Urinary Tract Infection with Sepsis
VerifiedAdded on 2023/01/23
|9
|2174
|59
AI Summary
This document provides an in-depth understanding of the pathogenesis of urinary tract infection (UTI) and sepsis. It discusses the risk factors, symptoms, and complications associated with UTI and sepsis. The document also includes a nursing strategy and interventions for managing fluid volume deficit. Additionally, it covers the diagnostic tests used to identify UTI and sepsis. If you need help with assignments or essays related to UTI and sepsis, Desklib is the right place to find solutions.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running header: URINARY TRACT INFECTION WITH SEPSIS 1
Urinary tract infection with sepsis
Unit code and title
Lecturer
Student Name
Student ID
Date of submission
Word count
Urinary tract infection with sepsis
Unit code and title
Lecturer
Student Name
Student ID
Date of submission
Word count
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
2
Urinary tract infection with severe sepsis
Pathogenesis of UTI and Sepsis
Urinary tract infections are mostly caused by colonic bacteria such as the staphylococcus
saprophticus, Klebsiella and the E.Coli. Urinary tract infection can be categorized into a
complicated and uncomplicated infection. Risk factors associated with UTI include
vesicoureteral reflux, functional neuromuscular disorders, and urinary stasis. E.coli settle in the
periurethral area where they accumulate and ascend the urethra to the bladder causing ascending
infections. P-fimbriae allows the bacteria to attach to the epithelial surface of the bladder
(Abraham, Soman, & Miao, 2015). After bacterial colonization occurs, the bacteria ascend to the
ureter and lastly towards the kidney. Infection of the kidney causes pyelonephritis. If the
inflammation continues, tubular obstruction and damage take place which leads to interstitial
nephritis. Infiltration of inflammatory cells in the renal parenchyma leads to the activation of the
innate immune response. This leads to the secretion of cytokines such as IL-6 and IL-1. These
cytokines lead to the development of sepsis (Abraham et al., 2015).
Dysuria or painful urination usually signifies an infection of the lower urinary tract. The
discomfort is mostly described as itching, burning or stinging sensation. Pain felt during the start
of urination indicates a urethral site of disease, whereas pain that occurs after voiding indicates
pathology within the bladder or prostate. The uropathogenic E.coli (UPEC) attachment with the
urothelium cytokine release which in turn facilitates neutrophil influx. UPEC contributes to
urothelial apoptosis and thus urothelial injury (Bhat, Katy, & Place, 2015). Chemokine's also act
by stimulating sensory afferent fibers in the bladder which leads to the sensation of pain.
Urinary tract infection with severe sepsis
Pathogenesis of UTI and Sepsis
Urinary tract infections are mostly caused by colonic bacteria such as the staphylococcus
saprophticus, Klebsiella and the E.Coli. Urinary tract infection can be categorized into a
complicated and uncomplicated infection. Risk factors associated with UTI include
vesicoureteral reflux, functional neuromuscular disorders, and urinary stasis. E.coli settle in the
periurethral area where they accumulate and ascend the urethra to the bladder causing ascending
infections. P-fimbriae allows the bacteria to attach to the epithelial surface of the bladder
(Abraham, Soman, & Miao, 2015). After bacterial colonization occurs, the bacteria ascend to the
ureter and lastly towards the kidney. Infection of the kidney causes pyelonephritis. If the
inflammation continues, tubular obstruction and damage take place which leads to interstitial
nephritis. Infiltration of inflammatory cells in the renal parenchyma leads to the activation of the
innate immune response. This leads to the secretion of cytokines such as IL-6 and IL-1. These
cytokines lead to the development of sepsis (Abraham et al., 2015).
Dysuria or painful urination usually signifies an infection of the lower urinary tract. The
discomfort is mostly described as itching, burning or stinging sensation. Pain felt during the start
of urination indicates a urethral site of disease, whereas pain that occurs after voiding indicates
pathology within the bladder or prostate. The uropathogenic E.coli (UPEC) attachment with the
urothelium cytokine release which in turn facilitates neutrophil influx. UPEC contributes to
urothelial apoptosis and thus urothelial injury (Bhat, Katy, & Place, 2015). Chemokine's also act
by stimulating sensory afferent fibers in the bladder which leads to the sensation of pain.
3
Pelvic pain is mostly caused by a kidney infection. There are two routes in which bacteria can
invade and spread in the kidney. This include; hematogenous route and the ascending route. The
urethra if first colonized by the bacteria, I then use its P-fimbriae to ascend the bladder causing
ascending infections. The uropathogens go into the bladder where they multiply and infection
develops. If the vesicoureteral reflux is present the bacteria pass to the ureters and finally to the
parenchyma causing infection which is later manifested as lower abdominal pain which radiates
into the right flank (Bhat et al., 2015).
