Combined Diet and Exercise for Health: Green Prescription Analysis
VerifiedAdded on 2023/01/20
|10
|7966
|99
Report
AI Summary
This research article, published in BMC Public Health in 2018, investigates the impact of the Green Prescription program in New Zealand, a primary care intervention focused on improving patient health through exercise prescriptions. The study analyzed data from a survey of 1488 patients, examining the effects of changing diet and increasing physical activity on various health parameters, including metabolic, physiological, and psychological outcomes. The findings reveal that combined diet and exercise interventions lead to superior health improvements compared to either diet or exercise alone, particularly in weight loss, blood pressure reduction, and cholesterol management. The study emphasizes the potential benefits of incorporating nutrition education into the Green Prescription initiative, especially for patients with metabolic health problems, and underscores the importance of addressing both physical activity and dietary behaviors to maximize positive health outcomes within primary care settings. The research highlights the need for policy-makers to consider nutrition education as a key component of the Green Prescription program, offering a comprehensive approach to disease prevention and health promotion.
R E S E A R C H A R T I C L E Open Access
Combined diet and physicalactivity is
better than diet or physicalactivity alone at
improving health outcomes for patients in
New Zealand’s primary care intervention
Catherine Anne Elliot* and MichaelJohn Hamlin
Abstract
Background:A dearth of knowledge exists regarding how multiple health behavior changes made within an
exercise prescription programme can improve health parameters.This study aimed to analyse the impact of
changing diet and increasing exercise on health improvements among exercise prescription patients.
Methods:In 2016,a representative sample of allenroled New Zealand exercise prescription programme (Green
Prescription) patients were surveyed (N = 1488,29% male,46% ≥ 60 yr).Seven subsamples were created according
to their associated health problems;metabolic (n = 1192),physiological(n = 627),psychological(n = 447),sleep
problems (n = 253),breathing difficulties (n = 243),fallprevention (n = 104),and smoking (n = 67).After controlling
for sex and age,multinomialregression analyses were executed.
Results:Overall,weight problems were most prevalent (n = 886,60%),followed by high blood pressure/risk of
stroke (n = 424,29%),arthritis (n = 397,27%),and back pain/problems (n = 382,26%).Among patients who
reported metabolic health problems,those who changed their diet were 7.2,2.4 and 3.5 times more likely to lose
weight,lower their blood pressure,and lower their cholesterol,respectively compared to the controlgroup.
Moreover,those who increased their physicalactivity levels were 5.2 times more likely to lose weight in comparison
to controls.Patients who both increased physicalactivity and improved diet revealed higher odds of experiencing
health improvements than those who only made one change.Most notably,the odds of losing weight were much
higher for patients changing both behaviours (17.5) versus changing only physicalactivity (5.2) or only diet (7.2).
Conclusions:Although it is not currently a programme objective,policy-makers could include nutrition education
within the Green Prescription initiative,particularly for the 55% of patients who changed their diet while in the
programme.Physicalactivity prescription with a complimentary nutrition education component could benefit t
largest group of patients who report metabolic health problems.
Keywords:Primary care intervention,Physicalactivity,Exercise prescription,Disease prevention,Diet,Metabolic
health,Physiologic,Psychologic,Behavior change,Nutrition
* Correspondence:catherine.elliot@lincoln.ac.nz
Department of Tourism,Sport and Society,Lincoln University,PO Box 85084,
Lincoln,Christchurch,Canterbury 7647,New Zealand
© The Author(s).2018 Open AccessThis article is distributed under the terms of the Creative Commons Attribution 4.0
InternationalLicense (http://creativecommons.org/licenses/by/4.0/),which permits unrestricted use,distribution,and
reproduction in any medium,provided you give appropriate credit to the originalauthor(s) and the source,provide a link to
the Creative Commons license,and indicate if changes were made.The Creative Commons Public Domain Dedication waiver
(http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article,unless otherwise stated.
Elliot and Hamlin BMC Public Health (2018) 18:230
https://doi.org/10.1186/s12889-018-5152-z
Combined diet and physicalactivity is
better than diet or physicalactivity alone at
improving health outcomes for patients in
New Zealand’s primary care intervention
Catherine Anne Elliot* and MichaelJohn Hamlin
Abstract
Background:A dearth of knowledge exists regarding how multiple health behavior changes made within an
exercise prescription programme can improve health parameters.This study aimed to analyse the impact of
changing diet and increasing exercise on health improvements among exercise prescription patients.
Methods:In 2016,a representative sample of allenroled New Zealand exercise prescription programme (Green
Prescription) patients were surveyed (N = 1488,29% male,46% ≥ 60 yr).Seven subsamples were created according
to their associated health problems;metabolic (n = 1192),physiological(n = 627),psychological(n = 447),sleep
problems (n = 253),breathing difficulties (n = 243),fallprevention (n = 104),and smoking (n = 67).After controlling
for sex and age,multinomialregression analyses were executed.
Results:Overall,weight problems were most prevalent (n = 886,60%),followed by high blood pressure/risk of
stroke (n = 424,29%),arthritis (n = 397,27%),and back pain/problems (n = 382,26%).Among patients who
reported metabolic health problems,those who changed their diet were 7.2,2.4 and 3.5 times more likely to lose
weight,lower their blood pressure,and lower their cholesterol,respectively compared to the controlgroup.
Moreover,those who increased their physicalactivity levels were 5.2 times more likely to lose weight in comparison
to controls.Patients who both increased physicalactivity and improved diet revealed higher odds of experiencing
health improvements than those who only made one change.Most notably,the odds of losing weight were much
higher for patients changing both behaviours (17.5) versus changing only physicalactivity (5.2) or only diet (7.2).
Conclusions:Although it is not currently a programme objective,policy-makers could include nutrition education
within the Green Prescription initiative,particularly for the 55% of patients who changed their diet while in the
programme.Physicalactivity prescription with a complimentary nutrition education component could benefit t
largest group of patients who report metabolic health problems.
Keywords:Primary care intervention,Physicalactivity,Exercise prescription,Disease prevention,Diet,Metabolic
health,Physiologic,Psychologic,Behavior change,Nutrition
* Correspondence:catherine.elliot@lincoln.ac.nz
Department of Tourism,Sport and Society,Lincoln University,PO Box 85084,
Lincoln,Christchurch,Canterbury 7647,New Zealand
© The Author(s).2018 Open AccessThis article is distributed under the terms of the Creative Commons Attribution 4.0
InternationalLicense (http://creativecommons.org/licenses/by/4.0/),which permits unrestricted use,distribution,and
reproduction in any medium,provided you give appropriate credit to the originalauthor(s) and the source,provide a link to
the Creative Commons license,and indicate if changes were made.The Creative Commons Public Domain Dedication waiver
(http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article,unless otherwise stated.
Elliot and Hamlin BMC Public Health (2018) 18:230
https://doi.org/10.1186/s12889-018-5152-z
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Background
A lack of physicalactivity,tobacco smoking and an
unhealthy dietcontribute to almost80% ofthe world’s
risk of cardiovascular disease and type 2 diabetes [1].Po-
sitioned as the leading cause of premature death globally
[2],cardiovascular disease is an epidemic driven by type
2 diabetesand the metabolic syndrome [3].Empirical
evidence suggests thatthe co-occurrence ofbehavioral
risk factors yield greater risks for chronic diseases than
the sum oftheir individualindependenteffects [4,5].
For instance,individuals who are diagnosed with meta-
bolic syndrome show a 50-60% higher risk ofhaving a
cardiovascular disease than those without metabolic syn-
drome [6].With an estimated 20-25% ofthe world’s
adult population presentingmetabolicsyndrome[3],
multiple disease risk factors are increasingly common in
adults [7].
Major risk factors of cardiovascular disease and meta-
bolic syndrome are physicalinactivity and poor diet [8]
with physicalinactivity positioned as the primary cause
of most chronic diseases[9]. Although compelling
evidence existsfor the efficacy ofimproving physical
activity and diet [10] in treating individuals with multiple
risk factors [11],usualcare relies on pharmacotherapies
which merely address disease symptoms [12].
Cardiovascular disease is the number one single cause
of death in New Zealand,accounting for 33% per annum
[13].In 1998,New Zealand actively addressed this con-
cern by initiating aprimary-careintervention strategy
called Green Prescription,whereby generalpractitioners
and practice nurses refer or prescribe eligible patients to
trained personnel[14].Nearly 40,000 Green Prescription
referrals were written by clinicians in New Zealand from
2013 to 2014 [15].Green Prescription patientsmight
receive an exercise prescription for any combination of
cardiorespiratory,metabolic,physiologicalor psycho-
logical reasons.Once enroled,patients meet with physical
activity specialists who customise a physicalactivity rou-
tine which is catered to the patients’needs and lifestyles
while addressing barrierssuch asasthma,injury,back
pain, etc.
The Green Prescription Programmeis akin to a
globallyadoptedhealth initiativecalled Exerciseis
Medicine.Since both programmes focus on increasing
physical activity a as means of chronic disease
prevention,there is little scope to focus on the nutri-
tional componentof the energybalanceequation.
Nevertheless,68% of survey respondentsreported
they have receivedinformationon healthy eating
through Green Prescription.Additionally,55% of
patientsin the subsamplesanalysedin this study
reported changingdiet as well as physicalactivity.
From a physiologicalperspective,the energy balance
behaviors ofincreasing physicalactivity and changing
diet are major preventivetherapies,particularlyfor
weightloss,[10,16] but also for metabolic syndrome
[11] and cardiovasculardisease[17]. Evidencesug-
gests an increasedlikelihood of weight loss when
multiple health behaviorchangesare implemented
compared to one [10,16, 18].From a behavioraland
motivationalself-regulationstandpoint,the synergistic
effectsof improvingdiet and physicalactivityhave
been investigated.A study from Mata et al. [19]
showed that physical activity self-determination
predicted eating self-regulation and fully mediated the
relationship between physicalactivity and eating self-
regulation during a lifestyle weight-management
programme[19]. This suggeststhat psychological
mechanismsinvolved in motivation may help explain
the association between physicalactivityand eating
behaviors.Nevertheless,there is a dearth of know-
ledge regarding the effects ofmultiple health behavior
changesby exercise prescription patientsto improve
metabolic,physiologicaland psychologicaloutcomes.
This study aimed to analyse the impactof changing
diet and increasing exercise on health improvements
among exercise prescription patients.
Methods
The ethics application for this study was considered and
subsequently waived by the Health and Disability Ethics
Committees in New Zealand due to the research being
an evaluation of an existing programme.Responses were
collected on an informed consentbasis as partof the
17th annualGreen Prescription patientsurvey.The
survey was administered by Research New Zealand as
contracted by the NZ Ministry of Health to measure the
performance of Green Prescription.
This mixed-method online,telephone and paper-based
survey wasconducted from March-May 2016 using a
stratified random sample.Green Prescription patients
who had contact with one ofthe 17 Green Prescription
contractholdersin all DistrictHealth Boardsover 6
months from July-December2015 were eligiblefor
sampling.
Sample
Contract holders throughout New Zealand,who are re-
sponsible for delivering the nationalGreen Prescription
Programme,submitted theirpatientlist to Research
New Zealand, totaling 18,849 Green Prescription
patients throughout the country.Historically,there have
been lower survey response rates among minority groups
enroled in Green Prescription,namely,Māori and Pacific.
Assuming a low response rate,an oversampling ofthese
groups was executed to help ensure a more ethnically-
representative sample ofpatients.In the total sample,
European New Zealanderrespondentscomprised 59%,
Elliot and Hamlin BMC Public Health (2018) 18:230 Page 2 of 10
A lack of physicalactivity,tobacco smoking and an
unhealthy dietcontribute to almost80% ofthe world’s
risk of cardiovascular disease and type 2 diabetes [1].Po-
sitioned as the leading cause of premature death globally
[2],cardiovascular disease is an epidemic driven by type
2 diabetesand the metabolic syndrome [3].Empirical
evidence suggests thatthe co-occurrence ofbehavioral
risk factors yield greater risks for chronic diseases than
the sum oftheir individualindependenteffects [4,5].
For instance,individuals who are diagnosed with meta-
bolic syndrome show a 50-60% higher risk ofhaving a
cardiovascular disease than those without metabolic syn-
drome [6].With an estimated 20-25% ofthe world’s
adult population presentingmetabolicsyndrome[3],
multiple disease risk factors are increasingly common in
adults [7].
Major risk factors of cardiovascular disease and meta-
bolic syndrome are physicalinactivity and poor diet [8]
with physicalinactivity positioned as the primary cause
of most chronic diseases[9]. Although compelling
evidence existsfor the efficacy ofimproving physical
activity and diet [10] in treating individuals with multiple
risk factors [11],usualcare relies on pharmacotherapies
which merely address disease symptoms [12].
Cardiovascular disease is the number one single cause
of death in New Zealand,accounting for 33% per annum
[13].In 1998,New Zealand actively addressed this con-
cern by initiating aprimary-careintervention strategy
called Green Prescription,whereby generalpractitioners
and practice nurses refer or prescribe eligible patients to
trained personnel[14].Nearly 40,000 Green Prescription
referrals were written by clinicians in New Zealand from
2013 to 2014 [15].Green Prescription patientsmight
receive an exercise prescription for any combination of
cardiorespiratory,metabolic,physiologicalor psycho-
logical reasons.Once enroled,patients meet with physical
activity specialists who customise a physicalactivity rou-
tine which is catered to the patients’needs and lifestyles
while addressing barrierssuch asasthma,injury,back
pain, etc.
The Green Prescription Programmeis akin to a
globallyadoptedhealth initiativecalled Exerciseis
Medicine.Since both programmes focus on increasing
physical activity a as means of chronic disease
prevention,there is little scope to focus on the nutri-
tional componentof the energybalanceequation.
