Impact of Diet on Colonoscopy Preparation
VerifiedAdded on 2020/03/28
|17
|4896
|88
AI Summary
This assignment delves into the impact of different dietary approaches on the success of colonoscopy preparation. Students are tasked with critically examining research papers and randomized controlled trials comparing the effectiveness of low-residue diets versus clear liquid diets in achieving optimal bowel cleansing for colonoscopy procedures. The analysis should encompass patient tolerance, quality of colon cleansing, and overall efficacy of each dietary regimen.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: NURSING
Research evidence and clinical practice
Name of the student:
Name of the university:
Author note:
Research evidence and clinical practice
Name of the student:
Name of the university:
Author note:
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1NURSING
This paper is based on the evidence based practice study. In this paper there is a
description about the clear liquid diet and its effectiveness. This study describes that the adult
patients from the age of 18-45 who is being prepared for some test or operation are on less
risk as compared to the patients who is in fasting for long time.
Clear liquid diet – A clear liquid diet is a type of fluid that helps a patient to stay
hydrated. It may consist of water, clear juices, tea or coffee. It is mainly used to provide rest
to the gastrointestinal before doing a test or an operation. These liquids diets are used so that
they can provide vitamins and minerals for generating energy so that it can keep our body
hydrated (Hookey et al., 2017). This type of diet helps the patient by providing them
important electrolytes and gives them energy when a proper diet cannot be provided to the
patient.
As a part of surgical department, it is noticed that some of the patient used to do
fasting for a long time without thinking about the condition of the patient and their surgery. It
is obvious that the medical experts are proceeding with the customary method for "nil by
mouth" from the midnight for any operations. The tradition of fasting before the operation is
to diminish the risk of complications (Brown and Heuberger, 2014). Clear liquids incorporate
water, natural product juice, clear genial, dark espresso and tea. As per Australian and New
Zealand school of Anaesthetists, 2016 (ANZCA), it had been prescribed to take constrained
non-greasy strong sustenance up to six hours and clear liquid weight control plans up to 2
hours preceding anaesthesia. It is not prescribed to apply the new fasting guideline to patients
who are at the danger of peri-operative spewing forth or heaving (Smith et al., 2011). This
incorporates patients experiencing crisis surgeries and those with associated deferred purging
with gastric substance, and obstetric patients who are in the process of giving birth (Smith et
al., 2011).
This paper is based on the evidence based practice study. In this paper there is a
description about the clear liquid diet and its effectiveness. This study describes that the adult
patients from the age of 18-45 who is being prepared for some test or operation are on less
risk as compared to the patients who is in fasting for long time.
Clear liquid diet – A clear liquid diet is a type of fluid that helps a patient to stay
hydrated. It may consist of water, clear juices, tea or coffee. It is mainly used to provide rest
to the gastrointestinal before doing a test or an operation. These liquids diets are used so that
they can provide vitamins and minerals for generating energy so that it can keep our body
hydrated (Hookey et al., 2017). This type of diet helps the patient by providing them
important electrolytes and gives them energy when a proper diet cannot be provided to the
patient.
As a part of surgical department, it is noticed that some of the patient used to do
fasting for a long time without thinking about the condition of the patient and their surgery. It
is obvious that the medical experts are proceeding with the customary method for "nil by
mouth" from the midnight for any operations. The tradition of fasting before the operation is
to diminish the risk of complications (Brown and Heuberger, 2014). Clear liquids incorporate
water, natural product juice, clear genial, dark espresso and tea. As per Australian and New
Zealand school of Anaesthetists, 2016 (ANZCA), it had been prescribed to take constrained
non-greasy strong sustenance up to six hours and clear liquid weight control plans up to 2
hours preceding anaesthesia. It is not prescribed to apply the new fasting guideline to patients
who are at the danger of peri-operative spewing forth or heaving (Smith et al., 2011). This
incorporates patients experiencing crisis surgeries and those with associated deferred purging
with gastric substance, and obstetric patients who are in the process of giving birth (Smith et
al., 2011).
2NURSING
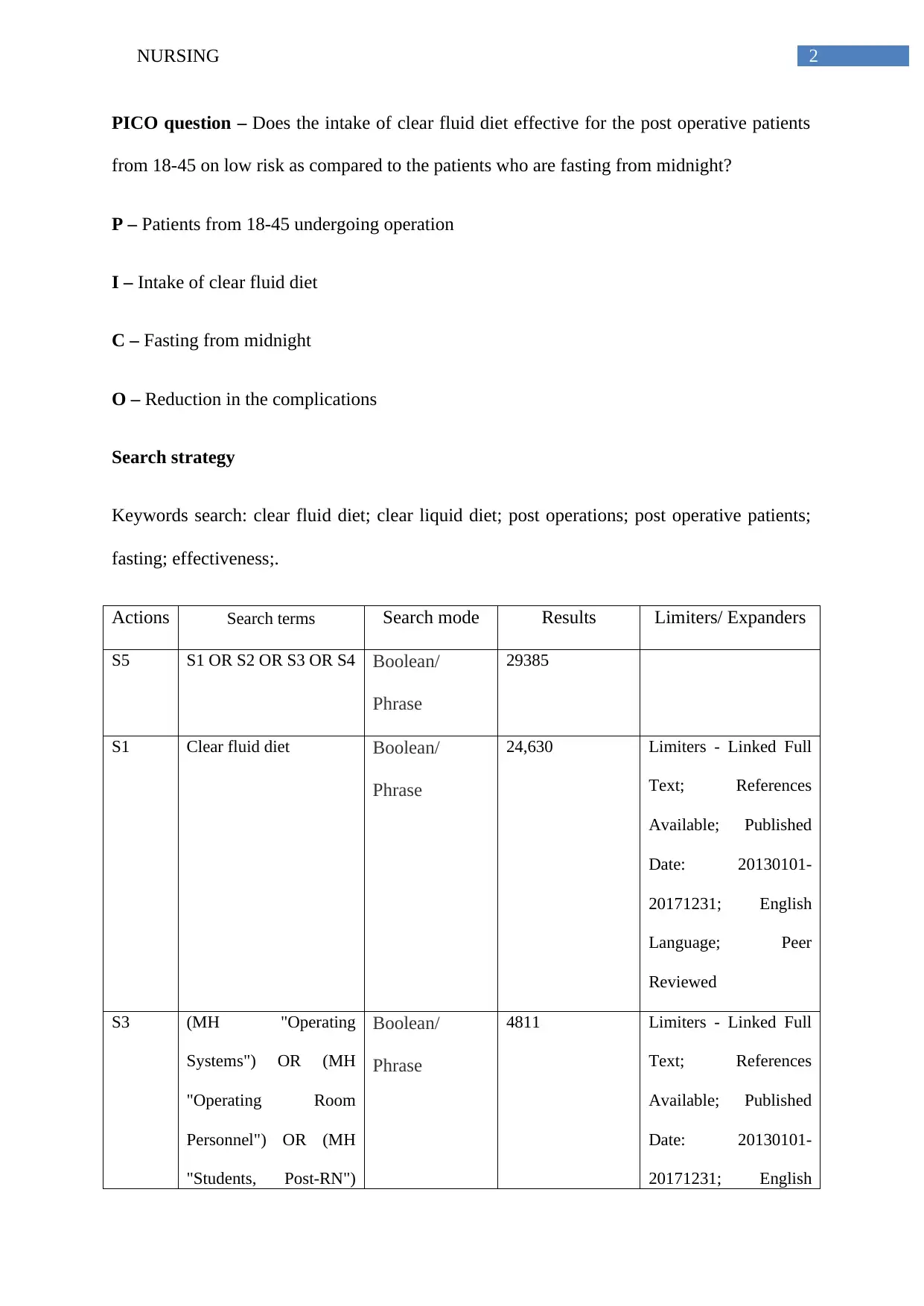
PICO question – Does the intake of clear fluid diet effective for the post operative patients
from 18-45 on low risk as compared to the patients who are fasting from midnight?
