Residential Care EHR Adoption: An Analysis of NCHS Data Brief 128
VerifiedAdded on 2023/06/13
|8
|3339
|84
Report
AI Summary
This report, based on the 2010 National Survey of Residential Care Facilities (NSRCF) data from the National Center for Health Statistics (NCHS), examines the adoption and usage of electronic health records (EHRs) in residential care communities across the United States. The study reveals that only 17% of residential care communities used EHRs in 2010, with adoption rates varying based on facility characteristics such as size, ownership, chain affiliation, and location. Facilities using EHRs were more likely to be larger, not-for-profit, chain-affiliated, colocated with other care settings, and located in non-metropolitan areas. The most common types of resident health information tracked electronically included medical provider information, resident demographics, individual service plans, and medication lists. Furthermore, 40% of facilities with EHRs supported electronic health information exchange with other providers, particularly pharmacies. The findings provide baseline data relevant to discussions on improving care coordination, reducing rehospitalizations, and managing chronic conditions in residential care settings.
NCHS Data Brief ■ No. 128 ■ September 2013
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES
Centers for Disease Control and Prevention
National Center for Health Statistics
Use of Electronic Health Records in
Residential Care Communities
Christine Caffrey, Ph.D., and Eunice Park-Lee, Ph.D.
Key findings
• In 2010, only 17% of
residential care communities
in the United States used
electronic health records.
• Residential care
communities that used
electronic health records
were more likely to be
larger, not-for-profit, chain-
affiliated, colocated with
another care setting, and in a
nonmetropolitan statistical area.
• The types of information
most commonly tracked
electronically by residential
care communities that used
electronic health records were
medical provider information,
resident demographics,
individual service plans, and
lists of residents’ medications
and active medication allergies.
• Four in 10 residential
care communities that used
electronic health records also
had support for electronic
exchange of health information
with service providers; nearly
25% could exchange with
pharmacies, and 17% could
exchange with physicians.
The ability to record and exchange health information electronically is
believed to improve the quality and efficiency of health care (1–4). It also has
the potential to increase coordination of care across a continuum of providers,
decrease duplication of testing (5), and allow providers timely access to
necessary health information. Although research has been done in other health
care settings (6–9), little has been focused on residential care communities’
use of electronic health records and their support for electronic exchange of
resident health information (10). This report provides baseline findings using
data from the 2010 National Survey of Residential Care Facilities (NSRCF).
Keywords: long-term care • health information technology • National Survey
of Residential Care Facilities
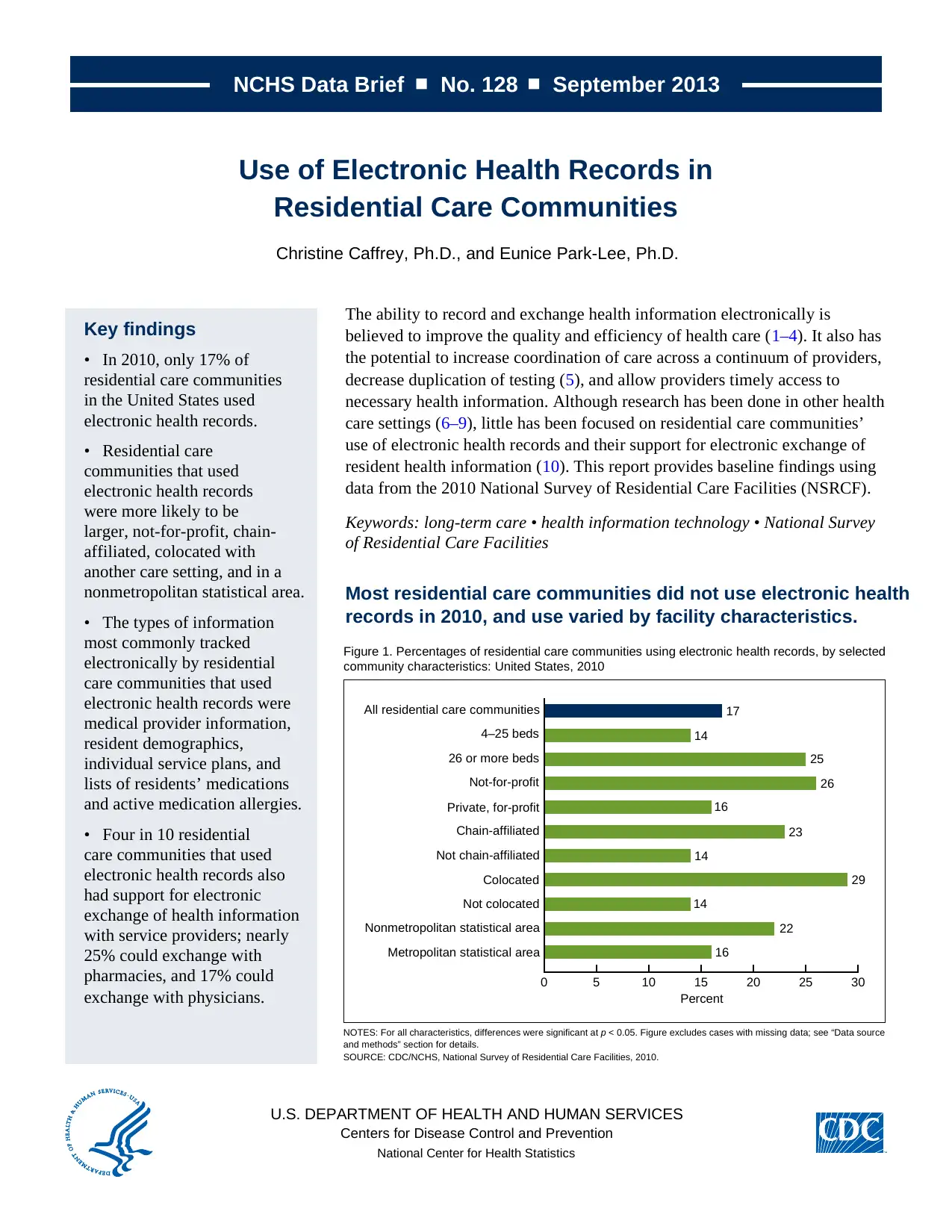
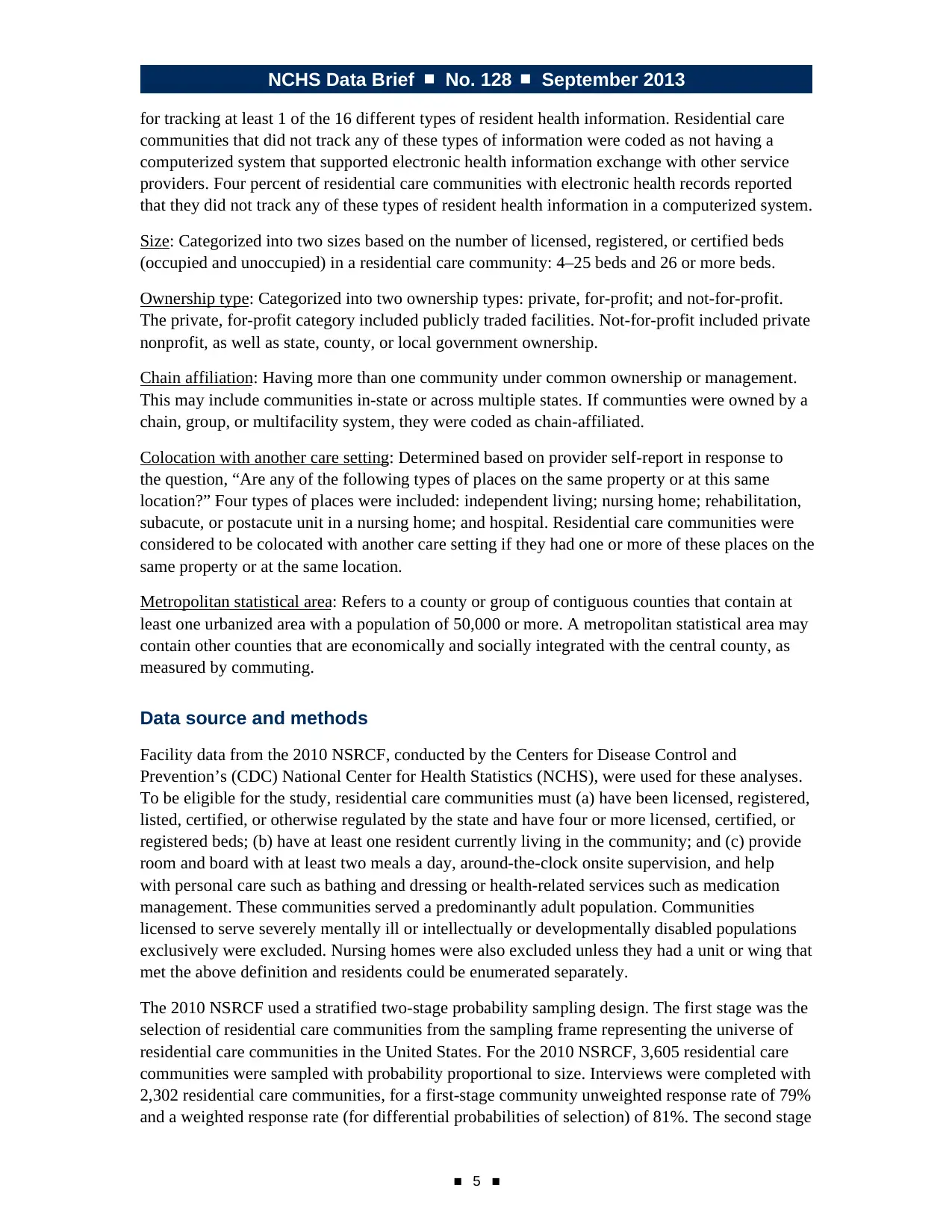
Most residential care communities did not use electronic health
records in 2010, and use varied by facility characteristics.
NOTES: For all characteristics, differences were significant at p < 0.05. Figure excludes cases with missing data; see “Data source
and methods” section for details.
SOURCE: CDC/NCHS, National Survey of Residential Care Facilities, 2010.
Figure 1. Percentages of residential care communities using electronic health records, by selected
community characteristics: United States, 2010