Nevertheless,68% of survey respondentsreported
they have receivedinformationon healthy eating
through Green Prescription.Additionally,55% of
patientsin the subsamplesanalysedin this study
reported changingdiet as well as physicalactivity.
From a physiologicalperspective,the energy balance
behaviors ofincreasing physicalactivity and changing
diet are major preventivetherapies,particularlyfor
weightloss,[10,16] but also for metabolic syndrome
[11] and cardiovasculardisease[17]. Evidencesug-
gests an increasedlikelihood of weight loss when
multiple health behaviorchangesare implemented
compared to one [10,16, 18].From a behavioraland
motivationalself-regulationstandpoint,the synergistic
effectsof improvingdiet and physicalactivityhave
been investigated.A study from Mata et al. [19]
showed that physical activity self-determination
predicted eating self-regulation and fully mediated the
relationship between physicalactivity and eating self-
regulation during a lifestyle weight-management
programme[19]. This suggeststhat psychological
mechanismsinvolved in motivation may help explain
the association between physicalactivityand eating
behaviors.Nevertheless,there is a dearth of know-
ledge regarding the effects ofmultiple health behavior
changesby exercise prescription patientsto improve
metabolic,physiologicaland psychologicaloutcomes.
This study aimed to analyse the impactof changing
diet and increasing exercise on health improvements
among exercise prescription patients.
Methods
The ethics application for this study was considered and
subsequently waived by the Health and Disability Ethics
Committees in New Zealand due to the research being
an evaluation of an existing programme.Responses were
collected on an informed consentbasis as partof the
17th annualGreen Prescription patientsurvey.The
survey was administered by Research New Zealand as
contracted by the NZ Ministry of Health to measure the
performance of Green Prescription.
This mixed-method online,telephone and paper-based
survey wasconducted from March-May 2016 using a
stratified random sample.Green Prescription patients
who had contact with one ofthe 17 Green Prescription
contractholdersin all DistrictHealth Boardsover 6
months from July-December2015 were eligiblefor
sampling.
Sample
Contract holders throughout New Zealand,who are re-
sponsible for delivering the nationalGreen Prescription
Programme,submitted theirpatientlist to Research
New Zealand, totaling 18,849 Green Prescription
patients throughout the country.Historically,there have
been lower survey response rates among minority groups
enroled in Green Prescription,namely,Māori and Pacific.
Assuming a low response rate,an oversampling ofthese
groups was executed to help ensure a more ethnically-
representative sample ofpatients.In the total sample,
European New Zealanderrespondentscomprised 59%,
Elliot and Hamlin BMC Public Health (2018) 18:230 Page 2 of 10
Māori 28% and Pacific 13%.The firststep in the data
collection processentailed separating largercontract
holders(with > 700patients)from smallercontract
holders.A sample of n = 2440Māori and Pacific
patientswas randomlyselected from thecombined
lists of the larger contractholders,proportionalto
the total numberof Māori and Pacific patientson
these lists.All patients with known contactdetails on
the lists of smallercontractholders(n = 4560)were
also selected.Finally, a random sample(n = 3000)
was selected from theremaininglists of the larger
contractholders in proportion with the totalnumber
of non-Māori/Pacific patients.
On 7th March 2016,selected patientsweresent a
letter from Research New Zealand invitingthem to
participate,along with a paper copy of the survey,and a
reply-paid envelope with three $250 giftvouchers used
as incentive.The letterintroduced the survey and its
purpose and gave instructions for completing the survey
on paper or online.On 30 March 2016,4657 patients
who had not yet responded were sent a reminder letter
and 1052 were sent a reminder email.Commencing 30
April 2015,a remindercall was made to all non-
responding Māoriand Pacific patients (n = 1973),and
non-Māori and Pacific patients (n = 960).Of these,1478
were contacted during the remindercall period (each
was called a maximum of five times).The main survey-
ing period ended on 15 May 2016.
To account for the varying sampling criteria applied to
large and small contract holders and the different participa-
tion rates,the results were weighted to be representative of
the proportion of patients from each contract holder.The
weighted results for the total sample have a maximum mar
gin of error of plus or minus 1.8%,at the 95% confidence
level (p. 15) [20].
Participation rate
A representative sample of10,000 patients were invited
to complete the survey.A totalof n = 2843 valid,com-
pleted responses were received during the survey period
(n = 2045 paper,n = 496 online,and n = 302 telephone),
representing a participation rate of28% [20].Data was
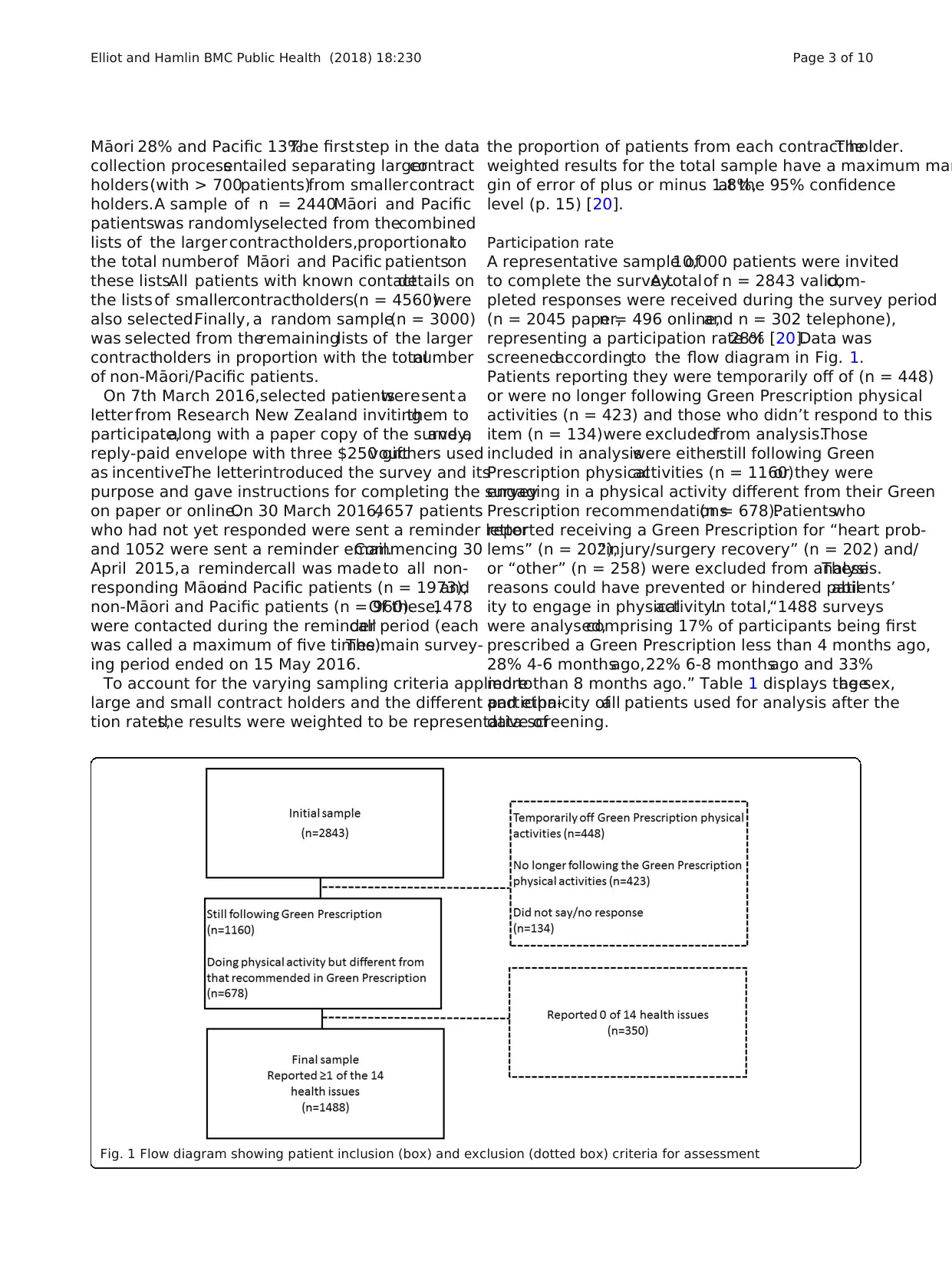
screenedaccordingto the flow diagram in Fig. 1.
Patients reporting they were temporarily off of (n = 448)
or were no longer following Green Prescription physical
activities (n = 423) and those who didn’t respond to this
item (n = 134)were excludedfrom analysis.Those
included in analysiswere eitherstill following Green
Prescription physicalactivities (n = 1160)or they were
engaging in a physical activity different from their Green
Prescription recommendations(n = 678).Patientswho
reported receiving a Green Prescription for “heart prob-
lems” (n = 202),“injury/surgery recovery” (n = 202) and/
or “other” (n = 258) were excluded from analysis.These
reasons could have prevented or hindered patients’abil-
ity to engage in physicalactivity.In total,“1488 surveys
were analysed,comprising 17% of participants being first
prescribed a Green Prescription less than 4 months ago,
28% 4-6 monthsago,22% 6-8 monthsago and 33%
more than 8 months ago.” Table 1 displays the sex,age
and ethnicity ofall patients used for analysis after the
data screening.
Fig. 1 Flow diagram showing patient inclusion (box) and exclusion (dotted box) criteria for assessment
Elliot and Hamlin BMC Public Health (2018) 18:230 Page 3 of 10
collection processentailed separating largercontract
holders(with > 700patients)from smallercontract
holders.A sample of n = 2440Māori and Pacific
patientswas randomlyselected from thecombined
lists of the larger contractholders,proportionalto
the total numberof Māori and Pacific patientson
these lists.All patients with known contactdetails on
the lists of smallercontractholders(n = 4560)were
also selected.Finally, a random sample(n = 3000)
was selected from theremaininglists of the larger
contractholders in proportion with the totalnumber
of non-Māori/Pacific patients.
On 7th March 2016,selected patientsweresent a
letter from Research New Zealand invitingthem to
participate,along with a paper copy of the survey,and a
reply-paid envelope with three $250 giftvouchers used
as incentive.The letterintroduced the survey and its
purpose and gave instructions for completing the survey
on paper or online.On 30 March 2016,4657 patients
who had not yet responded were sent a reminder letter
and 1052 were sent a reminder email.Commencing 30
April 2015,a remindercall was made to all non-
responding Māoriand Pacific patients (n = 1973),and
non-Māori and Pacific patients (n = 960).Of these,1478
were contacted during the remindercall period (each
was called a maximum of five times).The main survey-
ing period ended on 15 May 2016.
To account for the varying sampling criteria applied to
large and small contract holders and the different participa-
tion rates,the results were weighted to be representative of
the proportion of patients from each contract holder.The
weighted results for the total sample have a maximum mar
gin of error of plus or minus 1.8%,at the 95% confidence
level (p. 15) [20].
Participation rate
A representative sample of10,000 patients were invited
to complete the survey.A totalof n = 2843 valid,com-
pleted responses were received during the survey period
(n = 2045 paper,n = 496 online,and n = 302 telephone),
representing a participation rate of28% [20].Data was
screenedaccordingto the flow diagram in Fig. 1.
Patients reporting they were temporarily off of (n = 448)
or were no longer following Green Prescription physical
activities (n = 423) and those who didn’t respond to this
item (n = 134)were excludedfrom analysis.Those
included in analysiswere eitherstill following Green
Prescription physicalactivities (n = 1160)or they were
engaging in a physical activity different from their Green
Prescription recommendations(n = 678).Patientswho
reported receiving a Green Prescription for “heart prob-
lems” (n = 202),“injury/surgery recovery” (n = 202) and/
or “other” (n = 258) were excluded from analysis.These
reasons could have prevented or hindered patients’abil-
ity to engage in physicalactivity.In total,“1488 surveys
were analysed,comprising 17% of participants being first
prescribed a Green Prescription less than 4 months ago,
28% 4-6 monthsago,22% 6-8 monthsago and 33%
more than 8 months ago.” Table 1 displays the sex,age
and ethnicity ofall patients used for analysis after the
data screening.
