Essay on Schizoaffective disorder
VerifiedAdded on 2022/11/17
|13
|3401
|196
AI Summary
This essay discusses Schizoaffective Disorder, its symptoms, diagnosis, treatment, and impact on patients. It provides insights into the demographic information based on Australia and the roles of a multidisciplinary team. The essay also covers the DSM 5 methodology of identification of the disease and the exploration of the prodromal phase. It concludes with the importance of prevention and the need for a collaborative effort to cure the illness.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Essay on Schizoaffective disorder
Essay on Schizoaffective disorder
Name of the Student
Roll NO
Subject Code
Essay on Schizoaffective disorder
Name of the Student
Roll NO
Subject Code
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1Essay on Schizoaffective disorder
An essay on Schizoaffective Disorder (SAD)
Schizoaffective disorder (SAD) is a chronic, psychotic disorder. SAD often has
melancholy mood and psychotic symptoms such as hallucination, mood swing and depression.
Schizoaffective was defined by Kraepelin's nosological as bifurcation of two disorders. It is a
variant of schizophrenia and affective disorders, the patient illness is somewhere between these
two disorders. In the extreme case the patient either shows schizophrenia disorder or affective
disorder. Schizophrenia is a disorder that appears during adolescences or early childhood. The
disorder is characterized by hallucination, delusions, and other cognitive disorders. It is not easy
to overcome schizophrenia (Sekar et al., 2016). The cause can be genetic or environmental
factors such as genetic disorder in the family, chemical imbalance in the brain or social
relationship issues. The affective disorder is generally called as the mood disorder (Hayes et al.,
2015). It can appear at any stage of life. It is seen least in children and more in adolescences. It
generally affects the patient in the mid 30s as studied by the researchers (Coryell, 2016).
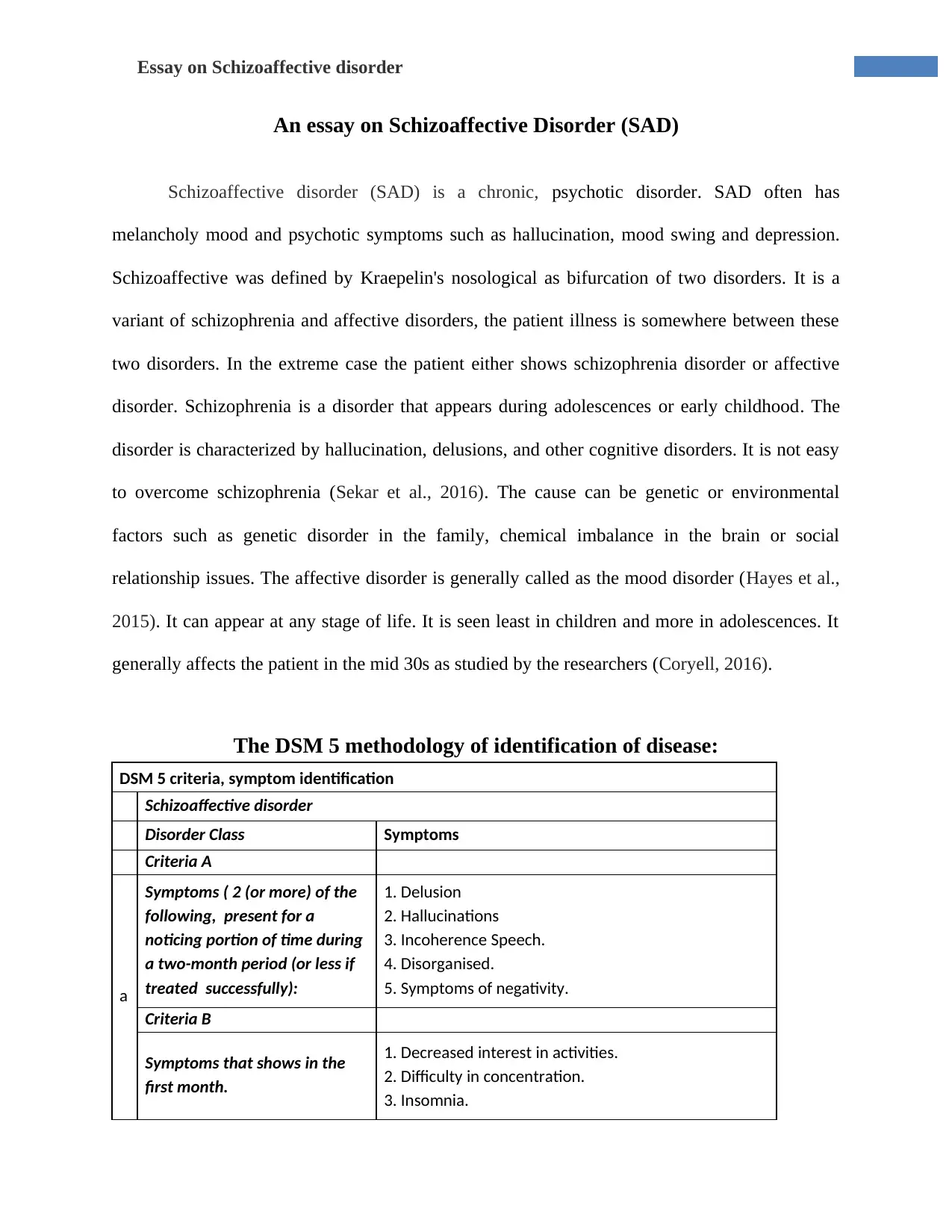
The DSM 5 methodology of identification of disease:
DSM 5 criteria, symptom identification
Schizoaffective disorder
Disorder Class Symptoms
Criteria A
a
Symptoms ( 2 (or more) of the
following, present for a
noticing portion of time during
a two-month period (or less if
treated successfully):
1. Delusion
2. Hallucinations
3. Incoherence Speech.
4. Disorganised.
5. Symptoms of negativity.
Criteria B
Symptoms that shows in the
first month.
