BNNS 6123 - Case Study: Wound Infection and Nursing Interventions
VerifiedAdded on 2023/04/22
|12
|4032
|294
Case Study
AI Summary
This case study focuses on Martha, a 65-year-old female patient with a severely infected diabetic foot ulcer. The assignment details Martha's medical history, including her struggle with diabetes management and family history of the disease. It covers the anatomy and physiology of the foot, explaining how peripheral neuropathy leads to foot ulcers. The pathophysiology of inflammation and infection is discussed, highlighting the role of high blood glucose levels and impaired immune response. The nursing assessment includes identifying signs of foot ulcers, skin assessment, and temperature measurements to classify the wound as moderately infected. The nursing diagnosis and care plan are outlined, focusing on inspecting the foot for blisters and cuts. Desklib provides students with access to similar solved assignments and past papers for comprehensive study support.
Running head: EPISODE OF WOUND INFECTION
EPISODE OF WOUND INFECTION
Name of the student:
Name of the university:
Author note:
Acknowledgement:
I would like to express my special thanks of gratitude towards my professor, unit head,
as well as our principal who helped throughout the development of this assignment. I would also
want to thank to my facilitator who helped me in gaining new knowledge and supported me
throughout my placement days.
Secondly, I would like to thank my parents as well as my friends who contributed in
finalizing this project within the limited period.
EPISODE OF WOUND INFECTION
Name of the student:
Name of the university:
Author note:
Acknowledgement:
I would like to express my special thanks of gratitude towards my professor, unit head,
as well as our principal who helped throughout the development of this assignment. I would also
want to thank to my facilitator who helped me in gaining new knowledge and supported me
throughout my placement days.
Secondly, I would like to thank my parents as well as my friends who contributed in
finalizing this project within the limited period.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1
EPISODE OF WOUND INFECTION
Introduction of the case:
Foot ulcers are one of the common complications that are faced by diabetic patients who
have unmanaged blood glucose level. Foot ulcers occur as a result of breaking of the skin
tissue and thereby exposing the layers underneath. They are usually common under the big
toes and the balls of the feet and can even affect to the range of bones (Yazdanpanah et al.,
2015). This assignment would be mainly based on caring for a patient named Martha who had
come to the ward with complaints of severely infected diabetic foot ulcer, seeking for support.
This assignment would mainly cover detailed data of the patient, pathophysiology and
inflammation of the wounds, nursing assessment and identification of the wounds. Nursing
diagnosis, interventions medicinal treatments and even clinical progress of Martha was also
covered in the assignment.
Status of the patient:
The patient is named Martha Samuels who is a female and is 65 years old. She lives
alone in her apartment and her immediate family members live in other cities. She is seen to
struggle with her diabetes management often forgetting her medications and not assessing her
blood glucose levels for long periods. She does not believe that any treatment can help her
EPISODE OF WOUND INFECTION
Introduction of the case:
Foot ulcers are one of the common complications that are faced by diabetic patients who
have unmanaged blood glucose level. Foot ulcers occur as a result of breaking of the skin
tissue and thereby exposing the layers underneath. They are usually common under the big
toes and the balls of the feet and can even affect to the range of bones (Yazdanpanah et al.,
2015). This assignment would be mainly based on caring for a patient named Martha who had
come to the ward with complaints of severely infected diabetic foot ulcer, seeking for support.
This assignment would mainly cover detailed data of the patient, pathophysiology and
inflammation of the wounds, nursing assessment and identification of the wounds. Nursing
diagnosis, interventions medicinal treatments and even clinical progress of Martha was also
covered in the assignment.
Status of the patient:
The patient is named Martha Samuels who is a female and is 65 years old. She lives
alone in her apartment and her immediate family members live in other cities. She is seen to
struggle with her diabetes management often forgetting her medications and not assessing her
blood glucose levels for long periods. She does not believe that any treatment can help her
2
EPISODE OF WOUND INFECTION
overcome the issues and is quite hopeless because of her suffering for last twelve years. Her
parents were also diabetic. She had not gone through any surgeries in her entire life. She had
left her education midway and started working in a departmental store from young age. Her
education level was low with no health literacy about how to manage her diabetes. Currently,
she had visited the ward with the complaints of wounds in her feet not healing for many days
and worsening of its condition day by day. She was fearful of leg-amputation as she had heard
one of her friend whose fingers had to be amputed because of such infections.
Anatomy and physiology of the organ that affected the service user:
The foot is divided into three sections. The first part is the forefoot that includes toes,
phalanges and other 14 toe bones along with five metatarsals. They help in propulsions and
provide attachment to several tendons. The second part is the midfoot made up of five
irregularly shaped bones called tarsals. They help in forming the arch of the foot and help in
weight bearing. The third part is the hind-foot consisting of two large bones called talus and
calcaneus (Van Netten et al., 2016). Other parts are the muscles controlling the movements of
the foot, originate in lower legs, and attached to bones in the foot with tendons. Tensions and
ligaments help in smooth movement of the bones and joints helping in walking, balancing and
many others. Diabetic foot ulcer due to peripheral neuropathy occurs when the nerves in the
foot extremities become numb resulting in loss of feeling of sensation (Hinchliffe et al., 2016).
This lack of sensation reduces the awareness of the patients when the feet develop cuts,
blisters and sores. The skin tissues and muscles might be infected with germs resulting in
severe conditions. Similar has been found to have occurred with Martha.
Pathophysiology of the inflammation and infection to the wound:
Diabetic peripheral neuropathy can be described as the precipitating factor that is found
in almost about 90% of the diabetic foot ulcers. Studies opine that high blood glucose level
results in damaging of the nerves that often include sensory, motor and even autonomic nerves.
