Facilitators and Barriers to Minority Blood Donation: A Review
VerifiedAdded on 2022/10/17
|9
|8509
|482
Report
AI Summary
This systematic review, published in Nursing Research, examines the facilitators and barriers to blood donation within minority populations in the United States. The study, conducted using various electronic databases, employed a meta-synthesis approach to analyze 15 articles and identify key themes. The findings highlight the complex interplay of factors influencing donation, including the impact of knowing a blood recipient, cultural and religious affiliations, and medical mistrust. The review emphasizes the need for community education and communication to rebuild trust and address the underrepresentation of minorities among blood donors, particularly crucial for individuals with sickle cell disease and thalassemia. The research recommends strategies to increase blood donations within minority communities.
Downloaded from https://journals.lww.com/nursingresearchonline by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3gDUFDls0jtTXFtI0IpkQ2pXag2MXLaJbefcaPVF5JxI= on 10/17/2019
Facilitators and Barriers to Minority
Blood Donations
A Systematic Review
Regena Spratling ▼ Raymona H. Lawrence
Background: Minority blood donations have historically been low in the United States; however, increasing the prop
minority blood donations is essential to reducing blood transfusion complications—particularly in African American
cell disease and thalassemia.
Objectives: The research question was as follows: What are the facilitators and barriers to blood donation in minori
Methods: Beginning August 2017, we conducted a literature search using the following electronic databases: CINAH
Full Text, Academic Search Complete, MEDLINE, PsycINFO, Sociological Collection, Cochrane Library, ProQuest Diss
and Theses, and PubMed, which continued through December 2017. Based on primarily descriptive data in the art
(n = 15), the systematic review proceeded as a meta-synthesis. An inductive approach was used to analyze comm
differences, patterns, and themes in the study findings; interpret the findings; and synthesize the findings to gener
knowledge about the phenomena of study.
Results: The themes included (a) knowing a blood recipient; (b) identifying with culture, race/ethnicity, and religiou
and (c) medical mistrust and misunderstanding. All were prominent in the descriptions of minorities on blood dona
as facilitators and barriers.
Discussion: The reviewed studies demonstrated that facilitators and barriers to minority blood donations are comp
concurrently. Community education and communication about blood donation have a positive effect on fellow com
members, including friends and family, in racial and ethnic minorities that are underrepresented among blood don
further suggest the need to rebuild trust among minority communities.
Key Words: blood donors minority groups qualitative research systematic review
Nursing Research, May/June 2019, Vol 68, No 3, 218–226
Minority blood donations have historically been low
in the United States (Yazer et al., 2017). Increasing
the proportion ofminority blood donations is
essential to reducing blood transfusion complications, par-
ticularly in individuals with sickle celldisease (SCD) and
thalassemia, for several reasons (Yazer et al., 2017). First, SCD
and thalassemia disproportionately affect minority racial and
ethnic populations in the United States. For example, SCD
occurs in about 1 in every 500 African American (AA) births,
1 in every 36,000 Hispanic-American births, and 1 in every
100,000 Caucasian births (Hassell,2010).Thalassemia is
prevalent in populations with roots in the Mediterranean,
Middle East,Indian subcontinent,Southeast Asia, and China
(Li, 2017). Second, blood from donors—with similar backg
as the recipients—is more likely to be a close match (Frye
et al., 2014). Unmatched blood can cause potentially seve
transfusion complications. Therefore, there is a critical nee
for blood donations from minorities to improve transfusion
outcomes in minority populations.
Individuals with hemoglobin disorders often need
transfusions—sometimes chronically and sometimes inter
mittently. If exposed to unmatched donor blood, the risk is
alloimmunization: the development of antibodies to the fo
eign red blood cellantigens (Charbonneau & Daigneault,
2016).Increasing blood donations among minorities can
ensure better access to minor antigen-matched units; how
ever,strategies for promoting donation in these popula-
tions require awareness ofthe unique characteristics of
minority groups and blood donation,as wellas programs
that address facilitators and barriers to minority blood don
tion (Charbonneau & Daigneault, 2016; Frye et al., 2014).
Regena Spratling, PhD, RN, APRN, CPNP, is Associate Professor and Associate
Dean & Chief Academic Officer for Nursing, Georgia State University, School
of Nursing, Byrdine F. Lewis College of Nursing & Health Professions, Atlanta.
Raymona H. Lawrence, DrPH, MPH, MCHES, is Associate Professor, Georgia
Southern University, Jiann Ping Hsu College of Public Health, Community
Health Behavior and Education, Statesboro.
This is an open-access article distributed under the terms of the Creative
Commons Attribution-Non Commercial-No Derivatives License 4.0 (CCBY-
NC-ND), where it is permissible to download and share the work provided it
is properly cited. The work cannot be changed in any way or used commer-
cially without permission from the journal.
Copyright © 2019 The Authors. Published by Wolters Kluwer Health, Inc.
DOI: 10.1097/NNR.0000000000000355
218 www.nursingresearchonline.com Nursing Research • May/June 2019• Volume 68• No. 3
Facilitators and Barriers to Minority
Blood Donations
A Systematic Review
Regena Spratling ▼ Raymona H. Lawrence
Background: Minority blood donations have historically been low in the United States; however, increasing the prop
minority blood donations is essential to reducing blood transfusion complications—particularly in African American
cell disease and thalassemia.
Objectives: The research question was as follows: What are the facilitators and barriers to blood donation in minori
Methods: Beginning August 2017, we conducted a literature search using the following electronic databases: CINAH
Full Text, Academic Search Complete, MEDLINE, PsycINFO, Sociological Collection, Cochrane Library, ProQuest Diss
and Theses, and PubMed, which continued through December 2017. Based on primarily descriptive data in the art
(n = 15), the systematic review proceeded as a meta-synthesis. An inductive approach was used to analyze comm
differences, patterns, and themes in the study findings; interpret the findings; and synthesize the findings to gener
knowledge about the phenomena of study.
Results: The themes included (a) knowing a blood recipient; (b) identifying with culture, race/ethnicity, and religiou
and (c) medical mistrust and misunderstanding. All were prominent in the descriptions of minorities on blood dona
as facilitators and barriers.
Discussion: The reviewed studies demonstrated that facilitators and barriers to minority blood donations are comp
concurrently. Community education and communication about blood donation have a positive effect on fellow com
members, including friends and family, in racial and ethnic minorities that are underrepresented among blood don
further suggest the need to rebuild trust among minority communities.
Key Words: blood donors minority groups qualitative research systematic review
Nursing Research, May/June 2019, Vol 68, No 3, 218–226
Minority blood donations have historically been low
in the United States (Yazer et al., 2017). Increasing
the proportion ofminority blood donations is
essential to reducing blood transfusion complications, par-
ticularly in individuals with sickle celldisease (SCD) and
thalassemia, for several reasons (Yazer et al., 2017). First, SCD
and thalassemia disproportionately affect minority racial and
ethnic populations in the United States. For example, SCD
occurs in about 1 in every 500 African American (AA) births,
1 in every 36,000 Hispanic-American births, and 1 in every
100,000 Caucasian births (Hassell,2010).Thalassemia is
prevalent in populations with roots in the Mediterranean,
Middle East,Indian subcontinent,Southeast Asia, and China
(Li, 2017). Second, blood from donors—with similar backg
as the recipients—is more likely to be a close match (Frye
et al., 2014). Unmatched blood can cause potentially seve
transfusion complications. Therefore, there is a critical nee
for blood donations from minorities to improve transfusion
outcomes in minority populations.
