Electronic Health Records: Improving Patient Safety and Delivery
VerifiedAdded on 2023/04/23
|14
|879
|154
Report
AI Summary
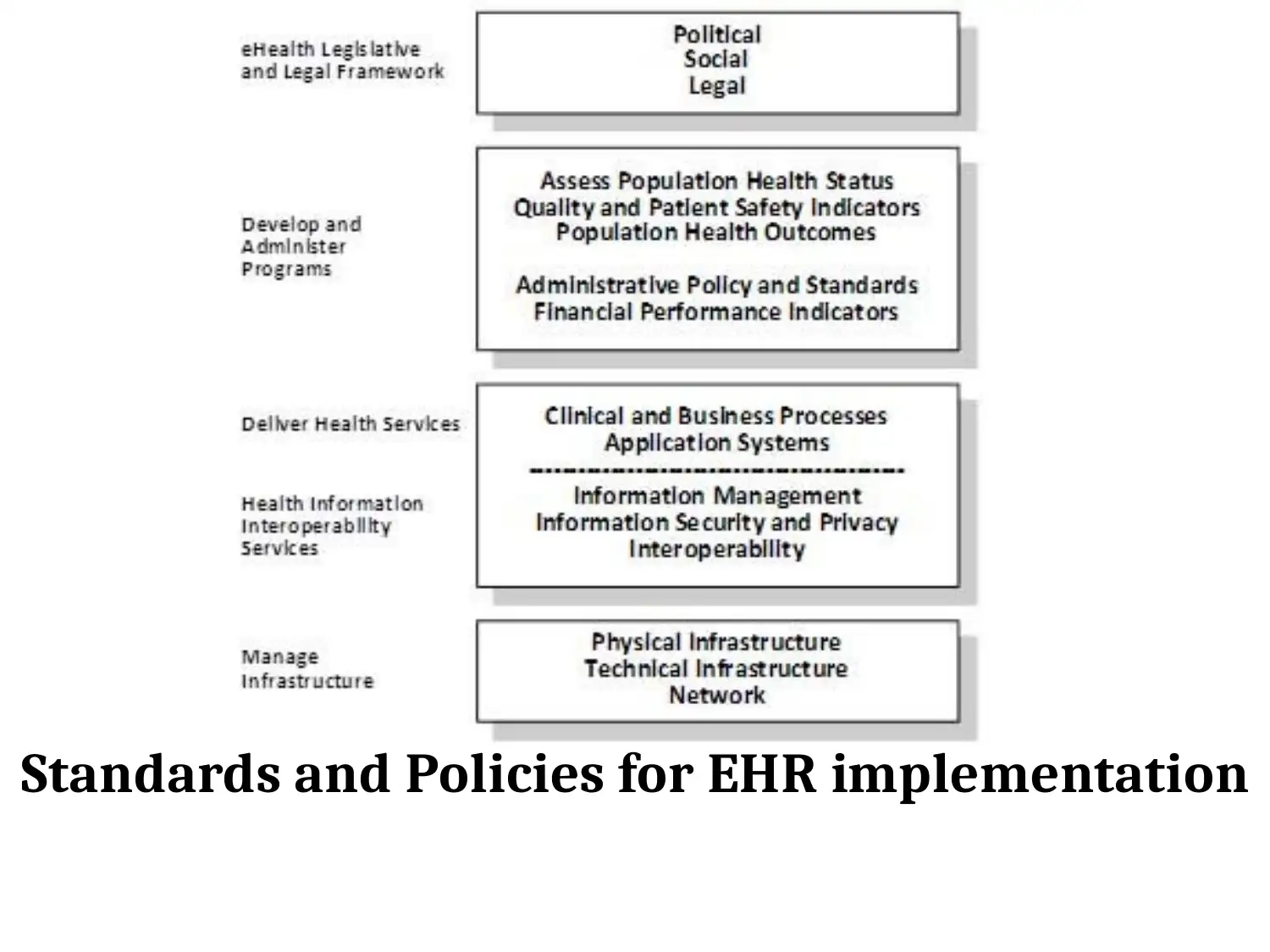
This report discusses the utilization of Electronic Health Records (EHR) as a strategy for improving patient safety and healthcare delivery, focusing on the context of Saudi Arabia's National eHealth Program. EHRs are presented as key tools for providing accurate patient information, reducing information accessibility time, enhancing information security, and enabling accurate diagnoses, ultimately increasing healthcare effectiveness through enhanced departmental connectedness, improved information relaying, cloud service accessibility, and live monitoring of emergency events. While EHRs promise to reduce medical errors, improve patient flow, and enable better delegation and response to clinical events, the report acknowledges existing limitations in safety, usability, and interoperability. Key recommendations include increased staff training, improved communication, and feedback mechanisms to combat these limitations, emphasizing the need for collaborative discussions, reviews with health professionals, educational workshops, and the integration of clinical and IT departments to ensure successful EHR implementation guided by national standards and policies.
1 out of 14



![[object Object]](/_next/static/media/star-bottom.7253800d.svg)