Case Study: Facilitating Workplace Learning in Nursing - Hong Kong
VerifiedAdded on 2023/01/18
|21
|5673
|78
Case Study
AI Summary
This case study examines a student's experience in facilitating workplace learning for an undergraduate nursing student in a Hong Kong hospital. The essay reflects on the preparation, delivery, and lessons learned during the facilitation process, highlighting the importance of understanding the learner's needs, providing support, and building a trusting professional relationship. The study also discusses the challenges encountered, such as balancing teaching goals with the learner's personal needs. The case study emphasizes the significance of student-centered teaching, cultural considerations, and the role of the facilitator in creating a supportive learning environment. The student also provides a plan for future facilitation, emphasizing the importance of an introductory session to understand the learner's background and potential challenges. The assignment concludes with a discussion on achieving student-centered teaching, the role of culture, and the importance of respect in the learning process. The case study underscores the multifaceted nature of workplace learning and the crucial role of the facilitator in fostering effective learning outcomes.

Facilitating Workplace Learning 1
Facilitating Workplace Learning
By (Name of Student)
Institution
City/State
Course Number
Professor
Date
Facilitating Workplace Learning
By (Name of Student)
Institution
City/State
Course Number
Professor
Date
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Facilitating Workplace Learning 2
Table of Contents
Part 1: Essay....................................................................................................................................3
Introduction......................................................................................................................................3
Section 1: Reflection....................................................................................................................3
Preparation and Delivery.........................................................................................................3
Lessons from Observed Session..............................................................................................4
Summary of Learning and Future Implication........................................................................7
Section 2: Discussion and Debate................................................................................................8
Achieving Student-Centered Teaching....................................................................................8
Culture of the Organization and Learning Outcomes............................................................10
Respecting Learners: Relationship with Student Nurses.......................................................11
Conclusion.....................................................................................................................................12
Appendix........................................................................................................................................14
Part 2: Plan for Facilitating Workplace Learning..........................................................................14
References......................................................................................................................................16
Table of Contents
Part 1: Essay....................................................................................................................................3
Introduction......................................................................................................................................3
Section 1: Reflection....................................................................................................................3
Preparation and Delivery.........................................................................................................3
Lessons from Observed Session..............................................................................................4
Summary of Learning and Future Implication........................................................................7
Section 2: Discussion and Debate................................................................................................8
Achieving Student-Centered Teaching....................................................................................8
Culture of the Organization and Learning Outcomes............................................................10
Respecting Learners: Relationship with Student Nurses.......................................................11
Conclusion.....................................................................................................................................12
Appendix........................................................................................................................................14
Part 2: Plan for Facilitating Workplace Learning..........................................................................14
References......................................................................................................................................16

Facilitating Workplace Learning 3
Facilitating Workplace Learning
Part 1: Essay
Introduction
The clinical environment is characterized by constant learning as part of quality
improvement in care and the training of new professionals. Workplace learning in nursing is an
essential part of professional development and skill enhancement among nursing students. Over
the years, scholars have pointed out the role that learning plays in a clinical environment (Adib-
Hajbaghery, MirBagher, and Heidari, 2012). Experienced nurses and other healthcare
professionals have played a significant role in improving the process of workplace learning by
adhering to available guidelines and principles. Undergraduate learners depend on workplace
learning in nursing to get their first-hand experiences and enhance their skills and exposure
(Antohe et al., 2016). The success of their learning depends on the effectiveness of the process
and the approach taken by the facilitator. Workplace learning entails different dimensions such
as ethics, the environment, guidelines, and culture, which should be considered by learning
facilitators to positively impact the outcome of workplace learning (Blomberg et al., 2014). This
paper provides a reflection on workplace learning facilitation experience and outlines key
concepts do consider as a facilitator.
Section 1: Reflection
Preparation and Delivery
In this workplace learning experience, the learner was an undergraduate nursing student
assigned to a local hospital in Hong Kong as part of the regular training program for nurses.
