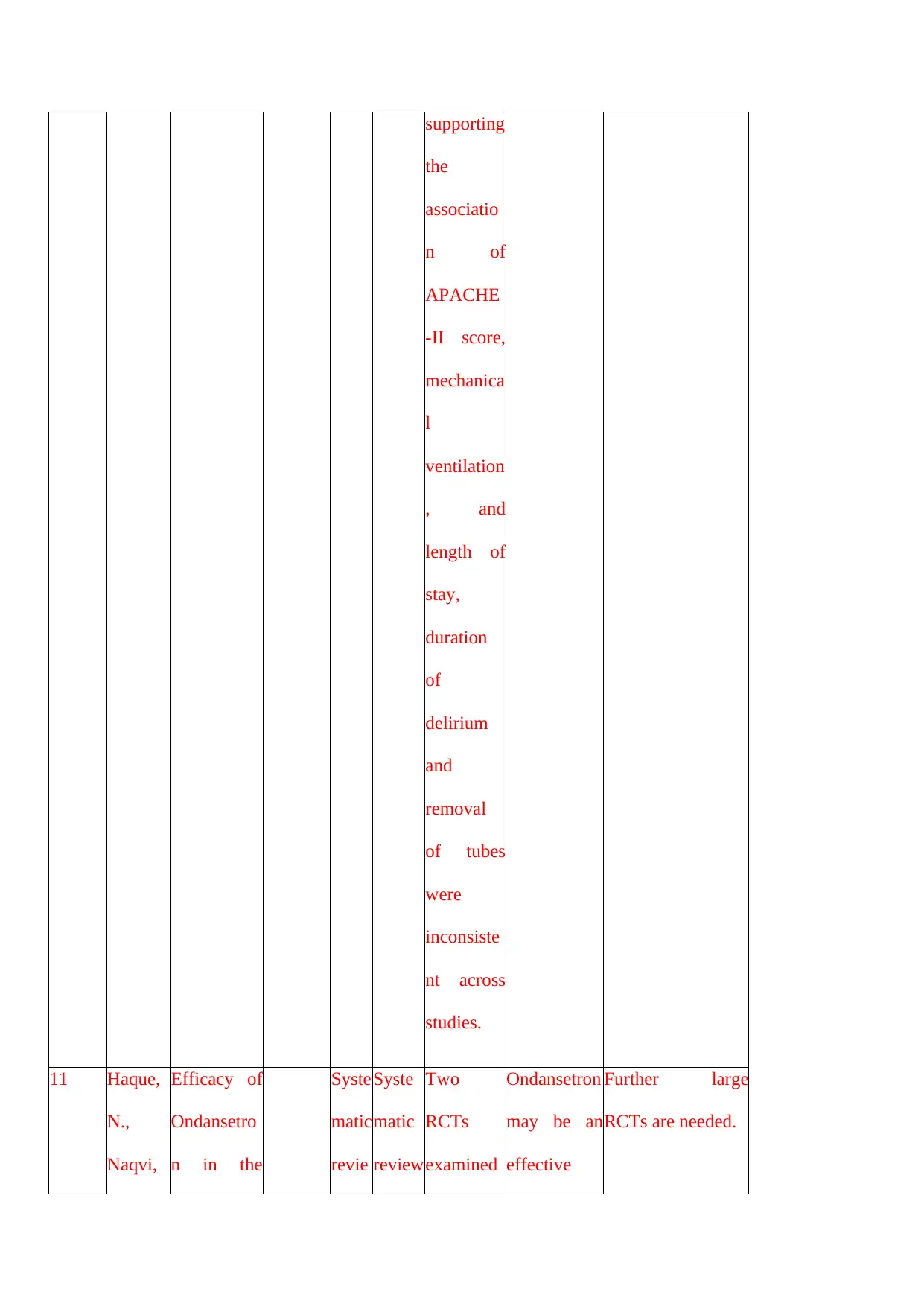
supporting
the
associatio
n of
APACHE
-II score,
mechanica
l
ventilation
, and
length of
stay,
duration
of
delirium
and
removal
of tubes
were
inconsiste
nt across
studies.
11 Haque,
N.,
Naqvi,
Efficacy of
Ondansetro
n in the
Syste
matic
revie
Syste
matic
review
Two
RCTs
examined
Ondansetron
may be an
effective
Further large
RCTs are needed.
the
associatio
n of
APACHE
-II score,
mechanica
l
ventilation
, and
length of
stay,
duration
of
delirium
and
removal
of tubes
were
inconsiste
nt across
studies.
11 Haque,
N.,
Naqvi,
Efficacy of
Ondansetro
n in the
Syste
matic
revie
Syste
matic
review
Two
RCTs
examined
Ondansetron
may be an
effective
Further large
RCTs are needed.
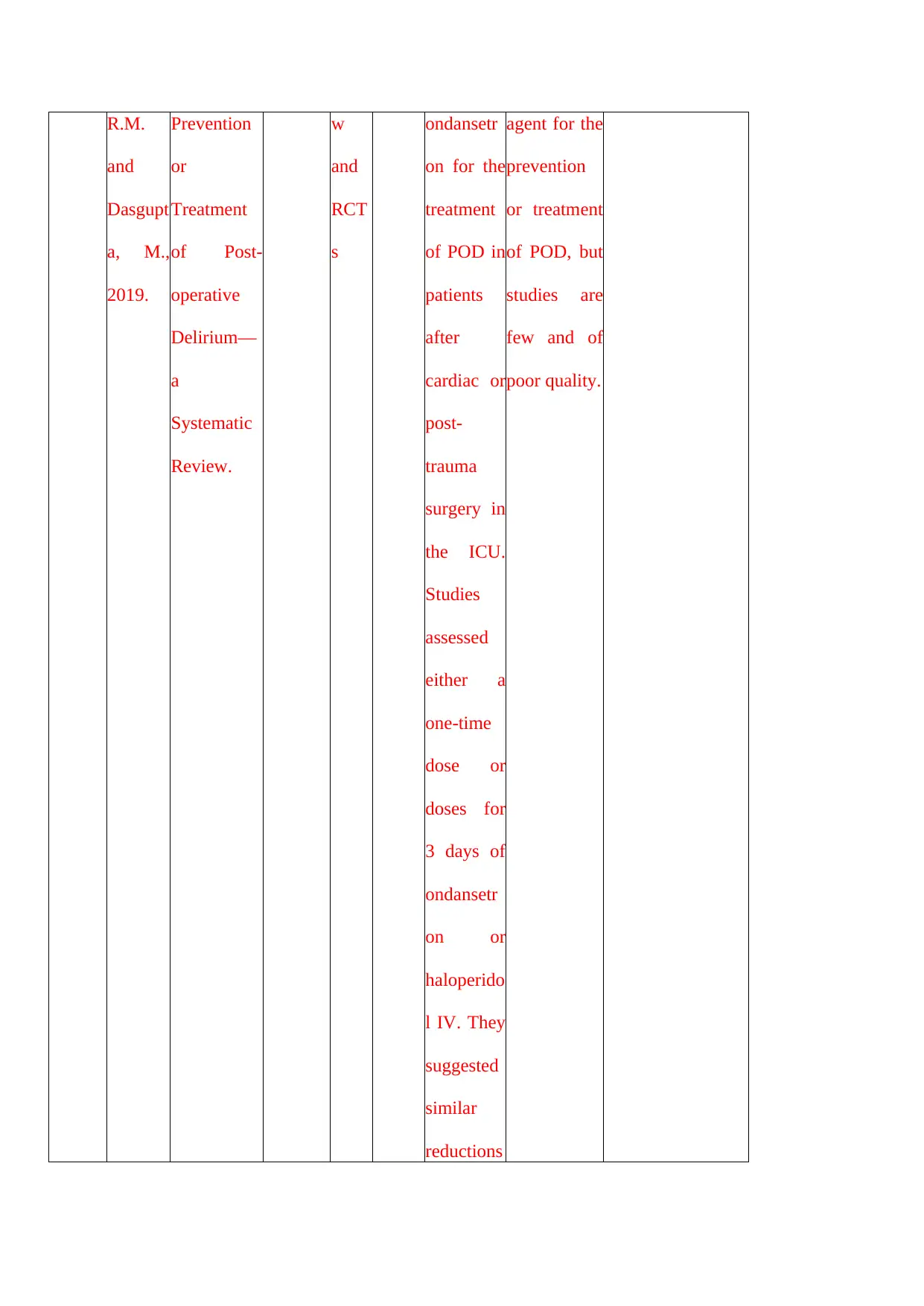
R.M.
and
Dasgupt
a, M.,
2019.
Prevention
or
Treatment
of Post-
operative
Delirium—
a
Systematic
Review.
w
and
RCT
s
ondansetr
on for the
treatment
of POD in
patients
after
cardiac or
post-
trauma
surgery in
the ICU.
Studies
assessed
either a
one-time
dose or
doses for
3 days of
ondansetr
on or
haloperido
l IV. They
suggested
similar
reductions
agent for the
prevention
or treatment
of POD, but
studies are
few and of
poor quality.
and
Dasgupt
a, M.,
2019.