Individuals with hemoglobin disorders often need
transfusions—sometimes chronically and sometimes inter
mittently. If exposed to unmatched donor blood, the risk is
alloimmunization: the development of antibodies to the fo
eign red blood cellantigens (Charbonneau & Daigneault,
2016).Increasing blood donations among minorities can
ensure better access to minor antigen-matched units; how
ever,strategies for promoting donation in these popula-
tions require awareness ofthe unique characteristics of
minority groups and blood donation,as wellas programs
that address facilitators and barriers to minority blood don
tion (Charbonneau & Daigneault, 2016; Frye et al., 2014).
Regena Spratling, PhD, RN, APRN, CPNP, is Associate Professor and Associate
Dean & Chief Academic Officer for Nursing, Georgia State University, School
of Nursing, Byrdine F. Lewis College of Nursing & Health Professions, Atlanta.
Raymona H. Lawrence, DrPH, MPH, MCHES, is Associate Professor, Georgia
Southern University, Jiann Ping Hsu College of Public Health, Community
Health Behavior and Education, Statesboro.
This is an open-access article distributed under the terms of the Creative
Commons Attribution-Non Commercial-No Derivatives License 4.0 (CCBY-
NC-ND), where it is permissible to download and share the work provided it
is properly cited. The work cannot be changed in any way or used commer-
cially without permission from the journal.
Copyright © 2019 The Authors. Published by Wolters Kluwer Health, Inc.
DOI: 10.1097/NNR.0000000000000355
218 www.nursingresearchonline.com Nursing Research • May/June 2019• Volume 68• No. 3
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
goals of this systematic review are to expand the knowledge of
facilitators and barriers to minority blood donation and to
recommend strategies thatwill increase blood donations
within minority communities.
Blood transfusions increase hemoglobin levels,increase
blood flow, improve oxygen delivery to the tissues, and dilute
the abnormal red blood cells containing sickled hemoglobin,
thus increasing the number of circulating normalred blood
cells (Estcourt, Fortin, Hopewell, Trivella, & Wang, 2017). Phe-
notypic incompatibility in blood transfusions results in the de-
velopment of antibodies over time that attack red blood cells,
making subsequent transfusions less effective and increasing the
risk of transfusion complications (Charbonneau & Daigneault,
2016). These antibodies to antigens, if present in subsequently
transfused blood, will trigger a dangerous hemolytic transfusion
reaction when transfused red blood cells are destroyed by the
immune system (Estcourt et al., 2017).
Minority blood donors are essential for a diverse supply
of blood because they provide greateraccessto corre-
sponding phenotypes, often rare ones, required for individ-
uals with diseases such as SCD and thalassemia. However,
minorities are historically underrepresented among blood
donors. In the United States, an estimated 11% to 21% of blood
donations are from minority populations based on the National
Blood Collection & Utilization Survey 2011 (U.S. Department
of Health and Human Services,2011).More recent surveys
from eight blood centers in 17 states noted decreasing blood
donations overall and a continued underrepresentation of mi-
nority donors. For example, Black or AA donors constituted
approximately 5% of alldonors from 2006 to 2015 (Yazer
et al., 2017). A decreased proportion of minority blood donors
has also been reported in Canada (Charbonneau & Daigneault,
2016) and France (Grassineau et al., 2007).
Increasing minority blood donations is a complex public
health issue with several barriers to minority blood donations.
Minorities have reported higher deferralrates and lack of
awareness about the process of blood donation (Frye et al.,
2014). Less than 1% of all donors experience events such as
fainting and fatigue (U.S.Department of Health and Human
Services, 2011); however, despite a relatively low occurrence
of adverse events, fear of these events is a commonly reported
barrier to blood donation among minority populations (Shaz,
Demmons, Hillyer, Jones, & Hillyer, 2009). Barriers to blood
donation also include defermentdue to low hemoglobin,
consisting of almost half (48%) of all deferrals from all poten-
tialdonors in the United States (U.S.Department of Health
and Human Services, 2011). Mobile blood drives remain the
major source (66%) of blood collections in the United States
(U.S. Department of Health and Human Services, 2011). These
blood drives often recruit minority populations in the commu-
nity, at local churches, and other gatherings, yet a substantial
or sustainable increase in donations from these blood drives
has not been found (Yazer et al., 2017).
The current knowledge on facilitators and barriers to
nority blood donations is limited. Systematic reviews on
donations and blood donors exist,although none address
blood donation issues specific to minorities and none rev
the race/ethnicity of study samples (Bagot, Murray, & Ma
2016; Bednall, Bove, Cheetham, & Murray, 2013; Godin,
Im, Bélanger-Gravel, & Amireault, 2012). In addition, Bed
et al. (2013) reviewed blood donation behavior and inten
and cited the need for research with minorities as they o
port additional barriers to blood donation. The purposes o
systematic review are to examine the facilitators and bar
minority blood donations and recommend strategies to in
donations in the community. Therefore, the following res
question was asked:Whatare the facilitators and barriers to
blood donation in minority populations?
METHODS
Search Strategy
Prior to beginning the systematic review, the principal in
gator (PI) conducted a preliminary search to ensure the a
sence of similar reviews and gain understanding of existi
literature on minority blood donations. We consulted exp
on systematic review and meta-analyses: a librarian with
tise in nursing and health literature and experts on mino
blood donation and blood transfusion complications asso
ated with the hemoglobinopathies of SCD and thalassem
on search approach and terminology and goals of the rev
The systematic review proceeded using Preferred Report
Items for Systematic Reviews and Meta-Analyses, and th
search question served as basis for identification,selection,
and appraisal of studies and collection and analysis of da
reviewed studies (Moher, Liberati, Tetzlaff, & Altman, 200
The literature search began in August 2017 using the
tronic databases CINAHL Plus With Full Text, Academic S
Complete, MEDLINE, PsycINFO, Sociological Collection,
Cochrane Library,ProQuest Dissertation and Theses,and
PubMed. Search alerts were also initiated for databases t
continued the search through December 2017. There we
no restrictions on publication year, publication type, or a
type. The keywords used in the search included combina
of the following words: blood donation, blood donor, mino
ity, AA, Black, race and ethnicity, and Hispanic or Latino.
The search databases and search combinations are prese
in Table 1.
Inclusion and Exclusion Criteria
Inclusion criteria were (a) data-based studies that sample
nority blood donors and minority blood donations or inclu
minorities in description of blood donor samples; (b) data
minority participants on process of blood donation;and (c)
English language. Exclusion criteria were (a) data-based
Nursing Research • May/June 2019• Volume 68• No. 3 Minority Blood Donations 219
facilitators and barriers to minority blood donation and to
recommend strategies thatwill increase blood donations
within minority communities.
Blood transfusions increase hemoglobin levels,increase
blood flow, improve oxygen delivery to the tissues, and dilute
the abnormal red blood cells containing sickled hemoglobin,
thus increasing the number of circulating normalred blood
cells (Estcourt, Fortin, Hopewell, Trivella, & Wang, 2017). Phe-
notypic incompatibility in blood transfusions results in the de-
velopment of antibodies over time that attack red blood cells,
making subsequent transfusions less effective and increasing the
risk of transfusion complications (Charbonneau & Daigneault,
2016). These antibodies to antigens, if present in subsequently
transfused blood, will trigger a dangerous hemolytic transfusion
reaction when transfused red blood cells are destroyed by the
immune system (Estcourt et al., 2017).