P – Patients from 18-45 undergoing operation
I – Intake of clear fluid diet
C – Fasting from midnight
O – Reduction in the complications
Search strategy
Keywords search: clear fluid diet; clear liquid diet; post operations; post operative patients;
fasting; effectiveness;.
Actions Search terms Search mode Results Limiters/ Expanders
S5 S1 OR S2 OR S3 OR S4 Boolean/
Phrase
29385
S1 Clear fluid diet Boolean/
Phrase
24,630 Limiters - Linked Full
Text; References
Available; Published
Date: 20130101-
20171231; English
Language; Peer
Reviewed
S3 (MH "Operating
Systems") OR (MH
"Operating Room
Personnel") OR (MH
"Students, Post-RN")
Boolean/
Phrase
4811 Limiters - Linked Full
Text; References
Available; Published
Date: 20130101-
20171231; English
PICO question – Does the intake of clear fluid diet effective for the post operative patients
from 18-45 on low risk as compared to the patients who are fasting from midnight?
P – Patients from 18-45 undergoing operation
I – Intake of clear fluid diet
C – Fasting from midnight
O – Reduction in the complications
Search strategy
Keywords search: clear fluid diet; clear liquid diet; post operations; post operative patients;
fasting; effectiveness;.
Actions Search terms Search mode Results Limiters/ Expanders
S5 S1 OR S2 OR S3 OR S4 Boolean/
Phrase
29385
S1 Clear fluid diet Boolean/
Phrase
24,630 Limiters - Linked Full
Text; References
Available; Published
Date: 20130101-
20171231; English
Language; Peer
Reviewed
S3 (MH "Operating
Systems") OR (MH
"Operating Room
Personnel") OR (MH
"Students, Post-RN")
Boolean/
Phrase
4811 Limiters - Linked Full
Text; References
Available; Published
Date: 20130101-
20171231; English
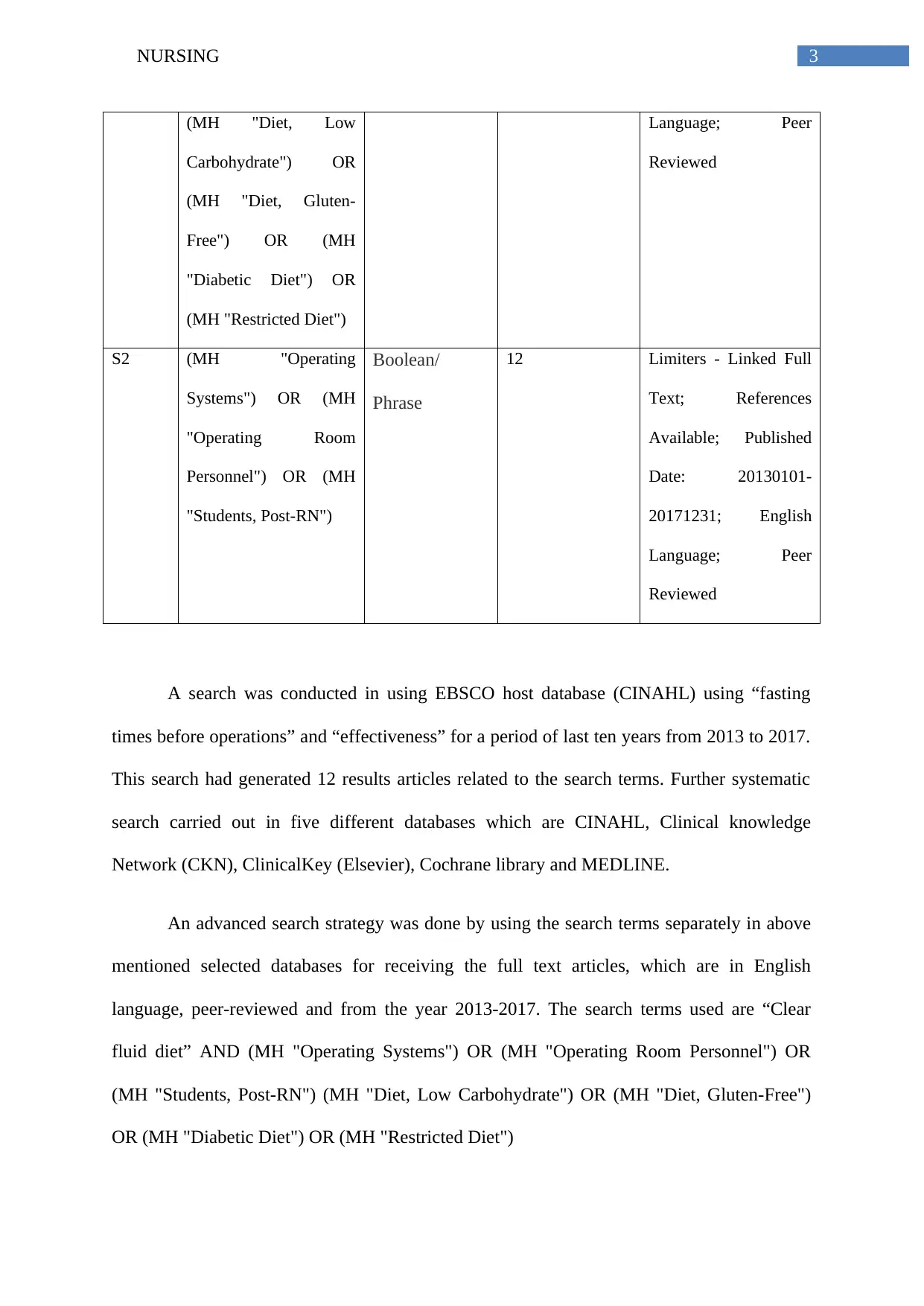
3NURSING
(MH "Diet, Low
Carbohydrate") OR
(MH "Diet, Gluten-
Free") OR (MH
"Diabetic Diet") OR
(MH "Restricted Diet")
Language; Peer
Reviewed
S2 (MH "Operating
Systems") OR (MH
"Operating Room
Personnel") OR (MH
"Students, Post-RN")
Boolean/
Phrase
12 Limiters - Linked Full
Text; References
Available; Published
Date: 20130101-
20171231; English
Language; Peer
Reviewed
A search was conducted in using EBSCO host database (CINAHL) using “fasting
times before operations” and “effectiveness” for a period of last ten years from 2013 to 2017.
