Challenges to Implementing Evidence Based Care in Mental Health Practice
VerifiedAdded on 2023/04/21
|14
|3427
|421
AI Summary
This essay discusses the challenges faced during the implementation of evidence based care in mental health practice. It explores the barriers and obstacles encountered in the process and provides recommendations for overcoming them.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: EVIDENCE BASED CARE
Essay
Name of the Student
Name of the University
Author Note
Essay
Name of the Student
Name of the University
Author Note
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1EVIDENCE BASED CARE
Part A- Essay
Introduction- Evidence based practice (EBP) refers to the interdisciplinary approach
that comprises of the careful, explicit and sensible use of contemporary best evidences in
making pronouncements about the care of patients. The process also encompasses the
integration of discrete clinical expertise with the best accessible external medical evidence
from organised research (LoBiondo-Wood et al., 2013). In other words, EBP can be defined
as the incorporation of clinical proficiency, patient standards, and the finest investigation
evidence into the process of clinical decision making, for ensuring health and safety of all
patients. The primary objective of EBP is to standardise the available health care services to
latest evidences, with the aim of minimising all forms of variation in patient care, and
avoiding subsequent unanticipated outcomes among the patients (Townsend & Morgan,
2017). In recent years, a plethora of EBP frameworks and models have been developed by
healthcare professionals. In the words of DiCenso, Guyatt and Ciliska (2014) these models
and outlines have meaningfully contributed to intensifying the clinical field by founding a
sound understanding of the abundant facets of the EBP, including the application and
information transformation procedures, the premeditated or structural change theory for
indorsing acceptance and implementation of new information, and its subsequent exchange.
This essay will elaborate on EBP and the challenges faced during its implementation in
mental health practice.
Mental health care setting- Primary care is associated with the procedure of providing
important healthcare services that are universally accessible to people and their family
members, in the community. Primary care is given based on the preferences and needs of the
target population (Corrigan, Druss & Perlick, 2014). Delivery of mental health services in
such settings encompasses the diagnosis and treatment of people suffering from mental
disorders, implementing effective strategies for preventing and managing their signs and
Part A- Essay
Introduction- Evidence based practice (EBP) refers to the interdisciplinary approach
that comprises of the careful, explicit and sensible use of contemporary best evidences in
making pronouncements about the care of patients. The process also encompasses the
integration of discrete clinical expertise with the best accessible external medical evidence
from organised research (LoBiondo-Wood et al., 2013). In other words, EBP can be defined
as the incorporation of clinical proficiency, patient standards, and the finest investigation
evidence into the process of clinical decision making, for ensuring health and safety of all
patients. The primary objective of EBP is to standardise the available health care services to
latest evidences, with the aim of minimising all forms of variation in patient care, and
avoiding subsequent unanticipated outcomes among the patients (Townsend & Morgan,
2017). In recent years, a plethora of EBP frameworks and models have been developed by
healthcare professionals. In the words of DiCenso, Guyatt and Ciliska (2014) these models
and outlines have meaningfully contributed to intensifying the clinical field by founding a
sound understanding of the abundant facets of the EBP, including the application and
information transformation procedures, the premeditated or structural change theory for
indorsing acceptance and implementation of new information, and its subsequent exchange.
This essay will elaborate on EBP and the challenges faced during its implementation in
mental health practice.
Mental health care setting- Primary care is associated with the procedure of providing
important healthcare services that are universally accessible to people and their family
members, in the community. Primary care is given based on the preferences and needs of the
target population (Corrigan, Druss & Perlick, 2014). Delivery of mental health services in
such settings encompasses the diagnosis and treatment of people suffering from mental
disorders, implementing effective strategies for preventing and managing their signs and
2EVIDENCE BASED CARE
symptoms, and ensuring the application of key behavioural and psychosocial skills such as,
counselling, interviewing, and interpersonal skills. According to Olfson et al. (2014) mental
health illnesses, such as, anxiety, depression, and substance abuse, are some of the most
common health conditions that are encountered in a mental health ward. These illnesses
typically co-occur with chronic and acute medical complications and are responsible for
considerably worsening the associated health outcomes among the affected people. This calls
for the need of implementing appropriate strategies for managing the illnesses. Under
situations when the mental health problems are not effectually managed, they result in an
impairment of self-care and obedience to therapeutic treatments. Furthermore, lack of EBP
implementation while treating patients suffering from mental disease are also allied with
augmented morbidity and mortality, amplified health care costs, and reduced productivity
(Vigo, Thornicroft & Atun, 2016).
Prevention and management of widely prevalent mental health diseases in primary
care comprises of the application of collective care interventions that are based on
contemporary evidences, thus increasing patient access to care, enhancing mental and
physical health outcomes, and improving the general cost-effectiveness of the interventions.
Owing to the huge variations in the readiness and capacity of mental health programs in a
hospital setting, it is imperative to adequately assess the patients and customise the treatment
services in relation to mental health care. Assessing the function, resources and goals of the
evidence based program is a vital step in implementation of EBP in mental health settings.
This should be followed by identification of the achievable and the shared objectives. Joint
valuation of the wants and viability of EBP integration, recognition of the exact steps that
need to be followed, providing training and support to the staff, and supervising the EBP
services are also essential in the clinical practice domain.
symptoms, and ensuring the application of key behavioural and psychosocial skills such as,
counselling, interviewing, and interpersonal skills. According to Olfson et al. (2014) mental
health illnesses, such as, anxiety, depression, and substance abuse, are some of the most
common health conditions that are encountered in a mental health ward. These illnesses
typically co-occur with chronic and acute medical complications and are responsible for
considerably worsening the associated health outcomes among the affected people. This calls
for the need of implementing appropriate strategies for managing the illnesses. Under
situations when the mental health problems are not effectually managed, they result in an
impairment of self-care and obedience to therapeutic treatments. Furthermore, lack of EBP
implementation while treating patients suffering from mental disease are also allied with
augmented morbidity and mortality, amplified health care costs, and reduced productivity
(Vigo, Thornicroft & Atun, 2016).