1. Decreased interest in activities.
2. Difficulty in concentration.
3. Insomnia.
An essay on Schizoaffective Disorder (SAD)
Schizoaffective disorder (SAD) is a chronic, psychotic disorder. SAD often has
melancholy mood and psychotic symptoms such as hallucination, mood swing and depression.
Schizoaffective was defined by Kraepelin's nosological as bifurcation of two disorders. It is a
variant of schizophrenia and affective disorders, the patient illness is somewhere between these
two disorders. In the extreme case the patient either shows schizophrenia disorder or affective
disorder. Schizophrenia is a disorder that appears during adolescences or early childhood. The
disorder is characterized by hallucination, delusions, and other cognitive disorders. It is not easy
to overcome schizophrenia (Sekar et al., 2016). The cause can be genetic or environmental
factors such as genetic disorder in the family, chemical imbalance in the brain or social
relationship issues. The affective disorder is generally called as the mood disorder (Hayes et al.,
2015). It can appear at any stage of life. It is seen least in children and more in adolescences. It
generally affects the patient in the mid 30s as studied by the researchers (Coryell, 2016).
The DSM 5 methodology of identification of disease:
DSM 5 criteria, symptom identification
Schizoaffective disorder
Disorder Class Symptoms
Criteria A
a
Symptoms ( 2 (or more) of the
following, present for a
noticing portion of time during
a two-month period (or less if
treated successfully):
1. Delusion
2. Hallucinations
3. Incoherence Speech.
4. Disorganised.
5. Symptoms of negativity.
Criteria B
Symptoms that shows in the
first month.
1. Decreased interest in activities.
2. Difficulty in concentration.
3. Insomnia.
2Essay on Schizoaffective disorder
4. A sense of out of control.
5. Depressed, angry, feeling worthless (Health line,
2019).
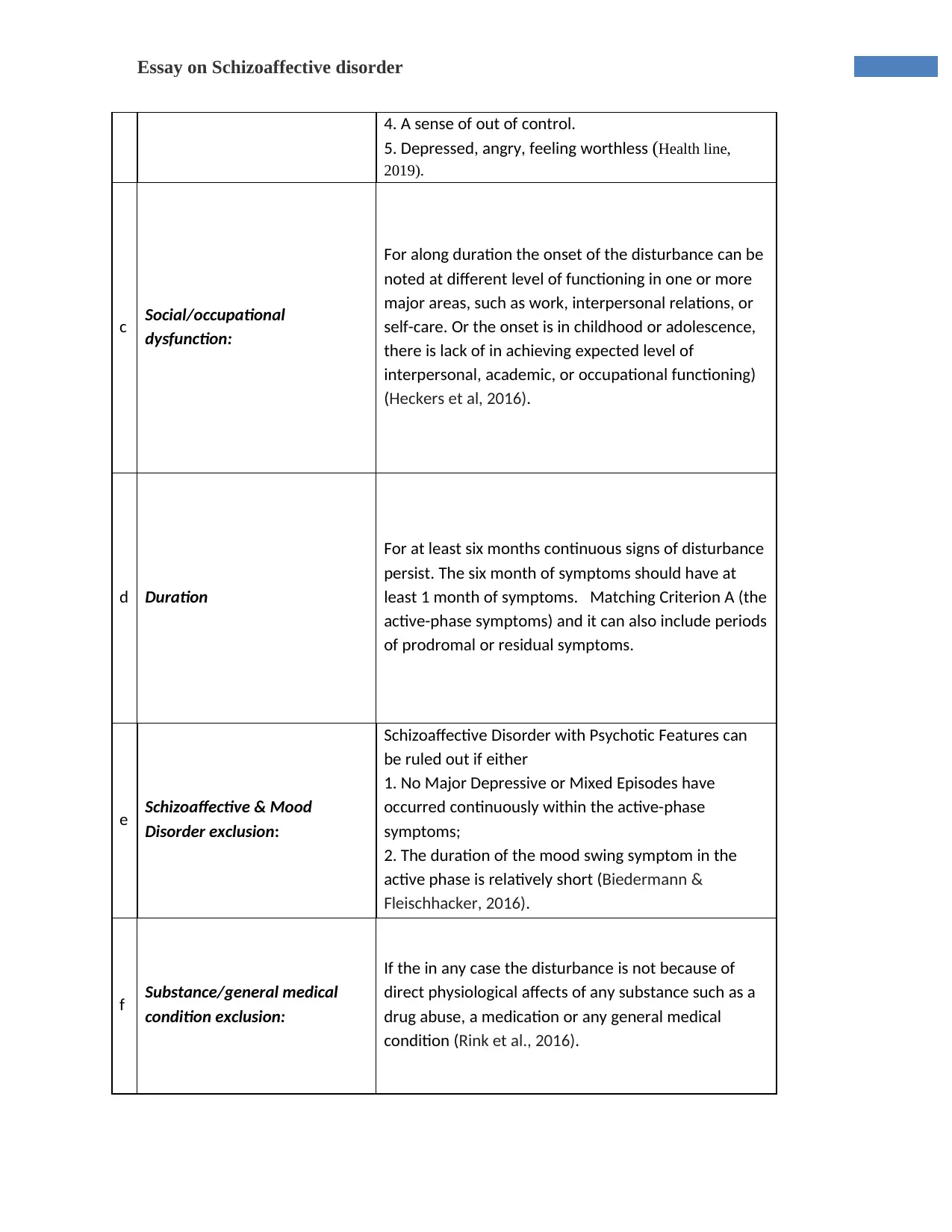
c Social/occupational
dysfunction:
For along duration the onset of the disturbance can be
noted at different level of functioning in one or more
major areas, such as work, interpersonal relations, or
self-care. Or the onset is in childhood or adolescence,
there is lack of in achieving expected level of
interpersonal, academic, or occupational functioning)
(Heckers et al, 2016).
d Duration
For at least six months continuous signs of disturbance
persist. The six month of symptoms should have at
least 1 month of symptoms. Matching Criterion A (the
active-phase symptoms) and it can also include periods
of prodromal or residual symptoms.
e Schizoaffective & Mood
Disorder exclusion:
Schizoaffective Disorder with Psychotic Features can
be ruled out if either
1. No Major Depressive or Mixed Episodes have
occurred continuously within the active-phase
symptoms;
2. The duration of the mood swing symptom in the
active phase is relatively short (Biedermann &
Fleischhacker, 2016).
f Substance/general medical
condition exclusion:
If the in any case the disturbance is not because of
direct physiological affects of any substance such as a
drug abuse, a medication or any general medical
condition (Rink et al., 2016).
