Effectiveness of Structured Hourly Nurse | Report
VerifiedAdded on 2022/10/04
|7
|4692
|24
Assignment
AI Summary
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
LWW/JNCQ JNCQ-D-14-00043 January 31, 2015 17:46
J Nurs Care Qual
Vol. 30, No. 2, pp. 153–159
Copyrightc 2015 Wolters Kluwer Health, Inc. All rights reserved.
Effectiveness of Structured
Hourly Nurse Rounding on
Patient Satisfaction and Clinical
Outcomes
Lisa A. Brosey, DNP, RN, CPHQ;
Karen S. March, PhD, RN, ACNS-BC
Structured hourly nurse rounding is an effective method to improve patient satisfaction and clin-
icaloutcomes.This program evaluation describes outcomes related to the implementation of
hourly nurse rounding in one medical-surgical unit in a large community hospital. Overall Hospital
Consumer Assessment of Healthcare Providers and Systems domain scores increased with the ex-
ception of responsiveness of staff. Patient falls and hospital-acquired pressure ulcers decreased dur-
ing the project period. Key words: accidental falls, evidence-based nursing/standards, hourly
rounding, PARiHS framework, patient satisfaction, pressure ulcer/prevention and control
ACUTE CARE FACILITIES continue to eval-
uate cost-effectiveness methodsto en-
hance patient satisfaction and improve patient
safety.A growing body of evidence describ-
ing the positive effects ofstructured nurse
rounding on patient satisfaction and clinical
outcomes has emerged within the past few
years.1−25 On the basis of this emerging evi-
dence and the positive effects demonstrated,
many organizations in the United States and
Author Affiliations: Lancaster General Health,
Lancaster, Pennsylvania (Dr Brosey), and The
Stabler Department of Nursing, York College of
Pennsylvania, York (Dr March).
No funding was received for this work.
The authors declare no conflict of interest.
Supplemental digital content is available for this article.
Direct URL citations appear in the printed text and are
provided in the HTML and PDF versions of this article
on the journal’s Web site (www.jncqjournal.com).
Correspondence:Lisa A. Brosey,DNP, RN, CPHQ,
Lancaster General Health, Lancaster, PA 17604
(labrosey@lghealth.org).
Accepted for publication: July 19, 2014
Published online before print: September 18, 2014
DOI: 10.1097/NCQ.0000000000000086
the United Kingdom have instituted hourly
nurse rounding as a standard component of
nursing practice in an attempt to improve pa-
tientsatisfaction and reduce patientharm.*
Hourly nurse rounding entails assessment of
3 to 12 elements on each patient every hour
between 6AMto 10PMand then every 2 hours
from 10PMto 6AM.1,6,9 Rounds are reduced
to every 2 hours during the night so that sleep
patterns are less disturbed and patients are not
awakened unnecessarily.
The most noted elementsassessed dur-
ing hourly nurse roundinginclude pain
level, need for toileting or elimination,
assessmentof the environmentincluding
room temperature,proximityof personal
items, safety hazards,and positioningof
the patientor need to change the patient’s
position.1,2,4,6,7,9,11−21,23−25
Studies on hourly
nurse rounding reveal that patients re-
port higherpatientsatisfaction,fewer pa-
tient falls and hospital-acquiredpressure
ulcers (HAPUs),and decreasedcall bell
activation.1−22,24,25Evidence further suggests
*References1 ,3 ,6 ,7 ,10-13,16, 17, 20-22.
Copyright © 2015 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
153
J Nurs Care Qual
Vol. 30, No. 2, pp. 153–159
Copyrightc 2015 Wolters Kluwer Health, Inc. All rights reserved.
Effectiveness of Structured
Hourly Nurse Rounding on
Patient Satisfaction and Clinical
Outcomes
Lisa A. Brosey, DNP, RN, CPHQ;
Karen S. March, PhD, RN, ACNS-BC
Structured hourly nurse rounding is an effective method to improve patient satisfaction and clin-
icaloutcomes.This program evaluation describes outcomes related to the implementation of
hourly nurse rounding in one medical-surgical unit in a large community hospital. Overall Hospital
Consumer Assessment of Healthcare Providers and Systems domain scores increased with the ex-
ception of responsiveness of staff. Patient falls and hospital-acquired pressure ulcers decreased dur-
ing the project period. Key words: accidental falls, evidence-based nursing/standards, hourly
rounding, PARiHS framework, patient satisfaction, pressure ulcer/prevention and control
ACUTE CARE FACILITIES continue to eval-
uate cost-effectiveness methodsto en-
hance patient satisfaction and improve patient
safety.A growing body of evidence describ-
ing the positive effects ofstructured nurse
rounding on patient satisfaction and clinical
outcomes has emerged within the past few
years.1−25 On the basis of this emerging evi-
dence and the positive effects demonstrated,
many organizations in the United States and
Author Affiliations: Lancaster General Health,
Lancaster, Pennsylvania (Dr Brosey), and The
Stabler Department of Nursing, York College of
Pennsylvania, York (Dr March).
No funding was received for this work.
The authors declare no conflict of interest.
Supplemental digital content is available for this article.
Direct URL citations appear in the printed text and are
provided in the HTML and PDF versions of this article
on the journal’s Web site (www.jncqjournal.com).
Correspondence:Lisa A. Brosey,DNP, RN, CPHQ,
Lancaster General Health, Lancaster, PA 17604
(labrosey@lghealth.org).
Accepted for publication: July 19, 2014
Published online before print: September 18, 2014
DOI: 10.1097/NCQ.0000000000000086
the United Kingdom have instituted hourly
nurse rounding as a standard component of
nursing practice in an attempt to improve pa-
tientsatisfaction and reduce patientharm.*
Hourly nurse rounding entails assessment of
3 to 12 elements on each patient every hour
between 6AMto 10PMand then every 2 hours
from 10PMto 6AM.1,6,9 Rounds are reduced
to every 2 hours during the night so that sleep
patterns are less disturbed and patients are not
awakened unnecessarily.
The most noted elementsassessed dur-
ing hourly nurse roundinginclude pain
level, need for toileting or elimination,
assessmentof the environmentincluding
room temperature,proximityof personal
items, safety hazards,and positioningof
the patientor need to change the patient’s
position.1,2,4,6,7,9,11−21,23−25
Studies on hourly
nurse rounding reveal that patients re-
port higherpatientsatisfaction,fewer pa-
tient falls and hospital-acquiredpressure
ulcers (HAPUs),and decreasedcall bell
activation.1−22,24,25Evidence further suggests
*References1 ,3 ,6 ,7 ,10-13,16, 17, 20-22.
