Literature Critique: Early COPD Intervention by Nurse-GP Teams EBP
VerifiedAdded on 2023/06/14
|8
|7215
|59
Essay
AI Summary
This essay presents a critique of the literature surrounding early intervention for Chronic Obstructive Pulmonary Disease (COPD) by practice nurse and GP teams, drawing from the PELICAN study and related research. The analysis focuses on the effectiveness of team-based management in improving the quality of life and adherence to clinical practice guidelines for newly diagnosed COPD patients. It examines the study's methodology, including the cluster randomized controlled trial design, case-finding methods, and intervention strategies involving nurse and GP education. The critique assesses the impact of the intervention on health-related quality of life, secondary outcomes such as lung function and patient knowledge, and the challenges in implementing evidence-based practices in primary care settings. The essay further reflects on the broader context of COPD management, including the role of smoking cessation, pulmonary rehabilitation, and disease management programs, highlighting the complexities and potential benefits of early intervention strategies.
© The Author 2016. Published by Oxford University Press. All rights reserved.
For permissions, please e-mail: journals.permissions@oup.com. 1
Family Practice, 2016, 1–8
doi:10.1093/fampra/cmw077
Health Service Research
Early intervention for chronic obstructive
pulmonary disease by practice nurse and GP
teams: a cluster randomized trial
Nicholas A Zwara,
*, Jeremy M Bunkera,†
, Helen K Reddelb, Sarah M Dennisc,d
,
Sandy Middletone, Onno C P van Schayckf, Alan J Crockettg, Iqbal Hasand,
Oshana Hermizd, Sanjyot Vagholkara, Wei Xuanh, Guy B Marksb,i
aSchool of Public Health and Community Medicine, UNSW Australia, UNSW Sydney, Australia,bWoolcock Institute
of Medical Research, University of Sydney, Glebe, Australia,cFaculty of Health Sciences, University of Sydney,
Lidcombe, Australia,dCentre for Primary Health Care and Equity, UNSW Australia, UNSW Sydney, Australia,eNursing
Research Institute, St Vincent’s Health Australia (Sydney) and Australian Catholic University, Darlinghurst, Australia,
fResearch School Caphri, Maastricht University, Maastricht, The Netherlands,gSchool of Health Sciences, University
of South Australia, Adelaide, Australia,hIngham Institute for Applied Medical Research, Liverpool, Australia and
iSouth Western Sydney Clinical School, UNSW Australia, Liverpool, Australia
*Correspondence to Nicholas A Zwar, School of Public Health and Community Medicine, UNSW Australia, UNSW Sydney
2052, Australia; E-mail: n.zwar@unsw.edu.au
†Deceased
Abstract
Background. Early detection and intervention for chronic obstructive pulmonary disease (COPD)
could potentially slow disease progress and minimize harm.
Objectives. To assess the effectiveness of early intervention by a practice nurse-GP team on
quality of life (QoL) and process of care in patients with newly diagnosed COPD, compared with
usual care. Nurses and GPs in intervention practices were educated to develop and implement
disease management plans for COPD.
Methods. A 12-month, multicentre, pragmatic randomized controlled trial with blinded outcome
assessment was conducted. Participants were current and former smokers aged 40 to 85 years
newly identified as having COPD on post-bronchodilator spirometry. The primary outcome was
health-related QoL, assessed with the St George’s Respiratory Questionnaire (SGRQ). Secondary
outcome measures were other QoL measures, lung function, disease knowledge, smoking and
immunization status, inhaler technique and health service use.
Results. Of the 10 234 patients from 36 practices in Sydney invited to a case-finding appointment,
1641 (16%) attended and 287 (18%) were diagnosed with COPD. Nineteen practices (144 patients)
were randomized to the intervention group and 17 practices (110 patients) to the control group.
Only 15.3% (n = 22) patients in the intervention group saw the nurse for COPD care following
case finding. There was no between-group difference in SGRQ score at follow-up (mean difference
−0.21; P = 0.86). Influenza vaccination was higher in the intervention group (OR 2.31: P = 0.035), but
there were no other significant between-group differences in outcomes.
Conclusion. Intervention uptake was low and had no additional beneficial effect, over usual care,
on participants’ health-related QoL.
Key words: Chronic disease, nursing, primary care, quality of care, respiratory diseases, smoking/tobacco use.
Family Practice Advance Access published August 17, 2016
at La Trobe University on October 28, 2016http://fampra.oxfordjournals.org/Downloaded from
For permissions, please e-mail: journals.permissions@oup.com. 1
Family Practice, 2016, 1–8
doi:10.1093/fampra/cmw077
Health Service Research
Early intervention for chronic obstructive
pulmonary disease by practice nurse and GP
teams: a cluster randomized trial
Nicholas A Zwara,
*, Jeremy M Bunkera,†
, Helen K Reddelb, Sarah M Dennisc,d
,
Sandy Middletone, Onno C P van Schayckf, Alan J Crockettg, Iqbal Hasand,
Oshana Hermizd, Sanjyot Vagholkara, Wei Xuanh, Guy B Marksb,i
aSchool of Public Health and Community Medicine, UNSW Australia, UNSW Sydney, Australia,bWoolcock Institute
of Medical Research, University of Sydney, Glebe, Australia,cFaculty of Health Sciences, University of Sydney,
Lidcombe, Australia,dCentre for Primary Health Care and Equity, UNSW Australia, UNSW Sydney, Australia,eNursing
Research Institute, St Vincent’s Health Australia (Sydney) and Australian Catholic University, Darlinghurst, Australia,
fResearch School Caphri, Maastricht University, Maastricht, The Netherlands,gSchool of Health Sciences, University
of South Australia, Adelaide, Australia,hIngham Institute for Applied Medical Research, Liverpool, Australia and
iSouth Western Sydney Clinical School, UNSW Australia, Liverpool, Australia
*Correspondence to Nicholas A Zwar, School of Public Health and Community Medicine, UNSW Australia, UNSW Sydney
2052, Australia; E-mail: n.zwar@unsw.edu.au
†Deceased
Abstract
Background. Early detection and intervention for chronic obstructive pulmonary disease (COPD)
could potentially slow disease progress and minimize harm.
Objectives. To assess the effectiveness of early intervention by a practice nurse-GP team on
quality of life (QoL) and process of care in patients with newly diagnosed COPD, compared with
usual care. Nurses and GPs in intervention practices were educated to develop and implement
disease management plans for COPD.
Methods. A 12-month, multicentre, pragmatic randomized controlled trial with blinded outcome
assessment was conducted. Participants were current and former smokers aged 40 to 85 years
newly identified as having COPD on post-bronchodilator spirometry. The primary outcome was
health-related QoL, assessed with the St George’s Respiratory Questionnaire (SGRQ). Secondary
outcome measures were other QoL measures, lung function, disease knowledge, smoking and
immunization status, inhaler technique and health service use.
Results. Of the 10 234 patients from 36 practices in Sydney invited to a case-finding appointment,
1641 (16%) attended and 287 (18%) were diagnosed with COPD. Nineteen practices (144 patients)
were randomized to the intervention group and 17 practices (110 patients) to the control group.
Only 15.3% (n = 22) patients in the intervention group saw the nurse for COPD care following
case finding. There was no between-group difference in SGRQ score at follow-up (mean difference
−0.21; P = 0.86). Influenza vaccination was higher in the intervention group (OR 2.31: P = 0.035), but
there were no other significant between-group differences in outcomes.
Conclusion. Intervention uptake was low and had no additional beneficial effect, over usual care,
on participants’ health-related QoL.
Key words: Chronic disease, nursing, primary care, quality of care, respiratory diseases, smoking/tobacco use.
Family Practice Advance Access published August 17, 2016
at La Trobe University on October 28, 2016http://fampra.oxfordjournals.org/Downloaded from
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Introduction
Chronic obstructive pulmonary disease (COPD) is a leading cause
of morbidity and mortality worldwide (1). In developed countries,
the most common risk factor is tobacco smoking, and it is estimated
that up to 50% of tobacco users will develop COPD (2). Even mild-
to-moderate COPD is associated with impaired health status and it
is well established that continued smoking is associated with more
rapid loss of lung function and poorer outcomes (3,4). If COPD
could be detected early and effective intervention provided, in par-
ticular to assist smoking cessation, then it follows that progression of
the disease could be slowed and the harms minimized (5,6). General
practice is well placed to conduct case finding for COPD and also to
provide early intervention (7,8). There is evidence that a case-finding
approach targeting at risk patients in primary care is feasible and
will identify substantial number of patients with previously undiag-
nosed COPD, though there are continuing challenges in educating
and supporting primary care clinicians in the conduct and interpre-
tation of spirometry (9,10).
Clinical practice guidelines for care of COPD provide evidence-
based recommendations for case finding and diagnosis, optimizing
function, slowing disease progression and management of exacerba-
tions as well as care planning and self-management support (2,11).
However evaluation of the care provided for patients with COPD in
community settings indicates low levels of awareness and implemen-
tation of these guidelines (12,13). Areas identified where implemen-
tation is suboptimal include support for smoking cessation, uptake
of pulmonary rehabilitation, adherence to medicines, inhaler tech-
nique and management of exacerbations.
There have been a number of studies on the role of special-
ized nurses in the care of patients with COPD, with evidence of
improvements in patient self-care, quality of life (QoL), quality of
care, patient knowledge and satisfaction (14–16). Cochrane review
of nursing outreach programmes for COPD found significant gains
in health-related QoL for patients with moderate COPD, but the
review highlighted the lack of high-quality studies and concluded
that further study was required (17). Furthermore, although crucial
to widespread implementation, there are few studies examining the
role of generalist practice nurses (PNs) working in partnership with
GPs in providing evidence-based care for patients with COPD.
There is also a growing body of evidence on disease management
programmes for COPD, often with a self-management support focus
(18,19). Some of these are based on programmes that have been
effective in improving health-related QoL and reducing hospitaliza-
tions in secondary care settings, but the benefits when implemented
in primary care remain uncertain and none have been applied to
newly diagnosed patients (20,21).
The Primary care EarLy Intervention for Copd mANagement
(PELICAN) study aimed to assess the effectiveness of PN-GP teams
developing and implementing an evidence-based disease manage-
ment plan for patients newly diagnosed with COPD. The study
hypothesis was that the intervention would lead to improved health-
related QoL and greater adherence to clinical practice guidelines for
patients with newly diagnosed COPD, compared with usual care.
Methods
Study design
A pragmatic cluster randomized controlled trial, with randomization
at the level of the practice, was conducted in accordance with the
published study protocol (22).
Recruitment
Practices were invited to participate with assistance from primary care
organizations in the greater Sydney area to identify potentially interested
practices and through an email to members of the Australia Primary
Healthcare Nurses Association. Practices were eligible to participate if
they had computer-based patient records, employed at least one PN,
and had a spirometer. Patients were potentially eligible for inclusion if
they had attended the practice at least twice, with at least one visit in the
preceding 12 months, and had risk factors for COPD (aged 40–85 years
and with a documented history of smoking). Practices performed a
search of their clinical information systems to identify patients meeting
these criteria. Patients were excluded if they had a recorded diagnosis
of COPD, were unable to understand English sufficiently to complete
study questionnaires or procedures or had cognitive impairment (as
assessed by the nurse and GP). A letter was sent to patients to invite
them to a case-finding visit and management of COPD if diagnosed.
Non-responders were followed up by practice staff through telephone.