0 5 10 15
Percent
20 25 30
All residential care communities 17
4–25 beds 14
26 or more beds 25
Not-for-profit 26
Private, for-profit 16
Chain-affiliated 23
Not chain-affiliated 14
Colocated 29
Not colocated 14
Nonmetropolitan statistical area 22
Metropolitan statistical area 16
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES
Centers for Disease Control and Prevention
National Center for Health Statistics
Use of Electronic Health Records in
Residential Care Communities
Christine Caffrey, Ph.D., and Eunice Park-Lee, Ph.D.
Key findings
• In 2010, only 17% of
residential care communities
in the United States used
electronic health records.
• Residential care
communities that used
electronic health records
were more likely to be
larger, not-for-profit, chain-
affiliated, colocated with
another care setting, and in a
nonmetropolitan statistical area.
• The types of information
most commonly tracked
electronically by residential
care communities that used
electronic health records were
medical provider information,
resident demographics,
individual service plans, and
lists of residents’ medications
and active medication allergies.
• Four in 10 residential
care communities that used
electronic health records also
had support for electronic
exchange of health information
with service providers; nearly
25% could exchange with
pharmacies, and 17% could
exchange with physicians.
The ability to record and exchange health information electronically is
believed to improve the quality and efficiency of health care (1–4). It also has
the potential to increase coordination of care across a continuum of providers,
decrease duplication of testing (5), and allow providers timely access to
necessary health information. Although research has been done in other health
care settings (6–9), little has been focused on residential care communities’
use of electronic health records and their support for electronic exchange of
resident health information (10). This report provides baseline findings using
data from the 2010 National Survey of Residential Care Facilities (NSRCF).
Keywords: long-term care • health information technology • National Survey
of Residential Care Facilities
Most residential care communities did not use electronic health
records in 2010, and use varied by facility characteristics.
NOTES: For all characteristics, differences were significant at p < 0.05. Figure excludes cases with missing data; see “Data source
and methods” section for details.
SOURCE: CDC/NCHS, National Survey of Residential Care Facilities, 2010.
Figure 1. Percentages of residential care communities using electronic health records, by selected
community characteristics: United States, 2010
0 5 10 15
Percent
20 25 30
All residential care communities 17
4–25 beds 14
26 or more beds 25
Not-for-profit 26
Private, for-profit 16
Chain-affiliated 23
Not chain-affiliated 14
Colocated 29
Not colocated 14
Nonmetropolitan statistical area 22
Metropolitan statistical area 16
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NCHS Data Brief ■ No. 128 ■ September 2013
■ 2 ■
• In 2010, only 17% of residential care communities used electronic health records (Figure 1).
• One-quarter of larger residential care communities (those with 26 or more beds) used
electronic health records, compared with 14% of smaller communities (4–25 beds).
• Not-for-profit (26%) and chain-affiliated (23%) residential care communities were
more likely to use electronic health records than for-profit (16%) and nonchain (14%)
communities.
• Residential care communities colocated with another care setting (29%) and located in a
nonmetropolitan statistical area (22%) were more likely than those not colocated (14%) and
in a metropolitan statistical area (16%) to use electronic health records.