Copyright © 2015 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
153
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
LWW/JNCQ JNCQ-D-14-00043 January 31, 2015 17:46
154 JOURNAL OFNURSINGCAREQUALITY/APRIL–JUNE2015
that nursingcare stronglycontributesto
patients’perceptionsof overallsatisfaction
and likelihood to recommend a facility to
others.26−30 SupplementalDigitalContent,
Table (availableat: http://links.lww.com/
JNCQ/A126),provides a summary of studies
on the effects of structured nurse rounding on
patient satisfaction,patient falls,HAPU,and
call light usage.
LOCAL PROBLEM
The project facilityadopted structured
hourly nurse rounding as a standard of nurs-
ing care in 2008;however,there was little
structure to and accountability for implemen-
tation of this practice. As a result, past efforts
with hourly nurse rounding were inconsistent
and ineffective. Discussions with the nursing
staff and observation of practice revealed min-
imal compliance with hourly nurse rounding
processor the intentto assesspain, elim-
ination,environment,and position (PEEP)
proactively in the current day. Therefore, the
projectleadermet with nursing leadership
to present current evidence and benefits as-
sociated with thisintervention and to gar-
ner support for implementation on one pilot
unit. The project unit was a 24-bed medical-
surgical nursing unit with private and semipri-
vate rooms. This unit was selected on the basis
of its need for improvement in patient satisfac-
tion scores (lowest rating of medical-surgical
units in facility) as well as its higher incidence
of patient falls (2 times the national mean) and
HAPUs (higher than facility mean).
Intended improvement/study question
The purpose of this project was to imple-
ment a standardized structured hourly nurse
rounding processand to monitorthe out-
comes of patient satisfaction, patient falls, and
HAPUs over a 3-month time period.
METHODS
Setting
Promoting Action on Research Implemen-
tation in Health Services(PARiHS)frame-
work was the translation model used for the
project.31 This framework isbased on the
premise that successful implementation of ev-
idence into practice is dependent on 3 fac-
tors:evidence,context or environment,and
facilitation. Each factor has equal importance
in the implementation process and is interre-
lated with other factors.For example,if the
evidence is strong and the environment is ac-
cessible to change, then the facilitation of the
change process willbe less rigorous and de-
manding.In contrast,if the evidence is not
strong and the environment is not adaptive to
change,the facilitation process may require
a higher levelof supportand change man-
agement skills for successful implementation
to occur. The framework requires evaluation
and presentation of the supporting evidence,
evaluation and analysis of the context or en-
vironment (including support from manage-
ment and the culture for change ofthe en-
vironment),and the use offacilitating tech-
niques that are fluid and adaptive to the chang-
ing environment.
For this project, the level of evidence was
rated low (mostof the evidence on hourly
nurse roundingincluded qualityimprove-
ment program evaluations) whereas context
or environment was rated high (demonstrated
by the expressed attitudesand beliefsof
the majority of staff members and leadership
aboutthe value ofimproving the care pro-
vided to patients and the desire to reduce
harm).Since the evidence componentwas
low and the contextcomponentwas high,
the facilitation method suggested by the PAR-
iHS framework was to enable and empower
the staff to take control of their learning and
change process needs through mentoring and
supportof staffdecisions.31 Discussions re-
garding current best practices and the posi-
tive effects of structured hourly nurse round-
ing practices were key elements in supporting
the staff to be active in the decision to move
forward with implementation. Institutional re-
view board–exemptapprovalwas obtained
for this evidence-based practice project.
Planning the intervention
A literature search was conducted using
CINAHL,PubMed,CochraneDatabaseof
Copyright © 2015 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
154 JOURNAL OFNURSINGCAREQUALITY/APRIL–JUNE2015
that nursingcare stronglycontributesto
patients’perceptionsof overallsatisfaction
and likelihood to recommend a facility to
others.26−30 SupplementalDigitalContent,
Table (availableat: http://links.lww.com/
JNCQ/A126),provides a summary of studies
on the effects of structured nurse rounding on
patient satisfaction,patient falls,HAPU,and
call light usage.
LOCAL PROBLEM
The project facilityadopted structured
hourly nurse rounding as a standard of nurs-
ing care in 2008;however,there was little
structure to and accountability for implemen-
tation of this practice. As a result, past efforts
with hourly nurse rounding were inconsistent
and ineffective. Discussions with the nursing
staff and observation of practice revealed min-
imal compliance with hourly nurse rounding
processor the intentto assesspain, elim-
ination,environment,and position (PEEP)
proactively in the current day. Therefore, the
projectleadermet with nursing leadership
to present current evidence and benefits as-
sociated with thisintervention and to gar-
ner support for implementation on one pilot
unit. The project unit was a 24-bed medical-
surgical nursing unit with private and semipri-
vate rooms. This unit was selected on the basis
of its need for improvement in patient satisfac-
tion scores (lowest rating of medical-surgical
units in facility) as well as its higher incidence
of patient falls (2 times the national mean) and
HAPUs (higher than facility mean).
Intended improvement/study question
The purpose of this project was to imple-
ment a standardized structured hourly nurse
rounding processand to monitorthe out-
comes of patient satisfaction, patient falls, and
HAPUs over a 3-month time period.
METHODS
Setting
Promoting Action on Research Implemen-
tation in Health Services(PARiHS)frame-
work was the translation model used for the
project.31 This framework isbased on the
premise that successful implementation of ev-
idence into practice is dependent on 3 fac-
tors:evidence,context or environment,and
facilitation. Each factor has equal importance
in the implementation process and is interre-
lated with other factors.For example,if the
evidence is strong and the environment is ac-
cessible to change, then the facilitation of the
change process willbe less rigorous and de-
manding.In contrast,if the evidence is not
strong and the environment is not adaptive to
change,the facilitation process may require
a higher levelof supportand change man-
agement skills for successful implementation
to occur. The framework requires evaluation
and presentation of the supporting evidence,
evaluation and analysis of the context or en-
vironment (including support from manage-
ment and the culture for change ofthe en-
vironment),and the use offacilitating tech-
niques that are fluid and adaptive to the chang-
ing environment.
For this project, the level of evidence was
rated low (mostof the evidence on hourly
nurse roundingincluded qualityimprove-
ment program evaluations) whereas context
or environment was rated high (demonstrated
by the expressed attitudesand beliefsof
the majority of staff members and leadership
aboutthe value ofimproving the care pro-
vided to patients and the desire to reduce
harm).Since the evidence componentwas
low and the contextcomponentwas high,
the facilitation method suggested by the PAR-
iHS framework was to enable and empower
the staff to take control of their learning and
change process needs through mentoring and
supportof staffdecisions.31 Discussions re-
garding current best practices and the posi-
tive effects of structured hourly nurse round-
ing practices were key elements in supporting
the staff to be active in the decision to move
forward with implementation. Institutional re-
view board–exemptapprovalwas obtained
for this evidence-based practice project.