Mr. Kirkman had a heart rate of 135, blood pressure 80/42, temperature 39, oxygen saturation
82% and a respiratory rate 35 chest movements per minute. Fever is a defensive mechanism
against UTI infection (Rodgers, 2014). The white blood cell and macrophage produce pyrogens
which interfere with the thermoregulation center in the hypothalamus. They act by deceiving the
hypothalamus that the body temperatures are low raising the body temperatures above normal
causing fever. High temperatures cause fluid loss due to diaphoresis. Decreased volume in the
circulatory system causes the heart to pump quickly so as to deliver oxygen in the tissues and
also results to lower pressure in the veins as evidenced by a blood pressure of 80/42. Decreased
oxygen saturation is caused by ineffective breathing caused by abdominal pain. Abdominal pain
alters the normal functioning of the diaphragm and intercostal muscles leading to the activation
of additional muscles known as accessory muscles (Rodgers, 2014).
Under normal conditions, urine color should be pale yellow. The average urine volume in 24
hours is 800-2000 milliliters which show that an individual is well hydrated. Mr. Kirkman
manifested with a dark urine output passed in small amounts approximately 40ml in the last 24
hours. Dehydration is the major cause of dark urine. Lack of enough fluids in the body may
change the natural balance of fluids in the body leads to health problems such as fast heart rate,
Pelvic pain is mostly caused by a kidney infection. There are two routes in which bacteria can
invade and spread in the kidney. This include; hematogenous route and the ascending route. The
urethra if first colonized by the bacteria, I then use its P-fimbriae to ascend the bladder causing
ascending infections. The uropathogens go into the bladder where they multiply and infection
develops. If the vesicoureteral reflux is present the bacteria pass to the ureters and finally to the
parenchyma causing infection which is later manifested as lower abdominal pain which radiates
into the right flank (Bhat et al., 2015).
Mr. Kirkman had a heart rate of 135, blood pressure 80/42, temperature 39, oxygen saturation
82% and a respiratory rate 35 chest movements per minute. Fever is a defensive mechanism
against UTI infection (Rodgers, 2014). The white blood cell and macrophage produce pyrogens
which interfere with the thermoregulation center in the hypothalamus. They act by deceiving the
hypothalamus that the body temperatures are low raising the body temperatures above normal
causing fever. High temperatures cause fluid loss due to diaphoresis. Decreased volume in the
circulatory system causes the heart to pump quickly so as to deliver oxygen in the tissues and
also results to lower pressure in the veins as evidenced by a blood pressure of 80/42. Decreased
oxygen saturation is caused by ineffective breathing caused by abdominal pain. Abdominal pain
alters the normal functioning of the diaphragm and intercostal muscles leading to the activation
of additional muscles known as accessory muscles (Rodgers, 2014).
Under normal conditions, urine color should be pale yellow. The average urine volume in 24
hours is 800-2000 milliliters which show that an individual is well hydrated. Mr. Kirkman
manifested with a dark urine output passed in small amounts approximately 40ml in the last 24
hours. Dehydration is the major cause of dark urine. Lack of enough fluids in the body may
change the natural balance of fluids in the body leads to health problems such as fast heart rate,
4
and low blood pressure. The major cause of dehydration was the fever. The abnormal
temperatures of 39 degrees Celsius were as a result of bacterial infection in the blood. High
temperatures cause loss of too much water and electrolytes in the body. These results to reduced
total body water which leads to a decreased urine output (Nichole, 2017).
