Emergency Nursing 12: Pediatric Case Study Report and Analysis
VerifiedAdded on 2021/05/31
|14
|3967
|46
Report
AI Summary
This report presents a comprehensive analysis of a pediatric emergency nursing case, addressing key aspects of patient care and management. The report begins with an interpretation of a 12-lead ECG, followed by the identification of abnormal findings, including potential rheumatic heart disease, and a discussion of relevant biomarkers such as Antistreptolysin O, NT-proBNP, C-reactive protein, and Troponin I. The analysis delves into the pathophysiology of the patient's condition, linking clinical observations to underlying mechanisms. The report also outlines the initial management strategies for the patient, emphasizing the importance of close monitoring, hemodynamic stabilization, and nursing interventions. The content covers important medical concepts in the context of emergency nursing care. The report is designed to assist students in understanding and applying their knowledge in a practical setting. The patient requires one on one nursing management in the emergency department. The continuous patient monitoring including the signs and symptoms as a result of the hemodynamic status and treatment requires close observation of the hemodynamic parameters that include assessing the vital signs of the patient after every five minutes until he is stable.

Running head: EMERGENCY NURSING 1
Emergency Nursing
Name
Institution
Emergency Nursing
Name
Institution
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
EMERGENCY NURSING 2
Emergency Nursing
Option 1: Pediatric Case
Question 1: 12 Lead ECG Interpretations
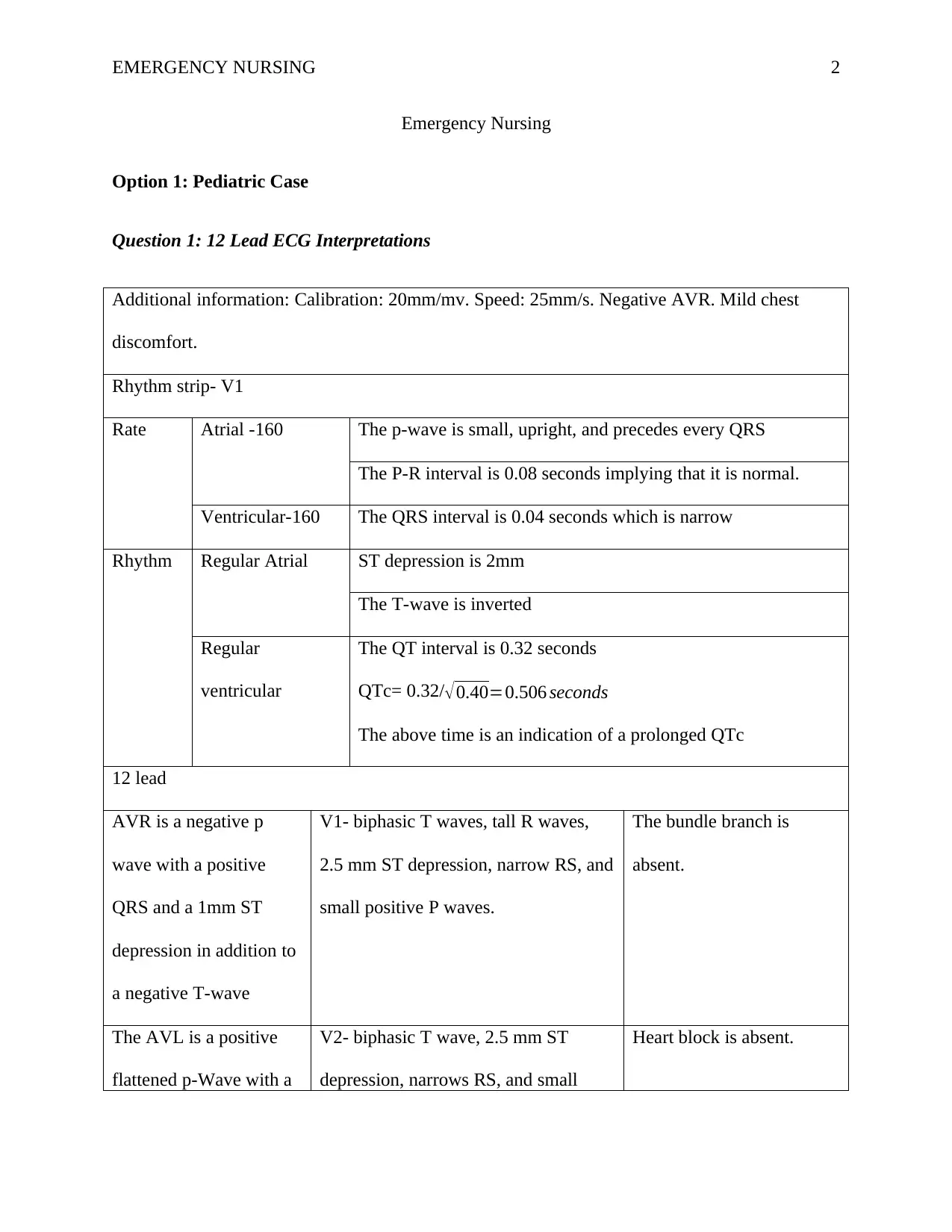
Additional information: Calibration: 20mm/mv. Speed: 25mm/s. Negative AVR. Mild chest
discomfort.
Rhythm strip- V1
Rate Atrial -160 The p-wave is small, upright, and precedes every QRS
The P-R interval is 0.08 seconds implying that it is normal.