Prevention
or
Treatment
of Post-
operative
Delirium—
a
Systematic
Review.
w
and
RCT
s
ondansetr
on for the
treatment
of POD in
patients
after
cardiac or
post-
trauma
surgery in
the ICU.
Studies
assessed
either a
one-time
dose or
doses for
3 days of
ondansetr
on or
haloperido
l IV. They
suggested
similar
reductions
agent for the
prevention
or treatment
of POD, but
studies are
few and of
poor quality.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
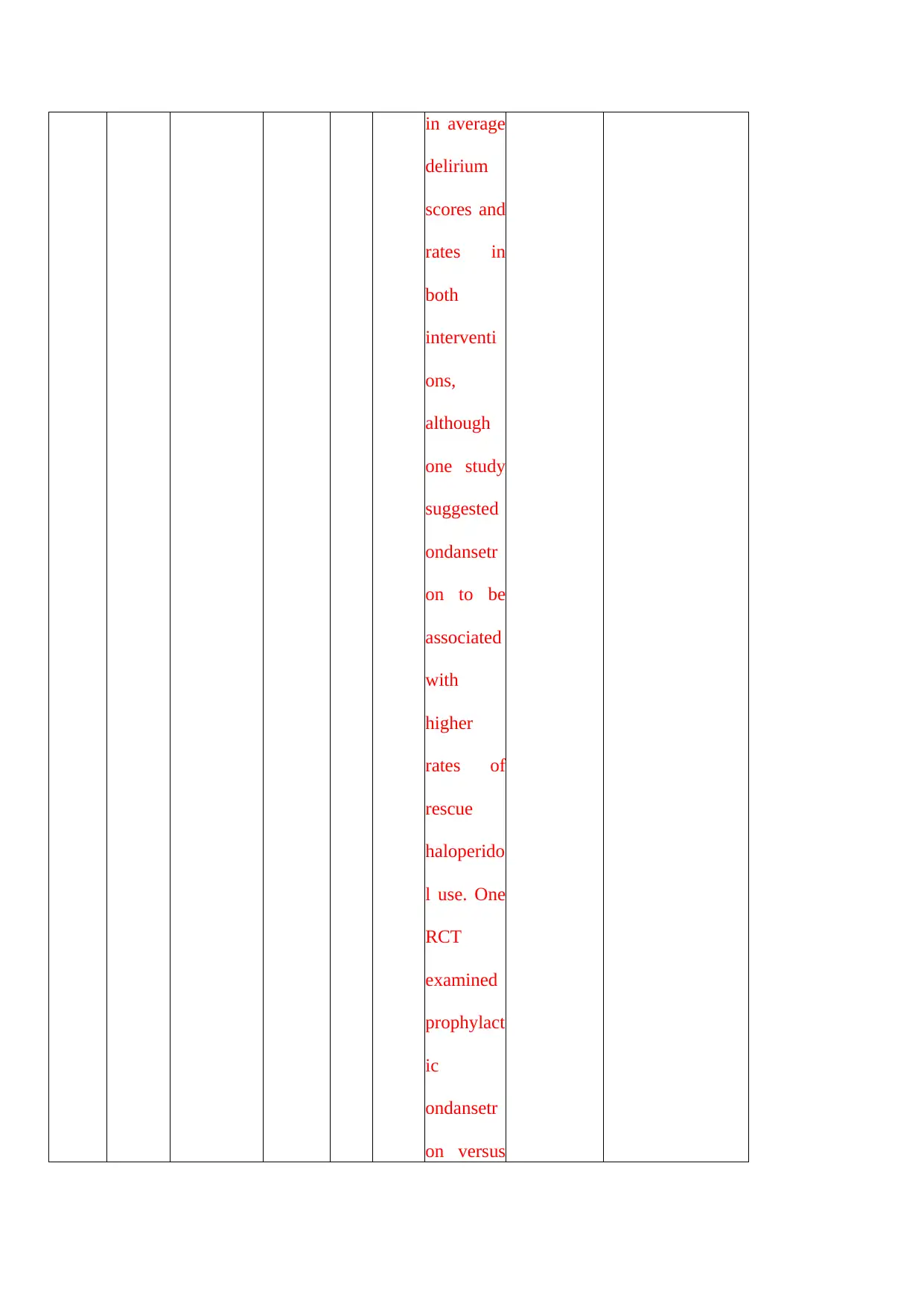
in average
delirium
scores and
rates in
both
interventi
ons,
although
one study
suggested
ondansetr
on to be
associated
with
higher
rates of
rescue
haloperido
l use. One
RCT
examined
prophylact
ic
ondansetr
on versus
delirium
scores and
rates in
both
interventi
ons,
although
one study
suggested
ondansetr
on to be
associated
with
higher
rates of
rescue
haloperido
l use. One
RCT
examined
prophylact
ic
ondansetr
on versus
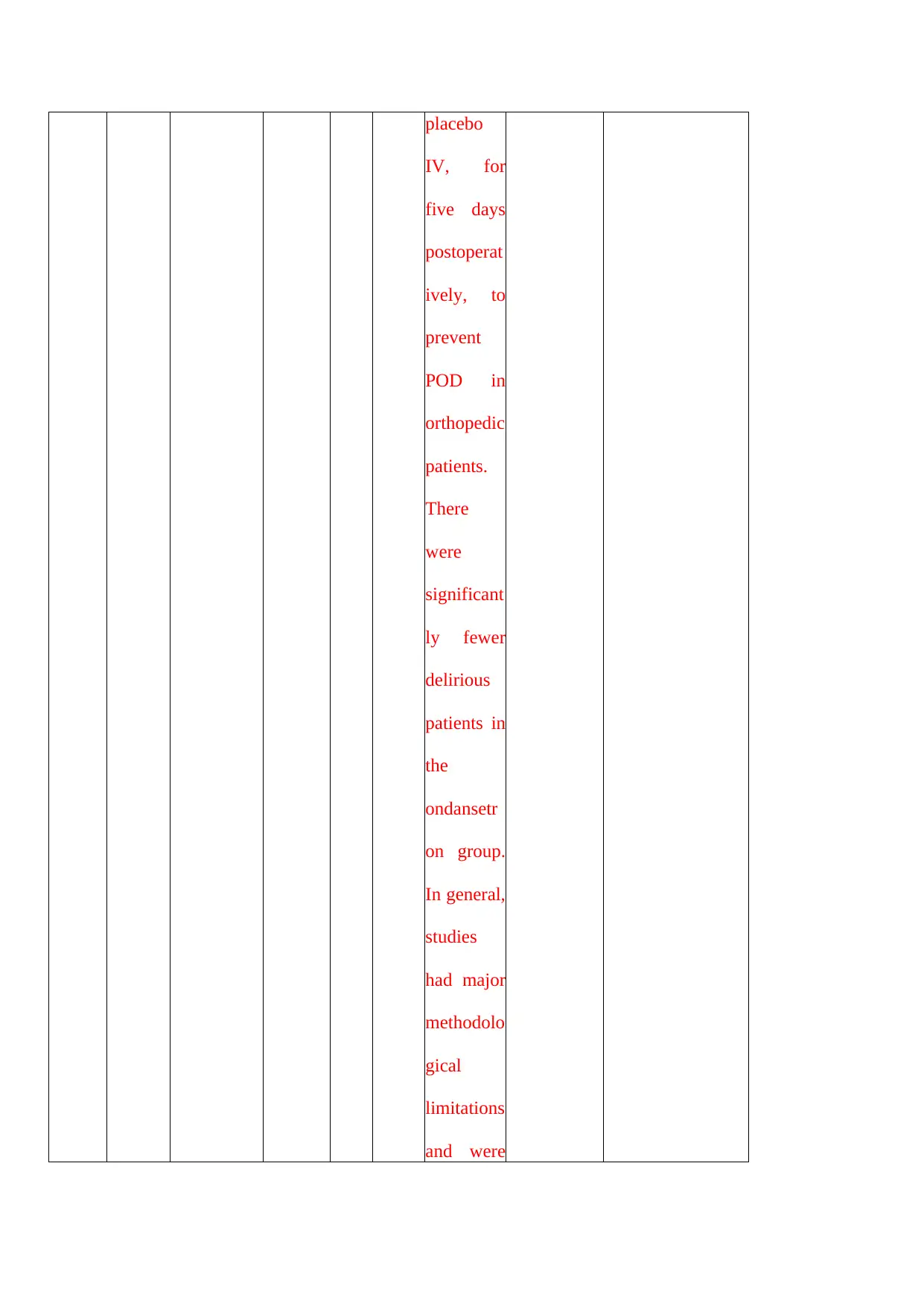
placebo
IV, for
five days
postoperat
ively, to
prevent
POD in
orthopedic
patients.
There
were
significant
ly fewer
delirious
patients in
the
ondansetr
on group.
In general,
studies
had major
methodolo
gical
limitations
and were
IV, for
five days
postoperat
ively, to
prevent
POD in
orthopedic
patients.
