NRS312: Critique of a Deteriorating Patient Scenario in Nursing Care
VerifiedAdded on 2022/08/31
|13
|3952
|52
Report
AI Summary
This report critically examines a nursing scenario involving Mrs. Sally Brown, a 73-year-old patient admitted for a total hip replacement who subsequently experiences an acute ischaemic stroke. The assignment, for the NRS312 Essential Nursing Care module, requires a critique of the recognition, escalation, and management of her deteriorating condition. It encompasses a description of the Clinical Emergency Response System (CERS), including Clinical Review and Rapid Response levels. The report analyzes the nurses' actions, focusing on the assessment of vital signs (respiratory rate, blood pressure, pulse, pain, consciousness level, and urine output), and the implementation of the ABCDE approach. The report emphasizes the importance of early detection, timely intervention, and effective communication within the multidisciplinary team to ensure patient safety and improve outcomes. The clinical reasoning cycle and ISBAR handover are also discussed within the context of this patient scenario.
Student Name: Enter your name
Student Number: Enter your number
Subject Code: NRS312
Subject Name: Essential Nursing Care: Managing the deteriorating patient
Subject Lecturer: Enter your lecturer
Assessment item: 3
Assessment title: Deteriorating Patient Scenario Critique
Due date: 09/04/20
Date of submission: Enter the date you are submitting your assignment to EASTS
Word count (excluding in text citations, reference list and appendices): Highlight the text in
the body of your paper, copy to a new document, remove citations and check the word count
1
Student Name: (enter your name) Student Number: (enter your number) NRS312 Assessment Item 3
Student Number: Enter your number
Subject Code: NRS312
Subject Name: Essential Nursing Care: Managing the deteriorating patient
Subject Lecturer: Enter your lecturer
Assessment item: 3
Assessment title: Deteriorating Patient Scenario Critique
Due date: 09/04/20
Date of submission: Enter the date you are submitting your assignment to EASTS
Word count (excluding in text citations, reference list and appendices): Highlight the text in
the body of your paper, copy to a new document, remove citations and check the word count
1
Student Name: (enter your name) Student Number: (enter your number) NRS312 Assessment Item 3
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Introduction
After a patient gets admitted to a hospital, it is expected that the nurses and hospital staff will
take proper care of the patient and ensure the safety and security of the patient and also
provide them with the best healthcare service. Even if the condition of the patient
deteriorates, the nurses will take the appropriate preventive measures to resolve it and prevent
the situation from worsening any further and manage it effectively(Bucknall et al, 2016).
However, this is always not the case; sometimes, the nurses fail to assess the patient’s
condition and cannot detect the early signs of deterioration, which leads to further health
complexities within a patient. Recognizing and responding to deteriorating patients is a
matter of great concern. So there is an urgent need for a solution to this problem or a strategy
that will assist the nurses in managing and interpreting the early signs of deterioration in a
patient(Cho et al, 2020). This paper focusses on the case of Sally Brown who was admitted to
the hospital for an elective Total Hip Replacement. This paper focusses on the process
through which the nurses recognized the early signs of deterioration of Mrs. Brown and
provided her with the necessary treatment and care for preventing the further worsening of
her condition.
Question 1: Recognise
a) The Clinical Emergency Response System, also known as CERS, is a facility that is
implemented in every healthcare organization for assisting the nurses in responding to
early detection of the signs of deterioration. The CERS consists of two levels namely
‘Clinical Review’ for the Yellow Zone criteria and ‘Rapid Response’ for Red Zone
criteria. The process of Clinical Review asks the nurse to respond within 30 minutes
whenever there is a breach in the clinical review criteria. The Rapid Response process
helps in providing immediate assistance in response to the breach in the Rapid
2
Student Name: (enter your name) Student Number: (enter your number) NRS312 Assessment Item 3
After a patient gets admitted to a hospital, it is expected that the nurses and hospital staff will
take proper care of the patient and ensure the safety and security of the patient and also
provide them with the best healthcare service. Even if the condition of the patient
deteriorates, the nurses will take the appropriate preventive measures to resolve it and prevent
the situation from worsening any further and manage it effectively(Bucknall et al, 2016).
However, this is always not the case; sometimes, the nurses fail to assess the patient’s
condition and cannot detect the early signs of deterioration, which leads to further health
complexities within a patient. Recognizing and responding to deteriorating patients is a
matter of great concern. So there is an urgent need for a solution to this problem or a strategy
that will assist the nurses in managing and interpreting the early signs of deterioration in a
patient(Cho et al, 2020). This paper focusses on the case of Sally Brown who was admitted to
the hospital for an elective Total Hip Replacement. This paper focusses on the process
through which the nurses recognized the early signs of deterioration of Mrs. Brown and
provided her with the necessary treatment and care for preventing the further worsening of
her condition.
Question 1: Recognise
a) The Clinical Emergency Response System, also known as CERS, is a facility that is
implemented in every healthcare organization for assisting the nurses in responding to
early detection of the signs of deterioration. The CERS consists of two levels namely
‘Clinical Review’ for the Yellow Zone criteria and ‘Rapid Response’ for Red Zone
criteria. The process of Clinical Review asks the nurse to respond within 30 minutes
whenever there is a breach in the clinical review criteria. The Rapid Response process
helps in providing immediate assistance in response to the breach in the Rapid
2
Student Name: (enter your name) Student Number: (enter your number) NRS312 Assessment Item 3
response criteria. When a patient shows signs of clinical deterioration, the
multidisciplinary team including the nurse and other healthcare personnel assess the
condition of the patient and looks after him under strict observation to ensure well-
being of the patient.
b) The recognition of the clinical deterioration in Mrs Brown’s case, which the nurses
should have noticed are the following:
Respiratory rate: It is the most critical and important sign of deterioration in a patient, an
increase of even 3-4 breaths from the normal rate can indicate respiratory distress among
patients and hypoxemia or it can act as a marker of acidosis.