Nurses undergo this process as part of their professional development. The learner did not have
Facilitating Workplace Learning
Part 1: Essay
Introduction
The clinical environment is characterized by constant learning as part of quality
improvement in care and the training of new professionals. Workplace learning in nursing is an
essential part of professional development and skill enhancement among nursing students. Over
the years, scholars have pointed out the role that learning plays in a clinical environment (Adib-
Hajbaghery, MirBagher, and Heidari, 2012). Experienced nurses and other healthcare
professionals have played a significant role in improving the process of workplace learning by
adhering to available guidelines and principles. Undergraduate learners depend on workplace
learning in nursing to get their first-hand experiences and enhance their skills and exposure
(Antohe et al., 2016). The success of their learning depends on the effectiveness of the process
and the approach taken by the facilitator. Workplace learning entails different dimensions such
as ethics, the environment, guidelines, and culture, which should be considered by learning
facilitators to positively impact the outcome of workplace learning (Blomberg et al., 2014). This
paper provides a reflection on workplace learning facilitation experience and outlines key
concepts do consider as a facilitator.
Section 1: Reflection
Preparation and Delivery
In this workplace learning experience, the learner was an undergraduate nursing student
assigned to a local hospital in Hong Kong as part of the regular training program for nurses.
Nurses undergo this process as part of their professional development. The learner did not have
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Facilitating Workplace Learning 4
any prior learning experiences apart from the current undergraduate nursing training program. In
this case, it implied that this was the first nursing qualification that the learner was pursuing. The
learner did not have substantial clinical experience apart from the firsthand training received
through the workplace learning sessions at the hospital as part of practicing what was learned in
class. I selected this learner because our interaction during the workplace learning provided
essential insights that could be used to improve the experience of other learners in the future. The
learner had several needs that cut across professional and personal dimensions. First, the reason
why the learner was assigned to the hospital was to gain nursing knowledge through practice and
involvement. The learner was expected acquire clinical experience and enhance cognitive
knowledge regarding nursing practice. At the same time, while undertaking the learning
program, the learner needed personal growth, career fulfillment, build practice responsibility,
and learn to work in group. Moreover, it was necessary to plan for the learning facilitation
process (Nasrin, Soroor, and Soodabeh, 2012). The first planning consideration was to outline
the learning objectives in line with the needs of the learner. On the other hand, I also evaluated
the factors that could impact the learning process and established a strategy that could effectively
benefit the learner. Finally, I identified the resources that could be used to improve the
facilitation process. The three factors allowed me to develop a facilitation plan that addressed
incorporated the key dimensions of learning through practice in nursing.
Lessons from Observed Session
During the learning facilitation, I came to realize that facilitators influence the outcomes
of workplace learning activities. The approach to supporting and teaching a learner determines
his/her experience and motivation. As a facilitator, I learned that it is my responsibility to ensure
that the learner’s needs are met based on the scope of the objectives outlined during the planning
any prior learning experiences apart from the current undergraduate nursing training program. In
this case, it implied that this was the first nursing qualification that the learner was pursuing. The
learner did not have substantial clinical experience apart from the firsthand training received
through the workplace learning sessions at the hospital as part of practicing what was learned in
class. I selected this learner because our interaction during the workplace learning provided
essential insights that could be used to improve the experience of other learners in the future. The
learner had several needs that cut across professional and personal dimensions. First, the reason
why the learner was assigned to the hospital was to gain nursing knowledge through practice and
involvement. The learner was expected acquire clinical experience and enhance cognitive
knowledge regarding nursing practice. At the same time, while undertaking the learning
program, the learner needed personal growth, career fulfillment, build practice responsibility,
and learn to work in group. Moreover, it was necessary to plan for the learning facilitation
process (Nasrin, Soroor, and Soodabeh, 2012). The first planning consideration was to outline
the learning objectives in line with the needs of the learner. On the other hand, I also evaluated
the factors that could impact the learning process and established a strategy that could effectively
benefit the learner. Finally, I identified the resources that could be used to improve the
facilitation process. The three factors allowed me to develop a facilitation plan that addressed
incorporated the key dimensions of learning through practice in nursing.
Lessons from Observed Session
During the learning facilitation, I came to realize that facilitators influence the outcomes
of workplace learning activities. The approach to supporting and teaching a learner determines
his/her experience and motivation. As a facilitator, I learned that it is my responsibility to ensure
that the learner’s needs are met based on the scope of the objectives outlined during the planning
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Facilitating Workplace Learning 5
process. When student nurses are undertaking their practice as part of their training, they depend
on the support from the assigned facilitator (Carlson and dvall, 2012). For example, during this
learning facilitation, the learner always looked forward to my guidance and direction. Every time
the learner needed help, I was the first person to be contacted. The learner believed that I had all
the answers to any query associated with nursing practice. I noticed that a facilitator should be
knowledgeable and experienced in the area that they teach for them to be in a position to assist a
learner. Lack of comprehensive knowledge in a particular field could negatively impact the
experience of the learner as well as the ability of the facilitator to meet the objectives of
workplace learning programs (Stenberg and Carlson, 2015). In nursing, knowledge, and
experience plays a key role when assisting student nurses to build their skills and confidence
(Chun and Barnett, 2012). Based on my interaction with the learner, I noticed that the roles of a
workplace learning facilitator go beyond teaching the skills and knowledge, that is, social,
emotional, and physical needs of the learner are equally fundamental.
