Urinary Tract Infection with Severe Sepsis
VerifiedAdded on 2023/01/23
|7
|1866
|44
AI Summary
This document discusses the pathogenesis of urinary tract infection (UTI) and sepsis, including the role of bacteria in ascending infection. It also explores the symptoms of UTI, such as painful urination and dark urine. The document further delves into the nursing strategy for managing fluid volume deficit in UTI patients. Additionally, it provides insights into the interpretation of arterial blood gas analysis, urinalysis, full blood count, and electrolyte, urea, and creatinine levels. References are included for further reading.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
Running header: URINARY TRACT INFECTION WITH SEVERE SEPSIS 1
Urinary tract infection with severe sepsis
Unit code and Title
Lecturer
Student Name
Student ID
Date of Submission
Word Count
Urinary tract infection with severe sepsis
Unit code and Title
Lecturer
Student Name
Student ID
Date of Submission
Word Count
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
2
Urinary tract infection with severe sepsis
Pathogenesis of UTI and Sepsis
Urinary tract infection involves the lower urinary tract infection or the upper urinary tract
infection. In lower urinary tract infection the bacteria colonize the periurethral area where it
accumulates and ascends to the bladder. The bacteria continue to replicate in the bladder, after
sufficient increase it ascends to the ureter towards the kidney (Woodford & George, 2017). It
uses it fimbria in the ascension process. The infection damages the renal parenchyma leading to a
condition called pyelonephritis. Severe infection may result in acute kidney injury where there
are tubular obstruction and damage. If the inflammation continues, inflammatory cells infiltrate
the renal parenchyma leading to activation of the innate immune system. This results in
cytokines which cause the development of sepsis (Woodford & George, 2017).
Painful urination mostly indicates a lower urinary tract infection. The burning sensation is
mostly felt at the opening of the urethra and less frequently over the bladder. Painful urination is
also known as dysuria. Dysuria is usually caused by urethral or bladder inflammation. The major
causes are urethritis and cystitis. Urethritis involves invasion by an infectious agent which
damages the local mucous membrane of epithelial cells (Nichole, 2017). This causes
inflammatory changes which involve the collection of leukocytes and chemical mediators such
as cytokines and antibodies. Accumulation of this mediators result in pain and swelling.
Inflammation can also cause continuous scarring which constricts the urethra. The swelling and
accumulation of fibrous tissue can make micturition painful and difficult (Nichole, 2017). The
obstruction of the urethra makes it impossible for one to void leading to a collection of stagnant
urine in the bladder, generally called urine stasis. Urine stasis brings about severe infection if not
Urinary tract infection with severe sepsis
Pathogenesis of UTI and Sepsis
Urinary tract infection involves the lower urinary tract infection or the upper urinary tract
infection. In lower urinary tract infection the bacteria colonize the periurethral area where it
accumulates and ascends to the bladder. The bacteria continue to replicate in the bladder, after
sufficient increase it ascends to the ureter towards the kidney (Woodford & George, 2017). It
uses it fimbria in the ascension process. The infection damages the renal parenchyma leading to a
condition called pyelonephritis. Severe infection may result in acute kidney injury where there
are tubular obstruction and damage. If the inflammation continues, inflammatory cells infiltrate
the renal parenchyma leading to activation of the innate immune system. This results in
cytokines which cause the development of sepsis (Woodford & George, 2017).
Painful urination mostly indicates a lower urinary tract infection. The burning sensation is
mostly felt at the opening of the urethra and less frequently over the bladder. Painful urination is
also known as dysuria. Dysuria is usually caused by urethral or bladder inflammation. The major
causes are urethritis and cystitis. Urethritis involves invasion by an infectious agent which
damages the local mucous membrane of epithelial cells (Nichole, 2017). This causes
inflammatory changes which involve the collection of leukocytes and chemical mediators such
as cytokines and antibodies. Accumulation of this mediators result in pain and swelling.