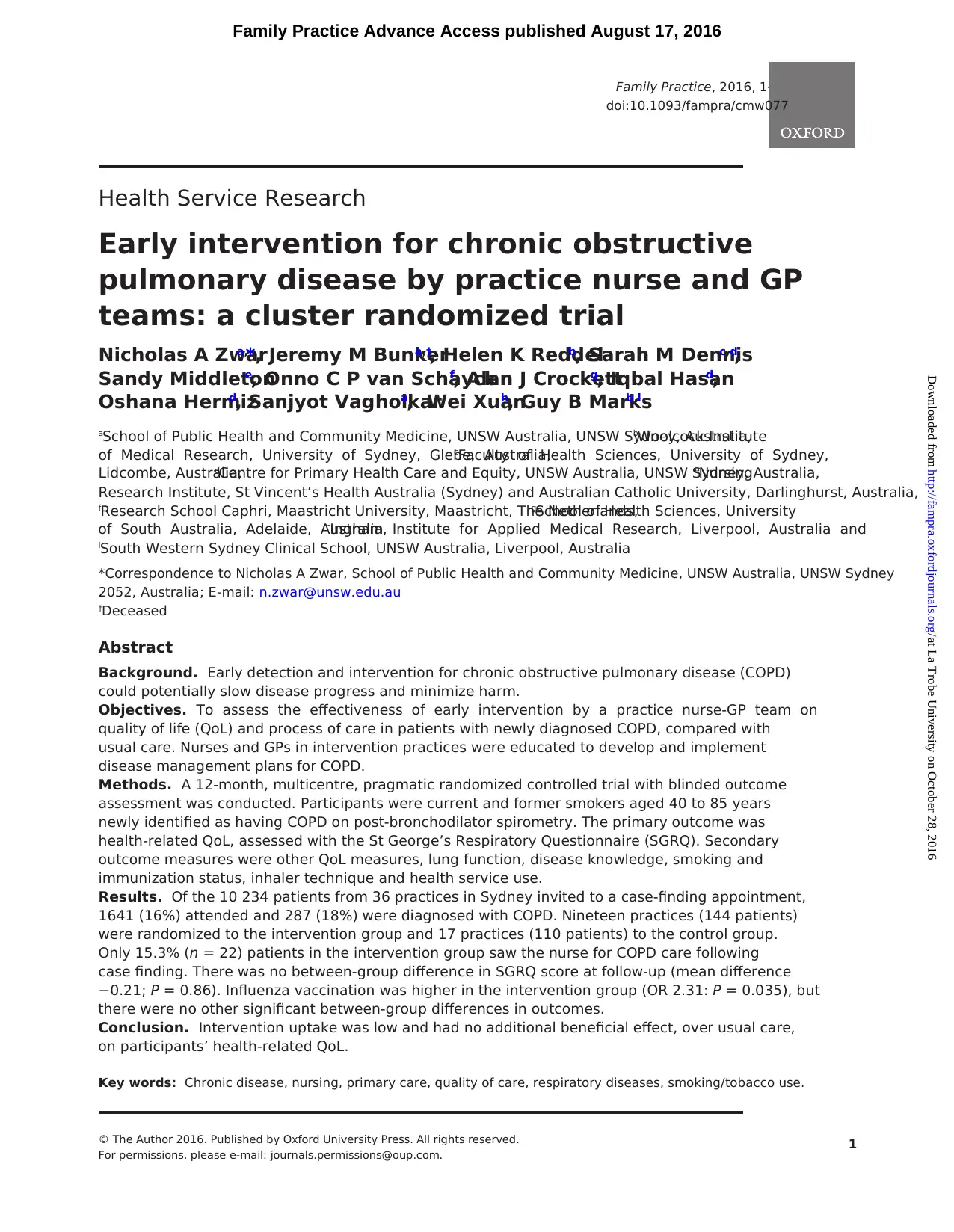
Case finding (all practices)
All PNs in the study completed 8 hours of training in case finding
for diagnosis of COPD including the conduct of the case-finding visit
and training in the performance and interpretation of spirometry
based on the 2005 ATS/ERS lung function guidelines (10,23,24). The
nurses were provided with a computer-based toolkit developed by
Lung Foundation Australia (Fig. 1) to assist with interpretation of
spirometry and identification of COPD, based on post-bronchodila-
tor forced expiratory volume in 1 second (FEV1)/forced vital capac-
ity (FVC) < 0.7 (25). Spirometry traces were sent to one investigator
(AC) for review and if necessary nurses were provided with feedback
by telephone on their spirometry performance.
Randomization and allocation concealment
Randomization was undertaken after PNs had completed spirom-
etry and case-finding training. Randomization and group allocation
of GP practices was performed by an independent statistician using
a computer-generated randomization program, with a minimization
algorithm to ensure a balance of practice characteristics that could
potentially affect study outcomes. These characteristics were practice
size, as indicated by the number of PNs (1 or >1); socio-economic sta-
tus, classified according to Socio-Economic Indexes for Areas (low:
SEIFA 1–5, high: SEIFA 6–10); and participation by the GP in signifi-
cant (>6 hours) COPD education activities within the last 6 months (yes
or no) (26). In this pragmatic trial participating GPs, PNs and patients
were not blind to the aims of the study or to their randomization group.
Project officers, who collected study outcome measures, and the statisti-
cian undertaking the analyses were blind to group allocation.
Intervention
Nurses and GPs from intervention practices attended further
workshops to receive practical education in team-based man-
agement of COPD. A description of the educational workshops
has previously been published (22). Topics covered in a 1-day
PN training included pathophysiology and assessment of COPD;
smoking cessation, including the use of lung age as a motiva-
tional tool (27); evidence-based COPD management (11); assess-
ment and instruction in inhaler technique (28); role of pulmonary
rehabilitation; management of exacerbations; the use and value
of nurse/GP joint care planning; and education about support-
ing behaviour change, teamwork and fostering partnerships. Care
planning templates were provided in an electronic form for use
2 Family Practice, 2016, Vol. 00, No. 00
at La Trobe University on October 28, 2016http://fampra.oxfordjournals.org/Downloaded from
Chronic obstructive pulmonary disease (COPD) is a leading cause
of morbidity and mortality worldwide (1). In developed countries,
the most common risk factor is tobacco smoking, and it is estimated
that up to 50% of tobacco users will develop COPD (2). Even mild-
to-moderate COPD is associated with impaired health status and it
is well established that continued smoking is associated with more
rapid loss of lung function and poorer outcomes (3,4). If COPD
could be detected early and effective intervention provided, in par-
ticular to assist smoking cessation, then it follows that progression of
the disease could be slowed and the harms minimized (5,6). General
practice is well placed to conduct case finding for COPD and also to
provide early intervention (7,8). There is evidence that a case-finding
approach targeting at risk patients in primary care is feasible and
will identify substantial number of patients with previously undiag-
nosed COPD, though there are continuing challenges in educating
and supporting primary care clinicians in the conduct and interpre-
tation of spirometry (9,10).
Clinical practice guidelines for care of COPD provide evidence-
based recommendations for case finding and diagnosis, optimizing
function, slowing disease progression and management of exacerba-
tions as well as care planning and self-management support (2,11).
However evaluation of the care provided for patients with COPD in
community settings indicates low levels of awareness and implemen-
tation of these guidelines (12,13). Areas identified where implemen-
tation is suboptimal include support for smoking cessation, uptake
of pulmonary rehabilitation, adherence to medicines, inhaler tech-
nique and management of exacerbations.
There have been a number of studies on the role of special-
ized nurses in the care of patients with COPD, with evidence of
improvements in patient self-care, quality of life (QoL), quality of
care, patient knowledge and satisfaction (14–16). Cochrane review
of nursing outreach programmes for COPD found significant gains
in health-related QoL for patients with moderate COPD, but the
review highlighted the lack of high-quality studies and concluded
that further study was required (17). Furthermore, although crucial
to widespread implementation, there are few studies examining the
role of generalist practice nurses (PNs) working in partnership with
GPs in providing evidence-based care for patients with COPD.
There is also a growing body of evidence on disease management
programmes for COPD, often with a self-management support focus
(18,19). Some of these are based on programmes that have been
effective in improving health-related QoL and reducing hospitaliza-
tions in secondary care settings, but the benefits when implemented
in primary care remain uncertain and none have been applied to
newly diagnosed patients (20,21).
The Primary care EarLy Intervention for Copd mANagement
(PELICAN) study aimed to assess the effectiveness of PN-GP teams
developing and implementing an evidence-based disease manage-
ment plan for patients newly diagnosed with COPD. The study
hypothesis was that the intervention would lead to improved health-
related QoL and greater adherence to clinical practice guidelines for
patients with newly diagnosed COPD, compared with usual care.
Methods
Study design
A pragmatic cluster randomized controlled trial, with randomization
at the level of the practice, was conducted in accordance with the
published study protocol (22).
Recruitment
Practices were invited to participate with assistance from primary care
organizations in the greater Sydney area to identify potentially interested
practices and through an email to members of the Australia Primary
Healthcare Nurses Association. Practices were eligible to participate if
they had computer-based patient records, employed at least one PN,
and had a spirometer. Patients were potentially eligible for inclusion if
they had attended the practice at least twice, with at least one visit in the
preceding 12 months, and had risk factors for COPD (aged 40–85 years
and with a documented history of smoking). Practices performed a
search of their clinical information systems to identify patients meeting
these criteria. Patients were excluded if they had a recorded diagnosis
of COPD, were unable to understand English sufficiently to complete
study questionnaires or procedures or had cognitive impairment (as
assessed by the nurse and GP). A letter was sent to patients to invite
them to a case-finding visit and management of COPD if diagnosed.
Non-responders were followed up by practice staff through telephone.
Case finding (all practices)
All PNs in the study completed 8 hours of training in case finding
for diagnosis of COPD including the conduct of the case-finding visit
and training in the performance and interpretation of spirometry
based on the 2005 ATS/ERS lung function guidelines (10,23,24). The
nurses were provided with a computer-based toolkit developed by
Lung Foundation Australia (Fig. 1) to assist with interpretation of
spirometry and identification of COPD, based on post-bronchodila-
tor forced expiratory volume in 1 second (FEV1)/forced vital capac-
ity (FVC) < 0.7 (25). Spirometry traces were sent to one investigator
(AC) for review and if necessary nurses were provided with feedback
by telephone on their spirometry performance.
Randomization and allocation concealment
Randomization was undertaken after PNs had completed spirom-
etry and case-finding training. Randomization and group allocation
of GP practices was performed by an independent statistician using
a computer-generated randomization program, with a minimization
algorithm to ensure a balance of practice characteristics that could
potentially affect study outcomes. These characteristics were practice
size, as indicated by the number of PNs (1 or >1); socio-economic sta-
tus, classified according to Socio-Economic Indexes for Areas (low:
SEIFA 1–5, high: SEIFA 6–10); and participation by the GP in signifi-
cant (>6 hours) COPD education activities within the last 6 months (yes
or no) (26). In this pragmatic trial participating GPs, PNs and patients
were not blind to the aims of the study or to their randomization group.
Project officers, who collected study outcome measures, and the statisti-
cian undertaking the analyses were blind to group allocation.
