Chronic Obstructive Pulmonary Disorder
VerifiedAdded on 2023/04/21
|12
|2436
|194
AI Summary
This document provides information about Chronic Obstructive Pulmonary Disorder (COPD), including a case presentation, subjective and objective data, medication details, safety requirements, patient education, contraindications, side effects, and nursing interventions. It also includes a summary of the information acquired from the case study.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running header: CHRONIC OBSTRUCTIVE PULMONARY DISORDER 1
Chronic obstructive pulmonary disorder
Student’s name
Students ID
Specialty area
Chronic obstructive pulmonary disorder
Student’s name
Students ID
Specialty area
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
2
Case presentation
a. Subjective data
Mr. X is a 50-year-old Caucasian male. He is married with six children and eight
grandchildren who all stay together in a rental house in the rural village. He was brought to
the emergency department with shortness of breath, wheezing and chest tightness. His
symptoms started three days before and have been progressively worsening with no relieving
or aggravating factors. Two years ago he was diagnosed with an acute obstructive pulmonary
disease which required immediate hospitalization. He was prescribed albuterol, nicotine
patches, and aminophylline. He denies abdominal pain, nausea, vomiting, and diarrhea. His
family history includes diabetes and prostate cancer. He has a positive social history of
smoking. He currently smokes eight cigarettes per day and drinks 6-8 bears per day.
b. Objective data
Physical examination
Vital signs: temperature 36.4 degrees Celsius, blood pressure 112/72mm/Hg, respiratory rate
32, a pulse of 68 beats/min and lastly oxygen partial saturation 80% on room air. Cardiovascular:
there is a regular rhythm and normal heart sounds with no murmurs. There is a strong pulse in all
four extremities. Respiratory: the client presents with tachypnea, wheezing, reduced air
movements bilaterally and bilateral rhonchi. The client is unable to finish a full sentence due to
dyspnea. Skin: the skin is very dry. ECG result indicated reduced voltage in lead I, III, aVL, aVR
and IVF. Chest X-ray showed bibasilar airspace disease indicating the presence of alveolar
edema. Lastly, there is the presence of small bilateral pleural effusions.
Case presentation
a. Subjective data
Mr. X is a 50-year-old Caucasian male. He is married with six children and eight
grandchildren who all stay together in a rental house in the rural village. He was brought to
the emergency department with shortness of breath, wheezing and chest tightness. His
symptoms started three days before and have been progressively worsening with no relieving
or aggravating factors. Two years ago he was diagnosed with an acute obstructive pulmonary
disease which required immediate hospitalization. He was prescribed albuterol, nicotine
patches, and aminophylline. He denies abdominal pain, nausea, vomiting, and diarrhea. His
family history includes diabetes and prostate cancer. He has a positive social history of
smoking. He currently smokes eight cigarettes per day and drinks 6-8 bears per day.
b. Objective data
Physical examination
Vital signs: temperature 36.4 degrees Celsius, blood pressure 112/72mm/Hg, respiratory rate
32, a pulse of 68 beats/min and lastly oxygen partial saturation 80% on room air. Cardiovascular:
there is a regular rhythm and normal heart sounds with no murmurs. There is a strong pulse in all
four extremities. Respiratory: the client presents with tachypnea, wheezing, reduced air
movements bilaterally and bilateral rhonchi. The client is unable to finish a full sentence due to
dyspnea. Skin: the skin is very dry. ECG result indicated reduced voltage in lead I, III, aVL, aVR
and IVF. Chest X-ray showed bibasilar airspace disease indicating the presence of alveolar
edema. Lastly, there is the presence of small bilateral pleural effusions.
3
Medication
Ipratropium bromide is used in the treatment of COPD. It is administered nasally to prevent
dyspnea, coughing and chest tightness. Ipratropium is classified as a bronchodilator. It acts by
widening constricted airways, thereby reducing airflow resistance (Neilsen, Biisgard and
Ifversen 2013, pp 2105-2109).
i. The rationale for the route of administration
Ipratropium is administered through nasal inhalation. It acts by blocking the action of
acetylcholine on bronchi and nasal passages. Ipratropium is administered nasally because it acts
directly on the airways at the lungs that are constricted. The nerves use acetylcholine to
communicate with muscle cells. In COPD, cholinergic nerves located in the nerves causes
constriction of airways by causing the muscles close to the airways to contract. The
anticholinergic effect of ipratropium is preventing the effect of cholinergic nerves that cause the
dilation of airways and relaxation of airways (Neild and Cameron 2014, pp 671-680). Nerves that
use acetylcholine also control mucus glands in the nose. By blocking acetylcholine, the drug
facilitates the symptoms of allergies by stopping the mucus glands from producing mucus.
ii. Indication for administration
Ipratropium bromide is used in the treatment or prevents symptoms such as shortness of
breath or wheezing associated with chronic obstructive pulmonary diseases such as emphysema
and chronic bronchitis. It also used in the treatment of rhinorrhea which is mostly caused by non-
allergic or allergic perennial rhinitis (More, Wenzel and Meyers 2016, pp 315-323).