Prevention and management of widely prevalent mental health diseases in primary
care comprises of the application of collective care interventions that are based on
contemporary evidences, thus increasing patient access to care, enhancing mental and
physical health outcomes, and improving the general cost-effectiveness of the interventions.
Owing to the huge variations in the readiness and capacity of mental health programs in a
hospital setting, it is imperative to adequately assess the patients and customise the treatment
services in relation to mental health care. Assessing the function, resources and goals of the
evidence based program is a vital step in implementation of EBP in mental health settings.
This should be followed by identification of the achievable and the shared objectives. Joint
valuation of the wants and viability of EBP integration, recognition of the exact steps that
need to be followed, providing training and support to the staff, and supervising the EBP
services are also essential in the clinical practice domain.
3EVIDENCE BASED CARE
Challenges to EBP- There is mounting evidence for the fact that for sustainable and
effective dissemination of EBP services, support from the management facilitates speed
initiation. Demonstrating consistency with the already existing practices are also crucial in
mental health ward (Karlin & Cross, 2014). Additionally, availability of necessary resources
for the implementation of EBP is crucial for enhancing the health and wellbeing of the
patients. Initial challenge is encountered during recruitment of the staff who are responsible
for implementation of the EBP in mental health ward. Most often the EBP necessary for
treatment of mental disorders require adequate expertise and training from the staff, working
in the department (Novins et al., 2013). Lack of proper cultural attitude in the hospital system
is another potential challenge encountered in the mental health ward. A common perception
lies among the management and hospital authorities that the nurses would not receive any
benefits or would not get any monetary advantages, upon the implementation of evidence
based strategies in the care setting. There is mounting evidence for the fact that under most
circumstances, providing adequate information to the patients on the evidence based
intervention confuses them (Warren et al., 2016). Complex information about the intervention
threatens their decision-making abilities, and make it difficult for the service users to exert
their opinion in relation to implementation of the proposed intervention. In addition, each
patients suffering from mental health problems have individual issues and associated
psychosocial concerns. EBP often fails to be specific and precise for all the individual factors
related to the patients.
Another common challenge encountered in clinical practice can be accredited to the
fact that although trainings have the potential of enhancing EBP and its role in clinical
settings, a lack of infrastructure present in the hospital often makes it difficult to conduct
training programs that are tailored in accordance to the needs of the practitioners (Gustafsson,
Molineux & Bennett, 2014). Although external workshops are able to train the practitioners
Challenges to EBP- There is mounting evidence for the fact that for sustainable and
effective dissemination of EBP services, support from the management facilitates speed
initiation. Demonstrating consistency with the already existing practices are also crucial in
mental health ward (Karlin & Cross, 2014). Additionally, availability of necessary resources
for the implementation of EBP is crucial for enhancing the health and wellbeing of the
patients. Initial challenge is encountered during recruitment of the staff who are responsible
for implementation of the EBP in mental health ward. Most often the EBP necessary for
treatment of mental disorders require adequate expertise and training from the staff, working
in the department (Novins et al., 2013). Lack of proper cultural attitude in the hospital system
is another potential challenge encountered in the mental health ward. A common perception
lies among the management and hospital authorities that the nurses would not receive any
benefits or would not get any monetary advantages, upon the implementation of evidence
based strategies in the care setting. There is mounting evidence for the fact that under most
circumstances, providing adequate information to the patients on the evidence based
intervention confuses them (Warren et al., 2016). Complex information about the intervention
threatens their decision-making abilities, and make it difficult for the service users to exert
their opinion in relation to implementation of the proposed intervention. In addition, each
patients suffering from mental health problems have individual issues and associated
psychosocial concerns. EBP often fails to be specific and precise for all the individual factors
related to the patients.
Another common challenge encountered in clinical practice can be accredited to the
fact that although trainings have the potential of enhancing EBP and its role in clinical
settings, a lack of infrastructure present in the hospital often makes it difficult to conduct
training programs that are tailored in accordance to the needs of the practitioners (Gustafsson,
Molineux & Bennett, 2014). Although external workshops are able to train the practitioners
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4EVIDENCE BASED CARE
in EBP, these are most often inadequate for meeting the vocational demands and preferences
of the target population. This calls for the need of a preference-based EBP program that is
effortlessly accessible that comprises of funding and needs personal class attendance (Weisz
et al., 2013). Another factor that has been identified as an obstacle in the implementation of
EBP is misunderstanding and undesirable attitudes on scientific research and EBP
application. It has been found that most healthcare professionals, specifically nurses portray a
negative approach towards clinical research and fail to understand the aspects that entail EBP.
This challenge is found to persist specifically under circumstances when there are old nurses
who hold the fear that a change in treatment strategy would result in modification of practice
culture (Nilsen & Bernhardsson, 2013). This fear of change is likely to be manifested by
senior nurses who demonstrate less positive attitude towards investigation and application of
EBP, in comparison to the younger nurses. Hence, lack of willingness for undertaking
extensive research results in problems while attempting to subject the patient to interventions
that have adequate evidence for success.
In addition, Berger (2013) stated that the healthcare staff often have insufficient
knowledge on the procedures that need to be followed for the application of EBP in mental
health practice. Of the plethora of factors that are responsible for determination of the way by
which the nurses utilise the contemporary scientific evidences, individual physiognomies of
the nurses, features of the concerned healthcare organization, and the environmental
characteristics are most responsible for creating barriers. It has also been found that lack of
understanding on the research design, statistical results and data interpretation leads to
inadequate skills. Multisystem collaboration is imperative for subjecting the patients to
treatment approaches that have proved effective in the management of conditions as
depression and schizophrenia, in clinical trials. Failure in engaging the key stakeholders in
the co-operative arrangement of EBP implementation prevents ensuring presence of adequate
in EBP, these are most often inadequate for meeting the vocational demands and preferences
of the target population. This calls for the need of a preference-based EBP program that is
effortlessly accessible that comprises of funding and needs personal class attendance (Weisz
et al., 2013). Another factor that has been identified as an obstacle in the implementation of
EBP is misunderstanding and undesirable attitudes on scientific research and EBP
application. It has been found that most healthcare professionals, specifically nurses portray a
negative approach towards clinical research and fail to understand the aspects that entail EBP.