Ventricular-160 The QRS interval is 0.04 seconds which is narrow
Rhythm Regular Atrial ST depression is 2mm
The T-wave is inverted
Regular
ventricular
The QT interval is 0.32 seconds
QTc= 0.32/√0.40=0.506 seconds
The above time is an indication of a prolonged QTc
12 lead
AVR is a negative p
wave with a positive
QRS and a 1mm ST
depression in addition to
a negative T-wave
V1- biphasic T waves, tall R waves,
2.5 mm ST depression, narrow RS, and
small positive P waves.
The bundle branch is
absent.
The AVL is a positive
flattened p-Wave with a
V2- biphasic T wave, 2.5 mm ST
depression, narrows RS, and small
Heart block is absent.
Emergency Nursing
Option 1: Pediatric Case
Question 1: 12 Lead ECG Interpretations
Additional information: Calibration: 20mm/mv. Speed: 25mm/s. Negative AVR. Mild chest
discomfort.
Rhythm strip- V1
Rate Atrial -160 The p-wave is small, upright, and precedes every QRS
The P-R interval is 0.08 seconds implying that it is normal.
Ventricular-160 The QRS interval is 0.04 seconds which is narrow
Rhythm Regular Atrial ST depression is 2mm
The T-wave is inverted
Regular
ventricular
The QT interval is 0.32 seconds
QTc= 0.32/√0.40=0.506 seconds
The above time is an indication of a prolonged QTc
12 lead
AVR is a negative p
wave with a positive
QRS and a 1mm ST
depression in addition to
a negative T-wave
V1- biphasic T waves, tall R waves,
2.5 mm ST depression, narrow RS, and
small positive P waves.
The bundle branch is
absent.
The AVL is a positive
flattened p-Wave with a
V2- biphasic T wave, 2.5 mm ST
depression, narrows RS, and small
Heart block is absent.
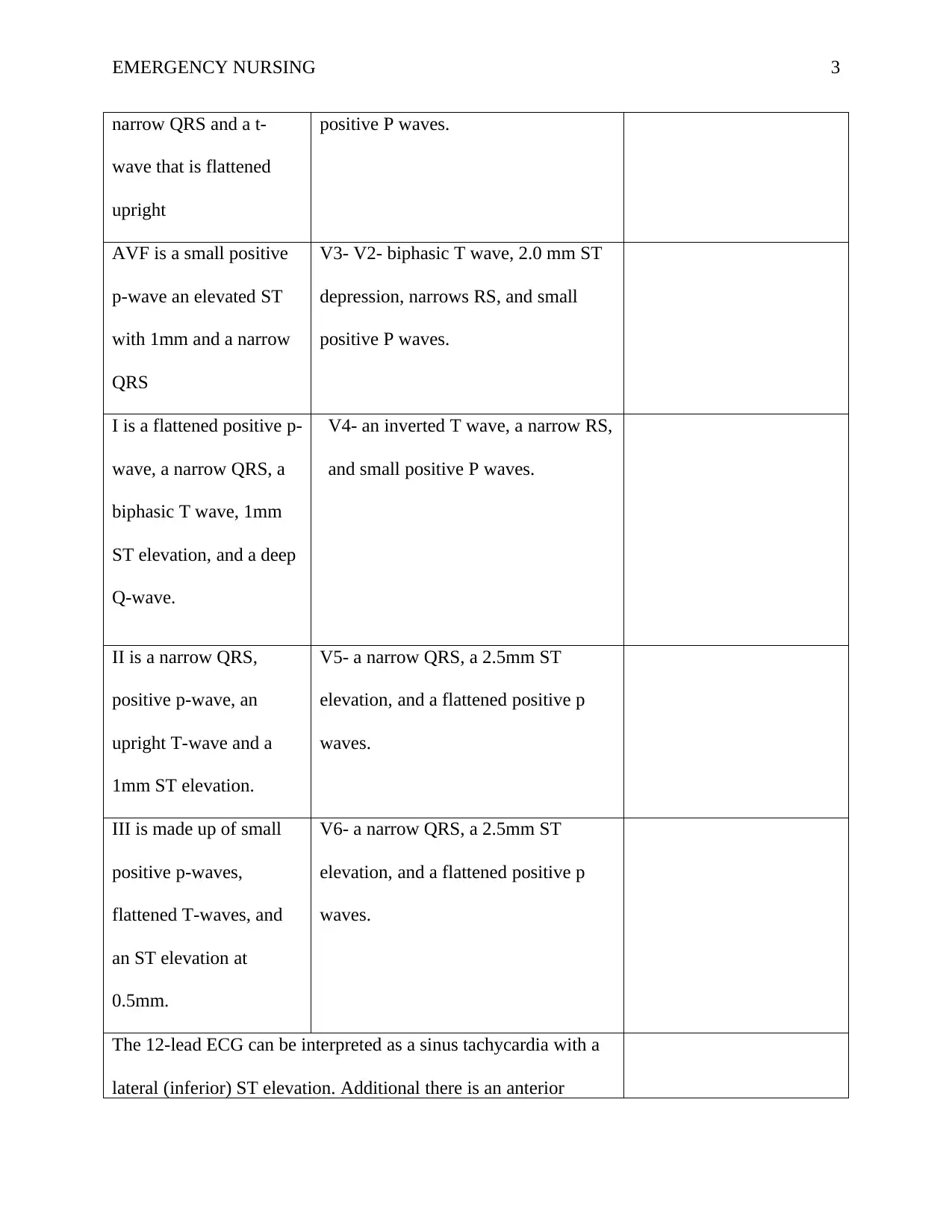
EMERGENCY NURSING 3
narrow QRS and a t-
wave that is flattened
upright
positive P waves.