Medication
Ipratropium bromide is used in the treatment of COPD. It is administered nasally to prevent
dyspnea, coughing and chest tightness. Ipratropium is classified as a bronchodilator. It acts by
widening constricted airways, thereby reducing airflow resistance (Neilsen, Biisgard and
Ifversen 2013, pp 2105-2109).
i. The rationale for the route of administration
Ipratropium is administered through nasal inhalation. It acts by blocking the action of
acetylcholine on bronchi and nasal passages. Ipratropium is administered nasally because it acts
directly on the airways at the lungs that are constricted. The nerves use acetylcholine to
communicate with muscle cells. In COPD, cholinergic nerves located in the nerves causes
constriction of airways by causing the muscles close to the airways to contract. The
anticholinergic effect of ipratropium is preventing the effect of cholinergic nerves that cause the
dilation of airways and relaxation of airways (Neild and Cameron 2014, pp 671-680). Nerves that
use acetylcholine also control mucus glands in the nose. By blocking acetylcholine, the drug
facilitates the symptoms of allergies by stopping the mucus glands from producing mucus.
ii. Indication for administration
Ipratropium bromide is used in the treatment or prevents symptoms such as shortness of
breath or wheezing associated with chronic obstructive pulmonary diseases such as emphysema
and chronic bronchitis. It also used in the treatment of rhinorrhea which is mostly caused by non-
allergic or allergic perennial rhinitis (More, Wenzel and Meyers 2016, pp 315-323).
4
iii. Safety requirement during an administration
Care must be taken not to allow the medication to get into the eyes. If the spray gets into the
eyes it may cause eye discomfort, mydriasis, blurred vision, and lastly corneal congestion. In
case the drugs are accidentally sprayed into the eyes, the patient is advised to consult their
physician. The client should stop taking the medication in case hypersensitivity reactions such as
skin rash, angioedema and laryngospasms occur (Rebuck, Chapman and Wolkove 2014, pp 59-
64).
iv. Patient education
Educate the client on how to use the intranasal route. The patient should blow the nose before
administration. Prior to use, pump by releasing the spray three times into the air. The drug should
also be stored at 25°C and avoid freezing. Discuss with the client on the specific use of the drug
and its side effects. The client may experience headache, pharyngitis and dry nose. Ask the client
to report immediately to the physician in case vision changes occur. Advice the patient to use
sugar-free gum so as to help with dry mouth, keep delivery devices clean and lastly taking a
missed dose the moment he remembers unless the time for the next dose is near (Restrepo 2015,
pp 833-851).
v. Contraindication
Driving or operation of machines
The common side effects of ipratropium are dizziness and blurred vision. Individuals who
drive or use heavy machines should take precaution in case they start experiencing these
symptoms (Westby, Gibson and Benson 2017, pp 56-60).
iii. Safety requirement during an administration
Care must be taken not to allow the medication to get into the eyes. If the spray gets into the
eyes it may cause eye discomfort, mydriasis, blurred vision, and lastly corneal congestion. In
case the drugs are accidentally sprayed into the eyes, the patient is advised to consult their
physician. The client should stop taking the medication in case hypersensitivity reactions such as
skin rash, angioedema and laryngospasms occur (Rebuck, Chapman and Wolkove 2014, pp 59-
64).
iv. Patient education
Educate the client on how to use the intranasal route. The patient should blow the nose before
administration. Prior to use, pump by releasing the spray three times into the air. The drug should
also be stored at 25°C and avoid freezing. Discuss with the client on the specific use of the drug
and its side effects. The client may experience headache, pharyngitis and dry nose. Ask the client
to report immediately to the physician in case vision changes occur. Advice the patient to use
sugar-free gum so as to help with dry mouth, keep delivery devices clean and lastly taking a
missed dose the moment he remembers unless the time for the next dose is near (Restrepo 2015,
pp 833-851).
v. Contraindication
Driving or operation of machines
The common side effects of ipratropium are dizziness and blurred vision. Individuals who
drive or use heavy machines should take precaution in case they start experiencing these
symptoms (Westby, Gibson and Benson 2017, pp 56-60).
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
5
Clients with urinary retention, bladder obstruction, and prostatic hypertrophy
Anticholinergic medication should be used cautiously in patients with this condition.
Ipratropium may induce urinary retention to clients with these conditions.
Clients with paradoxical bronchospasm or acute bronchospasm
Ipratropium is similar to atropine. Its use is contraindicated in clients with ipratropium
bromide hypersensitivity. The drug produces paradoxical bronchospasms which can be life-
threatening to some patient. This problem is mostly seen in patients who have inhaled the newly
opened canister for the first time (Westby, Gibson and Benson 2017, pp 56-60).
Clients the closed angle glaucoma
All anticholinergic should be used with precaution for clients with closed-angle glaucoma.
Ipratropium raises aqueous outflow resistance and intraocular pressure for clients with closed
angle glaucoma. If the drug gets into the eyes, it may lead to blurred vision, pain and lastly visual
impairment (Westby, Gibson and Benson 2017, pp 56-60).
vi. Side effects/ adverse effects
Severe effects include anaphylactoid reactions, angioedema, laryngospasms, visual
impairment, arrhythmia exacerbation and bronchospasms (Roughead and Lexchin 2013, pp 315-
316).
Moderate side effects include hypotension, blurred vision, urinary retention, sinus
tachycardia, palpitations, constipation, conjunctivitis, oral ulcerations, sinus tachycardia and
dyspnea (Roughead and Lexchin 2013, pp 315-316).
Clients with urinary retention, bladder obstruction, and prostatic hypertrophy
Anticholinergic medication should be used cautiously in patients with this condition.