There
were
significant
ly fewer
delirious
patients in
the
ondansetr
on group.
In general,
studies
had major
methodolo
gical
limitations
and were
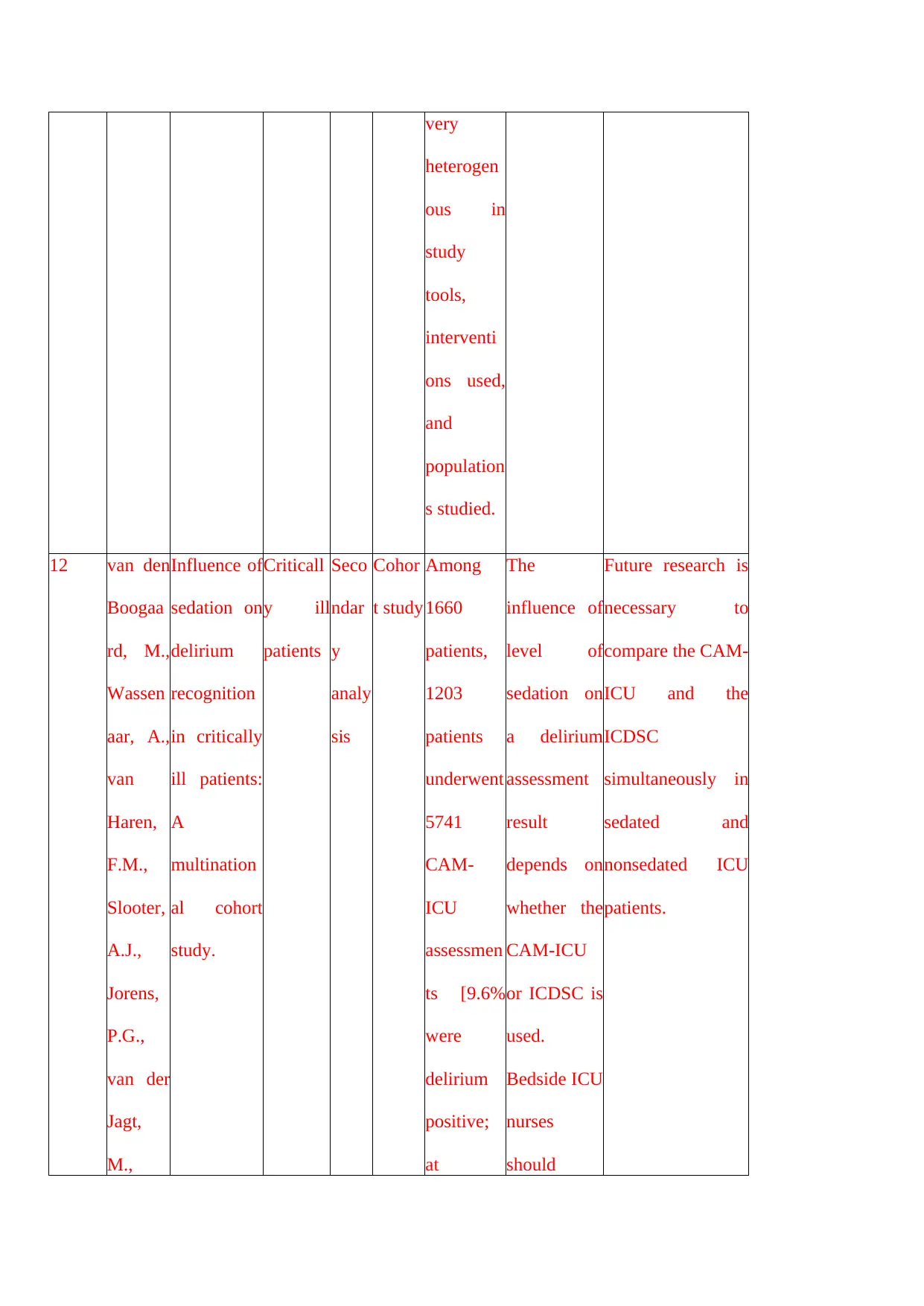
very
heterogen
ous in
study
tools,
interventi
ons used,
and
population
s studied.
12 van den
Boogaa
rd, M.,
Wassen
aar, A.,
van
Haren,
F.M.,
Slooter,
A.J.,
Jorens,
P.G.,
van der
Jagt,
M.,
Influence of
sedation on
delirium
recognition
in critically
ill patients:
A
multination
al cohort
study.
Criticall
y ill
patients
Seco
ndar
y
analy
sis
Cohor
t study
Among
1660
patients,
1203
patients
underwent
5741
CAM-
ICU
assessmen
ts [9.6%
were
delirium
positive;
at
The
influence of
level of
sedation on
a delirium
assessment
result
depends on
whether the
CAM-ICU
or ICDSC is
used.
Bedside ICU
nurses
should
Future research is
necessary to
compare the CAM-
ICU and the
ICDSC
simultaneously in
sedated and
nonsedated ICU
patients.
heterogen
ous in
study
tools,
interventi
ons used,
and
population
s studied.
12 van den
Boogaa
rd, M.,
Wassen
aar, A.,
van
Haren,
F.M.,
Slooter,
A.J.,
Jorens,
P.G.,
van der
Jagt,
M.,
Influence of
sedation on
delirium
recognition
in critically
ill patients:
A
multination
al cohort
study.
Criticall
y ill
patients
Seco
ndar
y
analy
sis
Cohor
t study
Among
1660
patients,
1203
patients
underwent
5741
CAM-
ICU
assessmen
ts [9.6%
were
delirium
positive;
at
The
influence of
level of
sedation on
a delirium
assessment
result
depends on
whether the
CAM-ICU
or ICDSC is
used.
Bedside ICU
nurses
should
Future research is
necessary to
compare the CAM-
ICU and the
ICDSC
simultaneously in
sedated and
nonsedated ICU
patients.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
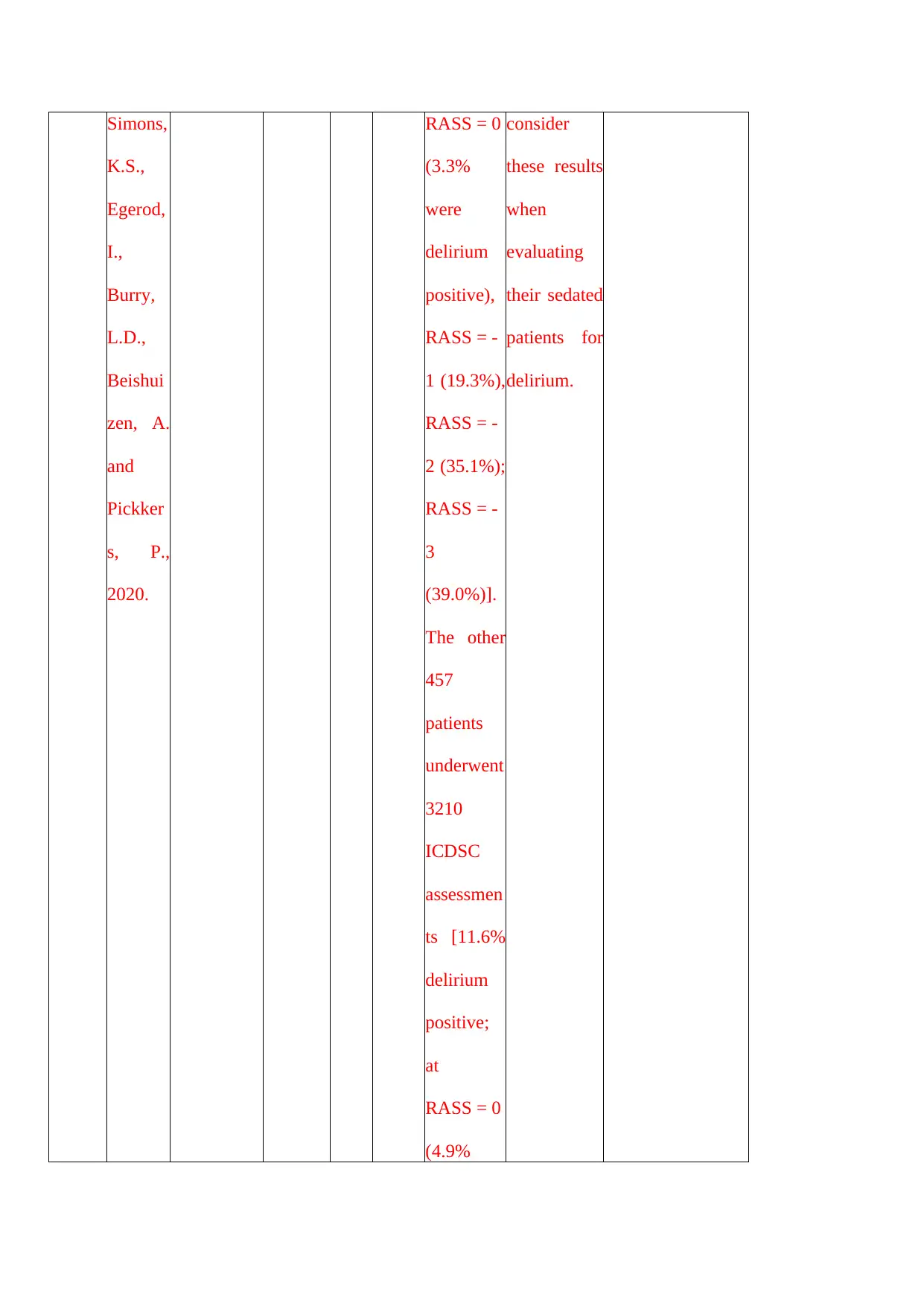
Simons,
K.S.,
Egerod,
I.,
Burry,
L.D.,
Beishui
zen, A.
and
Pickker
s, P.,
2020.