AVF is a small positive
p-wave an elevated ST
with 1mm and a narrow
QRS
V3- V2- biphasic T wave, 2.0 mm ST
depression, narrows RS, and small
positive P waves.
I is a flattened positive p-
wave, a narrow QRS, a
biphasic T wave, 1mm
ST elevation, and a deep
Q-wave.
V4- an inverted T wave, a narrow RS,
and small positive P waves.
II is a narrow QRS,
positive p-wave, an
upright T-wave and a
1mm ST elevation.
V5- a narrow QRS, a 2.5mm ST
elevation, and a flattened positive p
waves.
III is made up of small
positive p-waves,
flattened T-waves, and
an ST elevation at
0.5mm.
V6- a narrow QRS, a 2.5mm ST
elevation, and a flattened positive p
waves.
The 12-lead ECG can be interpreted as a sinus tachycardia with a
lateral (inferior) ST elevation. Additional there is an anterior
narrow QRS and a t-
wave that is flattened
upright
positive P waves.
AVF is a small positive
p-wave an elevated ST
with 1mm and a narrow
QRS
V3- V2- biphasic T wave, 2.0 mm ST
depression, narrows RS, and small
positive P waves.
I is a flattened positive p-
wave, a narrow QRS, a
biphasic T wave, 1mm
ST elevation, and a deep
Q-wave.
V4- an inverted T wave, a narrow RS,
and small positive P waves.
II is a narrow QRS,
positive p-wave, an
upright T-wave and a
1mm ST elevation.
V5- a narrow QRS, a 2.5mm ST
elevation, and a flattened positive p
waves.
III is made up of small
positive p-waves,
flattened T-waves, and
an ST elevation at
0.5mm.
V6- a narrow QRS, a 2.5mm ST
elevation, and a flattened positive p
waves.
The 12-lead ECG can be interpreted as a sinus tachycardia with a
lateral (inferior) ST elevation. Additional there is an anterior
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
EMERGENCY NURSING 4
(septal) ST depression with a prolonged QT.
Question 2: Abnormal Findings from the Case
According to Bernstein (2016), a rheumatic heart disease (RHD) is a consequence of an
acute rheumatic fever due to an infection by a group A streptococcus that further leads to the
damage of the heart valves. Sika-Paotonu, Beaton, Raghu, Steer, & Carapetis (2016) ascertain
that the rheumatic heart disease is a condition that results from single or multiple recurrent
episodes of acute rheumatic fever. The acute rheumatic fever is common among children aged
between 5 years to 14 years (Sika-Paotonu et al., 2017). It is, however, important to note that
there has been a dramatic reduction in the cases of the acute rheumatic fever recorded since
penicillin was introduced. According to Pellekaan & Best (2015), this complication is still
widely common among the Aboriginal and Torres Strait Islander communities that are found in
Australia.
Cross-reactivity between group A streptococcus and antigens of the cardiac is referred to
as molecular mimicry. This reactivity is responsible for the immunologic activation and
consequently the destruction of the heart tissues (Nulu, Bukhman, & Kwan, 2017). According to
Bernstein (2016), endothelial damage mediated by antibodies results in the activation of the T-
cells in addition to the infiltration and scarring of the valves of the heart. Bernstein (2016) further
adds that the scarring witnessed in the mitral valve usually begins as a small lesion made up of
blood cells and fibrin. A severe and repeated attack by an acute rheumatic fever leads to the
involvement of the chordae tendinae and the endocardium walls (Bernstein, 2016). The
insufficiency of the mitral is as a result of the changes in the valve structure which are mostly
(septal) ST depression with a prolonged QT.
Question 2: Abnormal Findings from the Case
According to Bernstein (2016), a rheumatic heart disease (RHD) is a consequence of an
acute rheumatic fever due to an infection by a group A streptococcus that further leads to the
damage of the heart valves. Sika-Paotonu, Beaton, Raghu, Steer, & Carapetis (2016) ascertain
that the rheumatic heart disease is a condition that results from single or multiple recurrent
episodes of acute rheumatic fever. The acute rheumatic fever is common among children aged
between 5 years to 14 years (Sika-Paotonu et al., 2017). It is, however, important to note that
there has been a dramatic reduction in the cases of the acute rheumatic fever recorded since
penicillin was introduced. According to Pellekaan & Best (2015), this complication is still
widely common among the Aboriginal and Torres Strait Islander communities that are found in
Australia.
Cross-reactivity between group A streptococcus and antigens of the cardiac is referred to
as molecular mimicry. This reactivity is responsible for the immunologic activation and
consequently the destruction of the heart tissues (Nulu, Bukhman, & Kwan, 2017). According to
Bernstein (2016), endothelial damage mediated by antibodies results in the activation of the T-
cells in addition to the infiltration and scarring of the valves of the heart. Bernstein (2016) further
adds that the scarring witnessed in the mitral valve usually begins as a small lesion made up of
blood cells and fibrin. A severe and repeated attack by an acute rheumatic fever leads to the
involvement of the chordae tendinae and the endocardium walls (Bernstein, 2016). The
insufficiency of the mitral is as a result of the changes in the valve structure which are mostly
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
EMERGENCY NURSING 5
accompanied by the loss of the properties of the valves which further makes the chordae tendinae
thick and shortened (Sika-Paotonu et al., 2017).