Ipratropium may induce urinary retention to clients with these conditions.
Clients with paradoxical bronchospasm or acute bronchospasm
Ipratropium is similar to atropine. Its use is contraindicated in clients with ipratropium
bromide hypersensitivity. The drug produces paradoxical bronchospasms which can be life-
threatening to some patient. This problem is mostly seen in patients who have inhaled the newly
opened canister for the first time (Westby, Gibson and Benson 2017, pp 56-60).
Clients the closed angle glaucoma
All anticholinergic should be used with precaution for clients with closed-angle glaucoma.
Ipratropium raises aqueous outflow resistance and intraocular pressure for clients with closed
angle glaucoma. If the drug gets into the eyes, it may lead to blurred vision, pain and lastly visual
impairment (Westby, Gibson and Benson 2017, pp 56-60).
vi. Side effects/ adverse effects
Severe effects include anaphylactoid reactions, angioedema, laryngospasms, visual
impairment, arrhythmia exacerbation and bronchospasms (Roughead and Lexchin 2013, pp 315-
316).
Moderate side effects include hypotension, blurred vision, urinary retention, sinus
tachycardia, palpitations, constipation, conjunctivitis, oral ulcerations, sinus tachycardia and
dyspnea (Roughead and Lexchin 2013, pp 315-316).
6
Mild side effects include vomiting, nasal congestion, infection, hoarseness, diarrhea, nausea
sinusitis epistaxis, back pain, pharyngitis, dyspepsia, urticarial, sinusitis, ocular irritation, ocular
pain and mydriasis (Roughead and Lexchin 2013, pp 315-316).
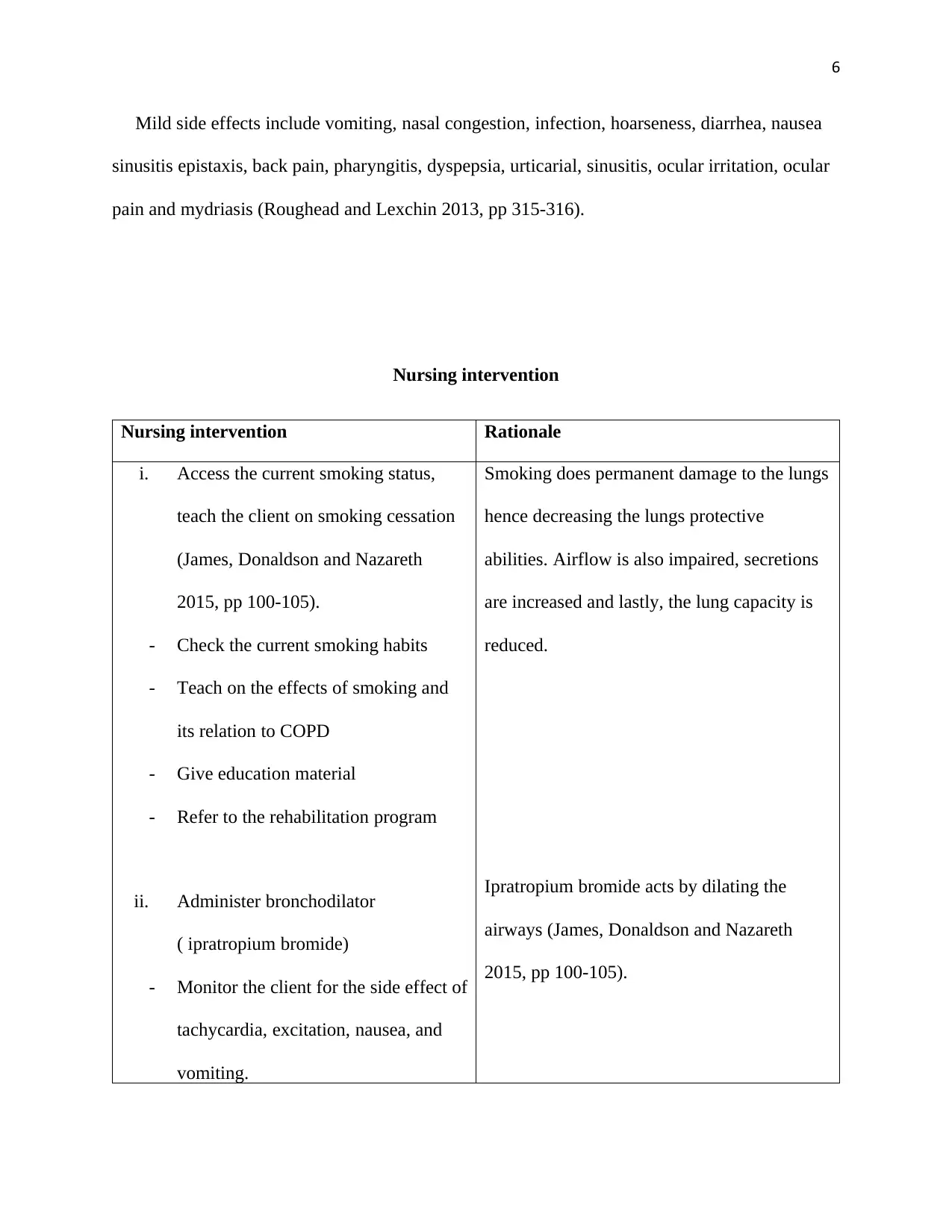
Nursing intervention
Nursing intervention Rationale
i. Access the current smoking status,
teach the client on smoking cessation
(James, Donaldson and Nazareth
2015, pp 100-105).