Intervention
Nurses and GPs from intervention practices attended further
workshops to receive practical education in team-based man-
agement of COPD. A description of the educational workshops
has previously been published (22). Topics covered in a 1-day
PN training included pathophysiology and assessment of COPD;
smoking cessation, including the use of lung age as a motiva-
tional tool (27); evidence-based COPD management (11); assess-
ment and instruction in inhaler technique (28); role of pulmonary
rehabilitation; management of exacerbations; the use and value
of nurse/GP joint care planning; and education about support-
ing behaviour change, teamwork and fostering partnerships. Care
planning templates were provided in an electronic form for use
2 Family Practice, 2016, Vol. 00, No. 00
at La Trobe University on October 28, 2016http://fampra.oxfordjournals.org/Downloaded from
by the nurse and GP in computerized clinical record systems. The
templates were designed for smokers and non-smokers respec-
tively and had prompts for assessment, goals and actions based on
the COPD guidelines. GPs completed a computer-based distance
learning activity on the management of COPD according to guide-
lines (11). Finally a 3-hour combined workshop for GPs and PNs
focused on each PN-GP team clarifying the individual elements
of their roles. Each practice was provided with a copy of national
guidelines (COPD-X) (11).
Control
After the case-finding training for nurses, staff in control practices
received no further intervention other than GPs in these practices
being mailed a copy of the COPD-X guidelines.
Outcome measures
The primary outcome measure was health-related QoL assessed by
the St George’s Respiratory Questionnaire (SGRQ) (29). The SGRQ
is scored from 0 to 100, where 0 indicates best QoL and 100 the
worst. A change ≥4 is considered to be clinically significant (29).
Secondary outcome measures were COPD Assessment Test (CAT, a
disease-specific QoL measure (30)); general health status (using the
preliminary question from SGRQ); awareness of diagnosis of COPD;
smoking status by self-report; immunization status for influenza and
pneumococcus; effective inhaler use (where prescribed); attend-
ance at pulmonary rehabilitation; patient knowledge of COPD
measured by a 12-item scale developed for a previous project (31);
and health care utilization and lung function (post-bronchodilator
FEV1). Project officers who were blind to group allocation collected
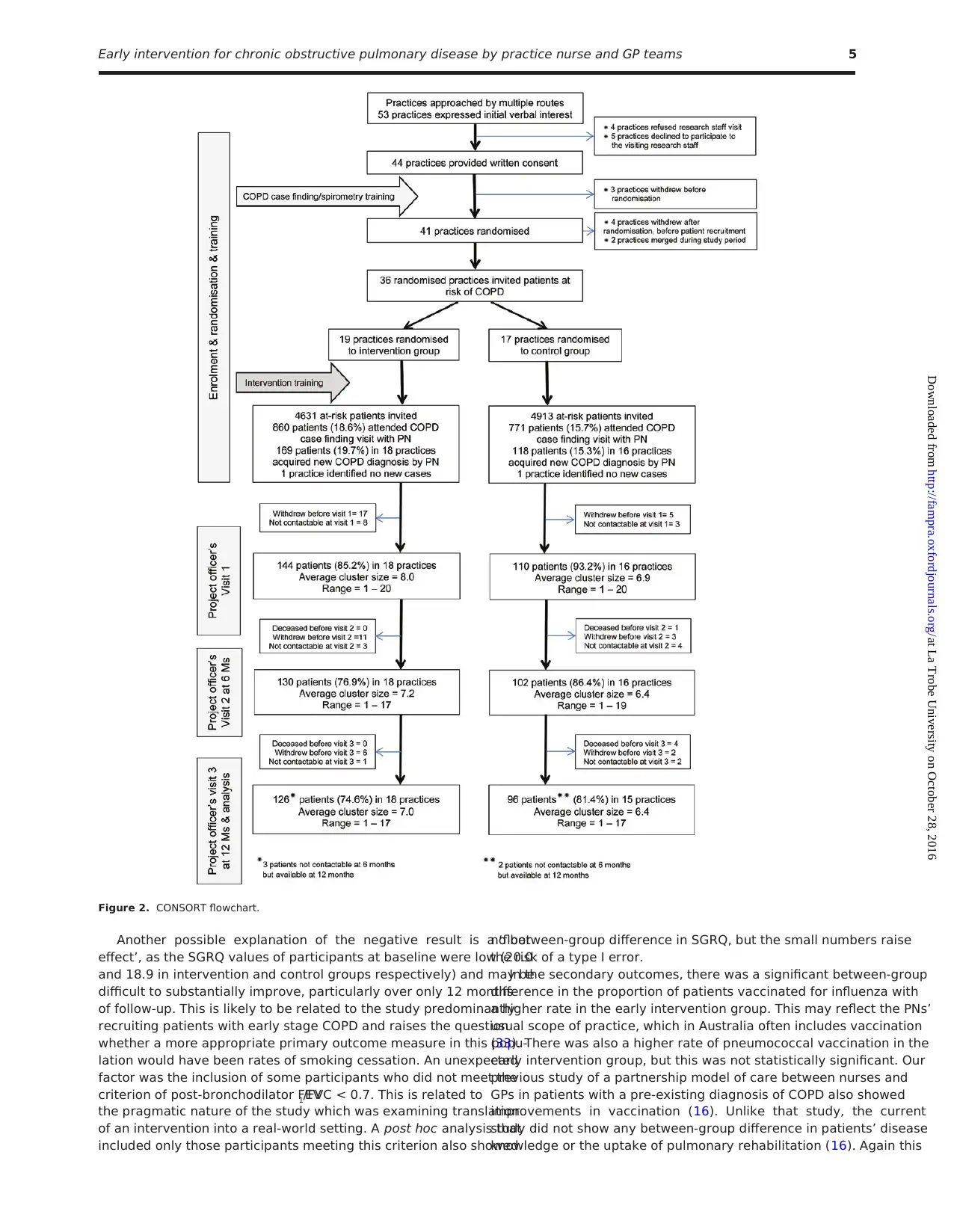
Figure 1. Primary care respiratory toolkit: Lung Foundation Australia.
Early intervention for chronic obstructive pulmonary disease by practice nurse and GP teams 3
at La Trobe University on October 28, 2016http://fampra.oxfordjournals.org/Downloaded from
templates were designed for smokers and non-smokers respec-
tively and had prompts for assessment, goals and actions based on
the COPD guidelines. GPs completed a computer-based distance
learning activity on the management of COPD according to guide-
lines (11). Finally a 3-hour combined workshop for GPs and PNs
focused on each PN-GP team clarifying the individual elements
of their roles. Each practice was provided with a copy of national
guidelines (COPD-X) (11).
Control
After the case-finding training for nurses, staff in control practices
received no further intervention other than GPs in these practices
being mailed a copy of the COPD-X guidelines.
Outcome measures
The primary outcome measure was health-related QoL assessed by
the St George’s Respiratory Questionnaire (SGRQ) (29). The SGRQ
is scored from 0 to 100, where 0 indicates best QoL and 100 the
worst. A change ≥4 is considered to be clinically significant (29).
Secondary outcome measures were COPD Assessment Test (CAT, a
disease-specific QoL measure (30)); general health status (using the
preliminary question from SGRQ); awareness of diagnosis of COPD;
smoking status by self-report; immunization status for influenza and
pneumococcus; effective inhaler use (where prescribed); attend-
ance at pulmonary rehabilitation; patient knowledge of COPD
measured by a 12-item scale developed for a previous project (31);
and health care utilization and lung function (post-bronchodilator
FEV1). Project officers who were blind to group allocation collected
Figure 1. Primary care respiratory toolkit: Lung Foundation Australia.
Early intervention for chronic obstructive pulmonary disease by practice nurse and GP teams 3
at La Trobe University on October 28, 2016http://fampra.oxfordjournals.org/Downloaded from
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
outcome data at home visits for the baseline and 12-month collec-
tion. The 6-month data collection was conducted by telephone, as it
did not involve lung function testing.
Data analysis
The primary analysis was by intention to treat and relied on the
diagnosis of COPD assigned by the PN/GP on the basis of case-
finding spirometry. This included patients whose diagnosis of COPD
was not subsequently confirmed by the researchers. Intra-cluster
(practice) correlation coefficients (ICCs) were determined for all pri-
mary outcome variables. The effect of the intervention on outcomes
measured on a continuous scale (such as SGRQ score) were esti-
mated and tested using mixed-model analysis of variance in which
time and treatment group were fixed effects and GP practice and
subject nested within practice were random effects. The effect of the
intervention on the dichotomous variables was analysed using gen-
eralized estimating equations with a logistic link and a model struc-
ture that is analogous to that described above. In the mixed-model
analysis, measurements performed at 6 and 12 months were treated
as dependent variables and the baseline measurement was included
as covariate. We also tested the treatment group by assessment–time
interaction. However, this interaction was not statistically significant
(P > 0.05) in any of the models. Therefore, it was excluded from
the final model. Only the main treatment group effect (intervention
versus control) was tested in the final model.
We estimated that the between-subject SD in SGRQ was 13 and
that the ICC for this outcome was 0.01 (31). Assuming a cluster size
(participants per practice) of 10, the resultant design effect is 1.09.
Based on these assumptions and prior data, we estimated that the
number of participant per group required to have 80% power to
detect a difference of 4 units or greater (29) as significant at the 5%
significance level was 200.