Additionally, Bernstein (2016) ascertains that an acute rheumatic fever accompanied with
serious cardiac impairments may lead to a heart failure which is caused by a dysfunction of the
mitral valve in combination with an inflammation of the pericardium, endocardium, and
myocardium. Hypertrophy of the left ventricular will develop due to an increase in the volume
load (Bernstein, 2016). From the patient’s chest radiograph, we can observe the inflammatory
process that shows an extremely dilated left ventricle. An increase in the left ventricular end-
diastolic pressure and a reduced stroke volume is due to the impairment of the left ventricular
function (Pike & Peterson, 2018). The increased left ventricular end-diastolic pressure leads to
an increased filtration of the protein-poor fluid into the interstitium and alveoli. This increased
filtration further leads to an increase in the hydrostatic pressure of the pulmonary capillary. It is
further necessary to note that the left atrium enlarges due to increase in the volume load when
blood regurgitates due to the insufficiency of the mitral valve that further creates soft heart
sounds and a gallop rhythm (Pike & Peterson, 2018). According to Sampson (2016), we can
observe an enlargement of the left atrial from the ECG diagram evidenced by bifid and widened
P-waves.
Interstitial edema reduces the compliance of the lung which may lead to an increase in
the work of breathing which is characterized by intermittent grunting and soft tissue retraction
which is further characterized by tracheal tugging during inspiration. As ascertained by Sika-
Paotonu et al. (2017), a failure of the left ventricular, an enlargement of the left atrial, and the
regurgitation of the mitral valve are some of the significant contributors of pulmonary edema.
This condition is responsible for the bilateral apical wheezes as a result of fluid accumulation in
accompanied by the loss of the properties of the valves which further makes the chordae tendinae
thick and shortened (Sika-Paotonu et al., 2017).
Additionally, Bernstein (2016) ascertains that an acute rheumatic fever accompanied with
serious cardiac impairments may lead to a heart failure which is caused by a dysfunction of the
mitral valve in combination with an inflammation of the pericardium, endocardium, and
myocardium. Hypertrophy of the left ventricular will develop due to an increase in the volume
load (Bernstein, 2016). From the patient’s chest radiograph, we can observe the inflammatory
process that shows an extremely dilated left ventricle. An increase in the left ventricular end-
diastolic pressure and a reduced stroke volume is due to the impairment of the left ventricular
function (Pike & Peterson, 2018). The increased left ventricular end-diastolic pressure leads to
an increased filtration of the protein-poor fluid into the interstitium and alveoli. This increased
filtration further leads to an increase in the hydrostatic pressure of the pulmonary capillary. It is
further necessary to note that the left atrium enlarges due to increase in the volume load when
blood regurgitates due to the insufficiency of the mitral valve that further creates soft heart
sounds and a gallop rhythm (Pike & Peterson, 2018). According to Sampson (2016), we can
observe an enlargement of the left atrial from the ECG diagram evidenced by bifid and widened
P-waves.
Interstitial edema reduces the compliance of the lung which may lead to an increase in
the work of breathing which is characterized by intermittent grunting and soft tissue retraction
which is further characterized by tracheal tugging during inspiration. As ascertained by Sika-
Paotonu et al. (2017), a failure of the left ventricular, an enlargement of the left atrial, and the
regurgitation of the mitral valve are some of the significant contributors of pulmonary edema.
This condition is responsible for the bilateral apical wheezes as a result of fluid accumulation in
EMERGENCY NURSING 6
the peribronchial-vascular or alveoli spaces leading to the narrowing of the small airways which
consequently hampers gaseous exchange (Pike & Petersin, 2018). Pulmonary edema also causes
the patient to be a cough, experience shortness of breath, and become increasingly exercise
intolerant. Alveolar edema, on the other hand, leads to an intrapulmonary shunting that causes
peripheral cyanosis and hypoxemia. The body of the patient, therefore, responds to these
conditions by increasing the rate of respiration which is characterized by tachypnea (Frey &
Arain, 2017). It additionally leads to orthopnea which is a characteristic of difficulty in breathing
when supine is manifested by the inability to lie flat (Pike & Peterson, 2018).
An enlargement of the patient’s left ventricle leads to a decrease in the cardiac output and
the stroke volume that leads to hypotension that can be witnessed by a blood pressure of 80/50
mmHg. There are also diminished radial pulses with a cool skin having a capillary refill time that
is more than 3 seconds which is an indication of poor perfusion and a heart failure characterized
by a low output (Pike & Peterson, 2018). The low blood pressure causes the activation of the
sympathetic nervous system and the renin-aldosterone-angiotensin system. This causes the
vasoconstriction of the arteries and veins, the retention of sodium and fluid as a mechanism of
compensation, and tachycardia (Pike & Peterson, 2016). Water retention leads to an increase in
the systemic venous pressure.
According to Bernstein (2016), elevation of the pressure of the pulmonary artery leads to
an enlargement of the right atrium and ventricle which then leads to right-sided heart failure.
