Endovascular vs. tPA for Ischemic Stroke: A Treatment Analysis
VerifiedAdded on 2019/09/18
|17
|5659
|368
Report
AI Summary
This report presents a systematic literature review comparing endovascular therapy and tissue plasminogen activator (tPA) for the treatment of acute ischemic stroke. The study analyzed eight multicenter, randomized clinical trials involving approximately 2,400 patients, assessing outcomes such as functional independence (measured by the modified Rankin Scale) and mortality rates. The findings indicate that endovascular intervention, when combined with medical management including IV tPA for eligible patients, improves outcomes for patients with large vessel occlusion. The report details the pathophysiology of ischemic stroke, methods used for the literature search and data analysis, and a comprehensive discussion of the results, including the characteristics of the included studies and a comparison of the benefits and limitations of each treatment approach. The study concludes with recommendations for future research and clinical practice, emphasizing the importance of timely intervention and appropriate patient selection for optimal outcomes. The report also discusses the evolution of treatment strategies, including the significance of the ischemic penumbra and the role of endovascular techniques in improving recanalization rates and clinical results.

Endovascular versus tissue plasminogen activator treatment for ischemic
stroke
1
stroke
1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Table of contents
S No Content Page
Abstract 3
1 Introduction 4
2 Pathophysiology of acute stroke 5
2.1 Ischemic Stroke 5
2.2. ICH 6
3 Resources and methods 6
3.1 Resources 6
3.2 Inclusion criteria 6
3.3 Methods 6
3.3.1 Literature search 6
3.3.2 Review of literature review and extraction of essentials 7
3.3.3 Statistical analysis 8
4 Results 8
4.1 Selection of study 8
4.2 Characteristics of the study 8
4.3 Comparison of hazard/advantage for the intervention Vs therapeutic administration 9
5.0 Discussion 13
6.0 Conclusions 14
7.0 Recommendations 14
References
Abstract
2
S No Content Page
Abstract 3
1 Introduction 4
2 Pathophysiology of acute stroke 5
2.1 Ischemic Stroke 5
2.2. ICH 6
3 Resources and methods 6
3.1 Resources 6
3.2 Inclusion criteria 6
3.3 Methods 6
3.3.1 Literature search 6
3.3.2 Review of literature review and extraction of essentials 7
3.3.3 Statistical analysis 8
4 Results 8
4.1 Selection of study 8
4.2 Characteristics of the study 8
4.3 Comparison of hazard/advantage for the intervention Vs therapeutic administration 9
5.0 Discussion 13
6.0 Conclusions 14
7.0 Recommendations 14
References
Abstract
2
Aim: The objective of paper is to compare the outcomes between endovascular and medical
management utilizing tissue plasminogen activator in the management of acute ischemic stroke
based on recent randomized controlled trials.
Methods: A systematic literature review was performed, and multicenter, prospective randomized
clinical trails were chosen to compare the endovascular therapy to medical management for patients
with acute ischemic stroke. The assessment was done in terms of modified Rankin Scale (mRS) and
mortality at 3 months for endovascular therapy and medical management.
Results: Eight multicenter, planned randomized clinical trails (Interventional Management of Stroke,
IMS III; Local Versus Systemic Thrombolysis for Acute Ischemic Stroke, SYN; Expansion, Mechanical
Retrieval and Recanalization of Stroke Clots Using Embolectomy RES; Multicenter Randomized
Clinical Trial of Endovascular Treatment for Acute Ischemic Stroke in the Netherlands, MRC;
Evaluation Study of Congestive Heart Failure and Pulmonary Artery Catheterization Effectiveness,
ESC;, Extending the Time for Thrombolysis in Emergency Neurological Deficits–Intra-Arterial, EXT;
Solitaire With the Intention For Thrombectomy as Primary Endovascular Treatment, SPR and
Endovascular Revascularization With Solitaire Device Versus Best Medical Therapy in Anterior
Circulation Stroke Within 8 Hours, REV) involving around 2,400 patients were incorporated. The
evaluation of information exhibited functional independence (mRS 0–2) at 3 months for endovascular
treatment (P<0.005). Subgroup investigation of the 5 trials that principally used stent retriever devices
in the intervention arm showed practical independence at 3 months for endovascular treatment
(P<0.05). No distinction was found for mortality at 3 months between endovascular treatment and
restorative administration in all investigations and subgroup examinations.
Conclusions: The evidences reveal that the endovascular intervention in combination with medical
management, including IV tissue plasminogen activator for eligible patients, improves the outcomes of
appropriately selected patients with acute ischemic stroke in the setting of large vessel occlusion.
1.0. Introduction
3
management utilizing tissue plasminogen activator in the management of acute ischemic stroke
based on recent randomized controlled trials.
Methods: A systematic literature review was performed, and multicenter, prospective randomized
clinical trails were chosen to compare the endovascular therapy to medical management for patients
with acute ischemic stroke. The assessment was done in terms of modified Rankin Scale (mRS) and
mortality at 3 months for endovascular therapy and medical management.
Results: Eight multicenter, planned randomized clinical trails (Interventional Management of Stroke,
IMS III; Local Versus Systemic Thrombolysis for Acute Ischemic Stroke, SYN; Expansion, Mechanical
Retrieval and Recanalization of Stroke Clots Using Embolectomy RES; Multicenter Randomized
Clinical Trial of Endovascular Treatment for Acute Ischemic Stroke in the Netherlands, MRC;
Evaluation Study of Congestive Heart Failure and Pulmonary Artery Catheterization Effectiveness,
ESC;, Extending the Time for Thrombolysis in Emergency Neurological Deficits–Intra-Arterial, EXT;
Solitaire With the Intention For Thrombectomy as Primary Endovascular Treatment, SPR and
Endovascular Revascularization With Solitaire Device Versus Best Medical Therapy in Anterior
Circulation Stroke Within 8 Hours, REV) involving around 2,400 patients were incorporated. The
evaluation of information exhibited functional independence (mRS 0–2) at 3 months for endovascular
treatment (P<0.005). Subgroup investigation of the 5 trials that principally used stent retriever devices
in the intervention arm showed practical independence at 3 months for endovascular treatment
(P<0.05). No distinction was found for mortality at 3 months between endovascular treatment and
restorative administration in all investigations and subgroup examinations.
Conclusions: The evidences reveal that the endovascular intervention in combination with medical
management, including IV tissue plasminogen activator for eligible patients, improves the outcomes of
appropriately selected patients with acute ischemic stroke in the setting of large vessel occlusion.