Inflammation can also cause continuous scarring which constricts the urethra. The swelling and
accumulation of fibrous tissue can make micturition painful and difficult (Nichole, 2017). The
obstruction of the urethra makes it impossible for one to void leading to a collection of stagnant
urine in the bladder, generally called urine stasis. Urine stasis brings about severe infection if not
3
managed earlier; the back pressure of urine results to a kidney infection which is manifested with
lower abdominal pain which radiates to the right flank (Nichole, 2017).
Mr. Kirmann had a heart rate of 135, blood pressure 80/42, temperature 39, oxygen saturation
of 82% and respiratory rate of 32. The abnormally high temperatures of 39C was a result of
bacterial infection in the blood. Pyrogens are released by white blood cells and macrophages.
This chemicals flow in the bloodstream to the hypothalamus in the brain which controls body
temperature. Pyrogens raise the set point of the hypothalamus through the action of prostaglandin
E2 (Rodgers, 2014). This causes the hypothalamus to increases the core body temperature to a
new set point causing fever. High temperatures cause an increase in breathing rate, heart rate and
blood circulation to the skin. An increased core body temperature causes the blood vessels to
dilate which decrease blood pressure. The dilation of blood vessels due to fever will result in an
increased heart rate so as to maintain the blood pressure. High temperatures also denature the
bond between iron in hemoglobin and O2 resulting in a decreased oxygen saturation (Rodgers,
2014).
Ideally, normal urine color should be pale yellow and a normal urine volume of 800-2000
milliliters in 24 hours which indicates that an individual is hydrated. Mr. Kirmann had a dark
urine output passed in small amounts of approximately 40ml in the last 8 hours. Dark urine is
usually a sign of dehydration which mostly occurs when there is less water in the body. Fever
causes increased sweating, fluid, and electrolyte loss. There is also a possibility of drinking less
water due to feeling unwell. Too much loss of water will cause a decreased urine output which
appears darker in color (Walker, Caparon, & Hultegren, 2015).
managed earlier; the back pressure of urine results to a kidney infection which is manifested with
lower abdominal pain which radiates to the right flank (Nichole, 2017).
Mr. Kirmann had a heart rate of 135, blood pressure 80/42, temperature 39, oxygen saturation
of 82% and respiratory rate of 32. The abnormally high temperatures of 39C was a result of
bacterial infection in the blood. Pyrogens are released by white blood cells and macrophages.
This chemicals flow in the bloodstream to the hypothalamus in the brain which controls body
temperature. Pyrogens raise the set point of the hypothalamus through the action of prostaglandin
E2 (Rodgers, 2014). This causes the hypothalamus to increases the core body temperature to a
new set point causing fever. High temperatures cause an increase in breathing rate, heart rate and
blood circulation to the skin. An increased core body temperature causes the blood vessels to
dilate which decrease blood pressure. The dilation of blood vessels due to fever will result in an
increased heart rate so as to maintain the blood pressure. High temperatures also denature the
bond between iron in hemoglobin and O2 resulting in a decreased oxygen saturation (Rodgers,
2014).
Ideally, normal urine color should be pale yellow and a normal urine volume of 800-2000
milliliters in 24 hours which indicates that an individual is hydrated. Mr. Kirmann had a dark
urine output passed in small amounts of approximately 40ml in the last 8 hours. Dark urine is
usually a sign of dehydration which mostly occurs when there is less water in the body. Fever
causes increased sweating, fluid, and electrolyte loss. There is also a possibility of drinking less
water due to feeling unwell. Too much loss of water will cause a decreased urine output which
appears darker in color (Walker, Caparon, & Hultegren, 2015).