Fig. 1 Flow diagram showing patient inclusion (box) and exclusion (dotted box) criteria for assessment
Elliot and Hamlin BMC Public Health (2018) 18:230 Page 3 of 10
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
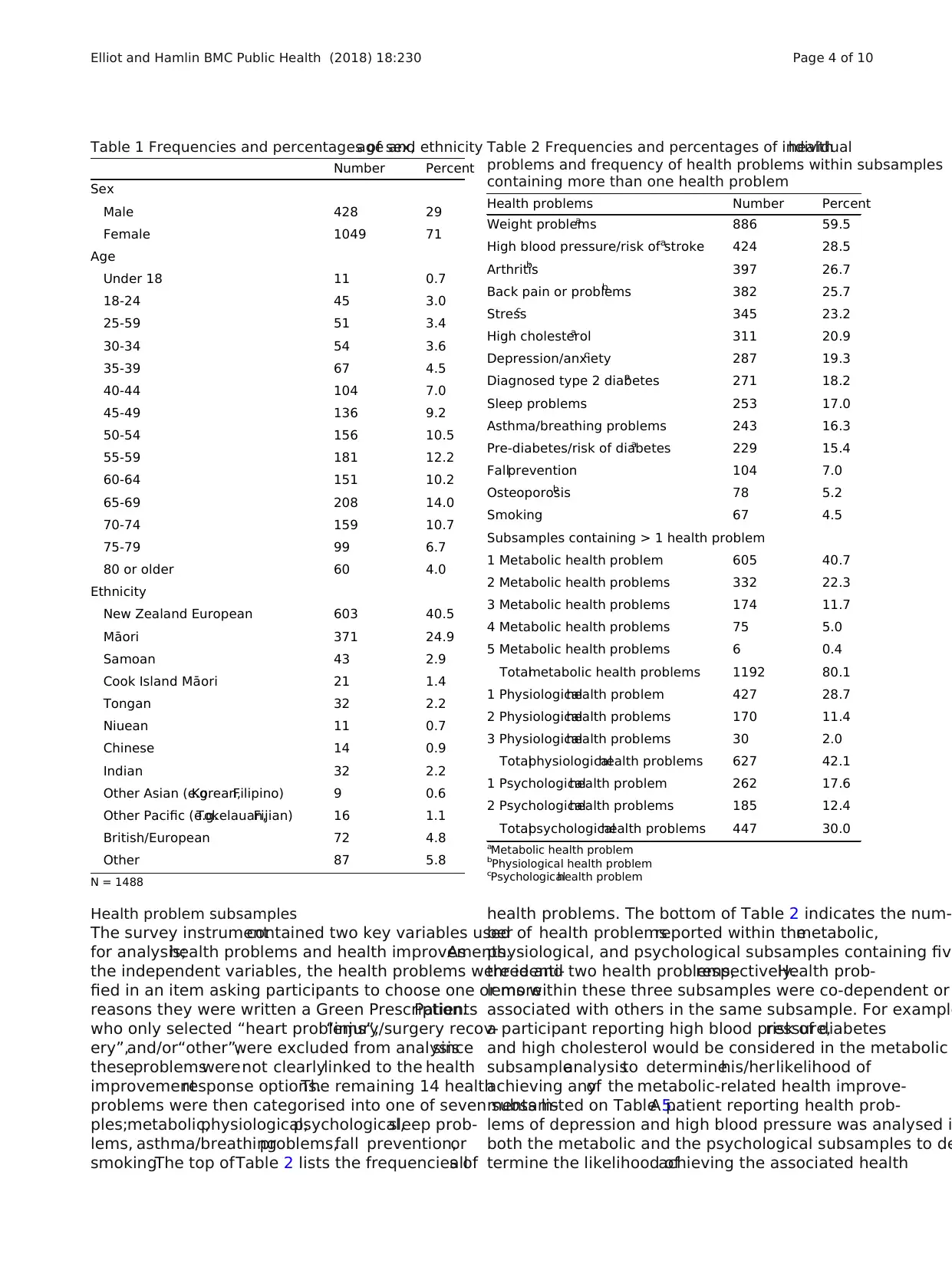
Health problem subsamples
The survey instrumentcontained two key variables used
for analysis;health problems and health improvements.As
the independent variables, the health problems were identi-
fied in an item asking participants to choose one or more
reasons they were written a Green Prescription.Patients
who only selected “heart problems”,“injury/surgery recov-
ery”,and/or“other”,were excluded from analysissince
theseproblemswerenot clearlylinked to the health
improvementresponse options.The remaining 14 health
problems were then categorised into one of seven subsam-
ples;metabolic,physiological,psychological,sleep prob-
lems, asthma/breathingproblems,fall prevention,or
smoking.The top ofTable 2 lists the frequencies ofall
health problems. The bottom of Table 2 indicates the num-
ber of health problemsreported within themetabolic,
physiological, and psychological subsamples containing five
three and two health problems,respectively.Health prob-
lems within these three subsamples were co-dependent or
associated with others in the same subsample. For example
a participant reporting high blood pressure,risk of diabetes
and high cholesterol would be considered in the metabolic
subsampleanalysisto determinehis/herlikelihood of
achieving anyof the metabolic-related health improve-
ments listed on Table 5.A patient reporting health prob-
lems of depression and high blood pressure was analysed i
both the metabolic and the psychological subsamples to de
termine the likelihood ofachieving the associated health
Table 1 Frequencies and percentages of sex,age and ethnicity
Number Percent
Sex
Male 428 29
Female 1049 71
Age
Under 18 11 0.7
18-24 45 3.0
25-59 51 3.4
30-34 54 3.6
35-39 67 4.5
40-44 104 7.0
45-49 136 9.2
50-54 156 10.5
55-59 181 12.2
60-64 151 10.2
65-69 208 14.0
70-74 159 10.7
75-79 99 6.7
80 or older 60 4.0
Ethnicity
New Zealand European 603 40.5
Māori 371 24.9
Samoan 43 2.9
Cook Island Māori 21 1.4
Tongan 32 2.2
Niuean 11 0.7
Chinese 14 0.9
Indian 32 2.2
Other Asian (e.g.Korean,Filipino) 9 0.6
Other Pacific (e.g.Tokelauan,Fijian) 16 1.1
British/European 72 4.8
Other 87 5.8
N = 1488
Table 2 Frequencies and percentages of individualhealth
problems and frequency of health problems within subsamples
containing more than one health problem
Health problems Number Percent
Weight problemsa 886 59.5
High blood pressure/risk of strokea 424 28.5
Arthritisb 397 26.7
Back pain or problemsb 382 25.7
Stressc 345 23.2
High cholesterola 311 20.9
Depression/anxietyc 287 19.3
Diagnosed type 2 diabetesa 271 18.2
Sleep problems 253 17.0
Asthma/breathing problems 243 16.3
Pre-diabetes/risk of diabetesa 229 15.4
Fallprevention 104 7.0
Osteoporosisb 78 5.2
Smoking 67 4.5
Subsamples containing > 1 health problem
1 Metabolic health problem 605 40.7
2 Metabolic health problems 332 22.3
3 Metabolic health problems 174 11.7
4 Metabolic health problems 75 5.0
5 Metabolic health problems 6 0.4
Totalmetabolic health problems 1192 80.1
1 Physiologicalhealth problem 427 28.7
2 Physiologicalhealth problems 170 11.4
3 Physiologicalhealth problems 30 2.0
Totalphysiologicalhealth problems 627 42.1
1 Psychologicalhealth problem 262 17.6
2 Psychologicalhealth problems 185 12.4
Totalpsychologicalhealth problems 447 30.0
aMetabolic health problem
bPhysiological health problem
cPsychologicalhealth problem
Elliot and Hamlin BMC Public Health (2018) 18:230 Page 4 of 10
The survey instrumentcontained two key variables used
for analysis;health problems and health improvements.As
the independent variables, the health problems were identi-
fied in an item asking participants to choose one or more
reasons they were written a Green Prescription.Patients
who only selected “heart problems”,“injury/surgery recov-
ery”,and/or“other”,were excluded from analysissince
theseproblemswerenot clearlylinked to the health
improvementresponse options.The remaining 14 health
problems were then categorised into one of seven subsam-
ples;metabolic,physiological,psychological,sleep prob-
lems, asthma/breathingproblems,fall prevention,or
smoking.The top ofTable 2 lists the frequencies ofall
health problems. The bottom of Table 2 indicates the num-
ber of health problemsreported within themetabolic,
physiological, and psychological subsamples containing five
three and two health problems,respectively.Health prob-
lems within these three subsamples were co-dependent or
associated with others in the same subsample. For example
a participant reporting high blood pressure,risk of diabetes
and high cholesterol would be considered in the metabolic
subsampleanalysisto determinehis/herlikelihood of
achieving anyof the metabolic-related health improve-
ments listed on Table 5.A patient reporting health prob-
lems of depression and high blood pressure was analysed i
both the metabolic and the psychological subsamples to de
termine the likelihood ofachieving the associated health
Table 1 Frequencies and percentages of sex,age and ethnicity
Number Percent
Sex
Male 428 29
Female 1049 71
Age
Under 18 11 0.7
18-24 45 3.0
25-59 51 3.4
30-34 54 3.6
35-39 67 4.5
40-44 104 7.0
45-49 136 9.2
50-54 156 10.5
55-59 181 12.2
60-64 151 10.2
65-69 208 14.0
70-74 159 10.7
75-79 99 6.7
80 or older 60 4.0
Ethnicity
New Zealand European 603 40.5
Māori 371 24.9
Samoan 43 2.9
Cook Island Māori 21 1.4
Tongan 32 2.2
Niuean 11 0.7
Chinese 14 0.9
Indian 32 2.2
Other Asian (e.g.Korean,Filipino) 9 0.6
Other Pacific (e.g.Tokelauan,Fijian) 16 1.1
British/European 72 4.8
Other 87 5.8
N = 1488
Table 2 Frequencies and percentages of individualhealth
problems and frequency of health problems within subsamples
containing more than one health problem
Health problems Number Percent
Weight problemsa 886 59.5
High blood pressure/risk of strokea 424 28.5
Arthritisb 397 26.7
Back pain or problemsb 382 25.7
Stressc 345 23.2
High cholesterola 311 20.9
Depression/anxietyc 287 19.3
Diagnosed type 2 diabetesa 271 18.2
Sleep problems 253 17.0
Asthma/breathing problems 243 16.3
Pre-diabetes/risk of diabetesa 229 15.4
Fallprevention 104 7.0
Osteoporosisb 78 5.2
Smoking 67 4.5
Subsamples containing > 1 health problem
1 Metabolic health problem 605 40.7
2 Metabolic health problems 332 22.3
3 Metabolic health problems 174 11.7
4 Metabolic health problems 75 5.0
5 Metabolic health problems 6 0.4
Totalmetabolic health problems 1192 80.1
1 Physiologicalhealth problem 427 28.7
2 Physiologicalhealth problems 170 11.4
3 Physiologicalhealth problems 30 2.0
Totalphysiologicalhealth problems 627 42.1
1 Psychologicalhealth problem 262 17.6
2 Psychologicalhealth problems 185 12.4
Totalpsychologicalhealth problems 447 30.0
aMetabolic health problem
bPhysiological health problem
cPsychologicalhealth problem
Elliot and Hamlin BMC Public Health (2018) 18:230 Page 4 of 10
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
improvements (i.e.lower blood pressure,feeling less de-
pressed/anxious). Combining health problems into subsam-
ples made for a more robust analysis.
Measures
Health behaviour
The health behaviorpredictorvariablewas used to
create fourbehaviourchange groupsfor comparison;
1. increased physicalactivity,2. changed diet(diet),3.
increased physicalactivity and changed diet(physical
activity and diet),or 4. no changes to physicalactivity
and diet(controlgroup).Groupingswere created by
using responsesfrom two items regardingbehavior
changesto physicalactivityand diet. The physical
activityitem was, “Compared with thetime before
you were first given a Green Prescription,are you
now spending more time being active,aboutthe same
amount of time being active or less time being
active?” Patients choosing the latter two options were
combinedinto the group “no increasein physical
activity.”The diet item was, “Haveyou made any
changes to your food and/or drink intake since being
given yourGreen Prescription?”and contained “yes”
and “no”response options.Table 3 indicates the fre-
quenciesof health problemsfor all four behaviour
change groups.
Health improvements
There were 15 health improvements analysed as dependent
variables.Patients who reported “yes” to noticing positive
changes since first being issued a Green Prescription were
then prompted to answer the follow-up item,“If yes,what
positive changes have you noticed?” There were originally 19
response options, but the options “feel stronger/fitter”,“gen-
erally feelbetter”,“more energy”,and/or “other” were ex-
cluded from analysisas theseoptionsdo not directly
associate with any one particular health problem. Descriptive
statistics of the 15 health improvements are listed in Table 4.
Analysis
A predictive analysis was conducted through multinomial
regression to interpret odds ratios (OR). A linear regression
was calculated to test the assumption ofmulticollinearity.
The minimum cut off for tolerance was set at 0.2 and the
maximum cut off for the variance inflation factor (VIF) was
5. All independent variables met these assumptions,with
tolerances ranging between .699 and .956 and VIF ranging
between 1.430 and 1.046.All other assumptions for multi-
nomial regression were met.Multinomial regressions were
conducted using the health behavior groups as the predic-
tors (physicalactivity,dietand physicalactivity and diet)
each compared to the control group (neither physical activ-
ity nor diet).Then,odds ratios (OR) were calculated with
95% confidence intervals.All multinomial regressions con-
trolled for sex and age groups (under 60, over 59).
