Edith Cowan University: NUM1102 Tuberculosis Clinical Update Report
VerifiedAdded on 2023/01/20
|15
|3096
|65
Report
AI Summary
This report provides a comprehensive clinical update on Tuberculosis, a disease caused by Mycobacterium tuberculosis. The report delves into the etiology and pathogenesis of TB, detailing the causative agent, transmission, and risk factors. It explores the anatomy and physiology related to TB, as well as the pathogenesis, including the body's immune response and the formation of lesions. The report also covers complications, public health implications, clinical manifestations, and the diagnostic processes, including skin and blood tests. Furthermore, it outlines both pharmacological and non-pharmacological treatment approaches, as well as health promotion strategies to prevent and control the spread of the disease. The report is a detailed overview of the disease and its management.
Running header: TUBERCULOSIS 1
Tuberculosis
Unit Title
Lecturer
Student Name
Student ID
Date of Submission
Word Count
Tuberculosis
Unit Title
Lecturer
Student Name
Student ID
Date of Submission
Word Count
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
2
Table of Contents
Introduction……………………………………………………………………………3
Etiology and pathogenesis……………………………………………………………..3
Etiology……………………………………………………………………………..3
Transmission………………………………………………………………………...4
Risk factors…………………………………………………………………………..4
Anatomy and physiology…………………………………………………………….5
Pathogenesis………………………………………………………………………….5
Complication……………………………………………………………………...….6
Implication to public health…………………………………………………………..6
Clinical manifestation………………………………………………………………...…7
Diagnostic process…………………………………………………………………….…8
Treatment………………………………………………………………………………...9
Pharmacological treatment......................................................................................…...9
Non-pharmacological treatment……………………………………………………....11
Health promotion………………………………………………………………………12
Conclusion………………………………………………………………………………...13
Table of Contents
Introduction……………………………………………………………………………3
Etiology and pathogenesis……………………………………………………………..3
Etiology……………………………………………………………………………..3
Transmission………………………………………………………………………...4
Risk factors…………………………………………………………………………..4
Anatomy and physiology…………………………………………………………….5
Pathogenesis………………………………………………………………………….5
Complication……………………………………………………………………...….6
Implication to public health…………………………………………………………..6
Clinical manifestation………………………………………………………………...…7
Diagnostic process…………………………………………………………………….…8
Treatment………………………………………………………………………………...9
Pharmacological treatment......................................................................................…...9
Non-pharmacological treatment……………………………………………………....11
Health promotion………………………………………………………………………12
Conclusion………………………………………………………………………………...13
3
TUBERCULOSIS
Introduction
Tuberculosis is disease caused by bacillus Mycobacterium tuberculosis (Mtb). Mtb is one of
the most dangerous bacterial infection responsible for an extreme increase in death cases. In
Australia, there are approximately 1200-1300 incidences of tuberculosis each year. Globally,
Australia is among the lowest risk countries. Individuals at risk of TB in Australia are those who
have spent their past life in countries with a high rate of the disease and have been infected
without their knowledge. According to WHO one-fourth of the world's population have
tuberculosis. In 2017 there were 1.3 million TB-related deaths globally (Ahmed, Soliman, &
Awad, 2014). This essay will critically discuss tuberculosis. The assignment will focus on four
key areas: etiology and pathogenesis, clinical manifestation, diagnostic processes, and lastly
treatment of the disease.
Etiology and Pathogenesis
Etiology.
TB is caused by M. tuberculosis, which is a facultative intracellular parasite and a slowing
growing parasite. The bacteria develop in parallel groups known as the cord. Mycobacterium
tuberculosis is non-motile, facultative, aerobic, non-spore forming and has curved intracellular
rods. Its cell wall contains mycocides, mycolic, long chain glycolipids, and acid-rich that shield
the mycobacteria from lysosomal attack.
TUBERCULOSIS
Introduction
Tuberculosis is disease caused by bacillus Mycobacterium tuberculosis (Mtb). Mtb is one of
the most dangerous bacterial infection responsible for an extreme increase in death cases. In
Australia, there are approximately 1200-1300 incidences of tuberculosis each year. Globally,
Australia is among the lowest risk countries. Individuals at risk of TB in Australia are those who
have spent their past life in countries with a high rate of the disease and have been infected
without their knowledge. According to WHO one-fourth of the world's population have
tuberculosis. In 2017 there were 1.3 million TB-related deaths globally (Ahmed, Soliman, &
Awad, 2014). This essay will critically discuss tuberculosis. The assignment will focus on four
key areas: etiology and pathogenesis, clinical manifestation, diagnostic processes, and lastly
treatment of the disease.
Etiology and Pathogenesis
Etiology.
TB is caused by M. tuberculosis, which is a facultative intracellular parasite and a slowing
growing parasite. The bacteria develop in parallel groups known as the cord. Mycobacterium
tuberculosis is non-motile, facultative, aerobic, non-spore forming and has curved intracellular
rods. Its cell wall contains mycocides, mycolic, long chain glycolipids, and acid-rich that shield
the mycobacteria from lysosomal attack.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
4
Transmission.
When individuals with active TB spit, speak, sneeze or cough they release infectious air
droplets approximately 0.5 to 0.5 um in diameter. These droplets main remain airborne for
minutes to hours after expectoration. (Wanyeki, Olson, & Brassard, 2016).