Blood Pressure: It is the pressure exerted by the blood against the walls of the atria, it is an
important and crucial sign to measure as it detects the flow of blood during systole and
diastole movement of the heart, thus indicating the delivery of oxygen throughout the body.
A sudden drop in the blood pressure reading s indicates cardiac arrest(Massey, Chaboyer &
Anderson, 2017).
Pulse rate: The pulse is a palpable and rhythmic expansion of the artery caused by increased
flow of blood into the vessels due to contraction and relaxation of the heart. The pulse can be
affected by age, fluid status and medications. The regularity, strength and equality in the
pulse beat should also be assessed.
Pain: Proper pain assessment(Post-operative) of the patients should be done and management
should be performed to decrease the length of their hospital stay and better health outcomes.
It also helps in the effectiveness of the administration of analgesics(Treacy & Caroline Stayt,
2019).
Consciousness level: The consciousness level of the patient should be assessed properly and
should not be overlooked, it should be a part of the patient routine management, since it acts
3
Student Name: (enter your name) Student Number: (enter your number) NRS312 Assessment Item 3
multidisciplinary team including the nurse and other healthcare personnel assess the
condition of the patient and looks after him under strict observation to ensure well-
being of the patient.
b) The recognition of the clinical deterioration in Mrs Brown’s case, which the nurses
should have noticed are the following:
Respiratory rate: It is the most critical and important sign of deterioration in a patient, an
increase of even 3-4 breaths from the normal rate can indicate respiratory distress among
patients and hypoxemia or it can act as a marker of acidosis.
Blood Pressure: It is the pressure exerted by the blood against the walls of the atria, it is an
important and crucial sign to measure as it detects the flow of blood during systole and
diastole movement of the heart, thus indicating the delivery of oxygen throughout the body.
A sudden drop in the blood pressure reading s indicates cardiac arrest(Massey, Chaboyer &
Anderson, 2017).
Pulse rate: The pulse is a palpable and rhythmic expansion of the artery caused by increased
flow of blood into the vessels due to contraction and relaxation of the heart. The pulse can be
affected by age, fluid status and medications. The regularity, strength and equality in the
pulse beat should also be assessed.
Pain: Proper pain assessment(Post-operative) of the patients should be done and management
should be performed to decrease the length of their hospital stay and better health outcomes.
It also helps in the effectiveness of the administration of analgesics(Treacy & Caroline Stayt,
2019).
Consciousness level: The consciousness level of the patient should be assessed properly and
should not be overlooked, it should be a part of the patient routine management, since it acts
3
Student Name: (enter your name) Student Number: (enter your number) NRS312 Assessment Item 3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
as a vital sign for the deterioration of neurological condition of the patient. Sometimes the
patient may get aggressive, violent or too much excited which may indicate sudden alcohol
withdrawal, hypoglycaemia, hypotension, hypoxia or medicinal side effects.
Urine output: Urine output of the patient should be measured as it helps to indicate whether
the patient has renal failure or not. It also helps in electrolyte imbalance(Sapiano, Sammut &
Trapani, 2018).
c) After Jeremy found Mrs. Brown was mumbling and notices that Mrs Brown’s face is
drooping on the right side and was making audible expiratory sounds with each
breath, she got worried and though that something might not be right for Mrs. Brown.
Jeremy immediately initiates a rapid response and calls out for help from another RN.
On observing the vital signs, it was found that the Blood pressure reading was
224/151 mmHg which was very high and is a clear identification of hypertension. The
nurse should have taken the necessary actions to reduce or control her blood pressure.
The heart rate was also found to be around 110 beats per minute, which was a sign of
tachycardia. Tachycardia is associated with increased risk of stroke and
cardiovascular problems. The nurse should take placed a pacemaker or an implantable
cardioverter dfribilator to reduce the heart rate and bring it to normal, suggest the
patient to keep relax and stress free. The respiratory rate was found to be 28 breaths
per minute which is abnormal and is a sign of anxiety, congestive heart failure or
overdose of drugs. The oxygen saturation level was also found below normal(89%),
which is an indication of hypoxemia. The nurses performed oxygen therapy providing
oxygen to the patient using a oxygen mask or a tube attached to the nose.
Question 2: Escalate
4
Student Name: (enter your name) Student Number: (enter your number) NRS312 Assessment Item 3
patient may get aggressive, violent or too much excited which may indicate sudden alcohol
withdrawal, hypoglycaemia, hypotension, hypoxia or medicinal side effects.
Urine output: Urine output of the patient should be measured as it helps to indicate whether
the patient has renal failure or not. It also helps in electrolyte imbalance(Sapiano, Sammut &
Trapani, 2018).
c) After Jeremy found Mrs. Brown was mumbling and notices that Mrs Brown’s face is
drooping on the right side and was making audible expiratory sounds with each
breath, she got worried and though that something might not be right for Mrs. Brown.
Jeremy immediately initiates a rapid response and calls out for help from another RN.
On observing the vital signs, it was found that the Blood pressure reading was
224/151 mmHg which was very high and is a clear identification of hypertension. The
nurse should have taken the necessary actions to reduce or control her blood pressure.