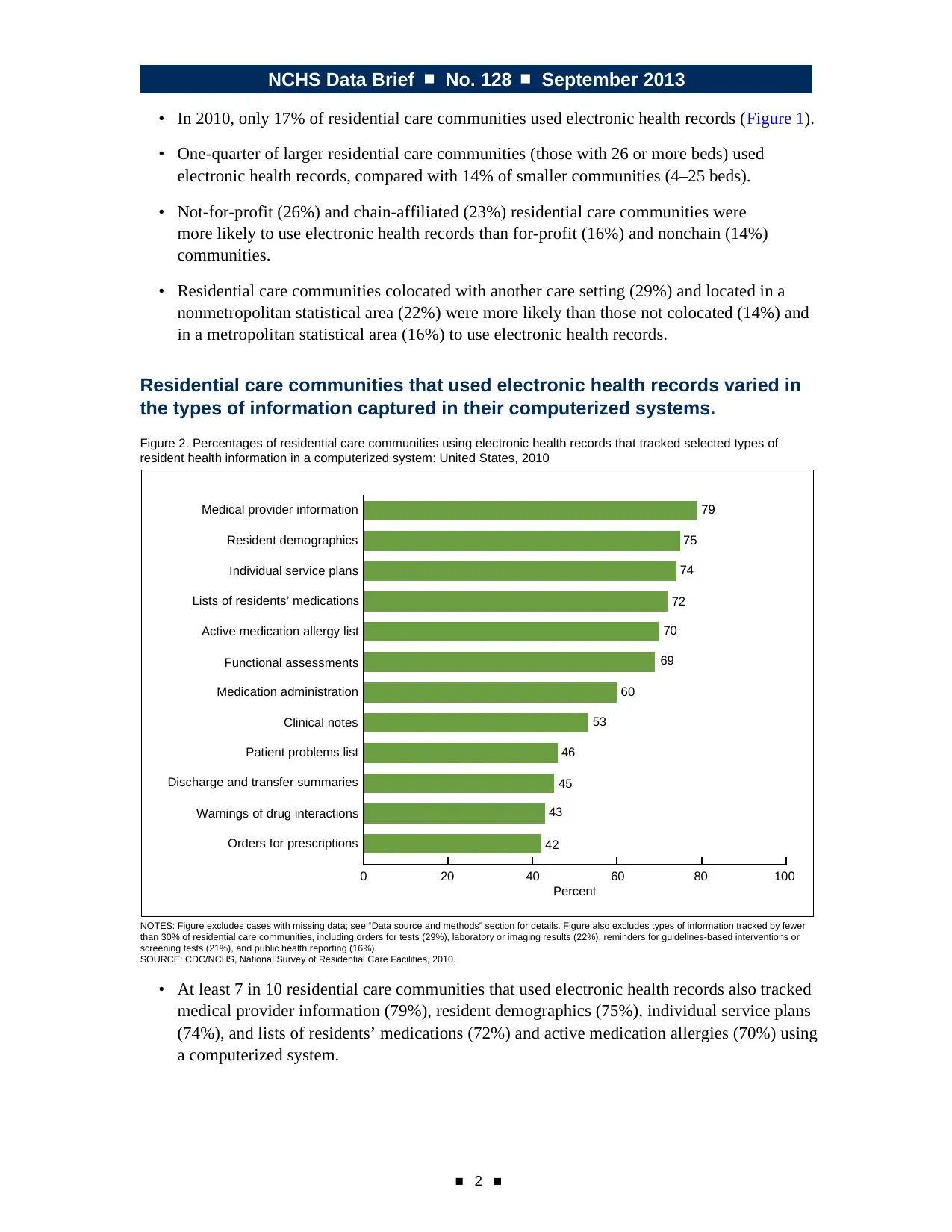
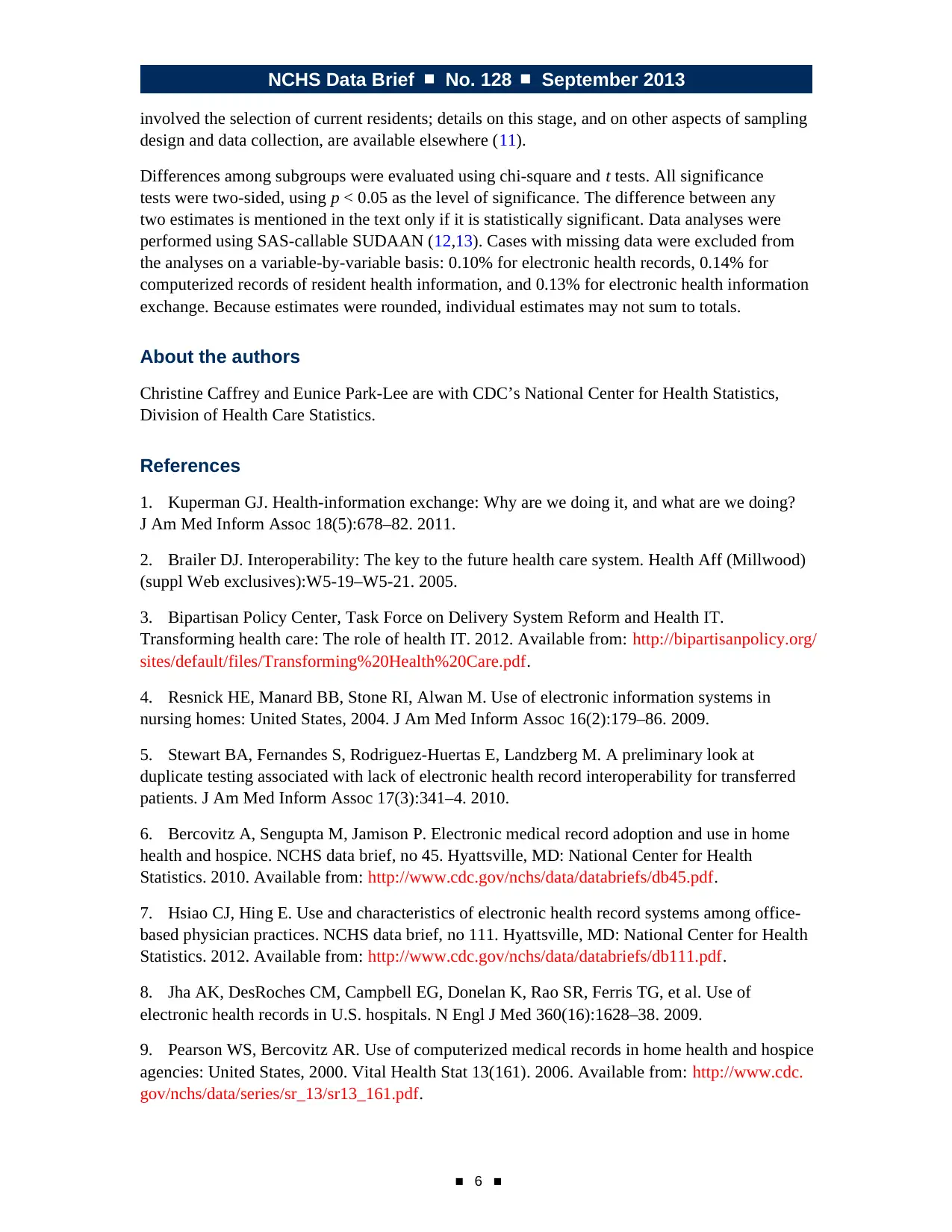
Residential care communities that used electronic health records varied in
the types of information captured in their computerized systems.