RASS = 0
(3.3%
were
delirium
positive),
RASS = -
1 (19.3%),
RASS = -
2 (35.1%);
RASS = -
3
(39.0%)].
The other
457
patients
underwent
3210
ICDSC
assessmen
ts [11.6%
delirium
positive;
at
RASS = 0
(4.9%
consider
these results
when
evaluating
their sedated
patients for
delirium.
K.S.,
Egerod,
I.,
Burry,
L.D.,
Beishui
zen, A.
and
Pickker
s, P.,
2020.
RASS = 0
(3.3%
were
delirium
positive),
RASS = -
1 (19.3%),
RASS = -
2 (35.1%);
RASS = -
3
(39.0%)].
The other
457
patients
underwent
3210
ICDSC
assessmen
ts [11.6%
delirium
positive;
at
RASS = 0
(4.9%
consider
these results
when
evaluating
their sedated
patients for
delirium.
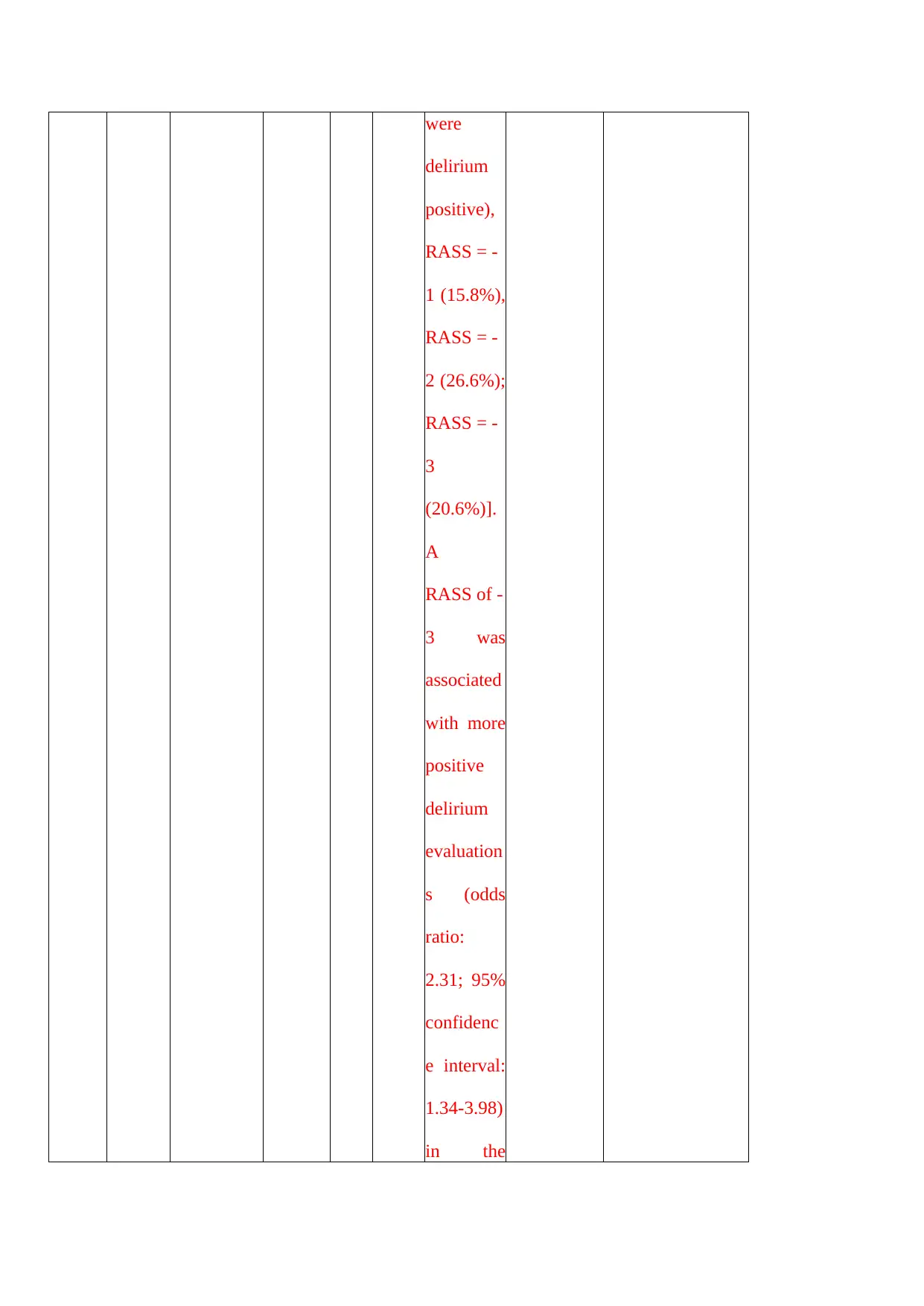
were
delirium
positive),
RASS = -
1 (15.8%),
RASS = -
2 (26.6%);
RASS = -
3
(20.6%)].
A
RASS of -
3 was
associated
with more
positive
delirium
evaluation
s (odds
ratio:
2.31; 95%
confidenc
e interval:
1.34-3.98)
in the
delirium
positive),
RASS = -
1 (15.8%),
RASS = -
2 (26.6%);
RASS = -
3
(20.6%)].
A
RASS of -
3 was
associated
with more
positive
delirium
evaluation
s (odds
ratio:
2.31; 95%
confidenc
e interval:
1.34-3.98)
in the
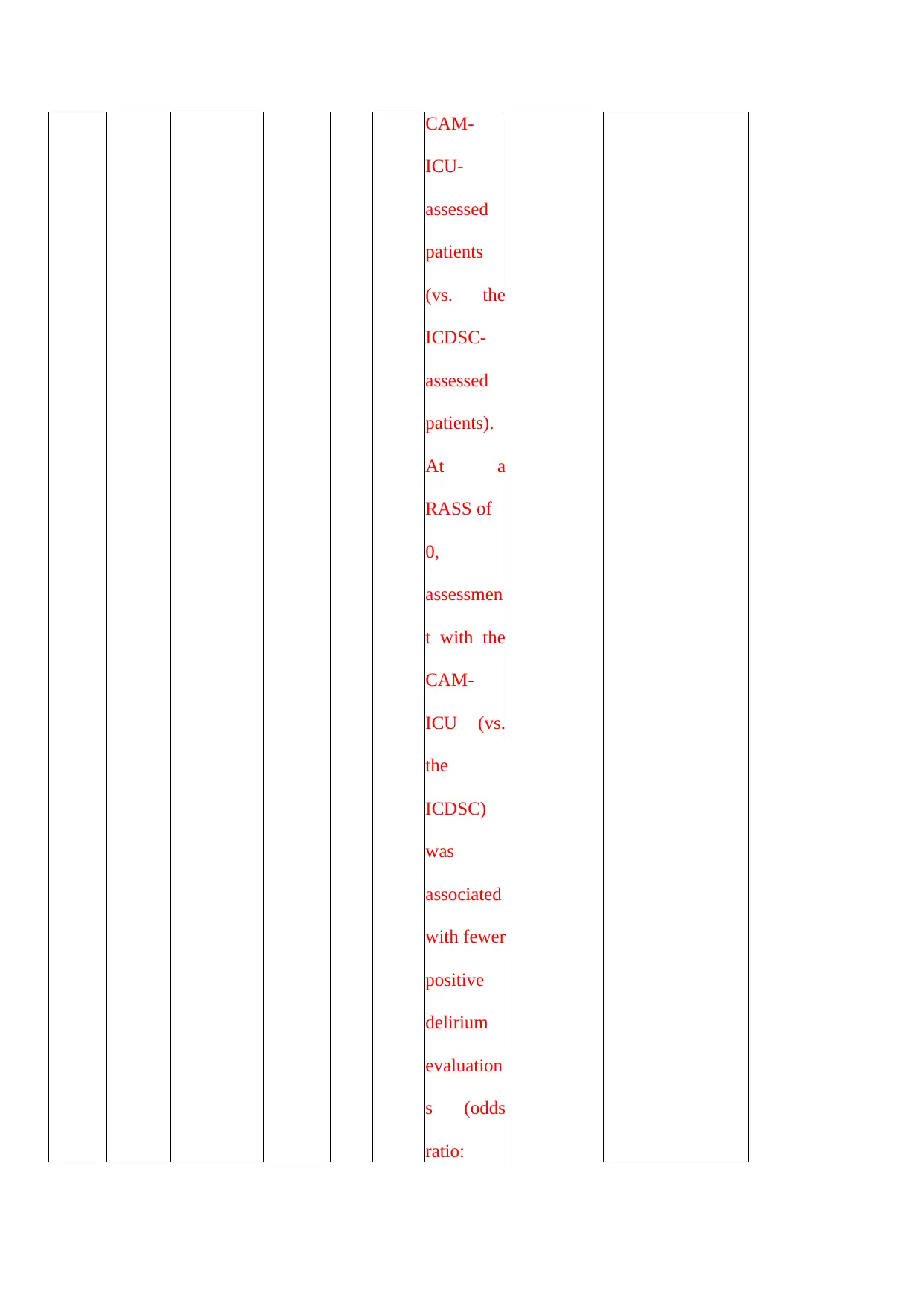
CAM-
ICU-
assessed
patients
(vs. the
ICDSC-
assessed
patients).