4. A sense of out of control.
5. Depressed, angry, feeling worthless (Health line,
2019).
c Social/occupational
dysfunction:
For along duration the onset of the disturbance can be
noted at different level of functioning in one or more
major areas, such as work, interpersonal relations, or
self-care. Or the onset is in childhood or adolescence,
there is lack of in achieving expected level of
interpersonal, academic, or occupational functioning)
(Heckers et al, 2016).
d Duration
For at least six months continuous signs of disturbance
persist. The six month of symptoms should have at
least 1 month of symptoms. Matching Criterion A (the
active-phase symptoms) and it can also include periods
of prodromal or residual symptoms.
e Schizoaffective & Mood
Disorder exclusion:
Schizoaffective Disorder with Psychotic Features can
be ruled out if either
1. No Major Depressive or Mixed Episodes have
occurred continuously within the active-phase
symptoms;
2. The duration of the mood swing symptom in the
active phase is relatively short (Biedermann &
Fleischhacker, 2016).
f Substance/general medical
condition exclusion:
If the in any case the disturbance is not because of
direct physiological affects of any substance such as a
drug abuse, a medication or any general medical
condition (Rink et al., 2016).
3Essay on Schizoaffective disorder
The above chart is based on DSM V method of analyzing the symptoms. It comprises of
the identification of the disease through better examination.
The demographic information based on Australia.
The psychotic illness is prevalent in most of the areas of Australia. A national survey is
done yearly to know the change in number of the affected patients. The national survey of
Mental Health and Well being 2017 of adult provides information on year prevalence of the
mental disorder in the Australian population (Goghari & Harrow, 2019).
The survey was done on the population age between16-85. It was estimated by the
studies that at least 45% of the population will suffer from mental disorder at any point in this
age. It has been found out that 1 in 5 had experienced a common mental disorder in last one year
which is around 4.9 million populations in 2017. The anxiety disorder was much prevalent than
the schizophrenia disorder. If the data is to be analyzed than it is found that 14.5% from anxiety
disorder, 6.2% of the population was suffering from Affective disorder, 5.1% from substance use
disorder, 3.% from schizoaffective disorder. It is a fact the most common disorder that is found
in the Australian population is the Schizophrenia recording to 47% of the population (Australian
Institute of Health and Welfare, 2017).
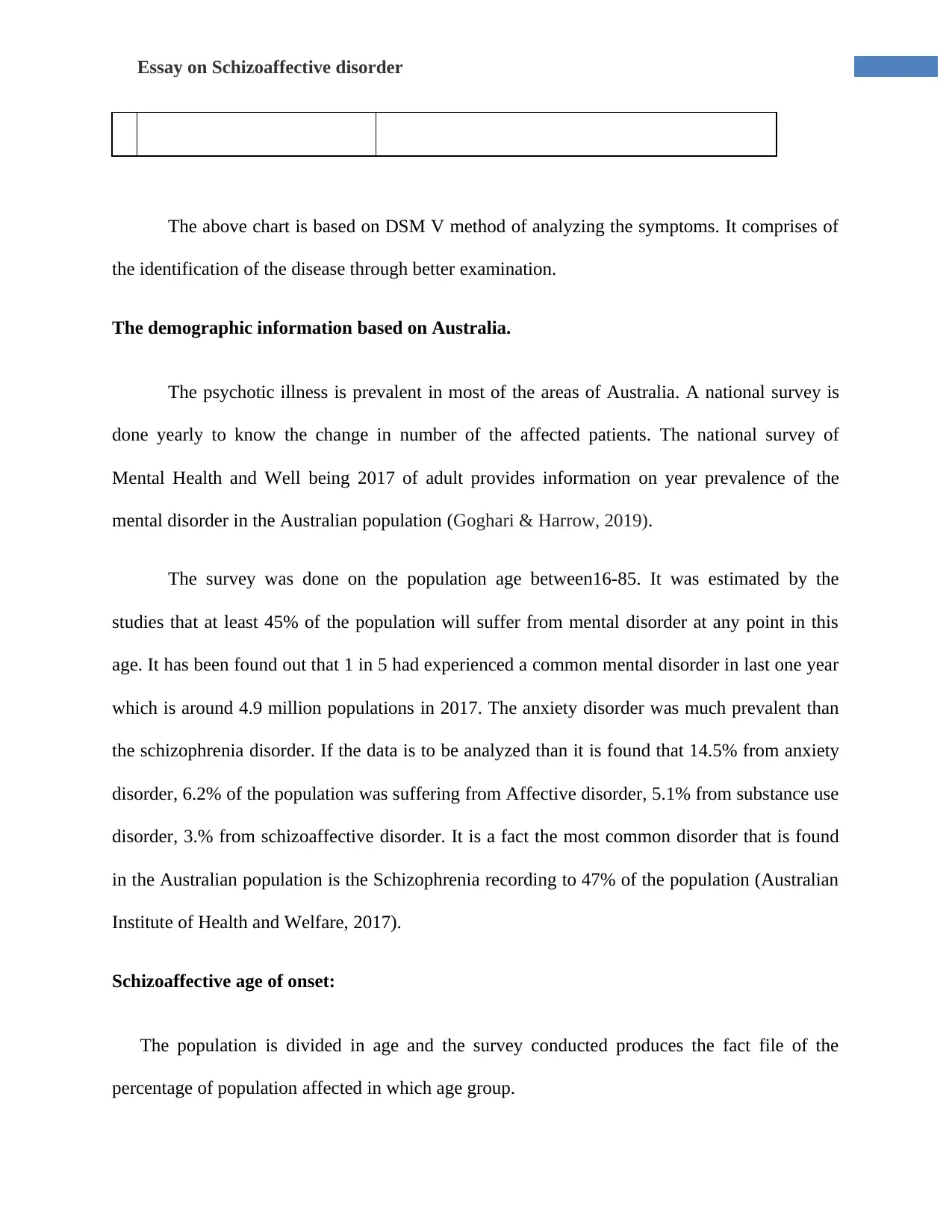
Schizoaffective age of onset:
The population is divided in age and the survey conducted produces the fact file of the
percentage of population affected in which age group.