Planning the intervention
A literature search was conducted using
CINAHL,PubMed,CochraneDatabaseof
Copyright © 2015 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
LWW/JNCQ JNCQ-D-14-00043 January 31, 2015 17:46
Effectiveness of Structured Hourly Nurse Rounding155
Systematic Reviews,and Nursing & Allied
Health Collection. The search was limited to
published literature between 2008 and 2014.
Key search words used were patient satisfac-
tion, patient fallprevention, pressure ulcer
prevention,and calllight.Additionalsearch
words of hospital and rounds were added to
the key word of patient satisfaction, and the
search word hospitalwas added to the key
words patientfall prevention and pressure
ulcer prevention. Peer-reviewed articles were
evaluated.Evaluation oftitles and abstracts
was performed with the following inclusion
criteria: inpatients in an acute care facility, an
intervention consisting ofstructured nurse
rounding, and written in the English language.
Studiesthat included every houror every
2 hours’structured nurse rounding and re-
ported outcomes were analyzed for strength
and quality ofevidence based on the Johns
Hopkins NursingEvidence-BasedPractice
Modeland Guidelines32 (see Supplemental
DigitalContent,Table,available at:http://
links.lww.com/JNCQ/A126).Evidencewas
classified into 1 of 5 (levels 1-5) hierarchical
levels dependent on the study design and then
a rating of quality (a,b, c) was assigned on
the basis of the overall study characteristics.
The process ofimplementation included
development of a structured approach to staff
education,historicaldata analysis,observa-
tions of staff workflow, evaluation of the cur-
rent state of hourly nurse rounding,and de-
velopment of guidelines for structured hourly
nurse rounding on the unit.First,a meeting
with the 8-member unit-based nursing gover-
nance council resulted in unanimous approval
for implementation of structured hourly nurse
rounding. A 20-minute education session that
included a review of evidence,working def-
inition of structured hourly nurse rounding,
review ofhistoricalperformance indicators,
and goals for improvement in the fiscalyear
were provided to every staff member on the
unit through group staff meetings or one-on-
one sessions.A fact sheet was presented to
the staff for their reference.
Observations and shadowing ofthe staff
on all3 shifts,on weekdays and weekends,
were performed for several weeks. These ob-
servations yielded information on workflow
patterns,usage and timelinessof response
to calllights,and length oftime needed to
complete a structured round with and with-
out need for toileting. Baseline data were col-
lected on compliance with performing hourly
nurse rounding, patient satisfaction, fall rates,
and HAPU rates.Key stakeholders included
the nurse manager,registered nurses,pa-
tient care assistants, and unit secretaries, who
were instrumental in developing the timeline
for implementation and were empowered to
make decisions throughout the project,and
the patients.Guidelines and principles out-
lining the accountabilities for performing the
nurse rounding were developed on the basis
of the published evidence, the observed time
needed for conducting nurse rounding,and
the workflow patterns of the staff.
Methods of evaluation
Baseline patient satisfaction scores on Hos-
pital ConsumerAssessmentof Healthcare
Providers and Systems (HCAHPS) surveys and
inpatientfall rates and HAPU rates through
the event report process were collected, an-
alyzed,and presented prior to implementa-
tion of structured nurse rounding. Structured
hourly nurse rounding compliance was also
determined during a 7-day period of time just
prior to implementation. Monthly data collec-
tion and outcome reporting were provided
on the performance indicators. Monitoring of
7-consecutive-day rounding compliance was
assessed each month during the project imple-
mentation period. Continuous monitoring of
compliance of structured hourly rounds was
not performed since manual collection of the
data was perceived by the staff as adding bur-
den to their other duties.Results were dis-
cussed monthly atstaffmeetings and were
graphically displayed in the staff lounge.
Analysis
Descriptive statistics were used to trend, or-
ganize, and describe the characteristics of the
data collected on hourly nurse rounding com-
pliance,inpatient fallrates,and HAPU rates.
Copyright © 2015 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
Effectiveness of Structured Hourly Nurse Rounding155
Systematic Reviews,and Nursing & Allied
Health Collection. The search was limited to
published literature between 2008 and 2014.
Key search words used were patient satisfac-
tion, patient fallprevention, pressure ulcer
prevention,and calllight.Additionalsearch
words of hospital and rounds were added to
the key word of patient satisfaction, and the
search word hospitalwas added to the key
words patientfall prevention and pressure
ulcer prevention. Peer-reviewed articles were
evaluated.Evaluation oftitles and abstracts
was performed with the following inclusion
criteria: inpatients in an acute care facility, an
intervention consisting ofstructured nurse
rounding, and written in the English language.
Studiesthat included every houror every
2 hours’structured nurse rounding and re-
ported outcomes were analyzed for strength
and quality ofevidence based on the Johns
Hopkins NursingEvidence-BasedPractice
Modeland Guidelines32 (see Supplemental
DigitalContent,Table,available at:http://
links.lww.com/JNCQ/A126).Evidencewas
classified into 1 of 5 (levels 1-5) hierarchical
levels dependent on the study design and then
a rating of quality (a,b, c) was assigned on
the basis of the overall study characteristics.
The process ofimplementation included
development of a structured approach to staff
education,historicaldata analysis,observa-
tions of staff workflow, evaluation of the cur-
rent state of hourly nurse rounding,and de-
velopment of guidelines for structured hourly
nurse rounding on the unit.First,a meeting
with the 8-member unit-based nursing gover-
nance council resulted in unanimous approval
for implementation of structured hourly nurse
rounding. A 20-minute education session that
included a review of evidence,working def-
inition of structured hourly nurse rounding,
review ofhistoricalperformance indicators,
and goals for improvement in the fiscalyear
were provided to every staff member on the
unit through group staff meetings or one-on-
one sessions.A fact sheet was presented to
the staff for their reference.
Observations and shadowing ofthe staff
on all3 shifts,on weekdays and weekends,
were performed for several weeks. These ob-
servations yielded information on workflow
patterns,usage and timelinessof response
to calllights,and length oftime needed to
complete a structured round with and with-
out need for toileting. Baseline data were col-
lected on compliance with performing hourly
nurse rounding, patient satisfaction, fall rates,
and HAPU rates.Key stakeholders included
the nurse manager,registered nurses,pa-
tient care assistants, and unit secretaries, who
were instrumental in developing the timeline
for implementation and were empowered to
make decisions throughout the project,and
the patients.Guidelines and principles out-
lining the accountabilities for performing the
nurse rounding were developed on the basis
of the published evidence, the observed time
needed for conducting nurse rounding,and
the workflow patterns of the staff.
Methods of evaluation
Baseline patient satisfaction scores on Hos-
pital ConsumerAssessmentof Healthcare
Providers and Systems (HCAHPS) surveys and
inpatientfall rates and HAPU rates through
the event report process were collected, an-
alyzed,and presented prior to implementa-
tion of structured nurse rounding. Structured
hourly nurse rounding compliance was also
determined during a 7-day period of time just
prior to implementation. Monthly data collec-
tion and outcome reporting were provided
on the performance indicators. Monitoring of
7-consecutive-day rounding compliance was
assessed each month during the project imple-
mentation period. Continuous monitoring of
compliance of structured hourly rounds was
not performed since manual collection of the
data was perceived by the staff as adding bur-
den to their other duties.Results were dis-
cussed monthly atstaffmeetings and were
graphically displayed in the staff lounge.