From the ECG diagram provided, we can note that there are dominant R waves in V1, V2, and
V3. Also, there are deep S waves in V4-V6 in addition to ST depressions and inversion of the T
wave in lead V1-V3. Furthermore, there is an ST elevation in V5-V6 accompanied by a
deviation in the right axis which is a characteristic of right ventricular hypertrophy (Sampson,
the peribronchial-vascular or alveoli spaces leading to the narrowing of the small airways which
consequently hampers gaseous exchange (Pike & Petersin, 2018). Pulmonary edema also causes
the patient to be a cough, experience shortness of breath, and become increasingly exercise
intolerant. Alveolar edema, on the other hand, leads to an intrapulmonary shunting that causes
peripheral cyanosis and hypoxemia. The body of the patient, therefore, responds to these
conditions by increasing the rate of respiration which is characterized by tachypnea (Frey &
Arain, 2017). It additionally leads to orthopnea which is a characteristic of difficulty in breathing
when supine is manifested by the inability to lie flat (Pike & Peterson, 2018).
An enlargement of the patient’s left ventricle leads to a decrease in the cardiac output and
the stroke volume that leads to hypotension that can be witnessed by a blood pressure of 80/50
mmHg. There are also diminished radial pulses with a cool skin having a capillary refill time that
is more than 3 seconds which is an indication of poor perfusion and a heart failure characterized
by a low output (Pike & Peterson, 2018). The low blood pressure causes the activation of the
sympathetic nervous system and the renin-aldosterone-angiotensin system. This causes the
vasoconstriction of the arteries and veins, the retention of sodium and fluid as a mechanism of
compensation, and tachycardia (Pike & Peterson, 2016). Water retention leads to an increase in
the systemic venous pressure.
According to Bernstein (2016), elevation of the pressure of the pulmonary artery leads to
an enlargement of the right atrium and ventricle which then leads to right-sided heart failure.
From the ECG diagram provided, we can note that there are dominant R waves in V1, V2, and
V3. Also, there are deep S waves in V4-V6 in addition to ST depressions and inversion of the T
wave in lead V1-V3. Furthermore, there is an ST elevation in V5-V6 accompanied by a
deviation in the right axis which is a characteristic of right ventricular hypertrophy (Sampson,
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
EMERGENCY NURSING 7
2016). The right-sided heart failure causes hepatomegaly which is characterized by an increase in
the size of the liver that leads to systemic venous congestion. We are additionally informed that
the patient complains about pain in the right upper abdomen accompanied by intermittent nausea
and vomiting. Furthermore, during an examination of the abdomen, there is an observation of
soft liver edges which is an indication of hepatomegaly as result of an increased venous
congestion and pressure from the right side of the heart into the hepatic vein via the inferior vena
cava. This causes the engorgement of the liver (Pike and Peterson, 2018).
Question 3: Biomarkers
Antistreptolysin O
It is an antibody that targets the production of streptolysin-O that is produced by group A
streptococcus (Chernecky & Berjer, 2012). They start rising after approximately seven days of
infection and reach peak levels after 21-35 days before gradually returning to the baseline after
6-12 months. Since the Antistreptolysin O titers remain high in patients that have post-
streptococcal infections, Chernecky & Berjer (2012), argue that the test can be used to determine
whether an acute rheumatic fever is as a result of a post-streptococcal disease. As confirmed by
Hanson-Manful et al. (2017), the disease specificity of Antistreptolysin O response tends to
occur due to a throat infection mostly. Antistreptolysin O has a specificity of 57.6% and a
sensitivity of 75% (Hanson-Manful et al., 2017). This biomarker is significant in the
determination of group A streptococcus bacteria which could precipitate acute rheumatic fever
(Chernecky & Berjer, 2012).
NT-proBNP
2016). The right-sided heart failure causes hepatomegaly which is characterized by an increase in
the size of the liver that leads to systemic venous congestion. We are additionally informed that
the patient complains about pain in the right upper abdomen accompanied by intermittent nausea
and vomiting. Furthermore, during an examination of the abdomen, there is an observation of
soft liver edges which is an indication of hepatomegaly as result of an increased venous
congestion and pressure from the right side of the heart into the hepatic vein via the inferior vena
cava. This causes the engorgement of the liver (Pike and Peterson, 2018).
Question 3: Biomarkers
Antistreptolysin O
It is an antibody that targets the production of streptolysin-O that is produced by group A
streptococcus (Chernecky & Berjer, 2012). They start rising after approximately seven days of
infection and reach peak levels after 21-35 days before gradually returning to the baseline after
6-12 months. Since the Antistreptolysin O titers remain high in patients that have post-
streptococcal infections, Chernecky & Berjer (2012), argue that the test can be used to determine
whether an acute rheumatic fever is as a result of a post-streptococcal disease. As confirmed by
Hanson-Manful et al. (2017), the disease specificity of Antistreptolysin O response tends to
occur due to a throat infection mostly. Antistreptolysin O has a specificity of 57.6% and a
sensitivity of 75% (Hanson-Manful et al., 2017). This biomarker is significant in the
determination of group A streptococcus bacteria which could precipitate acute rheumatic fever
(Chernecky & Berjer, 2012).