This search had generated 12 results articles related to the search terms. Further systematic
search carried out in five different databases which are CINAHL, Clinical knowledge
Network (CKN), ClinicalKey (Elsevier), Cochrane library and MEDLINE.
An advanced search strategy was done by using the search terms separately in above
mentioned selected databases for receiving the full text articles, which are in English
language, peer-reviewed and from the year 2013-2017. The search terms used are “Clear
fluid diet” AND (MH "Operating Systems") OR (MH "Operating Room Personnel") OR
(MH "Students, Post-RN") (MH "Diet, Low Carbohydrate") OR (MH "Diet, Gluten-Free")
OR (MH "Diabetic Diet") OR (MH "Restricted Diet")
(MH "Diet, Low
Carbohydrate") OR
(MH "Diet, Gluten-
Free") OR (MH
"Diabetic Diet") OR
(MH "Restricted Diet")
Language; Peer
Reviewed
S2 (MH "Operating
Systems") OR (MH
"Operating Room
Personnel") OR (MH
"Students, Post-RN")
Boolean/
Phrase
12 Limiters - Linked Full
Text; References
Available; Published
Date: 20130101-
20171231; English
Language; Peer
Reviewed
A search was conducted in using EBSCO host database (CINAHL) using “fasting
times before operations” and “effectiveness” for a period of last ten years from 2013 to 2017.
This search had generated 12 results articles related to the search terms. Further systematic
search carried out in five different databases which are CINAHL, Clinical knowledge
Network (CKN), ClinicalKey (Elsevier), Cochrane library and MEDLINE.
An advanced search strategy was done by using the search terms separately in above
mentioned selected databases for receiving the full text articles, which are in English
language, peer-reviewed and from the year 2013-2017. The search terms used are “Clear
fluid diet” AND (MH "Operating Systems") OR (MH "Operating Room Personnel") OR
(MH "Students, Post-RN") (MH "Diet, Low Carbohydrate") OR (MH "Diet, Gluten-Free")
OR (MH "Diabetic Diet") OR (MH "Restricted Diet")
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4NURSING
(MH "Operating Systems") OR ("Operating Room Personnel") OR ("Students, Post-RN")
The selection of articles also refined to English only academic articles and articles related to a
group of adults aged from 18-45 year of age (Bozzetti & Mariani, 2014).
Electronic searches
The following electronic databases were searched for finding the journals or articles:
The Cochrane Library
Ovid MEDLINE
Ovid EMBASE
EBSCO CINAHL
Critique using CASP Tool
Effect of Early Post Caesarean Feeding on Gastrointestinal Complications
In this article, the authors Adeli et al., (2013) had addressed about the gastrointestinal
complications in the patients of the caesarean section. The authors had clearly addressed that
postoperative complications is the gastro intestinal problems causing ileus, nausea and
vomiting and can cause a longer stay in hospital. 82 women were chosen for this study those
who had gone through caesarean operation. The recruitment criteria of the participants
include those who having a pregnancy, having a caesarean operation, a gestational age
between 38 and 42 weeks. This group was treated with oral fluids after the four hours of
surgery and then followed by regular diet (Crickmer et al., 2016). As they were provided with
the clear fluid diet they did not experienced any complications in their body. In this
investigation none of the mothers were prohibited because of an absence of want for
drinking. Begin of a normal eating regimen in the early bolstering bunch was shorter on the
grounds that the first defecation time in the early-feeding group was not as much as the
(MH "Operating Systems") OR ("Operating Room Personnel") OR ("Students, Post-RN")
The selection of articles also refined to English only academic articles and articles related to a
group of adults aged from 18-45 year of age (Bozzetti & Mariani, 2014).
Electronic searches
The following electronic databases were searched for finding the journals or articles:
The Cochrane Library
Ovid MEDLINE
Ovid EMBASE
EBSCO CINAHL
Critique using CASP Tool
Effect of Early Post Caesarean Feeding on Gastrointestinal Complications
In this article, the authors Adeli et al., (2013) had addressed about the gastrointestinal
complications in the patients of the caesarean section. The authors had clearly addressed that
postoperative complications is the gastro intestinal problems causing ileus, nausea and
vomiting and can cause a longer stay in hospital. 82 women were chosen for this study those
who had gone through caesarean operation. The recruitment criteria of the participants
include those who having a pregnancy, having a caesarean operation, a gestational age
between 38 and 42 weeks. This group was treated with oral fluids after the four hours of
surgery and then followed by regular diet (Crickmer et al., 2016). As they were provided with
the clear fluid diet they did not experienced any complications in their body. In this
investigation none of the mothers were prohibited because of an absence of want for
drinking. Begin of a normal eating regimen in the early bolstering bunch was shorter on the
grounds that the first defecation time in the early-feeding group was not as much as the
5NURSING
customary gathering. Their flatulence was less so moms had a tendency to eat sooner.
Shamaeian Razavi, Malhotra and Teoh et al., additionally presumed that early liquid eating
routine caused early customary eating routine and strong eating routine resilience in a shorter
period (Kular et al., 2014). They did not felt any kind of nausea or vomiting and are able to
stay in the normal position. This study was carried out by randomized controlled trial in
which the participants are divided into two groups and the patients were provided with
written information consent. The trial was done properly on time and they were informed that
both of the groups will be studied as randomized groups. The authors did not disclose the
early feeds to the patients for keeping them blind to the treatment. The groups taken were
similar at the beginning of the trial. The patients were randomizes immediately after surgery:
the early fed group and the traditional group. The early fed group was provided with 30mL of
clear fluid diet. If they can tolerate the fluid intake then the fluid diet is doubled and given to
the patients. For the traditional group the patients were provided with 1.5 litre of fluid
intravenously, if in these patients the bowel sounds are heard then they are allowed for the
intake of clear fluid diet (Lau et al., 2014). The authors had taken the collected the data
through questionnaire interviews and checklist. After this study the authors confirmed that
the patients those who were fed immediately after the operation can be accepted and there are
no significant chances of complications in the body.
Early versus delayed oral fluids and food for reducing complications after major
abdominal gynaecologic surgery
In this article, Charoenkwan and Matovinovic (2014), had discussed about the early
intake of clear liquid diet is good for the post operative patients. The authors described that
the women having gynaecologic surgery are at a risk of complications such as vomiting,
rupturing of the wound and gastrointestinal disruptions. Recuperation of bowel function was
much faster in those with early feeding. There was no distinction in rates of sickness or
customary gathering. Their flatulence was less so moms had a tendency to eat sooner.