Analysis
Descriptive statistics were used to trend, or-
ganize, and describe the characteristics of the
data collected on hourly nurse rounding com-
pliance,inpatient fallrates,and HAPU rates.
Copyright © 2015 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.

LWW/JNCQ JNCQ-D-14-00043 January 31, 2015 17:46
156 JOURNAL OFNURSINGCAREQUALITY/APRIL–JUNE2015
A Cox-Stuart trend analysis was performed on
the historical inpatient fall data to effectively
illustrate that fall rates declined more consis-
tently postimplementation.Frequency distri-
bution analysis of the HCAHPS responses was
performed. Data were compared with appro-
priate benchmarks for patient satisfaction, in-
patient fall, and HAPU rates.
RESULTS
Outcomes
An overallgoalof more than 80% hourly
nurse rounding compliance was set after the
baseline assessmentand prior to the imple-
mentation ofhourly nurse rounding.Prein-
tervention baseline hourly nurse rounding
compliance was 48.4%.Additionalmonthly
compliancereviews were performedfor
7-consecutive-day periods revealing compli-
ance rates of 69.4%, 44.3%, and 59.2%. Overall
compliance was calculated by the total num-
ber ofrounds completed divided by the to-
tal number of possible events.Hourly nurse
rounding was considered to have been per-
formed when a staff member entered the pa-
tient’s room, evaluated the patient for PEEP,
and documented the activity on designated
flow sheets.
The projectunit discharged 582 eligible
patients during the project period. Eighty-one
HCAHPS surveys were returned.Percentage
of “always” declined slightly in the HCAHPS
composite domain score ofresponsiveness
of staff to 48.6% (n = 81) from patients
discharged postimplementation as compared
with a result of 49.3% (n = 35) preimplemen-
tation. However, the other domain responses
allincreased 6.1% to 30.9% postintervention
when compared with preintervention.The
Table displays the comparisons.
A patientfall was counted anytime a pa-
tient descended to the floor with or without
assistance from the hospitalstaff.A patient
fallrate was calculated by the totalnumber
of falls reported divided by the total number
of patient-days multiplied by 1000.A rate of
7.02 patient falls per 1000 patient-days was
noted in the prior year (November 2011 to
February 2012) and a rate of 3.18 resulted fol-
lowing implementation (November 15, 2012,
to February 14, 2013). This reflected a 57.7%
reduction from the previous year during sim-
ilar time periods.
Patientfall rateshad decreased on the
project unit prior to implementationof
structured hourly nurse rounding.A Cox-
Stuart trend analysis was performed on data
from the preceding12 months prior to
Table.Percentage of“Always,” “Yes,” and “9 or10” Reponses in each HCAHPS Domain
Composite Results Pre- and Postimplementation of Hourly Nurse Rounding
HCAHPS Domain
Pre %
(n = 35)
Post %
(n = 81)
1 y After Project
Implementation
(n = 472)
Overall satisfaction 48.6 72.3 72.2
Communication with nurses 70.5 76.6 78.8
Responsiveness of hospital staff 49.3 48.6 57.6
Communication with doctors 69.2 76.7 75.7
Hospital environment 49.1 61.8 59.8
Pain management 58.3 69.8 70.1
Communication about medicines 50.8 81.7 59.1
Discharge information 72.7 86.3 85.8
Likelihood to recommend 60.0 74.7 76.6
Abbreviation: HCAHPS, Hospital Consumer Assessment of Healthcare Providers and Systems.
Copyright © 2015 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
156 JOURNAL OFNURSINGCAREQUALITY/APRIL–JUNE2015
A Cox-Stuart trend analysis was performed on
the historical inpatient fall data to effectively
illustrate that fall rates declined more consis-
tently postimplementation.Frequency distri-
bution analysis of the HCAHPS responses was
performed. Data were compared with appro-
priate benchmarks for patient satisfaction, in-
patient fall, and HAPU rates.
RESULTS
Outcomes
An overallgoalof more than 80% hourly
nurse rounding compliance was set after the
baseline assessmentand prior to the imple-
mentation ofhourly nurse rounding.Prein-
tervention baseline hourly nurse rounding
compliance was 48.4%.Additionalmonthly
compliancereviews were performedfor
7-consecutive-day periods revealing compli-
ance rates of 69.4%, 44.3%, and 59.2%. Overall
compliance was calculated by the total num-
ber ofrounds completed divided by the to-
tal number of possible events.Hourly nurse
rounding was considered to have been per-
formed when a staff member entered the pa-
tient’s room, evaluated the patient for PEEP,
and documented the activity on designated
flow sheets.
The projectunit discharged 582 eligible
patients during the project period. Eighty-one
HCAHPS surveys were returned.Percentage
of “always” declined slightly in the HCAHPS
composite domain score ofresponsiveness
of staff to 48.6% (n = 81) from patients
discharged postimplementation as compared
with a result of 49.3% (n = 35) preimplemen-
tation. However, the other domain responses
allincreased 6.1% to 30.9% postintervention
when compared with preintervention.The
Table displays the comparisons.
A patientfall was counted anytime a pa-
tient descended to the floor with or without
assistance from the hospitalstaff.A patient
fallrate was calculated by the totalnumber
of falls reported divided by the total number
of patient-days multiplied by 1000.A rate of
7.02 patient falls per 1000 patient-days was
noted in the prior year (November 2011 to
February 2012) and a rate of 3.18 resulted fol-
lowing implementation (November 15, 2012,
to February 14, 2013). This reflected a 57.7%
reduction from the previous year during sim-
ilar time periods.
Patientfall rateshad decreased on the
project unit prior to implementationof
structured hourly nurse rounding.A Cox-
Stuart trend analysis was performed on data
from the preceding12 months prior to
Table.Percentage of“Always,” “Yes,” and “9 or10” Reponses in each HCAHPS Domain
Composite Results Pre- and Postimplementation of Hourly Nurse Rounding
HCAHPS Domain
Pre %
(n = 35)
Post %
(n = 81)
1 y After Project
Implementation
(n = 472)
Overall satisfaction 48.6 72.3 72.2
Communication with nurses 70.5 76.6 78.8
Responsiveness of hospital staff 49.3 48.6 57.6
Communication with doctors 69.2 76.7 75.7
Hospital environment 49.1 61.8 59.8
Pain management 58.3 69.8 70.1
Communication about medicines 50.8 81.7 59.1
Discharge information 72.7 86.3 85.8
Likelihood to recommend 60.0 74.7 76.6
Abbreviation: HCAHPS, Hospital Consumer Assessment of Healthcare Providers and Systems.