4
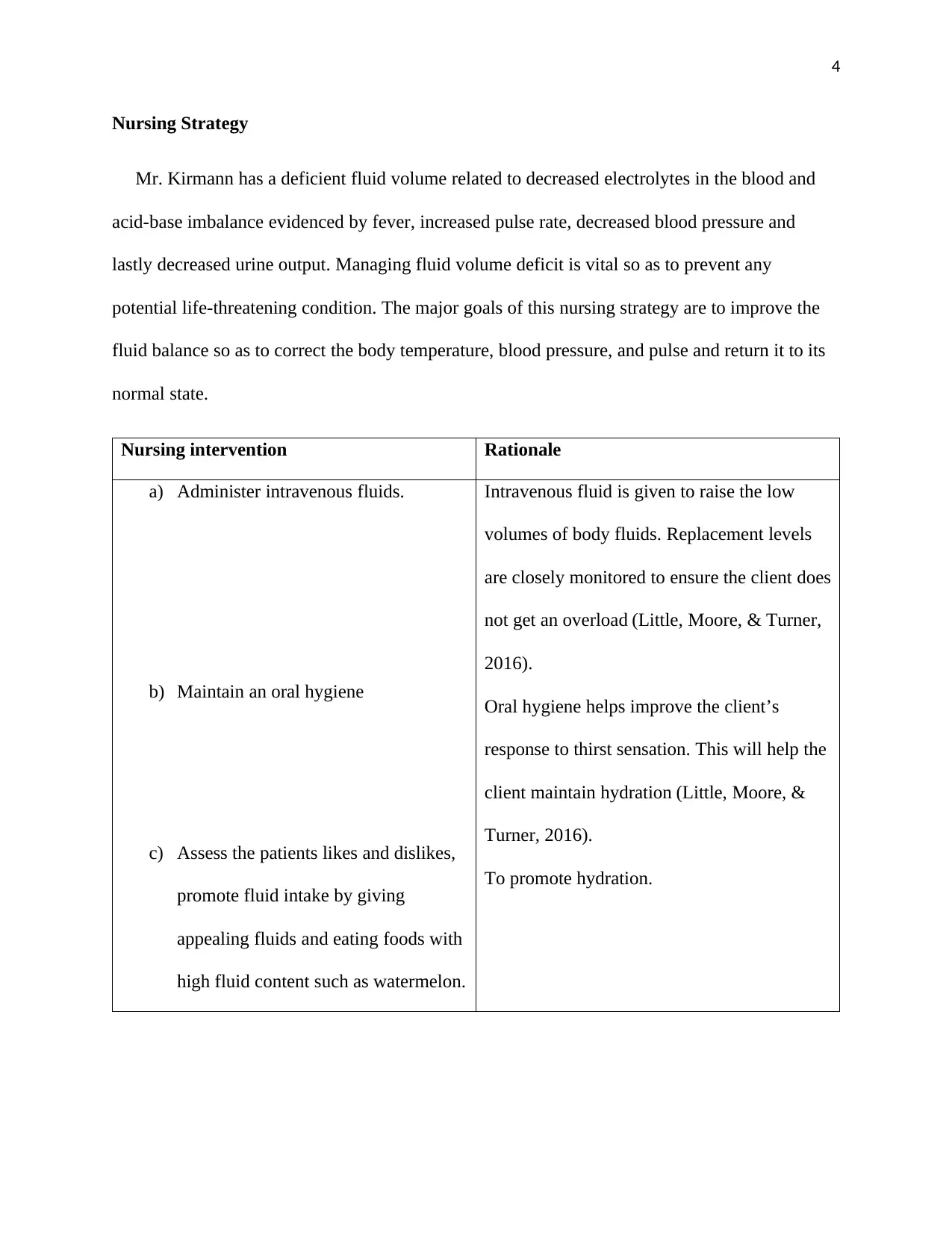
Nursing Strategy
Mr. Kirmann has a deficient fluid volume related to decreased electrolytes in the blood and
acid-base imbalance evidenced by fever, increased pulse rate, decreased blood pressure and
lastly decreased urine output. Managing fluid volume deficit is vital so as to prevent any
potential life-threatening condition. The major goals of this nursing strategy are to improve the
fluid balance so as to correct the body temperature, blood pressure, and pulse and return it to its
normal state.