At a
RASS of
0,
assessmen
t with the
CAM-
ICU (vs.
the
ICDSC)
was
associated
with fewer
positive
delirium
evaluation
s (odds
ratio:
ICU-
assessed
patients
(vs. the
ICDSC-
assessed
patients).
At a
RASS of
0,
assessmen
t with the
CAM-
ICU (vs.
the
ICDSC)
was
associated
with fewer
positive
delirium
evaluation
s (odds
ratio:
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
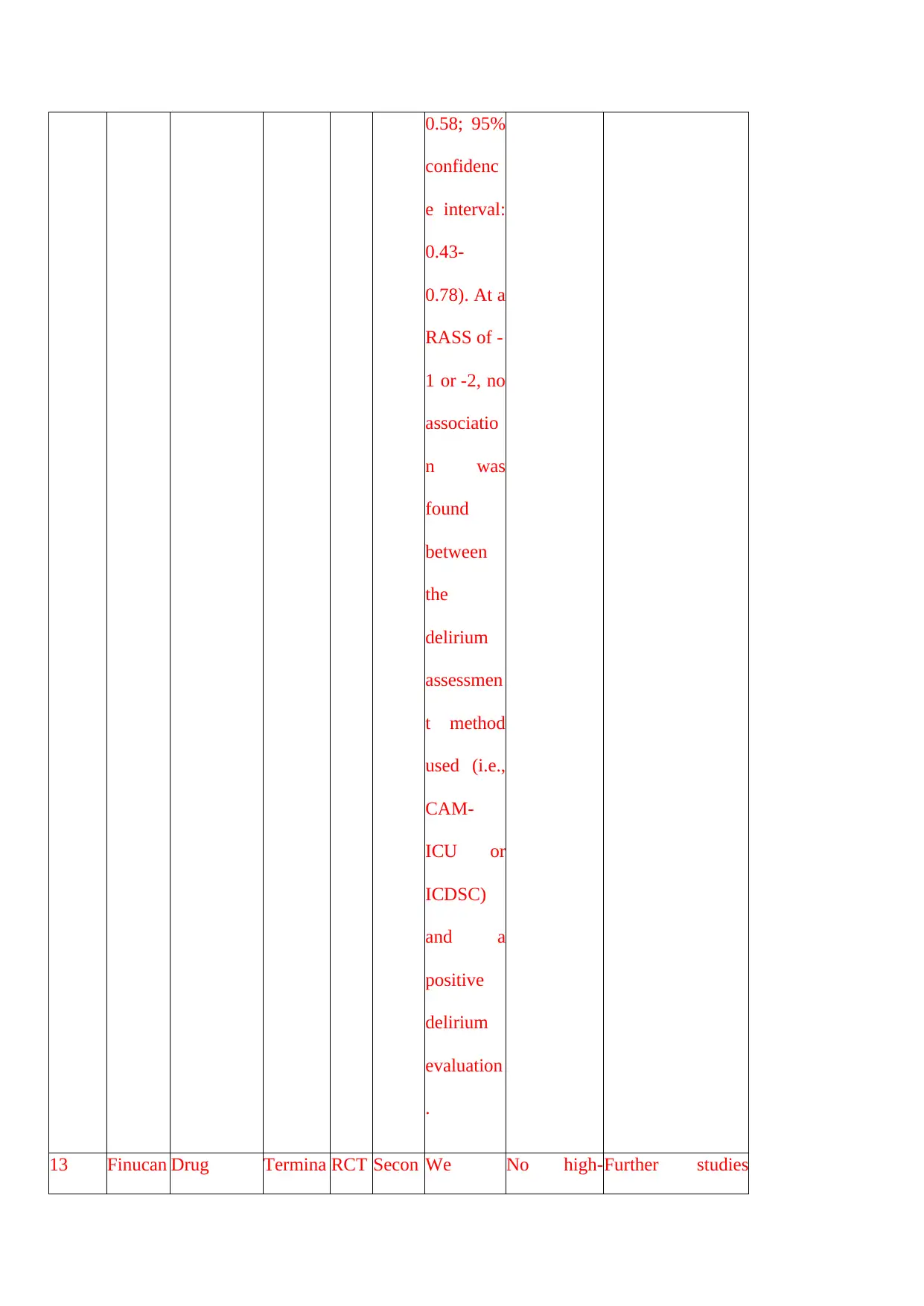
0.58; 95%
confidenc
e interval:
0.43-
0.78). At a
RASS of -
1 or -2, no
associatio
n was
found
between
the
delirium
assessmen
t method
used (i.e.,
CAM-
ICU or
ICDSC)
and a
positive
delirium
evaluation
.
13 Finucan Drug Termina RCT Secon We No high‐Further studies
confidenc
e interval:
0.43-
0.78). At a
RASS of -
1 or -2, no
associatio
n was
found
between
the
delirium
assessmen
t method
used (i.e.,
CAM-
ICU or
ICDSC)
and a
positive
delirium
evaluation
.
13 Finucan Drug Termina RCT Secon We No high‐Further studies
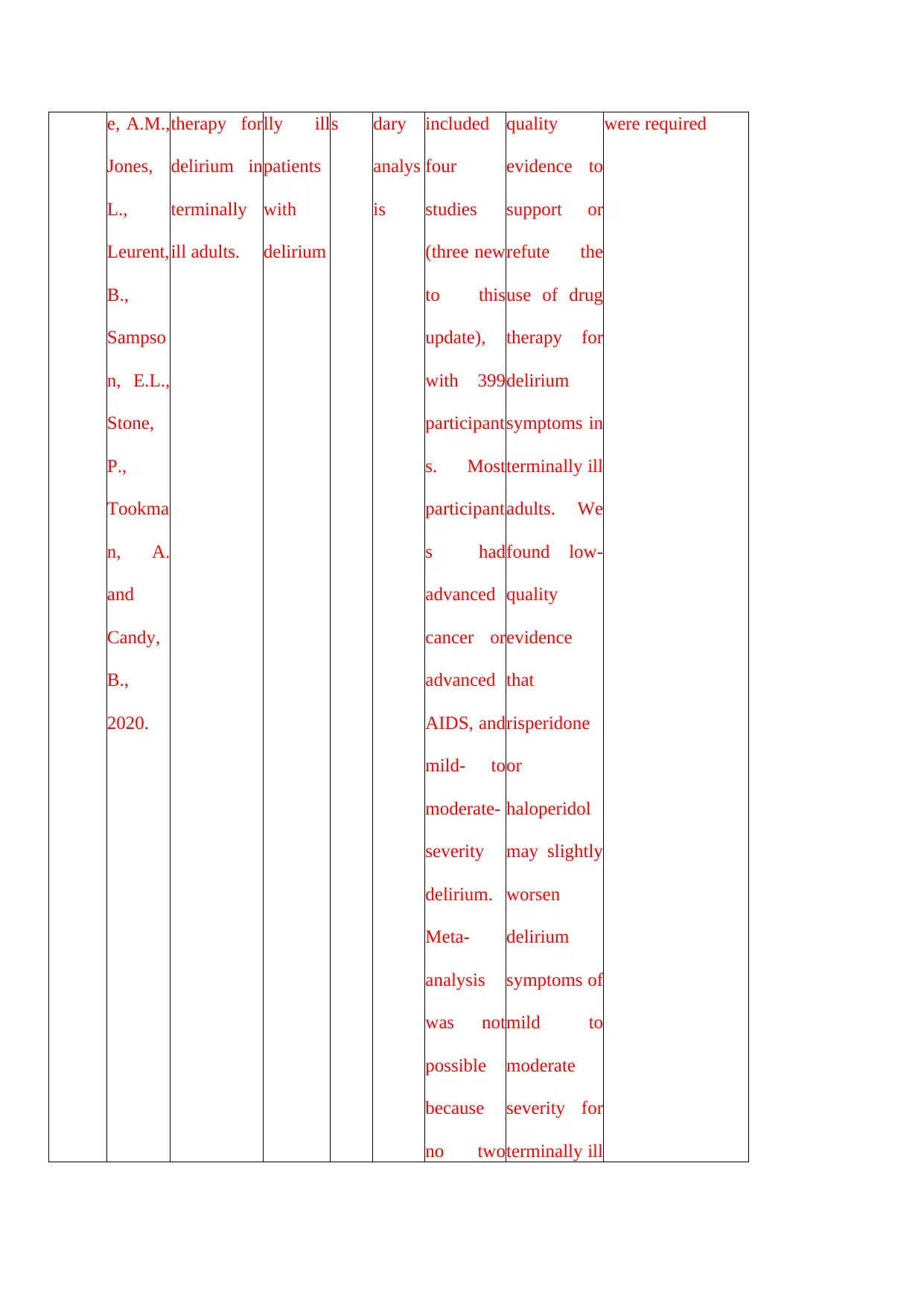
e, A.M.,
Jones,
L.,
Leurent,
B.,
Sampso
n, E.L.,
Stone,
P.,
Tookma
n, A.