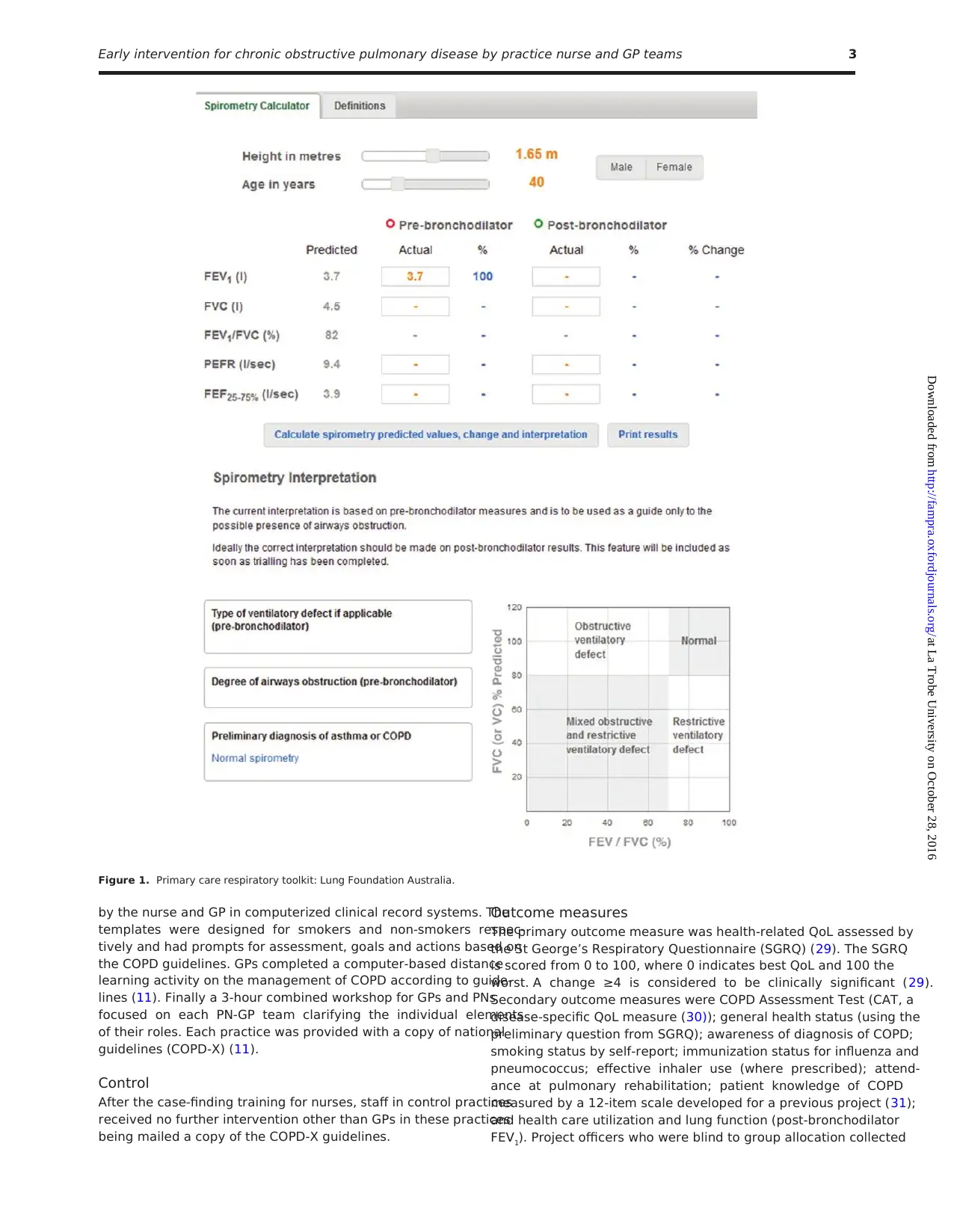
Results
The study involved GPs (n = 55) and PNs (n = 55) working in 36
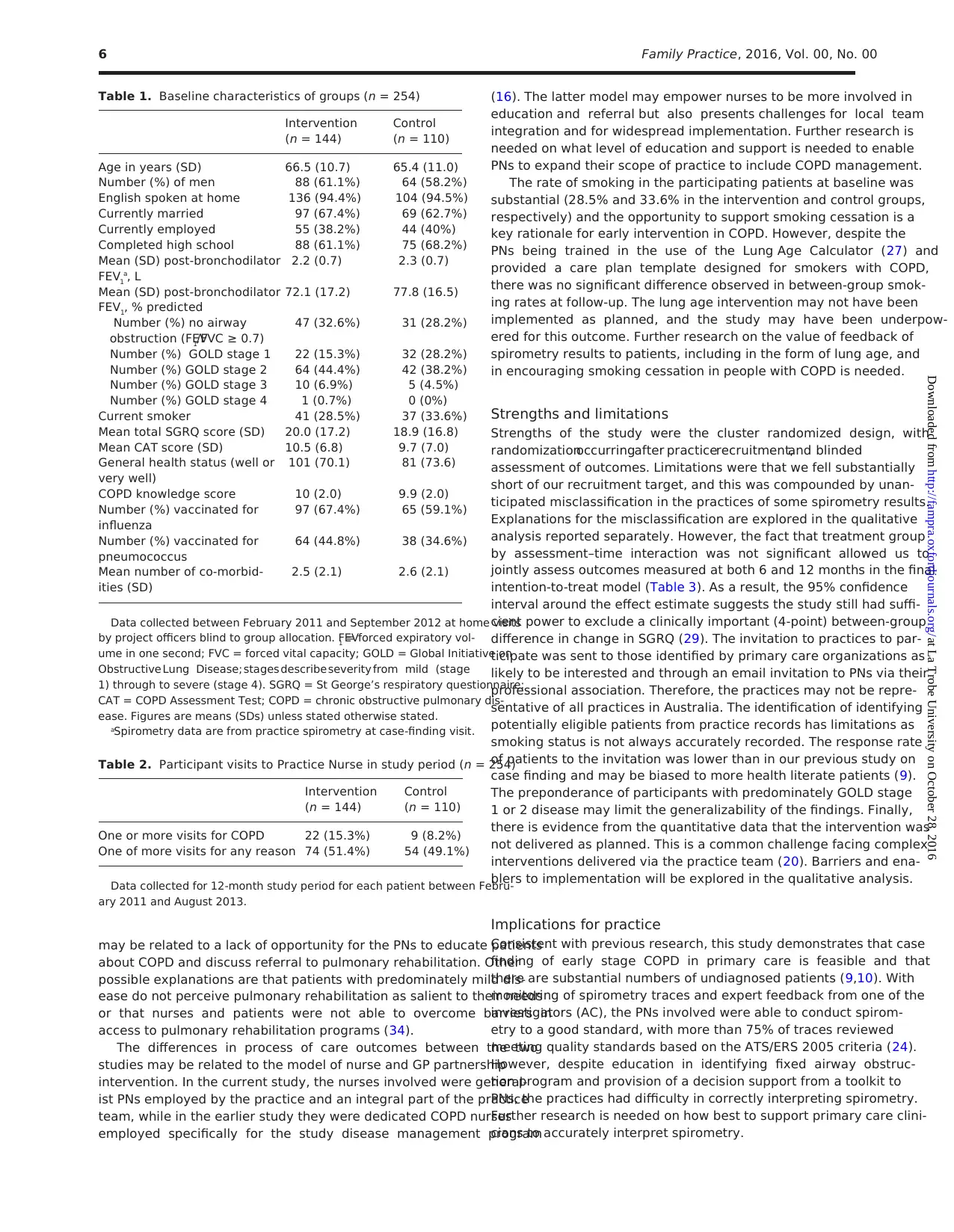
practices in greater Sydney area. Figure 2 shows the CONSORT
flow chart for the study. The medical record search identified 10 234
patients meeting the criteria for invitation for a case-finding appoint-
ment. Of these, 1641 (16%) attended to see the PN for assessment
and had pre- and post-bronchodilator spirometry performed. Based
on the practice’s (PN/GP) interpretation of the spirometry, there were
287 patients (18%) who had a new diagnosis of COPD and con-
sented to take part in the study. A number of patients (35, 12.2%)
withdrew from the study soon after the case-finding appointment
(Fig. 2) and 254 were available for project officer home visits and
had baseline data collected. The median time between the case-find-
ing visit and baseline data collection was 14.5 days (interquartile
range 16 days). Patient recruitment occurred from February 2011 to
September 2012. The 12-month follow-up was completed in August
2013. Six-month follow-up data were collected by telephone for 232
patients and 12-month data were collected at a further home visit
from 222 patients.
Baseline characteristics of patients are shown in Table 1. The
participants had a mean age of 66.0 years, 60% were male and
31% were current smokers. The majority of participants (n = 160)
had GOLD stage 1 or stage 2 disease (FEV1 ≥80% predicted; FEV1
≥50%, <80% predicted, respectively). On review of spirometry
traces, more than 75% (n = X) met quality standards based on the
ATS/ERS 2005 criteria (23,24). There were 78 (31%) patients for
whom the practice clinician had assigned a diagnosis of COPD but,
on later review of the practice spirometry data by the study team,
it was found that the post-bronchodilator FEV1/FVC ratio was not
<0.7. The mean health-related QoL as measured by the SGRQ was
in the mild range (20.0 in the intervention and 19.9 in the control
group) (32). The groups did not differ substantially in mean SGRQ
or in other characteristics.
Intervention uptake was low with only 22 (15.3%) patients in
the intervention group reporting one or more visits to the PN for
COPD care following the assessment visit compared with 9 (8.2%)
patients in the usual care group (Table 2). Only 24 (16.7%) and 16
(14.5%) patients in the intervention and control groups, respectively,
reported that a care plan had been developed for them during the
study period.
There was no statistically significant difference in the mean
SGRQ score between intervention and control groups during fol-
low-up (16.9 versus 17.1; difference −0.2; 95% confidence interval
−2.6 to 2.1; P = 0.86). The ICC for the SGRQ was 0.055 which was
higher than the estimate of 0.01 used in the sample size calculation.
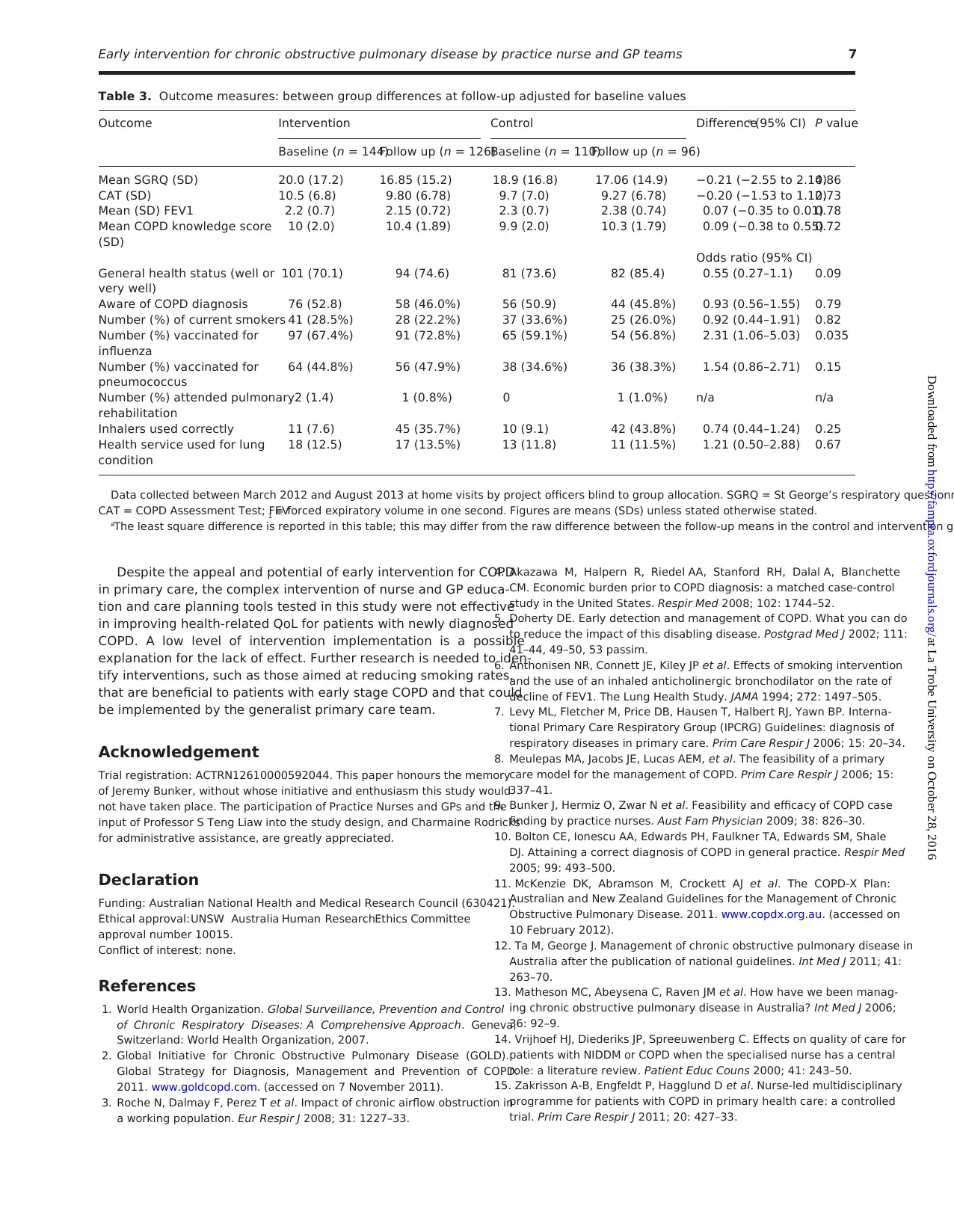
The analysis of secondary outcomes also showed no between-
group differences (Table 3) with the exception of significantly higher
rates of influenza vaccination in the intervention compared with
the control group, after adjustment for baseline differences (72.8%
versus 56.8%; OR 2.33; 95% confidence interval 1.06 to 5.03;
P = 0.04). The ICC for the CAT score was 0.054 and for post-bron-
chodilator FEV1 was 0.154.