1.0. Introduction
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Ischemic stroke (IS) influences around 8,00,000 patients in the United States every year (Mozaffarian
et al., 2015). The nearness of large vessel impediment of a major intracranial artery at middle cerebral
region or inward carotid artery is evaluated to happen in roughly 33% to one-portion of acute IS
(Smith et al., 2009). To tackle such obstruction now a day, the main treatment for IS with
demonstrated adequacy was IV tissue plasminogen activator controlled within 4.5 hours of side effect
onset (Hacke et al., 2008). In any case, recanalization rates of IS with substantial vessel impediment
after IV-tissue plasminogen activator are low and connected with poor clinical results (Bhatia et al.,
2010). The utilization of tissue plasminogen activator in stroke has been broadly evaluated and was
demonstrated a brilliant results for the administration of intense IS (Liang, et al., 2008). As per reports,
the utilization of tissue plasminogen activator in patients matured 90 years or more established for
intense ischemic stroke had poor 30-day utilitarian results and were died (Mateen et al., 2009).
Another method of treatment is endovascular treatment for the intense IS. The method of treatment is
a possibly solid subordinate to IV tissue plasminogen activator for patients for real intense ischemic
stroke created by significant front flow supply route impediments. The method of treatment is thought
to be better than intravenous thrombolysis and restorative administration (Leslie-Mazwi et al., 2016).
The treatment ought to happen as fast as is sensibly conceivable. All patients with direct to serious
manifestations (National Institutes of Health stroke scale >8) and a treatable impediment should be
considered. In spite of positive results of endovascular treatment, there exist certain fizzled
randomized controlled trials of endovascular stroke treatment fundamentally hosed the underlying
eagerness for endovascular intercession (Ciccone et al., 2013). Methodological shortcomings have
been the primary cause of these trials (Przybylowski et al., 2014). All the more as of late, a few
endovascular stroke trials have tended to the inadequacies of the underlying trials, and all have
revealed predominant results with endovascular treatment for IS (Saver et al., 2015).
From the literature scan, it can be understood that the two modes of treatment is associated with
merits and demerits. To assess the best mode it is desired to investigate the benefits and limitations
from clinical perceptive. Therefore, it was aimed to compare the rates of functional independence,
mortality, and symptomatic intracranial haemorrhage between endovascular and plasminogen
activator treatment for IS. A depth literature search has been carried and the summary of outcome is
presented in sequential manner followed by conclusions and future recommendations.
2.0. Pathophysiology of acute stroke
4
et al., 2015). The nearness of large vessel impediment of a major intracranial artery at middle cerebral
region or inward carotid artery is evaluated to happen in roughly 33% to one-portion of acute IS
(Smith et al., 2009). To tackle such obstruction now a day, the main treatment for IS with
demonstrated adequacy was IV tissue plasminogen activator controlled within 4.5 hours of side effect
onset (Hacke et al., 2008). In any case, recanalization rates of IS with substantial vessel impediment
after IV-tissue plasminogen activator are low and connected with poor clinical results (Bhatia et al.,
2010). The utilization of tissue plasminogen activator in stroke has been broadly evaluated and was
demonstrated a brilliant results for the administration of intense IS (Liang, et al., 2008). As per reports,
the utilization of tissue plasminogen activator in patients matured 90 years or more established for
intense ischemic stroke had poor 30-day utilitarian results and were died (Mateen et al., 2009).
Another method of treatment is endovascular treatment for the intense IS. The method of treatment is
a possibly solid subordinate to IV tissue plasminogen activator for patients for real intense ischemic
stroke created by significant front flow supply route impediments. The method of treatment is thought
to be better than intravenous thrombolysis and restorative administration (Leslie-Mazwi et al., 2016).
The treatment ought to happen as fast as is sensibly conceivable. All patients with direct to serious
manifestations (National Institutes of Health stroke scale >8) and a treatable impediment should be
considered. In spite of positive results of endovascular treatment, there exist certain fizzled
randomized controlled trials of endovascular stroke treatment fundamentally hosed the underlying
eagerness for endovascular intercession (Ciccone et al., 2013). Methodological shortcomings have
been the primary cause of these trials (Przybylowski et al., 2014). All the more as of late, a few
endovascular stroke trials have tended to the inadequacies of the underlying trials, and all have
revealed predominant results with endovascular treatment for IS (Saver et al., 2015).
From the literature scan, it can be understood that the two modes of treatment is associated with
merits and demerits. To assess the best mode it is desired to investigate the benefits and limitations
from clinical perceptive. Therefore, it was aimed to compare the rates of functional independence,
mortality, and symptomatic intracranial haemorrhage between endovascular and plasminogen
activator treatment for IS. A depth literature search has been carried and the summary of outcome is
presented in sequential manner followed by conclusions and future recommendations.
2.0. Pathophysiology of acute stroke
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
It is required to understand the mechanism behind the development of acute stroke before continuing