Nursing strategy
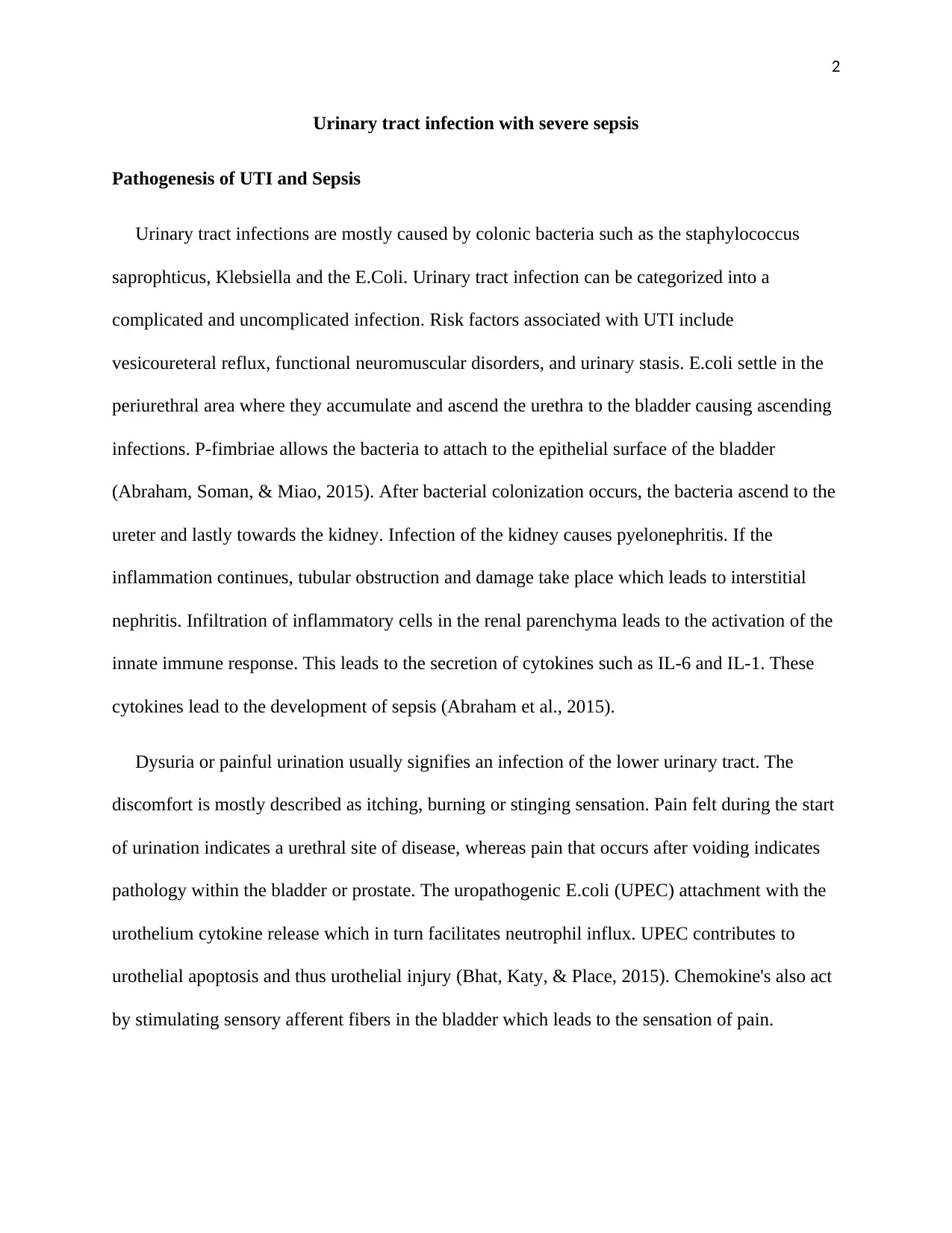
Mr. Kirman has a fluid volume deficit related to a decreased electrolyte and acid-base
imbalance evidenced by hypotension, decreased urine output, rapid heart rate, and an increased
respiratory rate. It is vital to plan the right intervention so as to correct the issue of fluid volume
deficiency. Deficient fluid volume care plan goals include the following; achieving a normal
fluid level and identifying the causative factors for behavior, deficit fluid volume and how to
prevent it (Walker, Caparon, & Hultegren, 2015).
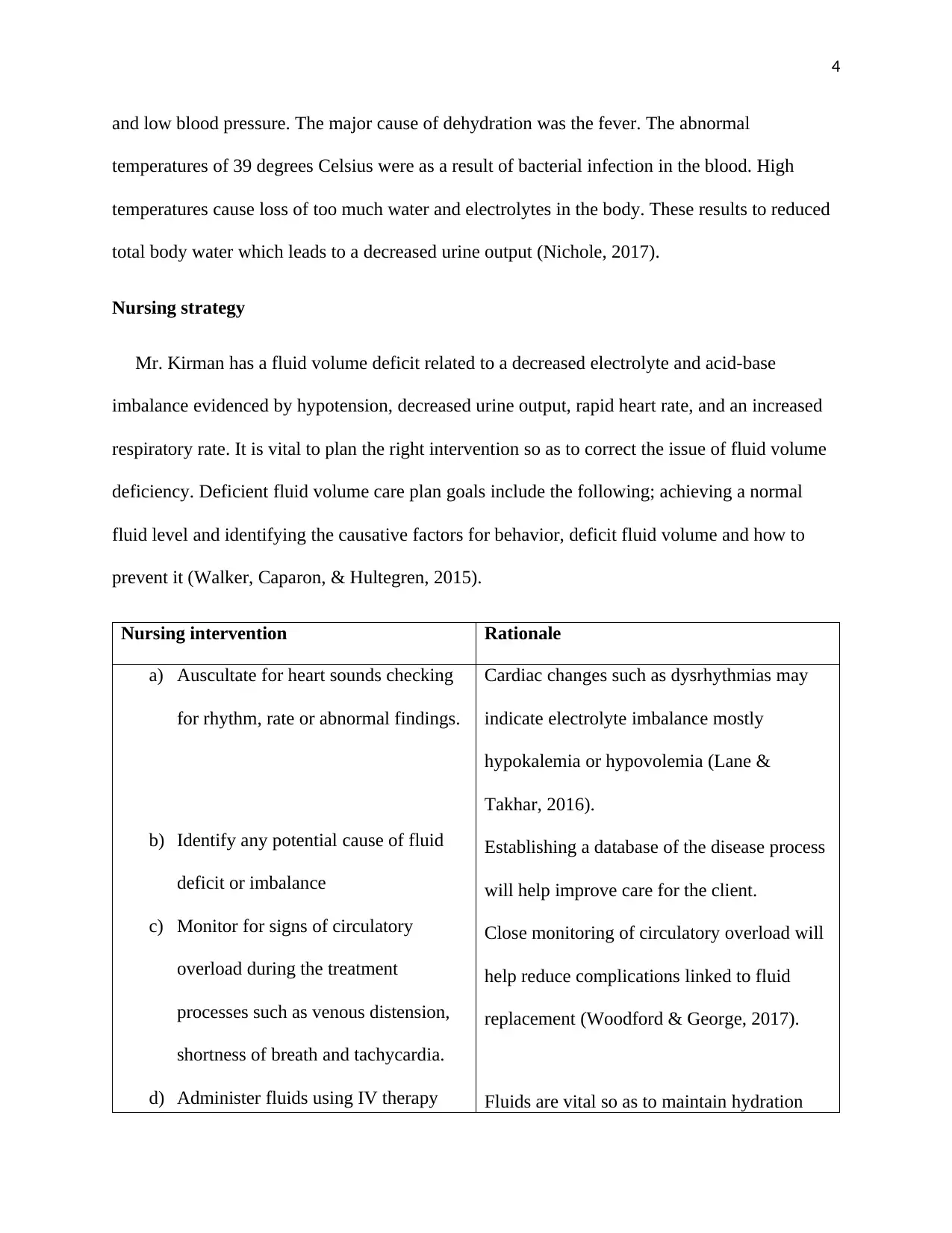
Nursing intervention Rationale
a) Auscultate for heart sounds checking
for rhythm, rate or abnormal findings.
b) Identify any potential cause of fluid
deficit or imbalance
c) Monitor for signs of circulatory
overload during the treatment
processes such as venous distension,
shortness of breath and tachycardia.
d) Administer fluids using IV therapy
Cardiac changes such as dysrhythmias may
indicate electrolyte imbalance mostly
hypokalemia or hypovolemia (Lane &
Takhar, 2016).
Establishing a database of the disease process
will help improve care for the client.
Close monitoring of circulatory overload will
help reduce complications linked to fluid
replacement (Woodford & George, 2017).
Fluids are vital so as to maintain hydration
and low blood pressure. The major cause of dehydration was the fever. The abnormal