Even the condition also affects the immune system that results in impairment of the ability of the
body for fighting infection. Sensory nerves mainly help in enabling people to feel pain as well as
temperature and other sensations. When such nerves of a diabetic person gets affected, they
may no longer be able to feel the cold, pain in their feet (Skafjeld et al., 2015). Any cut or foot
sores as well as burn from hot water and even exposure to extreme cold might completely get
unnoticed by persons because of lack of sensation and numbness. The sore or the cut areas
EPISODE OF WOUND INFECTION
overcome the issues and is quite hopeless because of her suffering for last twelve years. Her
parents were also diabetic. She had not gone through any surgeries in her entire life. She had
left her education midway and started working in a departmental store from young age. Her
education level was low with no health literacy about how to manage her diabetes. Currently,
she had visited the ward with the complaints of wounds in her feet not healing for many days
and worsening of its condition day by day. She was fearful of leg-amputation as she had heard
one of her friend whose fingers had to be amputed because of such infections.
Anatomy and physiology of the organ that affected the service user:
The foot is divided into three sections. The first part is the forefoot that includes toes,
phalanges and other 14 toe bones along with five metatarsals. They help in propulsions and
provide attachment to several tendons. The second part is the midfoot made up of five
irregularly shaped bones called tarsals. They help in forming the arch of the foot and help in
weight bearing. The third part is the hind-foot consisting of two large bones called talus and
calcaneus (Van Netten et al., 2016). Other parts are the muscles controlling the movements of
the foot, originate in lower legs, and attached to bones in the foot with tendons. Tensions and
ligaments help in smooth movement of the bones and joints helping in walking, balancing and
many others. Diabetic foot ulcer due to peripheral neuropathy occurs when the nerves in the
foot extremities become numb resulting in loss of feeling of sensation (Hinchliffe et al., 2016).
This lack of sensation reduces the awareness of the patients when the feet develop cuts,
blisters and sores. The skin tissues and muscles might be infected with germs resulting in
severe conditions. Similar has been found to have occurred with Martha.
Pathophysiology of the inflammation and infection to the wound:
Diabetic peripheral neuropathy can be described as the precipitating factor that is found
in almost about 90% of the diabetic foot ulcers. Studies opine that high blood glucose level
results in damaging of the nerves that often include sensory, motor and even autonomic nerves.
Even the condition also affects the immune system that results in impairment of the ability of the
body for fighting infection. Sensory nerves mainly help in enabling people to feel pain as well as
temperature and other sensations. When such nerves of a diabetic person gets affected, they
may no longer be able to feel the cold, pain in their feet (Skafjeld et al., 2015). Any cut or foot
sores as well as burn from hot water and even exposure to extreme cold might completely get
unnoticed by persons because of lack of sensation and numbness. The sore or the cut areas
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3
EPISODE OF WOUND INFECTION
can then become infected and might not heal properly because the impaired ability of the body
in fighting infection.
This condition also results in development of muscle weakness as well as loss of
reflexes mainly at the ankle region. This might cause various changes when the person walks
and lead to different types of foot abnormalities (Boulton, 2018). Similar such limping had been
noticed when Martha was asked to walk down in order to identify the pressure areas on her foot.
Studies are of the opinion that this plays an important role in the development of pathway of
diabetic foot ulcers because they result in contributing to abnormal pressures like that in the
plantar areas like heel and bottom predisposing it to ulceration. Often it has been seen that
shoes that no longer fits the new condition due to the abnormalities as well as deformed foot
ulcers the rates of the foot that are numb because of the sensory neuropathy. When such
conditions are not treated promptly, the ulcers are infected and spread to bone causing
osteomyelitis. However, Martha’s foot condition was not found to be such serious that surgery
was required as osteomyelitis had not occurred in her.
Inflammation is the first stage of wound healing procedure that mainly stops after
bleeding stops. It can be described as the procedure by which chemicals from the white blood
cells are released into the wound sites thereby causing symptoms like redness and warmth
(Bus et al., 2016). This action is important as inflammation helps in protection of the affected
areas in from harmful bacteria and viruses. Chemicals also cause leakage of the fluids causing
swelling and stimulation of the nerves that create pain that people feel during inflammation.
Studies opine that these are normal steps of wound healing. However, they also suggest that in
certain cases, inflammation may be excessive and this leads to many health complications with
excessive swelling, redness and other symptoms. In case if Martha, she complained that the
inflammation and swelling wee not reducing and the wounds were not healing at all.
Often many researchers have the query as to why diabetic ulcers cannot be healed
entirely. Proteases namely metalloprteinases cause degradiation of the extraclleular matrix so
that they can be remodelled into mature tissue with appropriate tensile strength. They help in
keratinocyte and fibroblast migration along with inflammation, tissue re-organisation and even
remodelling of the wounded tissue. Higher concentrations of pro-inflammatory cytokines in case
of diabetic foot ulcers cause the MMP activities to increase by 30 fold as in comparison to that
of acute wound healing (Rasmussen et al., 2015). MMP-9 and MMP -2 over-expression are the
main causes that result in non-healing of the wounds in diabetic foot ulcers balance in the ratio
EPISODE OF WOUND INFECTION
can then become infected and might not heal properly because the impaired ability of the body
in fighting infection.
This condition also results in development of muscle weakness as well as loss of
reflexes mainly at the ankle region. This might cause various changes when the person walks
and lead to different types of foot abnormalities (Boulton, 2018). Similar such limping had been
noticed when Martha was asked to walk down in order to identify the pressure areas on her foot.