One of the key occurrences was when the learner was facing a financial problem and
could not concentrate during the learning session. I felt it was my responsibility to assist the
learner to cope up with the circumstances that prevailed during that period. We came up with a
plan that could enable the learner to address the financial problem. Social, cultural, and
environmental factors impact workplace learning outcomes and processes (Stenberg and Carlson,
2015). In nursing, the facilitators are mandated with the obligation of determining how these
external factors could impede the ability of the learner to meet the underpinning objectives
(Dehghani et al., 2016). It is important to come up with a strategy that could support the learners’
experience within and beyond the learning settings or environment. As seen in this case, I had to
support the learner by collaboratively planning on how to solve the financial problem because it
process. When student nurses are undertaking their practice as part of their training, they depend
on the support from the assigned facilitator (Carlson and dvall, 2012). For example, during this
learning facilitation, the learner always looked forward to my guidance and direction. Every time
the learner needed help, I was the first person to be contacted. The learner believed that I had all
the answers to any query associated with nursing practice. I noticed that a facilitator should be
knowledgeable and experienced in the area that they teach for them to be in a position to assist a
learner. Lack of comprehensive knowledge in a particular field could negatively impact the
experience of the learner as well as the ability of the facilitator to meet the objectives of
workplace learning programs (Stenberg and Carlson, 2015). In nursing, knowledge, and
experience plays a key role when assisting student nurses to build their skills and confidence
(Chun and Barnett, 2012). Based on my interaction with the learner, I noticed that the roles of a
workplace learning facilitator go beyond teaching the skills and knowledge, that is, social,
emotional, and physical needs of the learner are equally fundamental.
One of the key occurrences was when the learner was facing a financial problem and
could not concentrate during the learning session. I felt it was my responsibility to assist the
learner to cope up with the circumstances that prevailed during that period. We came up with a
plan that could enable the learner to address the financial problem. Social, cultural, and
environmental factors impact workplace learning outcomes and processes (Stenberg and Carlson,
2015). In nursing, the facilitators are mandated with the obligation of determining how these
external factors could impede the ability of the learner to meet the underpinning objectives
(Dehghani et al., 2016). It is important to come up with a strategy that could support the learners’
experience within and beyond the learning settings or environment. As seen in this case, I had to
support the learner by collaboratively planning on how to solve the financial problem because it
Facilitating Workplace Learning 6
was directly affecting the learning experience. I felt that this occurrence, as well as other
encounters during this period, created a baseline for a professional social relationship build on
trust. Student nurses expect respect and acknowledgment from their facilitators during workplace
learning; however, support is among the key factors that encourage the existence of a supportive
environment (Farzi, Haghani, and Farzi, 2016). Based on this encounter, the learner became free
to share any other problems experienced within the learning settings as well as outside the scope
of nursing practice. I learned that trust enhances the strength of professional relationships
between student nurses and their supervisors.
Moreover, I felt that my performance during this learning facilitation was outstanding
based on the outcomes at the end of the session. I was able to build a mutual relationship with the
learner. Effective professional relationship at the workplace plays a key role in improving
performance outcomes (Nasrin, Soroor, and Soodabeh, 2012). When experienced nurses interact
with student nurses in a non-coercive and non-threatening manner, the latter is encouraged to
advance their skills and improve performance (Haghani and Fakhari, 2014). Through such
relationships, learners are motivated, feel confident, and are free to share their experiences. I was
also able to support the learner to develop courage when handling nursing tasks. At the end of
the session, the learner was able to understand and conduct the anticipated nursing procedures as
outlined in the learning guidelines. However, one of the challenges faced during this workplace
learning facilitation involved creating a balance between meeting the teaching goals while at the
same time meeting the needs of the learner beyond the scope nursing practice. For example, the
financial problem that the learner faced negatively impacted the learning schedule. Nevertheless,
effective learning could only occur when the learner’s physical, mental, and social wellbeing was
guaranteed. I, therefore, learned that facilitators should strive to achieve effective balance
was directly affecting the learning experience. I felt that this occurrence, as well as other
encounters during this period, created a baseline for a professional social relationship build on
trust. Student nurses expect respect and acknowledgment from their facilitators during workplace
learning; however, support is among the key factors that encourage the existence of a supportive
environment (Farzi, Haghani, and Farzi, 2016). Based on this encounter, the learner became free
to share any other problems experienced within the learning settings as well as outside the scope
of nursing practice. I learned that trust enhances the strength of professional relationships
between student nurses and their supervisors.