temperatures of 39 degrees Celsius were as a result of bacterial infection in the blood. High
temperatures cause loss of too much water and electrolytes in the body. These results to reduced
total body water which leads to a decreased urine output (Nichole, 2017).
Nursing strategy
Mr. Kirman has a fluid volume deficit related to a decreased electrolyte and acid-base
imbalance evidenced by hypotension, decreased urine output, rapid heart rate, and an increased
respiratory rate. It is vital to plan the right intervention so as to correct the issue of fluid volume
deficiency. Deficient fluid volume care plan goals include the following; achieving a normal
fluid level and identifying the causative factors for behavior, deficit fluid volume and how to
prevent it (Walker, Caparon, & Hultegren, 2015).
Nursing intervention Rationale
a) Auscultate for heart sounds checking
for rhythm, rate or abnormal findings.
b) Identify any potential cause of fluid
deficit or imbalance
c) Monitor for signs of circulatory
overload during the treatment
processes such as venous distension,
shortness of breath and tachycardia.
d) Administer fluids using IV therapy
Cardiac changes such as dysrhythmias may
indicate electrolyte imbalance mostly
hypokalemia or hypovolemia (Lane &
Takhar, 2016).
Establishing a database of the disease process
will help improve care for the client.
Close monitoring of circulatory overload will
help reduce complications linked to fluid
replacement (Woodford & George, 2017).