and
Candy,
B.,
2020.
therapy for
delirium in
terminally
ill adults.
lly ill
patients
with
delirium
s dary
analys
is
included
four
studies
(three new
to this
update),
with 399
participant
s. Most
participant
s had
advanced
cancer or
advanced
AIDS, and
mild‐ to
moderate‐
severity
delirium.
Meta‐
analysis
was not
possible
because
no two
quality
evidence to
support or
refute the
use of drug
therapy for
delirium
symptoms in
terminally ill
adults. We
found low‐
quality
evidence
that
risperidone
or
haloperidol
may slightly
worsen
delirium
symptoms of
mild to
moderate
severity for
terminally ill
were required
Jones,
L.,
Leurent,
B.,
Sampso
n, E.L.,
Stone,
P.,
Tookma
n, A.
and
Candy,
B.,
2020.
therapy for
delirium in
terminally
ill adults.
lly ill
patients
with
delirium
s dary
analys
is
included
four
studies
(three new
to this
update),
with 399
participant
s. Most
participant
s had
advanced
cancer or
advanced
AIDS, and
mild‐ to
moderate‐
severity
delirium.
Meta‐
analysis
was not
possible
because
no two
quality
evidence to
support or
refute the
use of drug
therapy for
delirium
symptoms in
terminally ill
adults. We
found low‐
quality
evidence
that
risperidone
or
haloperidol
may slightly
worsen
delirium
symptoms of
mild to
moderate
severity for
terminally ill
were required
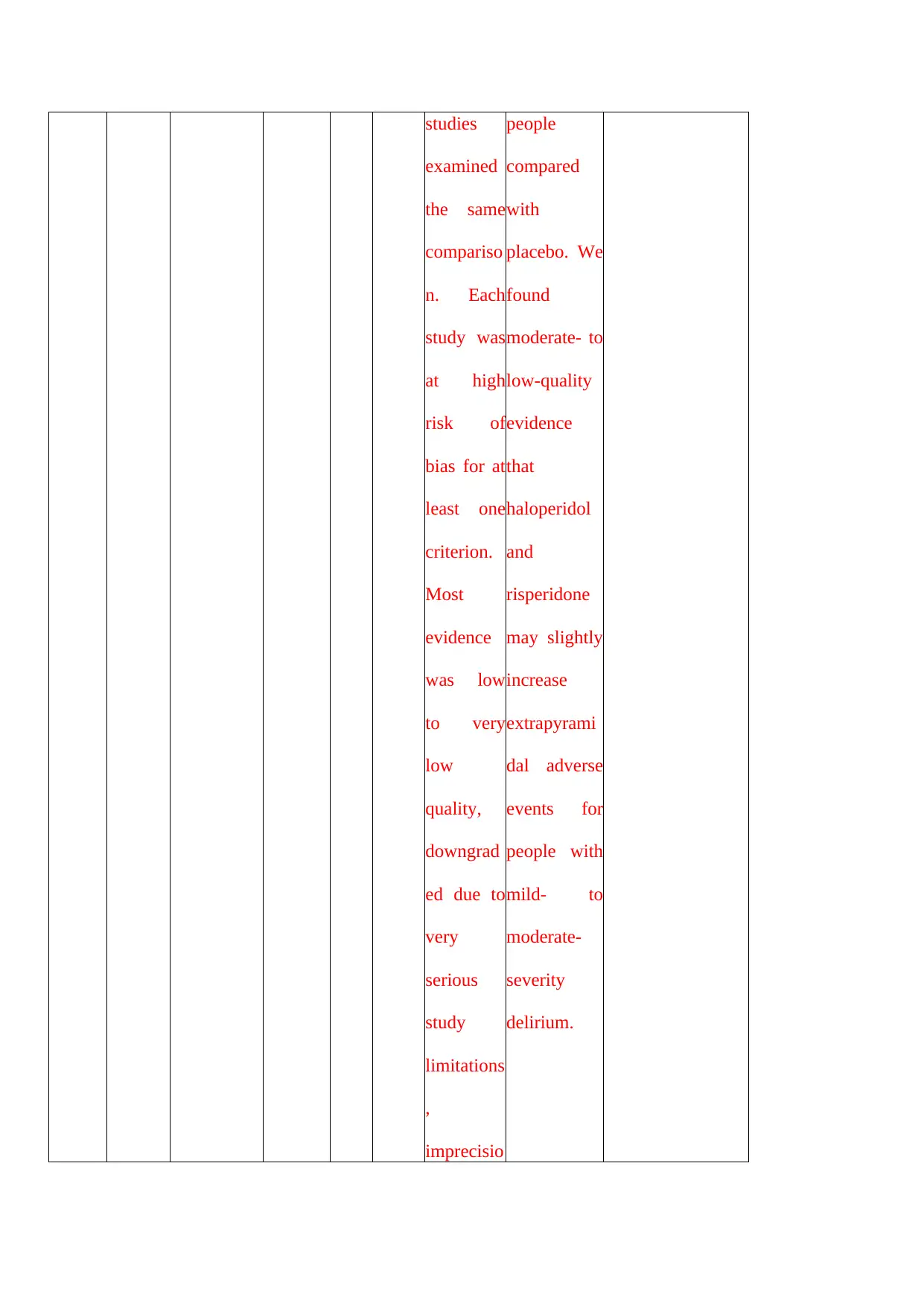
studies
examined
the same
compariso
n. Each
study was
at high
risk of
bias for at
least one
criterion.
Most
evidence
was low
to very
low
quality,
downgrad
ed due to
very
serious
study
limitations
,
imprecisio
people
compared
with
placebo. We
found
moderate‐ to
low‐quality
evidence
that
haloperidol
and
risperidone
may slightly
increase
extrapyrami
dal adverse
events for
people with
mild‐ to
moderate‐
severity
delirium.
examined
the same
compariso
n. Each
study was
at high
risk of
bias for at
least one
criterion.