Figure 2. Percentages of residential care communities using electronic health records that tracked selected types of
resident health information in a computerized system: United States, 2010
NOTES: Figure excludes cases with missing data; see “Data source and methods” section for details. Figure also excludes types of information tracked by fewer
than 30% of residential care communities, including orders for tests (29%), laboratory or imaging results (22%), reminders for guidelines-based interventions or
screening tests (21%), and public health reporting (16%).
SOURCE: CDC/NCHS, National Survey of Residential Care Facilities, 2010.
0 20 40 60
Percent
80
79
75
74
72
70
69
60
53
46
45
43
42
100
Orders for prescriptions
Warnings of drug interactions
Discharge and transfer summaries
Patient problems list
Clinical notes
Medication administration
Functional assessments
Active medication allergy list
Lists of residents’ medications
Individual service plans
Resident demographics
Medical provider information
• At least 7 in 10 residential care communities that used electronic health records also tracked
medical provider information (79%), resident demographics (75%), individual service plans
(74%), and lists of residents’ medications (72%) and active medication allergies (70%) using
a computerized system.
■ 2 ■
• In 2010, only 17% of residential care communities used electronic health records (Figure 1).
• One-quarter of larger residential care communities (those with 26 or more beds) used
electronic health records, compared with 14% of smaller communities (4–25 beds).
• Not-for-profit (26%) and chain-affiliated (23%) residential care communities were
more likely to use electronic health records than for-profit (16%) and nonchain (14%)
communities.
• Residential care communities colocated with another care setting (29%) and located in a
nonmetropolitan statistical area (22%) were more likely than those not colocated (14%) and
in a metropolitan statistical area (16%) to use electronic health records.
Residential care communities that used electronic health records varied in
the types of information captured in their computerized systems.
Figure 2. Percentages of residential care communities using electronic health records that tracked selected types of
resident health information in a computerized system: United States, 2010
NOTES: Figure excludes cases with missing data; see “Data source and methods” section for details. Figure also excludes types of information tracked by fewer
than 30% of residential care communities, including orders for tests (29%), laboratory or imaging results (22%), reminders for guidelines-based interventions or
screening tests (21%), and public health reporting (16%).
SOURCE: CDC/NCHS, National Survey of Residential Care Facilities, 2010.
0 20 40 60
Percent
80
79
75
74
72
70
69
60
53
46
45
43
42
100
Orders for prescriptions
Warnings of drug interactions
Discharge and transfer summaries
Patient problems list
Clinical notes
Medication administration
Functional assessments
Active medication allergy list
Lists of residents’ medications
Individual service plans
Resident demographics
Medical provider information
• At least 7 in 10 residential care communities that used electronic health records also tracked
medical provider information (79%), resident demographics (75%), individual service plans
(74%), and lists of residents’ medications (72%) and active medication allergies (70%) using
a computerized system.
NCHS Data Brief ■ No. 128 ■ September 2013
■ 3 ■