Studies are of the opinion that this plays an important role in the development of pathway of
diabetic foot ulcers because they result in contributing to abnormal pressures like that in the
plantar areas like heel and bottom predisposing it to ulceration. Often it has been seen that
shoes that no longer fits the new condition due to the abnormalities as well as deformed foot
ulcers the rates of the foot that are numb because of the sensory neuropathy. When such
conditions are not treated promptly, the ulcers are infected and spread to bone causing
osteomyelitis. However, Martha’s foot condition was not found to be such serious that surgery
was required as osteomyelitis had not occurred in her.
Inflammation is the first stage of wound healing procedure that mainly stops after
bleeding stops. It can be described as the procedure by which chemicals from the white blood
cells are released into the wound sites thereby causing symptoms like redness and warmth
(Bus et al., 2016). This action is important as inflammation helps in protection of the affected
areas in from harmful bacteria and viruses. Chemicals also cause leakage of the fluids causing
swelling and stimulation of the nerves that create pain that people feel during inflammation.
Studies opine that these are normal steps of wound healing. However, they also suggest that in
certain cases, inflammation may be excessive and this leads to many health complications with
excessive swelling, redness and other symptoms. In case if Martha, she complained that the
inflammation and swelling wee not reducing and the wounds were not healing at all.
Often many researchers have the query as to why diabetic ulcers cannot be healed
entirely. Proteases namely metalloprteinases cause degradiation of the extraclleular matrix so
that they can be remodelled into mature tissue with appropriate tensile strength. They help in
keratinocyte and fibroblast migration along with inflammation, tissue re-organisation and even
remodelling of the wounded tissue. Higher concentrations of pro-inflammatory cytokines in case
of diabetic foot ulcers cause the MMP activities to increase by 30 fold as in comparison to that
of acute wound healing (Rasmussen et al., 2015). MMP-9 and MMP -2 over-expression are the
main causes that result in non-healing of the wounds in diabetic foot ulcers balance in the ratio
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4
EPISODE OF WOUND INFECTION
of MMP and tissue inhibitor of metalloproteinase called TIMP helps in maintaining the
proteolytic balance and this ratio is seen to get disturbed in diabetic ulcer causing non-healing
conditions.
Nursing assessment of the patient for identifying the issue of wound infection:
One of the first sign of the foot ulcer that was noticed in the patient named Martha was
her drainage from the foot that had stained her socks and leaked out in her shoes. Some of the
identification signs that help nurses to develop a preliminary idea about the occurrence of foot
ulcer in the patients are unusual swelling, redness, irritation, redness and even odors from one
foot or both the feet (Kumarasinghe et al., 2018)). In case of Martha, it was found that her feet
were unusually swelled up and there were redness surrounding the wounds. These
assessments along with consideration of the medical history of the patient about unmanaged
diabetes and high level of blood glucose level helped in considering the wound to be a
complication of diabetes only. One of the most visible sign of serious foot ulcer is the black
tissue called the Escher surrounding the ulcer (Torkington-Stokes et al., 2016). Such black
tissues were found to be present in the wounds created by foot ulcer in Martha. Partial
gangrene was also found in the wounds. Studies suggest that partial as well as complete
gangrene mainly refers to the tissue death that occur due to infections and these are seen to
appear around the ulcers (Schaarup et al., ). In such cases, odorous discharge and even
numbness can occur (Tsang et al., 2016). Martha was also complaining of such discharge from
her wound sites and certain discharge although less in amount was found. This helped to
understand that gangrenous condition was developing in the wounds of Martha.
Skin assessment was done for Martha. Studies are of the opinion that general
dermatologic assessment helps in understanding the skin quality and whether there is any form
of trophic changes that would include xerosis, alopecia, previous areas of scarring, atrophies
blanche as well as condition of the nails (Yusuf et al., 2016). It was found that Martha had dry
and fragile skin. Wound assessment also needs to include different wound measurements that
would include length, width as well as depth of the wounds. Wound assessment was also done
in case of Martha also to find out whether there were exposed structures or probe towards bone
or preiwind condition, presence of callus as well as edges of the wound, quality of the exudates
and even local or spreading signs of the infection.
It also becomes important for the nursing professionals to measure the foot temperature
in order to assess the condition of the wounds. Studies state that tether are five important
EPISODE OF WOUND INFECTION
of MMP and tissue inhibitor of metalloproteinase called TIMP helps in maintaining the
proteolytic balance and this ratio is seen to get disturbed in diabetic ulcer causing non-healing
conditions.
Nursing assessment of the patient for identifying the issue of wound infection:
One of the first sign of the foot ulcer that was noticed in the patient named Martha was
her drainage from the foot that had stained her socks and leaked out in her shoes. Some of the
identification signs that help nurses to develop a preliminary idea about the occurrence of foot
ulcer in the patients are unusual swelling, redness, irritation, redness and even odors from one
foot or both the feet (Kumarasinghe et al., 2018)). In case of Martha, it was found that her feet
were unusually swelled up and there were redness surrounding the wounds. These
assessments along with consideration of the medical history of the patient about unmanaged
diabetes and high level of blood glucose level helped in considering the wound to be a
complication of diabetes only. One of the most visible sign of serious foot ulcer is the black
tissue called the Escher surrounding the ulcer (Torkington-Stokes et al., 2016). Such black
tissues were found to be present in the wounds created by foot ulcer in Martha. Partial
gangrene was also found in the wounds. Studies suggest that partial as well as complete
gangrene mainly refers to the tissue death that occur due to infections and these are seen to
appear around the ulcers (Schaarup et al., ). In such cases, odorous discharge and even
numbness can occur (Tsang et al., 2016). Martha was also complaining of such discharge from
her wound sites and certain discharge although less in amount was found. This helped to
understand that gangrenous condition was developing in the wounds of Martha.