Fluids are vital so as to maintain hydration
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
5
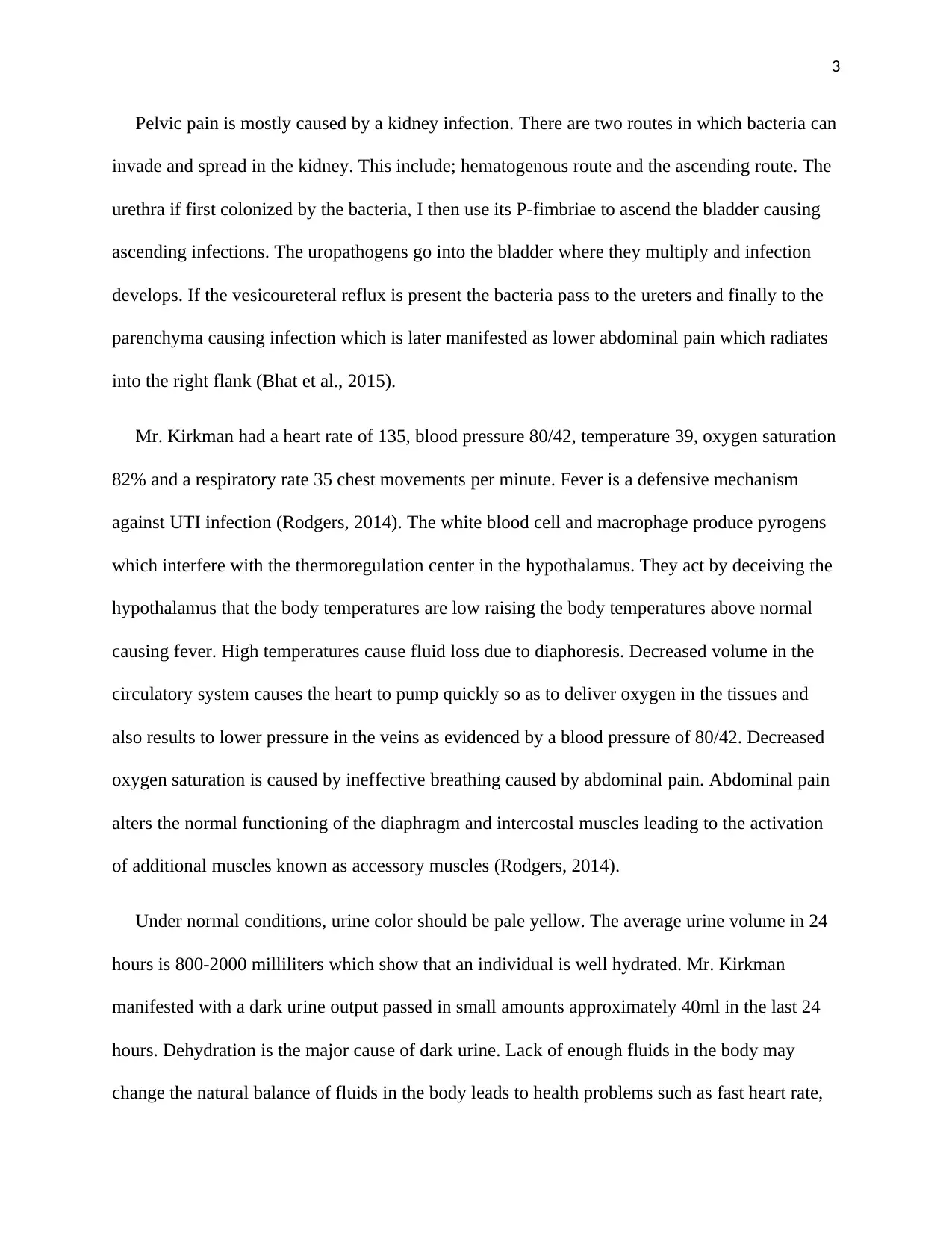
since the client has abnormal vital
signs.
e) Administer antipyretics to prevent
excessive electrolyte loss.
status.
Antipyretics reduce fever and fluid loss due to
diaphoresis (Lane & Takhar, 2016).
Diagnostics
Urinalysis.