Due the unexpectedfinding of misclassificationof practice
spirometry results for a substantial number of participants, we
undertook a post hoc subgroup analysis to explore the impact of this
misdiagnosis. The primary analysis was repeated for the subgroup
of participants (n = 163) whose initial spirometry (performed by the
PN) was confirmed as showing evidence of post-bronchodilator air-
way obstruction (i.e. post-bronchodilator FEV1/FVC < 0.7). In this
subgroup, there was no significant between-treatment group differ-
ence in SGRQ scores (17.2 versus 17.2; difference −0.008; 95% con-
fidence interval −2.8 to 2.9; P = 0.99).
Discussion
The study, which educated PNs and GPs to work in partnership to
identify patients with COPD and initiate an evidence-based early
intervention program, found no between-group difference in the
primary outcome measure (SGRQ) at follow-up. Although there
have been a number of studies showing positive effects of disease
management interventions on health-related QoL, exercise capacity
and health service use (18), our negative result is consistent with a
recent primary care-based study of a disease management program
in the Netherlands (20). Our intervention had a self-management
focus but, like Bischoff et al. (21), we did not find an effect on health-
related QoL when this approach was implemented in primary care.
Despite the education and care planning tools provided to the PNs
and GPs, lack of their adoption is strongly suggested by the low
rates of both attendances to the PNs for COPD and development
of care plans in the early intervention group, and this could explain
the absence of between-group differences at follow-up. The lack of
contact between patients and the PN after the case-finding appoint-
ment was despite education for the PNs in use of an electronic care
planning template that prompted implementation of evidence-based
COPD care. How the case-finding and management intervention
was utilized has been explored with a qualitative evaluation of semi-
structured interviews with PNs, GPs and patients, and this will be
reported separately.
4 Family Practice, 2016, Vol. 00, No. 00
at La Trobe University on October 28, 2016http://fampra.oxfordjournals.org/Downloaded from
tion. The 6-month data collection was conducted by telephone, as it
did not involve lung function testing.
Data analysis
The primary analysis was by intention to treat and relied on the
diagnosis of COPD assigned by the PN/GP on the basis of case-
finding spirometry. This included patients whose diagnosis of COPD
was not subsequently confirmed by the researchers. Intra-cluster
(practice) correlation coefficients (ICCs) were determined for all pri-
mary outcome variables. The effect of the intervention on outcomes
measured on a continuous scale (such as SGRQ score) were esti-
mated and tested using mixed-model analysis of variance in which
time and treatment group were fixed effects and GP practice and
subject nested within practice were random effects. The effect of the
intervention on the dichotomous variables was analysed using gen-
eralized estimating equations with a logistic link and a model struc-
ture that is analogous to that described above. In the mixed-model
analysis, measurements performed at 6 and 12 months were treated
as dependent variables and the baseline measurement was included
as covariate. We also tested the treatment group by assessment–time
interaction. However, this interaction was not statistically significant
(P > 0.05) in any of the models. Therefore, it was excluded from
the final model. Only the main treatment group effect (intervention
versus control) was tested in the final model.
We estimated that the between-subject SD in SGRQ was 13 and
that the ICC for this outcome was 0.01 (31). Assuming a cluster size
(participants per practice) of 10, the resultant design effect is 1.09.
Based on these assumptions and prior data, we estimated that the
number of participant per group required to have 80% power to
detect a difference of 4 units or greater (29) as significant at the 5%
significance level was 200.
Results
The study involved GPs (n = 55) and PNs (n = 55) working in 36
practices in greater Sydney area. Figure 2 shows the CONSORT
flow chart for the study. The medical record search identified 10 234
patients meeting the criteria for invitation for a case-finding appoint-
ment. Of these, 1641 (16%) attended to see the PN for assessment
and had pre- and post-bronchodilator spirometry performed. Based
on the practice’s (PN/GP) interpretation of the spirometry, there were
287 patients (18%) who had a new diagnosis of COPD and con-
sented to take part in the study. A number of patients (35, 12.2%)
withdrew from the study soon after the case-finding appointment
(Fig. 2) and 254 were available for project officer home visits and
had baseline data collected. The median time between the case-find-
ing visit and baseline data collection was 14.5 days (interquartile
range 16 days). Patient recruitment occurred from February 2011 to
September 2012. The 12-month follow-up was completed in August
2013. Six-month follow-up data were collected by telephone for 232
patients and 12-month data were collected at a further home visit
from 222 patients.
Baseline characteristics of patients are shown in Table 1. The
participants had a mean age of 66.0 years, 60% were male and
31% were current smokers. The majority of participants (n = 160)
had GOLD stage 1 or stage 2 disease (FEV1 ≥80% predicted; FEV1
≥50%, <80% predicted, respectively). On review of spirometry
traces, more than 75% (n = X) met quality standards based on the
ATS/ERS 2005 criteria (23,24). There were 78 (31%) patients for
whom the practice clinician had assigned a diagnosis of COPD but,
on later review of the practice spirometry data by the study team,
it was found that the post-bronchodilator FEV1/FVC ratio was not
<0.7. The mean health-related QoL as measured by the SGRQ was
in the mild range (20.0 in the intervention and 19.9 in the control
group) (32). The groups did not differ substantially in mean SGRQ
or in other characteristics.
Intervention uptake was low with only 22 (15.3%) patients in
the intervention group reporting one or more visits to the PN for
COPD care following the assessment visit compared with 9 (8.2%)
patients in the usual care group (Table 2). Only 24 (16.7%) and 16
(14.5%) patients in the intervention and control groups, respectively,
reported that a care plan had been developed for them during the
study period.
There was no statistically significant difference in the mean
SGRQ score between intervention and control groups during fol-
low-up (16.9 versus 17.1; difference −0.2; 95% confidence interval
−2.6 to 2.1; P = 0.86). The ICC for the SGRQ was 0.055 which was
higher than the estimate of 0.01 used in the sample size calculation.
The analysis of secondary outcomes also showed no between-
group differences (Table 3) with the exception of significantly higher
rates of influenza vaccination in the intervention compared with
the control group, after adjustment for baseline differences (72.8%
versus 56.8%; OR 2.33; 95% confidence interval 1.06 to 5.03;
P = 0.04). The ICC for the CAT score was 0.054 and for post-bron-
chodilator FEV1 was 0.154.
Due the unexpectedfinding of misclassificationof practice
spirometry results for a substantial number of participants, we
undertook a post hoc subgroup analysis to explore the impact of this
misdiagnosis. The primary analysis was repeated for the subgroup
of participants (n = 163) whose initial spirometry (performed by the
PN) was confirmed as showing evidence of post-bronchodilator air-
way obstruction (i.e. post-bronchodilator FEV1/FVC < 0.7). In this
subgroup, there was no significant between-treatment group differ-
ence in SGRQ scores (17.2 versus 17.2; difference −0.008; 95% con-
fidence interval −2.8 to 2.9; P = 0.99).
Discussion
The study, which educated PNs and GPs to work in partnership to
identify patients with COPD and initiate an evidence-based early
intervention program, found no between-group difference in the
primary outcome measure (SGRQ) at follow-up. Although there
have been a number of studies showing positive effects of disease
management interventions on health-related QoL, exercise capacity
and health service use (18), our negative result is consistent with a
recent primary care-based study of a disease management program
in the Netherlands (20). Our intervention had a self-management
focus but, like Bischoff et al. (21), we did not find an effect on health-
related QoL when this approach was implemented in primary care.
Despite the education and care planning tools provided to the PNs
and GPs, lack of their adoption is strongly suggested by the low
rates of both attendances to the PNs for COPD and development
of care plans in the early intervention group, and this could explain
the absence of between-group differences at follow-up. The lack of
contact between patients and the PN after the case-finding appoint-
ment was despite education for the PNs in use of an electronic care
planning template that prompted implementation of evidence-based
COPD care. How the case-finding and management intervention
was utilized has been explored with a qualitative evaluation of semi-
structured interviews with PNs, GPs and patients, and this will be
reported separately.
4 Family Practice, 2016, Vol. 00, No. 00
at La Trobe University on October 28, 2016http://fampra.oxfordjournals.org/Downloaded from
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Another possible explanation of the negative result is a ‘floor
effect’, as the SGRQ values of participants at baseline were low (20.0
and 18.9 in intervention and control groups respectively) and may be
difficult to substantially improve, particularly over only 12 months
of follow-up. This is likely to be related to the study predominantly
recruiting patients with early stage COPD and raises the question
whether a more appropriate primary outcome measure in this popu-
lation would have been rates of smoking cessation. An unexpected
factor was the inclusion of some participants who did not meet the
criterion of post-bronchodilator FEV1/FVC < 0.7. This is related to
the pragmatic nature of the study which was examining translation
of an intervention into a real-world setting. A post hoc analysis that
included only those participants meeting this criterion also showed
no between-group difference in SGRQ, but the small numbers raise
the risk of a type I error.
In the secondary outcomes, there was a significant between-group
difference in the proportion of patients vaccinated for influenza with
a higher rate in the early intervention group. This may reflect the PNs’
usual scope of practice, which in Australia often includes vaccination
(33). There was also a higher rate of pneumococcal vaccination in the
early intervention group, but this was not statistically significant. Our
previous study of a partnership model of care between nurses and
GPs in patients with a pre-existing diagnosis of COPD also showed
improvements in vaccination (16). Unlike that study, the current
study did not show any between-group difference in patients’ disease
knowledge or the uptake of pulmonary rehabilitation (16). Again this
Figure 2. CONSORT flowchart.
Early intervention for chronic obstructive pulmonary disease by practice nurse and GP teams 5
at La Trobe University on October 28, 2016http://fampra.oxfordjournals.org/Downloaded from
effect’, as the SGRQ values of participants at baseline were low (20.0
and 18.9 in intervention and control groups respectively) and may be
difficult to substantially improve, particularly over only 12 months
of follow-up. This is likely to be related to the study predominantly
recruiting patients with early stage COPD and raises the question
whether a more appropriate primary outcome measure in this popu-
lation would have been rates of smoking cessation. An unexpected
factor was the inclusion of some participants who did not meet the
criterion of post-bronchodilator FEV1/FVC < 0.7. This is related to
the pragmatic nature of the study which was examining translation
of an intervention into a real-world setting. A post hoc analysis that
included only those participants meeting this criterion also showed
no between-group difference in SGRQ, but the small numbers raise
the risk of a type I error.
In the secondary outcomes, there was a significant between-group
difference in the proportion of patients vaccinated for influenza with
a higher rate in the early intervention group. This may reflect the PNs’
usual scope of practice, which in Australia often includes vaccination
(33). There was also a higher rate of pneumococcal vaccination in the
early intervention group, but this was not statistically significant. Our
previous study of a partnership model of care between nurses and
GPs in patients with a pre-existing diagnosis of COPD also showed
improvements in vaccination (16). Unlike that study, the current
study did not show any between-group difference in patients’ disease
knowledge or the uptake of pulmonary rehabilitation (16). Again this
Figure 2. CONSORT flowchart.
Early intervention for chronic obstructive pulmonary disease by practice nurse and GP teams 5
at La Trobe University on October 28, 2016http://fampra.oxfordjournals.org/Downloaded from
may be related to a lack of opportunity for the PNs to educate patients
about COPD and discuss referral to pulmonary rehabilitation. Other
possible explanations are that patients with predominately mild dis-
ease do not perceive pulmonary rehabilitation as salient to their needs
or that nurses and patients were not able to overcome barriers in
access to pulmonary rehabilitation programs (34).