the comparisons of benefits of two modes of treatment. The two primary improvements fundamental
restorative advances in stroke are the depiction of the ischemic penumbra in ischemic stroke and the
perception of haematoma development in intracerebral haemorrhage (ICH)
2.1. Ischemic Stroke
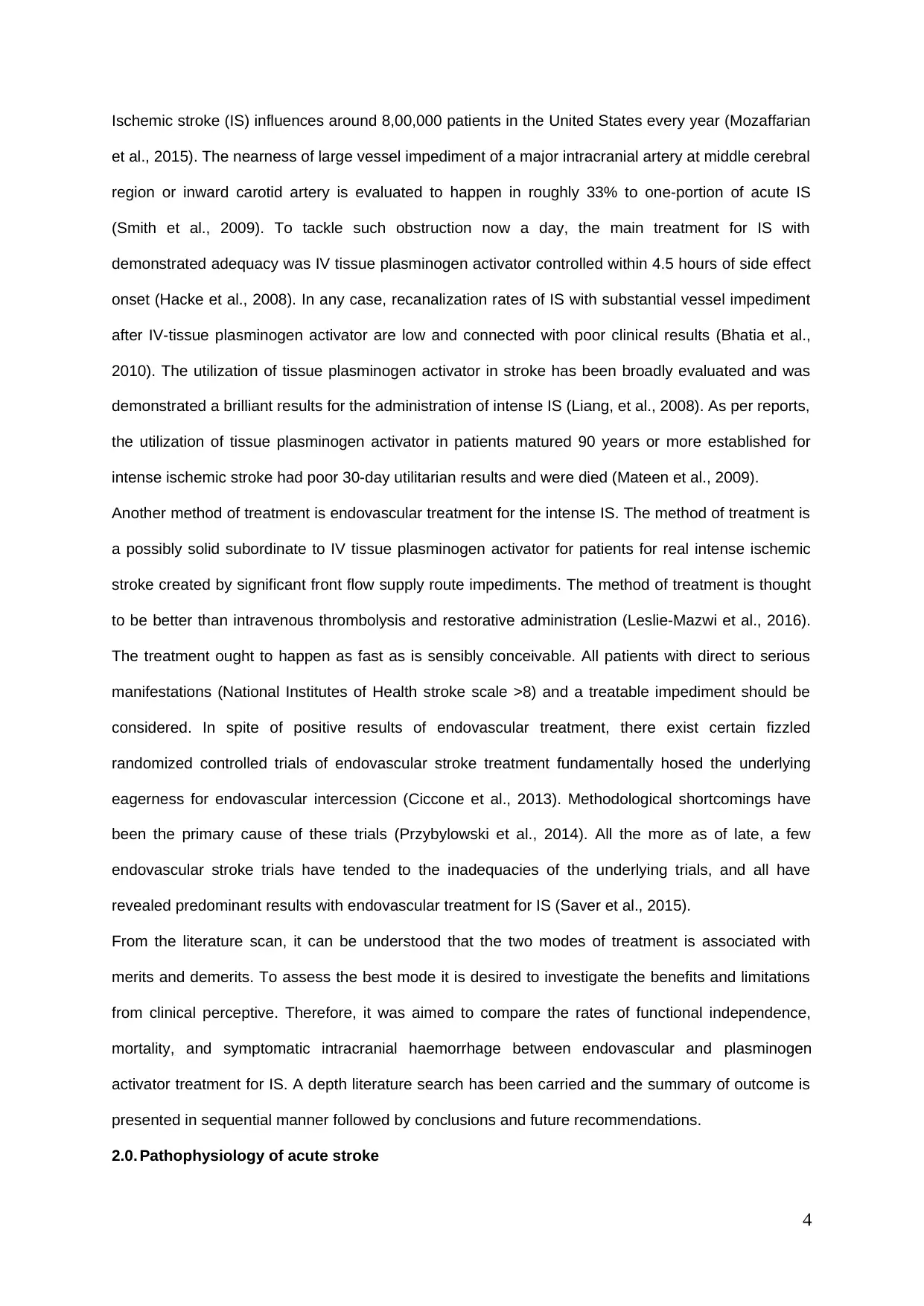
The seriousness of an intense ischemic stroke relies on upon the level of hindrance of cerebral blood
stream and the opportunity to reperfusion. As the ischemic procedure develops, most usually due to
thromboembolism due to blood vessel impediment, there is a dynamic diminishing in cerebral blood
stream. At the point when this tumbles from typical levels of roughly 50 to <10 ml/100 g/min, neuronal
cell demise quickly happens. However, between the ischemic center and the typically perfused mind
at the fringe lies the ischemic penumbra, a zone of decently decreased cerebral blood stream, reliant
on the proximal blood vessel impediment and insurance supply (Fig-1). Inside the ischemic
penumbra, the neurones are hypoxic, practically idle, yet at the same time reasonable, and this is the
locale focused by intense stroke treatments. The penumbra is a dynamic, time-based area in which
cerebrum tissue will experience rot over hours to days because of perfusion suppression and an
auxiliary course of harming biochemical reactions.
Fig-1: Showing the pictures of vast ischaemic penumbra perfusion (PWI); dissemination weighted
imaging (DWI) and magnetic resonance angiogram (MRA). MRA demonstrates an impeded right
center cerebral course.
5
the comparisons of benefits of two modes of treatment. The two primary improvements fundamental
restorative advances in stroke are the depiction of the ischemic penumbra in ischemic stroke and the
perception of haematoma development in intracerebral haemorrhage (ICH)
2.1. Ischemic Stroke
The seriousness of an intense ischemic stroke relies on upon the level of hindrance of cerebral blood
stream and the opportunity to reperfusion. As the ischemic procedure develops, most usually due to
thromboembolism due to blood vessel impediment, there is a dynamic diminishing in cerebral blood
stream. At the point when this tumbles from typical levels of roughly 50 to <10 ml/100 g/min, neuronal
cell demise quickly happens. However, between the ischemic center and the typically perfused mind
at the fringe lies the ischemic penumbra, a zone of decently decreased cerebral blood stream, reliant
on the proximal blood vessel impediment and insurance supply (Fig-1). Inside the ischemic
penumbra, the neurones are hypoxic, practically idle, yet at the same time reasonable, and this is the
locale focused by intense stroke treatments. The penumbra is a dynamic, time-based area in which
cerebrum tissue will experience rot over hours to days because of perfusion suppression and an
auxiliary course of harming biochemical reactions.
Fig-1: Showing the pictures of vast ischaemic penumbra perfusion (PWI); dissemination weighted
imaging (DWI) and magnetic resonance angiogram (MRA). MRA demonstrates an impeded right
center cerebral course.
5
These neurotoxic procedures comprises of secretion of glutamate, initiation of N-methyl-d-aspartate
and other cell receptors, flood of sodium and calcium into cells, arrival of free-radical species and, at
last, cell annihilation. The critical time for compelling reperfusion, in view of attractive reverberation
imaging studies, might be around 4.5 h, with prior reclamation prompting to more noteworthy tissue
rescue (Butcher et al., 2003). In any case, the helpful time windows in ischemia stay questionable.
Later, pathophysiological forms incorporate fiery responses and free-radical discharge (Dirnagl et al.,
1999). A restricted remedial window of chance underlies the idea that 'time is mind', and current
modes to deal with treatment are gone for constraining stroke harm and enhancing useful results.
2.2. ICH
Later reviews have demonstrated that ICH is likewise a dynamic procedure and possibly amiable to
helpful intercession. An imminent review in ICH demonstrated that 38% of patients displayed
generous haematoma development (more noteworthy than 33% expansion in volume) if imaged with
computerized tomography (CT) inside 3 h of onset of stroke and rehashed 24 h later (Brott et al.,
1997). The greater part of this development (26%) happened inside 1 h of the principal examine. This
development is presumably because of continued draining or re-dying. This perception prompted to
the speculation that haemostatic treatment could diminish the volume of the haematoma and result in
enhanced results (Mayer, 2003).
3.0. Resources and methods
3.1. Resources
Web based resources for data collection, statistical tools for data assessment and healthcare
professional for healthy discussion. Patients suffering from IS and those are under the treatment with
medical management.
3.2. Inclusion criteria
The criteria for the inclusion of patients in the study are as per the following: (i) the review must be a
multicenter, imminent, randomized clinical trial (ii) the review should straightforwardly think about
results between endovascular treatment and plasminogen activator treatment for patients with IS.
3.3. Methods
3.3.1. Literature search
6
and other cell receptors, flood of sodium and calcium into cells, arrival of free-radical species and, at
last, cell annihilation. The critical time for compelling reperfusion, in view of attractive reverberation
imaging studies, might be around 4.5 h, with prior reclamation prompting to more noteworthy tissue
rescue (Butcher et al., 2003). In any case, the helpful time windows in ischemia stay questionable.
Later, pathophysiological forms incorporate fiery responses and free-radical discharge (Dirnagl et al.,
1999). A restricted remedial window of chance underlies the idea that 'time is mind', and current
modes to deal with treatment are gone for constraining stroke harm and enhancing useful results.