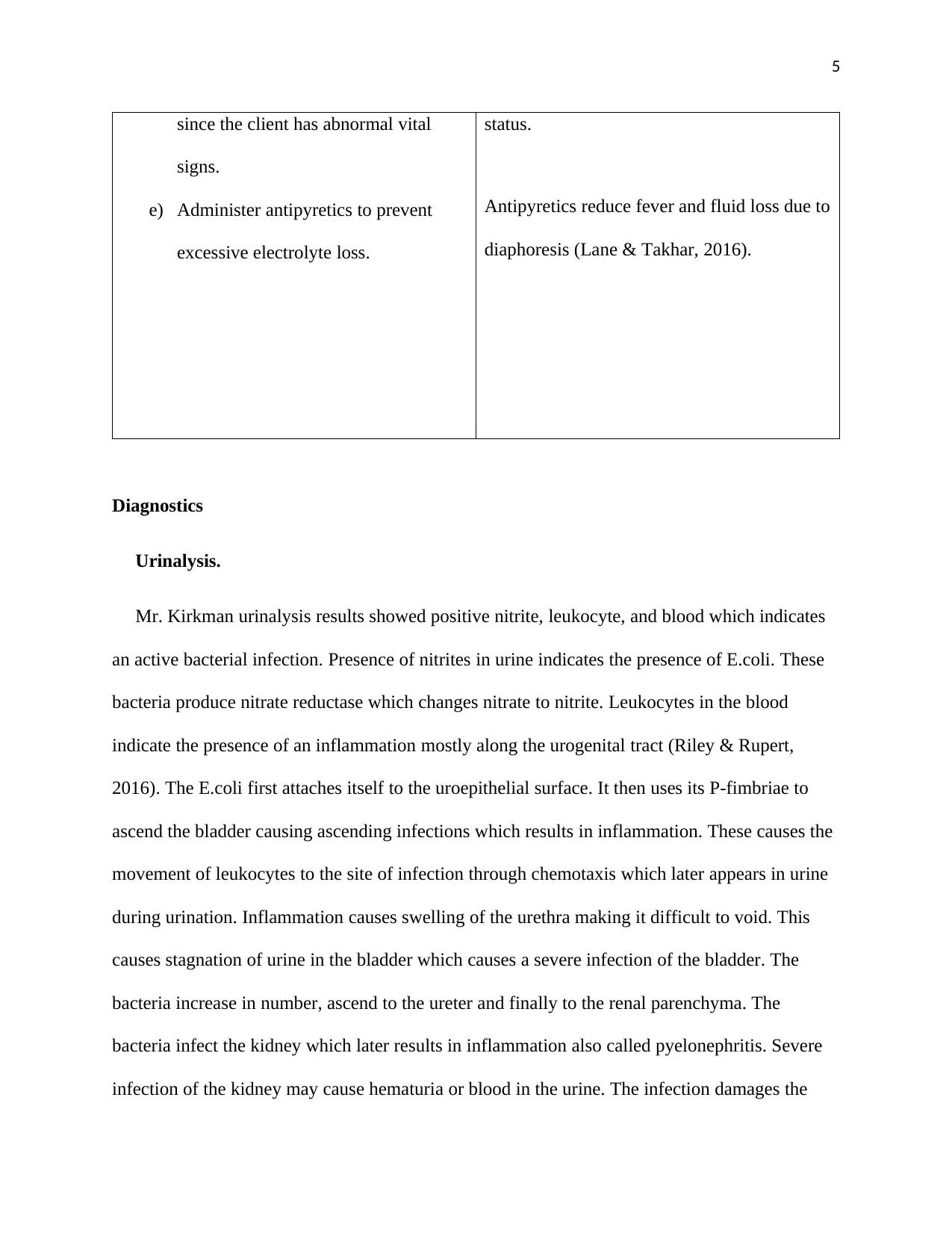
Mr. Kirkman urinalysis results showed positive nitrite, leukocyte, and blood which indicates
an active bacterial infection. Presence of nitrites in urine indicates the presence of E.coli. These
bacteria produce nitrate reductase which changes nitrate to nitrite. Leukocytes in the blood
indicate the presence of an inflammation mostly along the urogenital tract (Riley & Rupert,
2016). The E.coli first attaches itself to the uroepithelial surface. It then uses its P-fimbriae to
ascend the bladder causing ascending infections which results in inflammation. These causes the
movement of leukocytes to the site of infection through chemotaxis which later appears in urine
during urination. Inflammation causes swelling of the urethra making it difficult to void. This
causes stagnation of urine in the bladder which causes a severe infection of the bladder. The
bacteria increase in number, ascend to the ureter and finally to the renal parenchyma. The
bacteria infect the kidney which later results in inflammation also called pyelonephritis. Severe
infection of the kidney may cause hematuria or blood in the urine. The infection damages the
since the client has abnormal vital
signs.
e) Administer antipyretics to prevent
excessive electrolyte loss.
status.
Antipyretics reduce fever and fluid loss due to
diaphoresis (Lane & Takhar, 2016).
Diagnostics
Urinalysis.
Mr. Kirkman urinalysis results showed positive nitrite, leukocyte, and blood which indicates
an active bacterial infection. Presence of nitrites in urine indicates the presence of E.coli. These
bacteria produce nitrate reductase which changes nitrate to nitrite. Leukocytes in the blood
indicate the presence of an inflammation mostly along the urogenital tract (Riley & Rupert,
2016). The E.coli first attaches itself to the uroepithelial surface. It then uses its P-fimbriae to
ascend the bladder causing ascending infections which results in inflammation. These causes the
movement of leukocytes to the site of infection through chemotaxis which later appears in urine
during urination. Inflammation causes swelling of the urethra making it difficult to void. This
causes stagnation of urine in the bladder which causes a severe infection of the bladder. The
bacteria increase in number, ascend to the ureter and finally to the renal parenchyma. The
bacteria infect the kidney which later results in inflammation also called pyelonephritis. Severe
infection of the kidney may cause hematuria or blood in the urine. The infection damages the
6
glomerular filtration barrier which promotes red blood cell passage throughout the layer which
later appears in urine (Riley & Rupert, 2016).