The differences in process of care outcomes between the two
studies may be related to the model of nurse and GP partnership
intervention. In the current study, the nurses involved were general-
ist PNs employed by the practice and an integral part of the practice
team, while in the earlier study they were dedicated COPD nurses
employed specifically for the study disease management program
(16). The latter model may empower nurses to be more involved in
education and referral but also presents challenges for local team
integration and for widespread implementation. Further research is
needed on what level of education and support is needed to enable
PNs to expand their scope of practice to include COPD management.
The rate of smoking in the participating patients at baseline was
substantial (28.5% and 33.6% in the intervention and control groups,
respectively) and the opportunity to support smoking cessation is a
key rationale for early intervention in COPD. However, despite the
PNs being trained in the use of the Lung Age Calculator (27) and
provided a care plan template designed for smokers with COPD,
there was no significant difference observed in between-group smok-
ing rates at follow-up. The lung age intervention may not have been
implemented as planned, and the study may have been underpow-
ered for this outcome. Further research on the value of feedback of
spirometry results to patients, including in the form of lung age, and
in encouraging smoking cessation in people with COPD is needed.
Strengths and limitations
Strengths of the study were the cluster randomized design, with
randomizationoccurringafter practicerecruitment,and blinded
assessment of outcomes. Limitations were that we fell substantially
short of our recruitment target, and this was compounded by unan-
ticipated misclassification in the practices of some spirometry results.
Explanations for the misclassification are explored in the qualitative
analysis reported separately. However, the fact that treatment group
by assessment–time interaction was not significant allowed us to
jointly assess outcomes measured at both 6 and 12 months in the final
intention-to-treat model (Table 3). As a result, the 95% confidence
interval around the effect estimate suggests the study still had suffi-
cient power to exclude a clinically important (4-point) between-group
difference in change in SGRQ (29). The invitation to practices to par-
ticipate was sent to those identified by primary care organizations as
likely to be interested and through an email invitation to PNs via their
professional association. Therefore, the practices may not be repre-
sentative of all practices in Australia. The identification of identifying
potentially eligible patients from practice records has limitations as
smoking status is not always accurately recorded. The response rate
of patients to the invitation was lower than in our previous study on
case finding and may be biased to more health literate patients (9).
The preponderance of participants with predominately GOLD stage
1 or 2 disease may limit the generalizability of the findings. Finally,
there is evidence from the quantitative data that the intervention was
not delivered as planned. This is a common challenge facing complex
interventions delivered via the practice team (20). Barriers and ena-
blers to implementation will be explored in the qualitative analysis.
Implications for practice
Consistent with previous research, this study demonstrates that case
finding of early stage COPD in primary care is feasible and that
there are substantial numbers of undiagnosed patients (9,10). With
monitoring of spirometry traces and expert feedback from one of the
investigators (AC), the PNs involved were able to conduct spirom-
etry to a good standard, with more than 75% of traces reviewed
meeting quality standards based on the ATS/ERS 2005 criteria (24).
However, despite education in identifying fixed airway obstruc-
tion program and provision of a decision support from a toolkit to
PNs, the practices had difficulty in correctly interpreting spirometry.
Further research is needed on how best to support primary care clini-
cians to accurately interpret spirometry.
Table 2. Participant visits to Practice Nurse in study period (n = 254)
Intervention
(n = 144)
Control
(n = 110)
One or more visits for COPD 22 (15.3%) 9 (8.2%)
One of more visits for any reason 74 (51.4%) 54 (49.1%)
Data collected for 12-month study period for each patient between Febru-
ary 2011 and August 2013.
Table 1. Baseline characteristics of groups (n = 254)
Intervention
(n = 144)
Control
(n = 110)
Age in years (SD) 66.5 (10.7) 65.4 (11.0)
Number (%) of men 88 (61.1%) 64 (58.2%)
English spoken at home 136 (94.4%) 104 (94.5%)
Currently married 97 (67.4%) 69 (62.7%)
Currently employed 55 (38.2%) 44 (40%)
Completed high school 88 (61.1%) 75 (68.2%)
Mean (SD) post-bronchodilator
FEV1
a, L
2.2 (0.7) 2.3 (0.7)
Mean (SD) post-bronchodilator
FEV1, % predicted
72.1 (17.2) 77.8 (16.5)
Number (%) no airway
obstruction (FEV1/FVC ≥ 0.7)
47 (32.6%) 31 (28.2%)
Number (%) GOLD stage 1 22 (15.3%) 32 (28.2%)
Number (%) GOLD stage 2 64 (44.4%) 42 (38.2%)
Number (%) GOLD stage 3 10 (6.9%) 5 (4.5%)
Number (%) GOLD stage 4 1 (0.7%) 0 (0%)
Current smoker 41 (28.5%) 37 (33.6%)
Mean total SGRQ score (SD) 20.0 (17.2) 18.9 (16.8)
Mean CAT score (SD) 10.5 (6.8) 9.7 (7.0)
General health status (well or
very well)
101 (70.1) 81 (73.6)
COPD knowledge score 10 (2.0) 9.9 (2.0)
Number (%) vaccinated for
influenza
97 (67.4%) 65 (59.1%)
Number (%) vaccinated for
pneumococcus
64 (44.8%) 38 (34.6%)
Mean number of co-morbid-
ities (SD)
2.5 (2.1) 2.6 (2.1)
Data collected between February 2011 and September 2012 at home visits
by project officers blind to group allocation. FEV1 = forced expiratory vol-
ume in one second; FVC = forced vital capacity; GOLD = Global Initiative on
Obstructive Lung Disease; stages describe severity from mild (stage
1) through to severe (stage 4). SGRQ = St George’s respiratory questionnaire;
CAT = COPD Assessment Test; COPD = chronic obstructive pulmonary dis-
ease. Figures are means (SDs) unless stated otherwise stated.
aSpirometry data are from practice spirometry at case-finding visit.
6 Family Practice, 2016, Vol. 00, No. 00
at La Trobe University on October 28, 2016http://fampra.oxfordjournals.org/Downloaded from
about COPD and discuss referral to pulmonary rehabilitation. Other
possible explanations are that patients with predominately mild dis-
ease do not perceive pulmonary rehabilitation as salient to their needs
or that nurses and patients were not able to overcome barriers in
access to pulmonary rehabilitation programs (34).
The differences in process of care outcomes between the two
studies may be related to the model of nurse and GP partnership
intervention. In the current study, the nurses involved were general-
ist PNs employed by the practice and an integral part of the practice
team, while in the earlier study they were dedicated COPD nurses
employed specifically for the study disease management program
(16). The latter model may empower nurses to be more involved in
education and referral but also presents challenges for local team
integration and for widespread implementation. Further research is
needed on what level of education and support is needed to enable
PNs to expand their scope of practice to include COPD management.
The rate of smoking in the participating patients at baseline was
substantial (28.5% and 33.6% in the intervention and control groups,
respectively) and the opportunity to support smoking cessation is a
key rationale for early intervention in COPD. However, despite the
PNs being trained in the use of the Lung Age Calculator (27) and
provided a care plan template designed for smokers with COPD,
there was no significant difference observed in between-group smok-
ing rates at follow-up. The lung age intervention may not have been
implemented as planned, and the study may have been underpow-
ered for this outcome. Further research on the value of feedback of
spirometry results to patients, including in the form of lung age, and
in encouraging smoking cessation in people with COPD is needed.
Strengths and limitations
Strengths of the study were the cluster randomized design, with
randomizationoccurringafter practicerecruitment,and blinded
assessment of outcomes. Limitations were that we fell substantially
short of our recruitment target, and this was compounded by unan-
ticipated misclassification in the practices of some spirometry results.
Explanations for the misclassification are explored in the qualitative
analysis reported separately. However, the fact that treatment group
by assessment–time interaction was not significant allowed us to
jointly assess outcomes measured at both 6 and 12 months in the final
intention-to-treat model (Table 3). As a result, the 95% confidence
interval around the effect estimate suggests the study still had suffi-
cient power to exclude a clinically important (4-point) between-group
difference in change in SGRQ (29). The invitation to practices to par-
ticipate was sent to those identified by primary care organizations as
likely to be interested and through an email invitation to PNs via their
professional association. Therefore, the practices may not be repre-
sentative of all practices in Australia. The identification of identifying
potentially eligible patients from practice records has limitations as
smoking status is not always accurately recorded. The response rate
of patients to the invitation was lower than in our previous study on
case finding and may be biased to more health literate patients (9).
The preponderance of participants with predominately GOLD stage
1 or 2 disease may limit the generalizability of the findings. Finally,
there is evidence from the quantitative data that the intervention was
not delivered as planned. This is a common challenge facing complex
interventions delivered via the practice team (20). Barriers and ena-
blers to implementation will be explored in the qualitative analysis.
Implications for practice
Consistent with previous research, this study demonstrates that case
finding of early stage COPD in primary care is feasible and that
there are substantial numbers of undiagnosed patients (9,10). With
monitoring of spirometry traces and expert feedback from one of the
investigators (AC), the PNs involved were able to conduct spirom-
etry to a good standard, with more than 75% of traces reviewed
meeting quality standards based on the ATS/ERS 2005 criteria (24).
However, despite education in identifying fixed airway obstruc-
tion program and provision of a decision support from a toolkit to
PNs, the practices had difficulty in correctly interpreting spirometry.
Further research is needed on how best to support primary care clini-
cians to accurately interpret spirometry.
Table 2. Participant visits to Practice Nurse in study period (n = 254)
Intervention
(n = 144)
Control
(n = 110)
One or more visits for COPD 22 (15.3%) 9 (8.2%)
One of more visits for any reason 74 (51.4%) 54 (49.1%)
Data collected for 12-month study period for each patient between Febru-
ary 2011 and August 2013.
Table 1. Baseline characteristics of groups (n = 254)
Intervention
(n = 144)
Control
(n = 110)
Age in years (SD) 66.5 (10.7) 65.4 (11.0)
Number (%) of men 88 (61.1%) 64 (58.2%)
English spoken at home 136 (94.4%) 104 (94.5%)
Currently married 97 (67.4%) 69 (62.7%)
Currently employed 55 (38.2%) 44 (40%)
Completed high school 88 (61.1%) 75 (68.2%)
Mean (SD) post-bronchodilator
FEV1
a, L
2.2 (0.7) 2.3 (0.7)
Mean (SD) post-bronchodilator
FEV1, % predicted
72.1 (17.2) 77.8 (16.5)
Number (%) no airway
obstruction (FEV1/FVC ≥ 0.7)
47 (32.6%) 31 (28.2%)
Number (%) GOLD stage 1 22 (15.3%) 32 (28.2%)
Number (%) GOLD stage 2 64 (44.4%) 42 (38.2%)
Number (%) GOLD stage 3 10 (6.9%) 5 (4.5%)
Number (%) GOLD stage 4 1 (0.7%) 0 (0%)
Current smoker 41 (28.5%) 37 (33.6%)
Mean total SGRQ score (SD) 20.0 (17.2) 18.9 (16.8)
Mean CAT score (SD) 10.5 (6.8) 9.7 (7.0)
General health status (well or
very well)
101 (70.1) 81 (73.6)
COPD knowledge score 10 (2.0) 9.9 (2.0)
Number (%) vaccinated for
influenza
97 (67.4%) 65 (59.1%)
Number (%) vaccinated for
pneumococcus
64 (44.8%) 38 (34.6%)
Mean number of co-morbid-
ities (SD)
2.5 (2.1) 2.6 (2.1)
Data collected between February 2011 and September 2012 at home visits
by project officers blind to group allocation. FEV1 = forced expiratory vol-
ume in one second; FVC = forced vital capacity; GOLD = Global Initiative on
Obstructive Lung Disease; stages describe severity from mild (stage
1) through to severe (stage 4). SGRQ = St George’s respiratory questionnaire;
CAT = COPD Assessment Test; COPD = chronic obstructive pulmonary dis-
ease. Figures are means (SDs) unless stated otherwise stated.
aSpirometry data are from practice spirometry at case-finding visit.