- Check the current smoking habits
- Teach on the effects of smoking and
its relation to COPD
- Give education material
- Refer to the rehabilitation program
ii. Administer bronchodilator
( ipratropium bromide)
- Monitor the client for the side effect of
tachycardia, excitation, nausea, and
vomiting.
Smoking does permanent damage to the lungs
hence decreasing the lungs protective
abilities. Airflow is also impaired, secretions
are increased and lastly, the lung capacity is
reduced.
Ipratropium bromide acts by dilating the
airways (James, Donaldson and Nazareth
2015, pp 100-105).
Mild side effects include vomiting, nasal congestion, infection, hoarseness, diarrhea, nausea
sinusitis epistaxis, back pain, pharyngitis, dyspepsia, urticarial, sinusitis, ocular irritation, ocular
pain and mydriasis (Roughead and Lexchin 2013, pp 315-316).
Nursing intervention
Nursing intervention Rationale
i. Access the current smoking status,
teach the client on smoking cessation
(James, Donaldson and Nazareth
2015, pp 100-105).
- Check the current smoking habits
- Teach on the effects of smoking and
its relation to COPD
- Give education material
- Refer to the rehabilitation program
ii. Administer bronchodilator
( ipratropium bromide)
- Monitor the client for the side effect of
tachycardia, excitation, nausea, and
vomiting.
Smoking does permanent damage to the lungs
hence decreasing the lungs protective
abilities. Airflow is also impaired, secretions
are increased and lastly, the lung capacity is
reduced.
Ipratropium bromide acts by dilating the
airways (James, Donaldson and Nazareth
2015, pp 100-105).
7
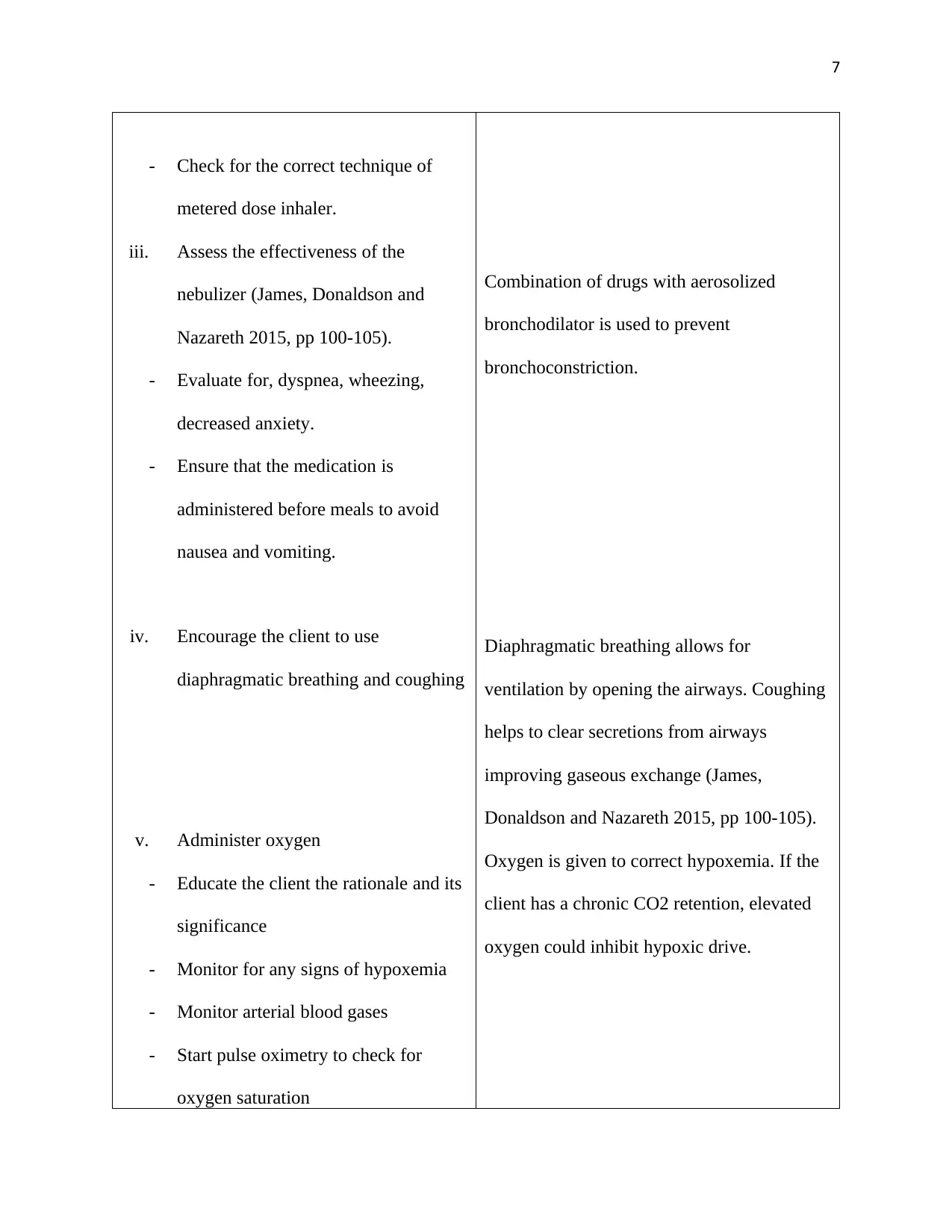
- Check for the correct technique of
metered dose inhaler.
iii. Assess the effectiveness of the
nebulizer (James, Donaldson and
Nazareth 2015, pp 100-105).