Arterial blood gases.
Mr. Kirkman has decreased PaO2, PaCO2, and HCO3. Kidney infection results in severe
lower abdominal pain which radiates to the right flank. Pain activates the sympathetic nervous
system. After its activation, it stimulates brainstem cells to release serotonin and noradrenaline
into the dorsal horn. Therefore, it increases the respiratory rate, heart rate, and blood pressure.
These physiologic changes, mostly for a person with a poor physiologic reserve may result in
hypoxia and thereafter ischemic damage. The common cause of metabolic acidosis in chronic
renal failure. Metabolic acidosis results in decreased PaCO2, HCO3, increased lactate and base
excess. One of the major function of the kidneys is to regulate acids in the body (Ballie, 2017).
The kidney performs this action by eliminating acid from the blood through urine. In metabolic
acidosis, there is an accumulation of acid in the body. This occurs when the kidney is not able to
remove acid from the body. Loss of function is caused by the UTI infection which ascended to
the bladder and lastly to the kidney causing pyelonephritis. Metabolic acidosis causes a reduction
in HCO3 concentrations. The respiratory system compensates for acidosis through
hyperventilating resulting in the reduction in PaCO2 (Ballie, 2017).
Full blood count.
Mr. Kirkman full blood count indicated an increased white blood cell production. He had
severe sepsis which is a life-threatening condition. Sepsis can lead to widespread inflammation.
Inflammation causes the attraction of white blood cells to the site of infection through
chemotaxis. White blood cells increase in response to infection (Rodgers, 2014).
glomerular filtration barrier which promotes red blood cell passage throughout the layer which
later appears in urine (Riley & Rupert, 2016).
Arterial blood gases.
Mr. Kirkman has decreased PaO2, PaCO2, and HCO3. Kidney infection results in severe
lower abdominal pain which radiates to the right flank. Pain activates the sympathetic nervous
system. After its activation, it stimulates brainstem cells to release serotonin and noradrenaline
into the dorsal horn. Therefore, it increases the respiratory rate, heart rate, and blood pressure.
These physiologic changes, mostly for a person with a poor physiologic reserve may result in
hypoxia and thereafter ischemic damage. The common cause of metabolic acidosis in chronic
renal failure. Metabolic acidosis results in decreased PaCO2, HCO3, increased lactate and base
excess. One of the major function of the kidneys is to regulate acids in the body (Ballie, 2017).
The kidney performs this action by eliminating acid from the blood through urine. In metabolic
acidosis, there is an accumulation of acid in the body. This occurs when the kidney is not able to
remove acid from the body. Loss of function is caused by the UTI infection which ascended to
the bladder and lastly to the kidney causing pyelonephritis. Metabolic acidosis causes a reduction
in HCO3 concentrations. The respiratory system compensates for acidosis through
hyperventilating resulting in the reduction in PaCO2 (Ballie, 2017).
Full blood count.
Mr. Kirkman full blood count indicated an increased white blood cell production. He had
severe sepsis which is a life-threatening condition. Sepsis can lead to widespread inflammation.
Inflammation causes the attraction of white blood cells to the site of infection through
chemotaxis. White blood cells increase in response to infection (Rodgers, 2014).
7
Electrolyte, urea, and creatinine.
Mr. Kirkman had increased sodium, potassium, chlorine, urea and creatinine. Sodium
functions by carrying an electrical charge when dissolved in the blood. In hypernatremia, an
individual contains little water for the amount of sodium. Sodium levels abnormally increase
when the rate of water loss exceeds sodium loss. Excess water loss is caused by dehydration such
as drinking little water or high fever which causes sweating excessively (Yee & Rabinstein,
2014). UTI leads to the damage of proximal convoluted tubule causing an increased level of
potassium and chlorine. Lactate acidosis happens when the production of lactic acid exceeds its
removal. Increased lactate production is caused by impaired tissue oxygenation which is brought
by difficulty in breathing due to abdominal pain. High levels of urea in the blood is a clinical
manifestation of kidney failure. Infection of the glomerulus causes an ineffective removal of urea
from the blood leading to uremia (Depner, 2015). Abnormally high level of creatinine indicates
malfunction or kidney failure. Creatinine levels increase in the blood due to ineffective clearance
of creatinine by the kidney (Shemesh, Golbetz, Kriss, & Myers, 2017).
References
Electrolyte, urea, and creatinine.