NT-proBNP
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
EMERGENCY NURSING 8
Cardiac muscles produce this biomarker due to an increase in the end-diastolic volume
and pressure. It can also be produced as a result of cardiac strain (Januzzi et al., 2018). Its
sensitivity is 81% while its specificity is 76%during the diagnosis of acute heart failure in
pediatric patients. According to Chernecky & Berjer (2012), an NT-proBNP level that is less
than 30pg/mL is an indication of unlikely heart failure. According to several pieces of evidence
by Januzzi et al. (2018), the levels of NT-proBNP correlates with prognosis, clinical status, and
diagnosis of patients who have congestive heart failure. NT-proBNP is normally elevated among
pediatric patients with different heart failure causes and it is thus recommended as an adjunctive
biomarker during a heart failure diagnosis.
C-reactive protein
According to Chernecky & Berjer (2012), the liver produces this protein during acute
inflammation. It is easy to detect during the first 6-10 hours of the inflammatory response of the
body which is stimulated and may even rise to as high as 4000 times during the peak of the acute
phase inflammatory response. The level of C-reactive protein tends to rise as a result of various
stimuli that include trauma, infection, ischemic tissue injury, and inflammation (Ansar & Ghosh,
2013). According to Paradhan et al. (2016), the sensitivity of C-reactive protein is 84.3% while
its specificity is 46.15%.
Troponin I
This biomarker is ultrasensitive and cardiac specific. Chernecky & Berjer (2012) argue
that it is detectable an hour after a myocardial injury. The specificity of this biomarker is 80%
while its sensitivity is 95% (Brush, Kaul, & Krumholz, 2016). According to several pieces of
evidence, Troponin I, in most cases is elevated in the blood within 3-8 hours of myocardial
Cardiac muscles produce this biomarker due to an increase in the end-diastolic volume
and pressure. It can also be produced as a result of cardiac strain (Januzzi et al., 2018). Its
sensitivity is 81% while its specificity is 76%during the diagnosis of acute heart failure in
pediatric patients. According to Chernecky & Berjer (2012), an NT-proBNP level that is less
than 30pg/mL is an indication of unlikely heart failure. According to several pieces of evidence
by Januzzi et al. (2018), the levels of NT-proBNP correlates with prognosis, clinical status, and
diagnosis of patients who have congestive heart failure. NT-proBNP is normally elevated among
pediatric patients with different heart failure causes and it is thus recommended as an adjunctive
biomarker during a heart failure diagnosis.
C-reactive protein
According to Chernecky & Berjer (2012), the liver produces this protein during acute
inflammation. It is easy to detect during the first 6-10 hours of the inflammatory response of the
body which is stimulated and may even rise to as high as 4000 times during the peak of the acute
phase inflammatory response. The level of C-reactive protein tends to rise as a result of various
stimuli that include trauma, infection, ischemic tissue injury, and inflammation (Ansar & Ghosh,
2013). According to Paradhan et al. (2016), the sensitivity of C-reactive protein is 84.3% while
its specificity is 46.15%.
Troponin I
This biomarker is ultrasensitive and cardiac specific. Chernecky & Berjer (2012) argue
that it is detectable an hour after a myocardial injury. The specificity of this biomarker is 80%
while its sensitivity is 95% (Brush, Kaul, & Krumholz, 2016). According to several pieces of
evidence, Troponin I, in most cases is elevated in the blood within 3-8 hours of myocardial
EMERGENCY NURSING 9
injury and peaks after 8-24 hours. As confirmed by Fox & Diercks (2016), Troponin I may
remain elevated in the bloodstream for approximately 1-2 weeks. The elevation is significant in
cases of cardiac injuries.
Question 4: Initial Management
According to Mebazza et al. (2015), the patient needs to be closely monitored by a highly
knowledgeable practitioner with the necessary expertise to respond to deteriorations. The first
step towards the determination of the severity of the instability of hemodynamic is founded on
the mental status, heart rhythm, hemodynamic status, and dyspnea levels. Due to the patient’s
high risk of clinical deterioration, he requires a one on one nursing management in the
emergency department. The continuous patient monitoring including the signs and symptoms as
a result of the hemodynamic status and treatment requires close observation of the hemodynamic
parameters that include assessing the vital signs of the patient after every five minutes until he is
stable. This implies that the blood pressure, heart rate, heart rhythm, saturation of oxygen,
respiratory rate, the temperature of the body, and pain should be stabilized (Mebazza et al.,
2015). It is additionally important to observe the mental status of the patient and his level of
consciousness after every five minutes thus promptly identifying the changes in the patient’s
clinical status. It is important to assess the patient’s orthopnea, the rate of respiration, the degree
of hypoxia, and work of breathing (Mebazza et al., 2015). Additionally, the practitioner needs to
determine the signs and symptoms of hypo-perfusion inclusive of mental status, cool extremities,
and narrow pulse pressure. It is also necessary to closely analyze the findings from the laboratory
tests including the electrolytes that are in some instances affected by diuretic therapy. It is also
significant to check the blood glucose level.
injury and peaks after 8-24 hours. As confirmed by Fox & Diercks (2016), Troponin I may
remain elevated in the bloodstream for approximately 1-2 weeks. The elevation is significant in
cases of cardiac injuries.