2.2. ICH
Later reviews have demonstrated that ICH is likewise a dynamic procedure and possibly amiable to
helpful intercession. An imminent review in ICH demonstrated that 38% of patients displayed
generous haematoma development (more noteworthy than 33% expansion in volume) if imaged with
computerized tomography (CT) inside 3 h of onset of stroke and rehashed 24 h later (Brott et al.,
1997). The greater part of this development (26%) happened inside 1 h of the principal examine. This
development is presumably because of continued draining or re-dying. This perception prompted to
the speculation that haemostatic treatment could diminish the volume of the haematoma and result in
enhanced results (Mayer, 2003).
3.0. Resources and methods
3.1. Resources
Web based resources for data collection, statistical tools for data assessment and healthcare
professional for healthy discussion. Patients suffering from IS and those are under the treatment with
medical management.
3.2. Inclusion criteria
The criteria for the inclusion of patients in the study are as per the following: (i) the review must be a
multicenter, imminent, randomized clinical trial (ii) the review should straightforwardly think about
results between endovascular treatment and plasminogen activator treatment for patients with IS.
3.3. Methods
3.3.1. Literature search
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
The available and popular sources were used to search for the evidences. The sources, diverse
online electronic resources including BNI (British Nursing Index), CINAHL (Cumulative Index to
Nursing and Allied Health Literature), EMBASE (the Excerpta Medica database), Pubmed, The DARE
(Database of Abstracts of Reviews of Effects), HTA (Health Technology Assessment Database) and
NHS (Economic Evaluation Database). In addition, the available textbooks, magazines and articles
from newspapers from library have been searched to find out the relevant literature for ischemic
stroke and its management. The search was made for past 25 years to collect the relevant sources
and link the evidences to the current context. Adequate measures were made to channel the quest for
the pertinent sources. The keywords utilized were ischemic stroke, treatment of acute ischemic
stroke, use of plasminogen activator, role of endothelial factors in ischemic stroke and progression of
treatment in ischemic stroke. The outcome of the search for the relevant sources has been depicted in
subsequent sections. More focus has been given for the stroke management utilizing endovascular
therapy and tissue plasminogen activator.
3.3.2. Review of literature review and extraction of essentials
Neither registered nor specific protocol was used in this investigation. This review takes after the rules
put forward by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses articulation.
Accessible review, statistic, standard clinical and radiographic, intercession, and results information
were segregated from the studies and included for examination. Study, statistic, and randomized
clinical and radiographic information included time for testing, number of focuses included, trial areas,
number of patients, and trial enlistment criteria, for example, time from manifestation onset, age,
substantial vessel impediment, Alberta Stroke Program Early CT Score and NIH Stroke Scale (Barber
et al., 2000). Large vessel occlusion alludes to the nearness of thrombus inside proximal intracranial
vessels on imaging, which might be because of carotid ailment, cardioembolism, or different
wellsprings of thromboembolus. Treatment information incorporated the restorative modalities used in
the intercession and control arms, number of goal to-treat patients, number of patients who
experienced mechanical thrombectomy, IV tissue plasminogen, NIHSS score, mean age, large vessel
impediment on imaging, number of patients who experienced general anesthesia, and interim from
manifestation onset to IV-tissue plasminogen activator or groin puncture. The outcome of data
included from effective angiographic revascularization, characterized as changed thrombolysis in
cerebral ischemia review, modified Rankin Scale (mRS) score at 3 months taking after intercession.
7
online electronic resources including BNI (British Nursing Index), CINAHL (Cumulative Index to
Nursing and Allied Health Literature), EMBASE (the Excerpta Medica database), Pubmed, The DARE
(Database of Abstracts of Reviews of Effects), HTA (Health Technology Assessment Database) and
NHS (Economic Evaluation Database). In addition, the available textbooks, magazines and articles
from newspapers from library have been searched to find out the relevant literature for ischemic
stroke and its management. The search was made for past 25 years to collect the relevant sources
and link the evidences to the current context. Adequate measures were made to channel the quest for
the pertinent sources. The keywords utilized were ischemic stroke, treatment of acute ischemic
stroke, use of plasminogen activator, role of endothelial factors in ischemic stroke and progression of
treatment in ischemic stroke. The outcome of the search for the relevant sources has been depicted in
subsequent sections. More focus has been given for the stroke management utilizing endovascular
therapy and tissue plasminogen activator.
3.3.2. Review of literature review and extraction of essentials
Neither registered nor specific protocol was used in this investigation. This review takes after the rules
put forward by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses articulation.
Accessible review, statistic, standard clinical and radiographic, intercession, and results information
were segregated from the studies and included for examination. Study, statistic, and randomized
clinical and radiographic information included time for testing, number of focuses included, trial areas,
number of patients, and trial enlistment criteria, for example, time from manifestation onset, age,
substantial vessel impediment, Alberta Stroke Program Early CT Score and NIH Stroke Scale (Barber
et al., 2000). Large vessel occlusion alludes to the nearness of thrombus inside proximal intracranial
vessels on imaging, which might be because of carotid ailment, cardioembolism, or different
wellsprings of thromboembolus. Treatment information incorporated the restorative modalities used in
the intercession and control arms, number of goal to-treat patients, number of patients who
experienced mechanical thrombectomy, IV tissue plasminogen, NIHSS score, mean age, large vessel
impediment on imaging, number of patients who experienced general anesthesia, and interim from
manifestation onset to IV-tissue plasminogen activator or groin puncture. The outcome of data
included from effective angiographic revascularization, characterized as changed thrombolysis in
cerebral ischemia review, modified Rankin Scale (mRS) score at 3 months taking after intercession.
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
3.3.3. Statistical analysis
The data was subjected for the calculation of descriptive statistics utilizing Minitab Version 17, while
factual investigations of pooled information looking at mRS scores and mortality. Under the suspicions
of conceivable clinical variability and methodological contrasts among the included reviews, a
random-effects model was actualized in the investigations to represent examining variety and
sampling variation from every individual review. Investigation heterogeneity was identified utilizing the
χ2 and I2 test insights. Significant heterogeneity was thought to be available when both the χ2 esteem
was inside 10% level of importance (p < 0.10) and the I2 esteem surpassed half. The risk was also
evaluated for each study level. Every factual test was 2-sided, and p < 0.05 was considered
measurably critical.
4.0. Results
4.1. Selection of study
The depth search yielded around eight multicenter, planned randomized clinical trials. Interventional
management of stroke, local versus systemic thrombolysis for ischemic stroke (SNT), Mechanical
recovery and recanalization of stroke clusters utilizing embolectomy (MRS), Multicenter randomized
clinical trial of endovascular treatment for intense ischemic stroke in the Netherlands (MCN),
Evaluation investigation of congestive heart failure and aspiratory supply route catheterization
adequacy (ESC), Extending the ideal opportunity for thrombolysis in crisis neurological shortfalls intra-
blood vessel (EXT), Solitaire with the expectation for thrombectomy as essential endovascular
treatment (SPR), and endovascular revascularization with solitaire gadget versus best medicinal
treatment in foremost dissemination stroke inside 8 h (REV), involving around 2500 patients for
incorporation (Ciccone et al., 2013; Campbell et al., 2015). All studies were looked into for risk of
inclination, and all exhibited low risk for determination, location, whittling down, and detailing
predispositions. However, the reviews were judged to have high hazard for execution predisposition,
since the members and treatment groups were not blinded. Different predispositions included early
review end in 5 examines (REV, SPR, IMI, EXT and ESC), a predetermined number of patients who
experienced mechanical thrombectomy in one review (SNT), and imaging convention infringement in
one review (ESC).