Results
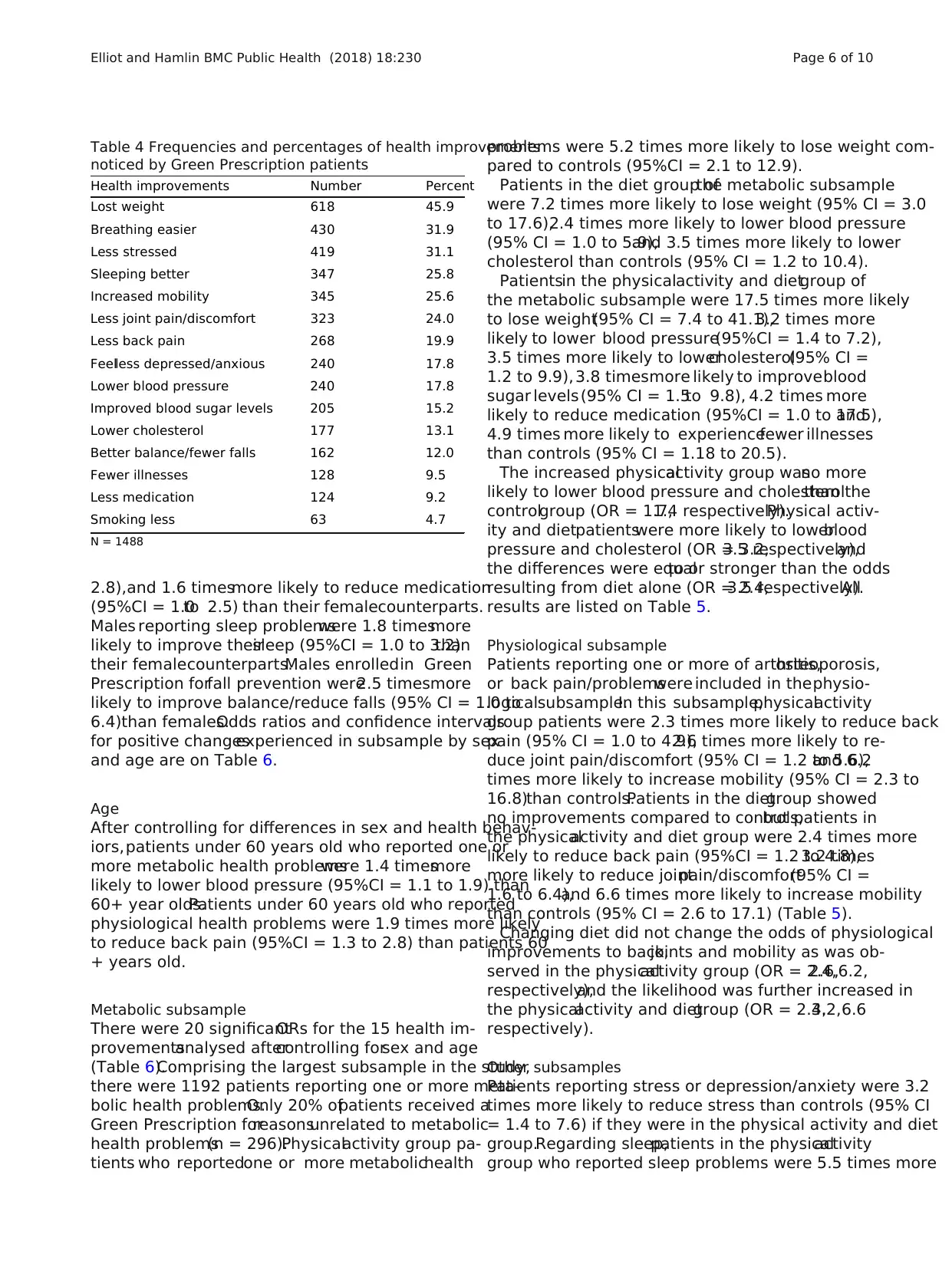
Overall,weightproblems were the mostcommonly re-
ported health problems (n = 886,60%),followed by high
blood pressure/risk ofstroke (n = 424,29%),arthritis
(n = 397,27%),and back pain/problems (n = 382,26%)
(Table 2).The most commonly reported health improve-
ments were weight loss (n = 618,46%),breathing easier
(n = 430,32%),and less stress (n = 419,31%) (Table 4).
After controlling forsex and age,patientsin the diet
group were more likely to improve 3 ofthe 15 possible
health problems listed,and the physicalactivity group
improved 6 of15, but the physicalactivityand diet
group was more likely to improve 11 of 15 health prob-
lems compared to the control group (Table 5).
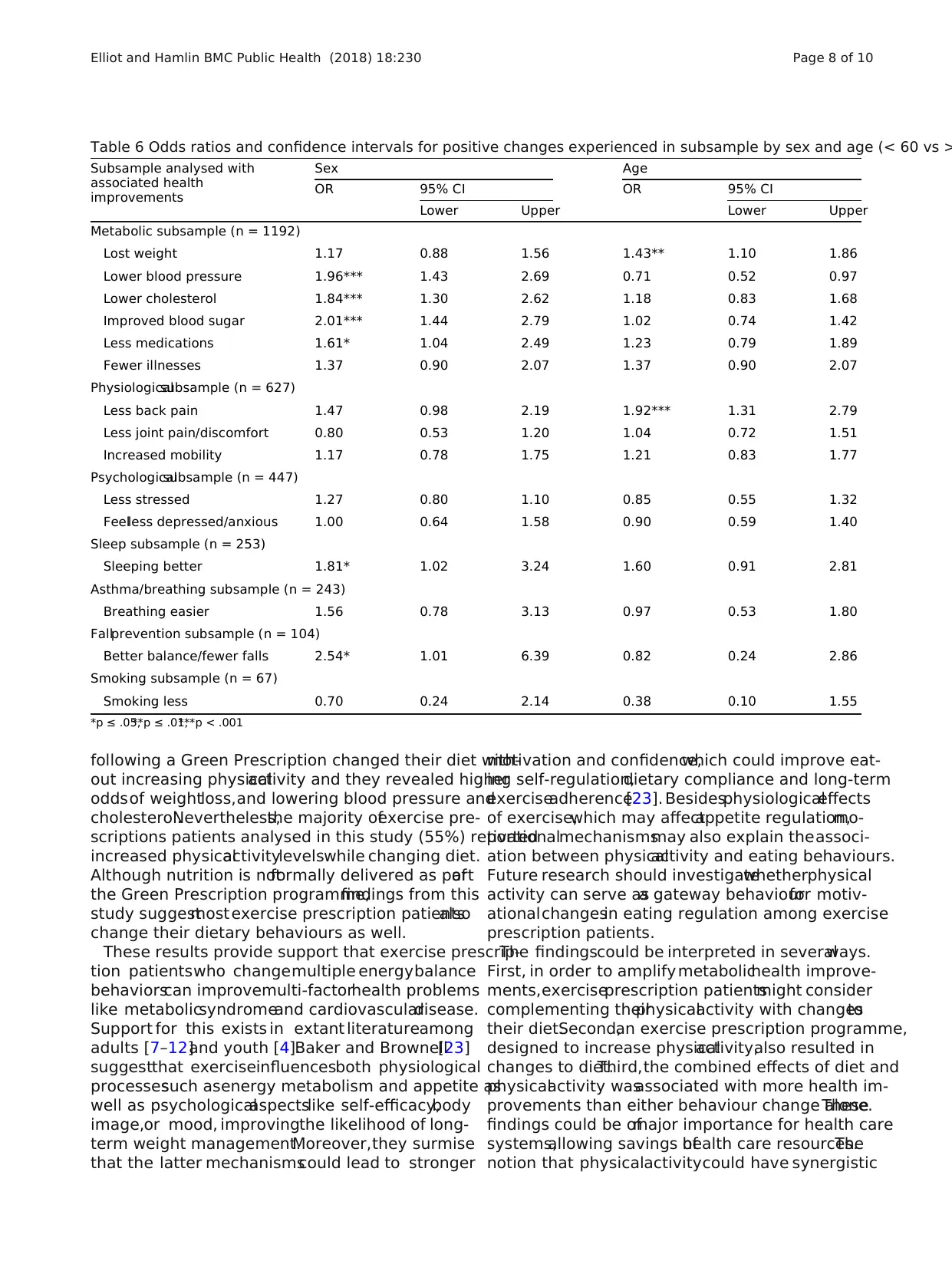
Sex
After controlling for differences in age and health behav-
ior, males who reported one or more metabolic health
problemswere2.0 timesmore likely to lower blood
pressure (95% CI = 1.4 to 2.7),1.8 times more likely to
lowercholesterol(95%CI = 1.3 to 2.6),2.0 timesmore
likely to improve blood sugarlevels(95% CI = 1.4 to
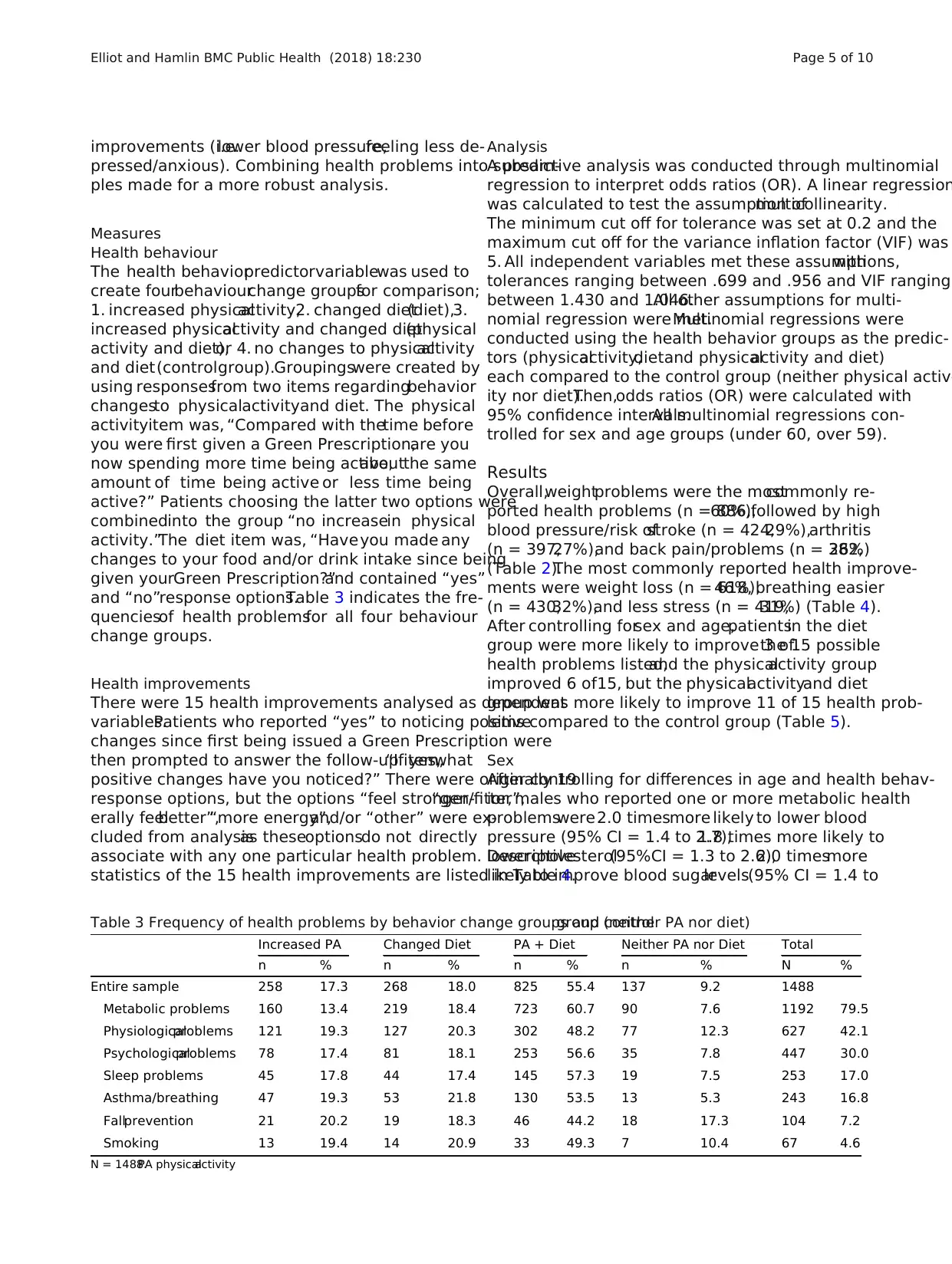
Table 3 Frequency of health problems by behavior change groups and controlgroup (neither PA nor diet)
Increased PA Changed Diet PA + Diet Neither PA nor Diet Total
n % n % n % n % N %
Entire sample 258 17.3 268 18.0 825 55.4 137 9.2 1488
Metabolic problems 160 13.4 219 18.4 723 60.7 90 7.6 1192 79.5
Physiologicalproblems 121 19.3 127 20.3 302 48.2 77 12.3 627 42.1
Psychologicalproblems 78 17.4 81 18.1 253 56.6 35 7.8 447 30.0
Sleep problems 45 17.8 44 17.4 145 57.3 19 7.5 253 17.0
Asthma/breathing 47 19.3 53 21.8 130 53.5 13 5.3 243 16.8
Fallprevention 21 20.2 19 18.3 46 44.2 18 17.3 104 7.2
Smoking 13 19.4 14 20.9 33 49.3 7 10.4 67 4.6
N = 1488.PA physicalactivity
Elliot and Hamlin BMC Public Health (2018) 18:230 Page 5 of 10
pressed/anxious). Combining health problems into subsam-
ples made for a more robust analysis.
Measures
Health behaviour
The health behaviorpredictorvariablewas used to
create fourbehaviourchange groupsfor comparison;
1. increased physicalactivity,2. changed diet(diet),3.
increased physicalactivity and changed diet(physical
activity and diet),or 4. no changes to physicalactivity
and diet(controlgroup).Groupingswere created by
using responsesfrom two items regardingbehavior
changesto physicalactivityand diet. The physical
activityitem was, “Compared with thetime before
you were first given a Green Prescription,are you
now spending more time being active,aboutthe same
amount of time being active or less time being
active?” Patients choosing the latter two options were
combinedinto the group “no increasein physical
activity.”The diet item was, “Haveyou made any
changes to your food and/or drink intake since being
given yourGreen Prescription?”and contained “yes”
and “no”response options.Table 3 indicates the fre-
quenciesof health problemsfor all four behaviour
change groups.
Health improvements
There were 15 health improvements analysed as dependent
variables.Patients who reported “yes” to noticing positive
changes since first being issued a Green Prescription were
then prompted to answer the follow-up item,“If yes,what
positive changes have you noticed?” There were originally 19
response options, but the options “feel stronger/fitter”,“gen-
erally feelbetter”,“more energy”,and/or “other” were ex-
cluded from analysisas theseoptionsdo not directly
associate with any one particular health problem. Descriptive
statistics of the 15 health improvements are listed in Table 4.
Analysis
A predictive analysis was conducted through multinomial
regression to interpret odds ratios (OR). A linear regression
was calculated to test the assumption ofmulticollinearity.
The minimum cut off for tolerance was set at 0.2 and the
maximum cut off for the variance inflation factor (VIF) was
5. All independent variables met these assumptions,with
tolerances ranging between .699 and .956 and VIF ranging
between 1.430 and 1.046.All other assumptions for multi-
nomial regression were met.Multinomial regressions were
conducted using the health behavior groups as the predic-
tors (physicalactivity,dietand physicalactivity and diet)
each compared to the control group (neither physical activ-
ity nor diet).Then,odds ratios (OR) were calculated with
95% confidence intervals.All multinomial regressions con-
trolled for sex and age groups (under 60, over 59).