Skin assessment was done for Martha. Studies are of the opinion that general
dermatologic assessment helps in understanding the skin quality and whether there is any form
of trophic changes that would include xerosis, alopecia, previous areas of scarring, atrophies
blanche as well as condition of the nails (Yusuf et al., 2016). It was found that Martha had dry
and fragile skin. Wound assessment also needs to include different wound measurements that
would include length, width as well as depth of the wounds. Wound assessment was also done
in case of Martha also to find out whether there were exposed structures or probe towards bone
or preiwind condition, presence of callus as well as edges of the wound, quality of the exudates
and even local or spreading signs of the infection.
It also becomes important for the nursing professionals to measure the foot temperature
in order to assess the condition of the wounds. Studies state that tether are five important
5
EPISODE OF WOUND INFECTION
cardinal signs of inflammation in foot ulcer cases that include pain, erythema, edema as well as
loss of function and heat (Uckay et al., 2018). The measuring of the skin temperature can be
seen as the marker for the inflammation as well as injury development in the insensate foot.
Many researchers have talked about the positive relationship among the inflammatory
procedures, tissue breakdowns and that of increasing in the local skin temperatures (Tsang et
al., 2017).Infrared thermography is one of the non-contact tools that help in detection
of the surface temperature of the particular point on an object (Orneholm et al.,
2017). It was used for Martha and her foot temperature was quite elevated showing
signs of worsened pathological procedures like that of soft tissue inflammation and
even subsequent breakdown.
From the entire investigation above, the foot ulcer investigation of Martha was classified
to be moderate. Studies are of the opinion that infection along with purulence and/or with one or
two manifestations of inflammation in patients (who is systematically well and metabolically
stable) are considered to be moderate. To consider the wound to be moderate, patients need to
have one of the characteristics that include “cellulitis extending more than 2 cm around the
ulcer; lymphangitic streaking; spread beneath the superficial fascia; deep tissue abscess;
gangrene; involvement of muscle, tendon, joint, or bone” (Muller et al., 2016). As Martha
satisfied the conditions with the presence of gangrene and purulence, it can be stated that she
has moderate wound infection.
Identification of the nursing diagnosis and nursing care plan:
When individuals are suspected to have foot ulcer, they are first ask to inspect the foot,
toes, toenails for any blisters, cuts as well as scratches and even ingrown nails leading to
ulcers. The nurse would then evaluate the rate of the blood flow in the foot by the feeling of
pulses. Martha was then asked to stand and walk. This helps the nurses to evaluate how the
weight of the body is distributed in the patients across the bones and joints in the feet. Limps
indicate structural damage and an uneven gait might cause the blister to form. X-ray was also
done to diagnose the disorder. This helps in assessing changes in the alignment of the bones in
the foot that contribute to ulcer development. It can also help in revealing loss of mass of bone.
This might occur as the result of hormonal imbalances related to diabetes (Orneholm et al.,
2017). MRI scans were also used for Martha. This helps in using the magnetic field and ratio
waves for creating three dimensional as well as computerized images of the soft tissues inside
EPISODE OF WOUND INFECTION
cardinal signs of inflammation in foot ulcer cases that include pain, erythema, edema as well as
loss of function and heat (Uckay et al., 2018). The measuring of the skin temperature can be
seen as the marker for the inflammation as well as injury development in the insensate foot.
Many researchers have talked about the positive relationship among the inflammatory
procedures, tissue breakdowns and that of increasing in the local skin temperatures (Tsang et
al., 2017).Infrared thermography is one of the non-contact tools that help in detection
of the surface temperature of the particular point on an object (Orneholm et al.,
2017). It was used for Martha and her foot temperature was quite elevated showing
signs of worsened pathological procedures like that of soft tissue inflammation and
even subsequent breakdown.
From the entire investigation above, the foot ulcer investigation of Martha was classified
to be moderate. Studies are of the opinion that infection along with purulence and/or with one or
two manifestations of inflammation in patients (who is systematically well and metabolically
stable) are considered to be moderate. To consider the wound to be moderate, patients need to
have one of the characteristics that include “cellulitis extending more than 2 cm around the
ulcer; lymphangitic streaking; spread beneath the superficial fascia; deep tissue abscess;
gangrene; involvement of muscle, tendon, joint, or bone” (Muller et al., 2016). As Martha
satisfied the conditions with the presence of gangrene and purulence, it can be stated that she
has moderate wound infection.
Identification of the nursing diagnosis and nursing care plan:
When individuals are suspected to have foot ulcer, they are first ask to inspect the foot,
toes, toenails for any blisters, cuts as well as scratches and even ingrown nails leading to
ulcers. The nurse would then evaluate the rate of the blood flow in the foot by the feeling of
pulses. Martha was then asked to stand and walk. This helps the nurses to evaluate how the
weight of the body is distributed in the patients across the bones and joints in the feet. Limps
indicate structural damage and an uneven gait might cause the blister to form. X-ray was also
done to diagnose the disorder. This helps in assessing changes in the alignment of the bones in
the foot that contribute to ulcer development. It can also help in revealing loss of mass of bone.
This might occur as the result of hormonal imbalances related to diabetes (Orneholm et al.,
2017). MRI scans were also used for Martha. This helps in using the magnetic field and ratio
waves for creating three dimensional as well as computerized images of the soft tissues inside
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6
EPISODE OF WOUND INFECTION
the body (Uckay et al., 2018). This was done by the nurse to find out extent of the damage
caused by the ulcer in Martha. When signs of infection like that of redness, selling and warmth
are found in wounds, doctors also recommend blood tests and similar was also done for
Martha.