The heart rate was also found to be around 110 beats per minute, which was a sign of
tachycardia. Tachycardia is associated with increased risk of stroke and
cardiovascular problems. The nurse should take placed a pacemaker or an implantable
cardioverter dfribilator to reduce the heart rate and bring it to normal, suggest the
patient to keep relax and stress free. The respiratory rate was found to be 28 breaths
per minute which is abnormal and is a sign of anxiety, congestive heart failure or
overdose of drugs. The oxygen saturation level was also found below normal(89%),
which is an indication of hypoxemia. The nurses performed oxygen therapy providing
oxygen to the patient using a oxygen mask or a tube attached to the nose.
Question 2: Escalate
4
Student Name: (enter your name) Student Number: (enter your number) NRS312 Assessment Item 3
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
a) In this case, Jeremy, the registered nurse after noticing the deterioration of Mrs.
Brown, specially the anomalous increase in the readings of her blood pressure,
discusses with the nurse in charge of the unit. She then approaches the Resident
Medical Officer to assess her condition, she also briefs about the patient medical
history, asked him to prescribe paracetamol and also have a closer look into Mrs.
Brown(Ludin, 2018). But the Resident Medical Officer failed to attend Mrs. Brown at
the surgical unit, since he got very busy. As a result, Jeremy continued to monitor her
blood pressure readings and notes it down. When Jermy came to Mrs. Brown to check
the vital signs, she found that, Mrs Brown is mumbling and incomprehensible. Jeremy
notices Mrs Brown’s face is drooping on the right side and she does not appear to
understand what Jeremy is saying to her. Seeing this condition she immediately
initiates a rapid respone and informs the other registered nurse about the condition of
Mrs. Brown, then they applied an oxygen face mask and also repositioned the patient.
When the Rapid Response team approached, the Medical Registrar performed a
neurological assessment of Mrs. Brown to find out that she is experiencing a stroke.
Then she is immediately transferred to radiology for a CT scan of head and to confirm
the diagnosis of an acute ischaemic stroke(Roberts, Are & McNair, 2018).
b) The nurses should continue routine check-ups and monitoring of the patient, assess
her condition to get every set of observation, if any abnormalities were detected they
should inform the registered nurses to further look into this matter. The registered
nurse then assess the patient, documents her reports and decides whether the patient
needs an escalation of care. Then the registered nurses urgently informs the
interdisciplinary team about the deteriorating condition of the patient, and urges a
clinician with core competencies and expertise to assess the acutely ill patient(Norris,
5
Student Name: (enter your name) Student Number: (enter your number) NRS312 Assessment Item 3
Brown, specially the anomalous increase in the readings of her blood pressure,
discusses with the nurse in charge of the unit. She then approaches the Resident
Medical Officer to assess her condition, she also briefs about the patient medical
history, asked him to prescribe paracetamol and also have a closer look into Mrs.
Brown(Ludin, 2018). But the Resident Medical Officer failed to attend Mrs. Brown at
the surgical unit, since he got very busy. As a result, Jeremy continued to monitor her
blood pressure readings and notes it down. When Jermy came to Mrs. Brown to check
the vital signs, she found that, Mrs Brown is mumbling and incomprehensible. Jeremy
notices Mrs Brown’s face is drooping on the right side and she does not appear to
understand what Jeremy is saying to her. Seeing this condition she immediately
initiates a rapid respone and informs the other registered nurse about the condition of
Mrs. Brown, then they applied an oxygen face mask and also repositioned the patient.
When the Rapid Response team approached, the Medical Registrar performed a
neurological assessment of Mrs. Brown to find out that she is experiencing a stroke.
Then she is immediately transferred to radiology for a CT scan of head and to confirm
the diagnosis of an acute ischaemic stroke(Roberts, Are & McNair, 2018).
b) The nurses should continue routine check-ups and monitoring of the patient, assess
her condition to get every set of observation, if any abnormalities were detected they
should inform the registered nurses to further look into this matter. The registered
nurse then assess the patient, documents her reports and decides whether the patient
needs an escalation of care. Then the registered nurses urgently informs the
interdisciplinary team about the deteriorating condition of the patient, and urges a
clinician with core competencies and expertise to assess the acutely ill patient(Norris,
5
Student Name: (enter your name) Student Number: (enter your number) NRS312 Assessment Item 3
New & Hinsberg, 2019). After continuous monitoring of the vital sign, the registered
nurse immediately informs the medical team caring for the patient that this should be
at least at Specialist Registrar level(Freathy et al, 2019). The multidisciplinary team
having critical care competencies then performs emergency assessment of the
deteriorating patient, if they find the patient’s condition is really worsening and the
situation is getting out of control, they consider the transfer of the patient to a level 2
or level 3 care facility which is a higher dependency or ITU(O'Leary, Nash & Lewis,
2016).
c) Question 3: Manage
a) In order to avoid unrecognised patient deterioration and to enhance patient safety, the
nurses should review their knowledge and enhance their skills for measuring the
blood pressure, oxygen saturation level, heart rate as those are the early signs of
patient’s deterioration. They should provide care in a systematic approach which
helps in timely detection and monitoring of the condition of the patient, thus
preventing any further worsening of their health(Hogan et al, 2019). The nurse should
follow the ABCDE(airway, breathing, circulation, disability and exposure) approach
while treating for Mrs. Brown. At first, the nurse should observe the patient to check
for any obstruction in the airway, once the airway obstruction has been identified then
they should look for proper oxygen supply to the body, assess the breathing rate to
detect signs for respiratory distress or inadequate ventilation(Cornish et al, 2019). The
respiratory rate should be counted. The normal respiratory rate is between 12-20
breaths per minute, It was noted that after the IV was administered to Mrs. Brown, the
respiratory rate increased from 18-22 breaths per minute. The oxygen saturation level
of the patient is measured with a pulse oximeter, the normal value of oxygen
saturation is between 94-98%, with a minimum level of 88%. In this case, the oxygen
6
Student Name: (enter your name) Student Number: (enter your number) NRS312 Assessment Item 3
nurse immediately informs the medical team caring for the patient that this should be
at least at Specialist Registrar level(Freathy et al, 2019). The multidisciplinary team
having critical care competencies then performs emergency assessment of the
deteriorating patient, if they find the patient’s condition is really worsening and the
situation is getting out of control, they consider the transfer of the patient to a level 2
or level 3 care facility which is a higher dependency or ITU(O'Leary, Nash & Lewis,
2016).