Risk factors.
Tuberculosis is able to be transmitted from one individual to the other through the following
ways;
i. Number of organisms expelled
ii. Immune status of the individual
iii. Duration of exposure to contaminated air
iv. The concentration of the mycobacteria
Factors that raise the risk of an individual to get active tuberculosis to include the following:
i. Weakened immune system
An individual with a strong immune system often fights TB bacteria, but the body is not
capable of producing a defense mechanism if the body resistance to infection is low. medication,
diseases, and condition can weaken the immune system such as HIV/AIDS and chemotherapy
drugs (Ferrara, Murray, & Winthrop, 2015).
ii. Traveling or residing in certain areas
Transmission.
When individuals with active TB spit, speak, sneeze or cough they release infectious air
droplets approximately 0.5 to 0.5 um in diameter. These droplets main remain airborne for
minutes to hours after expectoration. (Wanyeki, Olson, & Brassard, 2016).
Risk factors.
Tuberculosis is able to be transmitted from one individual to the other through the following
ways;
i. Number of organisms expelled
ii. Immune status of the individual
iii. Duration of exposure to contaminated air
iv. The concentration of the mycobacteria
Factors that raise the risk of an individual to get active tuberculosis to include the following:
i. Weakened immune system
An individual with a strong immune system often fights TB bacteria, but the body is not
capable of producing a defense mechanism if the body resistance to infection is low. medication,
diseases, and condition can weaken the immune system such as HIV/AIDS and chemotherapy
drugs (Ferrara, Murray, & Winthrop, 2015).
ii. Traveling or residing in certain areas
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
5
The risk of getting tuberculosis is greater in people who reside or journey to areas which have
a high incidence rate of tuberculosis and drug-resistant tuberculosis. These areas include; Russia,
Africa, Asia, Eastern Europe and Caribbean islands (Ferrara, Murray, & Winthrop, 2015).
iii. Poverty and substance use
An individual who has a low financial gain resides in a populated area or homeless may not
be able to get healthcare needed to treat TB and is also at high risk of contracting TB (Ferrara,
Murray, & Winthrop, 2015).
Anatomy and physiology.
The lung is a major site for the development of TB. Extrapulmonary TB can also take place.
Extrapulmonary sites may serve as reactivation sites. These sites include cervical, retroperitoneal
and mediastinal lymph nodes. The other sites are the GI tract, meninges, adrenal, and vertebral
bodies.
Pathogenesis.
Once the contagious droplets have been inhaled they settle in the upper respiratory tract. Most
bacteria settle in areas that contain mucus-secreting goblet. The goblet cells act by producing
mucus which helps trap dust particles and other foreign objects. Mycobacterium found in air
droplets bypass the mucociliary system and travel to the alveoli where they are quickly confined
on all sides and engulfed by the alveolar macrophages (Houben, Nguyen, & Pieters, 2016).
Alveolar macrophages exist in great quantity in the alveolar space. These macrophages are the
first line of host defense and help destroy invading mycobacterium and prevent infection. This
immune response continues 2-12 weeks, the mycobacterium continues to multiply until it
reaches a sufficient number to evoke a cell-mediated response (Wallstedt & Maeurer, 2017).
The risk of getting tuberculosis is greater in people who reside or journey to areas which have
a high incidence rate of tuberculosis and drug-resistant tuberculosis. These areas include; Russia,
Africa, Asia, Eastern Europe and Caribbean islands (Ferrara, Murray, & Winthrop, 2015).
iii. Poverty and substance use
An individual who has a low financial gain resides in a populated area or homeless may not
be able to get healthcare needed to treat TB and is also at high risk of contracting TB (Ferrara,
Murray, & Winthrop, 2015).
Anatomy and physiology.
The lung is a major site for the development of TB. Extrapulmonary TB can also take place.
Extrapulmonary sites may serve as reactivation sites. These sites include cervical, retroperitoneal
and mediastinal lymph nodes. The other sites are the GI tract, meninges, adrenal, and vertebral
bodies.
Pathogenesis.
Once the contagious droplets have been inhaled they settle in the upper respiratory tract. Most
bacteria settle in areas that contain mucus-secreting goblet. The goblet cells act by producing
mucus which helps trap dust particles and other foreign objects. Mycobacterium found in air
droplets bypass the mucociliary system and travel to the alveoli where they are quickly confined
on all sides and engulfed by the alveolar macrophages (Houben, Nguyen, & Pieters, 2016).
Alveolar macrophages exist in great quantity in the alveolar space. These macrophages are the
first line of host defense and help destroy invading mycobacterium and prevent infection. This
immune response continues 2-12 weeks, the mycobacterium continues to multiply until it
reaches a sufficient number to evoke a cell-mediated response (Wallstedt & Maeurer, 2017).
6
Various mechanism are involved in the ingestion of the mycobacterium. The complement
system is activated, so as the phagocytosis of bacteria can occur. After ingestion of the
mycobacterium by macrophages, the bacterium increases slowly with cell division occurring
after every 25 to 32 hours. This causes the release of cytokines and proteolytic enzyme by
macrophages which degrades the bacteria. The release of cytokines in the blood causes the
attraction of T lymphocytes to the site. Macrophages then introduce the mycobacterial antigen to
the T cells (Ling, Flores, & Riley, 2017).