The above chart is based on DSM V method of analyzing the symptoms. It comprises of
the identification of the disease through better examination.
The demographic information based on Australia.
The psychotic illness is prevalent in most of the areas of Australia. A national survey is
done yearly to know the change in number of the affected patients. The national survey of
Mental Health and Well being 2017 of adult provides information on year prevalence of the
mental disorder in the Australian population (Goghari & Harrow, 2019).
The survey was done on the population age between16-85. It was estimated by the
studies that at least 45% of the population will suffer from mental disorder at any point in this
age. It has been found out that 1 in 5 had experienced a common mental disorder in last one year
which is around 4.9 million populations in 2017. The anxiety disorder was much prevalent than
the schizophrenia disorder. If the data is to be analyzed than it is found that 14.5% from anxiety
disorder, 6.2% of the population was suffering from Affective disorder, 5.1% from substance use
disorder, 3.% from schizoaffective disorder. It is a fact the most common disorder that is found
in the Australian population is the Schizophrenia recording to 47% of the population (Australian
Institute of Health and Welfare, 2017).
Schizoaffective age of onset:
The population is divided in age and the survey conducted produces the fact file of the
percentage of population affected in which age group.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4Essay on Schizoaffective disorder
Almost 64.9%of the population experienced their first episode even before the age of 25
years.
The male percentage affect was 34.3% and female to be 40.1% on or at 25 years.
It was found that 32.1% of people the disorder onset was gradual, taking one month to six
months time, and 45% developed it in the course of six month (Australian Institute of
Health and Welfare, 2017).
Graph 1. The case registered and treated for Schizoaffective disorder (Australia, 2017).
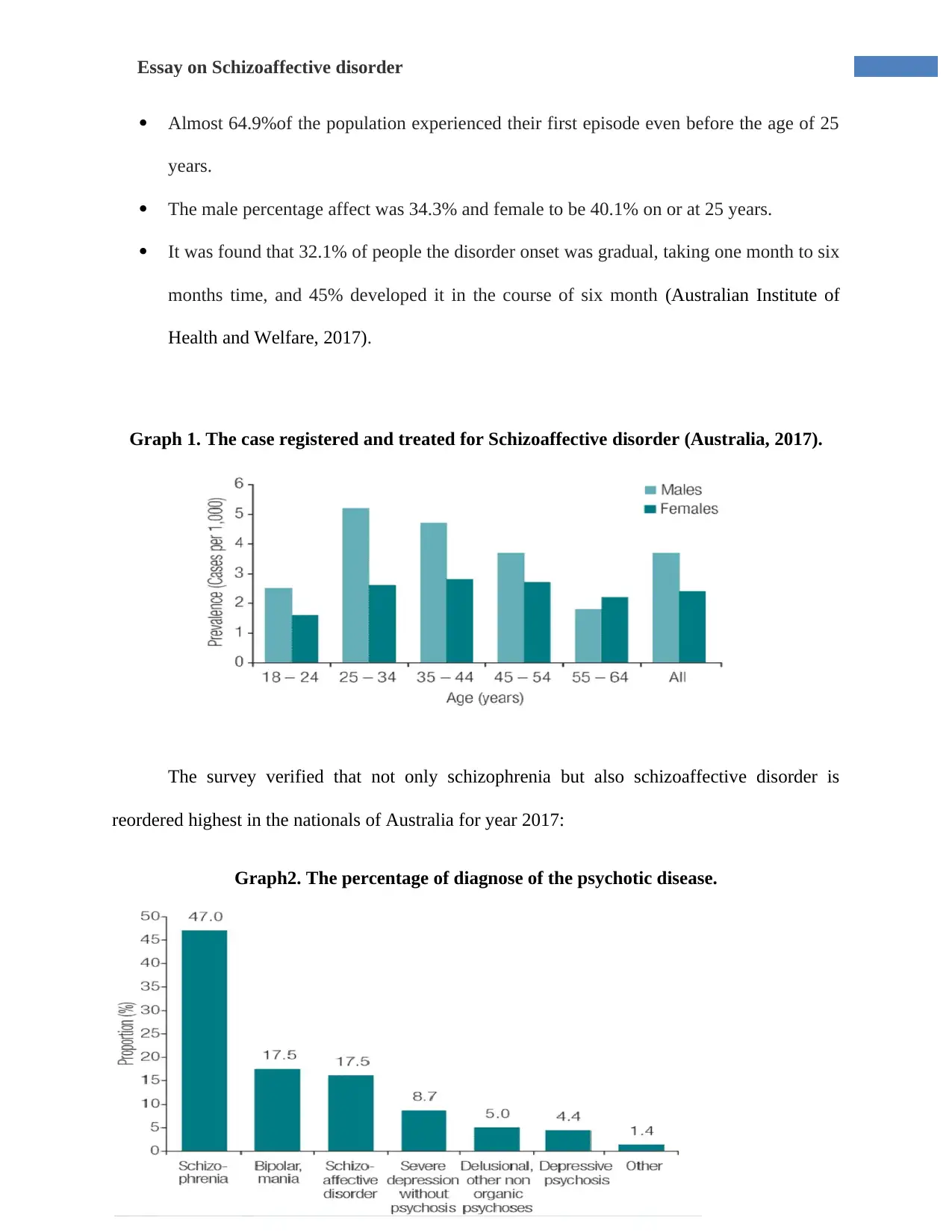
The survey verified that not only schizophrenia but also schizoaffective disorder is
reordered highest in the nationals of Australia for year 2017:
Graph2. The percentage of diagnose of the psychotic disease.