Results
Overall,weightproblems were the mostcommonly re-
ported health problems (n = 886,60%),followed by high
blood pressure/risk ofstroke (n = 424,29%),arthritis
(n = 397,27%),and back pain/problems (n = 382,26%)
(Table 2).The most commonly reported health improve-
ments were weight loss (n = 618,46%),breathing easier
(n = 430,32%),and less stress (n = 419,31%) (Table 4).
After controlling forsex and age,patientsin the diet
group were more likely to improve 3 ofthe 15 possible
health problems listed,and the physicalactivity group
improved 6 of15, but the physicalactivityand diet
group was more likely to improve 11 of 15 health prob-
lems compared to the control group (Table 5).
Sex
After controlling for differences in age and health behav-
ior, males who reported one or more metabolic health
problemswere2.0 timesmore likely to lower blood
pressure (95% CI = 1.4 to 2.7),1.8 times more likely to
lowercholesterol(95%CI = 1.3 to 2.6),2.0 timesmore
likely to improve blood sugarlevels(95% CI = 1.4 to
Table 3 Frequency of health problems by behavior change groups and controlgroup (neither PA nor diet)
Increased PA Changed Diet PA + Diet Neither PA nor Diet Total
n % n % n % n % N %
Entire sample 258 17.3 268 18.0 825 55.4 137 9.2 1488
Metabolic problems 160 13.4 219 18.4 723 60.7 90 7.6 1192 79.5
Physiologicalproblems 121 19.3 127 20.3 302 48.2 77 12.3 627 42.1
Psychologicalproblems 78 17.4 81 18.1 253 56.6 35 7.8 447 30.0
Sleep problems 45 17.8 44 17.4 145 57.3 19 7.5 253 17.0
Asthma/breathing 47 19.3 53 21.8 130 53.5 13 5.3 243 16.8
Fallprevention 21 20.2 19 18.3 46 44.2 18 17.3 104 7.2
Smoking 13 19.4 14 20.9 33 49.3 7 10.4 67 4.6
N = 1488.PA physicalactivity
Elliot and Hamlin BMC Public Health (2018) 18:230 Page 5 of 10
2.8),and 1.6 timesmore likely to reduce medication
(95%CI = 1.0to 2.5) than their femalecounterparts.
Males reporting sleep problemswere 1.8 timesmore
likely to improve theirsleep (95%CI = 1.0 to 3.2)than
their femalecounterparts.Males enrolledin Green
Prescription forfall prevention were2.5 timesmore
likely to improve balance/reduce falls (95% CI = 1.0 to
6.4)than females.Odds ratios and confidence intervals
for positive changesexperienced in subsample by sex
and age are on Table 6.
Age
After controlling for differences in sex and health behav-
iors,patients under 60 years old who reported one or
more metabolic health problemswere 1.4 timesmore
likely to lower blood pressure (95%CI = 1.1 to 1.9) than
60+ year olds.Patients under 60 years old who reported
physiological health problems were 1.9 times more likely
to reduce back pain (95%CI = 1.3 to 2.8) than patients 60
+ years old.
Metabolic subsample
There were 20 significantORs for the 15 health im-
provementsanalysed aftercontrolling forsex and age
(Table 6).Comprising the largest subsample in the study,
there were 1192 patients reporting one or more meta-
bolic health problems.Only 20% ofpatients received a
Green Prescription forreasonsunrelated to metabolic
health problems(n = 296).Physicalactivity group pa-
tients who reportedone or more metabolichealth
problems were 5.2 times more likely to lose weight com-
pared to controls (95%CI = 2.1 to 12.9).
Patients in the diet group ofthe metabolic subsample
were 7.2 times more likely to lose weight (95% CI = 3.0
to 17.6),2.4 times more likely to lower blood pressure
(95% CI = 1.0 to 5.9),and 3.5 times more likely to lower
cholesterol than controls (95% CI = 1.2 to 10.4).
Patientsin the physicalactivity and dietgroup of
the metabolic subsample were 17.5 times more likely
to lose weight(95% CI = 7.4 to 41.1),3.2 times more
likely to lower blood pressure(95%CI = 1.4 to 7.2),
3.5 times more likely to lowercholesterol(95% CI =
1.2 to 9.9), 3.8 timesmore likely to improveblood
sugar levels(95% CI = 1.5to 9.8), 4.2 times more
likely to reduce medication (95%CI = 1.0 to 17.5),and
4.9 times more likely to experiencefewer illnesses
than controls (95% CI = 1.18 to 20.5).
The increased physicalactivity group wasno more
likely to lower blood pressure and cholesterolthan the
controlgroup (OR = 1.7,1.4 respectively).Physical activ-
ity and dietpatientswere more likely to lowerblood
pressure and cholesterol (OR = 3.2,3.5 respectively),and
the differences were equalto or stronger than the odds
resulting from diet alone (OR = 2.4,3.5 respectively).All
results are listed on Table 5.
Physiological subsample
Patients reporting one or more of arthritis,osteoporosis,
or back pain/problemswere included in thephysio-
logicalsubsample.In this subsample,physicalactivity
group patients were 2.3 times more likely to reduce back
pain (95% CI = 1.0 to 4.9),2.6 times more likely to re-
duce joint pain/discomfort (95% CI = 1.2 to 5.6),and 6.2
times more likely to increase mobility (95% CI = 2.3 to
16.8)than controls.Patients in the dietgroup showed
no improvements compared to controls,but patients in
the physicalactivity and diet group were 2.4 times more
likely to reduce back pain (95%CI = 1.2 to 4.8),3.2 times
more likely to reduce jointpain/discomfort(95% CI =
1.6 to 6.4),and 6.6 times more likely to increase mobility
than controls (95% CI = 2.6 to 17.1) (Table 5).
Changing diet did not change the odds of physiological
improvements to back,joints and mobility as was ob-
served in the physicalactivity group (OR = 2.4,2.6,6.2,
respectively),and the likelihood was further increased in
the physicalactivity and dietgroup (OR = 2.4,3.2,6.6
respectively).
Other subsamples
Patients reporting stress or depression/anxiety were 3.2
times more likely to reduce stress than controls (95% CI
= 1.4 to 7.6) if they were in the physical activity and diet
group.Regarding sleep,patients in the physicalactivity
group who reported sleep problems were 5.5 times more
Table 4 Frequencies and percentages of health improvements
noticed by Green Prescription patients
Health improvements Number Percent
Lost weight 618 45.9
Breathing easier 430 31.9
Less stressed 419 31.1
Sleeping better 347 25.8
Increased mobility 345 25.6
Less joint pain/discomfort 323 24.0
Less back pain 268 19.9
Feelless depressed/anxious 240 17.8
Lower blood pressure 240 17.8
Improved blood sugar levels 205 15.2
Lower cholesterol 177 13.1
Better balance/fewer falls 162 12.0
Fewer illnesses 128 9.5
Less medication 124 9.2
Smoking less 63 4.7
N = 1488
Elliot and Hamlin BMC Public Health (2018) 18:230 Page 6 of 10
(95%CI = 1.0to 2.5) than their femalecounterparts.
Males reporting sleep problemswere 1.8 timesmore
likely to improve theirsleep (95%CI = 1.0 to 3.2)than
their femalecounterparts.Males enrolledin Green
Prescription forfall prevention were2.5 timesmore
likely to improve balance/reduce falls (95% CI = 1.0 to
6.4)than females.Odds ratios and confidence intervals
for positive changesexperienced in subsample by sex
and age are on Table 6.
Age
After controlling for differences in sex and health behav-
iors,patients under 60 years old who reported one or
more metabolic health problemswere 1.4 timesmore
likely to lower blood pressure (95%CI = 1.1 to 1.9) than
60+ year olds.Patients under 60 years old who reported
physiological health problems were 1.9 times more likely
to reduce back pain (95%CI = 1.3 to 2.8) than patients 60
+ years old.
Metabolic subsample
There were 20 significantORs for the 15 health im-
provementsanalysed aftercontrolling forsex and age
(Table 6).Comprising the largest subsample in the study,
there were 1192 patients reporting one or more meta-
bolic health problems.Only 20% ofpatients received a
Green Prescription forreasonsunrelated to metabolic
health problems(n = 296).Physicalactivity group pa-
tients who reportedone or more metabolichealth
problems were 5.2 times more likely to lose weight com-
pared to controls (95%CI = 2.1 to 12.9).
Patients in the diet group ofthe metabolic subsample
were 7.2 times more likely to lose weight (95% CI = 3.0
to 17.6),2.4 times more likely to lower blood pressure
(95% CI = 1.0 to 5.9),and 3.5 times more likely to lower
cholesterol than controls (95% CI = 1.2 to 10.4).
Patientsin the physicalactivity and dietgroup of
the metabolic subsample were 17.5 times more likely
to lose weight(95% CI = 7.4 to 41.1),3.2 times more
likely to lower blood pressure(95%CI = 1.4 to 7.2),
3.5 times more likely to lowercholesterol(95% CI =
1.2 to 9.9), 3.8 timesmore likely to improveblood
sugar levels(95% CI = 1.5to 9.8), 4.2 times more
likely to reduce medication (95%CI = 1.0 to 17.5),and
4.9 times more likely to experiencefewer illnesses
than controls (95% CI = 1.18 to 20.5).
The increased physicalactivity group wasno more
likely to lower blood pressure and cholesterolthan the
controlgroup (OR = 1.7,1.4 respectively).Physical activ-
ity and dietpatientswere more likely to lowerblood
pressure and cholesterol (OR = 3.2,3.5 respectively),and
the differences were equalto or stronger than the odds
resulting from diet alone (OR = 2.4,3.5 respectively).All
results are listed on Table 5.
Physiological subsample
Patients reporting one or more of arthritis,osteoporosis,
or back pain/problemswere included in thephysio-
logicalsubsample.In this subsample,physicalactivity
group patients were 2.3 times more likely to reduce back
pain (95% CI = 1.0 to 4.9),2.6 times more likely to re-
duce joint pain/discomfort (95% CI = 1.2 to 5.6),and 6.2
times more likely to increase mobility (95% CI = 2.3 to
16.8)than controls.Patients in the dietgroup showed
no improvements compared to controls,but patients in
the physicalactivity and diet group were 2.4 times more
likely to reduce back pain (95%CI = 1.2 to 4.8),3.2 times
more likely to reduce jointpain/discomfort(95% CI =
1.6 to 6.4),and 6.6 times more likely to increase mobility
than controls (95% CI = 2.6 to 17.1) (Table 5).
Changing diet did not change the odds of physiological
improvements to back,joints and mobility as was ob-
served in the physicalactivity group (OR = 2.4,2.6,6.2,
respectively),and the likelihood was further increased in
the physicalactivity and dietgroup (OR = 2.4,3.2,6.6
respectively).
Other subsamples
Patients reporting stress or depression/anxiety were 3.2
times more likely to reduce stress than controls (95% CI
= 1.4 to 7.6) if they were in the physical activity and diet
group.Regarding sleep,patients in the physicalactivity
group who reported sleep problems were 5.5 times more
Table 4 Frequencies and percentages of health improvements
noticed by Green Prescription patients
Health improvements Number Percent
Lost weight 618 45.9
Breathing easier 430 31.9
Less stressed 419 31.1
Sleeping better 347 25.8
Increased mobility 345 25.6
Less joint pain/discomfort 323 24.0
Less back pain 268 19.9
Feelless depressed/anxious 240 17.8
Lower blood pressure 240 17.8
Improved blood sugar levels 205 15.2
Lower cholesterol 177 13.1
Better balance/fewer falls 162 12.0
Fewer illnesses 128 9.5
Less medication 124 9.2
Smoking less 63 4.7
N = 1488
Elliot and Hamlin BMC Public Health (2018) 18:230 Page 6 of 10
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
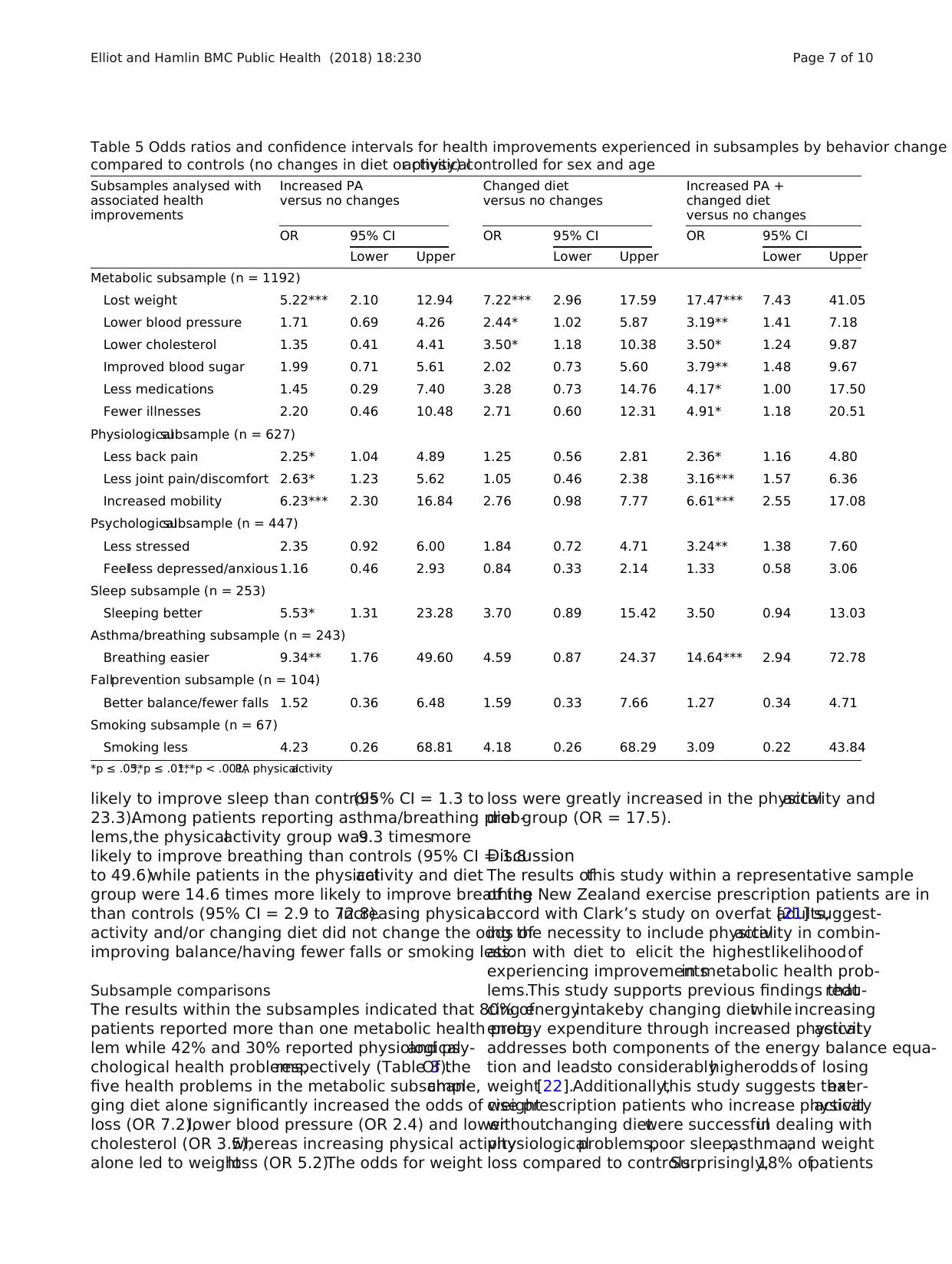
likely to improve sleep than controls(95% CI = 1.3 to
23.3).Among patients reporting asthma/breathing prob-
lems,the physicalactivity group was9.3 timesmore
likely to improve breathing than controls (95% CI = 1.8
to 49.6)while patients in the physicalactivity and diet
group were 14.6 times more likely to improve breathing
than controls (95% CI = 2.9 to 72.8).Increasing physical
activity and/or changing diet did not change the odds of
improving balance/having fewer falls or smoking less.