• More than one-half of residential care communities that used electronic health records
tracked functional assessments (69%), medication administration (60%), and clinical notes
(53%).
• About 4 in 10 residential care communities that used electronic health records tracked
patient problems (46%), discharge and transfer summaries (45%), warnings of drug
interactions or contraindications (43%), and orders for prescriptions (42%) (Figure 2).
• Less than one-third of residential care communities that used electronic health records
tracked orders for tests (29%), laboratory or imaging results (22%), reminders for
guidelines-based interventions or screening tests (21%), and public health reporting (16%).
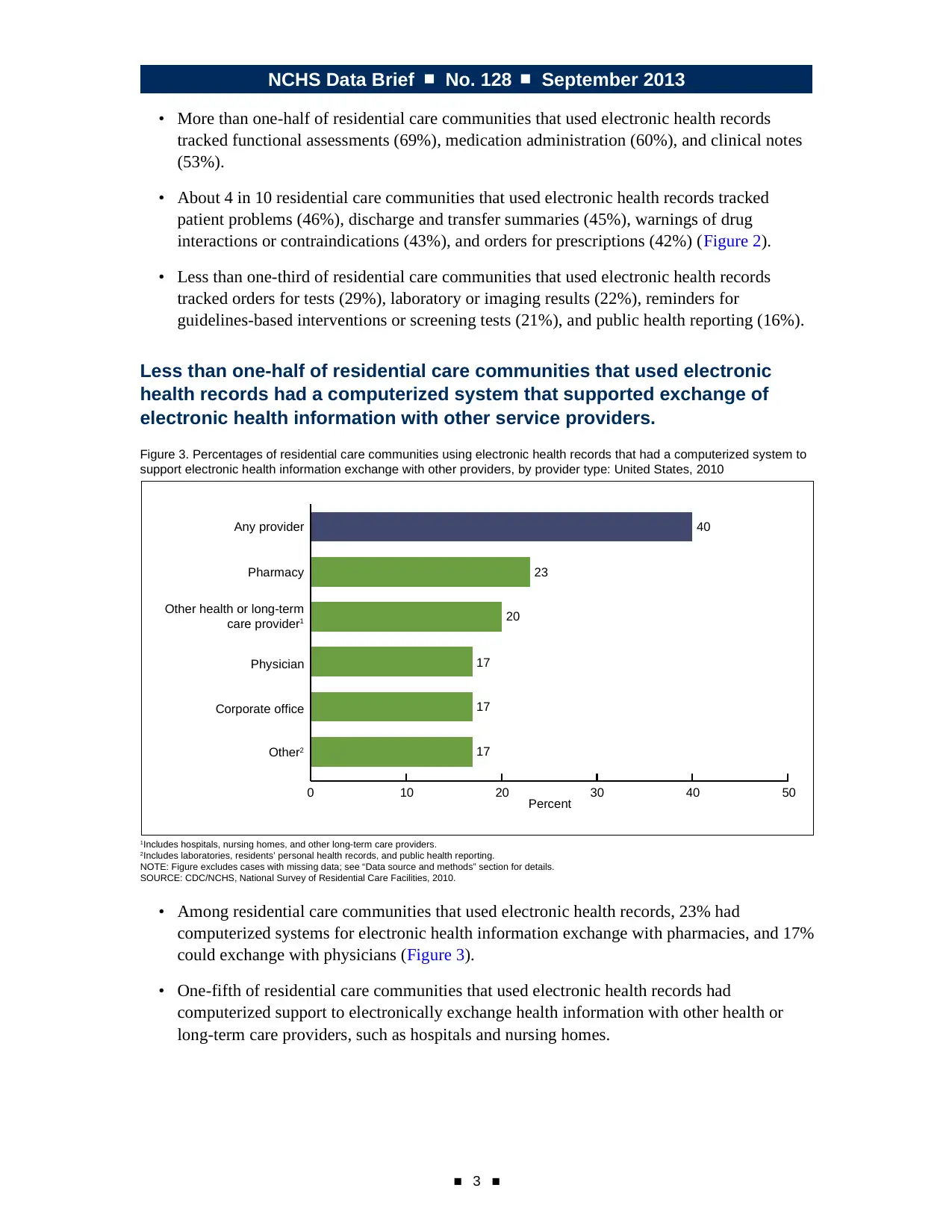
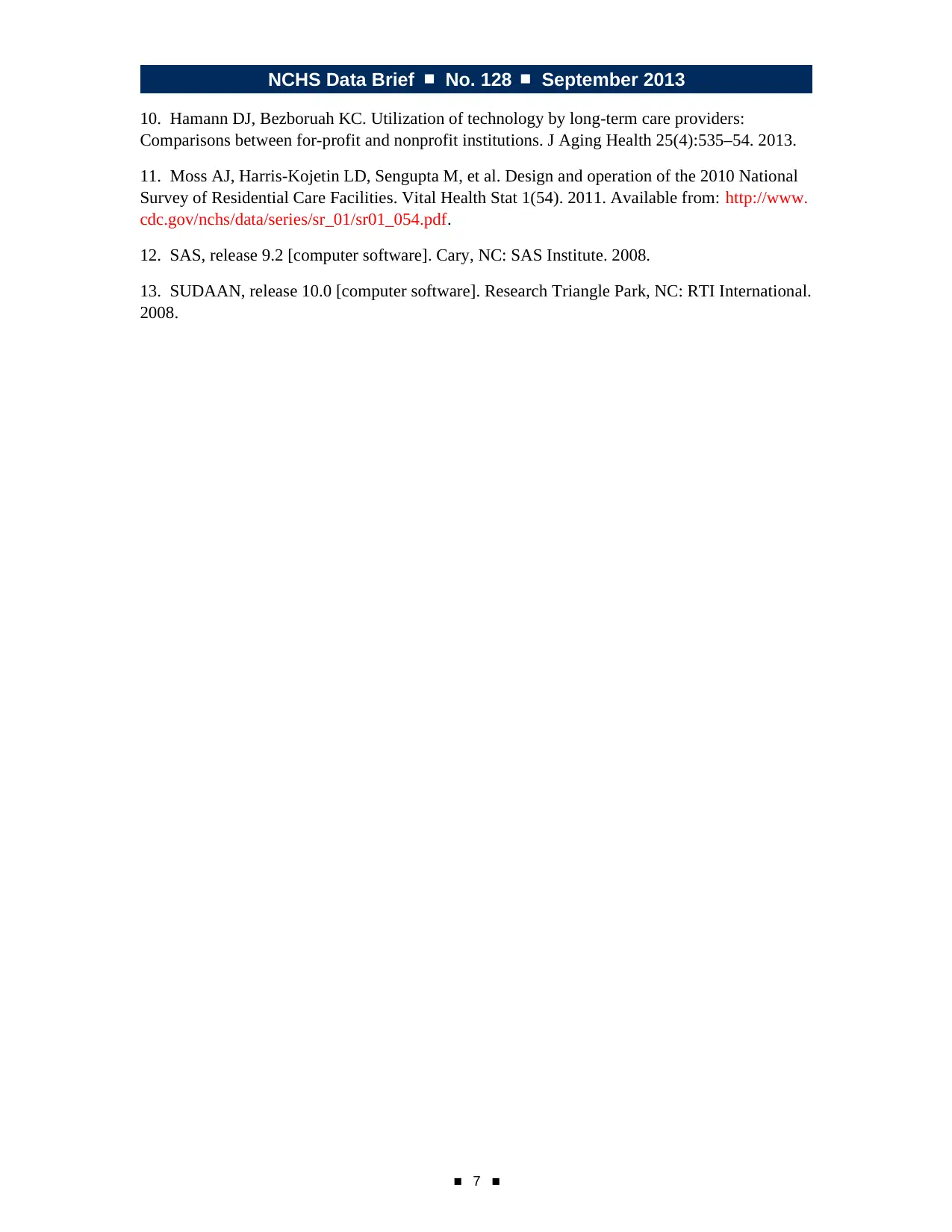
Less than one-half of residential care communities that used electronic
health records had a computerized system that supported exchange of
electronic health information with other service providers.
Figure 3. Percentages of residential care communities using electronic health records that had a computerized system to
support electronic health information exchange with other providers, by provider type: United States, 2010
1Includes hospitals, nursing homes, and other long-term care providers.
2Includes laboratories, residents’ personal health records, and public health reporting.
NOTE: Figure excludes cases with missing data; see “Data source and methods” section for details.
SOURCE: CDC/NCHS, National Survey of Residential Care Facilities, 2010.
0 10 20 30
Percent 40 50
40
23
20
17
17
17Other2
Corporate office
Physician
Other health or long-term
care provider1
Pharmacy
Any provider
• Among residential care communities that used electronic health records, 23% had
computerized systems for electronic health information exchange with pharmacies, and 17%
could exchange with physicians (Figure 3).
• One-fifth of residential care communities that used electronic health records had
computerized support to electronically exchange health information with other health or
long-term care providers, such as hospitals and nursing homes.
■ 3 ■
• More than one-half of residential care communities that used electronic health records
tracked functional assessments (69%), medication administration (60%), and clinical notes
(53%).
• About 4 in 10 residential care communities that used electronic health records tracked
patient problems (46%), discharge and transfer summaries (45%), warnings of drug
interactions or contraindications (43%), and orders for prescriptions (42%) (Figure 2).
• Less than one-third of residential care communities that used electronic health records
tracked orders for tests (29%), laboratory or imaging results (22%), reminders for
guidelines-based interventions or screening tests (21%), and public health reporting (16%).
Less than one-half of residential care communities that used electronic
health records had a computerized system that supported exchange of
electronic health information with other service providers.
Figure 3. Percentages of residential care communities using electronic health records that had a computerized system to
support electronic health information exchange with other providers, by provider type: United States, 2010
1Includes hospitals, nursing homes, and other long-term care providers.
2Includes laboratories, residents’ personal health records, and public health reporting.
NOTE: Figure excludes cases with missing data; see “Data source and methods” section for details.
SOURCE: CDC/NCHS, National Survey of Residential Care Facilities, 2010.