This challenge is found to persist specifically under circumstances when there are old nurses
who hold the fear that a change in treatment strategy would result in modification of practice
culture (Nilsen & Bernhardsson, 2013). This fear of change is likely to be manifested by
senior nurses who demonstrate less positive attitude towards investigation and application of
EBP, in comparison to the younger nurses. Hence, lack of willingness for undertaking
extensive research results in problems while attempting to subject the patient to interventions
that have adequate evidence for success.
In addition, Berger (2013) stated that the healthcare staff often have insufficient
knowledge on the procedures that need to be followed for the application of EBP in mental
health practice. Of the plethora of factors that are responsible for determination of the way by
which the nurses utilise the contemporary scientific evidences, individual physiognomies of
the nurses, features of the concerned healthcare organization, and the environmental
characteristics are most responsible for creating barriers. It has also been found that lack of
understanding on the research design, statistical results and data interpretation leads to
inadequate skills. Multisystem collaboration is imperative for subjecting the patients to
treatment approaches that have proved effective in the management of conditions as
depression and schizophrenia, in clinical trials. Failure in engaging the key stakeholders in
the co-operative arrangement of EBP implementation prevents ensuring presence of adequate
5EVIDENCE BASED CARE
resources, enticements, and necessities, thus impeding success of the overall program (Casey
et al., 2017). Likewise, multisystem collaboration comprises of buying-in from the greater
system, and also includes key personnel from the health department and mental health
network, which in turn is difficult to accomplish. The role of greater system variations, such
as, rearrangement of the progress notes are imperative in instructing the mental health teams
on their commitment to EBP routine (Mick, 2014). Thus, lack of support from the system
results in great financial burden and acts in the form of a hurdle to their participation in EBP
exercise. Creating provisions that hold the potential of compensating healthcare personnel for
the time they spent in consultation and training is typically considered fruitful. However,
asking the mental health teams for their participation in EBP exercise efforts, besides their
customary responsibilities is often reflected as a barrier in practice (Foster & Flanders, 2014).
Owing to the fact that EBP implementation in mental health practice requires changes
in health care policies that promote integration of the services in the setting, obstacles are
often faced in convincing the authorities and administration for reimbursing the healthcare
professionals who are entitled with the duty of promoting integration of the intervention.
Most of the time, the authorities fail to recognise the need of replacing conventional
treatment procedures by those that have been proved effective in several scholarly articles
(Young, 2012). Low levels of engagement among the patients and their family members
often results in a drop out, in the mental health setting, owing to lack of motivation for them
to remain enrolled in the treatment procedure. According to Cullen (2018) certain strategies
need to be adopted for effectively engaging the patients in the EBP event such as,
acknowledging the delivery of good treatment, addressing their values and preferences,
reinforcing efforts taken to change the treatment, and providing options for accomplishment
of the intended goals. However, the professionals often fail to elicit self-motivational
modifying statements, thus resulting in their failure in recognising, developing and
resources, enticements, and necessities, thus impeding success of the overall program (Casey
et al., 2017). Likewise, multisystem collaboration comprises of buying-in from the greater
system, and also includes key personnel from the health department and mental health
network, which in turn is difficult to accomplish. The role of greater system variations, such
as, rearrangement of the progress notes are imperative in instructing the mental health teams
on their commitment to EBP routine (Mick, 2014). Thus, lack of support from the system
results in great financial burden and acts in the form of a hurdle to their participation in EBP
exercise. Creating provisions that hold the potential of compensating healthcare personnel for
the time they spent in consultation and training is typically considered fruitful. However,
asking the mental health teams for their participation in EBP exercise efforts, besides their
customary responsibilities is often reflected as a barrier in practice (Foster & Flanders, 2014).
Owing to the fact that EBP implementation in mental health practice requires changes
in health care policies that promote integration of the services in the setting, obstacles are
often faced in convincing the authorities and administration for reimbursing the healthcare
professionals who are entitled with the duty of promoting integration of the intervention.
Most of the time, the authorities fail to recognise the need of replacing conventional
treatment procedures by those that have been proved effective in several scholarly articles
(Young, 2012). Low levels of engagement among the patients and their family members
often results in a drop out, in the mental health setting, owing to lack of motivation for them
to remain enrolled in the treatment procedure. According to Cullen (2018) certain strategies
need to be adopted for effectively engaging the patients in the EBP event such as,
acknowledging the delivery of good treatment, addressing their values and preferences,
reinforcing efforts taken to change the treatment, and providing options for accomplishment
of the intended goals. However, the professionals often fail to elicit self-motivational
modifying statements, thus resulting in their failure in recognising, developing and
6EVIDENCE BASED CARE
implementing plans for making the patients adhere to the proposed treatments (Weist et al.,
2014).
Adequate provisions must be there for accessing the internet and search engines, in
order to retrieve scholarly evidences that contain relevant information on the efficacy of
certain pharmacological and non-pharmacological interventions, for the management of
mental disorders. However, at most instances there is lack of adequate internet facilities in the
healthcare setting, which in turn prevents the nursing staff from extracting contemporary
evidences to treat a phenomenon under investigation. Collection of adequate scientific
information requires unrestricted access to a rich library that acts as a repository of nursing
journals (Gosselin, Dalton & Penne, 2015). This organisational barrier also makes it difficult
to access the high quality evidences that are pertinent to different mental disorders from
which the admitted patients suffer. Despite the increase in the demand for nursing health
professionals in mental health wards, the employment rates are constant, thereby leading to a
shortage in the workforce. Lessening pipeline of mental nurses can also be accredited to a
shortage of faculty, which in turn makes the nursing staff working in the mental ward work
for prolonged hours under stressful conditions (Hosking et al., 2016). Subsequent onset of
injury, fatigue and job dissatisfaction makes the staff lose interest in implementing better
procedures for treating mental disorders, and also increases their likelihood of making
medical errors.