Mr. Kirkman had increased sodium, potassium, chlorine, urea and creatinine. Sodium
functions by carrying an electrical charge when dissolved in the blood. In hypernatremia, an
individual contains little water for the amount of sodium. Sodium levels abnormally increase
when the rate of water loss exceeds sodium loss. Excess water loss is caused by dehydration such
as drinking little water or high fever which causes sweating excessively (Yee & Rabinstein,
2014). UTI leads to the damage of proximal convoluted tubule causing an increased level of
potassium and chlorine. Lactate acidosis happens when the production of lactic acid exceeds its
removal. Increased lactate production is caused by impaired tissue oxygenation which is brought
by difficulty in breathing due to abdominal pain. High levels of urea in the blood is a clinical
manifestation of kidney failure. Infection of the glomerulus causes an ineffective removal of urea
from the blood leading to uremia (Depner, 2015). Abnormally high level of creatinine indicates
malfunction or kidney failure. Creatinine levels increase in the blood due to ineffective clearance
of creatinine by the kidney (Shemesh, Golbetz, Kriss, & Myers, 2017).
References
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
8
Abraham, S., Soman, N., & Miao, Y. (2015). The nature of immune responses to urinary tract
infections. Nature Reviews. Immunology, 15(10), 655-663.
Ballie, J. (2017). Simple, easily memorized 'rules of thumb' for the rapid assessment of
physiological compensation for acid-base disorders. Thorax, 63(3), 289-290.
Bhat, R., Katy, T., & Place, F. (2015). Pediatric urinary tract infections. Emergency Medicine
Clinics of North America, 29(3), 637-653.
Depner, T. (2015). Uremic Toxicity: Urea and Beyond. Semin. Dial, 14(4), 246-251.
Lane, D., & Takhar, S. (2016). Diagnosis and management of urinary tract infection and
pyelonephritis. Emergency Medicine Clinics of North America, 29(3), 539-552.
Nichole, L. (2017). Uncomplicated urinary tract infection in adults including uncomplicated
pyelonephritis. rol Clin North Am, 35(1), 1-12.
Riley, L., & Rupert, J. (2016). Evaluation of Patients with Leukocytosis. Am Fam
Physician, 92(11), 1004-1011.
Rodgers, K. (2014). Leukocytosis definition Blood: Physiology and Circulation. Basics of
Clinical Assessment, 198, 67-69.
Shemesh, O., Golbetz, H., Kriss, P., & Myers, B. (2017). Limitations of creatinine as a filtration
marker in glomerulopathic patients. Kidney Int, 28(5), 830-838.
Walker, J., Caparon, M., & Hultegren, M. (2015). Urinary tract infections: epidemiology,
mechanisms of infection and treatment options. Nature Reviews. Microbiology, 13(5),
269-284.
Woodford, H., & George, J. (2017). Diagnosis and management of urinary infections in older
people. Clinical Medicine, 11(1), 80-83.
Abraham, S., Soman, N., & Miao, Y. (2015). The nature of immune responses to urinary tract
infections. Nature Reviews. Immunology, 15(10), 655-663.
Ballie, J. (2017). Simple, easily memorized 'rules of thumb' for the rapid assessment of
physiological compensation for acid-base disorders. Thorax, 63(3), 289-290.
Bhat, R., Katy, T., & Place, F. (2015). Pediatric urinary tract infections. Emergency Medicine
Clinics of North America, 29(3), 637-653.
Depner, T. (2015). Uremic Toxicity: Urea and Beyond. Semin. Dial, 14(4), 246-251.
Lane, D., & Takhar, S. (2016). Diagnosis and management of urinary tract infection and
pyelonephritis. Emergency Medicine Clinics of North America, 29(3), 539-552.
Nichole, L. (2017). Uncomplicated urinary tract infection in adults including uncomplicated
pyelonephritis. rol Clin North Am, 35(1), 1-12.
Riley, L., & Rupert, J. (2016). Evaluation of Patients with Leukocytosis. Am Fam
Physician, 92(11), 1004-1011.
Rodgers, K. (2014). Leukocytosis definition Blood: Physiology and Circulation. Basics of
Clinical Assessment, 198, 67-69.
Shemesh, O., Golbetz, H., Kriss, P., & Myers, B. (2017). Limitations of creatinine as a filtration
marker in glomerulopathic patients. Kidney Int, 28(5), 830-838.
Walker, J., Caparon, M., & Hultegren, M. (2015). Urinary tract infections: epidemiology,
mechanisms of infection and treatment options. Nature Reviews. Microbiology, 13(5),
269-284.
Woodford, H., & George, J. (2017). Diagnosis and management of urinary infections in older
people. Clinical Medicine, 11(1), 80-83.
9
Yee, A., & Rabinstein, A. (2014). Neurologic presentations of acid-base imbalance, electrolyte
abnormalities, and endocrine emergencies. Neurol Clin, 28(1), 1-16.
Yee, A., & Rabinstein, A. (2014). Neurologic presentations of acid-base imbalance, electrolyte
abnormalities, and endocrine emergencies. Neurol Clin, 28(1), 1-16.
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