Question 4: Initial Management
According to Mebazza et al. (2015), the patient needs to be closely monitored by a highly
knowledgeable practitioner with the necessary expertise to respond to deteriorations. The first
step towards the determination of the severity of the instability of hemodynamic is founded on
the mental status, heart rhythm, hemodynamic status, and dyspnea levels. Due to the patient’s
high risk of clinical deterioration, he requires a one on one nursing management in the
emergency department. The continuous patient monitoring including the signs and symptoms as
a result of the hemodynamic status and treatment requires close observation of the hemodynamic
parameters that include assessing the vital signs of the patient after every five minutes until he is
stable. This implies that the blood pressure, heart rate, heart rhythm, saturation of oxygen,
respiratory rate, the temperature of the body, and pain should be stabilized (Mebazza et al.,
2015). It is additionally important to observe the mental status of the patient and his level of
consciousness after every five minutes thus promptly identifying the changes in the patient’s
clinical status. It is important to assess the patient’s orthopnea, the rate of respiration, the degree
of hypoxia, and work of breathing (Mebazza et al., 2015). Additionally, the practitioner needs to
determine the signs and symptoms of hypo-perfusion inclusive of mental status, cool extremities,
and narrow pulse pressure. It is also necessary to closely analyze the findings from the laboratory
tests including the electrolytes that are in some instances affected by diuretic therapy. It is also
significant to check the blood glucose level.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
EMERGENCY NURSING 10
The recommended mode of delivering oxygen for hypoxic patients that have heart failure
but do not require any intubation is a non-invasive positive pressure ventilation therapy. This
therapy may consist of Bi-level positive airway pressure and continuous positive airway pressure
(Kato, Suda, & Kasai, 2014). The non-invasive positive pressure ventilation therapy on the
collapsed alveoli is helpful in sustaining the alveolar pressure thus preventing the collapse of the
alveoli and at the same time improving gaseous exchange. Kato et al. (2014) further confirm that
the non-invasive positive pressure ventilation induces a shift of fluids from the interstitial space
and the alveoli back into the circulation of the pulmonary. This is done through the
counterbalancing of the capillary or interstitial hydrostatic pressure. The shift leads to a decrease
in the amount of intrapulmonary shunting and consequently improves gaseous exchange. Purvey
& Allen (2014) confirm that non-invasive positive pressure ventilation should be commenced at
100% oxygen concentration and titrated until an oxygen saturation ranging between 92%-96% is
achieved. It reduces the muscle load on the respiratory system thus improving the function of the
lung and work of breathing. This is done through lung inflation and maintaining the functional
residual capacity. Non-invasive positive pressure ventilation is fundamental in improving the
cardiac output. This is done by improving the intrathoracic pressure. Kato et al. (2014) further
ascertain that the increased intrathoracic pressure helps in decreasing the systemic venous return
and the preload in the right ventricular thus leading to an increased cardiac output. The decrease
in the preload could result in low blood pressure or hypotension, and it is therefore important to
closely monitor the blood pressure (Purvey & Allen, 2014).
The primary goal of this management optimizes the delivery of oxygen by raising the
cardiac input while at the same time reducing the metabolic demand. The recommended
medication in during this management includes epinephrine, milrinone, and dobutamine
The recommended mode of delivering oxygen for hypoxic patients that have heart failure
but do not require any intubation is a non-invasive positive pressure ventilation therapy. This
therapy may consist of Bi-level positive airway pressure and continuous positive airway pressure
(Kato, Suda, & Kasai, 2014). The non-invasive positive pressure ventilation therapy on the
collapsed alveoli is helpful in sustaining the alveolar pressure thus preventing the collapse of the
alveoli and at the same time improving gaseous exchange. Kato et al. (2014) further confirm that
the non-invasive positive pressure ventilation induces a shift of fluids from the interstitial space
and the alveoli back into the circulation of the pulmonary. This is done through the
counterbalancing of the capillary or interstitial hydrostatic pressure. The shift leads to a decrease
in the amount of intrapulmonary shunting and consequently improves gaseous exchange. Purvey
& Allen (2014) confirm that non-invasive positive pressure ventilation should be commenced at
100% oxygen concentration and titrated until an oxygen saturation ranging between 92%-96% is
achieved. It reduces the muscle load on the respiratory system thus improving the function of the
lung and work of breathing. This is done through lung inflation and maintaining the functional
residual capacity. Non-invasive positive pressure ventilation is fundamental in improving the
cardiac output. This is done by improving the intrathoracic pressure. Kato et al. (2014) further
ascertain that the increased intrathoracic pressure helps in decreasing the systemic venous return
and the preload in the right ventricular thus leading to an increased cardiac output. The decrease
in the preload could result in low blood pressure or hypotension, and it is therefore important to
closely monitor the blood pressure (Purvey & Allen, 2014).
The primary goal of this management optimizes the delivery of oxygen by raising the
cardiac input while at the same time reducing the metabolic demand. The recommended
medication in during this management includes epinephrine, milrinone, and dobutamine
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
EMERGENCY NURSING 11
specifically in refractory hypotension. The mode of action of milrinone is by increasing the
contractility of the heart thus decreasing the resistance of the pulmonary ventricular.
Additionally, this drug leads to the vasodilation thus helping in reducing afterloads and
improving contraction. It is imperative to note that diuretics are used to reduce preloads but
caution must be exercised during its administration so as not to worsen hypotension.
The patient’s management of pain is divided into two classes that include
pharmacological and non-pharmacological. According to Newcombe & Brady (2017),
pharmacological management is made up of oral pain medications that include ibuprofen and
paracetamol. According to Kasowsky (2013), fentanyl exhibit minimal hemodynamic effects in
getting rid of the pain. KAsowsky (2013) further adds that the administration of opioids for
example morphine should be carefully done because it has the capability of causing hypotension.