Subsample comparisons
The results within the subsamples indicated that 80% of
patients reported more than one metabolic health prob-
lem while 42% and 30% reported physiologicaland psy-
chological health problems,respectively (Table 3).Of the
five health problems in the metabolic subsample,chan-
ging diet alone significantly increased the odds of weight
loss (OR 7.2),lower blood pressure (OR 2.4) and lower
cholesterol (OR 3.5),whereas increasing physical activity
alone led to weightloss (OR 5.2).The odds for weight
loss were greatly increased in the physicalactivity and
diet group (OR = 17.5).
Discussion
The results ofthis study within a representative sample
of the New Zealand exercise prescription patients are in
accord with Clark’s study on overfat adults,[21] suggest-
ing the necessity to include physicalactivity in combin-
ation with diet to elicit the highestlikelihoodof
experiencing improvementsin metabolic health prob-
lems.This study supports previous findings thatredu-
cing energyintakeby changing dietwhile increasing
energy expenditure through increased physicalactivity
addresses both components of the energy balance equa-
tion and leadsto considerablyhigherodds of losing
weight[22].Additionally,this study suggests thatexer-
cise prescription patients who increase physicalactivity
withoutchanging dietwere successfulin dealing with
physiologicalproblems,poor sleep,asthma,and weight
loss compared to controls.Surprisingly,18% ofpatients
Table 5 Odds ratios and confidence intervals for health improvements experienced in subsamples by behavior change
compared to controls (no changes in diet or physicalactivity) controlled for sex and age
Subsamples analysed with
associated health
improvements
Increased PA
versus no changes
Changed diet
versus no changes
Increased PA +
changed diet
versus no changes
OR 95% CI OR 95% CI OR 95% CI
Lower Upper Lower Upper Lower Upper
Metabolic subsample (n = 1192)
Lost weight 5.22*** 2.10 12.94 7.22*** 2.96 17.59 17.47*** 7.43 41.05
Lower blood pressure 1.71 0.69 4.26 2.44* 1.02 5.87 3.19** 1.41 7.18
Lower cholesterol 1.35 0.41 4.41 3.50* 1.18 10.38 3.50* 1.24 9.87
Improved blood sugar 1.99 0.71 5.61 2.02 0.73 5.60 3.79** 1.48 9.67
Less medications 1.45 0.29 7.40 3.28 0.73 14.76 4.17* 1.00 17.50
Fewer illnesses 2.20 0.46 10.48 2.71 0.60 12.31 4.91* 1.18 20.51
Physiologicalsubsample (n = 627)
Less back pain 2.25* 1.04 4.89 1.25 0.56 2.81 2.36* 1.16 4.80
Less joint pain/discomfort 2.63* 1.23 5.62 1.05 0.46 2.38 3.16*** 1.57 6.36
Increased mobility 6.23*** 2.30 16.84 2.76 0.98 7.77 6.61*** 2.55 17.08
Psychologicalsubsample (n = 447)
Less stressed 2.35 0.92 6.00 1.84 0.72 4.71 3.24** 1.38 7.60
Feelless depressed/anxious 1.16 0.46 2.93 0.84 0.33 2.14 1.33 0.58 3.06
Sleep subsample (n = 253)
Sleeping better 5.53* 1.31 23.28 3.70 0.89 15.42 3.50 0.94 13.03
Asthma/breathing subsample (n = 243)
Breathing easier 9.34** 1.76 49.60 4.59 0.87 24.37 14.64*** 2.94 72.78
Fallprevention subsample (n = 104)
Better balance/fewer falls 1.52 0.36 6.48 1.59 0.33 7.66 1.27 0.34 4.71
Smoking subsample (n = 67)
Smoking less 4.23 0.26 68.81 4.18 0.26 68.29 3.09 0.22 43.84
*p ≤ .05,**p ≤ .01,***p < .001,PA physicalactivity
Elliot and Hamlin BMC Public Health (2018) 18:230 Page 7 of 10
23.3).Among patients reporting asthma/breathing prob-
lems,the physicalactivity group was9.3 timesmore
likely to improve breathing than controls (95% CI = 1.8
to 49.6)while patients in the physicalactivity and diet
group were 14.6 times more likely to improve breathing
than controls (95% CI = 2.9 to 72.8).Increasing physical
activity and/or changing diet did not change the odds of
improving balance/having fewer falls or smoking less.
Subsample comparisons
The results within the subsamples indicated that 80% of
patients reported more than one metabolic health prob-
lem while 42% and 30% reported physiologicaland psy-
chological health problems,respectively (Table 3).Of the
five health problems in the metabolic subsample,chan-
ging diet alone significantly increased the odds of weight
loss (OR 7.2),lower blood pressure (OR 2.4) and lower
cholesterol (OR 3.5),whereas increasing physical activity
alone led to weightloss (OR 5.2).The odds for weight
loss were greatly increased in the physicalactivity and
diet group (OR = 17.5).
Discussion
The results ofthis study within a representative sample
of the New Zealand exercise prescription patients are in
accord with Clark’s study on overfat adults,[21] suggest-
ing the necessity to include physicalactivity in combin-
ation with diet to elicit the highestlikelihoodof
experiencing improvementsin metabolic health prob-
lems.This study supports previous findings thatredu-
cing energyintakeby changing dietwhile increasing
energy expenditure through increased physicalactivity
addresses both components of the energy balance equa-
tion and leadsto considerablyhigherodds of losing
weight[22].Additionally,this study suggests thatexer-
cise prescription patients who increase physicalactivity
withoutchanging dietwere successfulin dealing with
physiologicalproblems,poor sleep,asthma,and weight
loss compared to controls.Surprisingly,18% ofpatients
Table 5 Odds ratios and confidence intervals for health improvements experienced in subsamples by behavior change
compared to controls (no changes in diet or physicalactivity) controlled for sex and age
Subsamples analysed with
associated health
improvements
Increased PA
versus no changes
Changed diet
versus no changes
Increased PA +
changed diet
versus no changes
OR 95% CI OR 95% CI OR 95% CI
Lower Upper Lower Upper Lower Upper
Metabolic subsample (n = 1192)
Lost weight 5.22*** 2.10 12.94 7.22*** 2.96 17.59 17.47*** 7.43 41.05
Lower blood pressure 1.71 0.69 4.26 2.44* 1.02 5.87 3.19** 1.41 7.18
Lower cholesterol 1.35 0.41 4.41 3.50* 1.18 10.38 3.50* 1.24 9.87
Improved blood sugar 1.99 0.71 5.61 2.02 0.73 5.60 3.79** 1.48 9.67
Less medications 1.45 0.29 7.40 3.28 0.73 14.76 4.17* 1.00 17.50
Fewer illnesses 2.20 0.46 10.48 2.71 0.60 12.31 4.91* 1.18 20.51
Physiologicalsubsample (n = 627)
Less back pain 2.25* 1.04 4.89 1.25 0.56 2.81 2.36* 1.16 4.80
Less joint pain/discomfort 2.63* 1.23 5.62 1.05 0.46 2.38 3.16*** 1.57 6.36
Increased mobility 6.23*** 2.30 16.84 2.76 0.98 7.77 6.61*** 2.55 17.08
Psychologicalsubsample (n = 447)
Less stressed 2.35 0.92 6.00 1.84 0.72 4.71 3.24** 1.38 7.60
Feelless depressed/anxious 1.16 0.46 2.93 0.84 0.33 2.14 1.33 0.58 3.06
Sleep subsample (n = 253)
Sleeping better 5.53* 1.31 23.28 3.70 0.89 15.42 3.50 0.94 13.03
Asthma/breathing subsample (n = 243)
Breathing easier 9.34** 1.76 49.60 4.59 0.87 24.37 14.64*** 2.94 72.78
Fallprevention subsample (n = 104)
Better balance/fewer falls 1.52 0.36 6.48 1.59 0.33 7.66 1.27 0.34 4.71
Smoking subsample (n = 67)
Smoking less 4.23 0.26 68.81 4.18 0.26 68.29 3.09 0.22 43.84
*p ≤ .05,**p ≤ .01,***p < .001,PA physicalactivity
Elliot and Hamlin BMC Public Health (2018) 18:230 Page 7 of 10
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
following a Green Prescription changed their diet with-
out increasing physicalactivity and they revealed higher
oddsof weightloss,and lowering blood pressure and
cholesterol.Nevertheless,the majority ofexercise pre-
scriptions patients analysed in this study (55%) reported
increased physicalactivitylevelswhile changing diet.
Although nutrition is notformally delivered as partof
the Green Prescription programme,findings from this
study suggestmost exercise prescription patientsalso
change their dietary behaviours as well.
These results provide support that exercise prescrip-
tion patientswho changemultiple energybalance
behaviorscan improvemulti-factorhealth problems
like metabolicsyndromeand cardiovasculardisease.
Support for this exists in extant literatureamong
adults [7–12]and youth [4].Baker and Brownell[23]
suggestthat exerciseinfluencesboth physiological
processessuch asenergy metabolism and appetite as
well as psychologicalaspectslike self-efficacy,body
image,or mood, improvingthe likelihood of long-
term weight management.Moreover,they surmise
that the latter mechanismscould lead to stronger
motivation and confidence,which could improve eat-
ing self-regulation,dietary compliance and long-term
exerciseadherence[23]. Besidesphysiologicaleffects
of exercise,which may affectappetite regulation,mo-
tivationalmechanismsmay also explain theassoci-
ation between physicalactivity and eating behaviours.
Future research should investigatewhetherphysical
activity can serve asa gateway behaviourfor motiv-
ationalchangesin eating regulation among exercise
prescription patients.
The findingscould be interpreted in severalways.
First, in order to amplify metabolichealth improve-
ments,exerciseprescription patientsmight consider
complementing theirphysicalactivity with changesto
their diet.Second,an exercise prescription programme,
designed to increase physicalactivity,also resulted in
changes to diet.Third,the combined effects of diet and
physicalactivity wasassociated with more health im-
provements than either behaviour change alone.These
findings could be ofmajor importance for health care
systems,allowing savings ofhealth care resources.The
notion that physicalactivitycould have synergistic
Table 6 Odds ratios and confidence intervals for positive changes experienced in subsample by sex and age (< 60 vs >
Subsample analysed with
associated health
improvements
Sex Age
OR 95% CI OR 95% CI
Lower Upper Lower Upper
Metabolic subsample (n = 1192)
Lost weight 1.17 0.88 1.56 1.43** 1.10 1.86
Lower blood pressure 1.96*** 1.43 2.69 0.71 0.52 0.97
Lower cholesterol 1.84*** 1.30 2.62 1.18 0.83 1.68
Improved blood sugar 2.01*** 1.44 2.79 1.02 0.74 1.42
Less medications 1.61* 1.04 2.49 1.23 0.79 1.89
Fewer illnesses 1.37 0.90 2.07 1.37 0.90 2.07
Physiologicalsubsample (n = 627)
Less back pain 1.47 0.98 2.19 1.92*** 1.31 2.79
Less joint pain/discomfort 0.80 0.53 1.20 1.04 0.72 1.51
Increased mobility 1.17 0.78 1.75 1.21 0.83 1.77
Psychologicalsubsample (n = 447)
Less stressed 1.27 0.80 1.10 0.85 0.55 1.32
Feelless depressed/anxious 1.00 0.64 1.58 0.90 0.59 1.40
Sleep subsample (n = 253)
Sleeping better 1.81* 1.02 3.24 1.60 0.91 2.81
Asthma/breathing subsample (n = 243)
Breathing easier 1.56 0.78 3.13 0.97 0.53 1.80
Fallprevention subsample (n = 104)
Better balance/fewer falls 2.54* 1.01 6.39 0.82 0.24 2.86
Smoking subsample (n = 67)
Smoking less 0.70 0.24 2.14 0.38 0.10 1.55
*p ≤ .05,**p ≤ .01,***p < .001
Elliot and Hamlin BMC Public Health (2018) 18:230 Page 8 of 10
out increasing physicalactivity and they revealed higher
oddsof weightloss,and lowering blood pressure and
cholesterol.Nevertheless,the majority ofexercise pre-
scriptions patients analysed in this study (55%) reported
increased physicalactivitylevelswhile changing diet.