The collection of macrophages and activated T lymphocytes leads to the formation of a
nodular type lesion. The micro-environment destroys the macrophages and prevents the spread
of Mycobacterium. After 2-3 weeks the necrotic environment is characterized by limited
nutrients, low oxygen, and low ph. This conditions limits further multiplication and establishes
latency. Lesions in clients with low immunity will progress to primary progressive tuberculosis
(Steingart & Henry, 2015).
Complication.
The pulmonary complication of TB includes chronic pulmonary aspergillosis, pneumothorax,
hemoptysis, bronchiectasis, malignancy, and lastly extensive pulmonary destruction (Nicas,
Nazaroff, & Hubard, 2014).
The implication for public health.
The physician is compelled by law to report any case of tuberculosis infection to the local
public health department immediately so as to start control measures in the area. Public health
intervenes by assessing the individual’s likely hood of contagiousness thereafter isolating the
individual. Individuals with active tuberculosis are closely monitored and assisted in finishing
Various mechanism are involved in the ingestion of the mycobacterium. The complement
system is activated, so as the phagocytosis of bacteria can occur. After ingestion of the
mycobacterium by macrophages, the bacterium increases slowly with cell division occurring
after every 25 to 32 hours. This causes the release of cytokines and proteolytic enzyme by
macrophages which degrades the bacteria. The release of cytokines in the blood causes the
attraction of T lymphocytes to the site. Macrophages then introduce the mycobacterial antigen to
the T cells (Ling, Flores, & Riley, 2017).
The collection of macrophages and activated T lymphocytes leads to the formation of a
nodular type lesion. The micro-environment destroys the macrophages and prevents the spread
of Mycobacterium. After 2-3 weeks the necrotic environment is characterized by limited
nutrients, low oxygen, and low ph. This conditions limits further multiplication and establishes
latency. Lesions in clients with low immunity will progress to primary progressive tuberculosis
(Steingart & Henry, 2015).
Complication.
The pulmonary complication of TB includes chronic pulmonary aspergillosis, pneumothorax,
hemoptysis, bronchiectasis, malignancy, and lastly extensive pulmonary destruction (Nicas,
Nazaroff, & Hubard, 2014).
The implication for public health.
The physician is compelled by law to report any case of tuberculosis infection to the local
public health department immediately so as to start control measures in the area. Public health
intervenes by assessing the individual’s likely hood of contagiousness thereafter isolating the
individual. Individuals with active tuberculosis are closely monitored and assisted in finishing
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
7
the prolonged course of treatment. Individuals who are homeless and infected with TB are
assisted with housing and food so as the patients can adhere to the tuberculosis treatment
regimen (Fikru, Mengisu, & Zenebe, 2015).
Clinical Manifestation
Clinical features associated with active TB include the following;
i. Chronic cough- An individual with TB usually manifest with a bad cough which usually
lasts 3 weeks or longer. The cough is usually worse at night when the individual is lying
flat in bed (Getahun, Ameni, & Medhin, 2016).
ii. Weight loss- unexplained weight loss is mostly caused by coughing and fever which
makes an individual lack appetite.
iii. Fever and night sweats- bacteria that causes TB is the major cause of fever. Fever tends
to increase during the night due to fatigue which results in night sweats (Getahun, Ameni,
& Medhin, 2016).
iv. Hemoptysis- coughing up blood is mostly caused by the infection of the lungs, a violent
cough causes the release of a small amount of blood-tinged sputum.
v. Chest pain- chest pain is caused by tuberculosis infection in the lungs which cause
inflammation of membranes lining the lungs, it mostly occurs during breathing in as the
lungs start expanding (Getahun, Ameni, & Medhin, 2016).
Diagnostic process
the prolonged course of treatment. Individuals who are homeless and infected with TB are
assisted with housing and food so as the patients can adhere to the tuberculosis treatment
regimen (Fikru, Mengisu, & Zenebe, 2015).
Clinical Manifestation
Clinical features associated with active TB include the following;
i. Chronic cough- An individual with TB usually manifest with a bad cough which usually
lasts 3 weeks or longer. The cough is usually worse at night when the individual is lying
flat in bed (Getahun, Ameni, & Medhin, 2016).
ii. Weight loss- unexplained weight loss is mostly caused by coughing and fever which
makes an individual lack appetite.
iii. Fever and night sweats- bacteria that causes TB is the major cause of fever. Fever tends
to increase during the night due to fatigue which results in night sweats (Getahun, Ameni,
& Medhin, 2016).
iv. Hemoptysis- coughing up blood is mostly caused by the infection of the lungs, a violent
cough causes the release of a small amount of blood-tinged sputum.
v. Chest pain- chest pain is caused by tuberculosis infection in the lungs which cause
inflammation of membranes lining the lungs, it mostly occurs during breathing in as the
lungs start expanding (Getahun, Ameni, & Medhin, 2016).