Almost 64.9%of the population experienced their first episode even before the age of 25
years.
The male percentage affect was 34.3% and female to be 40.1% on or at 25 years.
It was found that 32.1% of people the disorder onset was gradual, taking one month to six
months time, and 45% developed it in the course of six month (Australian Institute of
Health and Welfare, 2017).
Graph 1. The case registered and treated for Schizoaffective disorder (Australia, 2017).
The survey verified that not only schizophrenia but also schizoaffective disorder is
reordered highest in the nationals of Australia for year 2017:
Graph2. The percentage of diagnose of the psychotic disease.
5Essay on Schizoaffective disorder
Mental disorder mainly varies in severity and can also be episodic and persistent in
nature. The mental and substance use disorder can be found to be responsible for 14.2% of the
total disease making it 3rd broad disease group after cancer and cardiovascular diseases (AIHW
2017).
The exploration of the prodromal phase :
The first phase is called the prodromal phase. The beginning phase in which the person
starts to experience the changes in themselves but not experiencing the full stretched psychotic
symptoms.
Schizoaffective is both a neurodevelopment and neurodegenerative disorder due to
abnormal brain development in the fetus or in adolescence (Dykxhoorn et al., 2018). As the brain
starts to mature with age the symptoms are visible, either it is hereditary or has suffered at early
stage of life. Psychotic disorders have origins in early age development but it is generally
manifested in latter adolescence as a result of the developmental inclination of the brain. As per
the Kraepelin’s observations, it has been noted that a longer duration of illness, also termed as
duration of untreated psychosis (DUP), is associated with functional disabilities and persistent
symptoms. The prodromal symptoms shows a predict symptoms. The distinction between the
negative and positive symptoms described by Strauss and Carpenter as the term to be extensively
researched in the modern psychology dimensions. There are three symptom dimensions: the
negative dimension, the positive dimension which was divided into- one including delusions and
the other including hallucinations, and third one a factor including bizarre behavior and thought
disorder (Gardner & Nasrallah, 2015).
Mental disorder mainly varies in severity and can also be episodic and persistent in
nature. The mental and substance use disorder can be found to be responsible for 14.2% of the
total disease making it 3rd broad disease group after cancer and cardiovascular diseases (AIHW
2017).
The exploration of the prodromal phase :
The first phase is called the prodromal phase. The beginning phase in which the person
starts to experience the changes in themselves but not experiencing the full stretched psychotic
symptoms.
Schizoaffective is both a neurodevelopment and neurodegenerative disorder due to
abnormal brain development in the fetus or in adolescence (Dykxhoorn et al., 2018). As the brain
starts to mature with age the symptoms are visible, either it is hereditary or has suffered at early
stage of life. Psychotic disorders have origins in early age development but it is generally
manifested in latter adolescence as a result of the developmental inclination of the brain. As per
the Kraepelin’s observations, it has been noted that a longer duration of illness, also termed as
duration of untreated psychosis (DUP), is associated with functional disabilities and persistent
symptoms. The prodromal symptoms shows a predict symptoms. The distinction between the
negative and positive symptoms described by Strauss and Carpenter as the term to be extensively
researched in the modern psychology dimensions. There are three symptom dimensions: the
negative dimension, the positive dimension which was divided into- one including delusions and
the other including hallucinations, and third one a factor including bizarre behavior and thought
disorder (Gardner & Nasrallah, 2015).
6Essay on Schizoaffective disorder
Initial symptoms include: hearing voices discussing about oneself; audible thoughts (able
to hear one’s own thoughts spoken aloud); delusional personalized interpretation; experiencing
one’s impulses, emotions or motor activity as being controlled by an external force, depression ,
anxiety, and sleep disturbances . it is also accompanied by the clinical presentation of psychotic
disorders. Patients are commonly experience difficulty in social and functional deficits like less
social contact, and maintaining employment & challenges to independent living that significantly
impact their quality of life (Martino, 2015).
The impact of mental disease:
Factors that generally affects the mental health of a person specially in childhood or
adolescence;
Self esteem It is the positive self-image & sense of self-worth in one self. People with high self
esteem tries to be satisfied with them self. Thus hurting the self esteem to an extent that it is not
recoverable is a major reason for psychotic illness (Jagsch et al., 2018).
Loved by surrounding: Children who are ignored, distrusted or hated are most likely to develop
the illness. Sometimes the society also plays a very important role in grooming the person. The
effect is highly impactful on the adolescence mind. That disturbs the person to an extent that
slowly they start to develop the psychotic illness.
Difficult behavior: people with bad past or disturbing adolescence develop behavior where they
try to harm themselves and the surroundings. They starts to develop wrong and distressing
behavior like using abusive language, acting violently, stealing, lying, refusing to follow rule in
school or home.
Initial symptoms include: hearing voices discussing about oneself; audible thoughts (able
to hear one’s own thoughts spoken aloud); delusional personalized interpretation; experiencing
one’s impulses, emotions or motor activity as being controlled by an external force, depression ,
anxiety, and sleep disturbances . it is also accompanied by the clinical presentation of psychotic
disorders. Patients are commonly experience difficulty in social and functional deficits like less
social contact, and maintaining employment & challenges to independent living that significantly
impact their quality of life (Martino, 2015).
The impact of mental disease:
Factors that generally affects the mental health of a person specially in childhood or
adolescence;
Self esteem It is the positive self-image & sense of self-worth in one self. People with high self
esteem tries to be satisfied with them self. Thus hurting the self esteem to an extent that it is not
recoverable is a major reason for psychotic illness (Jagsch et al., 2018).