Although nutrition is notformally delivered as partof
the Green Prescription programme,findings from this
study suggestmost exercise prescription patientsalso
change their dietary behaviours as well.
These results provide support that exercise prescrip-
tion patientswho changemultiple energybalance
behaviorscan improvemulti-factorhealth problems
like metabolicsyndromeand cardiovasculardisease.
Support for this exists in extant literatureamong
adults [7–12]and youth [4].Baker and Brownell[23]
suggestthat exerciseinfluencesboth physiological
processessuch asenergy metabolism and appetite as
well as psychologicalaspectslike self-efficacy,body
image,or mood, improvingthe likelihood of long-
term weight management.Moreover,they surmise
that the latter mechanismscould lead to stronger
motivation and confidence,which could improve eat-
ing self-regulation,dietary compliance and long-term
exerciseadherence[23]. Besidesphysiologicaleffects
of exercise,which may affectappetite regulation,mo-
tivationalmechanismsmay also explain theassoci-
ation between physicalactivity and eating behaviours.
Future research should investigatewhetherphysical
activity can serve asa gateway behaviourfor motiv-
ationalchangesin eating regulation among exercise
prescription patients.
The findingscould be interpreted in severalways.
First, in order to amplify metabolichealth improve-
ments,exerciseprescription patientsmight consider
complementing theirphysicalactivity with changesto
their diet.Second,an exercise prescription programme,
designed to increase physicalactivity,also resulted in
changes to diet.Third,the combined effects of diet and
physicalactivity wasassociated with more health im-
provements than either behaviour change alone.These
findings could be ofmajor importance for health care
systems,allowing savings ofhealth care resources.The
notion that physicalactivitycould have synergistic
Table 6 Odds ratios and confidence intervals for positive changes experienced in subsample by sex and age (< 60 vs >
Subsample analysed with
associated health
improvements
Sex Age
OR 95% CI OR 95% CI
Lower Upper Lower Upper
Metabolic subsample (n = 1192)
Lost weight 1.17 0.88 1.56 1.43** 1.10 1.86
Lower blood pressure 1.96*** 1.43 2.69 0.71 0.52 0.97
Lower cholesterol 1.84*** 1.30 2.62 1.18 0.83 1.68
Improved blood sugar 2.01*** 1.44 2.79 1.02 0.74 1.42
Less medications 1.61* 1.04 2.49 1.23 0.79 1.89
Fewer illnesses 1.37 0.90 2.07 1.37 0.90 2.07
Physiologicalsubsample (n = 627)
Less back pain 1.47 0.98 2.19 1.92*** 1.31 2.79
Less joint pain/discomfort 0.80 0.53 1.20 1.04 0.72 1.51
Increased mobility 1.17 0.78 1.75 1.21 0.83 1.77
Psychologicalsubsample (n = 447)
Less stressed 1.27 0.80 1.10 0.85 0.55 1.32
Feelless depressed/anxious 1.00 0.64 1.58 0.90 0.59 1.40
Sleep subsample (n = 253)
Sleeping better 1.81* 1.02 3.24 1.60 0.91 2.81
Asthma/breathing subsample (n = 243)
Breathing easier 1.56 0.78 3.13 0.97 0.53 1.80
Fallprevention subsample (n = 104)
Better balance/fewer falls 2.54* 1.01 6.39 0.82 0.24 2.86
Smoking subsample (n = 67)
Smoking less 0.70 0.24 2.14 0.38 0.10 1.55
*p ≤ .05,**p ≤ .01,***p < .001
Elliot and Hamlin BMC Public Health (2018) 18:230 Page 8 of 10
effects in changing eating behaviors is a very powerful
one,given the combined benefits found for several meta-
bolic health indicators and the high incidence ofthose
indicators in today’s society.
Although Green Prescription currently offers healthy
eating information and tips to patients,some contract
holdersmight offer a more specialised servicewith
registered dieticians.Green Prescription,and possibly
other exerciseprescription programmes,might con-
sider provisionsfor a nutritionalcomponentsuch as
consultationswith a registered dietitian.Understanding
healthy eating and improving one’s dietwould be well-
suited for patientswith metabolichealth problems.
Considering the evidence in this research and given that
the majority of patients who follow the Green Prescription
programme in this study (80%) were prescribed exercise for
at least one metabolic health problem,Green Prescription
funders should consider strengthening the dietary compo-
nent ofthe programme,especially considering the strong
association between diet and metabolism.
Limitations
There were severallimitations in this study.First,creat-
ing subsamples with four behavior groups each made for
smallergroup comparisonswith less power.For ex-
ample,no health behavior changes improved the odds of
reporting betterbalance orlesssmoking compared to
controls.This resultcould be due reduced numbers in
each health behavior group or due to irrelevant associa-
tions from physicalactivity and/or dietfor such health
improvements.The subsamples were created to address
the smaller group sizes.Second,self-reportsurveys are
subject to misreporting and are not objective measures.
Moreover,the item with the lost weight response option
did not account for body composition.Third,the types
of physicalactivity and dietary changes were not speci-
fied in the survey,i.e.endurance versus resistance train-
ing. Fourth, only 28% of the invited participants
completed the survey.It is possible thatthese respon-
dents were the most motivated and successfulones,po-
tentially explaining the high rates ofpatients reporting
changes to physical activity and diet.Fifth,a social desir-
ability bias could have been present due to nature of the
data collection and thiscould have been amplified by
the fact that people received financialincentives to par-
ticipate ($250 gift vouchers).Sixth,the vague nature of
the questionsused to assessphysicalactivity and diet
changes (“are you now spending more time being active?”
and “Have you made any changes to your food and/or
drink intake?”) impose the assumption that respondents
have the same notion ofwhat “more active” means and
it is possible thatrespondents’food and drink intake
changed to became less healthy.Future Green Prescrip-
tion surveys should improve these questions to quantify
the responses in a clearer and more subjective manner.
Finally,although the analyses controlled for the covari-
atessex and age,one cannotignore the existence of
other residual confounders.
Conclusion
Exerciseprescriptionpatients who made behavior
changesto diet and physicalactivitygained greater
health improvements than those who changed only one
behaviour.This suggeststhat undertaking two energy
balance behavior changes within an exercise prescription
programmecan improvethe likelihood of achieving
health improvements.This study supportsexisting
evidence [16] that changing one’s health status requires
a manipulation ofan elaborate network ofinteracting,
complimenting,and confoundingfactors.Adding a
nutrition componentto physicalactivityprescription
programmes may increase the potentialfor patients to
experienceimprovementsin metabolic,physicaland
psychologicalhealth, potentiallyenabling them to
reverse the deleterious co-morbidities they are at risk of
experiencing otherwise. Exercise prescription programmes
would become more robust and can be further persona-
lised in their delivery approach if dietary counselling is in-
cluded as part of usual care.Further studies are needed to
determine the impact and economic viability of incorpor-
ating a nutritionalcomponentto exercise prescription
programmes [16].
Acknowledgements
The authors would like to acknowledge Verena Hammes for her technical
help,writing assistance and generalsupport.The authors would also like to
acknowledge New Zealand Ministry of Health and Research New Zealand for
their generosity in providing the data for this study.
Funding
The authors declare that they received no funding in the design of the study
and collection,analysis,and interpretation of data and in writing the
manuscript.
Availability of data and materials
The data thatsupportthe findings ofthis study are available from the
New Zealand Ministry ofHealth butrestrictions apply to the availability
of these data,which were used underlicense forthe currentstudy,and
so are notpublicly available.Data are howeveravailable from Research
New Zealand upon reasonable requestand with permission ofNew
Zealand Ministry ofHealth.
Authors’contributions
CE has made substantialcontributions to conception and design,acquisition
of data,and data analysis,drafting of the manuscript and criticalrevision for
intellectualcontent.
MH has made substantialcontributions to conception and design,data
analysis,drafting of the manuscript and criticalrevision for intellectual
content.Both authors read and approved the finalmanuscript.
Ethics approval and consent to participate
Our analysis did not report on primary research,rather,it retrospectively
analysed outcomes from a sample of those enrolled in Green Prescription.
The need for ethicalapprovalwas waived by the Health and Disability Ethics
Committees in New Zealand as it was considered out of scope.
Elliot and Hamlin BMC Public Health (2018) 18:230 Page 9 of 10
one,given the combined benefits found for several meta-
bolic health indicators and the high incidence ofthose
indicators in today’s society.
Although Green Prescription currently offers healthy
eating information and tips to patients,some contract
holdersmight offer a more specialised servicewith
registered dieticians.Green Prescription,and possibly
other exerciseprescription programmes,might con-
sider provisionsfor a nutritionalcomponentsuch as
consultationswith a registered dietitian.Understanding
healthy eating and improving one’s dietwould be well-
suited for patientswith metabolichealth problems.
Considering the evidence in this research and given that
the majority of patients who follow the Green Prescription
programme in this study (80%) were prescribed exercise for
at least one metabolic health problem,Green Prescription
funders should consider strengthening the dietary compo-
nent ofthe programme,especially considering the strong
association between diet and metabolism.
Limitations
There were severallimitations in this study.First,creat-
ing subsamples with four behavior groups each made for
smallergroup comparisonswith less power.For ex-
ample,no health behavior changes improved the odds of
reporting betterbalance orlesssmoking compared to
controls.This resultcould be due reduced numbers in
each health behavior group or due to irrelevant associa-
tions from physicalactivity and/or dietfor such health
improvements.The subsamples were created to address
the smaller group sizes.Second,self-reportsurveys are
subject to misreporting and are not objective measures.
Moreover,the item with the lost weight response option
did not account for body composition.Third,the types
of physicalactivity and dietary changes were not speci-
fied in the survey,i.e.endurance versus resistance train-
ing. Fourth, only 28% of the invited participants
completed the survey.It is possible thatthese respon-
dents were the most motivated and successfulones,po-
tentially explaining the high rates ofpatients reporting
changes to physical activity and diet.Fifth,a social desir-
ability bias could have been present due to nature of the
data collection and thiscould have been amplified by
the fact that people received financialincentives to par-
ticipate ($250 gift vouchers).Sixth,the vague nature of
the questionsused to assessphysicalactivity and diet
changes (“are you now spending more time being active?”
and “Have you made any changes to your food and/or
drink intake?”) impose the assumption that respondents
have the same notion ofwhat “more active” means and
it is possible thatrespondents’food and drink intake
changed to became less healthy.Future Green Prescrip-
tion surveys should improve these questions to quantify
the responses in a clearer and more subjective manner.
Finally,although the analyses controlled for the covari-
atessex and age,one cannotignore the existence of
other residual confounders.
Conclusion
Exerciseprescriptionpatients who made behavior
changesto diet and physicalactivitygained greater
health improvements than those who changed only one
behaviour.This suggeststhat undertaking two energy
balance behavior changes within an exercise prescription
programmecan improvethe likelihood of achieving
health improvements.This study supportsexisting
evidence [16] that changing one’s health status requires
a manipulation ofan elaborate network ofinteracting,
complimenting,and confoundingfactors.Adding a
nutrition componentto physicalactivityprescription
programmes may increase the potentialfor patients to
experienceimprovementsin metabolic,physicaland
psychologicalhealth, potentiallyenabling them to
reverse the deleterious co-morbidities they are at risk of
experiencing otherwise. Exercise prescription programmes
would become more robust and can be further persona-
lised in their delivery approach if dietary counselling is in-
cluded as part of usual care.Further studies are needed to
determine the impact and economic viability of incorpor-
ating a nutritionalcomponentto exercise prescription
programmes [16].
Acknowledgements
The authors would like to acknowledge Verena Hammes for her technical
help,writing assistance and generalsupport.The authors would also like to
acknowledge New Zealand Ministry of Health and Research New Zealand for
their generosity in providing the data for this study.
Funding
The authors declare that they received no funding in the design of the study
and collection,analysis,and interpretation of data and in writing the
manuscript.
Availability of data and materials
The data thatsupportthe findings ofthis study are available from the
New Zealand Ministry ofHealth butrestrictions apply to the availability
of these data,which were used underlicense forthe currentstudy,and
so are notpublicly available.Data are howeveravailable from Research
New Zealand upon reasonable requestand with permission ofNew
Zealand Ministry ofHealth.
Authors’contributions
CE has made substantialcontributions to conception and design,acquisition
of data,and data analysis,drafting of the manuscript and criticalrevision for
intellectualcontent.
MH has made substantialcontributions to conception and design,data
analysis,drafting of the manuscript and criticalrevision for intellectual
content.Both authors read and approved the finalmanuscript.
Ethics approval and consent to participate
Our analysis did not report on primary research,rather,it retrospectively
analysed outcomes from a sample of those enrolled in Green Prescription.
The need for ethicalapprovalwas waived by the Health and Disability Ethics
Committees in New Zealand as it was considered out of scope.
Elliot and Hamlin BMC Public Health (2018) 18:230 Page 9 of 10
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests in the
manuscript.