Minority blood donors are essential for a diverse supply
of blood because they provide greateraccessto corre-
sponding phenotypes, often rare ones, required for individ-
uals with diseases such as SCD and thalassemia. However,
minorities are historically underrepresented among blood
donors. In the United States, an estimated 11% to 21% of blood
donations are from minority populations based on the National
Blood Collection & Utilization Survey 2011 (U.S. Department
of Health and Human Services,2011).More recent surveys
from eight blood centers in 17 states noted decreasing blood
donations overall and a continued underrepresentation of mi-
nority donors. For example, Black or AA donors constituted
approximately 5% of alldonors from 2006 to 2015 (Yazer
et al., 2017). A decreased proportion of minority blood donors
has also been reported in Canada (Charbonneau & Daigneault,
2016) and France (Grassineau et al., 2007).
Increasing minority blood donations is a complex public
health issue with several barriers to minority blood donations.
Minorities have reported higher deferralrates and lack of
awareness about the process of blood donation (Frye et al.,
2014). Less than 1% of all donors experience events such as
fainting and fatigue (U.S.Department of Health and Human
Services, 2011); however, despite a relatively low occurrence
of adverse events, fear of these events is a commonly reported
barrier to blood donation among minority populations (Shaz,
Demmons, Hillyer, Jones, & Hillyer, 2009). Barriers to blood
donation also include defermentdue to low hemoglobin,
consisting of almost half (48%) of all deferrals from all poten-
tialdonors in the United States (U.S.Department of Health
and Human Services, 2011). Mobile blood drives remain the
major source (66%) of blood collections in the United States
(U.S. Department of Health and Human Services, 2011). These
blood drives often recruit minority populations in the commu-
nity, at local churches, and other gatherings, yet a substantial
or sustainable increase in donations from these blood drives
has not been found (Yazer et al., 2017).
The current knowledge on facilitators and barriers to
nority blood donations is limited. Systematic reviews on
donations and blood donors exist,although none address
blood donation issues specific to minorities and none rev
the race/ethnicity of study samples (Bagot, Murray, & Ma
2016; Bednall, Bove, Cheetham, & Murray, 2013; Godin,
Im, Bélanger-Gravel, & Amireault, 2012). In addition, Bed
et al. (2013) reviewed blood donation behavior and inten
and cited the need for research with minorities as they o
port additional barriers to blood donation. The purposes o
systematic review are to examine the facilitators and bar
minority blood donations and recommend strategies to in
donations in the community. Therefore, the following res
question was asked:Whatare the facilitators and barriers to
blood donation in minority populations?
METHODS
Search Strategy
Prior to beginning the systematic review, the principal in
gator (PI) conducted a preliminary search to ensure the a
sence of similar reviews and gain understanding of existi
literature on minority blood donations. We consulted exp
on systematic review and meta-analyses: a librarian with
tise in nursing and health literature and experts on mino
blood donation and blood transfusion complications asso
ated with the hemoglobinopathies of SCD and thalassem
on search approach and terminology and goals of the rev
The systematic review proceeded using Preferred Report
Items for Systematic Reviews and Meta-Analyses, and th
search question served as basis for identification,selection,
and appraisal of studies and collection and analysis of da
reviewed studies (Moher, Liberati, Tetzlaff, & Altman, 200
The literature search began in August 2017 using the
tronic databases CINAHL Plus With Full Text, Academic S
Complete, MEDLINE, PsycINFO, Sociological Collection,
Cochrane Library,ProQuest Dissertation and Theses,and
PubMed. Search alerts were also initiated for databases t
continued the search through December 2017. There we
no restrictions on publication year, publication type, or a
type. The keywords used in the search included combina
of the following words: blood donation, blood donor, mino
ity, AA, Black, race and ethnicity, and Hispanic or Latino.
The search databases and search combinations are prese
in Table 1.
Inclusion and Exclusion Criteria
Inclusion criteria were (a) data-based studies that sample
nority blood donors and minority blood donations or inclu
minorities in description of blood donor samples; (b) data
minority participants on process of blood donation;and (c)
English language. Exclusion criteria were (a) data-based
Nursing Research • May/June 2019• Volume 68• No. 3 Minority Blood Donations 219
on blood donation using blood center or national survey data
and (b) methodologicaland theoreticalstudies.In addition,
in multiple data-based reports of a single study sample, only
one sample was reported with data from each study analyzed.
The title and abstract of each article in the search pool
(n = 1,352) were carefully reviewed by the PI. Initial review fo-
cused on removal of duplicate articles and exclusion of articles
obviously not relevant to search terms (e.g.,animalstudies,
etc.). The resulting pool (n = 545) was further refined by ex-
cluding articles that focused on viral and bacterial infections,
genetic components of bloods, and risk for alloimmunization.
Articles originating from countries outside of the United States
were retained as long as the abstracts were in English. Detailed
review of abstracts excluded summary reports, historicalre-
views, literature reviews, editorials, periodicals, or news briefs
and articles that were not data based.
The remaining 42 full-text articles were reviewed in their
entirety. Of the articles reviewed, 18 articles contained demo-
graphic data from blood centers or “blood banks” and national
surveys.Some articles reported data from blood centers re-
garding the effectiveness of an intervention or program; how-
ever, the data were not linked to participants (e.g., an increase
in blood donations in a blood center was attributed to a pro-
gram without data to indicate that donors were engaged or
participated in program). We excluded articles that focused
on blood centers without data from minority blood donors
on donations.
Of the 24 remaining articles, 5 were qualitative studies, 2
were mixed methods, and 17 were quantitative descriptive.
Eight of the quantitative descriptive articles included qualita-
tive data and descriptions from participants, while 9 contained
quantitative data only.Statisticalmethods are relevantto a
meta-analysis to integrate the results of studies—particularly
intervention studies (Moher et al., 2009). Based on the pri-
marily descriptive data from the articles and the lack of interven-
tion studies, the systematic review proceeded as a descriptive
meta-synthesis (Finfgeld,2003),focusing on the facilitators
and barriers to blood donation in minority populations with
15 articles.
Meta-synthesis is the qualitative aggregation and interpre-
tation of descriptive findings that have been abstracted from
study findings (Finfgeld-Connett,2010).Similar to a meta-
analysis, a meta-synthesis includes a purpose, research ques-
tion, inclusion criteria,study and sample characteristics,
and qualitative data collection and data analysis technique
(Sherwood, 1999). A meta-synthesis examines a broad ph
nomenon (Finfgeld, 2003), such as facilitators and barriers
to blood donations in minority populations.
Data Abstraction
Data were abstracted from 15 articles in the following cate
gories: study design and data analysis methods, sample s
participant race/ethnicity and gender, donor type (nondon
or experienced donor), geographic location (United States
or other country), and community location (e.g., communi
church,college,etc.).Narratives from participants,themes,
and strategies presented were abstracted from the finding
cussions, and conclusions.
Data Analysis
An inductive approach was used to analyze commonalities
ferences,patterns,and themes in study findings;interpret the
findings; and synthesize the findings to generate new kno
about the phenomena of study (Finfgeld, 2003; Paterson,
The findings were categorized and later collapsed into the
(Finfgeld-Connett, 2010). The steps of the thematic analys
cluded (a) translating the findings of each study into them
(b) comparing and contrasting the themes by identifying s
ilarities and differences among themes, and (c) determinin
the key themes and hypothesizing how themes relate to e
other (Paterson, 2001).