Nursing intervention Rationale
a) Administer intravenous fluids.
b) Maintain an oral hygiene
c) Assess the patients likes and dislikes,
promote fluid intake by giving
appealing fluids and eating foods with
high fluid content such as watermelon.
Intravenous fluid is given to raise the low
volumes of body fluids. Replacement levels
are closely monitored to ensure the client does
not get an overload (Little, Moore, & Turner,
2016).
Oral hygiene helps improve the client’s
response to thirst sensation. This will help the
client maintain hydration (Little, Moore, &
Turner, 2016).
To promote hydration.
Nursing Strategy
Mr. Kirmann has a deficient fluid volume related to decreased electrolytes in the blood and
acid-base imbalance evidenced by fever, increased pulse rate, decreased blood pressure and
lastly decreased urine output. Managing fluid volume deficit is vital so as to prevent any
potential life-threatening condition. The major goals of this nursing strategy are to improve the
fluid balance so as to correct the body temperature, blood pressure, and pulse and return it to its
normal state.
Nursing intervention Rationale
a) Administer intravenous fluids.
b) Maintain an oral hygiene
c) Assess the patients likes and dislikes,
promote fluid intake by giving
appealing fluids and eating foods with
high fluid content such as watermelon.
Intravenous fluid is given to raise the low
volumes of body fluids. Replacement levels
are closely monitored to ensure the client does
not get an overload (Little, Moore, & Turner,
2016).
Oral hygiene helps improve the client’s
response to thirst sensation. This will help the
client maintain hydration (Little, Moore, &
Turner, 2016).
To promote hydration.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
5
Arterial Blood Gas Analysis
Urinalysis.
Mr. Kirkman urinalysis results showed positive nitrite, leukocyte, and blood which indicated
an active bacterial infection. A positive nitrite test indicates a UTI infection mostly caused by E.
coli. Nitrites existence in urine is due to change of nitrates to nitrites by the bacteria. Leukocytes
in urine indicate inflammation specifically the urogenital tract. Before anything, the bacteria first
attaches itself to the urinary tract to prevent washing out during micturition (Simerville, Maxted,
& Pahira, 2018). After attachment, it accumulates in the uroepithelial causing injury. Injury to
the uroepithelial surface leads to inflammation (Das, Towle, & Van, 2107, p. xx). This causes the
movement of macrophage into the area of infection. Macrophages release chemokines such as
IL-1 and IL-6 which cause attraction of leukocyte to urinary tract through chemotaxis which later
appears in urine during micturition. Bacteria from the urethra colonizes and ascends to the
bladder where colonization occurs and ascends to ureter towards the kidney causing
pyelonephritis. The bacteria damage the glomerular filtration barrier (Das, Towle, & Van, 2107,
p. xx). The barrier ends to sieve molecules which are 50-100nm hence preventing RBC which
have 6.2-8.2 μm from getting out. Damage of this barrier increases the fenestration allowing the
red blood cells to filter out.
Arterial blood gas.
Mr. Kirmann has a decreased PAO2, PaCO2, HCO3, and base excess. Decreased oxygen
saturation is caused by high fever brought about by bacterial infection in the blood. Pyrogens
released by the macrophages raise the set point of the hypothalamus increasing the core body
(Kofstad, 2017). High temperatures increase skin blood flow. Thereafter, it decreases tolerance
Arterial Blood Gas Analysis
Urinalysis.