- Evaluate for, dyspnea, wheezing,
decreased anxiety.
- Ensure that the medication is
administered before meals to avoid
nausea and vomiting.
iv. Encourage the client to use
diaphragmatic breathing and coughing
v. Administer oxygen
- Educate the client the rationale and its
significance
- Monitor for any signs of hypoxemia
- Monitor arterial blood gases
- Start pulse oximetry to check for
oxygen saturation
Combination of drugs with aerosolized
bronchodilator is used to prevent
bronchoconstriction.
Diaphragmatic breathing allows for
ventilation by opening the airways. Coughing
helps to clear secretions from airways
improving gaseous exchange (James,
Donaldson and Nazareth 2015, pp 100-105).
Oxygen is given to correct hypoxemia. If the
client has a chronic CO2 retention, elevated
oxygen could inhibit hypoxic drive.
- Check for the correct technique of
metered dose inhaler.
iii. Assess the effectiveness of the
nebulizer (James, Donaldson and
Nazareth 2015, pp 100-105).
- Evaluate for, dyspnea, wheezing,
decreased anxiety.
- Ensure that the medication is
administered before meals to avoid
nausea and vomiting.
iv. Encourage the client to use
diaphragmatic breathing and coughing
v. Administer oxygen
- Educate the client the rationale and its
significance
- Monitor for any signs of hypoxemia
- Monitor arterial blood gases
- Start pulse oximetry to check for
oxygen saturation
Combination of drugs with aerosolized
bronchodilator is used to prevent
bronchoconstriction.
Diaphragmatic breathing allows for
ventilation by opening the airways. Coughing
helps to clear secretions from airways
improving gaseous exchange (James,
Donaldson and Nazareth 2015, pp 100-105).
Oxygen is given to correct hypoxemia. If the
client has a chronic CO2 retention, elevated
oxygen could inhibit hypoxic drive.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
8
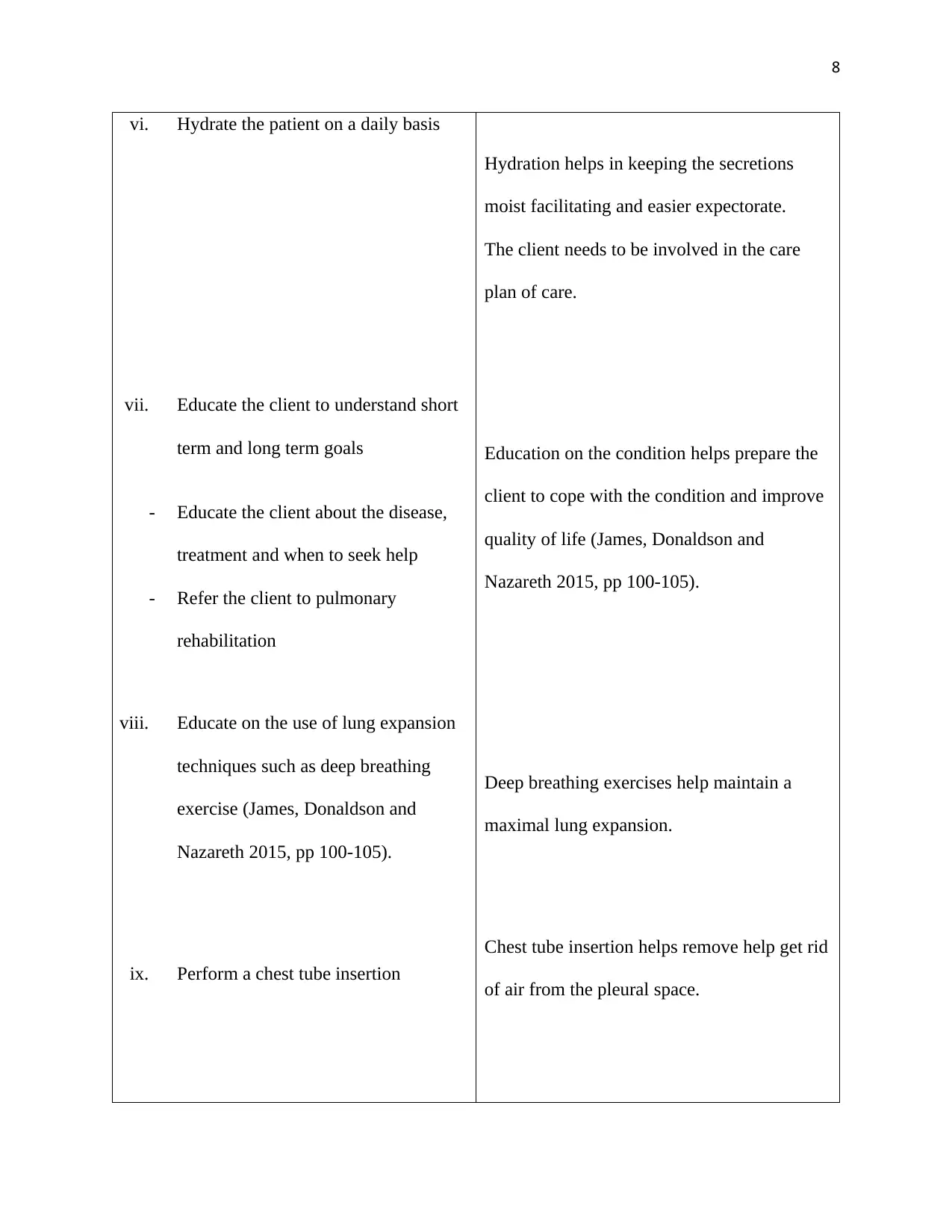
vi. Hydrate the patient on a daily basis
vii. Educate the client to understand short
term and long term goals
- Educate the client about the disease,
treatment and when to seek help
- Refer the client to pulmonary
rehabilitation
viii. Educate on the use of lung expansion
techniques such as deep breathing
exercise (James, Donaldson and
Nazareth 2015, pp 100-105).