In the analysis, each study was reviewed by the PI, and
themes were validated by the PI and the research team w
a total of three members (Paterson, 2001). The research t
had expertise with minority blood donations, minority pop
lations with SCD and thalassemia,research with minorities,
and qualitative methods. Sampling and data analysis deci
were recorded in field notes and an audit trail, and consen
on decisions was achieved among the research team (Finf
Connett, 2010; Paterson, 2001).
RESULTS
Study Selection
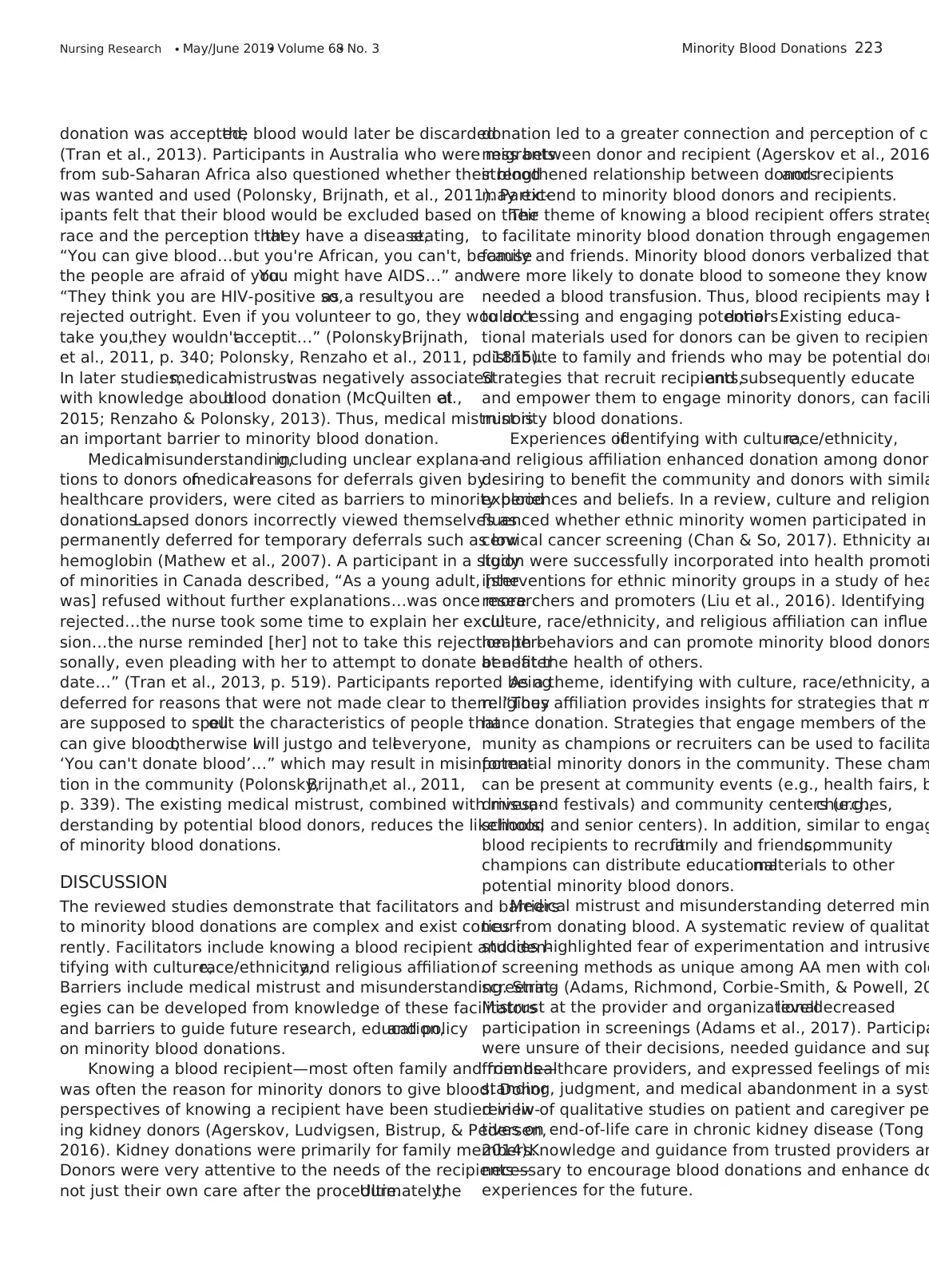
The initial search yielded 1,352 articles. After eliminating
cates and nonrelevant articles (n = 807), excluding article
abstract (n = 503), and excluding articles by full text (n =
15 articles were included in this systematic review (See Fi
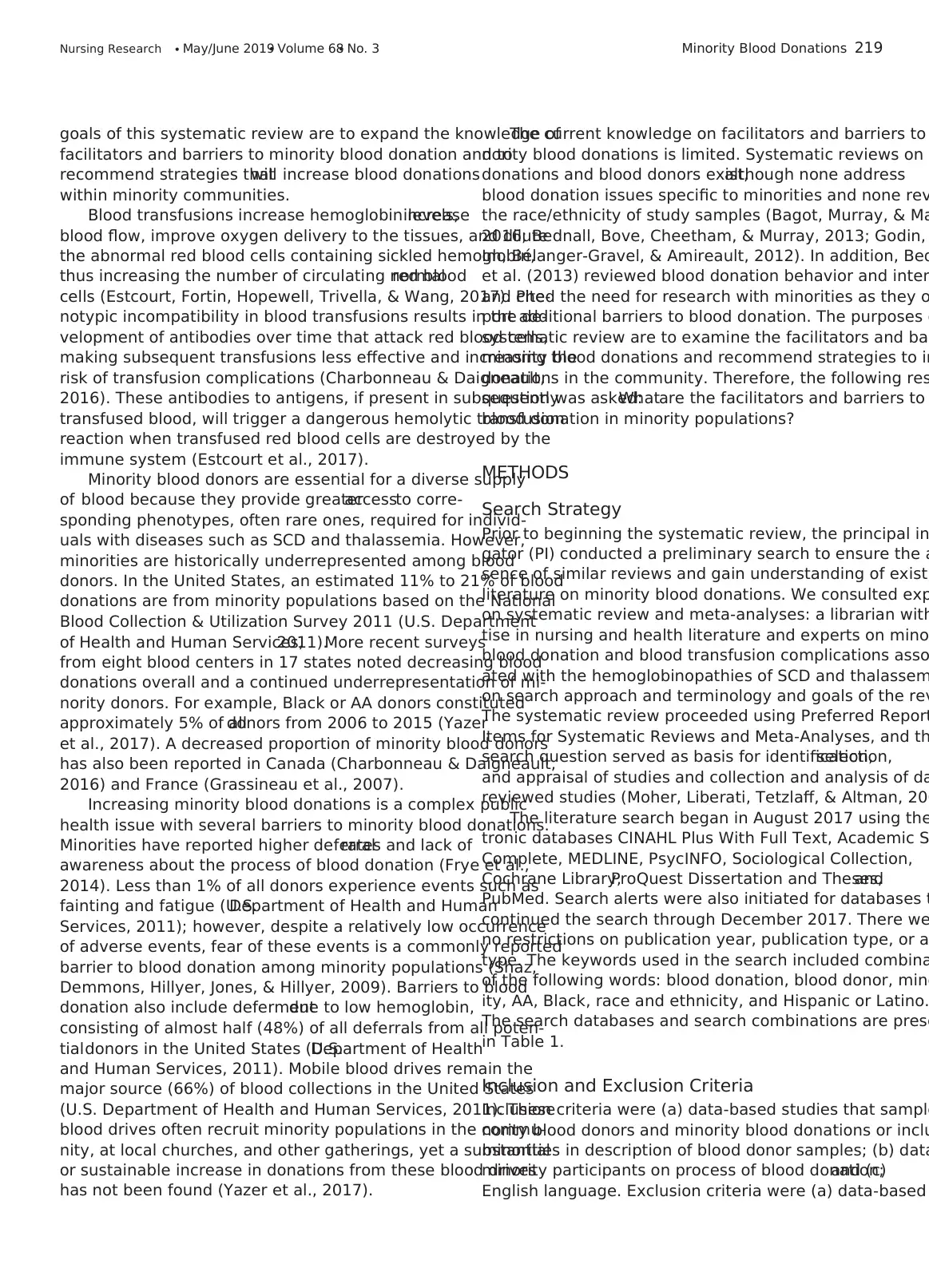
TABLE 1. Search Strategy
Database Search Terms Articles
CINAHL Plus with Full Text, Academic Search
Complete, MEDLINE, PsycINFO, Sociological
Collection
Blood donation OR Blood donor AND Minority groups
OR African American OR Black OR (Race and
ethnicity) OR (Hispanic or Latino)
n = 718
Cochrane Library, Proquest Dissertation and
Theses, PubMed
Blood donation OR blood donor AND minority OR
African-American OR race
n = 634
220 Minority Blood Donations www.nursingresearchonline.com
and (b) methodologicaland theoreticalstudies.In addition,
in multiple data-based reports of a single study sample, only
one sample was reported with data from each study analyzed.