Shamaeian Razavi, Malhotra and Teoh et al., additionally presumed that early liquid eating
routine caused early customary eating routine and strong eating routine resilience in a shorter
period (Kular et al., 2014). They did not felt any kind of nausea or vomiting and are able to
stay in the normal position. This study was carried out by randomized controlled trial in
which the participants are divided into two groups and the patients were provided with
written information consent. The trial was done properly on time and they were informed that
both of the groups will be studied as randomized groups. The authors did not disclose the
early feeds to the patients for keeping them blind to the treatment. The groups taken were
similar at the beginning of the trial. The patients were randomizes immediately after surgery:
the early fed group and the traditional group. The early fed group was provided with 30mL of
clear fluid diet. If they can tolerate the fluid intake then the fluid diet is doubled and given to
the patients. For the traditional group the patients were provided with 1.5 litre of fluid
intravenously, if in these patients the bowel sounds are heard then they are allowed for the
intake of clear fluid diet (Lau et al., 2014). The authors had taken the collected the data
through questionnaire interviews and checklist. After this study the authors confirmed that
the patients those who were fed immediately after the operation can be accepted and there are
no significant chances of complications in the body.
Early versus delayed oral fluids and food for reducing complications after major
abdominal gynaecologic surgery
In this article, Charoenkwan and Matovinovic (2014), had discussed about the early
intake of clear liquid diet is good for the post operative patients. The authors described that
the women having gynaecologic surgery are at a risk of complications such as vomiting,
rupturing of the wound and gastrointestinal disruptions. Recuperation of bowel function was
much faster in those with early feeding. There was no distinction in rates of sickness or
6NURSING
retching, stomach distension, requirement for a postoperative nasogastric tube or time to first
solid discharge, yet early sustaining was related with a shorter time to gut sounds and
beginning of gas (D’Ugo et al., 2014). The early bolstering bunch continued a strong eating
regimen 1½ days sooner than those have postponed encouraging and the clinic stay was one
day shorter. Additionally, the early nourishing gathering was happier with the bolstering plan,
albeit just a single report revealed this.
Early feeding seemed safe, without expanded postoperative confusions and with less
irresistible inconveniences generally speaking. The authors had done a randomized controlled
trial study in which they compared the effect of the intake of fluids for the post operative
patients according to the time (Macarthur et al., 2015). For this study the authors had taken
some papers and accepted the details for oral intake of liquid within 24 hours of post surgery.
They then examine the data using mean difference and tables. The evidence that were
collected was of moderate quality. The limitations of the study were lack of blind
examination which can influence the results and give some possible subjective outcomes such
as self-reported symptoms or quality of life (Moss et al., 2015). Thus it can be suggested that
eating and drinking before and after the surgery is safe and can help in reducing the length of
the stay in hospital.
The meanings of right on time and deferred nourishing timetable fluctuated among
included investigations in that:
For the early sustaining gathering, the eating routine calendar connected in Amatyakul
2001, Minig 2009a, and Minig 2009b, had all the earmarks of being more forceful. In
Amatyakul 2001, ladies were begun on a delicate eating routine in the morning of the main
postoperative day and continued to a standard strong eating regimen on the second
postoperative day. In Minig 2009a and Minig 2009b, members were offered fluids, mineral
retching, stomach distension, requirement for a postoperative nasogastric tube or time to first
solid discharge, yet early sustaining was related with a shorter time to gut sounds and
beginning of gas (D’Ugo et al., 2014). The early bolstering bunch continued a strong eating
regimen 1½ days sooner than those have postponed encouraging and the clinic stay was one
day shorter. Additionally, the early nourishing gathering was happier with the bolstering plan,
albeit just a single report revealed this.
Early feeding seemed safe, without expanded postoperative confusions and with less
irresistible inconveniences generally speaking. The authors had done a randomized controlled
trial study in which they compared the effect of the intake of fluids for the post operative
patients according to the time (Macarthur et al., 2015). For this study the authors had taken
some papers and accepted the details for oral intake of liquid within 24 hours of post surgery.
They then examine the data using mean difference and tables. The evidence that were
collected was of moderate quality. The limitations of the study were lack of blind
examination which can influence the results and give some possible subjective outcomes such
as self-reported symptoms or quality of life (Moss et al., 2015). Thus it can be suggested that
eating and drinking before and after the surgery is safe and can help in reducing the length of
the stay in hospital.
The meanings of right on time and deferred nourishing timetable fluctuated among
included investigations in that:
For the early sustaining gathering, the eating routine calendar connected in Amatyakul
2001, Minig 2009a, and Minig 2009b, had all the earmarks of being more forceful. In
Amatyakul 2001, ladies were begun on a delicate eating routine in the morning of the main
postoperative day and continued to a standard strong eating regimen on the second
postoperative day. In Minig 2009a and Minig 2009b, members were offered fluids, mineral
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7NURSING
water (still), tea, chamomile mixture, or squeezed apple amid the initial 24 hours. In the event
that no sickness and heaving, a consistent eating regimen of bubbled or flame broiled
hamburger, chicken, or fish was given beginning on day 1 and proceeded for the whole clinic
remain. In the rest of the examinations the members started an unmistakable fluid eating
routine on the main postoperative day and after that best in class to a normal eating regimen
as endured (Panis et al., 2014).
For the postponed nourishing gathering, the calendar utilized as a part of Amatyakul
2001 was marginally more traditionalist than others. After indications of the arrival of entrail
work, ladies were permitted to have just tastes of water before progressing to a fluid eating
regimen at night of that day, while in alternate examinations ladies were promptly begun on a
fluid eating regimen after the nearness of those signs (Nguyen et al., 2016) . We take note of
that the criteria for an arrival of gut work were comparative in all investigations.
Results
Steed 2002 announced the occurrence of postoperative ileus, which was characterized
as more than two scenes of retching of no less than 100 ml each inside a 24-hour day and age,
with related stomach distension and no entrail sounds. Alternate examinations in a
roundabout way evaluated the event of postoperative ileus through the frequency of related
postoperative gastrointestinal bleakness (Rey, 2013). Pearl 1998 revealed the rate of
queasiness, regurgitating, stomach distension, and nasogastric tube utilize. Amatyakul 2001
announced the rate of spewing and stomach distension. Minig 2009 detailed force of stomach
agony and nearness of queasiness and emesis. With respect to on postoperative time interims
to the arrival of entrail work, time to the nearness of gut sound was accounted for in Pearl
1998,. Time to the principal entry of flatus and time to the start or resistance of strong
nourishment were accounted for in Pearl 1998, Amatyakul 2001, Minig 2009a, and Minig
water (still), tea, chamomile mixture, or squeezed apple amid the initial 24 hours. In the event
that no sickness and heaving, a consistent eating regimen of bubbled or flame broiled
hamburger, chicken, or fish was given beginning on day 1 and proceeded for the whole clinic
remain. In the rest of the examinations the members started an unmistakable fluid eating
routine on the main postoperative day and after that best in class to a normal eating regimen
as endured (Panis et al., 2014).