ix. Perform a chest tube insertion
Hydration helps in keeping the secretions
moist facilitating and easier expectorate.
The client needs to be involved in the care
plan of care.
Education on the condition helps prepare the
client to cope with the condition and improve
quality of life (James, Donaldson and
Nazareth 2015, pp 100-105).
Deep breathing exercises help maintain a
maximal lung expansion.
Chest tube insertion helps remove help get rid
of air from the pleural space.
vi. Hydrate the patient on a daily basis
vii. Educate the client to understand short
term and long term goals
- Educate the client about the disease,
treatment and when to seek help
- Refer the client to pulmonary
rehabilitation
viii. Educate on the use of lung expansion
techniques such as deep breathing
exercise (James, Donaldson and
Nazareth 2015, pp 100-105).
ix. Perform a chest tube insertion
Hydration helps in keeping the secretions
moist facilitating and easier expectorate.
The client needs to be involved in the care
plan of care.
Education on the condition helps prepare the
client to cope with the condition and improve
quality of life (James, Donaldson and
Nazareth 2015, pp 100-105).
Deep breathing exercises help maintain a
maximal lung expansion.
Chest tube insertion helps remove help get rid
of air from the pleural space.
9
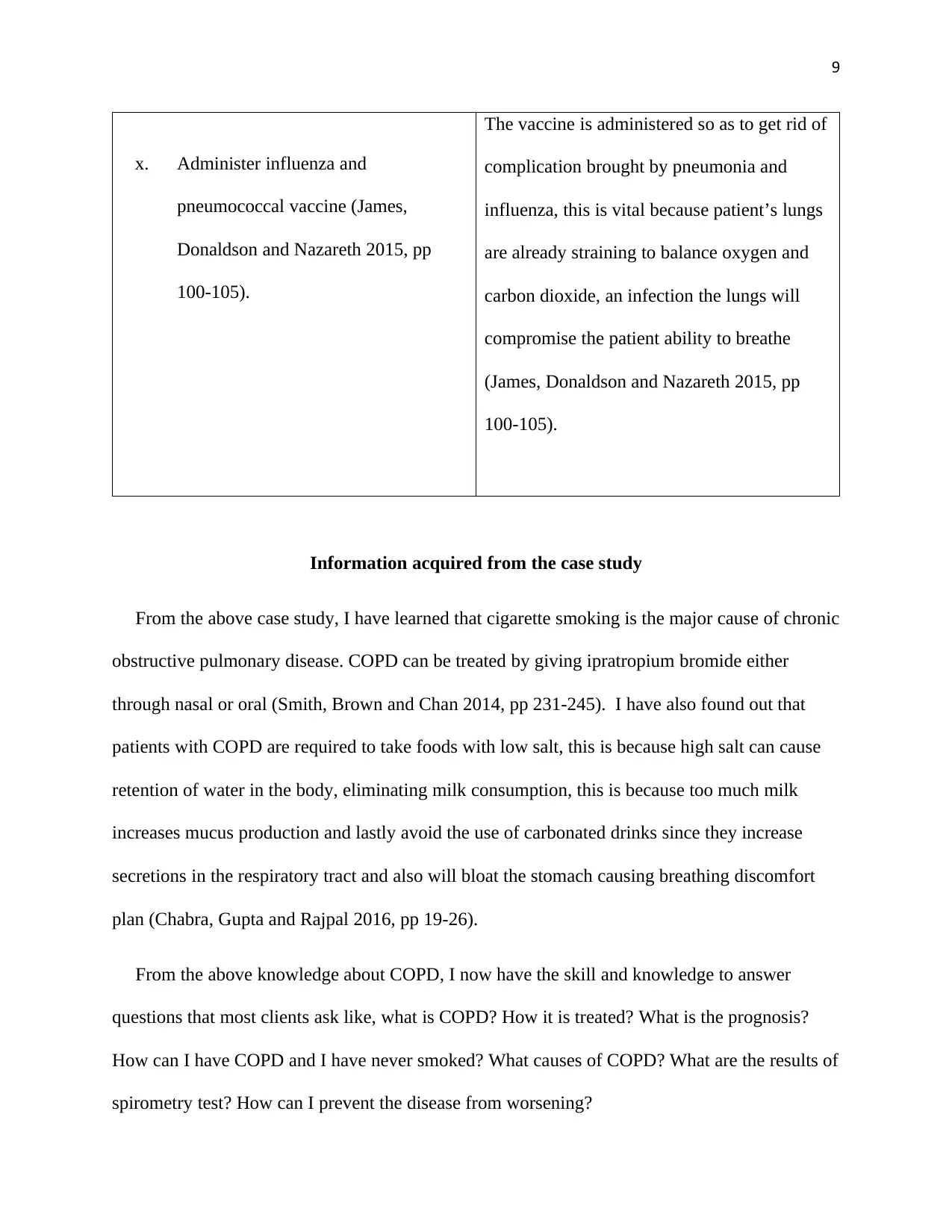
x. Administer influenza and
pneumococcal vaccine (James,
Donaldson and Nazareth 2015, pp
100-105).