Conclusion- Thus, it can be concluded that collaboration, mentorship,
interdisciplinary communiqué, proper professional network, and helpful organisation as
critical to EBP adoption. It is imperative for nurses working in the mental ward to remain
equipped to formulating necessary questions, critically assessing their practice, and
evaluating the guidelines and evidence levels, for operation in the hospital settings. Despite
functional development and organisations in place to indorse EBP, most authorities and
implementing plans for making the patients adhere to the proposed treatments (Weist et al.,
2014).
Adequate provisions must be there for accessing the internet and search engines, in
order to retrieve scholarly evidences that contain relevant information on the efficacy of
certain pharmacological and non-pharmacological interventions, for the management of
mental disorders. However, at most instances there is lack of adequate internet facilities in the
healthcare setting, which in turn prevents the nursing staff from extracting contemporary
evidences to treat a phenomenon under investigation. Collection of adequate scientific
information requires unrestricted access to a rich library that acts as a repository of nursing
journals (Gosselin, Dalton & Penne, 2015). This organisational barrier also makes it difficult
to access the high quality evidences that are pertinent to different mental disorders from
which the admitted patients suffer. Despite the increase in the demand for nursing health
professionals in mental health wards, the employment rates are constant, thereby leading to a
shortage in the workforce. Lessening pipeline of mental nurses can also be accredited to a
shortage of faculty, which in turn makes the nursing staff working in the mental ward work
for prolonged hours under stressful conditions (Hosking et al., 2016). Subsequent onset of
injury, fatigue and job dissatisfaction makes the staff lose interest in implementing better
procedures for treating mental disorders, and also increases their likelihood of making
medical errors.
Conclusion- Thus, it can be concluded that collaboration, mentorship,
interdisciplinary communiqué, proper professional network, and helpful organisation as
critical to EBP adoption. It is imperative for nurses working in the mental ward to remain
equipped to formulating necessary questions, critically assessing their practice, and
evaluating the guidelines and evidence levels, for operation in the hospital settings. Despite
functional development and organisations in place to indorse EBP, most authorities and
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7EVIDENCE BASED CARE
administration have yet to assimilate an evidence-based care model. This calls for the need of
addressing the identified barriers and creating provisions that will facilitate the
implementation of interventions and strategies that are able to effectively reduce severity of
mental illnesses, thus enhancing the health and wellbeing of the patients.
administration have yet to assimilate an evidence-based care model. This calls for the need of
addressing the identified barriers and creating provisions that will facilitate the
implementation of interventions and strategies that are able to effectively reduce severity of
mental illnesses, thus enhancing the health and wellbeing of the patients.
8EVIDENCE BASED CARE
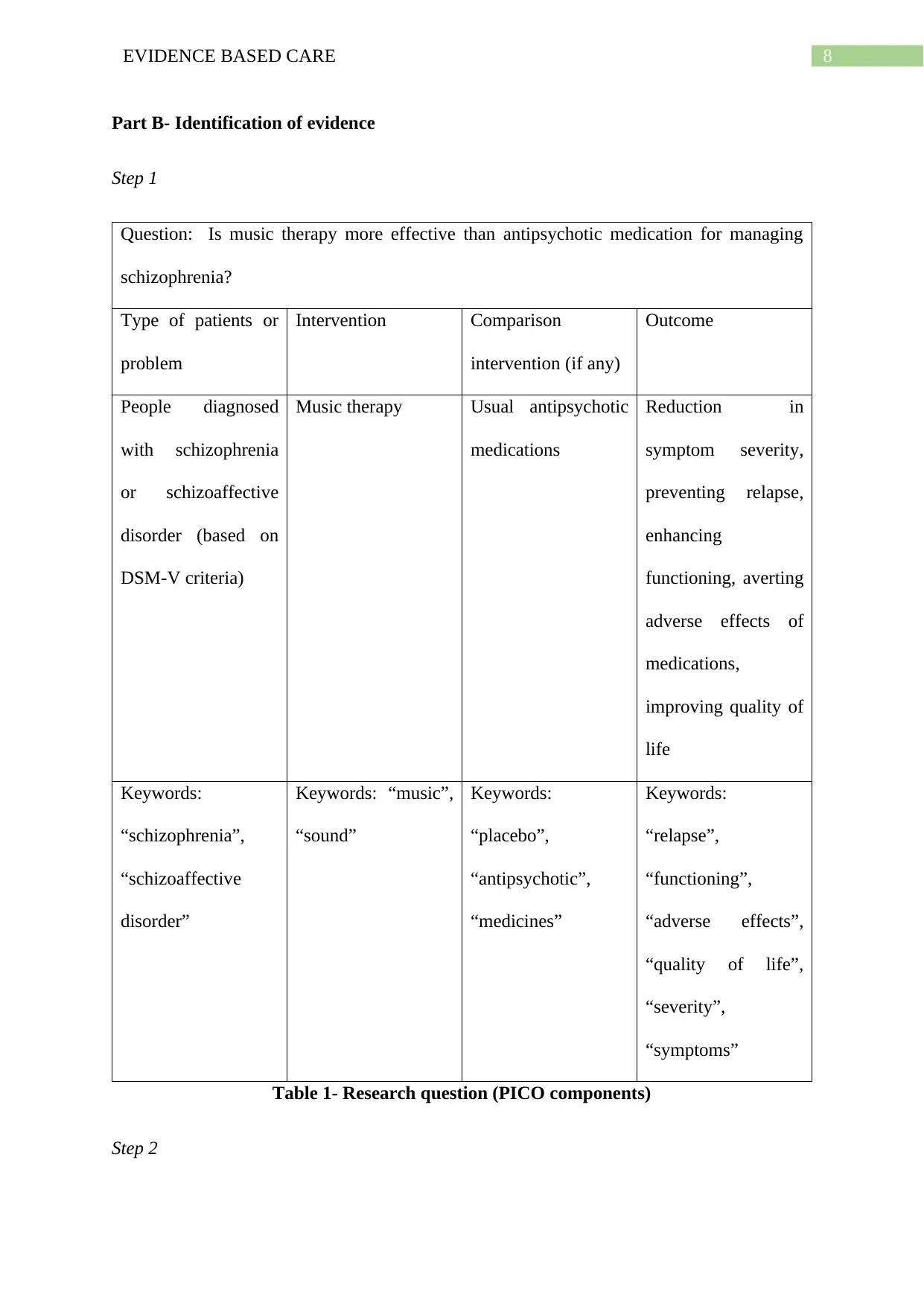
Part B- Identification of evidence
Step 1
Question: Is music therapy more effective than antipsychotic medication for managing
schizophrenia?