c) Question 3: Manage
a) In order to avoid unrecognised patient deterioration and to enhance patient safety, the
nurses should review their knowledge and enhance their skills for measuring the
blood pressure, oxygen saturation level, heart rate as those are the early signs of
patient’s deterioration. They should provide care in a systematic approach which
helps in timely detection and monitoring of the condition of the patient, thus
preventing any further worsening of their health(Hogan et al, 2019). The nurse should
follow the ABCDE(airway, breathing, circulation, disability and exposure) approach
while treating for Mrs. Brown. At first, the nurse should observe the patient to check
for any obstruction in the airway, once the airway obstruction has been identified then
they should look for proper oxygen supply to the body, assess the breathing rate to
detect signs for respiratory distress or inadequate ventilation(Cornish et al, 2019). The
respiratory rate should be counted. The normal respiratory rate is between 12-20
breaths per minute, It was noted that after the IV was administered to Mrs. Brown, the
respiratory rate increased from 18-22 breaths per minute. The oxygen saturation level
of the patient is measured with a pulse oximeter, the normal value of oxygen
saturation is between 94-98%, with a minimum level of 88%. In this case, the oxygen
6
Student Name: (enter your name) Student Number: (enter your number) NRS312 Assessment Item 3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
saturation level of Mrs Brown was within the normal range. After checking the heart
rate of Mrs. Brown it was observed that before handover, her heart rate was
normal(92bpm), but after handover, her heart rate increased to 125bpm which
signifies that the patient is feeling stress and anxiety. Then the body temperature is
checked, the normal body temperature of an individual is between 37-38o C Then the
blood pressure is measured to detect the rate of cardiac output. Low blood pressure
can be a sign for patient deterioration. In this case, the blood pressure of Mrs. Brown
was very high 220/145 mmHg, it might indicate that she has suffered acute stroke or
ischemic heart disease, as she was once a heavy smoker and consumed alcohol every
week, it has lead to atrial fibrillation(Lavoie, Pepin & Cossette, 2017).
b) The clinical reasoning cycle assist the nurse to consider the patient condition, collect
the different cues and information such as patient report, history or background of the
patient, the previous health complications of the patient. Then the nurse further
performs experiments to gather new information about the patient’s health(Chung et
al, 2018). Then the nurse process all those information, relate the signs and symptoms
with the clinical knowledge and interpret or analyse the patient’s observed readings
with the normal ones and predicts an outcome based on such deductions.
Conclusion
In conclusion, it can be said that detecting the early signs of patient deterioration is very
essential for ensuring the patient safety. This can be done by monitoring the vital signs of the
patient, by observing and measuring the clinical indicators of early detection of deterioration
such as blood pressure, temperature, heart rate by the nurses and other clinical staffs. The
early identification triggers appropriate management, thus reducing the need for higher acuity
care, and reducing the length of stay in the hospital for the patient, lowering the healthcare
cost and also lowering the rates of morbidity. Improved monitoring also helps to reduce the
7
Student Name: (enter your name) Student Number: (enter your number) NRS312 Assessment Item 3
rate of Mrs. Brown it was observed that before handover, her heart rate was
normal(92bpm), but after handover, her heart rate increased to 125bpm which
signifies that the patient is feeling stress and anxiety. Then the body temperature is
checked, the normal body temperature of an individual is between 37-38o C Then the
blood pressure is measured to detect the rate of cardiac output. Low blood pressure
can be a sign for patient deterioration. In this case, the blood pressure of Mrs. Brown
was very high 220/145 mmHg, it might indicate that she has suffered acute stroke or
ischemic heart disease, as she was once a heavy smoker and consumed alcohol every
week, it has lead to atrial fibrillation(Lavoie, Pepin & Cossette, 2017).
b) The clinical reasoning cycle assist the nurse to consider the patient condition, collect
the different cues and information such as patient report, history or background of the
patient, the previous health complications of the patient. Then the nurse further
performs experiments to gather new information about the patient’s health(Chung et
al, 2018). Then the nurse process all those information, relate the signs and symptoms
with the clinical knowledge and interpret or analyse the patient’s observed readings
with the normal ones and predicts an outcome based on such deductions.
Conclusion
In conclusion, it can be said that detecting the early signs of patient deterioration is very
essential for ensuring the patient safety. This can be done by monitoring the vital signs of the
patient, by observing and measuring the clinical indicators of early detection of deterioration
such as blood pressure, temperature, heart rate by the nurses and other clinical staffs. The
early identification triggers appropriate management, thus reducing the need for higher acuity
care, and reducing the length of stay in the hospital for the patient, lowering the healthcare
cost and also lowering the rates of morbidity. Improved monitoring also helps to reduce the
7
Student Name: (enter your name) Student Number: (enter your number) NRS312 Assessment Item 3
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
failure-to-rescue rates. The nurses should facilitate communication with each other and the
interdisciplinary team to be able to trigger an efficient and rapid response and escalate the
patient to a higher quality of care.
Reference List
Bucknall, T. K., Forbes, H., Phillips, N. M., Hewitt, N. A., Cooper, S., Bogossian, F., &
First2Act Investigators. (2016). An analysis of nursing students’ decision‐making in
teams during simulations of acute patient deterioration. Journal of advanced
nursing, 72(10), 2482-2494.