The title and abstract of each article in the search pool
(n = 1,352) were carefully reviewed by the PI. Initial review fo-
cused on removal of duplicate articles and exclusion of articles
obviously not relevant to search terms (e.g.,animalstudies,
etc.). The resulting pool (n = 545) was further refined by ex-
cluding articles that focused on viral and bacterial infections,
genetic components of bloods, and risk for alloimmunization.
Articles originating from countries outside of the United States
were retained as long as the abstracts were in English. Detailed
review of abstracts excluded summary reports, historicalre-
views, literature reviews, editorials, periodicals, or news briefs
and articles that were not data based.
The remaining 42 full-text articles were reviewed in their
entirety. Of the articles reviewed, 18 articles contained demo-
graphic data from blood centers or “blood banks” and national
surveys.Some articles reported data from blood centers re-
garding the effectiveness of an intervention or program; how-
ever, the data were not linked to participants (e.g., an increase
in blood donations in a blood center was attributed to a pro-
gram without data to indicate that donors were engaged or
participated in program). We excluded articles that focused
on blood centers without data from minority blood donors
on donations.
Of the 24 remaining articles, 5 were qualitative studies, 2
were mixed methods, and 17 were quantitative descriptive.
Eight of the quantitative descriptive articles included qualita-
tive data and descriptions from participants, while 9 contained
quantitative data only.Statisticalmethods are relevantto a
meta-analysis to integrate the results of studies—particularly
intervention studies (Moher et al., 2009). Based on the pri-
marily descriptive data from the articles and the lack of interven-
tion studies, the systematic review proceeded as a descriptive
meta-synthesis (Finfgeld,2003),focusing on the facilitators
and barriers to blood donation in minority populations with
15 articles.
Meta-synthesis is the qualitative aggregation and interpre-
tation of descriptive findings that have been abstracted from
study findings (Finfgeld-Connett,2010).Similar to a meta-
analysis, a meta-synthesis includes a purpose, research ques-
tion, inclusion criteria,study and sample characteristics,
and qualitative data collection and data analysis technique
(Sherwood, 1999). A meta-synthesis examines a broad ph
nomenon (Finfgeld, 2003), such as facilitators and barriers
to blood donations in minority populations.
Data Abstraction
Data were abstracted from 15 articles in the following cate
gories: study design and data analysis methods, sample s
participant race/ethnicity and gender, donor type (nondon
or experienced donor), geographic location (United States
or other country), and community location (e.g., communi
church,college,etc.).Narratives from participants,themes,
and strategies presented were abstracted from the finding
cussions, and conclusions.
Data Analysis
An inductive approach was used to analyze commonalities
ferences,patterns,and themes in study findings;interpret the
findings; and synthesize the findings to generate new kno
about the phenomena of study (Finfgeld, 2003; Paterson,
The findings were categorized and later collapsed into the
(Finfgeld-Connett, 2010). The steps of the thematic analys
cluded (a) translating the findings of each study into them
(b) comparing and contrasting the themes by identifying s
ilarities and differences among themes, and (c) determinin
the key themes and hypothesizing how themes relate to e
other (Paterson, 2001).
In the analysis, each study was reviewed by the PI, and
themes were validated by the PI and the research team w
a total of three members (Paterson, 2001). The research t
had expertise with minority blood donations, minority pop
lations with SCD and thalassemia,research with minorities,
and qualitative methods. Sampling and data analysis deci
were recorded in field notes and an audit trail, and consen
on decisions was achieved among the research team (Finf
Connett, 2010; Paterson, 2001).