6 Family Practice, 2016, Vol. 00, No. 00
at La Trobe University on October 28, 2016http://fampra.oxfordjournals.org/Downloaded from
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Despite the appeal and potential of early intervention for COPD
in primary care, the complex intervention of nurse and GP educa-
tion and care planning tools tested in this study were not effective
in improving health-related QoL for patients with newly diagnosed
COPD. A low level of intervention implementation is a possible
explanation for the lack of effect. Further research is needed to iden-
tify interventions, such as those aimed at reducing smoking rates,
that are beneficial to patients with early stage COPD and that could
be implemented by the generalist primary care team.
Acknowledgement
Trial registration: ACTRN12610000592044. This paper honours the memory
of Jeremy Bunker, without whose initiative and enthusiasm this study would
not have taken place. The participation of Practice Nurses and GPs and the
input of Professor S Teng Liaw into the study design, and Charmaine Rodricks
for administrative assistance, are greatly appreciated.
Declaration
Funding: Australian National Health and Medical Research Council (630421).
Ethical approval: UNSW Australia Human ResearchEthics Committee
approval number 10015.
Conflict of interest: none.
References
1. World Health Organization. Global Surveillance, Prevention and Control
of Chronic Respiratory Diseases: A Comprehensive Approach. Geneva,
Switzerland: World Health Organization, 2007.
2. Global Initiative for Chronic Obstructive Pulmonary Disease (GOLD).
Global Strategy for Diagnosis, Management and Prevention of COPD.
2011. www.goldcopd.com. (accessed on 7 November 2011).
3. Roche N, Dalmay F, Perez T et al. Impact of chronic airflow obstruction in
a working population. Eur Respir J 2008; 31: 1227–33.
4. Akazawa M, Halpern R, Riedel AA, Stanford RH, Dalal A, Blanchette
CM. Economic burden prior to COPD diagnosis: a matched case-control
study in the United States. Respir Med 2008; 102: 1744–52.
5. Doherty DE. Early detection and management of COPD. What you can do
to reduce the impact of this disabling disease. Postgrad Med J 2002; 111:
41–44, 49–50, 53 passim.
6. Anthonisen NR, Connett JE, Kiley JP et al. Effects of smoking intervention
and the use of an inhaled anticholinergic bronchodilator on the rate of
decline of FEV1. The Lung Health Study. JAMA 1994; 272: 1497–505.
7. Levy ML, Fletcher M, Price DB, Hausen T, Halbert RJ, Yawn BP. Interna-
tional Primary Care Respiratory Group (IPCRG) Guidelines: diagnosis of
respiratory diseases in primary care. Prim Care Respir J 2006; 15: 20–34.
8. Meulepas MA, Jacobs JE, Lucas AEM, et al. The feasibility of a primary
care model for the management of COPD. Prim Care Respir J 2006; 15:
337–41.
9. Bunker J, Hermiz O, Zwar N et al. Feasibility and efficacy of COPD case
finding by practice nurses. Aust Fam Physician 2009; 38: 826–30.
10. Bolton CE, Ionescu AA, Edwards PH, Faulkner TA, Edwards SM, Shale
DJ. Attaining a correct diagnosis of COPD in general practice. Respir Med
2005; 99: 493–500.
11. McKenzie DK, Abramson M, Crockett AJ et al. The COPD-X Plan:
Australian and New Zealand Guidelines for the Management of Chronic
Obstructive Pulmonary Disease. 2011. www.copdx.org.au. (accessed on
10 February 2012).
12. Ta M, George J. Management of chronic obstructive pulmonary disease in
Australia after the publication of national guidelines. Int Med J 2011; 41:
263–70.
13. Matheson MC, Abeysena C, Raven JM et al. How have we been manag-
ing chronic obstructive pulmonary disease in Australia? Int Med J 2006;
36: 92–9.
14. Vrijhoef HJ, Diederiks JP, Spreeuwenberg C. Effects on quality of care for
patients with NIDDM or COPD when the specialised nurse has a central
role: a literature review. Patient Educ Couns 2000; 41: 243–50.
15. Zakrisson A-B, Engfeldt P, Hagglund D et al. Nurse-led multidisciplinary
programme for patients with COPD in primary health care: a controlled
trial. Prim Care Respir J 2011; 20: 427–33.
Table 3. Outcome measures: between group differences at follow-up adjusted for baseline values
Outcome Intervention Control Differencea (95% CI) P value
Baseline (n = 144)Follow up (n = 126)Baseline (n = 110)Follow up (n = 96)
Mean SGRQ (SD) 20.0 (17.2) 16.85 (15.2) 18.9 (16.8) 17.06 (14.9) −0.21 (−2.55 to 2.14)0.86
CAT (SD) 10.5 (6.8) 9.80 (6.78) 9.7 (7.0) 9.27 (6.78) −0.20 (−1.53 to 1.12)0.73
Mean (SD) FEV1 2.2 (0.7) 2.15 (0.72) 2.3 (0.7) 2.38 (0.74) 0.07 (−0.35 to 0.01)0.78
Mean COPD knowledge score
(SD)
10 (2.0) 10.4 (1.89) 9.9 (2.0) 10.3 (1.79) 0.09 (−0.38 to 0.55)0.72
Odds ratio (95% CI)
General health status (well or
very well)
101 (70.1) 94 (74.6) 81 (73.6) 82 (85.4) 0.55 (0.27–1.1) 0.09
Aware of COPD diagnosis 76 (52.8) 58 (46.0%) 56 (50.9) 44 (45.8%) 0.93 (0.56–1.55) 0.79
Number (%) of current smokers 41 (28.5%) 28 (22.2%) 37 (33.6%) 25 (26.0%) 0.92 (0.44–1.91) 0.82
Number (%) vaccinated for
influenza
97 (67.4%) 91 (72.8%) 65 (59.1%) 54 (56.8%) 2.31 (1.06–5.03) 0.035
Number (%) vaccinated for
pneumococcus
64 (44.8%) 56 (47.9%) 38 (34.6%) 36 (38.3%) 1.54 (0.86–2.71) 0.15
Number (%) attended pulmonary
rehabilitation
2 (1.4) 1 (0.8%) 0 1 (1.0%) n/a n/a
Inhalers used correctly 11 (7.6) 45 (35.7%) 10 (9.1) 42 (43.8%) 0.74 (0.44–1.24) 0.25
Health service used for lung
condition
18 (12.5) 17 (13.5%) 13 (11.8) 11 (11.5%) 1.21 (0.50–2.88) 0.67
Data collected between March 2012 and August 2013 at home visits by project officers blind to group allocation. SGRQ = St George’s respiratory questionn
CAT = COPD Assessment Test; FEV1 = forced expiratory volume in one second. Figures are means (SDs) unless stated otherwise stated.
aThe least square difference is reported in this table; this may differ from the raw difference between the follow-up means in the control and intervention g
Early intervention for chronic obstructive pulmonary disease by practice nurse and GP teams 7
at La Trobe University on October 28, 2016http://fampra.oxfordjournals.org/Downloaded from
in primary care, the complex intervention of nurse and GP educa-
tion and care planning tools tested in this study were not effective
in improving health-related QoL for patients with newly diagnosed
COPD. A low level of intervention implementation is a possible
explanation for the lack of effect. Further research is needed to iden-
tify interventions, such as those aimed at reducing smoking rates,
that are beneficial to patients with early stage COPD and that could
be implemented by the generalist primary care team.
Acknowledgement
Trial registration: ACTRN12610000592044. This paper honours the memory
of Jeremy Bunker, without whose initiative and enthusiasm this study would
not have taken place. The participation of Practice Nurses and GPs and the
input of Professor S Teng Liaw into the study design, and Charmaine Rodricks
for administrative assistance, are greatly appreciated.
Declaration
Funding: Australian National Health and Medical Research Council (630421).
Ethical approval: UNSW Australia Human ResearchEthics Committee
approval number 10015.
Conflict of interest: none.
References
1. World Health Organization. Global Surveillance, Prevention and Control
of Chronic Respiratory Diseases: A Comprehensive Approach. Geneva,
Switzerland: World Health Organization, 2007.
2. Global Initiative for Chronic Obstructive Pulmonary Disease (GOLD).
Global Strategy for Diagnosis, Management and Prevention of COPD.
2011. www.goldcopd.com. (accessed on 7 November 2011).
3. Roche N, Dalmay F, Perez T et al. Impact of chronic airflow obstruction in
a working population. Eur Respir J 2008; 31: 1227–33.
4. Akazawa M, Halpern R, Riedel AA, Stanford RH, Dalal A, Blanchette
CM. Economic burden prior to COPD diagnosis: a matched case-control
study in the United States. Respir Med 2008; 102: 1744–52.
5. Doherty DE. Early detection and management of COPD. What you can do
to reduce the impact of this disabling disease. Postgrad Med J 2002; 111:
41–44, 49–50, 53 passim.
6. Anthonisen NR, Connett JE, Kiley JP et al. Effects of smoking intervention
and the use of an inhaled anticholinergic bronchodilator on the rate of
decline of FEV1. The Lung Health Study. JAMA 1994; 272: 1497–505.
7. Levy ML, Fletcher M, Price DB, Hausen T, Halbert RJ, Yawn BP. Interna-
tional Primary Care Respiratory Group (IPCRG) Guidelines: diagnosis of
respiratory diseases in primary care. Prim Care Respir J 2006; 15: 20–34.
8. Meulepas MA, Jacobs JE, Lucas AEM, et al. The feasibility of a primary
care model for the management of COPD. Prim Care Respir J 2006; 15:
337–41.
9. Bunker J, Hermiz O, Zwar N et al. Feasibility and efficacy of COPD case
finding by practice nurses. Aust Fam Physician 2009; 38: 826–30.
10. Bolton CE, Ionescu AA, Edwards PH, Faulkner TA, Edwards SM, Shale
DJ. Attaining a correct diagnosis of COPD in general practice. Respir Med
2005; 99: 493–500.
11. McKenzie DK, Abramson M, Crockett AJ et al. The COPD-X Plan:
Australian and New Zealand Guidelines for the Management of Chronic
Obstructive Pulmonary Disease. 2011. www.copdx.org.au. (accessed on
10 February 2012).
12. Ta M, George J. Management of chronic obstructive pulmonary disease in
Australia after the publication of national guidelines. Int Med J 2011; 41:
263–70.
13. Matheson MC, Abeysena C, Raven JM et al. How have we been manag-
ing chronic obstructive pulmonary disease in Australia? Int Med J 2006;
36: 92–9.
14. Vrijhoef HJ, Diederiks JP, Spreeuwenberg C. Effects on quality of care for
patients with NIDDM or COPD when the specialised nurse has a central
role: a literature review. Patient Educ Couns 2000; 41: 243–50.