Copyright © 2015 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
LWW/JNCQ JNCQ-D-14-00043 January 31, 2015 17:46
Effectiveness of Structured Hourly Nurse Rounding157
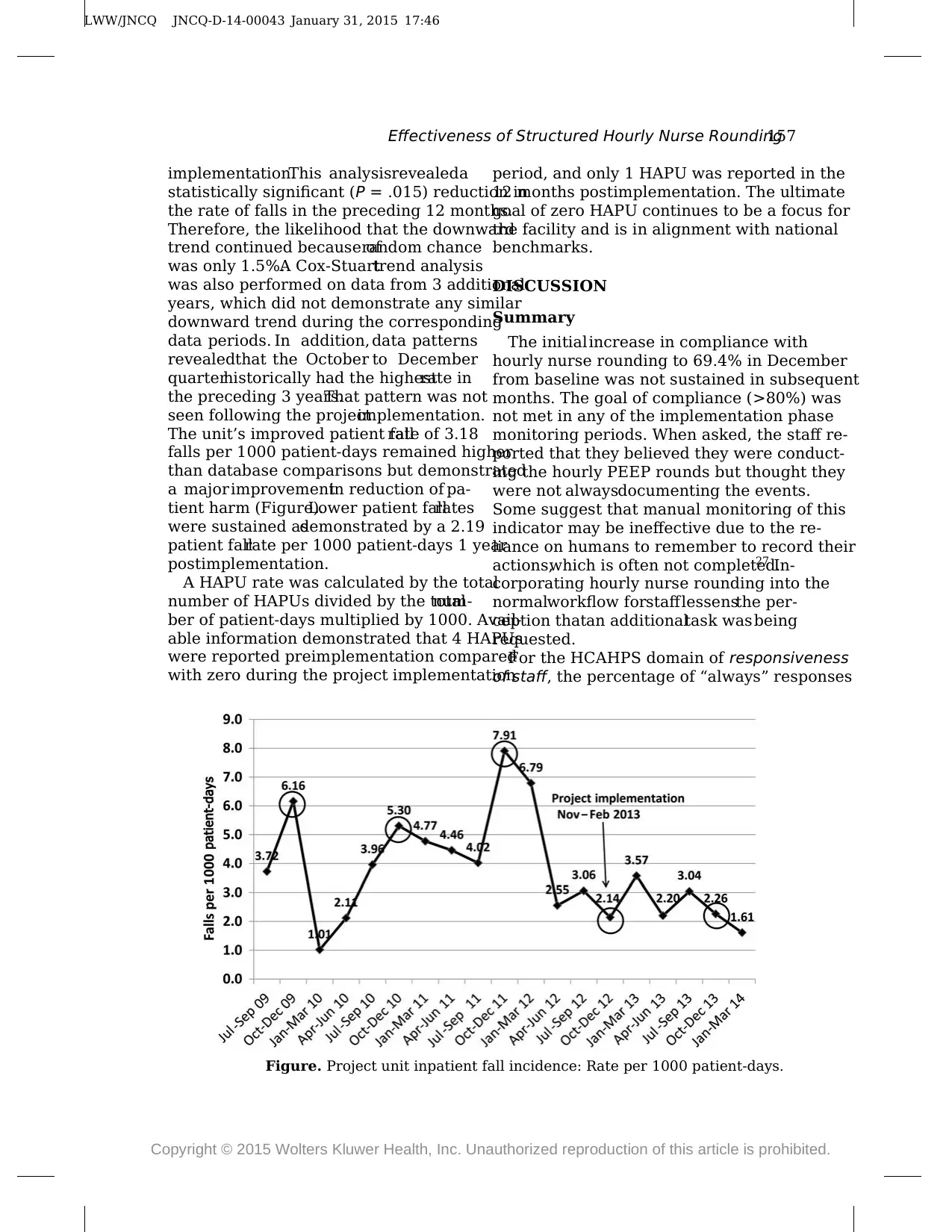
implementation.This analysisrevealeda
statistically significant (P = .015) reduction in
the rate of falls in the preceding 12 months.
Therefore, the likelihood that the downward
trend continued because ofrandom chance
was only 1.5%.A Cox-Stuarttrend analysis
was also performed on data from 3 additional
years, which did not demonstrate any similar
downward trend during the corresponding
data periods. In addition, data patterns
revealedthat the October to December
quarterhistorically had the highestrate in
the preceding 3 years.That pattern was not
seen following the projectimplementation.
The unit’s improved patient fallrate of 3.18
falls per 1000 patient-days remained higher
than database comparisons but demonstrated
a major improvementin reduction of pa-
tient harm (Figure).Lower patient fallrates
were sustained asdemonstrated by a 2.19
patient fallrate per 1000 patient-days 1 year
postimplementation.
A HAPU rate was calculated by the total
number of HAPUs divided by the totalnum-
ber of patient-days multiplied by 1000. Avail-
able information demonstrated that 4 HAPUs
were reported preimplementation compared
with zero during the project implementation
period, and only 1 HAPU was reported in the
12 months postimplementation. The ultimate
goal of zero HAPU continues to be a focus for
the facility and is in alignment with national
benchmarks.
DISCUSSION
Summary
The initialincrease in compliance with
hourly nurse rounding to 69.4% in December
from baseline was not sustained in subsequent
months. The goal of compliance (>80%) was
not met in any of the implementation phase
monitoring periods. When asked, the staff re-
ported that they believed they were conduct-
ing the hourly PEEP rounds but thought they
were not alwaysdocumenting the events.
Some suggest that manual monitoring of this
indicator may be ineffective due to the re-
liance on humans to remember to record their
actions,which is often not completed.27 In-
corporating hourly nurse rounding into the
normalworkflow forstafflessensthe per-
ception thatan additionaltask wasbeing
requested.
For the HCAHPS domain of responsiveness
of staff, the percentage of “always” responses
Figure. Project unit inpatient fall incidence: Rate per 1000 patient-days.
Copyright © 2015 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
Effectiveness of Structured Hourly Nurse Rounding157
implementation.This analysisrevealeda
statistically significant (P = .015) reduction in
the rate of falls in the preceding 12 months.
Therefore, the likelihood that the downward
trend continued because ofrandom chance
was only 1.5%.A Cox-Stuarttrend analysis
was also performed on data from 3 additional
years, which did not demonstrate any similar
downward trend during the corresponding
data periods. In addition, data patterns
revealedthat the October to December
quarterhistorically had the highestrate in
the preceding 3 years.That pattern was not
seen following the projectimplementation.
The unit’s improved patient fallrate of 3.18
falls per 1000 patient-days remained higher
than database comparisons but demonstrated
a major improvementin reduction of pa-
tient harm (Figure).Lower patient fallrates
were sustained asdemonstrated by a 2.19
patient fallrate per 1000 patient-days 1 year
postimplementation.