Loved by surrounding: Children who are ignored, distrusted or hated are most likely to develop
the illness. Sometimes the society also plays a very important role in grooming the person. The
effect is highly impactful on the adolescence mind. That disturbs the person to an extent that
slowly they start to develop the psychotic illness.
Difficult behavior: people with bad past or disturbing adolescence develop behavior where they
try to harm themselves and the surroundings. They starts to develop wrong and distressing
behavior like using abusive language, acting violently, stealing, lying, refusing to follow rule in
school or home.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7Essay on Schizoaffective disorder
Physical ill health- Sometimes the poor health, long time illness or injuries can lead to mental
illness. Physical illness like birth trauma, brain injury or drug abuse affects the brain chemistry
and contributes to mental illness. A bad stature or bad physical health can affect the ability of the
people lead a happy life. Which ultimately leads to the metal depression.
Abuse- The child brain development comes to a risky point when they are abused by anyone.
The abuse can be physical, sexual , psychological or verbal and these abuses are not tolerable
(Chouinard et al., 2016).
The impact on the kids or adolescences who are diagnosed with mental illness faces a lot
of societal stigma. They go through depression which lets them down and kills their creativity.
The matter is how someone feels and thinks about them. This impacts their happiness and
physical activity. They avoid interaction with their surrounding, they find peace in closed
compounds. They keep stressed out due to diagnose. They are targeted by the crowd for being
different. They face the wrath of the society by being ignored, talked about and made fun of.
These are the major drawbacks of being diagnosed by mental illness. The person as an
adolescent has very low maturity to understand the benefit of being treated. The treatment is as
important as life itself. The diagnoses in the right time help save lives of young people and
bringing them back to a normal state. By supporting young people and letting them to open up is
the best thing to do for them.
Treatment-
The treatment of Psychotic illness is both therapy as well as medication. The medication
is very important to keep the chemical balance of the brain. The therapy helps the person to come
Physical ill health- Sometimes the poor health, long time illness or injuries can lead to mental
illness. Physical illness like birth trauma, brain injury or drug abuse affects the brain chemistry
and contributes to mental illness. A bad stature or bad physical health can affect the ability of the
people lead a happy life. Which ultimately leads to the metal depression.
Abuse- The child brain development comes to a risky point when they are abused by anyone.
The abuse can be physical, sexual , psychological or verbal and these abuses are not tolerable
(Chouinard et al., 2016).
The impact on the kids or adolescences who are diagnosed with mental illness faces a lot
of societal stigma. They go through depression which lets them down and kills their creativity.
The matter is how someone feels and thinks about them. This impacts their happiness and
physical activity. They avoid interaction with their surrounding, they find peace in closed
compounds. They keep stressed out due to diagnose. They are targeted by the crowd for being
different. They face the wrath of the society by being ignored, talked about and made fun of.
These are the major drawbacks of being diagnosed by mental illness. The person as an
adolescent has very low maturity to understand the benefit of being treated. The treatment is as
important as life itself. The diagnoses in the right time help save lives of young people and
bringing them back to a normal state. By supporting young people and letting them to open up is
the best thing to do for them.
Treatment-
The treatment of Psychotic illness is both therapy as well as medication. The medication
is very important to keep the chemical balance of the brain. The therapy helps the person to come
8Essay on Schizoaffective disorder
out of the depression and stigma step by step. There are trained Psychiatric doctors that keep the
procedure easy to be followed by the patients (Chue & Chue, 2016). The therapy involves:
Being healthy-They patient is encouraged to eat healthy food, do physical exercise and keep self
active.
Involve in activity- they are asked to involve in constructive activities that makes them feel
happy. They are made to do activities in groups to boost the confidence.
Care taking (Family care method)- its important to make them feel loved. They are cared and
loved by the instructor and the doctors. They are given attention.
Involving in activities of well being- they are involved in activities that is a part of doing well
being to others. That creates a kindness in the patient which increases the emotional intelligence.
Talking to them- the most important factor is to talk to them. Listen what they want to say.
They might not speak every time but they are encouraged to express what they feel or what they
want to say.
The medication is important as they regulate the chemical reaction in the brain and
controls the hormones that trigger the illness. Its used to regulate the emotions and thought
process of the patient. The medication is Antipsychotics Food and Drug Administration and
Antidepressants (Lally, Tully & MacCabe, 2016).
Issues with family and care giver when supporting a teen with SAD.
The problem is very common the patient will not accept that he or she is depressed so to
make them realize is wrong and generally a care giver or parent do this in the first step of
out of the depression and stigma step by step. There are trained Psychiatric doctors that keep the
procedure easy to be followed by the patients (Chue & Chue, 2016). The therapy involves:
Being healthy-They patient is encouraged to eat healthy food, do physical exercise and keep self
active.
Involve in activity- they are asked to involve in constructive activities that makes them feel
happy. They are made to do activities in groups to boost the confidence.
Care taking (Family care method)- its important to make them feel loved. They are cared and
loved by the instructor and the doctors. They are given attention.
Involving in activities of well being- they are involved in activities that is a part of doing well
being to others. That creates a kindness in the patient which increases the emotional intelligence.
Talking to them- the most important factor is to talk to them. Listen what they want to say.
They might not speak every time but they are encouraged to express what they feel or what they
want to say.
The medication is important as they regulate the chemical reaction in the brain and
controls the hormones that trigger the illness. Its used to regulate the emotions and thought
process of the patient. The medication is Antipsychotics Food and Drug Administration and
Antidepressants (Lally, Tully & MacCabe, 2016).
Issues with family and care giver when supporting a teen with SAD.