Nitroglycerin is believed to cause vasodilation thus reducing preload and decrease the heart’s
demand for oxygen. This drug can, therefore, be administered for chest pains that result from
ischemic changes. Non-pharmacological, on the other hand, constitutes pacing of activities,
techniques of distraction, guided imagery, the involvement of parents or primary care, and
comforting touch.
Management plans include the alleviation of the anxiety of the patient by maintaining a
free and open communication between a patient and their family during patient care. It is also
important to strictly adhere to the hand hygiene protocol which helps in controlling infection and
managing infection prevention.
specifically in refractory hypotension. The mode of action of milrinone is by increasing the
contractility of the heart thus decreasing the resistance of the pulmonary ventricular.
Additionally, this drug leads to the vasodilation thus helping in reducing afterloads and
improving contraction. It is imperative to note that diuretics are used to reduce preloads but
caution must be exercised during its administration so as not to worsen hypotension.
The patient’s management of pain is divided into two classes that include
pharmacological and non-pharmacological. According to Newcombe & Brady (2017),
pharmacological management is made up of oral pain medications that include ibuprofen and
paracetamol. According to Kasowsky (2013), fentanyl exhibit minimal hemodynamic effects in
getting rid of the pain. KAsowsky (2013) further adds that the administration of opioids for
example morphine should be carefully done because it has the capability of causing hypotension.
Nitroglycerin is believed to cause vasodilation thus reducing preload and decrease the heart’s
demand for oxygen. This drug can, therefore, be administered for chest pains that result from
ischemic changes. Non-pharmacological, on the other hand, constitutes pacing of activities,
techniques of distraction, guided imagery, the involvement of parents or primary care, and
comforting touch.
Management plans include the alleviation of the anxiety of the patient by maintaining a
free and open communication between a patient and their family during patient care. It is also
important to strictly adhere to the hand hygiene protocol which helps in controlling infection and
managing infection prevention.
EMERGENCY NURSING 12
References
Ansar, W., & Ghosh, S. (2013). C-reactive protein and the biology of disease. Immunologic
research, 56(1), 131-142.
Bernstein, D. (2016). Rheumatic heart disease. In R. M. Kliegman, B. F. Stanton, J. W. St Geme,
& N. F. Schor (Eds.), Nelson Textbook of Paediatrics (20th ed.). (pp. 2269-2271).
Philadelphia, USA: Elsevier, Inc.
Brush, J. E., Kaul, S., & Krumholz, H. M. (2016). Troponin testing for clinicians. Journal of the
American College of Cardiology, 68(21), 2365-2375.
Chernecky, C. C., & Berger, B. J. (2012). Laboratory test and diagnostic procedures,
Saunders. Philadelphia, 19932, 401.
Fox, W. R., & Diercks, D. B. (2016). Troponin assay use in the emergency department for
management of patients with potential acute coronary syndrome: current use and future
directions. Clinical and experimental emergency medicine, 3(1), 1.
Frey, T., & Arain, N. (2018). Pediatric Viral Myocarditis--A Review. South Dakota
Medicine, 71(1).
Hanson-Manful, P., Whitcombe, A. L., Young, P. G., Carr, P. E. A., Bell, A., Didsbury, A., ... &
Moreland, N. J. (2017). The novel Group A Streptococcus antigen SpnA combined with
bead-based immunoassay technology improves streptococcal serology for the diagnosis
of acute rheumatic fever. Journal of Infection.
Januzzi, J. L., Chen-Tournoux, A. A., Christenson, R. H., Doros, G., Hollander, J. E., Levy, P.
D., ... & Peacock, W. F. (2018). N-Terminal Pro–B-Type Natriuretic Peptide in the
References
Ansar, W., & Ghosh, S. (2013). C-reactive protein and the biology of disease. Immunologic
research, 56(1), 131-142.
Bernstein, D. (2016). Rheumatic heart disease. In R. M. Kliegman, B. F. Stanton, J. W. St Geme,
& N. F. Schor (Eds.), Nelson Textbook of Paediatrics (20th ed.). (pp. 2269-2271).
Philadelphia, USA: Elsevier, Inc.
Brush, J. E., Kaul, S., & Krumholz, H. M. (2016). Troponin testing for clinicians. Journal of the
American College of Cardiology, 68(21), 2365-2375.
Chernecky, C. C., & Berger, B. J. (2012). Laboratory test and diagnostic procedures,
Saunders. Philadelphia, 19932, 401.
Fox, W. R., & Diercks, D. B. (2016). Troponin assay use in the emergency department for
management of patients with potential acute coronary syndrome: current use and future
directions. Clinical and experimental emergency medicine, 3(1), 1.
Frey, T., & Arain, N. (2018). Pediatric Viral Myocarditis--A Review. South Dakota
Medicine, 71(1).
Hanson-Manful, P., Whitcombe, A. L., Young, P. G., Carr, P. E. A., Bell, A., Didsbury, A., ... &
Moreland, N. J. (2017). The novel Group A Streptococcus antigen SpnA combined with
bead-based immunoassay technology improves streptococcal serology for the diagnosis
of acute rheumatic fever. Journal of Infection.
Januzzi, J. L., Chen-Tournoux, A. A., Christenson, R. H., Doros, G., Hollander, J. E., Levy, P.
D., ... & Peacock, W. F. (2018). N-Terminal Pro–B-Type Natriuretic Peptide in the
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 14
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.