RESULTS
Study Selection
The initial search yielded 1,352 articles. After eliminating
cates and nonrelevant articles (n = 807), excluding article
abstract (n = 503), and excluding articles by full text (n =
15 articles were included in this systematic review (See Fi
TABLE 1. Search Strategy
Database Search Terms Articles
CINAHL Plus with Full Text, Academic Search
Complete, MEDLINE, PsycINFO, Sociological
Collection
Blood donation OR Blood donor AND Minority groups
OR African American OR Black OR (Race and
ethnicity) OR (Hispanic or Latino)
n = 718
Cochrane Library, Proquest Dissertation and
Theses, PubMed
Blood donation OR blood donor AND minority OR
African-American OR race
n = 634
220 Minority Blood Donations www.nursingresearchonline.com
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
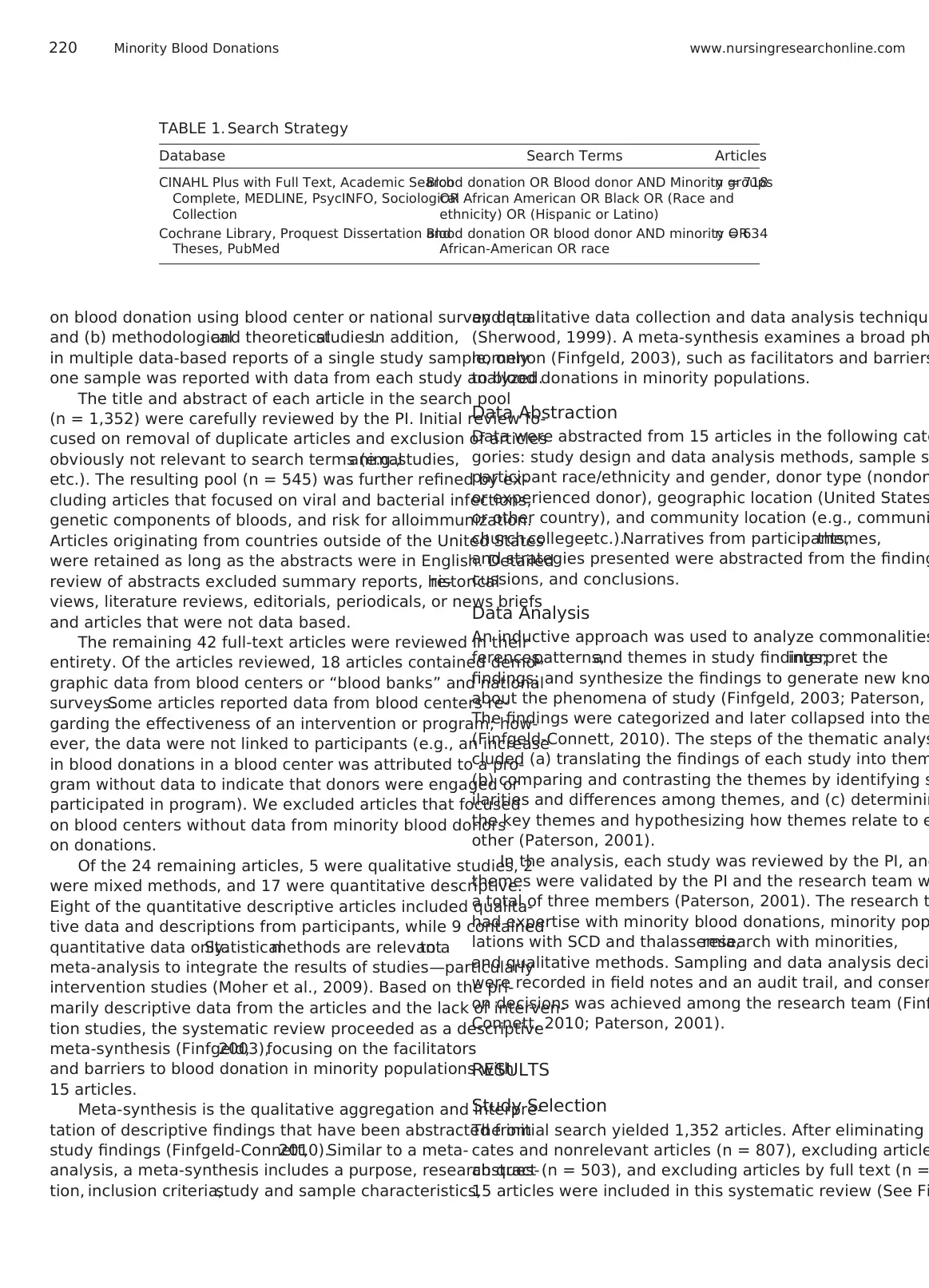
Evaluation of Article Pool
The final review article pool included 15 articles. Of note,
seven articles (47%) were published in the journal Transfusion,
a publication dedicated to blood banking and transfusion
medicine topics. Other articles were published in transfusion
medicine,hematology,and laboratory/pathology journals
(n = 5; 33%). Few articles were published in general medi-
cal and health-related journals (n = 3; 20%). All articles were
published in peer-reviewed journals.
Study and Sample Characteristics
The study sample included 3,698 participants.Participants'
race/ethnicity and gender were not described in allstudies.
Of the participants described, participants were Black or AA
(n = 2,125), White or Caucasian (n = 874), or other/not de-
fined (n = 699). Hispanic (n = 32) or Non-Hispanic (n = 134)
participants were also represented.
When reported, there were more male (n = 1,665) than fe-
male (n = 1,353) participants. There was variation in how stud-
ies presented donor data (e.g., never, first-time, repeat, routine,
“multi-gallon”); thus, participants were grouped as experienced
donors (n = 1,634) with a history of blood donation or nonex-
perienced donors (n = 799) with no history of blood donation.
Studies recruited from the community (n = 11 studies), blood
centers (n = 3),and colleges (n = 1) in the United States
(n = 7),Australia (n = 4),Canada (n = 2),and regions of
Africa (n = 2).
Themes
The themes that were identified from the data provided i
sights into the experiences of minorities with blood dona
Common themes emerged from the analysis of the descr
tions and narratives.Shared themes included (a) knowing a
blood recipient;(b) identifying with culture,race/ethnicity,
and religious affiliation; and (c) medical mistrust and mis
standing. These themes are described below, and data a
sented to support the themes.
Knowing a Blood RecipientThe theme of knowing a blood
recipient reflected connection to family and friends in ne
of blood transfusions (Amoyal et al., 2013; Asenso-Mensa
Achina, Appiah, Owusu-Ofori, &Allain, 2014; Charbonnea
Tran,2013;Royse & Doochin,1995;Tran,Charbonneau,
Valderrama-Benitez, 2013). Donors were characterized a
rect family (parents,siblings,or children),indirect family
(grandparents, uncle or aunt, or spouse), and not family
church member, school, or work mate) in a study of dono
potentially becoming repeatdonorsin sub-Saharan Africa
(Asenso-Mensah et al., 2014). The participants donated b
FIGURE 1. Article selection pool for the systematic review.
Nursing Research • May/June 2019• Volume 68• No. 3 Minority Blood Donations 221
The final review article pool included 15 articles. Of note,
seven articles (47%) were published in the journal Transfusion,
a publication dedicated to blood banking and transfusion
medicine topics. Other articles were published in transfusion
medicine,hematology,and laboratory/pathology journals
(n = 5; 33%). Few articles were published in general medi-
cal and health-related journals (n = 3; 20%). All articles were
published in peer-reviewed journals.
Study and Sample Characteristics
The study sample included 3,698 participants.Participants'
race/ethnicity and gender were not described in allstudies.
Of the participants described, participants were Black or AA
(n = 2,125), White or Caucasian (n = 874), or other/not de-
fined (n = 699). Hispanic (n = 32) or Non-Hispanic (n = 134)
participants were also represented.
When reported, there were more male (n = 1,665) than fe-
male (n = 1,353) participants. There was variation in how stud-
ies presented donor data (e.g., never, first-time, repeat, routine,
“multi-gallon”); thus, participants were grouped as experienced
donors (n = 1,634) with a history of blood donation or nonex-
perienced donors (n = 799) with no history of blood donation.
Studies recruited from the community (n = 11 studies), blood
centers (n = 3),and colleges (n = 1) in the United States
(n = 7),Australia (n = 4),Canada (n = 2),and regions of
Africa (n = 2).
Themes
The themes that were identified from the data provided i
sights into the experiences of minorities with blood dona
Common themes emerged from the analysis of the descr
tions and narratives.Shared themes included (a) knowing a
blood recipient;(b) identifying with culture,race/ethnicity,
and religious affiliation; and (c) medical mistrust and mis
standing. These themes are described below, and data a
sented to support the themes.
Knowing a Blood RecipientThe theme of knowing a blood
recipient reflected connection to family and friends in ne
of blood transfusions (Amoyal et al., 2013; Asenso-Mensa
Achina, Appiah, Owusu-Ofori, &Allain, 2014; Charbonnea
Tran,2013;Royse & Doochin,1995;Tran,Charbonneau,
Valderrama-Benitez, 2013). Donors were characterized a
rect family (parents,siblings,or children),indirect family
(grandparents, uncle or aunt, or spouse), and not family
church member, school, or work mate) in a study of dono
potentially becoming repeatdonorsin sub-Saharan Africa
(Asenso-Mensah et al., 2014). The participants donated b
FIGURE 1. Article selection pool for the systematic review.