4.2. Characteristics of the study
8
The data was subjected for the calculation of descriptive statistics utilizing Minitab Version 17, while
factual investigations of pooled information looking at mRS scores and mortality. Under the suspicions
of conceivable clinical variability and methodological contrasts among the included reviews, a
random-effects model was actualized in the investigations to represent examining variety and
sampling variation from every individual review. Investigation heterogeneity was identified utilizing the
χ2 and I2 test insights. Significant heterogeneity was thought to be available when both the χ2 esteem
was inside 10% level of importance (p < 0.10) and the I2 esteem surpassed half. The risk was also
evaluated for each study level. Every factual test was 2-sided, and p < 0.05 was considered
measurably critical.
4.0. Results
4.1. Selection of study
The depth search yielded around eight multicenter, planned randomized clinical trials. Interventional
management of stroke, local versus systemic thrombolysis for ischemic stroke (SNT), Mechanical
recovery and recanalization of stroke clusters utilizing embolectomy (MRS), Multicenter randomized
clinical trial of endovascular treatment for intense ischemic stroke in the Netherlands (MCN),
Evaluation investigation of congestive heart failure and aspiratory supply route catheterization
adequacy (ESC), Extending the ideal opportunity for thrombolysis in crisis neurological shortfalls intra-
blood vessel (EXT), Solitaire with the expectation for thrombectomy as essential endovascular
treatment (SPR), and endovascular revascularization with solitaire gadget versus best medicinal
treatment in foremost dissemination stroke inside 8 h (REV), involving around 2500 patients for
incorporation (Ciccone et al., 2013; Campbell et al., 2015). All studies were looked into for risk of
inclination, and all exhibited low risk for determination, location, whittling down, and detailing
predispositions. However, the reviews were judged to have high hazard for execution predisposition,
since the members and treatment groups were not blinded. Different predispositions included early
review end in 5 examines (REV, SPR, IMI, EXT and ESC), a predetermined number of patients who
experienced mechanical thrombectomy in one review (SNT), and imaging convention infringement in
one review (ESC).
4.2. Characteristics of the study
8
The summary of the reviews led in about 190 centers was shown in table-1. The result of intervention
and control arms was shown in table-2. The numbers of ITT patients in the mediation and control
arms were 1,313 and 1,110 patients. Tissue plasminogen was controlled in 990 (75%) and 986 (89%)
patients of the intercession and control arms, separately. Mechanical thrombectomy utilizing
retrievable (stent retriever) gadgets was performed in 569 (43%) patients of the intercession arm.
Tissue plasminogen IA was controlled in 498 (38%) patients of the mediation arm. Extensive vessel
impediment was available in 888 (78%) and 799 (86%) patients of the intercession and control arms,
separately. General anesthesia was managed in 143 (30%) patients of the intercession arm.
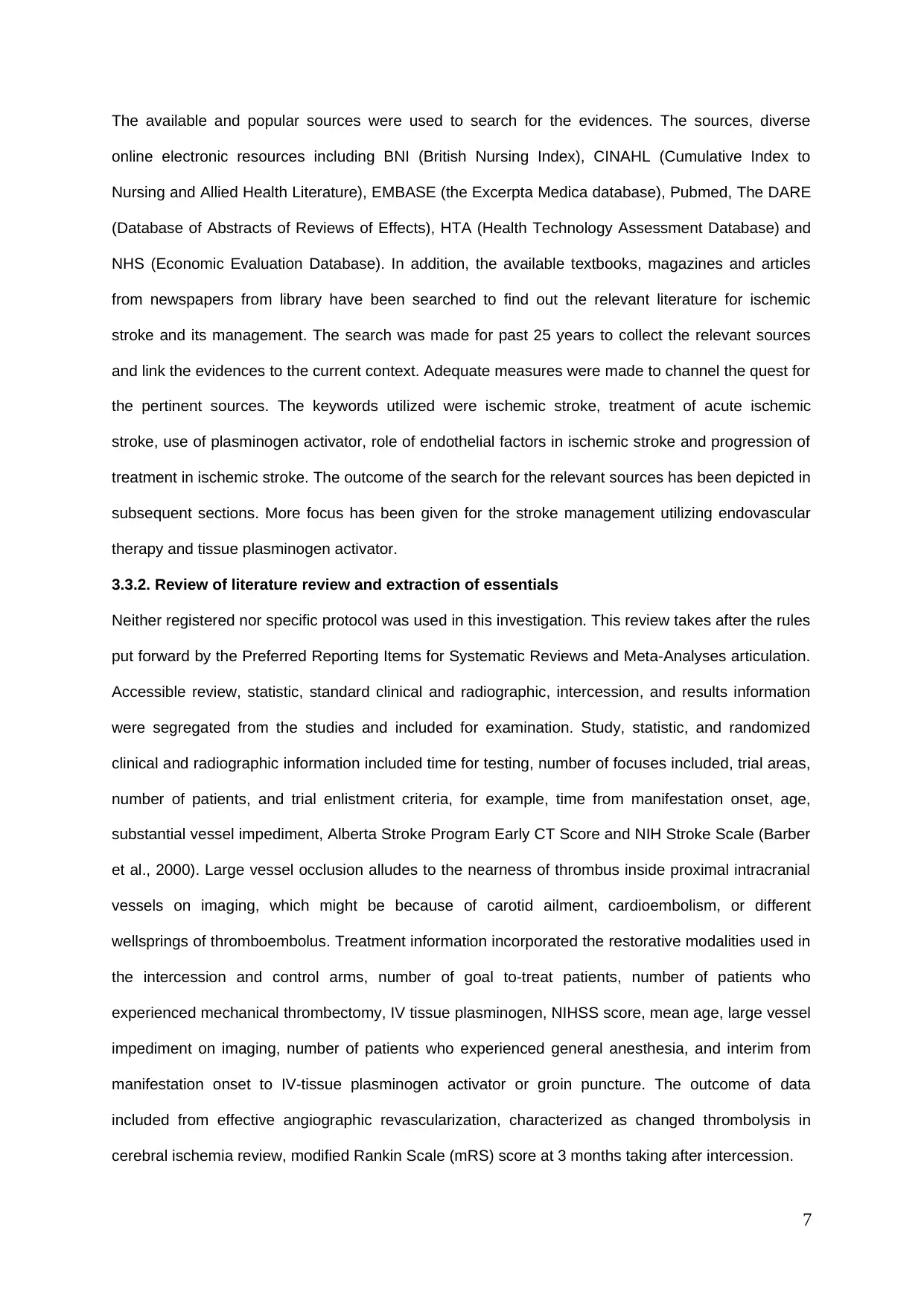
4.3. Comparison of hazard/advantage for the intervention Vs therapeutic administration
The mRS values for the intervention and control groups was shown in table-1 and complications in
table-2. Among the 1200 patients, 12%, 16%, 15%, 17%, 15%, 5% and 18% patients had a mRS
estimations of 0, 1, 2, 3, 4, 5, and 6 at 90 days, individually. Out of eight reviews, 3 concentrates
observed to be of irrelevant distinction between the two time frames. The five reviews demonstrated
better result with endovascular treatment. The utilitarian autonomy regarding mRS score was
obviously clear at 3 months for endovascular stroke intervention (Fig-1)
Fig-1: Comparison of functional independence for intervention and control arms, where 1,2, 3, 4, 5
and 6 are rescpetively for MRS, REV, SPR, ESC, EXT and MCN
9
Study group
% of Improvement
and control arms was shown in table-2. The numbers of ITT patients in the mediation and control
arms were 1,313 and 1,110 patients. Tissue plasminogen was controlled in 990 (75%) and 986 (89%)
patients of the intercession and control arms, separately. Mechanical thrombectomy utilizing
retrievable (stent retriever) gadgets was performed in 569 (43%) patients of the intercession arm.