Moreover, I felt that my performance during this learning facilitation was outstanding
based on the outcomes at the end of the session. I was able to build a mutual relationship with the
learner. Effective professional relationship at the workplace plays a key role in improving
performance outcomes (Nasrin, Soroor, and Soodabeh, 2012). When experienced nurses interact
with student nurses in a non-coercive and non-threatening manner, the latter is encouraged to
advance their skills and improve performance (Haghani and Fakhari, 2014). Through such
relationships, learners are motivated, feel confident, and are free to share their experiences. I was
also able to support the learner to develop courage when handling nursing tasks. At the end of
the session, the learner was able to understand and conduct the anticipated nursing procedures as
outlined in the learning guidelines. However, one of the challenges faced during this workplace
learning facilitation involved creating a balance between meeting the teaching goals while at the
same time meeting the needs of the learner beyond the scope nursing practice. For example, the
financial problem that the learner faced negatively impacted the learning schedule. Nevertheless,
effective learning could only occur when the learner’s physical, mental, and social wellbeing was
guaranteed. I, therefore, learned that facilitators should strive to achieve effective balance
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Facilitating Workplace Learning 7
regarding the needs of the nursing students without jeopardizing the objectives and the process of
learning (Hellström-Hyson, Mårtensson, and Kristofferzon, 2012).
Summary of Learning and Future Implication
Workplace learning facilitation was an important experience that enhanced my
experience in nursing. In summary, I learned that it is important to effectively plan for the
facilitation by taking into consideration key factors such as the available resources, learning
environment, and the needs of the learner. While these factors are essential, facilitators should
ensure that they have enough knowledge and experience to conduct the learning process. I also
learned that the facilitator should collaborate with the learner throughout the entire period to
guarantee the achievement of the outlined learning objectives. At the same time, the experience
revealed that learners could encounter some challenges outside the scope of learning and this
could negatively impact the workplace learning process. In such situations, I have realized that it
is important for the facilitator to assist the nursing student to overcome the external limitations
encountered.
Based on the lesson learned, I will ensure that in my subsequent learning facilitation, I
will have an introductory session with the learner before proceeding with the nursing activities.
In this preliminary session, I will seek to understand the social issues that the learner could be
experiencing. I believe that having a clear picture of the learner before starting the learning
sessions could provide essential insights on how to assist the student nurse overcome external
challenges that impact skill development (Stenberg and Carlson, 2015). Moreover, this move
will ensure that I have a clear picture of the socio-cultural background and perspective of the
learner, which is important when managing learning process in clinical environment (Liljedahl et
al., 2016). Scholarly literature ascertains that medical students depend on the support of senior
regarding the needs of the nursing students without jeopardizing the objectives and the process of
learning (Hellström-Hyson, Mårtensson, and Kristofferzon, 2012).
Summary of Learning and Future Implication
Workplace learning facilitation was an important experience that enhanced my
experience in nursing. In summary, I learned that it is important to effectively plan for the
facilitation by taking into consideration key factors such as the available resources, learning
environment, and the needs of the learner. While these factors are essential, facilitators should
ensure that they have enough knowledge and experience to conduct the learning process. I also
learned that the facilitator should collaborate with the learner throughout the entire period to
guarantee the achievement of the outlined learning objectives. At the same time, the experience
revealed that learners could encounter some challenges outside the scope of learning and this
could negatively impact the workplace learning process. In such situations, I have realized that it
is important for the facilitator to assist the nursing student to overcome the external limitations
encountered.
Based on the lesson learned, I will ensure that in my subsequent learning facilitation, I
will have an introductory session with the learner before proceeding with the nursing activities.