Mr. Kirkman urinalysis results showed positive nitrite, leukocyte, and blood which indicated
an active bacterial infection. A positive nitrite test indicates a UTI infection mostly caused by E.
coli. Nitrites existence in urine is due to change of nitrates to nitrites by the bacteria. Leukocytes
in urine indicate inflammation specifically the urogenital tract. Before anything, the bacteria first
attaches itself to the urinary tract to prevent washing out during micturition (Simerville, Maxted,
& Pahira, 2018). After attachment, it accumulates in the uroepithelial causing injury. Injury to
the uroepithelial surface leads to inflammation (Das, Towle, & Van, 2107, p. xx). This causes the
movement of macrophage into the area of infection. Macrophages release chemokines such as
IL-1 and IL-6 which cause attraction of leukocyte to urinary tract through chemotaxis which later
appears in urine during micturition. Bacteria from the urethra colonizes and ascends to the
bladder where colonization occurs and ascends to ureter towards the kidney causing
pyelonephritis. The bacteria damage the glomerular filtration barrier (Das, Towle, & Van, 2107,
p. xx). The barrier ends to sieve molecules which are 50-100nm hence preventing RBC which
have 6.2-8.2 μm from getting out. Damage of this barrier increases the fenestration allowing the
red blood cells to filter out.
Arterial blood gas.
Mr. Kirmann has a decreased PAO2, PaCO2, HCO3, and base excess. Decreased oxygen
saturation is caused by high fever brought about by bacterial infection in the blood. Pyrogens
released by the macrophages raise the set point of the hypothalamus increasing the core body
(Kofstad, 2017). High temperatures increase skin blood flow. Thereafter, it decreases tolerance
6
to central hypovolemia. Hemoglobin carries out its function by delivering oxygen to tissues.
High temperatures alter the affinity of hemoglobin to oxygen. High temperatures reduce the
affinity of hemoglobin and oxygen offload. The common cause of metabolic acidosis is a renal
failure which results in decreased PaCO2, HCO3, increased lactate and base excess.
Accumulations of acids in the body occur when the kidney is unable to eliminate the acids
leading to the accumulation of acids in the body. Metabolic acidosis causes decreased HCO3
concentrations and thus the respiratory system compensates for acidosis through hyperventilating
resulting in a reduction in PaCO2 (Kofstad, 2017).
Full blood count.
Mr. Kirkman full blood count indicated an increased white blood cell production. The
abnormal rise of WBC is caused by bacteria in the blood. Increased leukocyte indicate that the
immune system is working effectively destroy infection (Rodgers, 2014).
Electrolytes, urea, and creatinine.
Urinary tract infection leads to the damage of proximal convoluted tubule which causes an
increase in sodium, chlorine, and potassium. Damage of this tubule interferes with selective
reabsorption of this electrolyte leading to their increase (Decaux, Andres, & Gankam, 2016). The
kidney uses tiny filtering units known as nephron to eliminate urea from the blood. Inflammation
of the nephron due to kidney infection will result in ineffective removal of urea from the blood
resulting in uremia. Creatinine is a waste product formed after the wear and tear of muscles.
Kidney infection caused by the bacteria results in the inability of the kidney to remove creatinine
(Shemesh, Golbetz, Kriss, & Myers, 2017).
to central hypovolemia. Hemoglobin carries out its function by delivering oxygen to tissues.
High temperatures alter the affinity of hemoglobin to oxygen. High temperatures reduce the
affinity of hemoglobin and oxygen offload. The common cause of metabolic acidosis is a renal
failure which results in decreased PaCO2, HCO3, increased lactate and base excess.
Accumulations of acids in the body occur when the kidney is unable to eliminate the acids
leading to the accumulation of acids in the body. Metabolic acidosis causes decreased HCO3
concentrations and thus the respiratory system compensates for acidosis through hyperventilating
resulting in a reduction in PaCO2 (Kofstad, 2017).
Full blood count.
Mr. Kirkman full blood count indicated an increased white blood cell production. The
abnormal rise of WBC is caused by bacteria in the blood. Increased leukocyte indicate that the
immune system is working effectively destroy infection (Rodgers, 2014).
Electrolytes, urea, and creatinine.