The problem is very common the patient will not accept that he or she is depressed so to
make them realize is wrong and generally a care giver or parent do this in the first step of
9Essay on Schizoaffective disorder
therapy. Thus the problem starts from her the patient will not accept the advice, medication or
therapy easily may be fussy and avoid to open up. The teen wants to make judgment or wants to
pass comments which may be uncomfortable for the listener. Thus its important that the care
giver lets the teen talk. There are chances that the person stops trying in the being if they are met
with resistance. Its important that they be respectful to what the teen or the kid wants to say or
express. Sometimes the concern seems to be too silly or imaginary. Its important they show
concern to the teen and listen to them. And accept their emotions seriously (Alphs, Fu & Turkoz,
2016).
Overview of the roles within a multidisciplinary team
Multidimensional treatment plan is based on defining both the problems and the
objectives to be achieved. Many functions of the team is related to the course and prognosis of
Sad. In the beginning of the evaluation it is very important to identify the list the problems,
multiaxial diagnosis, and determine the module of treatment. Next comes the evaluation of rate
of progress and the level of involvement and degree of therapeutic engagement possible between
patient and team. This determines the efficacy of the proposed intervention. The
multidisciplinary team plays lots of important roles, like providing education about the disease,
managing co morbidities, and encouraging positive lifestyle for patients. They also evaluate the
social support model given to patient. Patient are given options, such as hospitals, group therapy,
and individual follow-up treatment. It makes the treatment easy and successful in the presence of
the multi disciplinary team (Puntis et al., 2019).
therapy. Thus the problem starts from her the patient will not accept the advice, medication or
therapy easily may be fussy and avoid to open up. The teen wants to make judgment or wants to
pass comments which may be uncomfortable for the listener. Thus its important that the care
giver lets the teen talk. There are chances that the person stops trying in the being if they are met
with resistance. Its important that they be respectful to what the teen or the kid wants to say or
express. Sometimes the concern seems to be too silly or imaginary. Its important they show
concern to the teen and listen to them. And accept their emotions seriously (Alphs, Fu & Turkoz,
2016).
Overview of the roles within a multidisciplinary team
Multidimensional treatment plan is based on defining both the problems and the
objectives to be achieved. Many functions of the team is related to the course and prognosis of
Sad. In the beginning of the evaluation it is very important to identify the list the problems,
multiaxial diagnosis, and determine the module of treatment. Next comes the evaluation of rate
of progress and the level of involvement and degree of therapeutic engagement possible between
patient and team. This determines the efficacy of the proposed intervention. The
multidisciplinary team plays lots of important roles, like providing education about the disease,
managing co morbidities, and encouraging positive lifestyle for patients. They also evaluate the
social support model given to patient. Patient are given options, such as hospitals, group therapy,
and individual follow-up treatment. It makes the treatment easy and successful in the presence of
the multi disciplinary team (Puntis et al., 2019).
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
10Essay on Schizoaffective disorder
Conclusion
Thus it can be concluded that from the onset to the cure it is the major responsibility of
the doctor, family, friends and society to work together to cure the Psychotic illness in patient.
The major role is played by the councilor who makes the patient open up and speak about their
feeling and state of mind. It takes lots of time for the patient to recover and join back the normal
life style. It is said that prevention is better than cure the problem should be tracked before it
becomes a stigma.
Conclusion
Thus it can be concluded that from the onset to the cure it is the major responsibility of
the doctor, family, friends and society to work together to cure the Psychotic illness in patient.
The major role is played by the councilor who makes the patient open up and speak about their
feeling and state of mind. It takes lots of time for the patient to recover and join back the normal
life style. It is said that prevention is better than cure the problem should be tracked before it
becomes a stigma.
11Essay on Schizoaffective disorder
References;
Alphs, L., Fu, D. J., & Turkoz, I. (2016). Paliperidone for the treatment of schizoaffective
disorder. Expert opinion on pharmacotherapy, 17(6), 871-883.
Australian Institute of Health and Welfare. (2017). Mental health services in Australia,
Prevalence and policies - Australian Institute of Health and Welfare. Retrieved from
https://www.aihw.gov.au/reports/mental-health-services/mental-health-services-in-
australia/report-contents/summary/prevalence-and-policies
Biedermann, F., & Fleischhacker, W. W. (2016). Psychotic disorders in DSM-5 and ICD-
11. CNS spectrums, 21(4), 349-354.
Chouinard, V. A., Pingali, S. M., Chouinard, G., Henderson, D. C., Mallya, S. G., Cypess, A. M.,
... & Öngür, D. (2016). Factors associated with overweight and obesity in schizophrenia,
schizoaffective and bipolar disorders. Psychiatry research, 237, 304-310.
Chue, P., & Chue, J. (2016). A critical appraisal of paliperidone long-acting injection in the
treatment of schizoaffective disorder. Therapeutics and clinical risk management, 12,
109.
Coryell, W. (2016). Schizoaffective and schizophreniform disorders. In The medical basis of
psychiatry (pp. 121-135). Springer, New York, NY.
Dykxhoorn, J., Hollander, A. C., Lewis, G., Magnusson, C., Dalman, C., & Kirkbride, J. B.
(2018). Risk of schizophrenia, schizoaffective, and bipolar disorders by migrant status,
region of origin, and age-at-migration: a national cohort study of 1.8 million
people. Psychological medicine, 1-10.
Gardner, K. N., & Nasrallah, H. A. (2015). Managing first-episode psychosis: an early stage of
schizophrenia with distinct treatment needs: minimize duration of untreated psychosis;
aim for remission. Current Psychiatry, 14(5), 32-41.
Goghari, V. M., & Harrow, M. (2019). Anxiety Symptoms across Twenty Years in
Schizoaffective Disorder, Bipolar Disorder, and Major Depressive Disorder. Psychiatry
Research.
Hayes, J. F., Miles, J., Walters, K., King, M., & Osborn, D. P. J. (2015). A systematic review and
meta‐analysis of premature mortality in bipolar affective disorder. Acta Psychiatrica
Scandinavica, 131(6), 417-425.
Healthline. (2019). Affective Disorders: Types, Symptoms, and Treatments. Retrieved from
https://www.healthline.com/health/affective-disorders
References;
Alphs, L., Fu, D. J., & Turkoz, I. (2016). Paliperidone for the treatment of schizoaffective
disorder. Expert opinion on pharmacotherapy, 17(6), 871-883.