For the postponed nourishing gathering, the calendar utilized as a part of Amatyakul
2001 was marginally more traditionalist than others. After indications of the arrival of entrail
work, ladies were permitted to have just tastes of water before progressing to a fluid eating
regimen at night of that day, while in alternate examinations ladies were promptly begun on a
fluid eating regimen after the nearness of those signs (Nguyen et al., 2016) . We take note of
that the criteria for an arrival of gut work were comparative in all investigations.
Results
Steed 2002 announced the occurrence of postoperative ileus, which was characterized
as more than two scenes of retching of no less than 100 ml each inside a 24-hour day and age,
with related stomach distension and no entrail sounds. Alternate examinations in a
roundabout way evaluated the event of postoperative ileus through the frequency of related
postoperative gastrointestinal bleakness (Rey, 2013). Pearl 1998 revealed the rate of
queasiness, regurgitating, stomach distension, and nasogastric tube utilize. Amatyakul 2001
announced the rate of spewing and stomach distension. Minig 2009 detailed force of stomach
agony and nearness of queasiness and emesis. With respect to on postoperative time interims
to the arrival of entrail work, time to the nearness of gut sound was accounted for in Pearl
1998,. Time to the principal entry of flatus and time to the start or resistance of strong
nourishment were accounted for in Pearl 1998, Amatyakul 2001, Minig 2009a, and Minig
8NURSING
2009b. Amatyakul 2001, Minig 2009a, and Minig 2009b revealed time to the primary entry
of stool.
An Exploratory Study: Clinical Dietitians Do Not View the Full Liquid Diet as Best
Practice for the Post-operative Patient.
The clear liquid diet has been utilized as a transitional eating regimen for as long as
100 years. A full fluid eating routine contains nourishments that are fluid, or condense at
room temperature, and are normally recommended to patients postoperatively in the healing
facility setting. The present dietary progressions in numerous clinical settings incorporate
changing from nil per Os (NPO) to an unmistakable fluid eating routine, to a full fluid eating
regimen and to a standard eating routine or eating routine as endured preceding release
(Sierzega et al., 2015). The full fluid eating regimen contains for the most part drain and
drain based items including pudding, frozen yogurt, oats, cream of wheat, cream based soups,
and some other fluid nourishments permitted on the reasonable fluid eating regimen. The
utilization of the full fluid eating routine is not prescribed for more than one to three days
without extra supplements recommended by enrolled dietitians (RDs).
The full fluid eating routine has been utilized as a transitional eating routine for as
long as 100 years. A full fluid eating routine contains nourishments that are fluid, or
condense at room temperature, and are regularly recommended to patients postoperatively in
the doctor's facility setting. The present dietary progressions in numerous clinical settings
incorporate changing from nil per Os (NPO) to an unmistakable fluid eating routine, to a full
fluid eating regimen and to a customary eating regimen or eating regimen as endured
preceding release (Mills et al., 2015). The full fluid eating regimen contains fundamentally
drain and drain based items including pudding, frozen yogurt, oats, cream of wheat, cream
based soups, and some other fluid nourishments permitted on the unmistakable fluid eating
2009b. Amatyakul 2001, Minig 2009a, and Minig 2009b revealed time to the primary entry
of stool.
An Exploratory Study: Clinical Dietitians Do Not View the Full Liquid Diet as Best
Practice for the Post-operative Patient.
The clear liquid diet has been utilized as a transitional eating regimen for as long as
100 years. A full fluid eating routine contains nourishments that are fluid, or condense at
room temperature, and are normally recommended to patients postoperatively in the healing
facility setting. The present dietary progressions in numerous clinical settings incorporate
changing from nil per Os (NPO) to an unmistakable fluid eating routine, to a full fluid eating
regimen and to a standard eating routine or eating routine as endured preceding release
(Sierzega et al., 2015). The full fluid eating regimen contains for the most part drain and
drain based items including pudding, frozen yogurt, oats, cream of wheat, cream based soups,
and some other fluid nourishments permitted on the reasonable fluid eating regimen. The
utilization of the full fluid eating routine is not prescribed for more than one to three days
without extra supplements recommended by enrolled dietitians (RDs).
The full fluid eating routine has been utilized as a transitional eating routine for as
long as 100 years. A full fluid eating routine contains nourishments that are fluid, or
condense at room temperature, and are regularly recommended to patients postoperatively in
the doctor's facility setting. The present dietary progressions in numerous clinical settings
incorporate changing from nil per Os (NPO) to an unmistakable fluid eating routine, to a full
fluid eating regimen and to a customary eating regimen or eating regimen as endured
preceding release (Mills et al., 2015). The full fluid eating regimen contains fundamentally
drain and drain based items including pudding, frozen yogurt, oats, cream of wheat, cream
based soups, and some other fluid nourishments permitted on the unmistakable fluid eating
9NURSING
routine. The utilization of the full fluid eating routine is not prescribed for more than one to
three days without extra supplements recommended by registered dietitians (RDs).
De witt, (2015) done a qualitative study which includes the present advancement in
diet Inna clinical setting that includes a transition from nil by mouth to a clear liquid diet,
which is then passed on to full liquid diet and regular diet. In this paper the author had an
electronic survey using software the survey results were then analysed using the statistical
formulas. In the methodology part the survey was done in the Academy of nutrition and
dietetics practice group was selected for the study The format for the survey was adopted
from a survey which was created by Sofia young and tennis and then in 2009. The survey
was then sent to 1914 registered dietician. The information from the software where removed
before the analyzation of the data and it was anonymously maintained. Out of the 1949
surveys delivered 25 responses were collected and the results were found that full liquid that
provide sufficient energy and keep so patient hydrated but it is only appropriate for short term
use and is harmful for the patients having diabetes.
Benefits of post-operative oral fluid supplementation in gastrointestinal surgery
patients: A systematic review of clinical trials
The objective of this paper is to perform trials with examine the oral fluid
supplementation in postoperative patients. Database searches (MEDLINE, BIOSIS,
EMBASE, Cochrane Trials, Cinahl, and CAB), searches of reference lists of relevant papers,
and expert referral were used to identify prospective randomized controlled clinical trials.
The following terms were used to locate articles: “oral’’ or “enteral’’ and “postoperative
care’’ or “post-surgical’’ and “fluids’’ or “milk fluids’’ or “dietary fluids’’ or “dietary
supplements’’ or “nutritional supplements’’.
routine. The utilization of the full fluid eating routine is not prescribed for more than one to
three days without extra supplements recommended by registered dietitians (RDs).