Cho, K. J., Kwon, O., Kwon, J. M., Lee, Y., Park, H., Jeon, K. H., ... & Oh, B. H. (2020).
Detecting Patient Deterioration Using Artificial Intelligence in a Rapid Response
System. Read Online: Critical Care Medicine| Society of Critical Care
Medicine, 48(4), e285-e289.
Chung, C., Cooper, S. J., Cant, R. P., Connell, C., McKay, A., Kinsman, L., ... & Evans, L.
(2018). The educational impact of web-based and face-to-face patient deterioration
simulation programs: An interventional trial. Nurse education today, 64, 93-98.
Cornish, L., Hill, A., Horswill, M. S., Becker, S. I., & Watson, M. O. (2019). Eye-tracking
reveals how observation chart design features affect the detection of patient
deterioration: An experimental study. Applied ergonomics, 75, 230-242.
Freathy, S., Smith, G. B., Schoonhoven, L., & Westwood, G. (2019). The response to patient
deterioration in the UK National Health Service—A survey of acute hospital
policies. Resuscitation, 139, 152-158.
Hogan, H., Hutchings, A., Wulff, J., Carver, C., Holdsworth, E., Welch, J., ... & Black, N.
(2019). A qualitative study of staff perspectives on measures to prevent patient
8
Student Name: (enter your name) Student Number: (enter your number) NRS312 Assessment Item 3
interdisciplinary team to be able to trigger an efficient and rapid response and escalate the
patient to a higher quality of care.
Reference List
Bucknall, T. K., Forbes, H., Phillips, N. M., Hewitt, N. A., Cooper, S., Bogossian, F., &
First2Act Investigators. (2016). An analysis of nursing students’ decision‐making in
teams during simulations of acute patient deterioration. Journal of advanced
nursing, 72(10), 2482-2494.
Cho, K. J., Kwon, O., Kwon, J. M., Lee, Y., Park, H., Jeon, K. H., ... & Oh, B. H. (2020).
Detecting Patient Deterioration Using Artificial Intelligence in a Rapid Response
System. Read Online: Critical Care Medicine| Society of Critical Care
Medicine, 48(4), e285-e289.
Chung, C., Cooper, S. J., Cant, R. P., Connell, C., McKay, A., Kinsman, L., ... & Evans, L.
(2018). The educational impact of web-based and face-to-face patient deterioration
simulation programs: An interventional trial. Nurse education today, 64, 93-98.
Cornish, L., Hill, A., Horswill, M. S., Becker, S. I., & Watson, M. O. (2019). Eye-tracking
reveals how observation chart design features affect the detection of patient
deterioration: An experimental study. Applied ergonomics, 75, 230-242.
Freathy, S., Smith, G. B., Schoonhoven, L., & Westwood, G. (2019). The response to patient
deterioration in the UK National Health Service—A survey of acute hospital
policies. Resuscitation, 139, 152-158.
Hogan, H., Hutchings, A., Wulff, J., Carver, C., Holdsworth, E., Welch, J., ... & Black, N.
(2019). A qualitative study of staff perspectives on measures to prevent patient
8
Student Name: (enter your name) Student Number: (enter your number) NRS312 Assessment Item 3
deterioration. In Interventions to reduce mortality from in-hospital cardiac arrest: a
mixed-methods study. NIHR Journals Library.
Lavoie, P., Pepin, J., & Cossette, S. (2017). Contribution of a reflective debriefing to nursing
students' clinical judgment in patient deterioration simulations: A mixed-methods
study. Nurse education today, 50, 51-56.
Ludin, S. M. (2018). Responding to Patient Deterioration: A Medical Records
Analysis. INTERNATIONAL JOURNAL OF CARE SCHOLARS, 1(2), 22-29.
Massey, D., Chaboyer, W., & Anderson, V. (2017). What factors influence ward nurses’
recognition of and response to patient deterioration? An integrative review of the
literature. Nursing open, 4(1), 6-23.
Norris, H., New, K., & Hinsberg, F. (2019). Patient Deterioration Simulation Education and
New Graduate Nurses’ Self-Confidence and Competence: A Pilot Study. Journal for
nurses in professional development, 35(6), 330-336.
O'Leary, J., Nash, R., & Lewis, P. (2016). Standard instruction versus simulation: Educating
registered nurses in the early recognition of patient deterioration in paediatric critical
care. Nurse education today, 36, 287-292.
Roberts, A., Are, S., & McNair, D. S. (2018). U.S. Patent Application No. 15/983,348.
Sapiano, A. B., Sammut, R., & Trapani, J. (2018). The effectiveness of virtual simulation in
improving student nurses' knowledge and performance during patient deterioration: A
pre and post test design. Nurse education today, 62, 128-133.
Treacy, M., & Caroline Stayt, L. (2019). To identify the factors that influence the recognizing
and responding to adult patient deterioration in acute hospitals. Journal of advanced
nursing, 75(12), 3272-3285.
9
Student Name: (enter your name) Student Number: (enter your number) NRS312 Assessment Item 3
mixed-methods study. NIHR Journals Library.
Lavoie, P., Pepin, J., & Cossette, S. (2017). Contribution of a reflective debriefing to nursing
students' clinical judgment in patient deterioration simulations: A mixed-methods
study. Nurse education today, 50, 51-56.
Ludin, S. M. (2018). Responding to Patient Deterioration: A Medical Records
Analysis. INTERNATIONAL JOURNAL OF CARE SCHOLARS, 1(2), 22-29.
Massey, D., Chaboyer, W., & Anderson, V. (2017). What factors influence ward nurses’
recognition of and response to patient deterioration? An integrative review of the
literature. Nursing open, 4(1), 6-23.