Nursing Research • May/June 2019• Volume 68• No. 3 Minority Blood Donations 221
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
“because they were asked” and because “the patient needed
blood” (Asenso-Mensah et al., 2014, p. 800). In a study of pro-
cesses of change to increase blood donation for AA in the
United States, responses were “hearing people's personal stories
is inspiring” and “something happens to someone in my family,”
when asked aboutemotions associated with donating blood
(Amoyal et al., 2013, p. 1283).
Donating blood to someone that they know was com-
monly described by minority participants. Both multigallon do-
nors and periodic donors reported having someone in their
families who had received blood as a reason to donate in a
study of differences among donor groups (Royse & Doochin,
1995). A request from friends or family was also a common
reason to donate blood in a study of AA church members in
Atlanta (Shaz et al.,2009).Participants described needing
transfusions themselves or knowing people who needed blood
transfusions,stating that they gave “for their children” or
“for their family and neighbors” (Charbonneau & Tran, 2013,
p. 177). One participant stated, “…it's very well looked upon
to give our blood to family…but giving to a stranger, I think
that's a little more limited,” suggesting that donating to family
was preferred overdonation to an unknown recipient
(Charbonneau & Tran,2013,p. 177).Participants revealed
that they were more inclined to donate to a member of their
family orcommunity,stating,“…if you know the person
and the person is sick…help with some blood…” and “Giving
to a member of the family or wife, say she is having a baby and
she is hemorrhaging, I'm sure most fathers would say, ‘hey,
give some blood because it's his wife and his kid…’” (Tran
et al., 2013, p. 519). Knowing a blood recipient made a donor
or potential donor more likely to donate blood.
Identifying With Culture, Race/Ethnicity, and Religious
AffiliationThe theme of identifying with culture, race/ethnicity,
and religious affiliation is an extended commitment beyond
family and friends to a larger community ofculture,race/
ethnicity, and/or religion. Participants identified cultural and
ethnic similarities and differences and religious beliefs that af-
fected blood donations (Charbonneau & Tran, 2013; Mathew
et al., 2007; Polonsky, Brijnath, & Renzaho, 2011; Renzaho &
Polonsky, 2013; Robbins et al., 2015; Tran et al., 2013).
Culture was the focus of studies of migrant minorities. In a
study of sub-Saharan AA migrants in Australia, the role of home
country culture included the need for approval from family as
partof their culture;however,participants acknowledged
they would disregard culture and family approvalif those
thatthey knew needed blood (Polonsky,Brijnath,et al.,
2011). In later studies, the authors found that acculturation
was not associated with blood donation for African migrants
in Australia and that their home culture beliefs were still
prevalent (McQuilten, Polonsky, & Renzaho, 2015; Renzaho
& Polonsky, 2013). Culture is a consideration in whether or
not an individual chooses to donate blood.
Participants expressed openness to messages promoti
blood donations in communities to specific races. For bloo
center employees, community leaders, and donors in Can
Black participants felt more comfortable donating to some
in the community and suggested the promotion of blood d
tion using strategies that focused on the community (Tran
2013). In a study of donors and nondonors by Mathew et a
(2007,p. 733),Black participants described community as
“the AA community” and felt that donating to benefit their
own community, such as blood drives for SCD or victims o
violence, was a motivator to donate blood. In a culturally t
lored intervention study to promote minority blood donatio
participants described “feeling guilty for notdonating” after
completing the intervention (Robbins et al., 2015, p. 232).
tifying with culture and race/ethnicity may increase the lik
hood of donating blood by minorities.
Ethnicity and religion are described as a unique part of
nority blood donations.Participants from ethnic minorities
perceived the uniqueness of their blood and described, “…
ing something good for society,” with giving blood being “
combination between a generous act and an obligation,for
you and the community…,” in a study of the symbolism of
blood donation in Canada (Charbonneau & Tran,2013,pp.
175–176). Religious values were associated with blood don
tion, with participants noting, “…blood is a symbol of sacri
fice, of life…” and “…you are giving life when you are givi
blood…” (Charbonneau & Tran,2013,p. 177).Identifying
with ethnicity and religion provided a reason to donate blo
for some minorities.
MedicalMistrust and MisunderstandingThe theme of
medical mistrust and misunderstanding, including not und
standing the medicalreasons for deferral, was described by
participants as barriers to minority blood donation (Boulwa
et al.,2002;Grossman,Watkins,Fleming & Debaun,2005;
Mathew et al., 2007; McQuilten et al., 2015; Oswalt & Gord
1993; Polonsky, Brijnath, et al.,2011;Polonsky,Renzaho,&
Brijnath, 2011; Renzaho & Polonsky, 2013; Tran et al., 201
Participants reported the lingering effects ofthe Tuskegee
Syphilis Study and other medical experiments that exploit
minorities, as well as exclusion from donating during the 1
during the human immunodeficiency virus (HIV) epidemic
barriers to donating (Polonsky, Brijnath, et al., 2011; Polon
Renzaho, et al., 2011; Tran et al., 2013). In a focus group s
of donors and nondonors, participants mentioned a news s
aboutthe waste ofdonated blood in the aftermath ofthe
September 11 in the United States as another reason to n
nate (Mathew et al., 2007).
A commonly held idea among Black participants was th
blood donation was somewhat suspicious, their blood was
wanted, and their blood should preferably not be given (Tr
et al., 2013). Black leaders from Caribbean and African ori
believed that they could not give blood, or that if their blo
222 Minority Blood Donations www.nursingresearchonline.com
blood” (Asenso-Mensah et al., 2014, p. 800). In a study of pro-
cesses of change to increase blood donation for AA in the
United States, responses were “hearing people's personal stories
is inspiring” and “something happens to someone in my family,”
when asked aboutemotions associated with donating blood
(Amoyal et al., 2013, p. 1283).
Donating blood to someone that they know was com-
monly described by minority participants. Both multigallon do-
nors and periodic donors reported having someone in their
families who had received blood as a reason to donate in a
study of differences among donor groups (Royse & Doochin,
1995). A request from friends or family was also a common
reason to donate blood in a study of AA church members in
Atlanta (Shaz et al.,2009).Participants described needing
transfusions themselves or knowing people who needed blood
transfusions,stating that they gave “for their children” or
“for their family and neighbors” (Charbonneau & Tran, 2013,
p. 177). One participant stated, “…it's very well looked upon
to give our blood to family…but giving to a stranger, I think
that's a little more limited,” suggesting that donating to family
was preferred overdonation to an unknown recipient
(Charbonneau & Tran,2013,p. 177).Participants revealed
that they were more inclined to donate to a member of their
family orcommunity,stating,“…if you know the person
and the person is sick…help with some blood…” and “Giving
to a member of the family or wife, say she is having a baby and
she is hemorrhaging, I'm sure most fathers would say, ‘hey,
give some blood because it's his wife and his kid…’” (Tran
et al., 2013, p. 519). Knowing a blood recipient made a donor
or potential donor more likely to donate blood.
Identifying With Culture, Race/Ethnicity, and Religious
AffiliationThe theme of identifying with culture, race/ethnicity,
and religious affiliation is an extended commitment beyond
family and friends to a larger community ofculture,race/
ethnicity, and/or religion. Participants identified cultural and
ethnic similarities and differences and religious beliefs that af-
fected blood donations (Charbonneau & Tran, 2013; Mathew
et al., 2007; Polonsky, Brijnath, & Renzaho, 2011; Renzaho &
Polonsky, 2013; Robbins et al., 2015; Tran et al., 2013).