Diagnostic process
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
8
There are two kinds of tests that are used to check for TB bacteria in an individual this
includes tuberculin skin test and tuberculosis blood test. A positive tuberculosis blood test and
tuberculin skin test confirms that the client has been contaminated either by the mycobacteria but
it doesn’t tell if the client has a latent TB or active TB (Cruciani, Scarparo, & Malena, 2016).
a) TB skin test
TB skin test is the most common method of diagnosing TB. In TB skin test a drug is injected
beneath the skin specifically under the arm. After 48-72 hours the individual should return to the
nurse or healthcare practitioner to check their arm. The nurse should check for a raised swelling
and measure its size. If the swelling is large in size the greater the probability that the individual
is infected with TB bacteria. TB skin test cannot tell if the individual has an active or latent TB
(Mazurek, Weisis, & Moonan, 2018).
Rationale
A test bump greater than 5mm indicates positive for TB. If the individual tests positive, it
shows that the individual has been infected with Mycobacterium tuberculosis. The infection
makes the body very sensitive to tuberculin injection, which makes the area injected increase in
size (Mazurek, Weisis, & Moonan, 2018).
b) Blood test
Individuals who have severe reactions to TB skin test, they are advocated for a blood test
called the interferon gamma release assay (IGRA).
i. TB interferon-gamma release assays (IGRAs)
There are two kinds of tests that are used to check for TB bacteria in an individual this
includes tuberculin skin test and tuberculosis blood test. A positive tuberculosis blood test and
tuberculin skin test confirms that the client has been contaminated either by the mycobacteria but
it doesn’t tell if the client has a latent TB or active TB (Cruciani, Scarparo, & Malena, 2016).
a) TB skin test
TB skin test is the most common method of diagnosing TB. In TB skin test a drug is injected
beneath the skin specifically under the arm. After 48-72 hours the individual should return to the
nurse or healthcare practitioner to check their arm. The nurse should check for a raised swelling
and measure its size. If the swelling is large in size the greater the probability that the individual