Australian Institute of Health and Welfare. (2017). Mental health services in Australia,
Prevalence and policies - Australian Institute of Health and Welfare. Retrieved from
https://www.aihw.gov.au/reports/mental-health-services/mental-health-services-in-
australia/report-contents/summary/prevalence-and-policies
Biedermann, F., & Fleischhacker, W. W. (2016). Psychotic disorders in DSM-5 and ICD-
11. CNS spectrums, 21(4), 349-354.
Chouinard, V. A., Pingali, S. M., Chouinard, G., Henderson, D. C., Mallya, S. G., Cypess, A. M.,
... & Öngür, D. (2016). Factors associated with overweight and obesity in schizophrenia,
schizoaffective and bipolar disorders. Psychiatry research, 237, 304-310.
Chue, P., & Chue, J. (2016). A critical appraisal of paliperidone long-acting injection in the
treatment of schizoaffective disorder. Therapeutics and clinical risk management, 12,
109.
Coryell, W. (2016). Schizoaffective and schizophreniform disorders. In The medical basis of
psychiatry (pp. 121-135). Springer, New York, NY.
Dykxhoorn, J., Hollander, A. C., Lewis, G., Magnusson, C., Dalman, C., & Kirkbride, J. B.
(2018). Risk of schizophrenia, schizoaffective, and bipolar disorders by migrant status,
region of origin, and age-at-migration: a national cohort study of 1.8 million
people. Psychological medicine, 1-10.
Gardner, K. N., & Nasrallah, H. A. (2015). Managing first-episode psychosis: an early stage of
schizophrenia with distinct treatment needs: minimize duration of untreated psychosis;
aim for remission. Current Psychiatry, 14(5), 32-41.
Goghari, V. M., & Harrow, M. (2019). Anxiety Symptoms across Twenty Years in
Schizoaffective Disorder, Bipolar Disorder, and Major Depressive Disorder. Psychiatry
Research.
Hayes, J. F., Miles, J., Walters, K., King, M., & Osborn, D. P. J. (2015). A systematic review and
meta‐analysis of premature mortality in bipolar affective disorder. Acta Psychiatrica
Scandinavica, 131(6), 417-425.
Healthline. (2019). Affective Disorders: Types, Symptoms, and Treatments. Retrieved from
https://www.healthline.com/health/affective-disorders
12Essay on Schizoaffective disorder
Heckers, S., Barch, D. M., Bustillo, J., Gaebel, W., Gur, R., Malaspina, D., ... & Van Os, J.
(2016). Structure of the Psychotic Disorders Classification in DSM-5. Focus, 14(3), 366-
369.
Jagsch, C., Dietmaier, G., Jagsch, M., & Roller, R. E. (2018). Schizophrenia spectrum disorders
in elderly patients: Analysis of reasons for admission to a department of geriatric
psychiatry. Zeitschrift fur Gerontologie und Geriatrie, 51(2), 206-212.
Lally, J., Tully, J., & MacCabe, J. H. (2016). Clozapine augmentation for treatment‐resistant
schizoaffective disorder. Cochrane Database of Systematic Reviews, (3).
Martino, D. J., Samamé, C., Ibañez, A., & Strejilevich, S. A. (2015). Neurocognitive functioning
in the premorbid stage and in the first episode of bipolar disorder: a systematic
review. Psychiatry research, 226(1), 23-30.
Puntis, S., Minichino, A., De Crescenzo, F., Cipriani, A., & Lennox, B. (2019). Specialised early
intervention teams (extended time) for first episode psychosis. Cochrane Database of
Systematic Reviews, (3).
Rink, L., Pagel, T., Franklin, J., & Baethge, C. (2016). Characteristics and heterogeneity of
schizoaffective disorder compared with unipolar depression and schizophrenia–A
systematic literature review and meta-analysis. Journal of affective disorders, 191, 8-14.
Sekar, A., Bialas, A. R., de Rivera, H., Davis, A., Hammond, T. R., Kamitaki, N., ... &
Genovese, G. (2016). Schizophrenia risk from complex variation of complement
component 4. Nature, 530(7589), 177.
Heckers, S., Barch, D. M., Bustillo, J., Gaebel, W., Gur, R., Malaspina, D., ... & Van Os, J.
(2016). Structure of the Psychotic Disorders Classification in DSM-5. Focus, 14(3), 366-
369.
Jagsch, C., Dietmaier, G., Jagsch, M., & Roller, R. E. (2018). Schizophrenia spectrum disorders
in elderly patients: Analysis of reasons for admission to a department of geriatric
psychiatry. Zeitschrift fur Gerontologie und Geriatrie, 51(2), 206-212.
Lally, J., Tully, J., & MacCabe, J. H. (2016). Clozapine augmentation for treatment‐resistant
schizoaffective disorder. Cochrane Database of Systematic Reviews, (3).
Martino, D. J., Samamé, C., Ibañez, A., & Strejilevich, S. A. (2015). Neurocognitive functioning
in the premorbid stage and in the first episode of bipolar disorder: a systematic
review. Psychiatry research, 226(1), 23-30.
Puntis, S., Minichino, A., De Crescenzo, F., Cipriani, A., & Lennox, B. (2019). Specialised early
intervention teams (extended time) for first episode psychosis. Cochrane Database of
Systematic Reviews, (3).
Rink, L., Pagel, T., Franklin, J., & Baethge, C. (2016). Characteristics and heterogeneity of
schizoaffective disorder compared with unipolar depression and schizophrenia–A
systematic literature review and meta-analysis. Journal of affective disorders, 191, 8-14.
Sekar, A., Bialas, A. R., de Rivera, H., Davis, A., Hammond, T. R., Kamitaki, N., ... &
Genovese, G. (2016). Schizophrenia risk from complex variation of complement
component 4. Nature, 530(7589), 177.
1 out of 13
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