Urinary tract infection leads to the damage of proximal convoluted tubule which causes an
increase in sodium, chlorine, and potassium. Damage of this tubule interferes with selective
reabsorption of this electrolyte leading to their increase (Decaux, Andres, & Gankam, 2016). The
kidney uses tiny filtering units known as nephron to eliminate urea from the blood. Inflammation
of the nephron due to kidney infection will result in ineffective removal of urea from the blood
resulting in uremia. Creatinine is a waste product formed after the wear and tear of muscles.
Kidney infection caused by the bacteria results in the inability of the kidney to remove creatinine
(Shemesh, Golbetz, Kriss, & Myers, 2017).
7
References
Das, R., Towle, V., & Van, P. (2107). Adverse outcomes in nursing home residents with
increased episodes of observed bacteriuria. Infect Control Hosp Epidemiol, 32(1), 84-86.
Decaux, G., Andres, C., & Gankam, K. (2016). Treatment of euvolemic hyponatremia in the
intensive care unit by urea. Critical Care, 14(5), 184.
Kofstad, J. (2017). Blood Gases and Hypothermia: Some Theoretical and Practical
Considerations. Scand J Clin Lab Invest, 224, 21-26.
Little, P., Moore, M., & Turner, S. (2016). Effectiveness of five different approaches in the
management of urinary tract infection: a randomized controlled trial. BMJ, 340, 199.
Nichole, L. (2017). Uncomplicated urinary tract infection in adults including uncomplicated
pyelonephritis. roll Clin North Am, 35(1), 1-12.
Rodgers, K. (2014). Leukocytosis definition Blood: Physiology and Circulation. Basics of
Clinical Assessment, 198, 67-69.
Shemesh, O., Golbetz, H., Kriss, P., & Myers, B. (2017). Limitations of creatinine as a filtration
marker in glomerulopathic patients. Kidney Int, 28(5), 830-838.
Simerville, J., Maxted, W., & Pahira, J. (2018). Urinalysis: a comprehensive review. American
Family Physician, 71(6), 1153-1162.
Walker, J., Caparon, M., & Hultegren, M. (2015). Urinary tract infections: epidemiology,
mechanisms of infection and treatment options. Nature Reviews. Microbiology, 13(5),
269-284.
Woodford, H., & George, J. (2017). Diagnosis and management of urinary infections in older
people. Clinical Medicine, 11(1), 80-83.
References
Das, R., Towle, V., & Van, P. (2107). Adverse outcomes in nursing home residents with
increased episodes of observed bacteriuria. Infect Control Hosp Epidemiol, 32(1), 84-86.
Decaux, G., Andres, C., & Gankam, K. (2016). Treatment of euvolemic hyponatremia in the
intensive care unit by urea. Critical Care, 14(5), 184.
Kofstad, J. (2017). Blood Gases and Hypothermia: Some Theoretical and Practical
Considerations. Scand J Clin Lab Invest, 224, 21-26.
Little, P., Moore, M., & Turner, S. (2016). Effectiveness of five different approaches in the
management of urinary tract infection: a randomized controlled trial. BMJ, 340, 199.
Nichole, L. (2017). Uncomplicated urinary tract infection in adults including uncomplicated
pyelonephritis. roll Clin North Am, 35(1), 1-12.
Rodgers, K. (2014). Leukocytosis definition Blood: Physiology and Circulation. Basics of
Clinical Assessment, 198, 67-69.
Shemesh, O., Golbetz, H., Kriss, P., & Myers, B. (2017). Limitations of creatinine as a filtration
marker in glomerulopathic patients. Kidney Int, 28(5), 830-838.
Simerville, J., Maxted, W., & Pahira, J. (2018). Urinalysis: a comprehensive review. American
Family Physician, 71(6), 1153-1162.
Walker, J., Caparon, M., & Hultegren, M. (2015). Urinary tract infections: epidemiology,
mechanisms of infection and treatment options. Nature Reviews. Microbiology, 13(5),
269-284.
Woodford, H., & George, J. (2017). Diagnosis and management of urinary infections in older
people. Clinical Medicine, 11(1), 80-83.
1 out of 7
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