is infected with TB bacteria. TB skin test cannot tell if the individual has an active or latent TB
(Mazurek, Weisis, & Moonan, 2018).
Rationale
A test bump greater than 5mm indicates positive for TB. If the individual tests positive, it
shows that the individual has been infected with Mycobacterium tuberculosis. The infection
makes the body very sensitive to tuberculin injection, which makes the area injected increase in
size (Mazurek, Weisis, & Moonan, 2018).
b) Blood test
Individuals who have severe reactions to TB skin test, they are advocated for a blood test
called the interferon gamma release assay (IGRA).
i. TB interferon-gamma release assays (IGRAs)
9
IGRA is a blood test used to check an individual's immune response to the bacteria. White
blood cells from an individual infected with Mycobacterium tuberculosis release cytokines. The
test is done by mixing fresh blood with antigens and control. This test depends on cell-mediated
immunity or the memory T-cell response (Chang & Leung, 2015).
Rationale
IGRA act by detecting cytokine specifically the interferon gamma cytokine. It can also be
used to check for latent TB if an individual test positive for Mantoux test or had previously had
BCG vaccination (Chang & Leung, 2015).
Treatment
Pharmacological management.
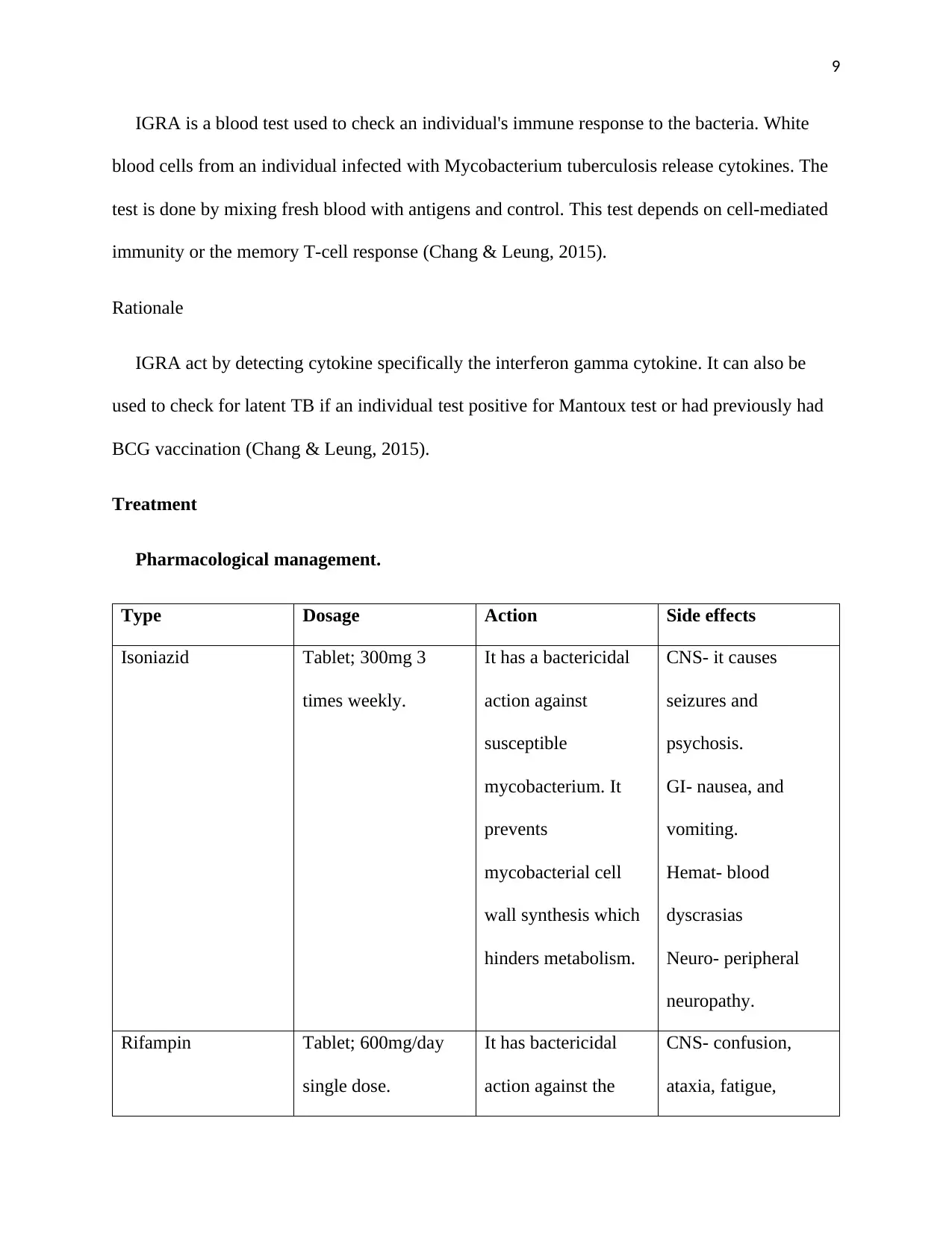
Type Dosage Action Side effects
Isoniazid Tablet; 300mg 3
times weekly.
It has a bactericidal
action against
susceptible
mycobacterium. It
prevents
mycobacterial cell
wall synthesis which
hinders metabolism.
CNS- it causes
seizures and
psychosis.
GI- nausea, and
vomiting.
Hemat- blood
dyscrasias
Neuro- peripheral
neuropathy.
Rifampin Tablet; 600mg/day
single dose.
It has bactericidal
action against the
CNS- confusion,
ataxia, fatigue,
IGRA is a blood test used to check an individual's immune response to the bacteria. White
blood cells from an individual infected with Mycobacterium tuberculosis release cytokines. The
test is done by mixing fresh blood with antigens and control. This test depends on cell-mediated
immunity or the memory T-cell response (Chang & Leung, 2015).
Rationale
IGRA act by detecting cytokine specifically the interferon gamma cytokine. It can also be
used to check for latent TB if an individual test positive for Mantoux test or had previously had
BCG vaccination (Chang & Leung, 2015).