Most
evidence
was low
to very
low
quality,
downgrad
ed due to
very
serious
study
limitations
,
imprecisio
people
compared
with
placebo. We
found
moderate‐ to
low‐quality
evidence
that
haloperidol
and
risperidone
may slightly
increase
extrapyrami
dal adverse
events for
people with
mild‐ to
moderate‐
severity
delirium.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
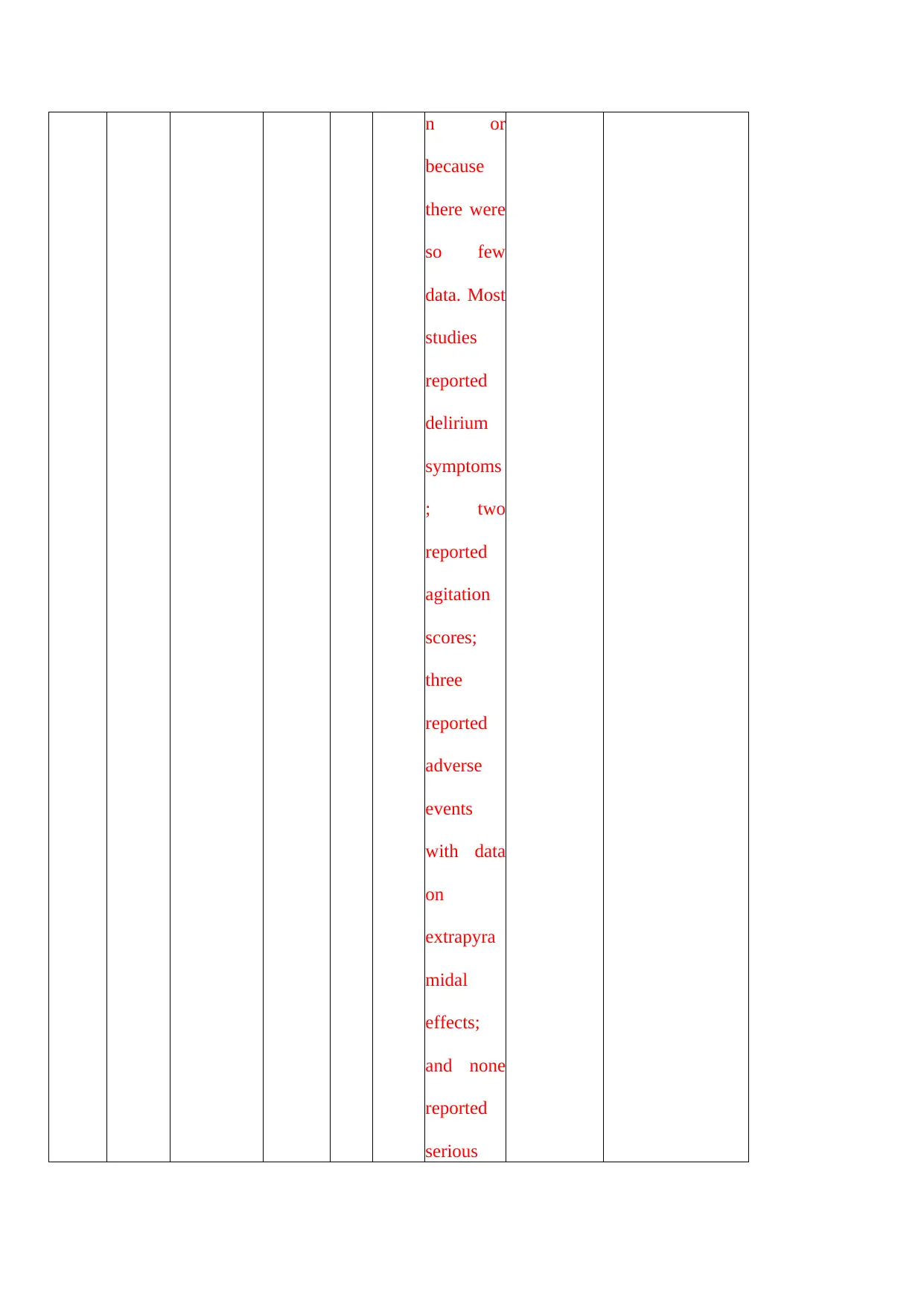
n or
because
there were
so few
data. Most
studies
reported
delirium
symptoms
; two
reported
agitation
scores;
three
reported
adverse
events
with data
on
extrapyra
midal
effects;
and none
reported
serious
because
there were
so few
data. Most
studies
reported
delirium
symptoms
; two
reported
agitation
scores;
three
reported
adverse
events
with data
on
extrapyra
midal
effects;
and none
reported
serious
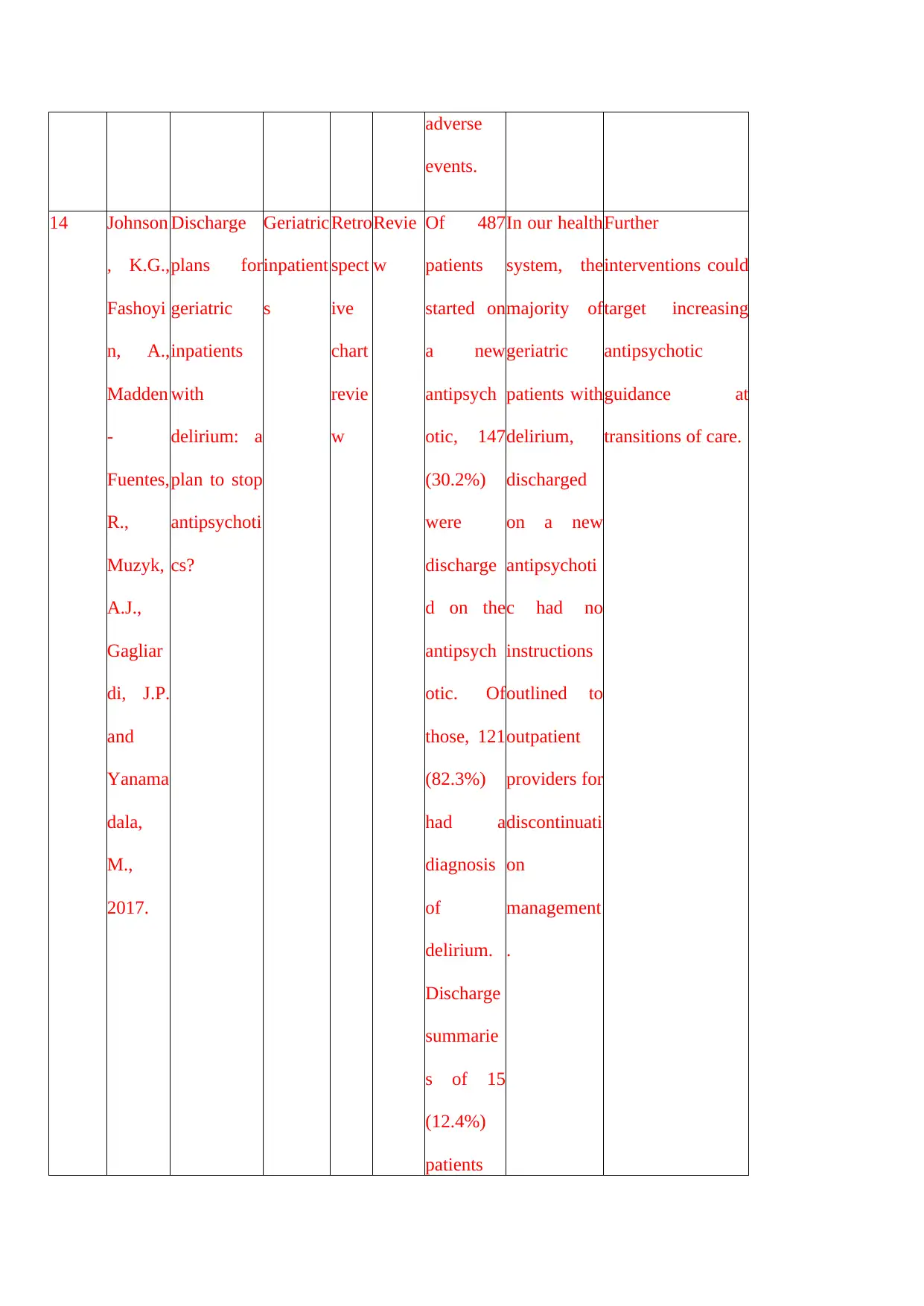
adverse
events.
14 Johnson
, K.G.,
Fashoyi
n, A.,
Madden
‐
Fuentes,
R.,
Muzyk,
A.J.,
Gagliar
di, J.P.
and
Yanama
dala,
M.,
2017.
Discharge
plans for
geriatric
inpatients
with
delirium: a
plan to stop
antipsychoti
cs?
Geriatric
inpatient
s
Retro
spect
ive
chart
revie
w
Revie
w
Of 487
patients
started on
a new
antipsych
otic, 147
(30.2%)
were
discharge
d on the
antipsych
otic. Of
those, 121
(82.3%)
had a
diagnosis
of
delirium.
Discharge
summarie
s of 15
(12.4%)
patients
In our health
system, the
majority of
geriatric
patients with
delirium,
discharged
on a new
antipsychoti
c had no
instructions
outlined to
outpatient
providers for
discontinuati
on
management
.
Further
interventions could
target increasing
antipsychotic
guidance at
transitions of care.
events.
14 Johnson
, K.G.,
Fashoyi
n, A.,
Madden
‐
Fuentes,
R.,
Muzyk,
A.J.,
Gagliar
di, J.P.
and
Yanama
dala,
M.,
2017.
Discharge
plans for
geriatric
inpatients
with
delirium: a
plan to stop
antipsychoti
cs?
Geriatric
inpatient
s
Retro
spect
ive
chart
revie
w
Revie
w
Of 487
patients
started on
a new
antipsych
otic, 147
(30.2%)
were
discharge
d on the
antipsych
otic. Of
those, 121
(82.3%)
had a
diagnosis
of
delirium.
Discharge
summarie
s of 15
(12.4%)
patients
In our health
system, the
majority of
geriatric
patients with
delirium,
discharged
on a new
antipsychoti
c had no
instructions
outlined to
outpatient
providers for
discontinuati
on
management
.
Further
interventions could
target increasing
antipsychotic
guidance at
transitions of care.