De witt, (2015) done a qualitative study which includes the present advancement in
diet Inna clinical setting that includes a transition from nil by mouth to a clear liquid diet,
which is then passed on to full liquid diet and regular diet. In this paper the author had an
electronic survey using software the survey results were then analysed using the statistical
formulas. In the methodology part the survey was done in the Academy of nutrition and
dietetics practice group was selected for the study The format for the survey was adopted
from a survey which was created by Sofia young and tennis and then in 2009. The survey
was then sent to 1914 registered dietician. The information from the software where removed
before the analyzation of the data and it was anonymously maintained. Out of the 1949
surveys delivered 25 responses were collected and the results were found that full liquid that
provide sufficient energy and keep so patient hydrated but it is only appropriate for short term
use and is harmful for the patients having diabetes.
Benefits of post-operative oral fluid supplementation in gastrointestinal surgery
patients: A systematic review of clinical trials
The objective of this paper is to perform trials with examine the oral fluid
supplementation in postoperative patients. Database searches (MEDLINE, BIOSIS,
EMBASE, Cochrane Trials, Cinahl, and CAB), searches of reference lists of relevant papers,
and expert referral were used to identify prospective randomized controlled clinical trials.
The following terms were used to locate articles: “oral’’ or “enteral’’ and “postoperative
care’’ or “post-surgical’’ and “fluids’’ or “milk fluids’’ or “dietary fluids’’ or “dietary
supplements’’ or “nutritional supplements’’.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
10NURSING
In this paper the clinical trials was studied from Publications between 1990 and 2014.
The data of the studies were evaluated using qualitative assessment tool and the results were
interpreted.
The clinical trials contains a randomised control study were examined where the oral
dietary supplementation for human gastrointestinal Operations. In this study the author
excluded the papers which involved in iteration or did not specify the amount of fluid
supplement it or patients who has supplemented by the time before operation only or not
published in English (Matsumura et al., 2015).
Data were collected by using the trials in which the inclusion criteria were
independently analysed and the discrepancies were resolved. The authors read the paper and
identify that the risk of danger in case of postoperative gastrointestinal surgery. Sample taken
gear range from 40 to 101. A total number of 529 patients were involved among which 262
had an intervention participles overtaken are the patients involved in gastrointestinal surgery.
The nutritional status of these patients before the operation was different which some of them
suffering from malnourishment. The intervention provided to the treatment group patients
that they received a post of the dove nutritional supplement in addition with their normal diet.
While the control groups we are provided with the normal diet (Matsumura et al., 2015).
According to the studies it can be concluded that the Clear fluid diet have positive effects in
terms of the recovery of a patient with the gastrointestinal surgery rather than the patient w
who is being provided with a normal diet. In this way, examination of the qualified reports
was hazardous. Constraints incorporated the way that protein and vitality content in TG
supplements were not proportionate in a large portion of the investigations. To be sure, just
the investigation by Saluja et al. depicted utilizing a settled measure of supplement for day by
day utilization, while the rest of the examinations took after a "not obligatory" approach.
Apparently, the last approach best mirrors "genuine living" clinical situations, nonetheless it
In this paper the clinical trials was studied from Publications between 1990 and 2014.
The data of the studies were evaluated using qualitative assessment tool and the results were
interpreted.
The clinical trials contains a randomised control study were examined where the oral
dietary supplementation for human gastrointestinal Operations. In this study the author
excluded the papers which involved in iteration or did not specify the amount of fluid
supplement it or patients who has supplemented by the time before operation only or not
published in English (Matsumura et al., 2015).
Data were collected by using the trials in which the inclusion criteria were
independently analysed and the discrepancies were resolved. The authors read the paper and
identify that the risk of danger in case of postoperative gastrointestinal surgery. Sample taken
gear range from 40 to 101. A total number of 529 patients were involved among which 262
had an intervention participles overtaken are the patients involved in gastrointestinal surgery.
The nutritional status of these patients before the operation was different which some of them
suffering from malnourishment. The intervention provided to the treatment group patients
that they received a post of the dove nutritional supplement in addition with their normal diet.
While the control groups we are provided with the normal diet (Matsumura et al., 2015).
According to the studies it can be concluded that the Clear fluid diet have positive effects in
terms of the recovery of a patient with the gastrointestinal surgery rather than the patient w
who is being provided with a normal diet. In this way, examination of the qualified reports
was hazardous. Constraints incorporated the way that protein and vitality content in TG
supplements were not proportionate in a large portion of the investigations. To be sure, just
the investigation by Saluja et al. depicted utilizing a settled measure of supplement for day by
day utilization, while the rest of the examinations took after a "not obligatory" approach.
Apparently, the last approach best mirrors "genuine living" clinical situations, nonetheless it
11NURSING
makes recognizing the genuine impact of protein supplementation troublesome. Moreover,
the attributes of the patient associates were not proportionate between thinks about, jumbling
between ponder examinations. For instance, the examination by Saluja et al occurred in Delhi
and incorporated a more prominent extent of crisis surgery patients, and patients with
tuberculosis, contrasted and the non-rising techniques portrayed in the Western European
reports. In addition, insufficient line up time with control and TGs was basic crosswise over
investigations, with some danger of inclination related with absence of blinding of members,
carers and assessors (Vanhauwaert et al., 2015). The energy of the investigations was
frequently too little, with one creator yielding remarkably that "numbers were too little for
significant factual analysis" and goal to treat examination was not utilized as a part of any of
the examinations. At long last, the latest of the qualified trials found in our inquiries was
distributed in 2004, apparently reflecting either a move in intrigue far from oral admission for
enteral and parenteral nourishment in this populace or an accentuation set on conventional
eating routine without supplement.
Feasibility and Outcomes of Early Oral Feeding After Total Gastrectomy for Cancer
The aim of this paper is to analyse the application of providing oral liquid diet before
the operation to a patient. In this study the medical records of 353 patients were analysed
who went through gastrectomy. These patients were provided with clear liquid diet on the
day of operation which is gradually followed by the solid diet before the day of operation. In
the methodology part the author has described that the database of all the patients who were
treated with gastric cancer (Melicharkova et al., 2013). Including the demographics details of
the surgical procedures and pathophysiological parameters were collected. Study was Limited
period of 2006 to 2012. All the procedures were carried out under the supervision of senior
surgeons who has treated almost 100 patients with gastric surgery. Initially the patient were
provided with oral friends on the postoperative before that was followed by a soft that on the
makes recognizing the genuine impact of protein supplementation troublesome. Moreover,
the attributes of the patient associates were not proportionate between thinks about, jumbling
between ponder examinations. For instance, the examination by Saluja et al occurred in Delhi
and incorporated a more prominent extent of crisis surgery patients, and patients with
tuberculosis, contrasted and the non-rising techniques portrayed in the Western European
reports. In addition, insufficient line up time with control and TGs was basic crosswise over
investigations, with some danger of inclination related with absence of blinding of members,
carers and assessors (Vanhauwaert et al., 2015). The energy of the investigations was
frequently too little, with one creator yielding remarkably that "numbers were too little for
significant factual analysis" and goal to treat examination was not utilized as a part of any of
the examinations. At long last, the latest of the qualified trials found in our inquiries was
distributed in 2004, apparently reflecting either a move in intrigue far from oral admission for
enteral and parenteral nourishment in this populace or an accentuation set on conventional
eating routine without supplement.