Treatment
Pharmacological management.
Type Dosage Action Side effects
Isoniazid Tablet; 300mg 3
times weekly.
It has a bactericidal
action against
susceptible
mycobacterium. It
prevents
mycobacterial cell
wall synthesis which
hinders metabolism.
CNS- it causes
seizures and
psychosis.
GI- nausea, and
vomiting.
Hemat- blood
dyscrasias
Neuro- peripheral
neuropathy.
Rifampin Tablet; 600mg/day
single dose.
It has bactericidal
action against the
CNS- confusion,
ataxia, fatigue,
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
10
susceptible organism,
it prevents RNA
synthesis by
hindering RNA
transcription in
susceptible
organisms.
headache, and
weakness.
GI- abdominal pain,
nausea, vomiting,
flatulence, and
diarrhea.
Genitourinary- red
discoloration of
urine.
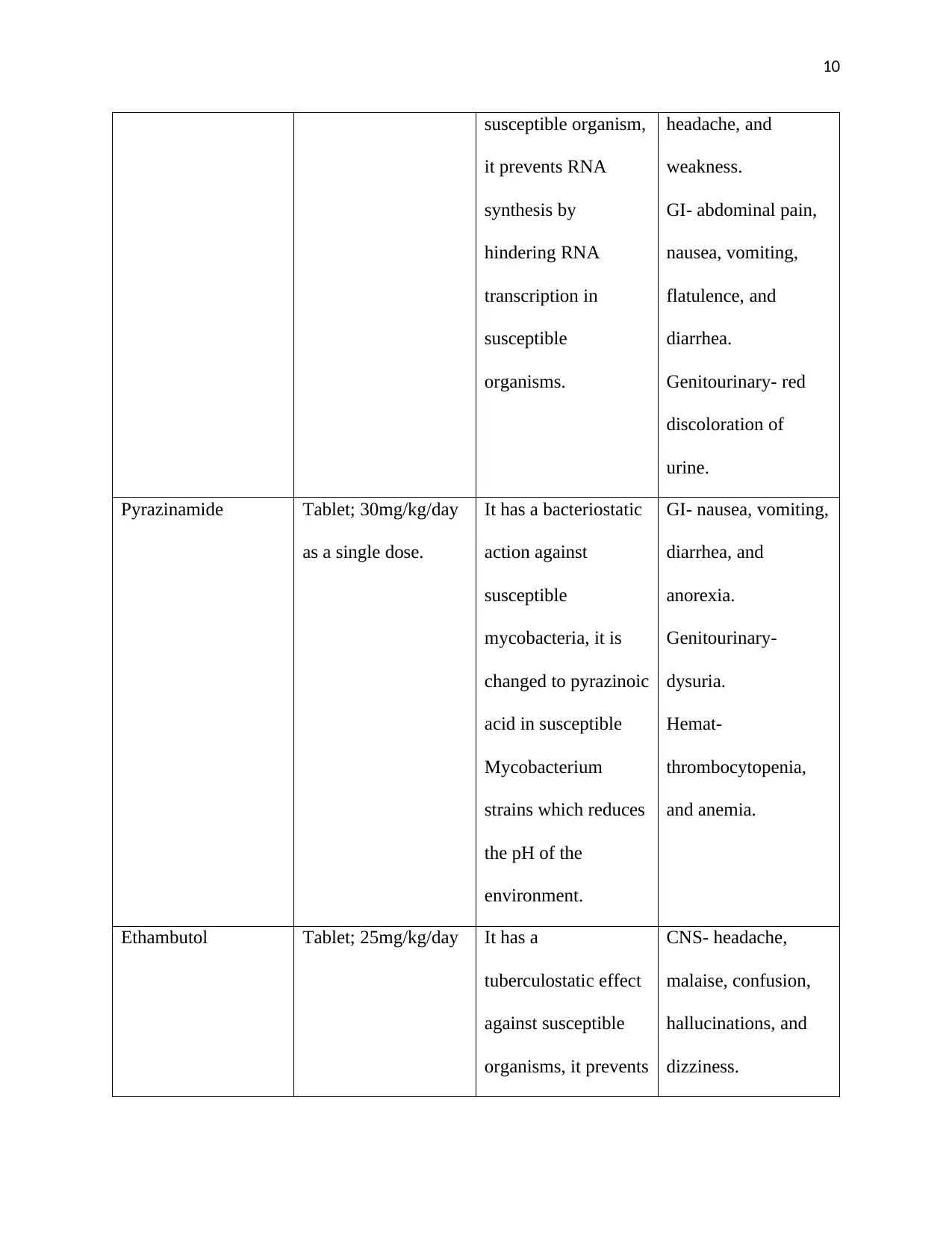
Pyrazinamide Tablet; 30mg/kg/day
as a single dose.
It has a bacteriostatic
action against
susceptible
mycobacteria, it is
changed to pyrazinoic
acid in susceptible
Mycobacterium
strains which reduces
the pH of the
environment.
GI- nausea, vomiting,
diarrhea, and
anorexia.
Genitourinary-
dysuria.
Hemat-
thrombocytopenia,
and anemia.
Ethambutol Tablet; 25mg/kg/day It has a
tuberculostatic effect
against susceptible
organisms, it prevents
CNS- headache,
malaise, confusion,
hallucinations, and
dizziness.
susceptible organism,
it prevents RNA
synthesis by
hindering RNA
transcription in
susceptible
organisms.
headache, and
weakness.
GI- abdominal pain,
nausea, vomiting,
flatulence, and
diarrhea.
Genitourinary- red
discoloration of
urine.
Pyrazinamide Tablet; 30mg/kg/day
as a single dose.
It has a bacteriostatic
action against
susceptible
mycobacteria, it is
changed to pyrazinoic
acid in susceptible
Mycobacterium
strains which reduces
the pH of the
environment.
GI- nausea, vomiting,
diarrhea, and
anorexia.
Genitourinary-
dysuria.
Hemat-
thrombocytopenia,
and anemia.
Ethambutol Tablet; 25mg/kg/day It has a
tuberculostatic effect
against susceptible
organisms, it prevents
CNS- headache,
malaise, confusion,
hallucinations, and
dizziness.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
11
the growth and
multiplication of
Mycobacterium
(Burman, Goldberg,
& Jonson, 2016).
GI- hepatitis,
anorexia, vomiting
and abdominal pain.
Respiratory-
pulmonary infiltrates.
Non-pharmacological management.