In this preliminary session, I will seek to understand the social issues that the learner could be
experiencing. I believe that having a clear picture of the learner before starting the learning
sessions could provide essential insights on how to assist the student nurse overcome external
challenges that impact skill development (Stenberg and Carlson, 2015). Moreover, this move
will ensure that I have a clear picture of the socio-cultural background and perspective of the
learner, which is important when managing learning process in clinical environment (Liljedahl et
al., 2016). Scholarly literature ascertains that medical students depend on the support of senior
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Facilitating Workplace Learning 8
practitioners during clinical learning sessions for professional and moral support as they
demonstrate adaptive capacity in nursing practice (Liljedahl et al., 2017).
Section 2: Discussion and Debate
Achieving Student-Centered Teaching
It is important to recall that the success of a workplace learning process depends on the
extent to which the planning and implementation focused on the learner. A student-centered
approach to learning in nursing practice focuses on practice and participation. Student nurses
could improve their skills, gain confidence, and focus on personal development when they are
constantly engaged in participatory learning (Hematimaslakpak and Khalilzadeh, 2012).
Learning facilitators are therefore expected to create a program that encouraged the student
nurses to learn by doing the assigned tasks. However, based on the sensitive nature of healthcare
interventions, the learning should be carried out under strict supervision to guarantee patients’
safety and experience. But at the same time, there is a need for empathic understanding to
encourage a positive attitude among student nurses. The facilitators support knowledge
development through resource sharing (Kamran et al., 2013). The needs of the learner also
revolve around knowledge development and professional growth. When the learning process is
student-centered, then the theoretical underpinnings acknowledge the learner as a partner to be
included in key decisions of the program. As active consumers of clinical education, nursing
students should be entrusted with care responsibilities under the guidance of the facilitators to
develop the required skills and expertise in practice.
Moreover, it is important to understand the role of culture when seeking to achieve
student-centered workplace learning during nursing practice. Learners differ from one another
and cultural background impacts how they think and perceive the environment. Nationality,
practitioners during clinical learning sessions for professional and moral support as they
demonstrate adaptive capacity in nursing practice (Liljedahl et al., 2017).
Section 2: Discussion and Debate
Achieving Student-Centered Teaching
It is important to recall that the success of a workplace learning process depends on the
extent to which the planning and implementation focused on the learner. A student-centered
approach to learning in nursing practice focuses on practice and participation. Student nurses
could improve their skills, gain confidence, and focus on personal development when they are
constantly engaged in participatory learning (Hematimaslakpak and Khalilzadeh, 2012).
Learning facilitators are therefore expected to create a program that encouraged the student
nurses to learn by doing the assigned tasks. However, based on the sensitive nature of healthcare
interventions, the learning should be carried out under strict supervision to guarantee patients’
safety and experience. But at the same time, there is a need for empathic understanding to
encourage a positive attitude among student nurses. The facilitators support knowledge
development through resource sharing (Kamran et al., 2013). The needs of the learner also
revolve around knowledge development and professional growth. When the learning process is
student-centered, then the theoretical underpinnings acknowledge the learner as a partner to be
included in key decisions of the program. As active consumers of clinical education, nursing
students should be entrusted with care responsibilities under the guidance of the facilitators to
develop the required skills and expertise in practice.
Moreover, it is important to understand the role of culture when seeking to achieve
student-centered workplace learning during nursing practice. Learners differ from one another
and cultural background impacts how they think and perceive the environment. Nationality,
Facilitating Workplace Learning 9
ethnic groups, religion, and gender are the key variables to be considered in terms of culture.
When facilitators are planning and implementing workplace learning programs for student
nurses, they are required to pay attention to how their attitudes and perceptions impact the
process (Nasrin, Soroor, and Soodabeh, 2012). Respecting the diversities could also open new
platforms for effective collaboration and learning between the student nurses and experienced
practitioners (Pourghane, 2013). Those mandated with the responsibility of teaching student
nurses are expected to review their experiences and use the acquired insight to create a favorable
framework that could meet the needs of the learner by paying attention to sustainability and
effectiveness.
Furthermore, student nurses could be insufficient in terms of learning capacity. Some
could be affected by fear. In such a case, the educators are required to provide necessary support
to encourage the learners to develop resilience and commitment towards the set milestones
(Nasrin, Soroor, and Soodabeh, 2012). A student-centered approach will consider the impact of
criticism. Limited self-confidence and lack of mastery of clinical skills by learners should be
handled empathically and professionally with the objective of assisting the student nurse to attain
the desired cognitive and professional growth and independence (Pourghane, 2013; Rajesh,
2017). At the same time, the learning environment, which is a clinical environment, determines
whether the learner will experience the best skill development during the practice sessions.