Type of patients or
problem
Intervention Comparison
intervention (if any)
Outcome
People diagnosed
with schizophrenia
or schizoaffective
disorder (based on
DSM-V criteria)
Music therapy Usual antipsychotic
medications
Reduction in
symptom severity,
preventing relapse,
enhancing
functioning, averting
adverse effects of
medications,
improving quality of
life
Keywords:
“schizophrenia”,
“schizoaffective
disorder”
Keywords: “music”,
“sound”
Keywords:
“placebo”,
“antipsychotic”,
“medicines”
Keywords:
“relapse”,
“functioning”,
“adverse effects”,
“quality of life”,
“severity”,
“symptoms”
Table 1- Research question (PICO components)
Step 2
Part B- Identification of evidence
Step 1
Question: Is music therapy more effective than antipsychotic medication for managing
schizophrenia?
Type of patients or
problem
Intervention Comparison
intervention (if any)
Outcome
People diagnosed
with schizophrenia
or schizoaffective
disorder (based on
DSM-V criteria)
Music therapy Usual antipsychotic
medications
Reduction in
symptom severity,
preventing relapse,
enhancing
functioning, averting
adverse effects of
medications,
improving quality of
life
Keywords:
“schizophrenia”,
“schizoaffective
disorder”
Keywords: “music”,
“sound”
Keywords:
“placebo”,
“antipsychotic”,
“medicines”
Keywords:
“relapse”,
“functioning”,
“adverse effects”,
“quality of life”,
“severity”,
“symptoms”
Table 1- Research question (PICO components)
Step 2
9EVIDENCE BASED CARE
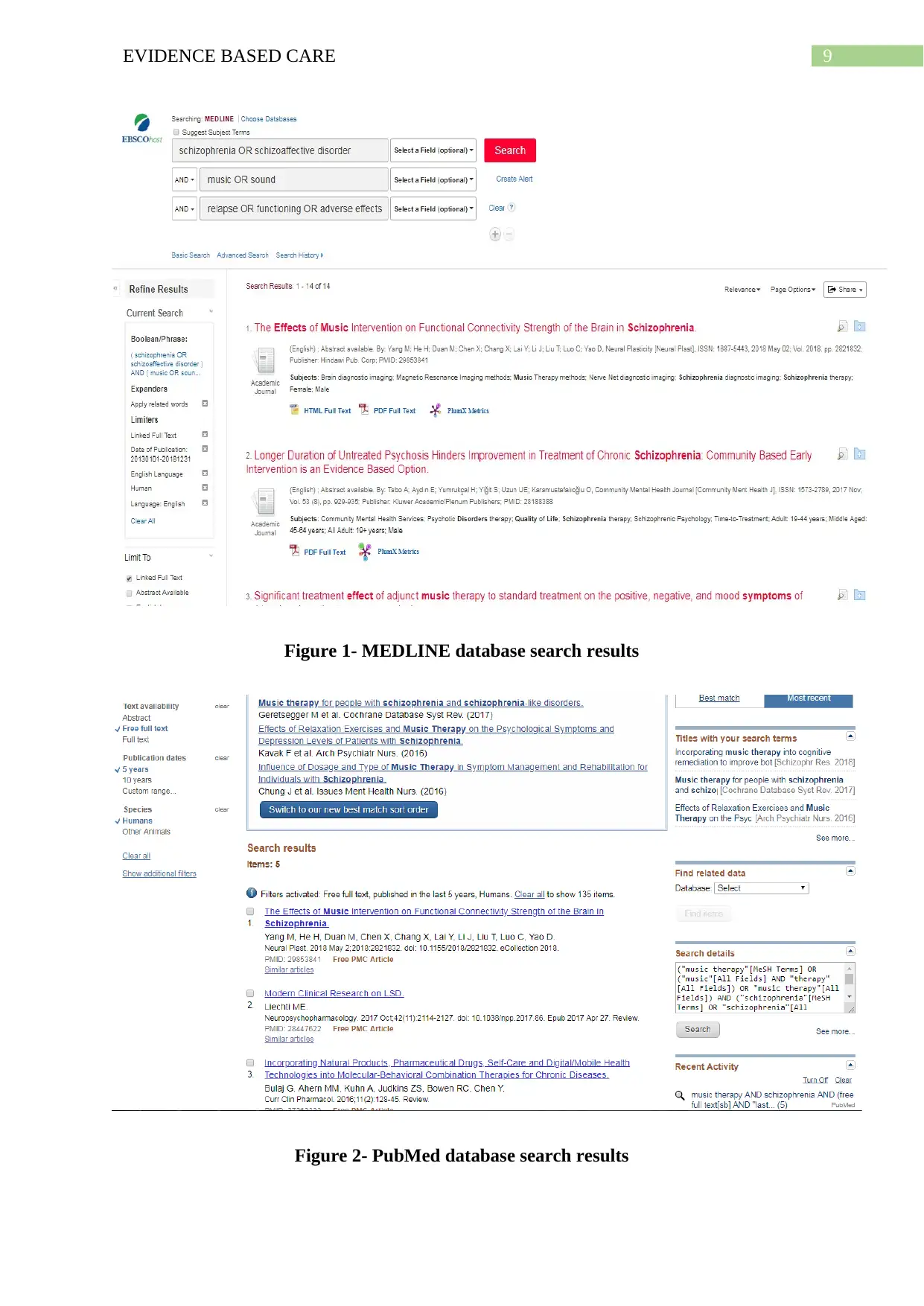
Figure 1- MEDLINE database search results
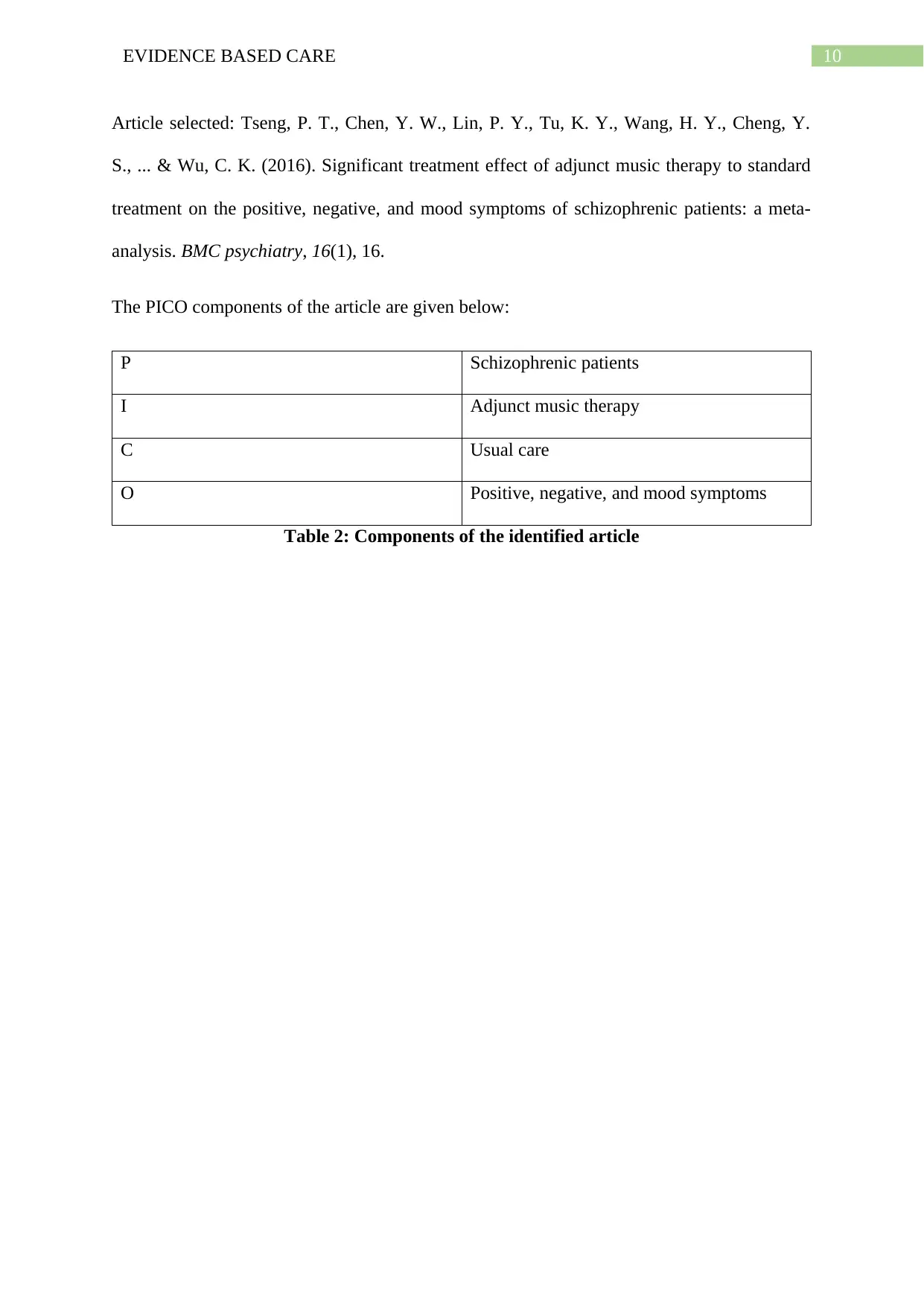
Figure 2- PubMed database search results
Figure 1- MEDLINE database search results
Figure 2- PubMed database search results
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
10EVIDENCE BASED CARE
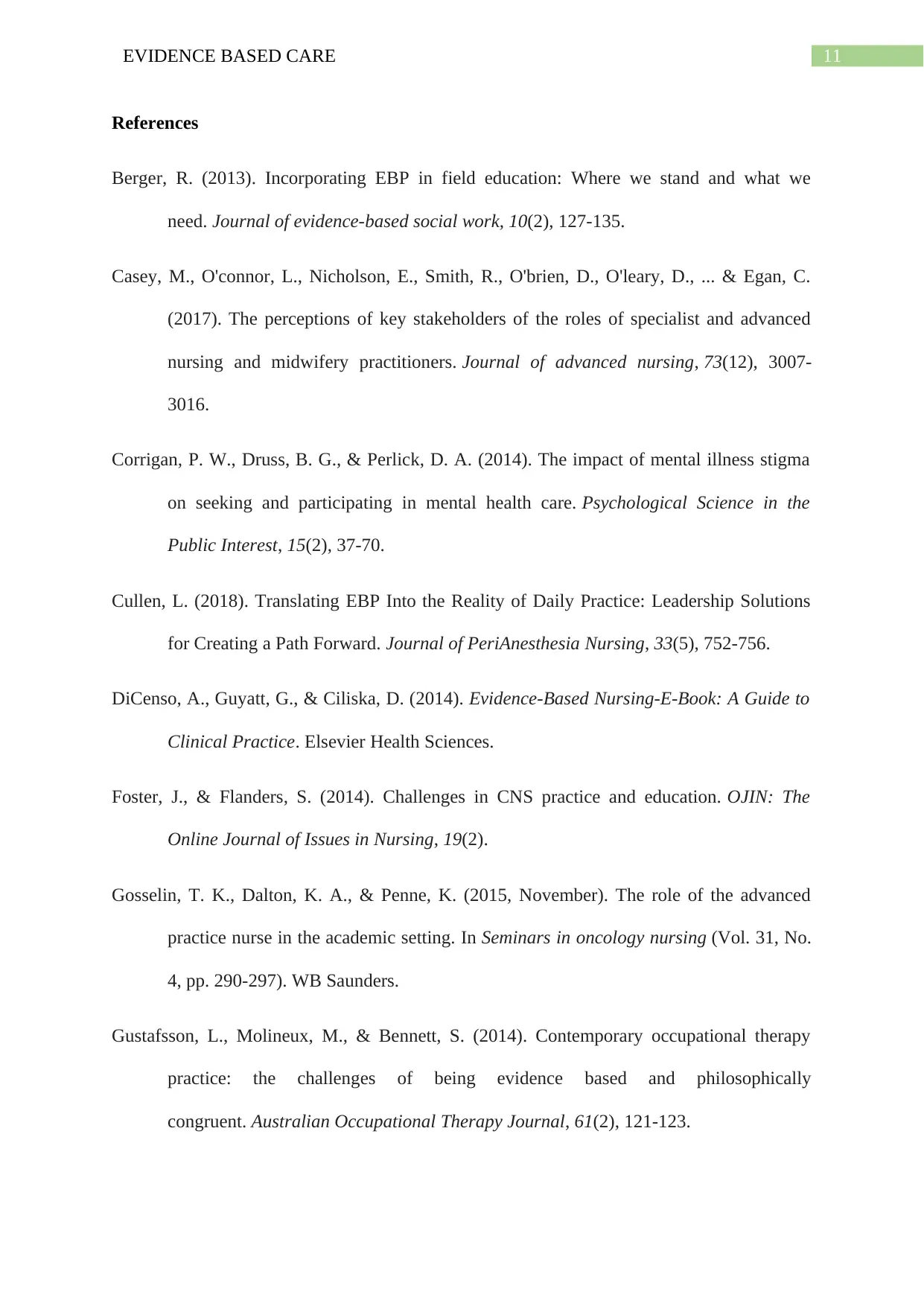
Article selected: Tseng, P. T., Chen, Y. W., Lin, P. Y., Tu, K. Y., Wang, H. Y., Cheng, Y.