The wound needs to be dressed for allowing careful inspection for the evidence of
healing as well as early identification of the new necrotic tissues. At first, the necrotic tissues in
the wounds of Martha were debrided with the help of topical debriding agents. Studies suggest
the removal of pressure from the foot wounds to be necessary for healing (Orneholm et al.,
2017). In Martha, this was achieved through the total contact with casting, removable cast
walkers as well as various ambulatory braces, splints, modified half shows and others. Studies
suggest that edema delay wound healing (Yusuf et al., 2016). Therefore, edema in her was
controlled with the help of compression stockings, leg elevation, and pneumatic pedal
compression device. This help in enhancing the healing processes. Studies suggest that many
tropical treatments are available for foot ulcers that include dressing containing silver or silver
sulphadizine cream or polyhexamethylene biguanide (PHMB) gel or solutions. Other studies
suggest iodine (either povidone or cadexomer) or medical grade honey in ointment or gel form.
For Martha, silver sulphadiazine cream-dressings were done. Treatment for Martha thereby
included preparation of the wound bed, cleaning of wounds, management of products that were
applied to the bed and perilesional skin, preapartion of physical exercise plan and continuous
client empowerment.
Medication treatment:
Various antibiotics need to be provided to the patient for treating of the ulcers. Many of
these antibiotics are seen to attack Staphylococcus aureus which are the bacteria that are
known for staph infections as well as for the ß-haemolytic Streptococcus that are present in
intestines (Uckay et al., 2018). Nursing professionals mainly tried to provide infections for
“streptococci, MRSA, aerobic gram-negative bacilli, and anaerobes”. Studies have put forward
different medications that include “ampicillin-sulbactam, piperacillin-tazobactam, meropenem, or
ertapenem” for gram-negative becateria. “ceftriaxone, cefepime, levofloxacin, moxifloxacin, or
aztreonam plus metronidazole also used for aerobic gram negative and anaerobic organisms
(Orneholm et al., 2017). For Martha, levofloxacin was suggested as bacterial analysis
showed presence of gram-negative bacteria in her wounds.
EPISODE OF WOUND INFECTION
the body (Uckay et al., 2018). This was done by the nurse to find out extent of the damage
caused by the ulcer in Martha. When signs of infection like that of redness, selling and warmth
are found in wounds, doctors also recommend blood tests and similar was also done for
Martha.
The wound needs to be dressed for allowing careful inspection for the evidence of
healing as well as early identification of the new necrotic tissues. At first, the necrotic tissues in
the wounds of Martha were debrided with the help of topical debriding agents. Studies suggest
the removal of pressure from the foot wounds to be necessary for healing (Orneholm et al.,
2017). In Martha, this was achieved through the total contact with casting, removable cast
walkers as well as various ambulatory braces, splints, modified half shows and others. Studies
suggest that edema delay wound healing (Yusuf et al., 2016). Therefore, edema in her was
controlled with the help of compression stockings, leg elevation, and pneumatic pedal
compression device. This help in enhancing the healing processes. Studies suggest that many
tropical treatments are available for foot ulcers that include dressing containing silver or silver
sulphadizine cream or polyhexamethylene biguanide (PHMB) gel or solutions. Other studies
suggest iodine (either povidone or cadexomer) or medical grade honey in ointment or gel form.
For Martha, silver sulphadiazine cream-dressings were done. Treatment for Martha thereby
included preparation of the wound bed, cleaning of wounds, management of products that were
applied to the bed and perilesional skin, preapartion of physical exercise plan and continuous
client empowerment.
Medication treatment:
Various antibiotics need to be provided to the patient for treating of the ulcers. Many of
these antibiotics are seen to attack Staphylococcus aureus which are the bacteria that are
known for staph infections as well as for the ß-haemolytic Streptococcus that are present in
intestines (Uckay et al., 2018). Nursing professionals mainly tried to provide infections for
“streptococci, MRSA, aerobic gram-negative bacilli, and anaerobes”. Studies have put forward
different medications that include “ampicillin-sulbactam, piperacillin-tazobactam, meropenem, or
ertapenem” for gram-negative becateria. “ceftriaxone, cefepime, levofloxacin, moxifloxacin, or
aztreonam plus metronidazole also used for aerobic gram negative and anaerobic organisms
(Orneholm et al., 2017). For Martha, levofloxacin was suggested as bacterial analysis
showed presence of gram-negative bacteria in her wounds.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

7
EPISODE OF WOUND INFECTION
Clinical progress of the patient:
The nursing professional caring for Martha first evaluated whether the discharge had
stopped or not. It was found that not only the discharge had stopped but also the inflammation
had reduced. The swelling as well as the redness had reduced. Moreover, the dressing
frequency of the wound had also decreased implying that the wounds were gradually healing.
Foot temperature had been also analyzed which showed that the foot temperature had reduced
indicating the infected wound was gradually healing.
EPISODE OF WOUND INFECTION
Clinical progress of the patient:
The nursing professional caring for Martha first evaluated whether the discharge had
stopped or not. It was found that not only the discharge had stopped but also the inflammation
had reduced. The swelling as well as the redness had reduced. Moreover, the dressing
frequency of the wound had also decreased implying that the wounds were gradually healing.
Foot temperature had been also analyzed which showed that the foot temperature had reduced
indicating the infected wound was gradually healing.