0 10 20 30
Percent 40 50
40
23
20
17
17
17Other2
Corporate office
Physician
Other health or long-term
care provider1
Pharmacy
Any provider
• Among residential care communities that used electronic health records, 23% had
computerized systems for electronic health information exchange with pharmacies, and 17%
could exchange with physicians (Figure 3).
• One-fifth of residential care communities that used electronic health records had
computerized support to electronically exchange health information with other health or
long-term care providers, such as hospitals and nursing homes.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
NCHS Data Brief ■ No. 128 ■ September 2013
■ 4 ■
Summary
In 2010, 17% of residential care communities reported that they used electronic health records.
These communities had different characteristics than those without electronic health records.
Communities that had electronic health records were more likely to be larger, to have
not-for-profit ownership, to be colocated with other care settings, and to be in a nonmetropolitan
statistical area. Medical provider information, resident demographics, individual service plans,
and lists of residents’ medications and active medication allergies were the most common
categories of resident health information recorded using a computerized system. Forty percent of
residential care communities that used electronic health records had a computerized system that
supported electronic health information exchange with one or more types of service providers.
Almost one-quarter had computerized support for exchanging electronic health information with
pharmacies.
This report has provided baseline findings on the use of electronic health record and electronic
health information exchange systems by residential care communities. This information should
be relevant to discussions on the role of residential care communities; the effective transition
from hospitals to residential care communities or other long-term care settings; avoidable
rehospitalizations; and helping persons who live with multiple chronic conditions better manage
their health care.
Definitions
Residential care communities: Includes assisted-living facilities and similar residential care
communities (e.g., personal care homes, adult care homes, board care homes, and adult foster
care) that meet the study eligibility criteria described in the “Data source and methods” section.
Electronic health records: Use was identified based on provider self-report in response to the
question, “Other than for accounting or billing purposes, does this facility use electronic health
records? This is a computerized version of the resident’s health and personal information used in
the management of the resident’s health care.” All providers were asked this question.
Computerized resident health information: Use was identified based on provider self-report
in response to the question, “Which of the following computerized capabilities does this
facility have?” Included were 16 types of computerized resident health information: resident
demographics, medical provider information, functional assessments, individual service plans,
clinical notes, patient problems list, medication administration, lists of residents’ medications
and active medication allergies, orders for prescriptions, warning of drug interactions or
contraindications, orders for tests, laboratory and imaging results, reminders for guidelines-based
interventions or screening tests, discharge and transfer summaries, and public health reporting.
All providers were asked this question.
Electronic health information exchange system: Use was identified based on provider self-report
in response to the question, “Does this facility’s computerized system support electronic health
information exchange with any of the following?” Nine different types of service providers were
included: physician, nursing home, hospital, pharmacy, laboratories, other health or long-term
care provider, residents’ personal health record, public health reporting, and corporate office.
To be asked this question, residential care communities had to have a computerized system
■ 4 ■
Summary
In 2010, 17% of residential care communities reported that they used electronic health records.
These communities had different characteristics than those without electronic health records.
Communities that had electronic health records were more likely to be larger, to have
not-for-profit ownership, to be colocated with other care settings, and to be in a nonmetropolitan
statistical area. Medical provider information, resident demographics, individual service plans,
and lists of residents’ medications and active medication allergies were the most common
categories of resident health information recorded using a computerized system. Forty percent of
residential care communities that used electronic health records had a computerized system that
supported electronic health information exchange with one or more types of service providers.
Almost one-quarter had computerized support for exchanging electronic health information with
pharmacies.
This report has provided baseline findings on the use of electronic health record and electronic
health information exchange systems by residential care communities. This information should
be relevant to discussions on the role of residential care communities; the effective transition
from hospitals to residential care communities or other long-term care settings; avoidable
rehospitalizations; and helping persons who live with multiple chronic conditions better manage
their health care.
Definitions
Residential care communities: Includes assisted-living facilities and similar residential care
communities (e.g., personal care homes, adult care homes, board care homes, and adult foster
care) that meet the study eligibility criteria described in the “Data source and methods” section.
Electronic health records: Use was identified based on provider self-report in response to the
question, “Other than for accounting or billing purposes, does this facility use electronic health
records? This is a computerized version of the resident’s health and personal information used in
the management of the resident’s health care.” All providers were asked this question.
Computerized resident health information: Use was identified based on provider self-report
in response to the question, “Which of the following computerized capabilities does this
facility have?” Included were 16 types of computerized resident health information: resident
demographics, medical provider information, functional assessments, individual service plans,
clinical notes, patient problems list, medication administration, lists of residents’ medications
and active medication allergies, orders for prescriptions, warning of drug interactions or
contraindications, orders for tests, laboratory and imaging results, reminders for guidelines-based
interventions or screening tests, discharge and transfer summaries, and public health reporting.
All providers were asked this question.
Electronic health information exchange system: Use was identified based on provider self-report
in response to the question, “Does this facility’s computerized system support electronic health
information exchange with any of the following?” Nine different types of service providers were
included: physician, nursing home, hospital, pharmacy, laboratories, other health or long-term
care provider, residents’ personal health record, public health reporting, and corporate office.
To be asked this question, residential care communities had to have a computerized system
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NCHS Data Brief ■ No. 128 ■ September 2013
■ 5 ■
for tracking at least 1 of the 16 different types of resident health information. Residential care
communities that did not track any of these types of information were coded as not having a
computerized system that supported electronic health information exchange with other service
providers. Four percent of residential care communities with electronic health records reported
that they did not track any of these types of resident health information in a computerized system.
Size: Categorized into two sizes based on the number of licensed, registered, or certified beds
(occupied and unoccupied) in a residential care community: 4–25 beds and 26 or more beds.
Ownership type: Categorized into two ownership types: private, for-profit; and not-for-profit.
The private, for-profit category included publicly traded facilities. Not-for-profit included private
nonprofit, as well as state, county, or local government ownership.
Chain affiliation: Having more than one community under common ownership or management.
This may include communities in-state or across multiple states. If communties were owned by a
chain, group, or multifacility system, they were coded as chain-affiliated.
Colocation with another care setting: Determined based on provider self-report in response to
the question, “Are any of the following types of places on the same property or at this same
location?” Four types of places were included: independent living; nursing home; rehabilitation,
subacute, or postacute unit in a nursing home; and hospital. Residential care communities were
considered to be colocated with another care setting if they had one or more of these places on the
same property or at the same location.
Metropolitan statistical area: Refers to a county or group of contiguous counties that contain at
least one urbanized area with a population of 50,000 or more. A metropolitan statistical area may
contain other counties that are economically and socially integrated with the central county, as
measured by commuting.
Data source and methods
Facility data from the 2010 NSRCF, conducted by the Centers for Disease Control and
Prevention’s (CDC) National Center for Health Statistics (NCHS), were used for these analyses.