Student nurses require a supportive environment where doctors and nurses are willing to improve
participation and involvement and foster the willingness to teach young professionals. A hostile
environment with limited resources, lack of support, and reduced participation discourage the
achievement of student-centered workplace learning (Pourghane, 2013).
ethnic groups, religion, and gender are the key variables to be considered in terms of culture.
When facilitators are planning and implementing workplace learning programs for student
nurses, they are required to pay attention to how their attitudes and perceptions impact the
process (Nasrin, Soroor, and Soodabeh, 2012). Respecting the diversities could also open new
platforms for effective collaboration and learning between the student nurses and experienced
practitioners (Pourghane, 2013). Those mandated with the responsibility of teaching student
nurses are expected to review their experiences and use the acquired insight to create a favorable
framework that could meet the needs of the learner by paying attention to sustainability and
effectiveness.
Furthermore, student nurses could be insufficient in terms of learning capacity. Some
could be affected by fear. In such a case, the educators are required to provide necessary support
to encourage the learners to develop resilience and commitment towards the set milestones
(Nasrin, Soroor, and Soodabeh, 2012). A student-centered approach will consider the impact of
criticism. Limited self-confidence and lack of mastery of clinical skills by learners should be
handled empathically and professionally with the objective of assisting the student nurse to attain
the desired cognitive and professional growth and independence (Pourghane, 2013; Rajesh,
2017). At the same time, the learning environment, which is a clinical environment, determines
whether the learner will experience the best skill development during the practice sessions.
Student nurses require a supportive environment where doctors and nurses are willing to improve
participation and involvement and foster the willingness to teach young professionals. A hostile
environment with limited resources, lack of support, and reduced participation discourage the
achievement of student-centered workplace learning (Pourghane, 2013).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Facilitating Workplace Learning 10
Culture of the Organization and Learning Outcomes
Organizational culture is a central concept when creating and managing effective
healthcare systems (Schein and Schein, 2017). A robust organizational culture in the healthcare
system entails an environment that supports learning and openness. It ensures that there is
collaboration between professionals with the objective of improving personal experiences and
organizational performance. Therefore, a good culture in a healthcare facility should focus on
patients, the system, and the workers (Nasrin, Soroor, and Soodabeh, 2012). Organizational
culture impacts workplace learning in nursing. The learned values embedded in the behavioral
system that guides employees will influence how and what student nurses will embrace as the
expected norms (Rajesh, 2017). It is expected that the leadership of a healthcare system will
from time to time conduct an internal assessment to determine the strengths, opportunities,
weaknesses, and threats characterizing the activities and processes being carried out. Student
nurses undertaking their learning by practice programs in a facility with robust systems are
bound to benefit in terms of professional development and personal growth. Such an outcome is
justified by the fact that a good organizational culture focuses on opportunities available by
maximizing the strengths while at the same time reducing threats and mitigating weaknesses
(Schein and Schein, 2017).. In fact, sustaining the success of a healthcare facility is associated
with flexibility of the internal culture in line with organizational learning.
Moreover, it is equally important to note how negative culture could also affect the
learning of student nurses. The facilitators or the educators are supposed to adhere to practice
standards when giving direction and support to the learners. In this case, the best practices are
shared across professional generations. Negative perceptions about workplace culture and
nursing practices could easily be embraced or learned by student nurses based on what they hear
Culture of the Organization and Learning Outcomes
Organizational culture is a central concept when creating and managing effective
healthcare systems (Schein and Schein, 2017). A robust organizational culture in the healthcare
system entails an environment that supports learning and openness. It ensures that there is
collaboration between professionals with the objective of improving personal experiences and
organizational performance. Therefore, a good culture in a healthcare facility should focus on
patients, the system, and the workers (Nasrin, Soroor, and Soodabeh, 2012). Organizational
culture impacts workplace learning in nursing. The learned values embedded in the behavioral
system that guides employees will influence how and what student nurses will embrace as the
expected norms (Rajesh, 2017). It is expected that the leadership of a healthcare system will
from time to time conduct an internal assessment to determine the strengths, opportunities,
weaknesses, and threats characterizing the activities and processes being carried out. Student
nurses undertaking their learning by practice programs in a facility with robust systems are
bound to benefit in terms of professional development and personal growth. Such an outcome is
justified by the fact that a good organizational culture focuses on opportunities available by
maximizing the strengths while at the same time reducing threats and mitigating weaknesses
(Schein and Schein, 2017).. In fact, sustaining the success of a healthcare facility is associated
with flexibility of the internal culture in line with organizational learning.