8
EPISODE OF WOUND INFECTION
References:
Boulton, A. J. (2018). The diabetic foot. Medicine. https://doi.org/10.1016/j.mpmed.2018.11.001
Bus, S. A., Armstrong, D. G., Van Deursen, R. W., Lewis, J. E. A., Caravaggi, C. F., Cavanagh,
P. R., & International Working Group on the Diabetic Foot (IWGDF). (2016). IWGDF
guidance on footwear and offloading interventions to prevent and heal foot ulcers in
patients with diabetes. Diabetes/metabolism research and reviews, 32, 25-36.
https://doi.org/10.1002/dmrr.2697
Hinchliffe, R. J., Brownrigg, J. R. W., Apelqvist, J., Boyko, E. J., Fitridge, R., Mills, J. L., ... &
International Working Group on the Diabetic Foot (IWGDF). (2016). IWGDF guidance on
the diagnosis, prognosis and management of peripheral artery disease in patients with
foot ulcers in diabetes. Diabetes/metabolism research and reviews, 32, 37-44.
https://doi.org/10.1002/dmrr.2698
Kumarasinghe, S. A., Hettiarachchi, P., & Wasalathanthri, S. (2018). Nurses' knowledge on
diabetic foot ulcer disease and their attitudes towards patients affected: A cross‐
sectional institution‐based study. Journal of clinical nursing, 27(1-2), e203-e212.
https://doi.org/10.1016/j.ijmedinf.2015.05.012
Muller, M., David-Tchouda, S., Margier, J., Oreglia, M., & Benhamou, P. Y. (2016). Comment on
rasmussen et al. a randomized controlled trial comparing telemedical and standard
outpatient monitoring of diabetic foot ulcers. diabetes care 2015; 38: 1723–
1729. Diabetes care, 39(1), e9-e10. https://doi.org/10.2337/dc15-1659
Örneholm, H., Apelqvist, J., Larsson, J., & Eneroth, M. (2017). Recurrent and other new foot
ulcers after healed plantar forefoot diabetic ulcer. Wound Repair and
Regeneration, 25(2), 309-315. https://doi.org/10.1111/wrr.12522
Rasmussen, B. S. B., Jensen, L. K., Froekjaer, J., Kidholm, K., Kensing, F., & Yderstraede, K.
B. (2015). A qualitative study of the key factors in implementing telemedical monitoring
of diabetic foot ulcer patients. International journal of medical informatics, 84(10), 799-
807. https://doi.org/10.1016/j.ijmedinf.2015.05.012
EPISODE OF WOUND INFECTION
References:
Boulton, A. J. (2018). The diabetic foot. Medicine. https://doi.org/10.1016/j.mpmed.2018.11.001
Bus, S. A., Armstrong, D. G., Van Deursen, R. W., Lewis, J. E. A., Caravaggi, C. F., Cavanagh,
P. R., & International Working Group on the Diabetic Foot (IWGDF). (2016). IWGDF
guidance on footwear and offloading interventions to prevent and heal foot ulcers in
patients with diabetes. Diabetes/metabolism research and reviews, 32, 25-36.
https://doi.org/10.1002/dmrr.2697
Hinchliffe, R. J., Brownrigg, J. R. W., Apelqvist, J., Boyko, E. J., Fitridge, R., Mills, J. L., ... &
International Working Group on the Diabetic Foot (IWGDF). (2016). IWGDF guidance on
the diagnosis, prognosis and management of peripheral artery disease in patients with
foot ulcers in diabetes. Diabetes/metabolism research and reviews, 32, 37-44.
https://doi.org/10.1002/dmrr.2698
Kumarasinghe, S. A., Hettiarachchi, P., & Wasalathanthri, S. (2018). Nurses' knowledge on
diabetic foot ulcer disease and their attitudes towards patients affected: A cross‐
sectional institution‐based study. Journal of clinical nursing, 27(1-2), e203-e212.
https://doi.org/10.1016/j.ijmedinf.2015.05.012
Muller, M., David-Tchouda, S., Margier, J., Oreglia, M., & Benhamou, P. Y. (2016). Comment on
rasmussen et al. a randomized controlled trial comparing telemedical and standard
outpatient monitoring of diabetic foot ulcers. diabetes care 2015; 38: 1723–
1729. Diabetes care, 39(1), e9-e10. https://doi.org/10.2337/dc15-1659
Örneholm, H., Apelqvist, J., Larsson, J., & Eneroth, M. (2017). Recurrent and other new foot
ulcers after healed plantar forefoot diabetic ulcer. Wound Repair and
Regeneration, 25(2), 309-315. https://doi.org/10.1111/wrr.12522
Rasmussen, B. S. B., Jensen, L. K., Froekjaer, J., Kidholm, K., Kensing, F., & Yderstraede, K.
B. (2015). A qualitative study of the key factors in implementing telemedical monitoring
of diabetic foot ulcer patients. International journal of medical informatics, 84(10), 799-
807. https://doi.org/10.1016/j.ijmedinf.2015.05.012
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9
EPISODE OF WOUND INFECTION
Schaarup, C., Pape-Haugaard, L., Jensen, M. H., Laursen, A. C., Bermark, S., & Hejlesen, O.