To be eligible for the study, residential care communities must (a) have been licensed, registered,
listed, certified, or otherwise regulated by the state and have four or more licensed, certified, or
registered beds; (b) have at least one resident currently living in the community; and (c) provide
room and board with at least two meals a day, around-the-clock onsite supervision, and help
with personal care such as bathing and dressing or health-related services such as medication
management. These communities served a predominantly adult population. Communities
licensed to serve severely mentally ill or intellectually or developmentally disabled populations
exclusively were excluded. Nursing homes were also excluded unless they had a unit or wing that
met the above definition and residents could be enumerated separately.
The 2010 NSRCF used a stratified two-stage probability sampling design. The first stage was the
selection of residential care communities from the sampling frame representing the universe of
residential care communities in the United States. For the 2010 NSRCF, 3,605 residential care
communities were sampled with probability proportional to size. Interviews were completed with
2,302 residential care communities, for a first-stage community unweighted response rate of 79%
and a weighted response rate (for differential probabilities of selection) of 81%. The second stage
■ 5 ■
for tracking at least 1 of the 16 different types of resident health information. Residential care
communities that did not track any of these types of information were coded as not having a
computerized system that supported electronic health information exchange with other service
providers. Four percent of residential care communities with electronic health records reported
that they did not track any of these types of resident health information in a computerized system.
Size: Categorized into two sizes based on the number of licensed, registered, or certified beds
(occupied and unoccupied) in a residential care community: 4–25 beds and 26 or more beds.
Ownership type: Categorized into two ownership types: private, for-profit; and not-for-profit.
The private, for-profit category included publicly traded facilities. Not-for-profit included private
nonprofit, as well as state, county, or local government ownership.
Chain affiliation: Having more than one community under common ownership or management.
This may include communities in-state or across multiple states. If communties were owned by a
chain, group, or multifacility system, they were coded as chain-affiliated.
Colocation with another care setting: Determined based on provider self-report in response to
the question, “Are any of the following types of places on the same property or at this same
location?” Four types of places were included: independent living; nursing home; rehabilitation,
subacute, or postacute unit in a nursing home; and hospital. Residential care communities were
considered to be colocated with another care setting if they had one or more of these places on the
same property or at the same location.
Metropolitan statistical area: Refers to a county or group of contiguous counties that contain at
least one urbanized area with a population of 50,000 or more. A metropolitan statistical area may
contain other counties that are economically and socially integrated with the central county, as
measured by commuting.
Data source and methods
Facility data from the 2010 NSRCF, conducted by the Centers for Disease Control and
Prevention’s (CDC) National Center for Health Statistics (NCHS), were used for these analyses.
To be eligible for the study, residential care communities must (a) have been licensed, registered,
listed, certified, or otherwise regulated by the state and have four or more licensed, certified, or
registered beds; (b) have at least one resident currently living in the community; and (c) provide
room and board with at least two meals a day, around-the-clock onsite supervision, and help
with personal care such as bathing and dressing or health-related services such as medication
management. These communities served a predominantly adult population. Communities
licensed to serve severely mentally ill or intellectually or developmentally disabled populations
exclusively were excluded. Nursing homes were also excluded unless they had a unit or wing that
met the above definition and residents could be enumerated separately.
The 2010 NSRCF used a stratified two-stage probability sampling design. The first stage was the
selection of residential care communities from the sampling frame representing the universe of
residential care communities in the United States. For the 2010 NSRCF, 3,605 residential care
communities were sampled with probability proportional to size. Interviews were completed with
2,302 residential care communities, for a first-stage community unweighted response rate of 79%
and a weighted response rate (for differential probabilities of selection) of 81%. The second stage
NCHS Data Brief ■ No. 128 ■ September 2013
■ 6 ■
involved the selection of current residents; details on this stage, and on other aspects of sampling
design and data collection, are available elsewhere (11).
Differences among subgroups were evaluated using chi-square and t tests. All significance
tests were two-sided, using p < 0.05 as the level of significance. The difference between any
two estimates is mentioned in the text only if it is statistically significant. Data analyses were
performed using SAS-callable SUDAAN (12,13). Cases with missing data were excluded from
the analyses on a variable-by-variable basis: 0.10% for electronic health records, 0.14% for
computerized records of resident health information, and 0.13% for electronic health information
exchange. Because estimates were rounded, individual estimates may not sum to totals.
About the authors
Christine Caffrey and Eunice Park-Lee are with CDC’s National Center for Health Statistics,
Division of Health Care Statistics.
References
1. Kuperman GJ. Health-information exchange: Why are we doing it, and what are we doing?
J Am Med Inform Assoc 18(5):678–82. 2011.
2. Brailer DJ. Interoperability: The key to the future health care system. Health Aff (Millwood)
(suppl Web exclusives):W5-19–W5-21. 2005.
3. Bipartisan Policy Center, Task Force on Delivery System Reform and Health IT.
Transforming health care: The role of health IT. 2012. Available from: http://bipartisanpolicy.org/
sites/default/files/Transforming%20Health%20Care.pdf.
4. Resnick HE, Manard BB, Stone RI, Alwan M. Use of electronic information systems in
nursing homes: United States, 2004. J Am Med Inform Assoc 16(2):179–86. 2009.
5. Stewart BA, Fernandes S, Rodriguez-Huertas E, Landzberg M. A preliminary look at
duplicate testing associated with lack of electronic health record interoperability for transferred
patients. J Am Med Inform Assoc 17(3):341–4. 2010.
6. Bercovitz A, Sengupta M, Jamison P. Electronic medical record adoption and use in home
health and hospice. NCHS data brief, no 45. Hyattsville, MD: National Center for Health
Statistics. 2010. Available from: http://www.cdc.gov/nchs/data/databriefs/db45.pdf.
7. Hsiao CJ, Hing E. Use and characteristics of electronic health record systems among office-
based physician practices. NCHS data brief, no 111. Hyattsville, MD: National Center for Health
Statistics. 2012. Available from: http://www.cdc.gov/nchs/data/databriefs/db111.pdf.
8. Jha AK, DesRoches CM, Campbell EG, Donelan K, Rao SR, Ferris TG, et al. Use of
electronic health records in U.S. hospitals. N Engl J Med 360(16):1628–38. 2009.
9. Pearson WS, Bercovitz AR. Use of computerized medical records in home health and hospice
agencies: United States, 2000. Vital Health Stat 13(161). 2006. Available from: http://www.cdc.
gov/nchs/data/series/sr_13/sr13_161.pdf.
■ 6 ■
involved the selection of current residents; details on this stage, and on other aspects of sampling
design and data collection, are available elsewhere (11).
Differences among subgroups were evaluated using chi-square and t tests. All significance
tests were two-sided, using p < 0.05 as the level of significance. The difference between any
two estimates is mentioned in the text only if it is statistically significant. Data analyses were
performed using SAS-callable SUDAAN (12,13). Cases with missing data were excluded from
the analyses on a variable-by-variable basis: 0.10% for electronic health records, 0.14% for
computerized records of resident health information, and 0.13% for electronic health information
exchange. Because estimates were rounded, individual estimates may not sum to totals.