A HAPU rate was calculated by the total
number of HAPUs divided by the totalnum-
ber of patient-days multiplied by 1000. Avail-
able information demonstrated that 4 HAPUs
were reported preimplementation compared
with zero during the project implementation
period, and only 1 HAPU was reported in the
12 months postimplementation. The ultimate
goal of zero HAPU continues to be a focus for
the facility and is in alignment with national
benchmarks.
DISCUSSION
Summary
The initialincrease in compliance with
hourly nurse rounding to 69.4% in December
from baseline was not sustained in subsequent
months. The goal of compliance (>80%) was
not met in any of the implementation phase
monitoring periods. When asked, the staff re-
ported that they believed they were conduct-
ing the hourly PEEP rounds but thought they
were not alwaysdocumenting the events.
Some suggest that manual monitoring of this
indicator may be ineffective due to the re-
liance on humans to remember to record their
actions,which is often not completed.27 In-
corporating hourly nurse rounding into the
normalworkflow forstafflessensthe per-
ception thatan additionaltask wasbeing
requested.
For the HCAHPS domain of responsiveness
of staff, the percentage of “always” responses
Figure. Project unit inpatient fall incidence: Rate per 1000 patient-days.
Copyright © 2015 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.

LWW/JNCQ JNCQ-D-14-00043 January 31, 2015 17:46
158 JOURNAL OFNURSINGCAREQUALITY/APRIL–JUNE2015
was the only domain in which the score
was lower postimplementation than preim-
plementation. The other domain percentages
all increased.All but one HCAHPS domain
demonstrated increases in the percentage of
“always, “yes,” and “9 and 10” responses dur-
ing the project period, which was consistent
with the evidence.
The rate of patient falls on the project unit
decreased prior to implementation ofstruc-
tured hourly nurse rounding possibly due to
a reemphasis on the Fall Prevention Program
in the nursing department. When comparing
falls rates from similartime periods,it ap-
peared there was a decline in fallrates,al-
though the trend began to decline prior to
project implementation. Historically, fall rates
had been highest in the October to December
time period. That usual pattern did not recur
during the project implementation (Figure).
A reduction of 11 fall incidences between the
pre- and postimplementation period reflected
a cost avoidance of $46 563 ($4322 × 11) for
the project implementation period.33
The reduction in the rate ofpatient falls,
when comparinganalogousyearly time
periods,was similarto reportsfrom other
projects and studiesdocumentedin the
literature. While the decline in fall rates dur-
ing implementation wasmodestcompared
with preceding quarters,it was clinically
significantfor the winter quarter especially
considering historic dataand case-mix in-
dices.Both Bourgaultet al13 and Krepper
et al16 noted no effectin patientfalls with
implementation of rounding following preex-
isting robust fall prevention programs and low
rates of patient falls prior to implementation.
HAPU rates per 1000 patient-days had also
declined in the 6 months prior to implemen-
tation on the project unit. However, a reduc-
tion of 4 HAPUs comparing pre-and postim-
plementation resulted in a cost avoidance of
$172 720 ($43 180 × 4).33 This reduction in
HAPU rate was similar to results reported by
Ellis,14 Sherrod et al,18 and the Studer Group.2
Limitations
This project was implementedon 1
medical-surgical unit in 1 hospital. In addition,
3 months is a short period of time to evaluate a
change in nursing workflow or cultural adop-
tion of this intervention for sustainability.
CONCLUSIONS
Change management strategies were used
to influence the culture of nursing practice, so
changes were not be perceived as simply ad-
ditional tasks to complete. Recommendations
for project sustainability include incorporat-
ing unit-based rounding champions to con-
tinue to stimulate enthusiasm and prioritize
discussions so thatthe initialimprovement
changes do not drift. Periodic monitoring and
public display of the data stimulate continual
focus on the results of this intervention.
Evidence indicates thatstructured hourly
nurse rounds are safe,efficient,and useful
in today’s practice.Performing hourly nurse
rounding may be cost-effective as an interven-
tion because it promotes cost avoidance by
reducing injuries related to patient falls and
pressure ulcer formation, both of which may
extend hospitallength ofstays.The corpus
of evidence suggested that structured nurse
rounding demonstrated favorable trendsin
improving patientsatisfaction and reducing
patient falls, HAPUs, and call light usage. This
project demonstrated overall improvement in
patient satisfaction indicators and decreased
patient harm through lower patient fall
and HAPU rates. Reduced patient harm
contributedmore than $200 000in cost
avoidance ofcare that is not reimbursed to
organizations.
REFERENCES
1. MeadeCM, BursellAL, Ketelsen L. Effects of
nursingrounds on patients’ call light use, sat-
isfaction,and safety. Am J Nurs. 2006;106(9):
58-70.
Copyright © 2015 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
158 JOURNAL OFNURSINGCAREQUALITY/APRIL–JUNE2015
was the only domain in which the score
was lower postimplementation than preim-
plementation. The other domain percentages
all increased.All but one HCAHPS domain
demonstrated increases in the percentage of
“always, “yes,” and “9 and 10” responses dur-
ing the project period, which was consistent
with the evidence.
The rate of patient falls on the project unit
decreased prior to implementation ofstruc-
tured hourly nurse rounding possibly due to
a reemphasis on the Fall Prevention Program
in the nursing department. When comparing
falls rates from similartime periods,it ap-
peared there was a decline in fallrates,al-
though the trend began to decline prior to
project implementation. Historically, fall rates
had been highest in the October to December
time period. That usual pattern did not recur
during the project implementation (Figure).
A reduction of 11 fall incidences between the
pre- and postimplementation period reflected
a cost avoidance of $46 563 ($4322 × 11) for
the project implementation period.33
The reduction in the rate ofpatient falls,
when comparinganalogousyearly time
periods,was similarto reportsfrom other
projects and studiesdocumentedin the
literature. While the decline in fall rates dur-
ing implementation wasmodestcompared
with preceding quarters,it was clinically
significantfor the winter quarter especially
considering historic dataand case-mix in-
dices.Both Bourgaultet al13 and Krepper
et al16 noted no effectin patientfalls with
implementation of rounding following preex-
isting robust fall prevention programs and low
rates of patient falls prior to implementation.
HAPU rates per 1000 patient-days had also
declined in the 6 months prior to implemen-
tation on the project unit. However, a reduc-
tion of 4 HAPUs comparing pre-and postim-
plementation resulted in a cost avoidance of
$172 720 ($43 180 × 4).33 This reduction in
HAPU rate was similar to results reported by
Ellis,14 Sherrod et al,18 and the Studer Group.2
Limitations
This project was implementedon 1
medical-surgical unit in 1 hospital. In addition,
3 months is a short period of time to evaluate a
change in nursing workflow or cultural adop-
tion of this intervention for sustainability.