The vaccine is administered so as to get rid of
complication brought by pneumonia and
influenza, this is vital because patient’s lungs
are already straining to balance oxygen and
carbon dioxide, an infection the lungs will
compromise the patient ability to breathe
(James, Donaldson and Nazareth 2015, pp
100-105).
Information acquired from the case study
From the above case study, I have learned that cigarette smoking is the major cause of chronic
obstructive pulmonary disease. COPD can be treated by giving ipratropium bromide either
through nasal or oral (Smith, Brown and Chan 2014, pp 231-245). I have also found out that
patients with COPD are required to take foods with low salt, this is because high salt can cause
retention of water in the body, eliminating milk consumption, this is because too much milk
increases mucus production and lastly avoid the use of carbonated drinks since they increase
secretions in the respiratory tract and also will bloat the stomach causing breathing discomfort
plan (Chabra, Gupta and Rajpal 2016, pp 19-26).
From the above knowledge about COPD, I now have the skill and knowledge to answer
questions that most clients ask like, what is COPD? How it is treated? What is the prognosis?
How can I have COPD and I have never smoked? What causes of COPD? What are the results of
spirometry test? How can I prevent the disease from worsening?
x. Administer influenza and
pneumococcal vaccine (James,
Donaldson and Nazareth 2015, pp
100-105).
The vaccine is administered so as to get rid of
complication brought by pneumonia and
influenza, this is vital because patient’s lungs
are already straining to balance oxygen and
carbon dioxide, an infection the lungs will
compromise the patient ability to breathe
(James, Donaldson and Nazareth 2015, pp
100-105).
Information acquired from the case study
From the above case study, I have learned that cigarette smoking is the major cause of chronic
obstructive pulmonary disease. COPD can be treated by giving ipratropium bromide either
through nasal or oral (Smith, Brown and Chan 2014, pp 231-245). I have also found out that
patients with COPD are required to take foods with low salt, this is because high salt can cause
retention of water in the body, eliminating milk consumption, this is because too much milk
increases mucus production and lastly avoid the use of carbonated drinks since they increase
secretions in the respiratory tract and also will bloat the stomach causing breathing discomfort
plan (Chabra, Gupta and Rajpal 2016, pp 19-26).
From the above knowledge about COPD, I now have the skill and knowledge to answer
questions that most clients ask like, what is COPD? How it is treated? What is the prognosis?
How can I have COPD and I have never smoked? What causes of COPD? What are the results of
spirometry test? How can I prevent the disease from worsening?

10
Reference
Chabra, S., Gupta, S. and Rajpal, S. (2016). A pattern of smoking in Delhi and comparison of
chronic respiratory morbidity among cigarette smokers. Indian J Chest Dis Allied Sci, [online]
43, pp.19-26. Available at: https://www.dovepress.com/efficacy-and-safety-of-ipratropium-
Reference
Chabra, S., Gupta, S. and Rajpal, S. (2016). A pattern of smoking in Delhi and comparison of
chronic respiratory morbidity among cigarette smokers. Indian J Chest Dis Allied Sci, [online]
43, pp.19-26. Available at: https://www.dovepress.com/efficacy-and-safety-of-ipratropium-
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
11
bromidesalbutamol-sulphate-administ-peer-reviewed-fulltext-article-COPD [Accessed 22 Mar.
2019].
James, G., Donaldson, G. and Nazareth, I. (2015). Trends in management and outcome of COPD
patients in primary care. NPJ Prim Care Respir Med, [online] 24, pp.100-105. Available at:
https://www.dovepress.com/efficacy-and-safety-of-ipratropium-bromidesalbutamol-sulphate-
administ-peer-reviewed-fulltext-article-COPD [Accessed 22 Mar. 2019].
More, W., Wenzel, S. and Meyers, D. (2016). Identification of asthma phenotypes using cluster
analysis in the Severe Asthma Research Program. Am J Respir Crit Care Med, 181(4), pp.315-
323. Available at: https://www.ncbi.nlm.nih.gov/pubmed/17594728 [Accessed 22 Mar. 2019].
Neild, J. and Cameron, R. (2014). Bronchoconstriction in response to suggestion: its prevention
by an inhaled anticholinergic agent. Br Med J, 290, pp.671-680. Available at:
https://www.ncbi.nlm.nih.gov/pubmed/17594728 [Accessed 22 Mar. 2019].
Neilsen, K., Biisgard, H. and Ifversen, M. (2013). Flow-dependent effect of formoterol dry-
powder inhaled from the Aerolizer. Eur Respir J, [online] 10(3), pp.2105-2109. Available at:
https://www.dovepress.com/efficacy-and-safety-of-ipratropium-bromidesalbutamol-sulphate-
administ-peer-reviewed-fulltext-article-COPD [Accessed 22 Mar. 2019].