About the authors
Christine Caffrey and Eunice Park-Lee are with CDC’s National Center for Health Statistics,
Division of Health Care Statistics.
References
1. Kuperman GJ. Health-information exchange: Why are we doing it, and what are we doing?
J Am Med Inform Assoc 18(5):678–82. 2011.
2. Brailer DJ. Interoperability: The key to the future health care system. Health Aff (Millwood)
(suppl Web exclusives):W5-19–W5-21. 2005.
3. Bipartisan Policy Center, Task Force on Delivery System Reform and Health IT.
Transforming health care: The role of health IT. 2012. Available from: http://bipartisanpolicy.org/
sites/default/files/Transforming%20Health%20Care.pdf.
4. Resnick HE, Manard BB, Stone RI, Alwan M. Use of electronic information systems in
nursing homes: United States, 2004. J Am Med Inform Assoc 16(2):179–86. 2009.
5. Stewart BA, Fernandes S, Rodriguez-Huertas E, Landzberg M. A preliminary look at
duplicate testing associated with lack of electronic health record interoperability for transferred
patients. J Am Med Inform Assoc 17(3):341–4. 2010.
6. Bercovitz A, Sengupta M, Jamison P. Electronic medical record adoption and use in home
health and hospice. NCHS data brief, no 45. Hyattsville, MD: National Center for Health
Statistics. 2010. Available from: http://www.cdc.gov/nchs/data/databriefs/db45.pdf.
7. Hsiao CJ, Hing E. Use and characteristics of electronic health record systems among office-
based physician practices. NCHS data brief, no 111. Hyattsville, MD: National Center for Health
Statistics. 2012. Available from: http://www.cdc.gov/nchs/data/databriefs/db111.pdf.
8. Jha AK, DesRoches CM, Campbell EG, Donelan K, Rao SR, Ferris TG, et al. Use of
electronic health records in U.S. hospitals. N Engl J Med 360(16):1628–38. 2009.
9. Pearson WS, Bercovitz AR. Use of computerized medical records in home health and hospice
agencies: United States, 2000. Vital Health Stat 13(161). 2006. Available from: http://www.cdc.
gov/nchs/data/series/sr_13/sr13_161.pdf.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
NCHS Data Brief ■ No. 128 ■ September 2013
■ 7 ■
10. Hamann DJ, Bezboruah KC. Utilization of technology by long-term care providers:
Comparisons between for-profit and nonprofit institutions. J Aging Health 25(4):535–54. 2013.
11. Moss AJ, Harris-Kojetin LD, Sengupta M, et al. Design and operation of the 2010 National
Survey of Residential Care Facilities. Vital Health Stat 1(54). 2011. Available from: http://www.
cdc.gov/nchs/data/series/sr_01/sr01_054.pdf.
12. SAS, release 9.2 [computer software]. Cary, NC: SAS Institute. 2008.
13. SUDAAN, release 10.0 [computer software]. Research Triangle Park, NC: RTI International.
2008.
■ 7 ■
10. Hamann DJ, Bezboruah KC. Utilization of technology by long-term care providers:
Comparisons between for-profit and nonprofit institutions. J Aging Health 25(4):535–54. 2013.
11. Moss AJ, Harris-Kojetin LD, Sengupta M, et al. Design and operation of the 2010 National
Survey of Residential Care Facilities. Vital Health Stat 1(54). 2011. Available from: http://www.
cdc.gov/nchs/data/series/sr_01/sr01_054.pdf.
12. SAS, release 9.2 [computer software]. Cary, NC: SAS Institute. 2008.
13. SUDAAN, release 10.0 [computer software]. Research Triangle Park, NC: RTI International.
2008.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NCHS Data Brief ■ No. 128 ■ September 2013
U.S. DEPARTMENT OF
HEALTH & HUMAN SERVICES
Centers for Disease Control and Prevention
National Center for Health Statistics
3311 Toledo Road, Room 5419
Hyattsville, MD 20782
OFFICIAL BUSINESS
PENALTY FOR PRIVATE USE, $300
FIRST CLASS MAIL
POSTAGE & FEES PAID
CDC/NCHS
PERMIT NO. G-284
Suggested citation
Caffrey C, Park-Lee E. Use of electronic
health records in residential care
communities. NCHS data brief, no 128.
Hyattsville, MD: National Center for Health
Statistics. 2013.
Copyright information
All material appearing in this report is in
the public domain and may be reproduced
or copied without permission; citation as to
source, however, is appreciated.
National Center for Health
Statistics
Charles J. Rothwell, M.S., Acting Director
Jennifer H. Madans, Ph.D., Associate
Director for Science
Division of Health Care Statistics
Clarice Brown, M.S., Director
For e-mail updates on NCHS publication
releases, subscribe online at:
http://www.cdc.gov/nchs/govdelivery.htm.
For questions or general information
about NCHS:
Tel: 1–800–CDC–INFO (1–800–232–4636)
TTY: 1–888–232–6348
Internet: http://www.cdc.gov/nchs
Online request form: http://www.cdc.gov/
cdc-info/requestform.html
ISSN 1941–4927 Print ed.
ISSN 1941–4935 Online ed.
DHHS Publication No. 2013–1209
CS242703
U.S. DEPARTMENT OF
HEALTH & HUMAN SERVICES
Centers for Disease Control and Prevention
National Center for Health Statistics
3311 Toledo Road, Room 5419
Hyattsville, MD 20782
OFFICIAL BUSINESS
PENALTY FOR PRIVATE USE, $300
FIRST CLASS MAIL
POSTAGE & FEES PAID
CDC/NCHS
PERMIT NO. G-284
Suggested citation
Caffrey C, Park-Lee E. Use of electronic
health records in residential care
communities. NCHS data brief, no 128.
Hyattsville, MD: National Center for Health
Statistics. 2013.
Copyright information
All material appearing in this report is in
the public domain and may be reproduced
or copied without permission; citation as to
source, however, is appreciated.
National Center for Health
Statistics
Charles J. Rothwell, M.S., Acting Director
Jennifer H. Madans, Ph.D., Associate
Director for Science
Division of Health Care Statistics
Clarice Brown, M.S., Director
For e-mail updates on NCHS publication
releases, subscribe online at:
http://www.cdc.gov/nchs/govdelivery.htm.
For questions or general information
about NCHS:
Tel: 1–800–CDC–INFO (1–800–232–4636)
TTY: 1–888–232–6348
Internet: http://www.cdc.gov/nchs
Online request form: http://www.cdc.gov/
cdc-info/requestform.html
ISSN 1941–4927 Print ed.
ISSN 1941–4935 Online ed.
DHHS Publication No. 2013–1209
CS242703
1 out of 8
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