CONCLUSIONS
Change management strategies were used
to influence the culture of nursing practice, so
changes were not be perceived as simply ad-
ditional tasks to complete. Recommendations
for project sustainability include incorporat-
ing unit-based rounding champions to con-
tinue to stimulate enthusiasm and prioritize
discussions so thatthe initialimprovement
changes do not drift. Periodic monitoring and
public display of the data stimulate continual
focus on the results of this intervention.
Evidence indicates thatstructured hourly
nurse rounds are safe,efficient,and useful
in today’s practice.Performing hourly nurse
rounding may be cost-effective as an interven-
tion because it promotes cost avoidance by
reducing injuries related to patient falls and
pressure ulcer formation, both of which may
extend hospitallength ofstays.The corpus
of evidence suggested that structured nurse
rounding demonstrated favorable trendsin
improving patientsatisfaction and reducing
patient falls, HAPUs, and call light usage. This
project demonstrated overall improvement in
patient satisfaction indicators and decreased
patient harm through lower patient fall
and HAPU rates. Reduced patient harm
contributedmore than $200 000in cost
avoidance ofcare that is not reimbursed to
organizations.
REFERENCES
1. MeadeCM, BursellAL, Ketelsen L. Effects of
nursingrounds on patients’ call light use, sat-
isfaction,and safety. Am J Nurs. 2006;106(9):
58-70.
Copyright © 2015 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
LWW/JNCQ JNCQ-D-14-00043 January 31, 2015 17:46
Effectiveness of Structured Hourly Nurse Rounding159
2. StuderGroup.Hourly rounding supplement.Best
Practice ed. http://www.studergroup.com/flash
hourlyrounding.Published 2007.Accessed Novem-
ber 15, 2012.
3. Culley T.Reduce calllightfrequency with hourly
rounds. Nurs Manag. 2008;39(3):50-52.
4. Murphy TH,Labonte P,Houser L.Falls prevention
for elders in acute care.An evidence-based nursing
practice initiative. Crit Care Nurs Q.2008;31(1):33-
39.
5. SobaskiT, Abraham M,FillmoreR, McFallDE,
Davidhizar R. The effect of routine rounding by nurs-
ing staff on patient satisfaction on a cardiac telemetry
unit. Health Care Manag. 2008;27(4):332-337.
6. Tea C, Ellison M, Feghali F. Proactive patient rounding
to increase customer service and satisfaction on an
orthopaedic unit. Orthop Nurs. 2008;27(4):233-240.
7. Weisgram B, Raymond S. Using evidence-based nurs-
ing rounds to improve patientoutcomes.Medsurg
Nurs. 2008;17(6):429-430.
8. Stefancyk AL.Safe and reliable care.Am J Nurs.
2009;109(7):70-71.
9. Ford BM. Hourly rounding:a strategyto im-
prove patientsatisfaction scores.Medsurg Nurs.
2010;19(3):188-191.
10. Berg K,Sailors C,Reimer R,O’Brien Y,Ward-Smith
P. Hourly rounding with a purpose. Iowa Nurs Rep.
2011;3:12-14.
11. Blakley D, Kroth M, Gregson J. The impact of nurse
rounding on patient satisfaction in a medical-surgical
hospital unit. Medsurg Nurs. 2011;20(6):327-332.
12. Bonuel N, Manjos A, Lockett L, Gray-Becknell T. Best
practice fall prevention strategies. Crit Care Nurs Q.
2011;34(2):154-158.
13. BourgaultAM, King MM,Hart P, CampbellMK,
Swartz S,Lou M.Does regular rounding by nursing
associates boostpatientsatisfaction?Nurs Manag.
2008;39(11):18-24.
14. Ellis E. Hourly nurse rounds help to reduce falls, pres-
sure ulcers, and call light use, and contribute to rise
in patient satisfaction. http://www.innovations.ahrq
.gov/content.aspx?id=3204.Published 2012. Ac-
cessed November 24, 2012.
15. Kessler B,Claude-Gutekunst M,Donchez AM,Dries
RF, Snyder MM. The merry-go-round of patient round-
ing: assure your patients get the brass ring. Medsurg
Nurs. 2012;21(4):240-245.
16. Krepper R,Vallejo B,Smith C,et al. Evaluation of
a standardized hourly rounding process (SHaRP).J
Healthc Q. 2014;36(2):62-69.
17. Olrich T, Kalman M, Nigolian C. Hourly rounding: a
replication study. Medsurg Nurs. 2012;21(1):23-26.
18. Sherrod BC, Brown R, Vroom J, Sullivan DT. Round
with purpose. Nurs Manag. 2012;43(1):33-38.
19. Tucker SJ,Bieber PL,Attlesey-Pries JM,Olson ME,
Dierkhising RA.Outcomes and challenges in imple-
menting hourly rounds to reduce falls in orthope-
dic units.Worldviews Evid Based Nurs.2012;9(1):
18-29.
20. Hutchings M, Ward P, Bloodworth K. “Caring around
the clock”: a new approach to intentional rounding.
Nurs Manag. 2013;20(5):24-30.
21. Dix G, Phillips J, Braide M. Engaging staff with inten-
tional rounding. Nurs Times. 2012;108(3):14-16.
22. Braide M.The effect of intentionalrounding on es-
sential care. Nurs Times. 2013;109(20):16-18.
23. Gardner G, Woollett K, Daly N, Richardson B. Measur-
ing the effect of patient comfort rounds on practice
environment and patient satisfaction:a pilot study.
Int J Nurs Pract. 2009;15(4):287-293.
24. Woodard JL.Effects of rounding on patient satisfac-
tion and patient safety on a medical-surgical unit. Clin
Nurs Spec. 2009;23:201-206.
25. Petras DM,Dudjak LA,Bender CM.Piloting patient
rounding as a quality improvementinitiative.Nurs
Manag. 2013;44(7):19-23.
26. Shattell M, Hogen B, Thomas S. “It’s the people that
make the environment good or bad.” The patient’s
experience of the acute care hospitalenvironment.
AACN Clin Issues. 2005;16(2):159-169.
27. Wagner D, Bear M. Patient satisfaction with nursing
care: a concept analysis within a nursing framework.
J Adv Nurs. 2008;65(3):692-701.
28. OtaniK, Herrmann PA,Kurz RS.Improving patient
evaluation of hospital care and increasing their inten-
tion to recommend:are they the same or different
constructs? Health Serv Manag Res.2010;23(2):60-
65.
29. Kennedy B,Craig JB,WetselM, Reimels E,Wright
J. Three nursing interventions’impacton HCAHPS
scores. J Nurs Care Qual. 2013;28(4):327-334.
30. Manary MP, Boulding W, Staelin R, Glickman SW. The
patientexperience and health outcomes.N Engl J
Med. 2013;368(3):201-203.