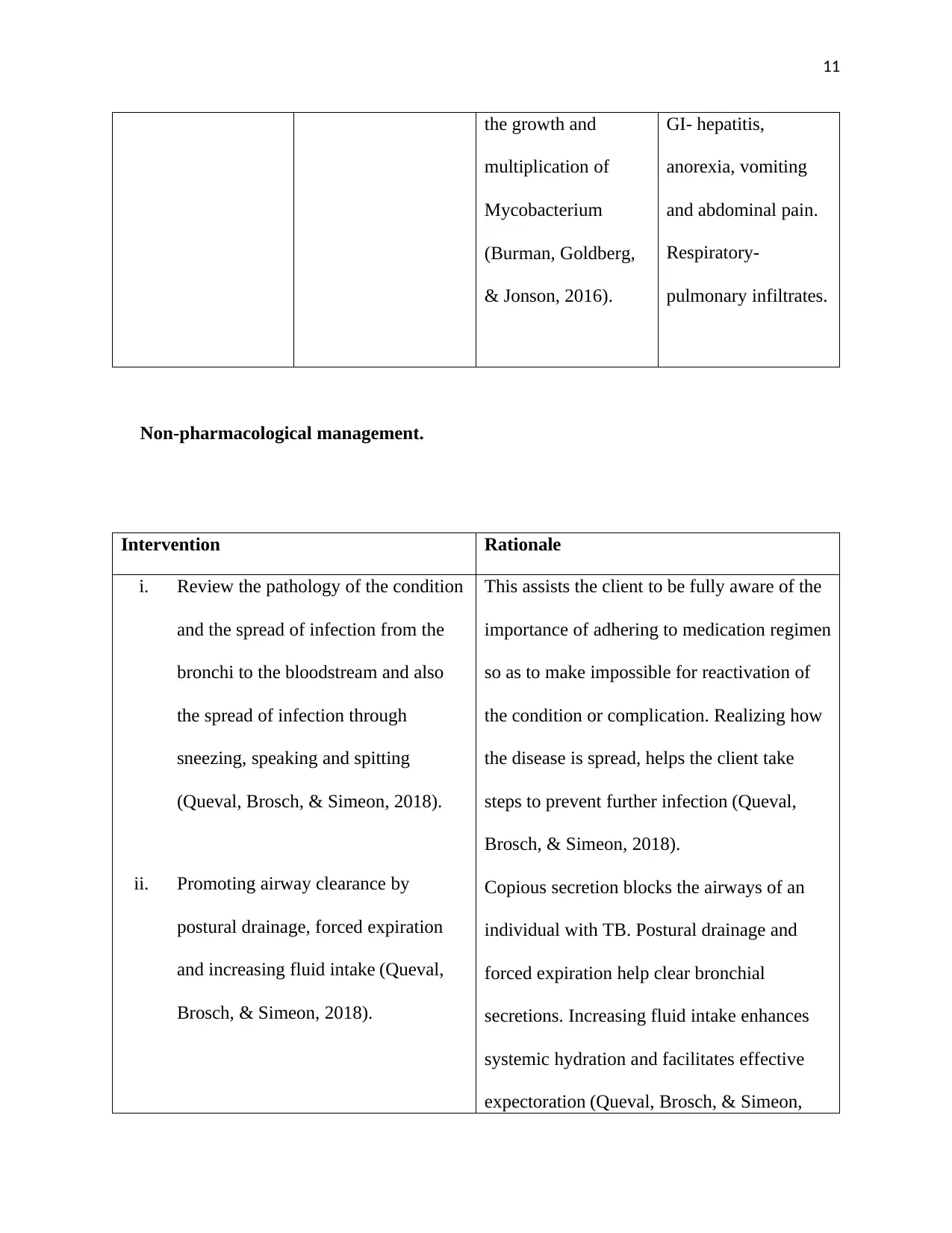
Intervention Rationale
i. Review the pathology of the condition
and the spread of infection from the
bronchi to the bloodstream and also
the spread of infection through
sneezing, speaking and spitting
(Queval, Brosch, & Simeon, 2018).
ii. Promoting airway clearance by
postural drainage, forced expiration
and increasing fluid intake (Queval,
Brosch, & Simeon, 2018).
This assists the client to be fully aware of the
importance of adhering to medication regimen
so as to make impossible for reactivation of
the condition or complication. Realizing how
the disease is spread, helps the client take
steps to prevent further infection (Queval,
Brosch, & Simeon, 2018).
Copious secretion blocks the airways of an
individual with TB. Postural drainage and
forced expiration help clear bronchial
secretions. Increasing fluid intake enhances
systemic hydration and facilitates effective
expectoration (Queval, Brosch, & Simeon,
the growth and
multiplication of
Mycobacterium
(Burman, Goldberg,
& Jonson, 2016).
GI- hepatitis,
anorexia, vomiting
and abdominal pain.
Respiratory-
pulmonary infiltrates.
Non-pharmacological management.
Intervention Rationale
i. Review the pathology of the condition
and the spread of infection from the
bronchi to the bloodstream and also
the spread of infection through
sneezing, speaking and spitting
(Queval, Brosch, & Simeon, 2018).
ii. Promoting airway clearance by
postural drainage, forced expiration
and increasing fluid intake (Queval,
Brosch, & Simeon, 2018).
This assists the client to be fully aware of the
importance of adhering to medication regimen
so as to make impossible for reactivation of
the condition or complication. Realizing how
the disease is spread, helps the client take
steps to prevent further infection (Queval,
Brosch, & Simeon, 2018).