K. (2017). Probing community nurses' professional basis: a situational case study in
diabetic foot ulcer treatment. British journal of community nursing, 22(Sup3), S46-S52.
https://doi.org/10.12968/bjcn.2017.22.Sup3.S46
Skafjeld, A., Iversen, M. M., Holme, I., Ribu, L., Hvaal, K., & Kilhovd, B. K. (2015). A pilot study
testing the feasibility of skin temperature monitoring to reduce recurrent foot ulcers in
patients with diabetes–a randomized controlled trial. BMC endocrine disorders, 15(1),
55. https://doi.org/10.1186/s12902-015-0054-x
Torkington-Stokes, R., Metcalf, D., & Bowler, P. (2016). Management of diabetic foot ulcers:
evaluation of case studies. British Journal of Nursing, 25(15), S27-S33.
https://doi.org/10.12968/bjon.2016.25.15.S27
Tsang, K. K. (2016). A pilot randomized controlled trial of nanocrystalline silver dressing against
manuka honey dressing and conventional dressing in healing diabetic foot
ulcer (Doctoral dissertation, The Hong Kong Polytechnic University).
http://ira.lib.polyu.edu.hk/handle/10397/67225
Tsang, K. K., Kwong, E. W. Y., To, T. S. S., Chung, J. W. Y., & Wong, T. K. S. (2017). A pilot
randomized, controlled study of nanocrystalline silver, manuka honey, and conventional
dressing in healing diabetic foot ulcer. Evidence-Based Complementary and Alternative
Medicine, 2017. https://doi.org/10.2337/dc15-1659
Uçkay, I., Kressmann, B., Malacarne, S., Toumanova, A., Jaafar, J., Lew, D., & Lipsky, B. A.
(2018). A randomized, controlled study to investigate the efficacy and safety of a topical
gentamicin-collagen sponge in combination with systemic antibiotic therapy in diabetic
patients with a moderate or severe foot ulcer infection. BMC infectious diseases, 18(1),
361. https://www.hindawi.com/journals/ecam/2017/5294890/abs/
Van Netten, J. J., Price, P. E., Lavery, L. A., Monteiro‐Soares, M., Rasmussen, A., Jubiz, Y., ...
& International Working Group on the Diabetic Foot (IWGDF). (2016). Prevention of foot
ulcers in the at‐risk patient with diabetes: a systematic review. Diabetes/metabolism
research and reviews, 32, 84-98. https://doi.org/10.1002/dmrr.2701
Yazdanpanah, L., Nasiri, M., & Adarvishi, S. (2015). Literature review on the management of
diabetic foot ulcer. World journal of diabetes, 6(1), 37. doi: 10.4239/wjd.v6.i1.37
EPISODE OF WOUND INFECTION
Schaarup, C., Pape-Haugaard, L., Jensen, M. H., Laursen, A. C., Bermark, S., & Hejlesen, O.
K. (2017). Probing community nurses' professional basis: a situational case study in
diabetic foot ulcer treatment. British journal of community nursing, 22(Sup3), S46-S52.
https://doi.org/10.12968/bjcn.2017.22.Sup3.S46
Skafjeld, A., Iversen, M. M., Holme, I., Ribu, L., Hvaal, K., & Kilhovd, B. K. (2015). A pilot study
testing the feasibility of skin temperature monitoring to reduce recurrent foot ulcers in
patients with diabetes–a randomized controlled trial. BMC endocrine disorders, 15(1),
55. https://doi.org/10.1186/s12902-015-0054-x
Torkington-Stokes, R., Metcalf, D., & Bowler, P. (2016). Management of diabetic foot ulcers:
evaluation of case studies. British Journal of Nursing, 25(15), S27-S33.
https://doi.org/10.12968/bjon.2016.25.15.S27
Tsang, K. K. (2016). A pilot randomized controlled trial of nanocrystalline silver dressing against
manuka honey dressing and conventional dressing in healing diabetic foot
ulcer (Doctoral dissertation, The Hong Kong Polytechnic University).
http://ira.lib.polyu.edu.hk/handle/10397/67225
Tsang, K. K., Kwong, E. W. Y., To, T. S. S., Chung, J. W. Y., & Wong, T. K. S. (2017). A pilot
randomized, controlled study of nanocrystalline silver, manuka honey, and conventional
dressing in healing diabetic foot ulcer. Evidence-Based Complementary and Alternative
Medicine, 2017. https://doi.org/10.2337/dc15-1659
Uçkay, I., Kressmann, B., Malacarne, S., Toumanova, A., Jaafar, J., Lew, D., & Lipsky, B. A.
(2018). A randomized, controlled study to investigate the efficacy and safety of a topical
gentamicin-collagen sponge in combination with systemic antibiotic therapy in diabetic
patients with a moderate or severe foot ulcer infection. BMC infectious diseases, 18(1),
361. https://www.hindawi.com/journals/ecam/2017/5294890/abs/
Van Netten, J. J., Price, P. E., Lavery, L. A., Monteiro‐Soares, M., Rasmussen, A., Jubiz, Y., ...
& International Working Group on the Diabetic Foot (IWGDF). (2016). Prevention of foot
ulcers in the at‐risk patient with diabetes: a systematic review. Diabetes/metabolism
research and reviews, 32, 84-98. https://doi.org/10.1002/dmrr.2701
Yazdanpanah, L., Nasiri, M., & Adarvishi, S. (2015). Literature review on the management of
diabetic foot ulcer. World journal of diabetes, 6(1), 37. doi: 10.4239/wjd.v6.i1.37
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10
EPISODE OF WOUND INFECTION
Yusuf, S., Okuwa, M., Irwan, M., Rassa, S., Laitung, B., Thalib, A., ... & Sugama, J. (2016).