31. Kitson AL,Rycroft-Malone J,Harvey G,McCormack
B, Seers K, Titchen A. Evaluating the successful imple-
mentation of evidence into practice using the PARiHS
framework: theoretical and practical challenges [de-
bate].ImplementSci. 2008;3:1.doi:10.1186/1748-
5908-3-1.
32. DearholtSL, Dang D. Johns Hopkins Nursing
Evidence-Based Practice: Model and Guidelines. 2nd
ed. Indianapolis,IN:Sigma Theta Tau International;
2012.
33. Schifalacqua MM,Mamula J,Mason AR.Return on
investmentimperative.The costof care calculator
for an evidence-based practice program.Nurs Adm
Q. 2011;35(1):15-20.
Copyright © 2015 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
Effectiveness of Structured Hourly Nurse Rounding159
2. StuderGroup.Hourly rounding supplement.Best
Practice ed. http://www.studergroup.com/flash
hourlyrounding.Published 2007.Accessed Novem-
ber 15, 2012.
3. Culley T.Reduce calllightfrequency with hourly
rounds. Nurs Manag. 2008;39(3):50-52.
4. Murphy TH,Labonte P,Houser L.Falls prevention
for elders in acute care.An evidence-based nursing
practice initiative. Crit Care Nurs Q.2008;31(1):33-
39.
5. SobaskiT, Abraham M,FillmoreR, McFallDE,
Davidhizar R. The effect of routine rounding by nurs-
ing staff on patient satisfaction on a cardiac telemetry
unit. Health Care Manag. 2008;27(4):332-337.
6. Tea C, Ellison M, Feghali F. Proactive patient rounding
to increase customer service and satisfaction on an
orthopaedic unit. Orthop Nurs. 2008;27(4):233-240.
7. Weisgram B, Raymond S. Using evidence-based nurs-
ing rounds to improve patientoutcomes.Medsurg
Nurs. 2008;17(6):429-430.
8. Stefancyk AL.Safe and reliable care.Am J Nurs.
2009;109(7):70-71.
9. Ford BM. Hourly rounding:a strategyto im-
prove patientsatisfaction scores.Medsurg Nurs.
2010;19(3):188-191.
10. Berg K,Sailors C,Reimer R,O’Brien Y,Ward-Smith
P. Hourly rounding with a purpose. Iowa Nurs Rep.
2011;3:12-14.
11. Blakley D, Kroth M, Gregson J. The impact of nurse
rounding on patient satisfaction in a medical-surgical
hospital unit. Medsurg Nurs. 2011;20(6):327-332.
12. Bonuel N, Manjos A, Lockett L, Gray-Becknell T. Best
practice fall prevention strategies. Crit Care Nurs Q.
2011;34(2):154-158.
13. BourgaultAM, King MM,Hart P, CampbellMK,
Swartz S,Lou M.Does regular rounding by nursing
associates boostpatientsatisfaction?Nurs Manag.
2008;39(11):18-24.
14. Ellis E. Hourly nurse rounds help to reduce falls, pres-
sure ulcers, and call light use, and contribute to rise
in patient satisfaction. http://www.innovations.ahrq
.gov/content.aspx?id=3204.Published 2012. Ac-
cessed November 24, 2012.
15. Kessler B,Claude-Gutekunst M,Donchez AM,Dries
RF, Snyder MM. The merry-go-round of patient round-
ing: assure your patients get the brass ring. Medsurg
Nurs. 2012;21(4):240-245.
16. Krepper R,Vallejo B,Smith C,et al. Evaluation of
a standardized hourly rounding process (SHaRP).J
Healthc Q. 2014;36(2):62-69.
17. Olrich T, Kalman M, Nigolian C. Hourly rounding: a
replication study. Medsurg Nurs. 2012;21(1):23-26.
18. Sherrod BC, Brown R, Vroom J, Sullivan DT. Round
with purpose. Nurs Manag. 2012;43(1):33-38.
19. Tucker SJ,Bieber PL,Attlesey-Pries JM,Olson ME,
Dierkhising RA.Outcomes and challenges in imple-
menting hourly rounds to reduce falls in orthope-
dic units.Worldviews Evid Based Nurs.2012;9(1):
18-29.
20. Hutchings M, Ward P, Bloodworth K. “Caring around
the clock”: a new approach to intentional rounding.
Nurs Manag. 2013;20(5):24-30.
21. Dix G, Phillips J, Braide M. Engaging staff with inten-
tional rounding. Nurs Times. 2012;108(3):14-16.
22. Braide M.The effect of intentionalrounding on es-
sential care. Nurs Times. 2013;109(20):16-18.
23. Gardner G, Woollett K, Daly N, Richardson B. Measur-
ing the effect of patient comfort rounds on practice
environment and patient satisfaction:a pilot study.
Int J Nurs Pract. 2009;15(4):287-293.
24. Woodard JL.Effects of rounding on patient satisfac-
tion and patient safety on a medical-surgical unit. Clin
Nurs Spec. 2009;23:201-206.
25. Petras DM,Dudjak LA,Bender CM.Piloting patient
rounding as a quality improvementinitiative.Nurs
Manag. 2013;44(7):19-23.
26. Shattell M, Hogen B, Thomas S. “It’s the people that
make the environment good or bad.” The patient’s
experience of the acute care hospitalenvironment.
AACN Clin Issues. 2005;16(2):159-169.
27. Wagner D, Bear M. Patient satisfaction with nursing
care: a concept analysis within a nursing framework.
J Adv Nurs. 2008;65(3):692-701.
28. OtaniK, Herrmann PA,Kurz RS.Improving patient
evaluation of hospital care and increasing their inten-
tion to recommend:are they the same or different
constructs? Health Serv Manag Res.2010;23(2):60-
65.
29. Kennedy B,Craig JB,WetselM, Reimels E,Wright
J. Three nursing interventions’impacton HCAHPS
scores. J Nurs Care Qual. 2013;28(4):327-334.
30. Manary MP, Boulding W, Staelin R, Glickman SW. The
patientexperience and health outcomes.N Engl J
Med. 2013;368(3):201-203.
31. Kitson AL,Rycroft-Malone J,Harvey G,McCormack
B, Seers K, Titchen A. Evaluating the successful imple-
mentation of evidence into practice using the PARiHS
framework: theoretical and practical challenges [de-
bate].ImplementSci. 2008;3:1.doi:10.1186/1748-
5908-3-1.
32. DearholtSL, Dang D. Johns Hopkins Nursing
Evidence-Based Practice: Model and Guidelines. 2nd
ed. Indianapolis,IN:Sigma Theta Tau International;
2012.
33. Schifalacqua MM,Mamula J,Mason AR.Return on
investmentimperative.The costof care calculator
for an evidence-based practice program.Nurs Adm
Q. 2011;35(1):15-20.
Copyright © 2015 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
1 out of 7
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.