Moreover, it is equally important to note how negative culture could also affect the
learning of student nurses. The facilitators or the educators are supposed to adhere to practice
standards when giving direction and support to the learners. In this case, the best practices are
shared across professional generations. Negative perceptions about workplace culture and
nursing practices could easily be embraced or learned by student nurses based on what they hear
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Facilitating Workplace Learning 11
and observe in the clinical environment (Ross and Bruderle, 2016). Therefore, nursing educators
should endeavor to motivate learners and help them build a positive workplace perspective. For
example, learners should be assessed based on the available guidelines in the organization, which
offers the opportunity for the student nurses to understand the progress they make or the areas
they need to improve. An organizational culture that supports regular and comprehensive
assessment also paves the way for skill and knowledge development for learners (Schein and
Schein, 2017). The role of assessment in healthcare training and learning is to maintain care
standards and foster adequate preparation for career and profession. Organizational culture in
healthcare also impacts the ability of educators to meet the professional development needs of
student nurses.
Respecting Learners: Relationship with Student Nurses
Another essential concept that dominates the process of workplace learning in healthcare
services and clinical settings is respect and relationship between the educators or facilitators and
student nurses as the learners. When undertaking the role of a workplace learning facilitator, it is
expected that the learners will respect and adhere to the available guidelines to guarantee smooth
interaction throughout the period. However, the greatest debate has been on whether the
facilitators are prepared to respect the learners and focus on building mutual but professional
relationships. Student nurses have their personal expectations, rights, and anticipations. During
the training sessions, they deserve respect and to be treated with dignity (Mary, 2014).
Facilitators cannot effectively support nursing students without first respecting their diversity,
perceptions, and needs. The educators are supposed to work collaboratively and incorporate their
choices when making fundamental decisions that directly impact the learners. Respect comes
with understanding the weaknesses and strengths of the learner and considering the ways in
and observe in the clinical environment (Ross and Bruderle, 2016). Therefore, nursing educators
should endeavor to motivate learners and help them build a positive workplace perspective. For
example, learners should be assessed based on the available guidelines in the organization, which
offers the opportunity for the student nurses to understand the progress they make or the areas
they need to improve. An organizational culture that supports regular and comprehensive
assessment also paves the way for skill and knowledge development for learners (Schein and
Schein, 2017). The role of assessment in healthcare training and learning is to maintain care
standards and foster adequate preparation for career and profession. Organizational culture in
healthcare also impacts the ability of educators to meet the professional development needs of
student nurses.
Respecting Learners: Relationship with Student Nurses
Another essential concept that dominates the process of workplace learning in healthcare
services and clinical settings is respect and relationship between the educators or facilitators and
student nurses as the learners. When undertaking the role of a workplace learning facilitator, it is
expected that the learners will respect and adhere to the available guidelines to guarantee smooth
interaction throughout the period. However, the greatest debate has been on whether the
facilitators are prepared to respect the learners and focus on building mutual but professional
relationships. Student nurses have their personal expectations, rights, and anticipations. During
the training sessions, they deserve respect and to be treated with dignity (Mary, 2014).