S., ... & Wu, C. K. (2016). Significant treatment effect of adjunct music therapy to standard
treatment on the positive, negative, and mood symptoms of schizophrenic patients: a meta-
analysis. BMC psychiatry, 16(1), 16.
The PICO components of the article are given below:
P Schizophrenic patients
I Adjunct music therapy
C Usual care
O Positive, negative, and mood symptoms
Table 2: Components of the identified article
Article selected: Tseng, P. T., Chen, Y. W., Lin, P. Y., Tu, K. Y., Wang, H. Y., Cheng, Y.
S., ... & Wu, C. K. (2016). Significant treatment effect of adjunct music therapy to standard
treatment on the positive, negative, and mood symptoms of schizophrenic patients: a meta-
analysis. BMC psychiatry, 16(1), 16.
The PICO components of the article are given below:
P Schizophrenic patients
I Adjunct music therapy
C Usual care
O Positive, negative, and mood symptoms
Table 2: Components of the identified article
11EVIDENCE BASED CARE
References
Berger, R. (2013). Incorporating EBP in field education: Where we stand and what we
need. Journal of evidence-based social work, 10(2), 127-135.
Casey, M., O'connor, L., Nicholson, E., Smith, R., O'brien, D., O'leary, D., ... & Egan, C.
(2017). The perceptions of key stakeholders of the roles of specialist and advanced
nursing and midwifery practitioners. Journal of advanced nursing, 73(12), 3007-
3016.
Corrigan, P. W., Druss, B. G., & Perlick, D. A. (2014). The impact of mental illness stigma
on seeking and participating in mental health care. Psychological Science in the
Public Interest, 15(2), 37-70.
Cullen, L. (2018). Translating EBP Into the Reality of Daily Practice: Leadership Solutions
for Creating a Path Forward. Journal of PeriAnesthesia Nursing, 33(5), 752-756.
DiCenso, A., Guyatt, G., & Ciliska, D. (2014). Evidence-Based Nursing-E-Book: A Guide to