Prevalence and risk factor of diabetic foot ulcers in a regional hospital, eastern
Indonesia. Open Journal of Nursing, 6(01), 1. DOI: 10.4236/ojn.2016.61001
Appendices:
Medications used:
1. Levofloxacin (Gram negative bacteria)
2. Aztreonam (Gram negative bacteria)
3. Ampilcillin-sulbactum (Gram negative bacteria)
4. Minocycline (Gram positive bacteria)
Wound healing process:
1. Debridement – removing of the necrotic tissues as well as callus, facilitating drainage
and stimulating healing
2. Infection control – reducing of the bacterial burden as well as restoring a stable bacterial
balance
3. Off-loading – redistributing the plantar pressure, help in reduction of the incidence of
ulceration
4. Regranex – had been used as the adjunct towards good ulcer care that help in
stimulating the recruitment as well as proliferation of the cells involved in wound repair
mechanisms.
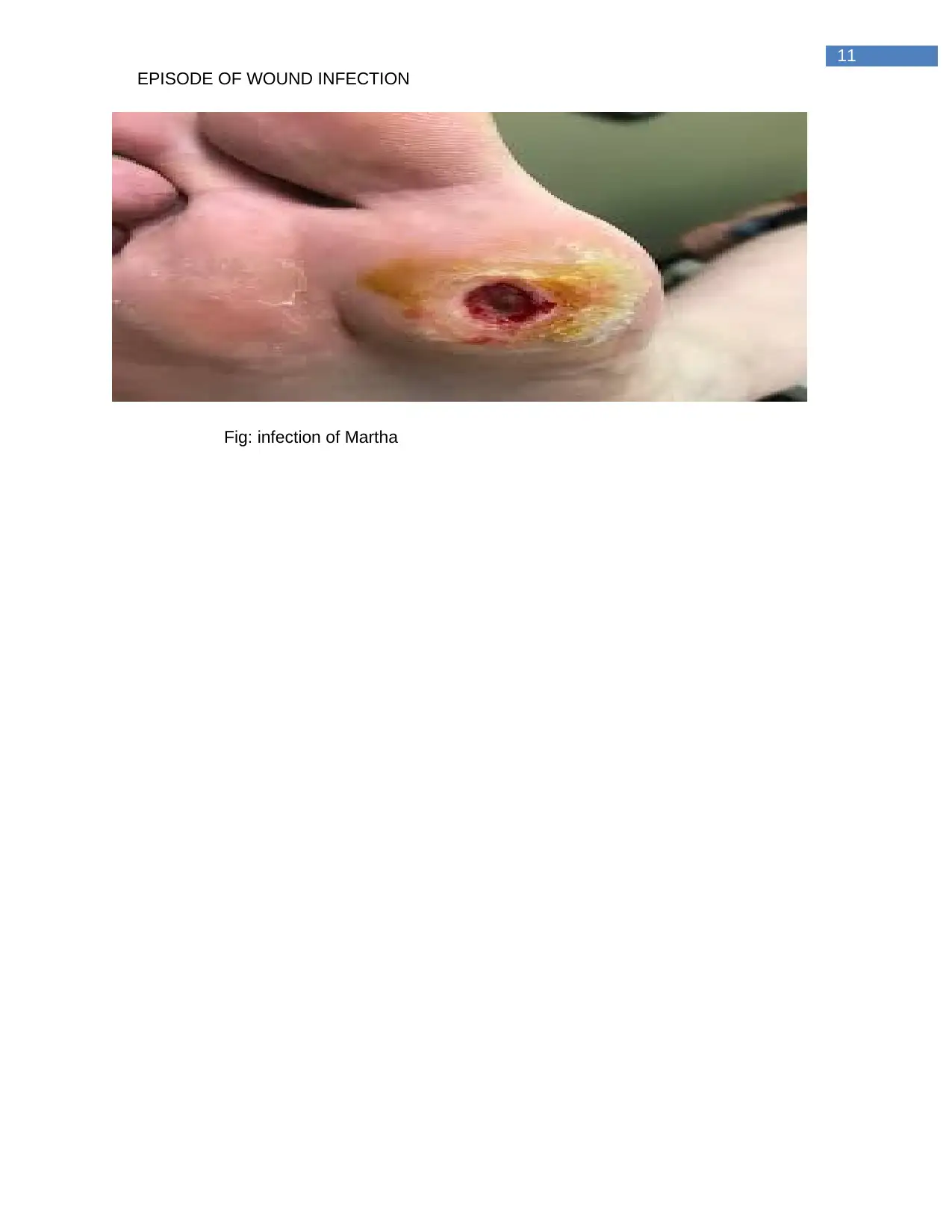
Diagrams:
EPISODE OF WOUND INFECTION
Yusuf, S., Okuwa, M., Irwan, M., Rassa, S., Laitung, B., Thalib, A., ... & Sugama, J. (2016).
Prevalence and risk factor of diabetic foot ulcers in a regional hospital, eastern
Indonesia. Open Journal of Nursing, 6(01), 1. DOI: 10.4236/ojn.2016.61001
Appendices:
Medications used:
1. Levofloxacin (Gram negative bacteria)
2. Aztreonam (Gram negative bacteria)
3. Ampilcillin-sulbactum (Gram negative bacteria)
4. Minocycline (Gram positive bacteria)
Wound healing process:
1. Debridement – removing of the necrotic tissues as well as callus, facilitating drainage
and stimulating healing
2. Infection control – reducing of the bacterial burden as well as restoring a stable bacterial
balance
3. Off-loading – redistributing the plantar pressure, help in reduction of the incidence of
ulceration
4. Regranex – had been used as the adjunct towards good ulcer care that help in
stimulating the recruitment as well as proliferation of the cells involved in wound repair
mechanisms.
Diagrams:
11
EPISODE OF WOUND INFECTION
Fig: infection of Martha
EPISODE OF WOUND INFECTION
Fig: infection of Martha
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