Facilitators cannot effectively support nursing students without first respecting their diversity,
perceptions, and needs. The educators are supposed to work collaboratively and incorporate their
choices when making fundamental decisions that directly impact the learners. Respect comes
with understanding the weaknesses and strengths of the learner and considering the ways in
Facilitating Workplace Learning 12
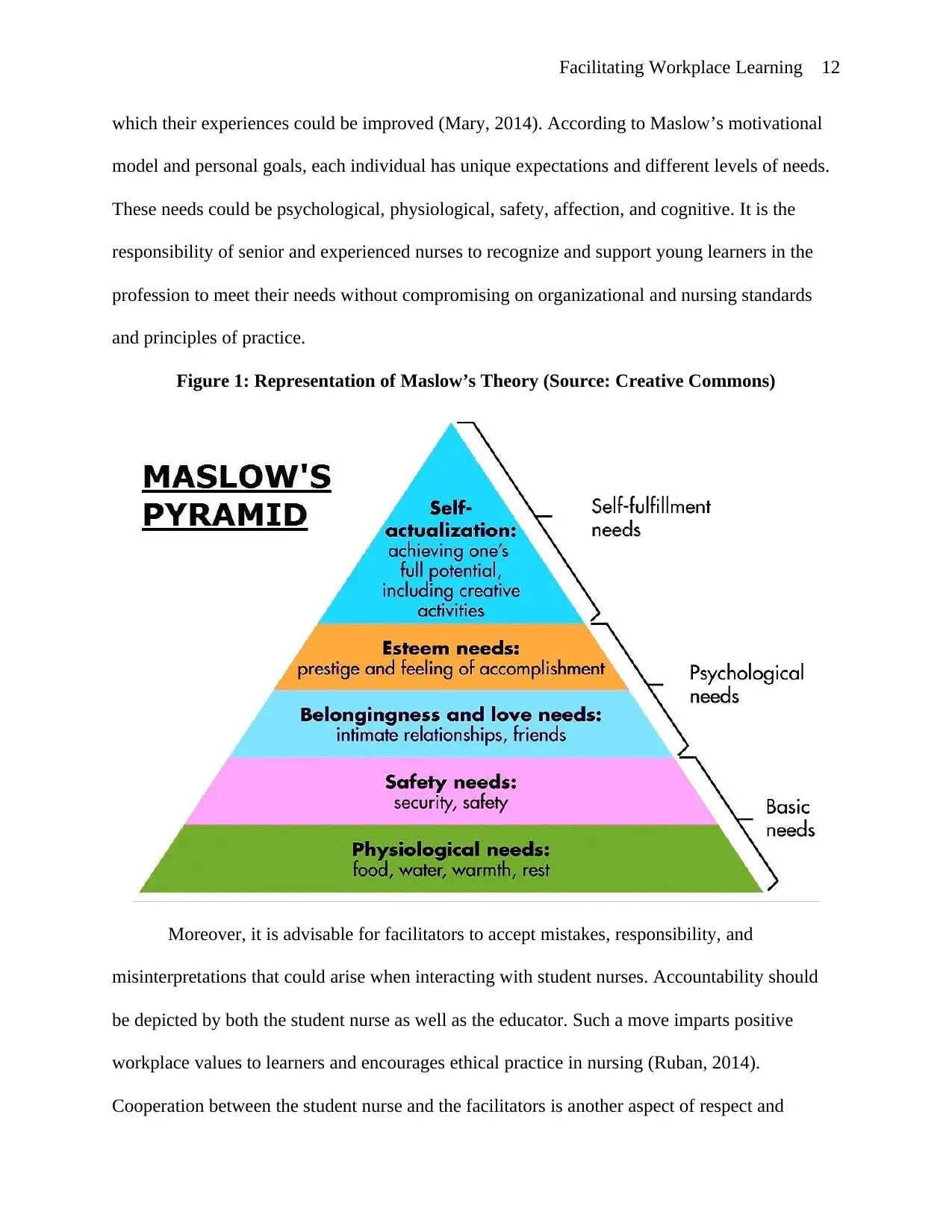
which their experiences could be improved (Mary, 2014). According to Maslow’s motivational
model and personal goals, each individual has unique expectations and different levels of needs.
These needs could be psychological, physiological, safety, affection, and cognitive. It is the
responsibility of senior and experienced nurses to recognize and support young learners in the
profession to meet their needs without compromising on organizational and nursing standards
and principles of practice.
Figure 1: Representation of Maslow’s Theory (Source: Creative Commons)
Moreover, it is advisable for facilitators to accept mistakes, responsibility, and
misinterpretations that could arise when interacting with student nurses. Accountability should
be depicted by both the student nurse as well as the educator. Such a move imparts positive
workplace values to learners and encourages ethical practice in nursing (Ruban, 2014).
Cooperation between the student nurse and the facilitators is another aspect of respect and
which their experiences could be improved (Mary, 2014). According to Maslow’s motivational
model and personal goals, each individual has unique expectations and different levels of needs.
These needs could be psychological, physiological, safety, affection, and cognitive. It is the
responsibility of senior and experienced nurses to recognize and support young learners in the
profession to meet their needs without compromising on organizational and nursing standards
and principles of practice.
Figure 1: Representation of Maslow’s Theory (Source: Creative Commons)
Moreover, it is advisable for facilitators to accept mistakes, responsibility, and
misinterpretations that could arise when interacting with student nurses. Accountability should
be depicted by both the student nurse as well as the educator. Such a move imparts positive
workplace values to learners and encourages ethical practice in nursing (Ruban, 2014).
Cooperation between the student nurse and the facilitators is another aspect of respect and
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 21
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