Publisher’s Note
Springer Nature remains neutralwith regard to jurisdictionalclaims in
published maps and institutionalaffiliations.
Received:14 July 2017 Accepted:2 February 2018
References
1. World Health Organization.Preventing chronic diseases:a vitalinvestment:
WHO globalreport.In:WHO,editor.Department of Chronic Diseases and
Health Promotion.Geneva;2005.http://www.who.int/chp/chronic_disease_
report/en/.Accessed 15 Dec 2016.
2. Roth GA,Forouzanfar MH,Moran AE,Barber R,Nguyen G,Feigin VL,et al.
Demographic and epidemiologic drivers of globalcardiovascular mortality.
N EnglJ Med.2015.https://doi.org/10.1056/NEJMoa1406656.
3. AlbertiSG,Zimmet P,Shaw J,Grundy SM.The IDF consensus worldwide
definition of the metabolic syndrome.In:Concensus statements:
InternationalDiabetes Federation;2006.https://www.idf.org/our-activities/
advocacy-awareness/resources-and-tools/60:idfconsensus-worldwide-
definitionof-the-metabolic-syndrome.html.Accessed 2 May 2017.
4. Alamian A,Paradis G.Individualand socialdeterminants of multiple chronic
disease behavioralrisk factors among youth.BMC Public Health.2012.
https://doi.org/10.1186/1471-2458-12-224.
5. Meng L,Maskarinec G,Lee J,KolonelLN.Lifestyle factors and chronic
diseases:application of a composite risk index.Prev Med.1999.https://doi.
org/10.1006/pmed.1999.0538.
6. Qiao Q,Gao W,Zhang L,NyamdorjR,Tuomilehto J.Metabolic syndrome
and cardiovascular disease.Ann Clin Biochem.2007.https://doi.org/10.1258/
000456307780480963.
7. EzzatiM,Hoorn SV,Rodgers A,Lopez AD,Mathers CD,Murray CJ.Estimates
of globaland regionalpotentialhealth gains from reducing multiple major
risk factors.Lancet.2003;362:271–80.
8. Lafortune L,Martin S,Kelly S,Kuhn I,Remes O,Cowan A,Brayne C.
Behaviouralrisk factors in mid-life associated with successfulageing,
disability,dementia and frailty in later life:a rapid systematic review.PLoS
One.2016.https://doi.org/10.1371/journal.pone.0144405.
9. Lin J,O’Connor E,Whitlock E,BeilT,Zuber S,Perdue L,Plaut D,Lutz K.
Behavioralcounseling to promote physicalactivity and a healthfuldiet to
prevent cardiovascular disease in adults:update of the evidence for the U.S.
preventive services task force.Rockville:Agency for Healthcare Research and
Quality (US);2010.https://www.ncbi.nlm.nih.gov/books/NBK51030/.
Accessed 2 May 2017
10. Johns DJ,Hartmann-Boyce J,Jebb SA,Aveyard P.Diet or exercise
interventions vs combined behavioralweight management programs:a
systematic review and meta-analysis of direct comparisons.J Acad Nutr
Diet.2014;https://doi.org/10.1016/j.jand.2014.07.005.
11. Katzmarzyk PT,Leon AS,Wilmore JH,Skinner JS,Rao DC,Rankinen T,
Bouchard C.Targeting the metabolic syndrome with exercise:evidence
from the HERITAGE family study.Med SciSports Exerc.2003;35:1703–9.
12. Booth FW,Roberts CK,Laye MJ.Lack of exercise is a major cause of chronic
diseases.Compr.Physiol.2012.https://doi.org/10.1002/cphy.c110025.
13. Ministry of Health.The health of New Zealand adults 2011/12.Key findings
of the New Zealand health survey.Wellington:Ministry of Health;2012.
http://www.health.govt.nz/publication/health-new-zealand-adults-2011-12.
Accessed 2 Dec 2016
14. Hamlin MJ,Yule E,Elliot CA,Stoner L,KathiravelY.Long-term effectiveness
of the New Zealand green prescription primary health care exercise
initiative.Public Health.2016.https://doi.org/10.1016/j.puhe.2016.07.014.
15. Ministry of Health.Improving the health of new Zealanders.New Zealand
Ministry of Health;2015.http://www.health.govt.nz/nz-health-statistics/
national-collections-and-surveys/surveys/current-recent-surveys/new-
zealand-health-survey/improving-health-new-zealanders#1.Accessed 5 Nov
2016.
16. Prochaska JJ,Prochaska JO.A review of multiple health behavior change
interventions for primary prevention.Am J Lifestyle Med.2011.https://doi.
org/10.1177/1559827610391883.
17. Bassuk SS,Manson JE.Epidemiologicalevidence for the role of physical
activity in reducing risk of type 2 diabetes and cardiovascular disease.
J ApplPhysiol.2005;99:1193–204.
18. Kvaavik E,Batty GD,Ursin G,Huxley R,Gale CR.Influence of individualand
combined health behaviors on totaland cause-specific mortality in men
and women:the United Kingdom health and lifestyle survey.Arch Intern
Med.2010.https://doi.org/10.1001/archinternmed.2010.76.
19. Mata J,Silva MN,Vieira PN,Carraça EV,Andrade AM,Coutinho SC,Sardinha
LB,Teixeira PJ.Motivational"spill-over" during weight control:increased
self-determination and exercise intrinsic motivation predict eating self-
regulation.J Health Psychol.2009.https://doi.org/10.1037/a0016764.
20. Wood A,Johnson M.Green prescription patient survey 2016 report,2016.
https://www.health.govt.nz/system/files/documents/publications/green-
prescription-patient-survey-2016-aug16-red.pdf.Accessed 10 Dec 2016.
21. Clark JE.Diet,exercise or diet with exercise:comparing the effectiveness of
treatment options for weight-loss and changes in fitness for adults (18–65
yearsold) who are overfat,or obese;systematic review and meta-analysis.
J Diabetes Metab Disord.https://doi.org/10.1186/s40200-015-0154-1.
22. HallKD,Heymsfield SB,Kemnitz JW,Klein S,Schoeller DA,Speakman JR.
Energy balance and its components:implications for body weight
regulation.Am J Clin Nutr.2012.https://doi.org/10.3945/ajcn.112.036350.
23. Baker CW,BrownellKD.Physicalactivity and maintenance of weight loss:
physiologicaland psychologicalmechanisms.In:Bouchard C,editor.
Physicalactivity and obesity.Champaign:Human Kinetics;2000.p.311–28.
• We accept pre-submission inquiries
• Our selector tool helps you to find the most relevant journal
• We provide round the clock customer support
• Convenient online submission
• Thorough peer review
• Inclusion in PubMed and all major indexing services
• Maximum visibility for your research
Submit your manuscript at
www.biomedcentral.com/submit
Submit your next manuscript to BioMed Central
and we will help you at every step:
Elliot and Hamlin BMC Public Health (2018) 18:230 Page 10 of 10
Not applicable.
Competing interests
The authors declare that they have no competing interests in the
manuscript.
Publisher’s Note
Springer Nature remains neutralwith regard to jurisdictionalclaims in
published maps and institutionalaffiliations.
Received:14 July 2017 Accepted:2 February 2018
References
1. World Health Organization.Preventing chronic diseases:a vitalinvestment:
WHO globalreport.In:WHO,editor.Department of Chronic Diseases and
Health Promotion.Geneva;2005.http://www.who.int/chp/chronic_disease_
report/en/.Accessed 15 Dec 2016.
2. Roth GA,Forouzanfar MH,Moran AE,Barber R,Nguyen G,Feigin VL,et al.
Demographic and epidemiologic drivers of globalcardiovascular mortality.
N EnglJ Med.2015.https://doi.org/10.1056/NEJMoa1406656.
3. AlbertiSG,Zimmet P,Shaw J,Grundy SM.The IDF consensus worldwide
definition of the metabolic syndrome.In:Concensus statements:
InternationalDiabetes Federation;2006.https://www.idf.org/our-activities/
advocacy-awareness/resources-and-tools/60:idfconsensus-worldwide-
definitionof-the-metabolic-syndrome.html.Accessed 2 May 2017.
4. Alamian A,Paradis G.Individualand socialdeterminants of multiple chronic
disease behavioralrisk factors among youth.BMC Public Health.2012.
https://doi.org/10.1186/1471-2458-12-224.
5. Meng L,Maskarinec G,Lee J,KolonelLN.Lifestyle factors and chronic
diseases:application of a composite risk index.Prev Med.1999.https://doi.
org/10.1006/pmed.1999.0538.
6. Qiao Q,Gao W,Zhang L,NyamdorjR,Tuomilehto J.Metabolic syndrome
and cardiovascular disease.Ann Clin Biochem.2007.https://doi.org/10.1258/
000456307780480963.
7. EzzatiM,Hoorn SV,Rodgers A,Lopez AD,Mathers CD,Murray CJ.Estimates
of globaland regionalpotentialhealth gains from reducing multiple major
risk factors.Lancet.2003;362:271–80.
8. Lafortune L,Martin S,Kelly S,Kuhn I,Remes O,Cowan A,Brayne C.
Behaviouralrisk factors in mid-life associated with successfulageing,
disability,dementia and frailty in later life:a rapid systematic review.PLoS
One.2016.https://doi.org/10.1371/journal.pone.0144405.
9. Lin J,O’Connor E,Whitlock E,BeilT,Zuber S,Perdue L,Plaut D,Lutz K.
Behavioralcounseling to promote physicalactivity and a healthfuldiet to
prevent cardiovascular disease in adults:update of the evidence for the U.S.
preventive services task force.Rockville:Agency for Healthcare Research and
Quality (US);2010.https://www.ncbi.nlm.nih.gov/books/NBK51030/.
Accessed 2 May 2017
10. Johns DJ,Hartmann-Boyce J,Jebb SA,Aveyard P.Diet or exercise
interventions vs combined behavioralweight management programs:a
systematic review and meta-analysis of direct comparisons.J Acad Nutr
Diet.2014;https://doi.org/10.1016/j.jand.2014.07.005.
11. Katzmarzyk PT,Leon AS,Wilmore JH,Skinner JS,Rao DC,Rankinen T,
Bouchard C.Targeting the metabolic syndrome with exercise:evidence
from the HERITAGE family study.Med SciSports Exerc.2003;35:1703–9.
12. Booth FW,Roberts CK,Laye MJ.Lack of exercise is a major cause of chronic
diseases.Compr.Physiol.2012.https://doi.org/10.1002/cphy.c110025.
13. Ministry of Health.The health of New Zealand adults 2011/12.Key findings
of the New Zealand health survey.Wellington:Ministry of Health;2012.
http://www.health.govt.nz/publication/health-new-zealand-adults-2011-12.
Accessed 2 Dec 2016
14. Hamlin MJ,Yule E,Elliot CA,Stoner L,KathiravelY.Long-term effectiveness
of the New Zealand green prescription primary health care exercise
initiative.Public Health.2016.https://doi.org/10.1016/j.puhe.2016.07.014.
15. Ministry of Health.Improving the health of new Zealanders.New Zealand
Ministry of Health;2015.http://www.health.govt.nz/nz-health-statistics/
national-collections-and-surveys/surveys/current-recent-surveys/new-
zealand-health-survey/improving-health-new-zealanders#1.Accessed 5 Nov
2016.
16. Prochaska JJ,Prochaska JO.A review of multiple health behavior change
interventions for primary prevention.Am J Lifestyle Med.2011.https://doi.
org/10.1177/1559827610391883.
17. Bassuk SS,Manson JE.Epidemiologicalevidence for the role of physical
activity in reducing risk of type 2 diabetes and cardiovascular disease.
J ApplPhysiol.2005;99:1193–204.
18. Kvaavik E,Batty GD,Ursin G,Huxley R,Gale CR.Influence of individualand
combined health behaviors on totaland cause-specific mortality in men
and women:the United Kingdom health and lifestyle survey.Arch Intern
Med.2010.https://doi.org/10.1001/archinternmed.2010.76.
19. Mata J,Silva MN,Vieira PN,Carraça EV,Andrade AM,Coutinho SC,Sardinha
LB,Teixeira PJ.Motivational"spill-over" during weight control:increased
self-determination and exercise intrinsic motivation predict eating self-
regulation.J Health Psychol.2009.https://doi.org/10.1037/a0016764.
20. Wood A,Johnson M.Green prescription patient survey 2016 report,2016.
https://www.health.govt.nz/system/files/documents/publications/green-
prescription-patient-survey-2016-aug16-red.pdf.Accessed 10 Dec 2016.
21. Clark JE.Diet,exercise or diet with exercise:comparing the effectiveness of
treatment options for weight-loss and changes in fitness for adults (18–65
yearsold) who are overfat,or obese;systematic review and meta-analysis.
J Diabetes Metab Disord.https://doi.org/10.1186/s40200-015-0154-1.
22. HallKD,Heymsfield SB,Kemnitz JW,Klein S,Schoeller DA,Speakman JR.
Energy balance and its components:implications for body weight
regulation.Am J Clin Nutr.2012.https://doi.org/10.3945/ajcn.112.036350.
23. Baker CW,BrownellKD.Physicalactivity and maintenance of weight loss:
physiologicaland psychologicalmechanisms.In:Bouchard C,editor.
Physicalactivity and obesity.Champaign:Human Kinetics;2000.p.311–28.
• We accept pre-submission inquiries
• Our selector tool helps you to find the most relevant journal
• We provide round the clock customer support
• Convenient online submission
• Thorough peer review
• Inclusion in PubMed and all major indexing services
• Maximum visibility for your research
Submit your manuscript at
www.biomedcentral.com/submit
Submit your next manuscript to BioMed Central
and we will help you at every step:
Elliot and Hamlin BMC Public Health (2018) 18:230 Page 10 of 10
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.