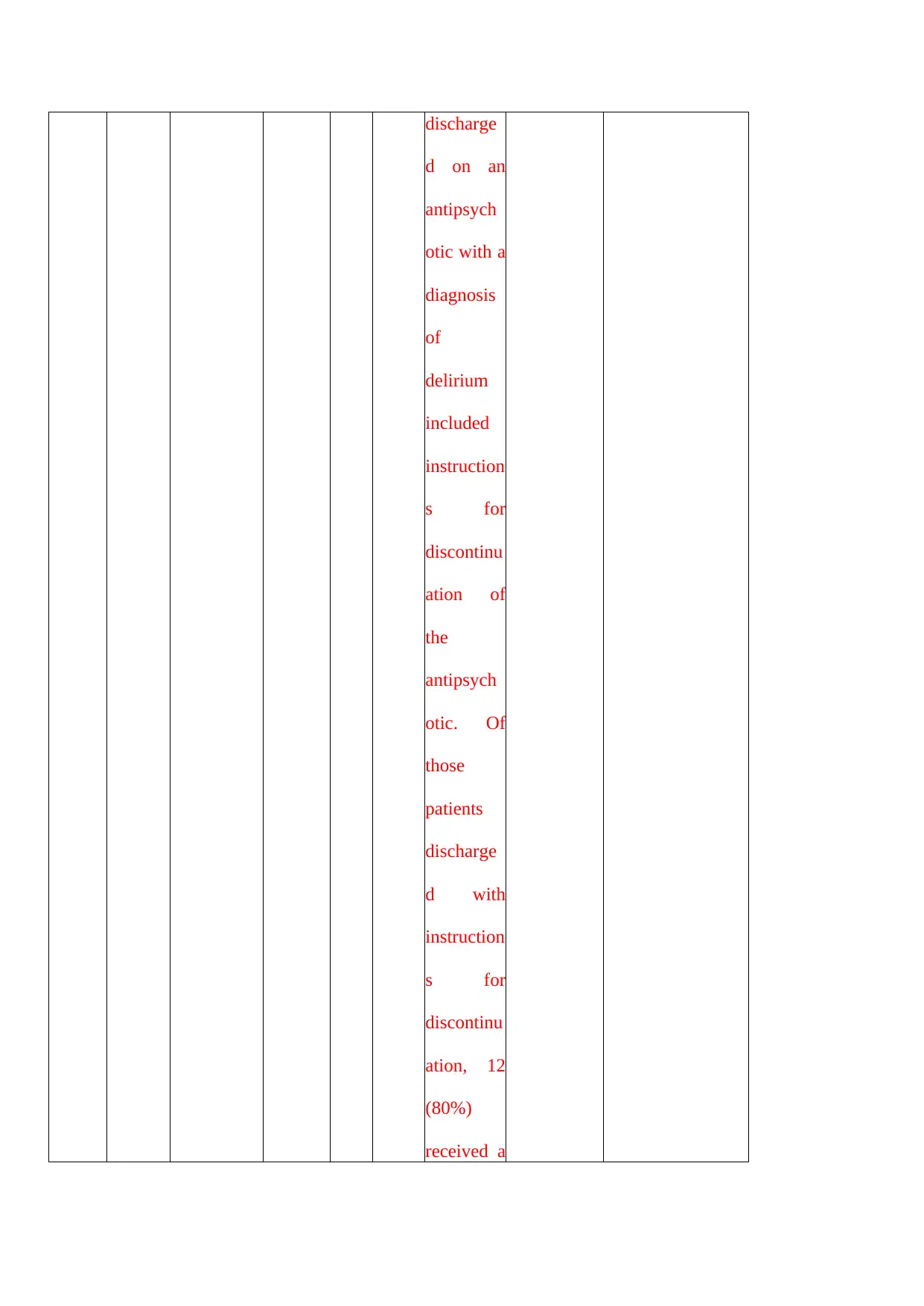
discharge
d on an
antipsych
otic with a
diagnosis
of
delirium
included
instruction
s for
discontinu
ation of
the
antipsych
otic. Of
those
patients
discharge
d with
instruction
s for
discontinu
ation, 12
(80%)
received a
d on an
antipsych
otic with a
diagnosis
of
delirium
included
instruction
s for
discontinu
ation of
the
antipsych
otic. Of
those
patients
discharge
d with
instruction
s for
discontinu
ation, 12
(80%)
received a
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
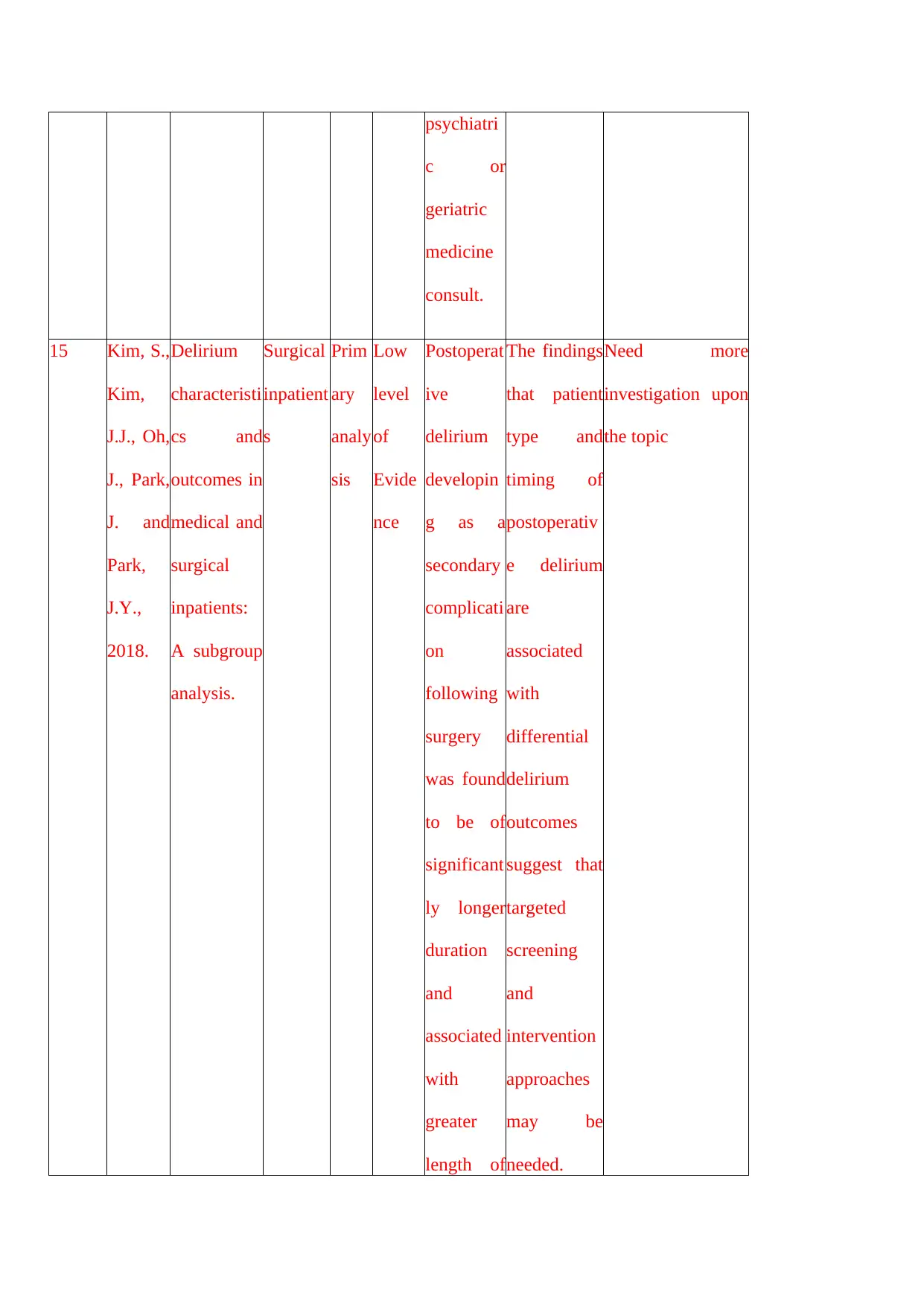
psychiatri
c or
geriatric
medicine
consult.
15 Kim, S.,
Kim,
J.J., Oh,
J., Park,
J. and
Park,
J.Y.,
2018.
Delirium
characteristi
cs and
outcomes in
medical and
surgical
inpatients:
A subgroup
analysis.
Surgical
inpatient
s
Prim
ary
analy
sis
Low
level
of
Evide
nce
Postoperat
ive
delirium
developin
g as a
secondary
complicati
on
following
surgery
was found
to be of
significant
ly longer
duration
and
associated
with
greater
length of
The findings
that patient
type and
timing of
postoperativ
e delirium
are
associated
with
differential
delirium
outcomes
suggest that
targeted
screening
and
intervention
approaches
may be
needed.
Need more
investigation upon
the topic
c or
geriatric
medicine
consult.
15 Kim, S.,
Kim,
J.J., Oh,
J., Park,
J. and
Park,
J.Y.,
2018.
Delirium
characteristi
cs and
outcomes in
medical and
surgical
inpatients:
A subgroup
analysis.
Surgical
inpatient
s
Prim
ary
analy
sis
Low
level
of
Evide
nce
Postoperat
ive
delirium
developin
g as a
secondary
complicati
on
following
surgery
was found
to be of
significant
ly longer
duration
and
associated
with
greater
length of
The findings
that patient
type and
timing of
postoperativ
e delirium
are
associated
with
differential
delirium
outcomes
suggest that
targeted
screening
and
intervention
approaches
may be
needed.
Need more
investigation upon
the topic
1 out of 53
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