Clinical Practice. Elsevier Health Sciences.
Foster, J., & Flanders, S. (2014). Challenges in CNS practice and education. OJIN: The
Online Journal of Issues in Nursing, 19(2).
Gosselin, T. K., Dalton, K. A., & Penne, K. (2015, November). The role of the advanced
practice nurse in the academic setting. In Seminars in oncology nursing (Vol. 31, No.
4, pp. 290-297). WB Saunders.
Gustafsson, L., Molineux, M., & Bennett, S. (2014). Contemporary occupational therapy
practice: the challenges of being evidence based and philosophically
congruent. Australian Occupational Therapy Journal, 61(2), 121-123.
References
Berger, R. (2013). Incorporating EBP in field education: Where we stand and what we
need. Journal of evidence-based social work, 10(2), 127-135.
Casey, M., O'connor, L., Nicholson, E., Smith, R., O'brien, D., O'leary, D., ... & Egan, C.
(2017). The perceptions of key stakeholders of the roles of specialist and advanced
nursing and midwifery practitioners. Journal of advanced nursing, 73(12), 3007-
3016.
Corrigan, P. W., Druss, B. G., & Perlick, D. A. (2014). The impact of mental illness stigma
on seeking and participating in mental health care. Psychological Science in the
Public Interest, 15(2), 37-70.
Cullen, L. (2018). Translating EBP Into the Reality of Daily Practice: Leadership Solutions
for Creating a Path Forward. Journal of PeriAnesthesia Nursing, 33(5), 752-756.
DiCenso, A., Guyatt, G., & Ciliska, D. (2014). Evidence-Based Nursing-E-Book: A Guide to
Clinical Practice. Elsevier Health Sciences.
Foster, J., & Flanders, S. (2014). Challenges in CNS practice and education. OJIN: The
Online Journal of Issues in Nursing, 19(2).
Gosselin, T. K., Dalton, K. A., & Penne, K. (2015, November). The role of the advanced
practice nurse in the academic setting. In Seminars in oncology nursing (Vol. 31, No.
4, pp. 290-297). WB Saunders.