Copious secretion blocks the airways of an
individual with TB. Postural drainage and
forced expiration help clear bronchial
secretions. Increasing fluid intake enhances
systemic hydration and facilitates effective
expectoration (Queval, Brosch, & Simeon,
12
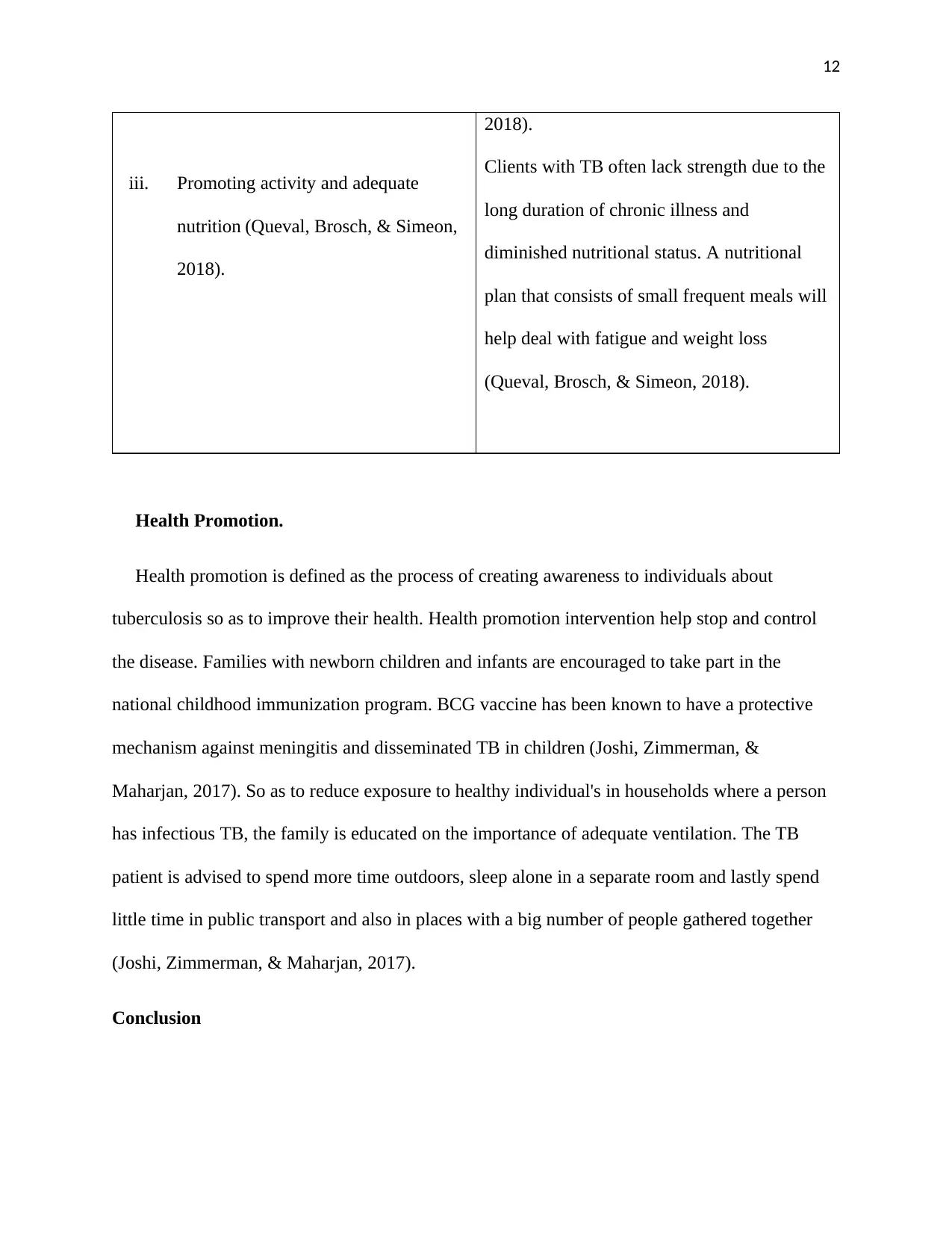
iii. Promoting activity and adequate
nutrition (Queval, Brosch, & Simeon,
2018).
2018).
Clients with TB often lack strength due to the
long duration of chronic illness and
diminished nutritional status. A nutritional
plan that consists of small frequent meals will
help deal with fatigue and weight loss
(Queval, Brosch, & Simeon, 2018).
Health Promotion.
Health promotion is defined as the process of creating awareness to individuals about
tuberculosis so as to improve their health. Health promotion intervention help stop and control
the disease. Families with newborn children and infants are encouraged to take part in the
national childhood immunization program. BCG vaccine has been known to have a protective
mechanism against meningitis and disseminated TB in children (Joshi, Zimmerman, &
Maharjan, 2017). So as to reduce exposure to healthy individual's in households where a person
has infectious TB, the family is educated on the importance of adequate ventilation. The TB
patient is advised to spend more time outdoors, sleep alone in a separate room and lastly spend
little time in public transport and also in places with a big number of people gathered together
(Joshi, Zimmerman, & Maharjan, 2017).
Conclusion
iii. Promoting activity and adequate
nutrition (Queval, Brosch, & Simeon,
2018).
2018).
Clients with TB often lack strength due to the
long duration of chronic illness and
diminished nutritional status. A nutritional
plan that consists of small frequent meals will
help deal with fatigue and weight loss
(Queval, Brosch, & Simeon, 2018).
Health Promotion.
Health promotion is defined as the process of creating awareness to individuals about
tuberculosis so as to improve their health. Health promotion intervention help stop and control
the disease. Families with newborn children and infants are encouraged to take part in the
national childhood immunization program. BCG vaccine has been known to have a protective
mechanism against meningitis and disseminated TB in children (Joshi, Zimmerman, &
Maharjan, 2017). So as to reduce exposure to healthy individual's in households where a person
has infectious TB, the family is educated on the importance of adequate ventilation. The TB
patient is advised to spend more time outdoors, sleep alone in a separate room and lastly spend
little time in public transport and also in places with a big number of people gathered together
(Joshi, Zimmerman, & Maharjan, 2017).
Conclusion
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 15
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.