15. Zakrisson A-B, Engfeldt P, Hagglund D et al. Nurse-led multidisciplinary
programme for patients with COPD in primary health care: a controlled
trial. Prim Care Respir J 2011; 20: 427–33.
Table 3. Outcome measures: between group differences at follow-up adjusted for baseline values
Outcome Intervention Control Differencea (95% CI) P value
Baseline (n = 144)Follow up (n = 126)Baseline (n = 110)Follow up (n = 96)
Mean SGRQ (SD) 20.0 (17.2) 16.85 (15.2) 18.9 (16.8) 17.06 (14.9) −0.21 (−2.55 to 2.14)0.86
CAT (SD) 10.5 (6.8) 9.80 (6.78) 9.7 (7.0) 9.27 (6.78) −0.20 (−1.53 to 1.12)0.73
Mean (SD) FEV1 2.2 (0.7) 2.15 (0.72) 2.3 (0.7) 2.38 (0.74) 0.07 (−0.35 to 0.01)0.78
Mean COPD knowledge score
(SD)
10 (2.0) 10.4 (1.89) 9.9 (2.0) 10.3 (1.79) 0.09 (−0.38 to 0.55)0.72
Odds ratio (95% CI)
General health status (well or
very well)
101 (70.1) 94 (74.6) 81 (73.6) 82 (85.4) 0.55 (0.27–1.1) 0.09
Aware of COPD diagnosis 76 (52.8) 58 (46.0%) 56 (50.9) 44 (45.8%) 0.93 (0.56–1.55) 0.79
Number (%) of current smokers 41 (28.5%) 28 (22.2%) 37 (33.6%) 25 (26.0%) 0.92 (0.44–1.91) 0.82
Number (%) vaccinated for
influenza
97 (67.4%) 91 (72.8%) 65 (59.1%) 54 (56.8%) 2.31 (1.06–5.03) 0.035
Number (%) vaccinated for
pneumococcus
64 (44.8%) 56 (47.9%) 38 (34.6%) 36 (38.3%) 1.54 (0.86–2.71) 0.15
Number (%) attended pulmonary
rehabilitation
2 (1.4) 1 (0.8%) 0 1 (1.0%) n/a n/a
Inhalers used correctly 11 (7.6) 45 (35.7%) 10 (9.1) 42 (43.8%) 0.74 (0.44–1.24) 0.25
Health service used for lung
condition
18 (12.5) 17 (13.5%) 13 (11.8) 11 (11.5%) 1.21 (0.50–2.88) 0.67
Data collected between March 2012 and August 2013 at home visits by project officers blind to group allocation. SGRQ = St George’s respiratory questionn
CAT = COPD Assessment Test; FEV1 = forced expiratory volume in one second. Figures are means (SDs) unless stated otherwise stated.
aThe least square difference is reported in this table; this may differ from the raw difference between the follow-up means in the control and intervention g
Early intervention for chronic obstructive pulmonary disease by practice nurse and GP teams 7
at La Trobe University on October 28, 2016http://fampra.oxfordjournals.org/Downloaded from
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

16. Zwar NA, Hermiz O, Comino E et al. Care of patients with a diagnosis
of chronic obstructive pulmonary disease: a cluster randomised controlled
trial. Med J Aust 2012; 197: 394–98.
17. Wong CX, Carson KV, Smith BJ. Home care by outreach nursing for
chronic obstructive pulmonary disease. Cochrane Database Syst Rev
2011; 3:CD000994.
18. Kruis AL, Smidt N, Assendelft WJ et al. Cochrane corner: is integrated
disease management for patients with COPD effective? Thorax 2014; 69:
1053–5.
19. Zwerink M, Brusse-Keizer M, van der Valk PD, et al. Self management for
patients with chronic obstructive pulmonary disease. Cochrane Database
Syst Rev 2014; 3: CD002990.
20. Kruis AL, Boland MR, Assendelft WJ et al. Effectiveness of integrated dis-
ease management for primary care chronic obstructive pulmonary disease
patients: results of cluster randomised trial. BMJ 2014; 349: g5392.
21. Bischoff EW, Akkermans R, Bourbeau J, van Weel C, Vercoulen JH,
Schermer TR. Comprehensive self management and routine monitoring in
chronic obstructive pulmonary disease patients in general practice: ran-
domised controlled trial. BMJ 2012; 345: e7642.
22. Bunker JM, Reddel HK, Dennis SM et al. A pragmatic cluster randomized
controlled trial of early intervention for chronic obstructive pulmonary
disease by practice nurse-general practitioner teams: Study Protocol.
Implement Sci 2012; 7: 83.
23. Miller MR, Crapo R, Hankinson J et al. General considerations for lung
function testing. Eur Respir J 2005; 26: 153–61.
24. Levy ML, Quanjer PH, Booker R et al. Diagnostic spirometry in primary
care: Proposed standards for general practice compliant with American
Thoracic Society and European Respiratory Society recommendations: a
General Practice Airways Group (GPIAG) document, in association with
the Association for Respiratory Technology & Physiology (ARTP) and
Education for Health. Prim Care Respir J 2009; 18: 130–47.
25. Primary Care Respiratory Toolkit. 2015. http://lungfoundation.com.au/
health-professionals/clinical-resources/copd/primary-care-respiratory-
toolkit/. (accessed on 11 March 2015).
26. Australian Bureau of Statistics. Socio-Economic Indices for Areas (technical
paper). 2006. http://www.abs.gov.au/ausstats/abs@.nsf/mf/2039.0.55.001/.
(accessed on 20 January 2009).
27. Parkes G, Greenhalgh T, Griffin M, Dent R. Effect on smoking quit rate of
telling patients their lung age: the Step2quit randomised controlled trial.
BMJ 2008; 336: 598–600.
28. National Asthma Council. Inhaler technique in adults with asthma or
COPD. 2008. http://www.nationalasthma.org.au/html/management/info_
inhaler/Inhaler_technique_in_adults_with_asthma_or_COPD.pdf.
(accessed 20 January 2009)
29. Jones PW, Quirk FH, Baveystock CM, Littlejohns P. A self-complete meas-
ure of health status for chronic airflow limitation. The St. George’s Res-
piratory Questionnaire. Am Rev Respir Dis 1992; 145: 1321–27.
30. Jones PW, Harding G, Berry P, Wiklund I, Chen WH, Kline Leidy N.
Development and first validation of the COPD Assessment Test. Eur Respir
J 2009; 34: 648–54.
31. HermizO, Comino E, Marks G, Daffurn K, Wilson S, Harris M.
Randomised controlled trial of home based care of patients with chronic
obstructive pulmonary disease. BMJ 2002; 325: 938.
32. Jones PW, Brusselle G, Dal Negro RW et al. Patient-centred assessment
of COPD in primary care: experience from a cross-sectional study of
health-related quality of life in Europe. Prim Care Respir J 2012; 21:
329–36.
33. Joyce CM, Piterman L. The work of nurses in Australian general practice:
A national survey. Int J Nurs Stud 2011; 48: 70–80.
34. Holland AE, Hill CJ, Glaspole I, Goh N, McDonald CF. Predictors of ben-
efit following pulmonary rehabilitation for interstitial lung disease. Respir
Med 2012; 106: 429–35.
8 Family Practice, 2016, Vol. 00, No. 00
at La Trobe University on October 28, 2016http://fampra.oxfordjournals.org/Downloaded from
of chronic obstructive pulmonary disease: a cluster randomised controlled
trial. Med J Aust 2012; 197: 394–98.
17. Wong CX, Carson KV, Smith BJ. Home care by outreach nursing for
chronic obstructive pulmonary disease. Cochrane Database Syst Rev
2011; 3:CD000994.
18. Kruis AL, Smidt N, Assendelft WJ et al. Cochrane corner: is integrated
disease management for patients with COPD effective? Thorax 2014; 69:
1053–5.
19. Zwerink M, Brusse-Keizer M, van der Valk PD, et al. Self management for
patients with chronic obstructive pulmonary disease. Cochrane Database
Syst Rev 2014; 3: CD002990.
20. Kruis AL, Boland MR, Assendelft WJ et al. Effectiveness of integrated dis-
ease management for primary care chronic obstructive pulmonary disease
patients: results of cluster randomised trial. BMJ 2014; 349: g5392.
21. Bischoff EW, Akkermans R, Bourbeau J, van Weel C, Vercoulen JH,
Schermer TR. Comprehensive self management and routine monitoring in
chronic obstructive pulmonary disease patients in general practice: ran-
domised controlled trial. BMJ 2012; 345: e7642.
22. Bunker JM, Reddel HK, Dennis SM et al. A pragmatic cluster randomized
controlled trial of early intervention for chronic obstructive pulmonary
disease by practice nurse-general practitioner teams: Study Protocol.
Implement Sci 2012; 7: 83.
23. Miller MR, Crapo R, Hankinson J et al. General considerations for lung
function testing. Eur Respir J 2005; 26: 153–61.
24. Levy ML, Quanjer PH, Booker R et al. Diagnostic spirometry in primary
care: Proposed standards for general practice compliant with American
Thoracic Society and European Respiratory Society recommendations: a
General Practice Airways Group (GPIAG) document, in association with
the Association for Respiratory Technology & Physiology (ARTP) and
Education for Health. Prim Care Respir J 2009; 18: 130–47.
25. Primary Care Respiratory Toolkit. 2015. http://lungfoundation.com.au/
health-professionals/clinical-resources/copd/primary-care-respiratory-
toolkit/. (accessed on 11 March 2015).
26. Australian Bureau of Statistics. Socio-Economic Indices for Areas (technical
paper). 2006. http://www.abs.gov.au/ausstats/abs@.nsf/mf/2039.0.55.001/.
(accessed on 20 January 2009).
27. Parkes G, Greenhalgh T, Griffin M, Dent R. Effect on smoking quit rate of
telling patients their lung age: the Step2quit randomised controlled trial.
BMJ 2008; 336: 598–600.
28. National Asthma Council. Inhaler technique in adults with asthma or
COPD. 2008. http://www.nationalasthma.org.au/html/management/info_
inhaler/Inhaler_technique_in_adults_with_asthma_or_COPD.pdf.
(accessed 20 January 2009)
29. Jones PW, Quirk FH, Baveystock CM, Littlejohns P. A self-complete meas-
ure of health status for chronic airflow limitation. The St. George’s Res-
piratory Questionnaire. Am Rev Respir Dis 1992; 145: 1321–27.
30. Jones PW, Harding G, Berry P, Wiklund I, Chen WH, Kline Leidy N.
Development and first validation of the COPD Assessment Test. Eur Respir
J 2009; 34: 648–54.
31. HermizO, Comino E, Marks G, Daffurn K, Wilson S, Harris M.
Randomised controlled trial of home based care of patients with chronic
obstructive pulmonary disease. BMJ 2002; 325: 938.
32. Jones PW, Brusselle G, Dal Negro RW et al. Patient-centred assessment
of COPD in primary care: experience from a cross-sectional study of
health-related quality of life in Europe. Prim Care Respir J 2012; 21:
329–36.
33. Joyce CM, Piterman L. The work of nurses in Australian general practice:
A national survey. Int J Nurs Stud 2011; 48: 70–80.
34. Holland AE, Hill CJ, Glaspole I, Goh N, McDonald CF. Predictors of ben-
efit following pulmonary rehabilitation for interstitial lung disease. Respir
Med 2012; 106: 429–35.
8 Family Practice, 2016, Vol. 00, No. 00
at La Trobe University on October 28, 2016http://fampra.oxfordjournals.org/Downloaded from
1 out of 8
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