Tissue plasminogen IA was controlled in 498 (38%) patients of the mediation arm. Extensive vessel
impediment was available in 888 (78%) and 799 (86%) patients of the intercession and control arms,
separately. General anesthesia was managed in 143 (30%) patients of the intercession arm.
4.3. Comparison of hazard/advantage for the intervention Vs therapeutic administration
The mRS values for the intervention and control groups was shown in table-1 and complications in
table-2. Among the 1200 patients, 12%, 16%, 15%, 17%, 15%, 5% and 18% patients had a mRS
estimations of 0, 1, 2, 3, 4, 5, and 6 at 90 days, individually. Out of eight reviews, 3 concentrates
observed to be of irrelevant distinction between the two time frames. The five reviews demonstrated
better result with endovascular treatment. The utilitarian autonomy regarding mRS score was
obviously clear at 3 months for endovascular stroke intervention (Fig-1)
Fig-1: Comparison of functional independence for intervention and control arms, where 1,2, 3, 4, 5
and 6 are rescpetively for MRS, REV, SPR, ESC, EXT and MCN
9
Study group
% of Improvement
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
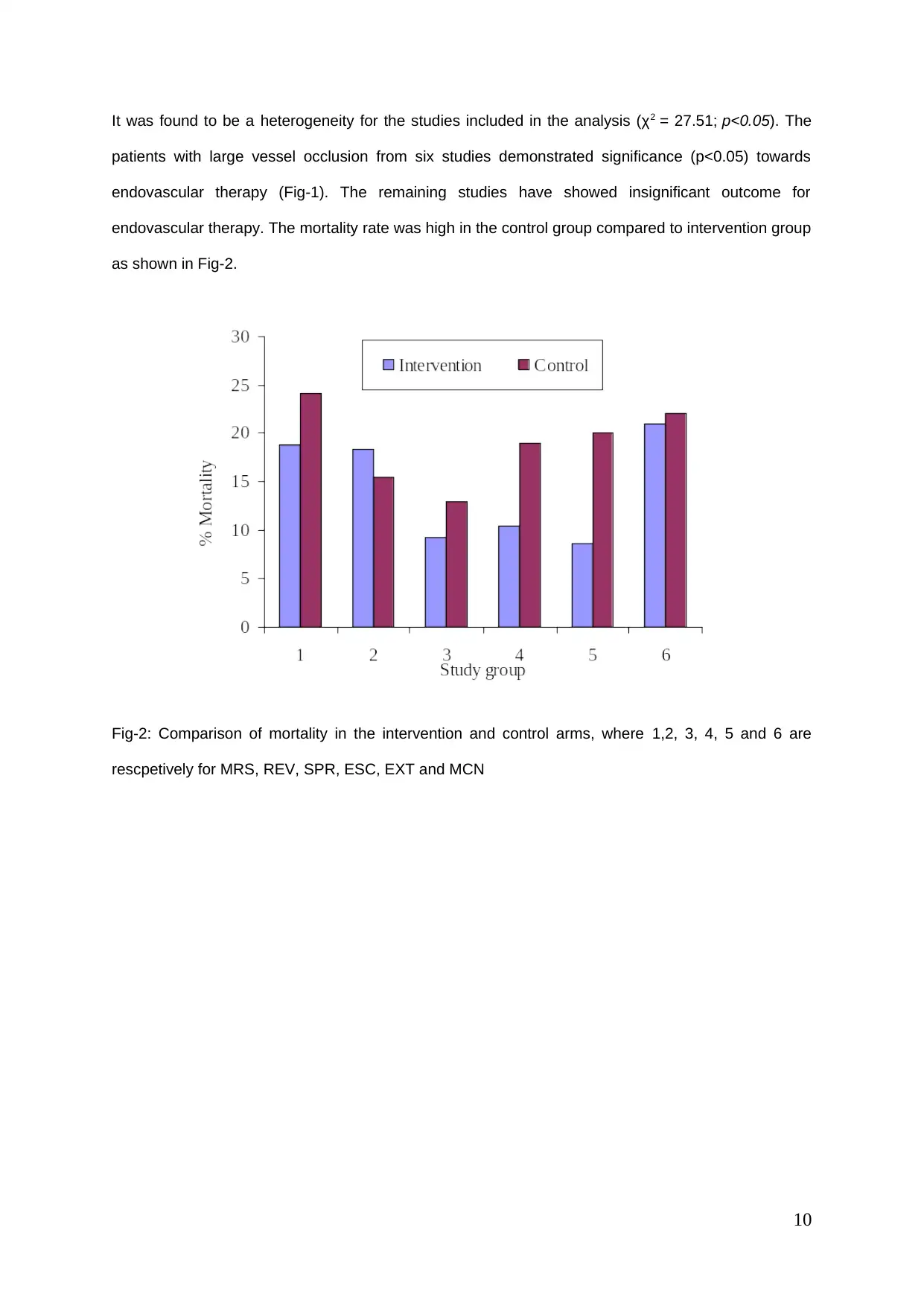
It was found to be a heterogeneity for the studies included in the analysis (χ2 = 27.51; p<0.05). The
patients with large vessel occlusion from six studies demonstrated significance (p<0.05) towards
endovascular therapy (Fig-1). The remaining studies have showed insignificant outcome for
endovascular therapy. The mortality rate was high in the control group compared to intervention group
as shown in Fig-2.