Gustafsson, L., Molineux, M., & Bennett, S. (2014). Contemporary occupational therapy
practice: the challenges of being evidence based and philosophically
congruent. Australian Occupational Therapy Journal, 61(2), 121-123.
12EVIDENCE BASED CARE
Hosking, J., Knox, K., Forman, J., Montgomery, L. A., Valde, J. G., & Cullen, L. (2016).
Evidence into practice: Leading new graduate nurses to evidence-based practice
through a nurse residency program. Journal of PeriAnesthesia Nursing, 31(3), 260-
265.
Karlin, B. E., & Cross, G. (2014). From the laboratory to the therapy room: National
dissemination and implementation of evidence-based psychotherapies in the US
Department of Veterans Affairs Health Care System. American Psychologist, 69(1),
19.
LoBiondo-Wood, G., Haber, J., Berry, C., & Yost, J. (2013). Study Guide for Nursing
Research-E-Book: Methods and Critical Appraisal for Evidence-Based Practice.
Elsevier Health Sciences.
Mick, J. (2014). Nurse interns’ experience with participation in the evidence-based practice
project requirement of a Nursing Internship Program. Nurse educator, 39(2), 54-55.
Nilsen, P., & Bernhardsson, S. (2013). Towards evidence-based physiotherapy–research
challenges and needs. Journal of physiotherapy, 59(3), 143-144.
Novins, D. K., Green, A. E., Legha, R. K., & Aarons, G. A. (2013). Dissemination and
implementation of evidence-based practices for child and adolescent mental health: A
systematic review. Journal of the American Academy of Child & Adolescent
Psychiatry, 52(10), 1009-1025.
Olfson, M., Blanco, C., Wang, S., Laje, G., & Correll, C. U. (2014). National trends in the
mental health care of children, adolescents, and adults by office-based
physicians. JAMA psychiatry, 71(1), 81-90.
Hosking, J., Knox, K., Forman, J., Montgomery, L. A., Valde, J. G., & Cullen, L. (2016).
Evidence into practice: Leading new graduate nurses to evidence-based practice
through a nurse residency program. Journal of PeriAnesthesia Nursing, 31(3), 260-
265.
Karlin, B. E., & Cross, G. (2014). From the laboratory to the therapy room: National
dissemination and implementation of evidence-based psychotherapies in the US
Department of Veterans Affairs Health Care System. American Psychologist, 69(1),
19.
LoBiondo-Wood, G., Haber, J., Berry, C., & Yost, J. (2013). Study Guide for Nursing
Research-E-Book: Methods and Critical Appraisal for Evidence-Based Practice.
Elsevier Health Sciences.
Mick, J. (2014). Nurse interns’ experience with participation in the evidence-based practice
project requirement of a Nursing Internship Program. Nurse educator, 39(2), 54-55.
Nilsen, P., & Bernhardsson, S. (2013). Towards evidence-based physiotherapy–research
challenges and needs. Journal of physiotherapy, 59(3), 143-144.
Novins, D. K., Green, A. E., Legha, R. K., & Aarons, G. A. (2013). Dissemination and
implementation of evidence-based practices for child and adolescent mental health: A
systematic review. Journal of the American Academy of Child & Adolescent
Psychiatry, 52(10), 1009-1025.
Olfson, M., Blanco, C., Wang, S., Laje, G., & Correll, C. U. (2014). National trends in the
mental health care of children, adolescents, and adults by office-based
physicians. JAMA psychiatry, 71(1), 81-90.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
13EVIDENCE BASED CARE
Townsend, M. C., & Morgan, K. I. (2017). Psychiatric mental health nursing: Concepts of
care in evidence-based practice. FA Davis.
Vigo, D., Thornicroft, G., & Atun, R. (2016). Estimating the true global burden of mental
illness. The Lancet Psychiatry, 3(2), 171-178.
Warren, J. I., McLaughlin, M., Bardsley, J., Eich, J., Esche, C. A., Kropkowski, L., & Risch,
S. (2016). The strengths and challenges of implementing EBP in healthcare
systems. Worldviews on Evidence
‐Based Nursing, 13(1), 15-24.
Weist, M. D., Youngstrom, E. A., Stephan, S., Lever, N., Fowler, J., Taylor, L., ... &
Hoagwood, K. (2014). Challenges and ideas from a research program on high-quality,
evidence-based practice in school mental health. Journal of Clinical Child &
Adolescent Psychology, 43(2), 244-255.
Weisz, J. R., Ugueto, A. M., Cheron, D. M., & Herren, J. (2013). Evidence-based youth
psychotherapy in the mental health ecosystem. Journal of Clinical Child &
Adolescent Psychology, 42(2), 274-286.
Young, M. (2012). Transitioning evidence to practice. Evidence-Based Practice for Nurses,
386-396.
Townsend, M. C., & Morgan, K. I. (2017). Psychiatric mental health nursing: Concepts of
care in evidence-based practice. FA Davis.
Vigo, D., Thornicroft, G., & Atun, R. (2016). Estimating the true global burden of mental
illness. The Lancet Psychiatry, 3(2), 171-178.
Warren, J. I., McLaughlin, M., Bardsley, J., Eich, J., Esche, C. A., Kropkowski, L., & Risch,
S. (2016). The strengths and challenges of implementing EBP in healthcare
systems. Worldviews on Evidence
‐Based Nursing, 13(1), 15-24.
Weist, M. D., Youngstrom, E. A., Stephan, S., Lever, N., Fowler, J., Taylor, L., ... &
Hoagwood, K. (2014). Challenges and ideas from a research program on high-quality,
evidence-based practice in school mental health. Journal of Clinical Child &
Adolescent Psychology, 43(2), 244-255.
Weisz, J. R., Ugueto, A. M., Cheron, D. M., & Herren, J. (2013). Evidence-based youth
psychotherapy in the mental health ecosystem. Journal of Clinical Child &
Adolescent Psychology, 42(2), 274-286.
Young, M. (2012). Transitioning evidence to practice. Evidence-Based Practice for Nurses,
386-396.
1 out of 14
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