Rebuck, A., Chapman, R., and Wolkove, N. (2014). Nebulized anticholinergic and
sympathomimetic treatment of asthma and chronic obstructive airways disease in the emergency
room. Am J Med, [online] 82(1), pp.59-64. Available at:
https://linkinghub.elsevier.com/retrieve/pii/0002934387903780 [Accessed 22 Mar. 2019].
bromidesalbutamol-sulphate-administ-peer-reviewed-fulltext-article-COPD [Accessed 22 Mar.
2019].
James, G., Donaldson, G. and Nazareth, I. (2015). Trends in management and outcome of COPD
patients in primary care. NPJ Prim Care Respir Med, [online] 24, pp.100-105. Available at:
https://www.dovepress.com/efficacy-and-safety-of-ipratropium-bromidesalbutamol-sulphate-
administ-peer-reviewed-fulltext-article-COPD [Accessed 22 Mar. 2019].
More, W., Wenzel, S. and Meyers, D. (2016). Identification of asthma phenotypes using cluster
analysis in the Severe Asthma Research Program. Am J Respir Crit Care Med, 181(4), pp.315-
323. Available at: https://www.ncbi.nlm.nih.gov/pubmed/17594728 [Accessed 22 Mar. 2019].
Neild, J. and Cameron, R. (2014). Bronchoconstriction in response to suggestion: its prevention
by an inhaled anticholinergic agent. Br Med J, 290, pp.671-680. Available at:
https://www.ncbi.nlm.nih.gov/pubmed/17594728 [Accessed 22 Mar. 2019].
Neilsen, K., Biisgard, H. and Ifversen, M. (2013). Flow-dependent effect of formoterol dry-
powder inhaled from the Aerolizer. Eur Respir J, [online] 10(3), pp.2105-2109. Available at:
https://www.dovepress.com/efficacy-and-safety-of-ipratropium-bromidesalbutamol-sulphate-
administ-peer-reviewed-fulltext-article-COPD [Accessed 22 Mar. 2019].
Rebuck, A., Chapman, R., and Wolkove, N. (2014). Nebulized anticholinergic and
sympathomimetic treatment of asthma and chronic obstructive airways disease in the emergency
room. Am J Med, [online] 82(1), pp.59-64. Available at:
https://linkinghub.elsevier.com/retrieve/pii/0002934387903780 [Accessed 22 Mar. 2019].
12
Restrepo, R. (2015). Use of inhaled anticholinergic agents in obstructive airway disease. Respire
Care, [online] 52(7), pp.833-851. Available at: https://www.ncbi.nlm.nih.gov/pubmed/17594728
[Accessed 22 Mar. 2019].
Roughead, E. and Lexchin, J. (2013). Adverse Drug Events: counting is not enough, action is
needed. Medical Journal of Australia, [online] 184(7), pp.315-316. Available at: http://www.
safetyandquality.gov.au/internet/safety/ publishing’s/Content/Patient ID-Resources-
Exp_Correct-Pat-Site-Proc [Accessed 22 Mar. 2019].
Smith, K., Brown, F. and Chan, K. (2014). Influence of flow rate on aerosol particle size
distributions from pressurized and breath-actuated inhalers. J Aerosol Med, [online] 11, pp.231-
245. Available at: https://www.dovepress.com/efficacy-and-safety-of-ipratropium-
bromidesalbutamol-sulphate-administ-peer-reviewed-fulltext-article-COPD [Accessed 22 Mar.
2019].
Westby, M., Gibson, P. and Benson, M. (2017). Anticholinergic agents for chronic asthma in
adults. Cochrane Database Syst Rev, [online] 31(2), pp.56-60. Available at:
https://www.ncbi.nlm.nih.gov/pubmed/17594728 [Accessed 22 Mar. 2019].
Restrepo, R. (2015). Use of inhaled anticholinergic agents in obstructive airway disease. Respire
Care, [online] 52(7), pp.833-851. Available at: https://www.ncbi.nlm.nih.gov/pubmed/17594728
[Accessed 22 Mar. 2019].
Roughead, E. and Lexchin, J. (2013). Adverse Drug Events: counting is not enough, action is
needed. Medical Journal of Australia, [online] 184(7), pp.315-316. Available at: http://www.
safetyandquality.gov.au/internet/safety/ publishing’s/Content/Patient ID-Resources-
Exp_Correct-Pat-Site-Proc [Accessed 22 Mar. 2019].
Smith, K., Brown, F. and Chan, K. (2014). Influence of flow rate on aerosol particle size
distributions from pressurized and breath-actuated inhalers. J Aerosol Med, [online] 11, pp.231-
245. Available at: https://www.dovepress.com/efficacy-and-safety-of-ipratropium-
bromidesalbutamol-sulphate-administ-peer-reviewed-fulltext-article-COPD [Accessed 22 Mar.
2019].
Westby, M., Gibson, P. and Benson, M. (2017). Anticholinergic agents for chronic asthma in
adults. Cochrane Database Syst Rev, [online] 31(2), pp.56-60. Available at:
https://www.ncbi.nlm.nih.gov/pubmed/17594728 [Accessed 22 Mar. 2019].
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