Fig-2: Comparison of mortality in the intervention and control arms, where 1,2, 3, 4, 5 and 6 are
rescpetively for MRS, REV, SPR, ESC, EXT and MCN
10
patients with large vessel occlusion from six studies demonstrated significance (p<0.05) towards
endovascular therapy (Fig-1). The remaining studies have showed insignificant outcome for
endovascular therapy. The mortality rate was high in the control group compared to intervention group
as shown in Fig-2.
Fig-2: Comparison of mortality in the intervention and control arms, where 1,2, 3, 4, 5 and 6 are
rescpetively for MRS, REV, SPR, ESC, EXT and MCN
10
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
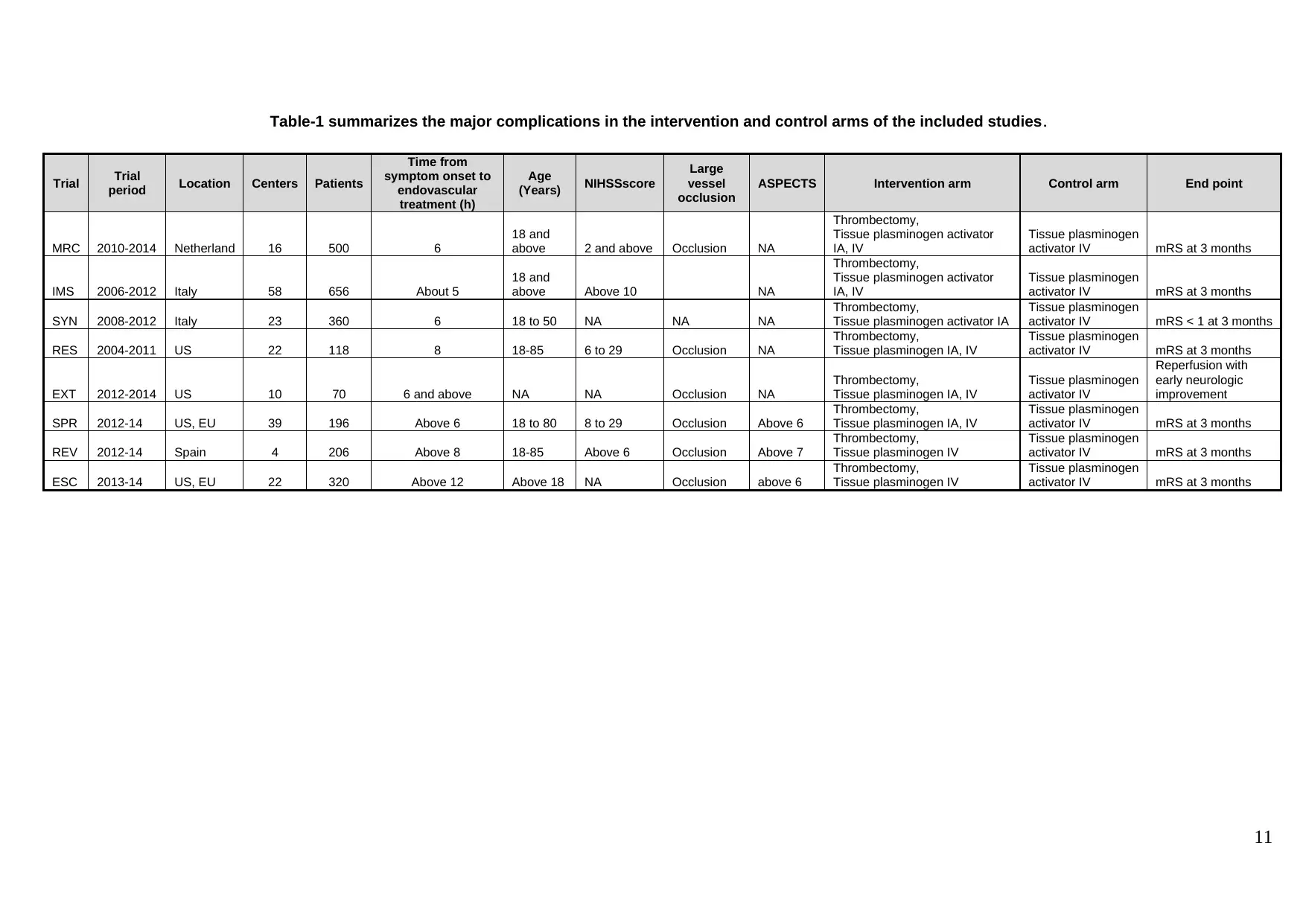
Table-1 summarizes the major complications in the intervention and control arms of the included studies.
Trial Trial
period Location Centers Patients
Time from
symptom onset to
endovascular
treatment (h)
Age
(Years) NIHSSscore
Large
vessel
occlusion
ASPECTS Intervention arm Control arm End point
MRC 2010-2014 Netherland 16 500 6
18 and
above 2 and above Occlusion NA
Thrombectomy,
Tissue plasminogen activator
IA, IV
Tissue plasminogen
activator IV mRS at 3 months
IMS 2006-2012 Italy 58 656 About 5
18 and
above Above 10 NA
Thrombectomy,
Tissue plasminogen activator
IA, IV
Tissue plasminogen
activator IV mRS at 3 months
SYN 2008-2012 Italy 23 360 6 18 to 50 NA NA NA
Thrombectomy,
Tissue plasminogen activator IA
Tissue plasminogen
activator IV mRS < 1 at 3 months
RES 2004-2011 US 22 118 8 18-85 6 to 29 Occlusion NA
Thrombectomy,
Tissue plasminogen IA, IV
Tissue plasminogen
activator IV mRS at 3 months
EXT 2012-2014 US 10 70 6 and above NA NA Occlusion NA
Thrombectomy,
Tissue plasminogen IA, IV
Tissue plasminogen
activator IV
Reperfusion with
early neurologic
improvement
SPR 2012-14 US, EU 39 196 Above 6 18 to 80 8 to 29 Occlusion Above 6
Thrombectomy,
Tissue plasminogen IA, IV
Tissue plasminogen
activator IV mRS at 3 months
REV 2012-14 Spain 4 206 Above 8 18-85 Above 6 Occlusion Above 7
Thrombectomy,
Tissue plasminogen IV
Tissue plasminogen
activator IV mRS at 3 months
ESC 2013-14 US, EU 22 320 Above 12 Above 18 NA Occlusion above 6
Thrombectomy,
Tissue plasminogen IV
Tissue plasminogen
activator IV mRS at 3 months
11
Trial Trial
period Location Centers Patients
Time from
symptom onset to
endovascular
treatment (h)