Norris, H., New, K., & Hinsberg, F. (2019). Patient Deterioration Simulation Education and
New Graduate Nurses’ Self-Confidence and Competence: A Pilot Study. Journal for
nurses in professional development, 35(6), 330-336.
O'Leary, J., Nash, R., & Lewis, P. (2016). Standard instruction versus simulation: Educating
registered nurses in the early recognition of patient deterioration in paediatric critical
care. Nurse education today, 36, 287-292.
Roberts, A., Are, S., & McNair, D. S. (2018). U.S. Patent Application No. 15/983,348.
Sapiano, A. B., Sammut, R., & Trapani, J. (2018). The effectiveness of virtual simulation in
improving student nurses' knowledge and performance during patient deterioration: A
pre and post test design. Nurse education today, 62, 128-133.
Treacy, M., & Caroline Stayt, L. (2019). To identify the factors that influence the recognizing
and responding to adult patient deterioration in acute hospitals. Journal of advanced
nursing, 75(12), 3272-3285.
9
Student Name: (enter your name) Student Number: (enter your number) NRS312 Assessment Item 3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

Vincent, J. L., Einav, S., Pearse, R., Jaber, S., Kranke, P., Overdyk, F. J., ... & Hoeft, A.
(2018). Improving detection of patient deterioration in the general hospital ward
environment. European journal of anaesthesiology, 35(5), 325.
10
Student Name: (enter your name) Student Number: (enter your number) NRS312 Assessment Item 3
(2018). Improving detection of patient deterioration in the general hospital ward
environment. European journal of anaesthesiology, 35(5), 325.
10
Student Name: (enter your name) Student Number: (enter your number) NRS312 Assessment Item 3
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
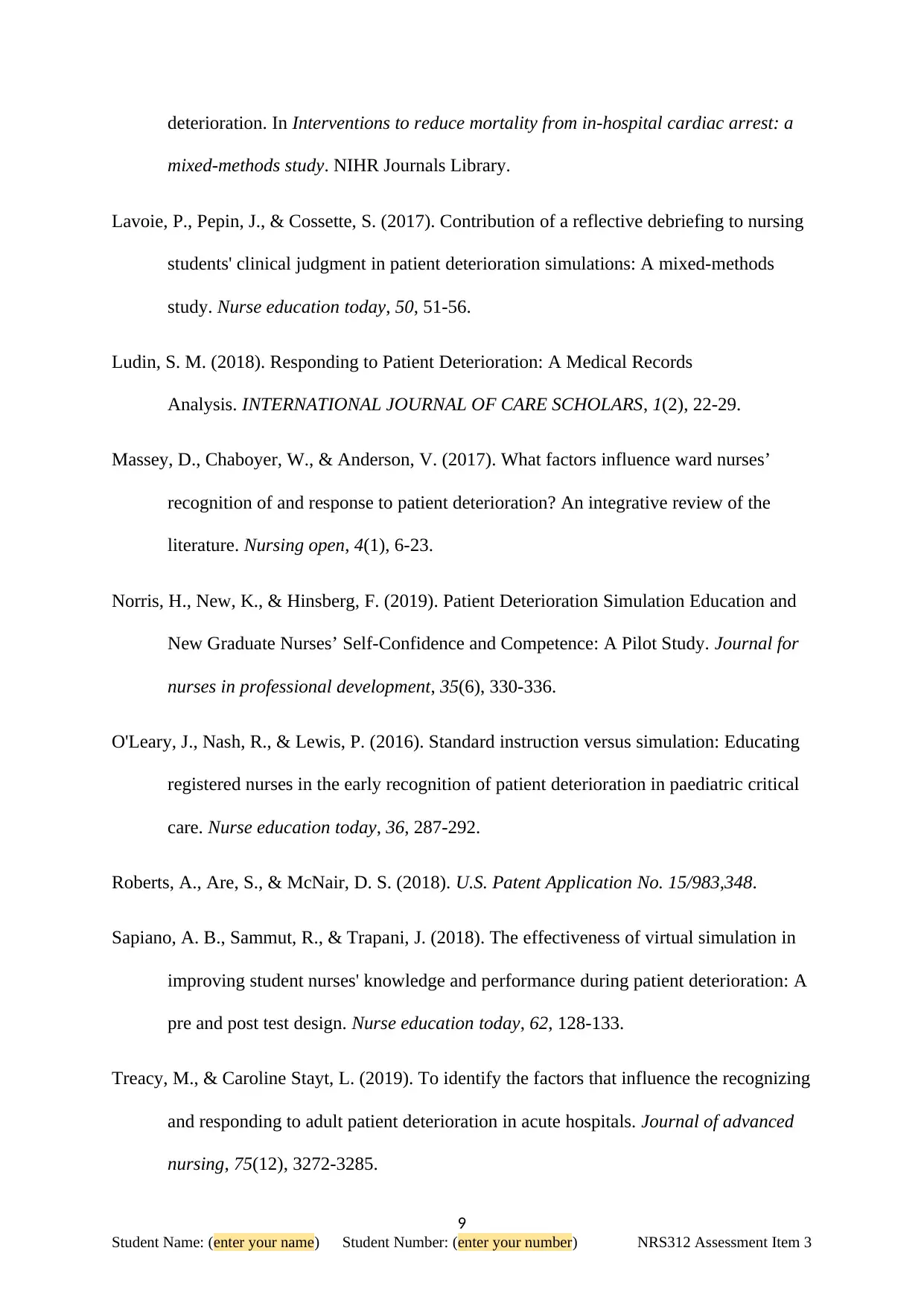
Appendix A: ISBAR Clinical Handover Table
IDENTIFY
I am Jeremy the Registered nurse of a rural hospital, briefing about the case of Mrs. Sally
Brown, a 73 years old female who is under my observation. I want the Registered Medical
Officer to visit the hospital and observe her closely.