Feasibility and Outcomes of Early Oral Feeding After Total Gastrectomy for Cancer
The aim of this paper is to analyse the application of providing oral liquid diet before
the operation to a patient. In this study the medical records of 353 patients were analysed
who went through gastrectomy. These patients were provided with clear liquid diet on the
day of operation which is gradually followed by the solid diet before the day of operation. In
the methodology part the author has described that the database of all the patients who were
treated with gastric cancer (Melicharkova et al., 2013). Including the demographics details of
the surgical procedures and pathophysiological parameters were collected. Study was Limited
period of 2006 to 2012. All the procedures were carried out under the supervision of senior
surgeons who has treated almost 100 patients with gastric surgery. Initially the patient were
provided with oral friends on the postoperative before that was followed by a soft that on the
12NURSING
5 and from there a regular solid. Early provision of oral diet did not increase postoperative
morbidity, including compromised integrity of an esophagojejunal anastomosis, in this
homogenous population of Western patients undergoing total gastrectomy for cancer.
Therefore, such nutritional intervention can be safely adapted to accelerated patient recovery
protocols. Because of the disadvantages characteristic in companion thinks about, this report
has a few restrictions (Stolpman et al., 2015). The investigation was not arranged as a formal
ERAS convention, and along these lines, not all components of the perioperative pathway
could be institutionalized, e.g., length of skin cut or early ambulation separate. In spite of the
way that every one of the information were gathered tentatively utilizing institutionalized
structures, the absence of randomization and review examination is possibly connected with
choice predisposition among patients treated in a high volume focus as proposed by low rates
of anastomotic disappointments.
5 and from there a regular solid. Early provision of oral diet did not increase postoperative
morbidity, including compromised integrity of an esophagojejunal anastomosis, in this
homogenous population of Western patients undergoing total gastrectomy for cancer.
Therefore, such nutritional intervention can be safely adapted to accelerated patient recovery
protocols. Because of the disadvantages characteristic in companion thinks about, this report
has a few restrictions (Stolpman et al., 2015). The investigation was not arranged as a formal
ERAS convention, and along these lines, not all components of the perioperative pathway
could be institutionalized, e.g., length of skin cut or early ambulation separate. In spite of the
way that every one of the information were gathered tentatively utilizing institutionalized
structures, the absence of randomization and review examination is possibly connected with
choice predisposition among patients treated in a high volume focus as proposed by low rates
of anastomotic disappointments.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
13NURSING
References
Adeli, M., Razmjoo, N., Tara, F., & Ebrahimzade, S. (2013). Effect of Early Post Cesarean
Feeding on Gastrointestinal Complications. Nursing and Midwifery Studies, 2(2),
176–181.
An Exploratory Study: Clinical Dietitians Do Not View the Full Liquid Diet as Best Practice
for the Post-operative Patient.
Bozzetti, F., & Mariani, L. (2014). Perioperative nutritional support of patients undergoing
pancreatic surgery in the age of ERAS. Nutrition, 30(11), 1267-1271.
Charoenkwan, K., & Matovinovic, E. (2014). Early versus delayed oral fluids and food for
reducing complications after major abdominal gynaecologic surgery. The Cochrane
Library.
Crickmer, M., Dunne, C. P., O’Regan, A., Coffey, J. C., & Dunne, S. S. (2016). Benefits of
post-operative oral protein supplementation in gastrointestinal surgery patients: A
systematic review of clinical trials. World Journal of Gastrointestinal Surgery, 8(7),
521–532. http://doi.org/10.4240/wjgs.v8.i7.521
D’Ugo, S., Gentileschi, P., Benavoli, D., Cerci, M., Gaspari, A., Berta, R. D., ... & Soricelli,
E. (2014). Comparative use of different techniques for leak and bleeding prevention
during laparoscopic sleeve gastrectomy: a multicenter study. Surgery for Obesity and
Related Diseases, 10(3), 450-454.
References
Adeli, M., Razmjoo, N., Tara, F., & Ebrahimzade, S. (2013). Effect of Early Post Cesarean
Feeding on Gastrointestinal Complications. Nursing and Midwifery Studies, 2(2),
176–181.
An Exploratory Study: Clinical Dietitians Do Not View the Full Liquid Diet as Best Practice
for the Post-operative Patient.
Bozzetti, F., & Mariani, L. (2014). Perioperative nutritional support of patients undergoing
pancreatic surgery in the age of ERAS. Nutrition, 30(11), 1267-1271.
Charoenkwan, K., & Matovinovic, E. (2014). Early versus delayed oral fluids and food for
reducing complications after major abdominal gynaecologic surgery. The Cochrane
Library.
Crickmer, M., Dunne, C. P., O’Regan, A., Coffey, J. C., & Dunne, S. S. (2016). Benefits of
post-operative oral protein supplementation in gastrointestinal surgery patients: A
systematic review of clinical trials. World Journal of Gastrointestinal Surgery, 8(7),
521–532. http://doi.org/10.4240/wjgs.v8.i7.521
D’Ugo, S., Gentileschi, P., Benavoli, D., Cerci, M., Gaspari, A., Berta, R. D., ... & Soricelli,
E. (2014). Comparative use of different techniques for leak and bleeding prevention
during laparoscopic sleeve gastrectomy: a multicenter study. Surgery for Obesity and
Related Diseases, 10(3), 450-454.
14NURSING
Hookey, L., Louw, J., Wiepjes, M., Rubinger, N., Van Weyenberg, S., Day, A. G., &
Paterson, W. (2017). Lack of benefit of active preparation compared with a clear
fluid–only diet in small-bowel visualization for video capsule endoscopy: results of a
randomized, blinded, controlled trial. Gastrointestinal endoscopy, 85(1), 187-193.
Kular, K. S., Manchanda, N., & Rutledge, R. (2014). Analysis of the five-year outcomes of
sleeve gastrectomy and mini gastric bypass: a report from the Indian sub-continent.
Obesity surgery, 24(10), 1724-1728.
Lau, C., Phillips, E., Bresee, C., & Fleshner, P. (2014). Early use of low residue diet is
superior to clear liquid diet after elective colorectal surgery: a randomized controlled
trial. Annals of surgery, 260(4), 641-649.
Macarthur, K. L., Leszczynski, A., Quatromoni, P. A., & Jacobson, B. C. (2015). Su1545 A
Multi-Cultural Approach to Dietary Restrictions in the Days Preceding Colonoscopy.
Gastrointestinal Endoscopy, 81(5), AB322-AB323.
Matsumura, T., Arai, M., Okimoto, K., Maruoka, D., Minemura, S., Ishigami, H., ... &
Yokosuka, O. (2015). Su1684 A Randomized Controlled Trial Comparing a
Prepackaged Low-Residue Diet Versus a Restricted Diet for Colonoscopy
Preparation. Gastrointestinal Endoscopy, 81(5), AB378.