Age
(Years) NIHSSscore
Large
vessel
occlusion
ASPECTS Intervention arm Control arm End point
MRC 2010-2014 Netherland 16 500 6
18 and
above 2 and above Occlusion NA
Thrombectomy,
Tissue plasminogen activator
IA, IV
Tissue plasminogen
activator IV mRS at 3 months
IMS 2006-2012 Italy 58 656 About 5
18 and
above Above 10 NA
Thrombectomy,
Tissue plasminogen activator
IA, IV
Tissue plasminogen
activator IV mRS at 3 months
SYN 2008-2012 Italy 23 360 6 18 to 50 NA NA NA
Thrombectomy,
Tissue plasminogen activator IA
Tissue plasminogen
activator IV mRS < 1 at 3 months
RES 2004-2011 US 22 118 8 18-85 6 to 29 Occlusion NA
Thrombectomy,
Tissue plasminogen IA, IV
Tissue plasminogen
activator IV mRS at 3 months
EXT 2012-2014 US 10 70 6 and above NA NA Occlusion NA
Thrombectomy,
Tissue plasminogen IA, IV
Tissue plasminogen
activator IV
Reperfusion with
early neurologic
improvement
SPR 2012-14 US, EU 39 196 Above 6 18 to 80 8 to 29 Occlusion Above 6
Thrombectomy,
Tissue plasminogen IA, IV
Tissue plasminogen
activator IV mRS at 3 months
REV 2012-14 Spain 4 206 Above 8 18-85 Above 6 Occlusion Above 7
Thrombectomy,
Tissue plasminogen IV
Tissue plasminogen
activator IV mRS at 3 months
ESC 2013-14 US, EU 22 320 Above 12 Above 18 NA Occlusion above 6
Thrombectomy,
Tissue plasminogen IV
Tissue plasminogen
activator IV mRS at 3 months
11
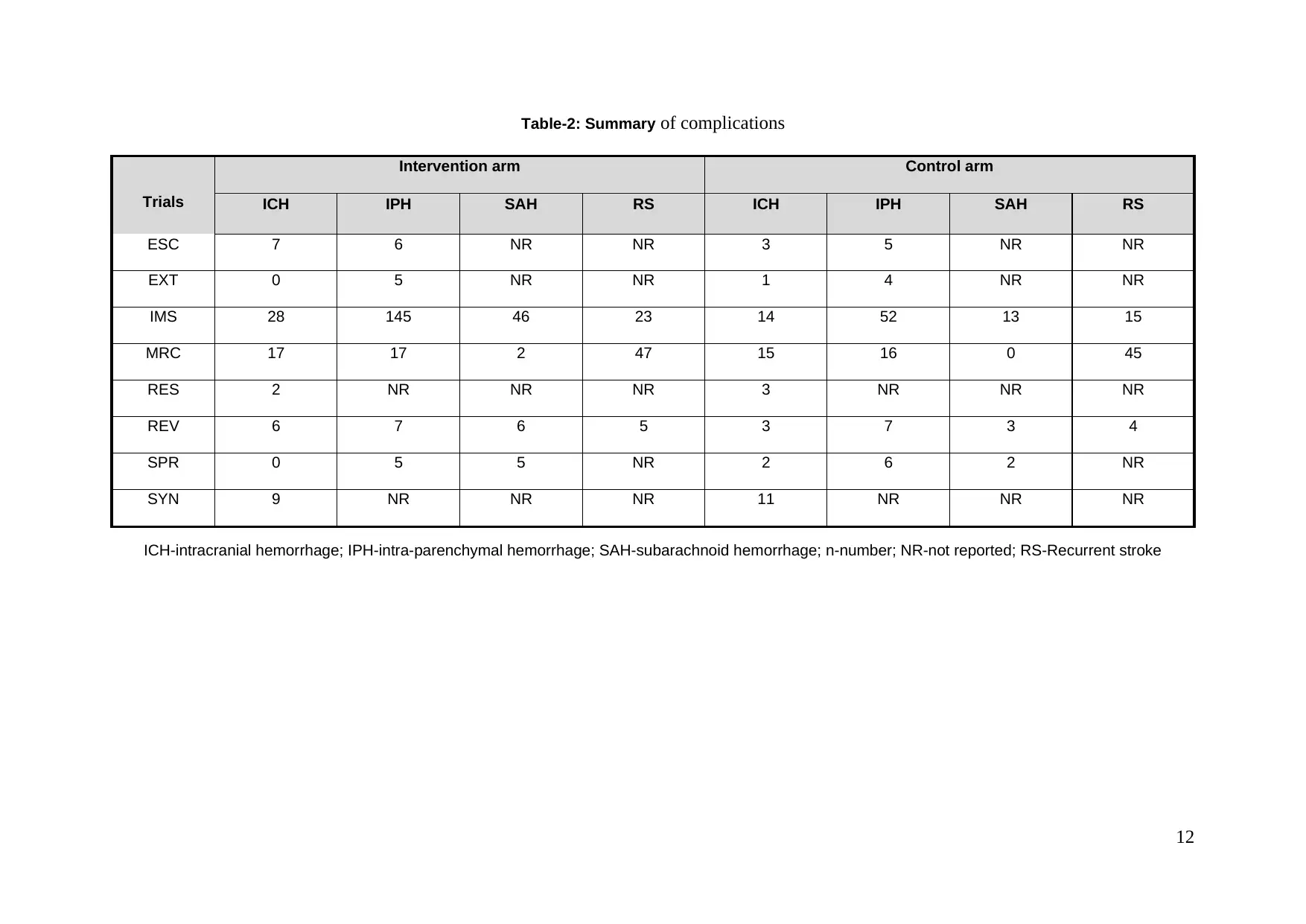
Table-2: Summary of complications
Trials
Intervention arm Control arm
ICH IPH SAH RS ICH IPH SAH RS
ESC 7 6 NR NR 3 5 NR NR
EXT 0 5 NR NR 1 4 NR NR
IMS 28 145 46 23 14 52 13 15
MRC 17 17 2 47 15 16 0 45
RES 2 NR NR NR 3 NR NR NR
REV 6 7 6 5 3 7 3 4
SPR 0 5 5 NR 2 6 2 NR
SYN 9 NR NR NR 11 NR NR NR
ICH-intracranial hemorrhage; IPH-intra-parenchymal hemorrhage; SAH-subarachnoid hemorrhage; n-number; NR-not reported; RS-Recurrent stroke
12
Trials
Intervention arm Control arm
ICH IPH SAH RS ICH IPH SAH RS
ESC 7 6 NR NR 3 5 NR NR
EXT 0 5 NR NR 1 4 NR NR
IMS 28 145 46 23 14 52 13 15
MRC 17 17 2 47 15 16 0 45
RES 2 NR NR NR 3 NR NR NR
REV 6 7 6 5 3 7 3 4
SPR 0 5 5 NR 2 6 2 NR
SYN 9 NR NR NR 11 NR NR NR
ICH-intracranial hemorrhage; IPH-intra-parenchymal hemorrhage; SAH-subarachnoid hemorrhage; n-number; NR-not reported; RS-Recurrent stroke
12
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 17
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