SITUATION
The reason I am calling is because of the high systolic blood pressure of Mrs. Brown, the
last time I checked it was around 185mmHg. She was also suffering from headache and
was only responding to verbal stimuli. It would be very helpful if you kindly visist the
hospital and have a closer look into this matter.
BACKGROUND
She is a retired school principal, has a medical history of osteoarthritis, Diabetes Mellitus
Type II, no allergic response noted. She had her left knee replacement in 2010 and was a
heavy smoker once and also drinks 4-5 glasses of wine per week. No drug abuse was
noted. She lived a moderately sedentary life with occasional gardening
ASSESSMENT
The ABCDE(airway, breathing, circulation, disability and exposure) approach was
followed:
Checked for any obstruction in the airway
Assess the breathing rate to detect signs for respiratory distress or inadequate
ventilation. It was noted that after the IV was administered to Mrs. Brown, the
respiratory rate increased from 18-22 breaths per minute.
The oxygen saturation level of the patient is measured with a pulse oximeter, the
normal value of oxygen saturation is between 94-98%, with a minimum level of
88%. In this case, the oxygen saturation level of Mrs Brown was within the normal
range.
After checking the heart rate of Mrs. Brown it was observed that before handover,
her heart rate was normal(92bpm), but after handover, her heart rate increased to
125bpm which signifies that the patient is feeling stress and anxiety.
Then the body temperature is checked,it was normal
The blood pressure is measured to detect the rate of cardiac output. Low blood
pressure can be a sign for patient deterioration. In this case, the blood pressure of
Mrs. Brown was very high 220/145 mmHg, it might indicate that she has suffered
acute stroke or ischemic heart disease, as she was once a heavy smoker and
consumed alcohol every week, it has lead to atrial fibrillation
11
Student Name: (enter your name) Student Number: (enter your number) NRS312 Assessment Item 3
IDENTIFY
I am Jeremy the Registered nurse of a rural hospital, briefing about the case of Mrs. Sally
Brown, a 73 years old female who is under my observation. I want the Registered Medical
Officer to visit the hospital and observe her closely.
SITUATION
The reason I am calling is because of the high systolic blood pressure of Mrs. Brown, the
last time I checked it was around 185mmHg. She was also suffering from headache and
was only responding to verbal stimuli. It would be very helpful if you kindly visist the
hospital and have a closer look into this matter.
BACKGROUND
She is a retired school principal, has a medical history of osteoarthritis, Diabetes Mellitus
Type II, no allergic response noted. She had her left knee replacement in 2010 and was a
heavy smoker once and also drinks 4-5 glasses of wine per week. No drug abuse was
noted. She lived a moderately sedentary life with occasional gardening
ASSESSMENT
The ABCDE(airway, breathing, circulation, disability and exposure) approach was
followed:
Checked for any obstruction in the airway
Assess the breathing rate to detect signs for respiratory distress or inadequate
ventilation. It was noted that after the IV was administered to Mrs. Brown, the
respiratory rate increased from 18-22 breaths per minute.
The oxygen saturation level of the patient is measured with a pulse oximeter, the
normal value of oxygen saturation is between 94-98%, with a minimum level of
88%. In this case, the oxygen saturation level of Mrs Brown was within the normal
range.
After checking the heart rate of Mrs. Brown it was observed that before handover,
her heart rate was normal(92bpm), but after handover, her heart rate increased to
125bpm which signifies that the patient is feeling stress and anxiety.
Then the body temperature is checked,it was normal
The blood pressure is measured to detect the rate of cardiac output. Low blood