Melicharkova, A., Flemming, J., Vanner, S., & Hookey, L. (2013). A low-residue breakfast
improves patient tolerance without impacting quality of low-volume colon cleansing
prior to colonoscopy: a randomized trial. The American journal of gastroenterology,
108(10), 1551.
Hookey, L., Louw, J., Wiepjes, M., Rubinger, N., Van Weyenberg, S., Day, A. G., &
Paterson, W. (2017). Lack of benefit of active preparation compared with a clear
fluid–only diet in small-bowel visualization for video capsule endoscopy: results of a
randomized, blinded, controlled trial. Gastrointestinal endoscopy, 85(1), 187-193.
Kular, K. S., Manchanda, N., & Rutledge, R. (2014). Analysis of the five-year outcomes of
sleeve gastrectomy and mini gastric bypass: a report from the Indian sub-continent.
Obesity surgery, 24(10), 1724-1728.
Lau, C., Phillips, E., Bresee, C., & Fleshner, P. (2014). Early use of low residue diet is
superior to clear liquid diet after elective colorectal surgery: a randomized controlled
trial. Annals of surgery, 260(4), 641-649.
Macarthur, K. L., Leszczynski, A., Quatromoni, P. A., & Jacobson, B. C. (2015). Su1545 A
Multi-Cultural Approach to Dietary Restrictions in the Days Preceding Colonoscopy.
Gastrointestinal Endoscopy, 81(5), AB322-AB323.
Matsumura, T., Arai, M., Okimoto, K., Maruoka, D., Minemura, S., Ishigami, H., ... &
Yokosuka, O. (2015). Su1684 A Randomized Controlled Trial Comparing a
Prepackaged Low-Residue Diet Versus a Restricted Diet for Colonoscopy
Preparation. Gastrointestinal Endoscopy, 81(5), AB378.
Melicharkova, A., Flemming, J., Vanner, S., & Hookey, L. (2013). A low-residue breakfast
improves patient tolerance without impacting quality of low-volume colon cleansing
prior to colonoscopy: a randomized trial. The American journal of gastroenterology,
108(10), 1551.
15NURSING
Mills, C. D., Swaine, A., Mccamley, C., & Swan, M. P. (2015). Su1686 The impact of carbon
dioxide insufflation on colonic polyp and adenoma detection rate. Gastrointestinal
Endoscopy, 81(5), AB378.
Moss, A., Williams, S. J., Hourigan, L. F., Brown, G., Tam, W., Singh, R., ... & Bourke, M.
J. (2015). Long-term adenoma recurrence following wide-field endoscopic mucosal
resection (WF-EMR) for advanced colonic mucosal neoplasia is infrequent: results
and risk factors in 1000 cases from the Australian Colonic EMR (ACE) study. Gut,
64(1), 57-65.
Nguyen, D. L., Jamal, M. M., Nguyen, E. T., Puli, S. R., & Bechtold, M. L. (2016). Low-
residue versus clear liquid diet before colonoscopy: a meta-analysis of randomized,
controlled trials. Gastrointestinal endoscopy, 83(3), 499-507.
Panis, Y., Lefevre, J. H., Senéjoux, A., Meurette, G., Zeitoun, J. D., Simon, M., &
Siproudhis, L. (2014). Early use of low residue diet is superior to clear liquid diet
after elective colorectal surgery. A randomized controlled trial. Côlon & Rectum,
8(4), 240-250.
Rey, J. F. (2013). The future of capsule endoscopy. The Keio journal of medicine, 62(2), 41-
46.
Sierzega, M., Choruz, R., Pietruszka, S., Kulig, P., Kolodziejczyk, P., & Kulig, J. (2015).
Feasibility and Outcomes of Early Oral Feeding After Total Gastrectomy for Cancer.
Journal of Gastrointestinal Surgery, 19(3), 473–479. http://doi.org/10.1007/s11605-
014-2720-0
Stolpman, D., Shaw, M., Solem, C., Eastlick, D., Mullen, D., & Adlis, S. (2013). 1024
Randomized Controlled Trial Comparing a Low Residue Diet vs. Clear Liquids in
Mills, C. D., Swaine, A., Mccamley, C., & Swan, M. P. (2015). Su1686 The impact of carbon
dioxide insufflation on colonic polyp and adenoma detection rate. Gastrointestinal
Endoscopy, 81(5), AB378.
Moss, A., Williams, S. J., Hourigan, L. F., Brown, G., Tam, W., Singh, R., ... & Bourke, M.
J. (2015). Long-term adenoma recurrence following wide-field endoscopic mucosal
resection (WF-EMR) for advanced colonic mucosal neoplasia is infrequent: results
and risk factors in 1000 cases from the Australian Colonic EMR (ACE) study. Gut,
64(1), 57-65.
Nguyen, D. L., Jamal, M. M., Nguyen, E. T., Puli, S. R., & Bechtold, M. L. (2016). Low-
residue versus clear liquid diet before colonoscopy: a meta-analysis of randomized,
controlled trials. Gastrointestinal endoscopy, 83(3), 499-507.
Panis, Y., Lefevre, J. H., Senéjoux, A., Meurette, G., Zeitoun, J. D., Simon, M., &
Siproudhis, L. (2014). Early use of low residue diet is superior to clear liquid diet
after elective colorectal surgery. A randomized controlled trial. Côlon & Rectum,
8(4), 240-250.
Rey, J. F. (2013). The future of capsule endoscopy. The Keio journal of medicine, 62(2), 41-
46.
Sierzega, M., Choruz, R., Pietruszka, S., Kulig, P., Kolodziejczyk, P., & Kulig, J. (2015).
Feasibility and Outcomes of Early Oral Feeding After Total Gastrectomy for Cancer.
Journal of Gastrointestinal Surgery, 19(3), 473–479. http://doi.org/10.1007/s11605-
014-2720-0
Stolpman, D., Shaw, M., Solem, C., Eastlick, D., Mullen, D., & Adlis, S. (2013). 1024
Randomized Controlled Trial Comparing a Low Residue Diet vs. Clear Liquids in
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.

16NURSING
Patients Receiving a Reduced-Volume Oral Sulfate Solution for Colonoscopy
Preparation. Gastroenterology, 144(5), S-191.
Vanhauwaert, E., Matthys, C., Verdonck, L., & De Preter, V. (2015). Low-residue and low-
fiber diets in gastrointestinal disease management. Advances in Nutrition: An
International Review Journal, 6(6), 820-827.
Patients Receiving a Reduced-Volume Oral Sulfate Solution for Colonoscopy
Preparation. Gastroenterology, 144(5), S-191.
Vanhauwaert, E., Matthys, C., Verdonck, L., & De Preter, V. (2015). Low-residue and low-
fiber diets in gastrointestinal disease management. Advances in Nutrition: An
International Review Journal, 6(6), 820-827.
1 out of 17
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.