pressure can be a sign for patient deterioration. In this case, the blood pressure of
Mrs. Brown was very high 220/145 mmHg, it might indicate that she has suffered
acute stroke or ischemic heart disease, as she was once a heavy smoker and
consumed alcohol every week, it has lead to atrial fibrillation
11
Student Name: (enter your name) Student Number: (enter your number) NRS312 Assessment Item 3
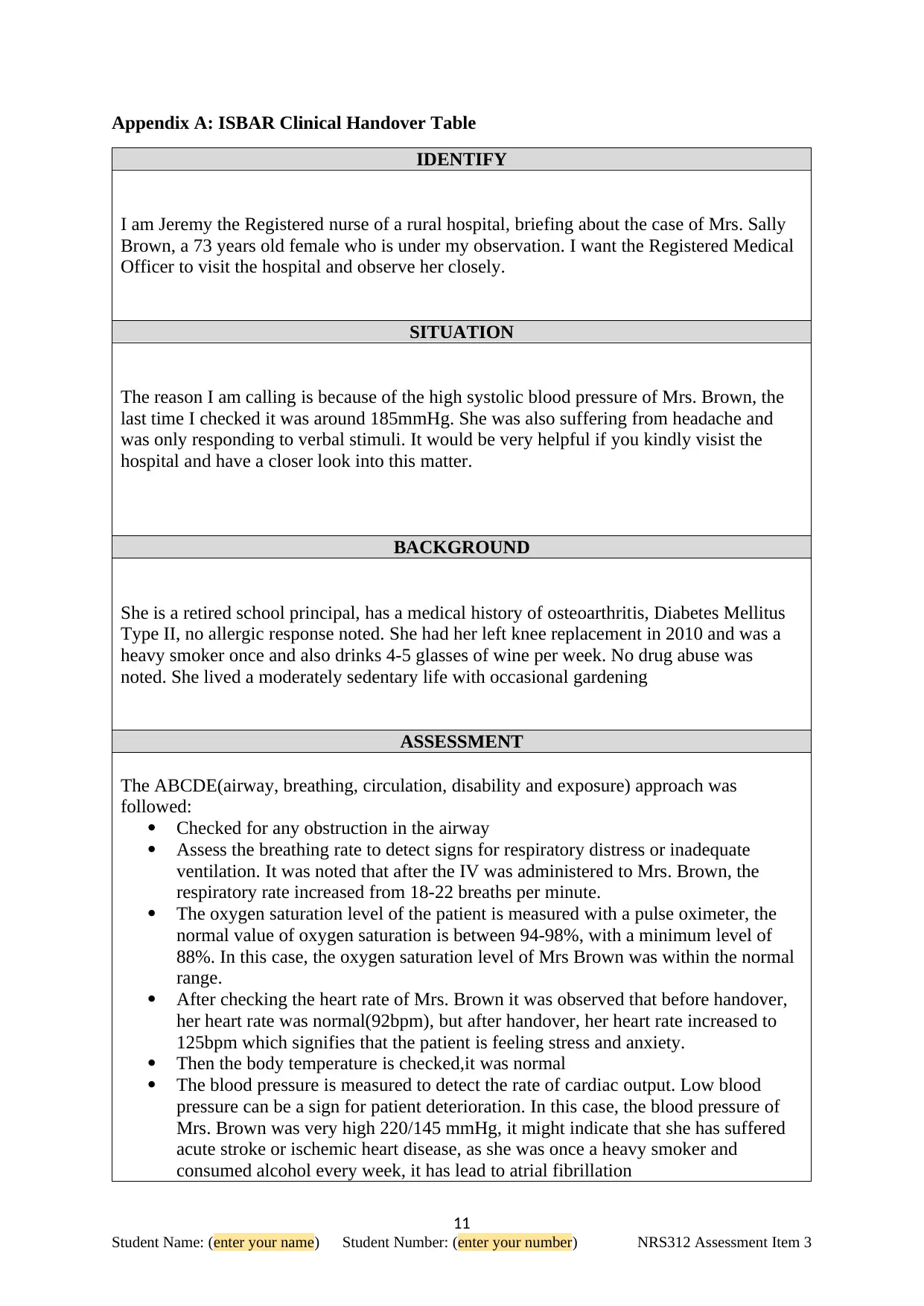
Also applied an oxygen face mask (Hudson Mask) to assist her in breathing
normally by supplying oxygen externally
RECOMMENDATION
I recommend the Registered Medical Officer to order paracetamol for Mrs. Brown and visit
the hospital urgently to have a closer look into this matter.
Appendix B: Clinical Reasoning Cycle Table
Consider the patient situation Provide an overview of the scenario
Mrs Sally Brown is a 73 year old woman, who was admitted to a rural hospital
for an elective Total Hip Replacement of her left hip. However, she undergoes an
uneventful operation and the observations remain stable throughout the procedure.
Collect cues / information Enter relevant assessment data and identify additional
assessment data that is required. Consider using a
systematic assessment framework to achieve this.
During her admission:
BP 135 / 90 mmHg
HR 90 bpm
RR 18 bpm
Temp 36.7°C
Oxygen Saturation level: 96%
No sign of pain
She has a medical history of osteoarthritis, Diabetes Mellitus Type II, no allergic response
noted. She had her left knee replacement in 2010 and was a heavy smoker once and also
drinks 4-5 glasses of wine per week. No drug abuse was noted. She lived a moderately
sedentary life
Process information Compare normal findings with those that seem
unusual or out-of-the-ordinary (‘abnormal’)
The abnormal values recorded are:
Blood Pressure - 224 / 151 mmHg (normal value: 120/90mmHg)
Heart Rate – 110bpm (Normal value: 70-80bpm)
Respiratory Rate – 28 breaths/ min (Normal value: 10-20breaths/min)
Identify problems / issues Synthesise the main issues that you have identified
12
Student Name: (enter your name) Student Number: (enter your number) NRS312 Assessment Item 3
normally by supplying oxygen externally
RECOMMENDATION
I recommend the Registered Medical Officer to order paracetamol for Mrs. Brown and visit
the hospital urgently to have a closer look into this matter.
Appendix B: Clinical Reasoning Cycle Table
Consider the patient situation Provide an overview of the scenario
Mrs Sally Brown is a 73 year old woman, who was admitted to a rural hospital
for an elective Total Hip Replacement of her left hip. However, she undergoes an
uneventful operation and the observations remain stable throughout the procedure.
Collect cues / information Enter relevant assessment data and identify additional
assessment data that is required. Consider using a
systematic assessment framework to achieve this.
During her admission:
BP 135 / 90 mmHg
HR 90 bpm
RR 18 bpm
Temp 36.7°C
Oxygen Saturation level: 96%
No sign of pain
She has a medical history of osteoarthritis, Diabetes Mellitus Type II, no allergic response
noted. She had her left knee replacement in 2010 and was a heavy smoker once and also
drinks 4-5 glasses of wine per week. No drug abuse was noted. She lived a moderately
sedentary life
Process information Compare normal findings with those that seem
unusual or out-of-the-ordinary (‘abnormal’)
The abnormal values recorded are:
Blood Pressure - 224 / 151 mmHg (normal value: 120/90mmHg)
Heart Rate – 110bpm (Normal value: 70-80bpm)
Respiratory Rate – 28 breaths/ min (Normal value: 10-20breaths/min)
Identify problems / issues Synthesise the main issues that you have identified
12
Student Name: (enter your name) Student Number: (enter your number) NRS312 Assessment Item 3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 13
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