Culture was the focus of studies of migrant minorities. In a
study of sub-Saharan AA migrants in Australia, the role of home
country culture included the need for approval from family as
partof their culture;however,participants acknowledged
they would disregard culture and family approvalif those
thatthey knew needed blood (Polonsky,Brijnath,et al.,
2011). In later studies, the authors found that acculturation
was not associated with blood donation for African migrants
in Australia and that their home culture beliefs were still
prevalent (McQuilten, Polonsky, & Renzaho, 2015; Renzaho
& Polonsky, 2013). Culture is a consideration in whether or
not an individual chooses to donate blood.
Participants expressed openness to messages promoti
blood donations in communities to specific races. For bloo
center employees, community leaders, and donors in Can
Black participants felt more comfortable donating to some
in the community and suggested the promotion of blood d
tion using strategies that focused on the community (Tran
2013). In a study of donors and nondonors by Mathew et a
(2007,p. 733),Black participants described community as
“the AA community” and felt that donating to benefit their
own community, such as blood drives for SCD or victims o
violence, was a motivator to donate blood. In a culturally t
lored intervention study to promote minority blood donatio
participants described “feeling guilty for notdonating” after
completing the intervention (Robbins et al., 2015, p. 232).
tifying with culture and race/ethnicity may increase the lik
hood of donating blood by minorities.
Ethnicity and religion are described as a unique part of
nority blood donations.Participants from ethnic minorities
perceived the uniqueness of their blood and described, “…
ing something good for society,” with giving blood being “
combination between a generous act and an obligation,for
you and the community…,” in a study of the symbolism of
blood donation in Canada (Charbonneau & Tran,2013,pp.
175–176). Religious values were associated with blood don
tion, with participants noting, “…blood is a symbol of sacri
fice, of life…” and “…you are giving life when you are givi
blood…” (Charbonneau & Tran,2013,p. 177).Identifying
with ethnicity and religion provided a reason to donate blo
for some minorities.
MedicalMistrust and MisunderstandingThe theme of
medical mistrust and misunderstanding, including not und
standing the medicalreasons for deferral, was described by
participants as barriers to minority blood donation (Boulwa
et al.,2002;Grossman,Watkins,Fleming & Debaun,2005;
Mathew et al., 2007; McQuilten et al., 2015; Oswalt & Gord
1993; Polonsky, Brijnath, et al.,2011;Polonsky,Renzaho,&
Brijnath, 2011; Renzaho & Polonsky, 2013; Tran et al., 201
Participants reported the lingering effects ofthe Tuskegee
Syphilis Study and other medical experiments that exploit
minorities, as well as exclusion from donating during the 1
during the human immunodeficiency virus (HIV) epidemic
barriers to donating (Polonsky, Brijnath, et al., 2011; Polon
Renzaho, et al., 2011; Tran et al., 2013). In a focus group s
of donors and nondonors, participants mentioned a news s
aboutthe waste ofdonated blood in the aftermath ofthe
September 11 in the United States as another reason to n
nate (Mathew et al., 2007).
A commonly held idea among Black participants was th
blood donation was somewhat suspicious, their blood was
wanted, and their blood should preferably not be given (Tr
et al., 2013). Black leaders from Caribbean and African ori
believed that they could not give blood, or that if their blo
222 Minority Blood Donations www.nursingresearchonline.com
donation was accepted,the blood would later be discarded
(Tran et al., 2013). Participants in Australia who were migrants
from sub-Saharan Africa also questioned whether their blood
was wanted and used (Polonsky, Brijnath, et al., 2011). Partic-
ipants felt that their blood would be excluded based on their
race and the perception thatthey have a disease,stating,
“You can give blood…but you're African, you can't, because
the people are afraid of you.You might have AIDS…” and
“They think you are HIV-positive so,as a result,you are
rejected outright. Even if you volunteer to go, they wouldn't
take you,they wouldn'tacceptit…” (Polonsky,Brijnath,
et al., 2011, p. 340; Polonsky, Renzaho et al., 2011, p. 1815).
In later studies,medicalmistrustwas negatively associated
with knowledge aboutblood donation (McQuilten etal.,
2015; Renzaho & Polonsky, 2013). Thus, medical mistrust is
an important barrier to minority blood donation.
Medicalmisunderstanding,including unclear explana-
tions to donors ofmedicalreasons for deferrals given by
healthcare providers, were cited as barriers to minority blood
donations.Lapsed donors incorrectly viewed themselves as
permanently deferred for temporary deferrals such as low
hemoglobin (Mathew et al., 2007). A participant in a study
of minorities in Canada described, “As a young adult, [she
was] refused without further explanations…was once more
rejected…the nurse took some time to explain her exclu-
sion…the nurse reminded [her] not to take this rejection per-
sonally, even pleading with her to attempt to donate at a later
date…” (Tran et al., 2013, p. 519). Participants reported being
deferred for reasons that were not made clear to them: “They
are supposed to spellout the characteristics of people that
can give blood,otherwise Iwill justgo and telleveryone,
‘You can't donate blood’…” which may result in misinforma-
tion in the community (Polonsky,Brijnath,et al., 2011,
p. 339). The existing medical mistrust, combined with misun-
derstanding by potential blood donors, reduces the likelihood
of minority blood donations.
DISCUSSION
The reviewed studies demonstrate that facilitators and barriers
to minority blood donations are complex and exist concur-
rently. Facilitators include knowing a blood recipient and iden-
tifying with culture,race/ethnicity,and religious affiliation.
Barriers include medical mistrust and misunderstanding. Strat-
egies can be developed from knowledge of these facilitators
and barriers to guide future research, education,and policy
on minority blood donations.
Knowing a blood recipient—most often family and friends—
was often the reason for minority donors to give blood. Donor
perspectives of knowing a recipient have been studied in liv-
ing kidney donors (Agerskov, Ludvigsen, Bistrup, & Pedersen,
2016). Kidney donations were primarily for family members.
Donors were very attentive to the needs of the recipients—
not just their own care after the procedure.Ultimately,the
donation led to a greater connection and perception of cl
ness between donor and recipient (Agerskov et al., 2016
strengthened relationship between donorsand recipients
may extend to minority blood donors and recipients.
The theme of knowing a blood recipient offers strateg
to facilitate minority blood donation through engagemen
family and friends. Minority blood donors verbalized that
were more likely to donate blood to someone they know
needed a blood transfusion. Thus, blood recipients may b
to accessing and engaging potentialdonors.Existing educa-
tional materials used for donors can be given to recipient
distribute to family and friends who may be potential don
Strategies that recruit recipients,and subsequently educate
and empower them to engage minority donors, can facili
minority blood donations.
Experiences ofidentifying with culture,race/ethnicity,
and religious affiliation enhanced donation among donor
desiring to benefit the community and donors with simila
experiences and beliefs. In a review, culture and religion
fluenced whether ethnic minority women participated in
cervical cancer screening (Chan & So, 2017). Ethnicity an
ligion were successfully incorporated into health promoti
interventions for ethnic minority groups in a study of hea
researchers and promoters (Liu et al., 2016). Identifying
culture, race/ethnicity, and religious affiliation can influen
health behaviors and can promote minority blood donors
benefit the health of others.
As a theme, identifying with culture, race/ethnicity, a
religious affiliation provides insights for strategies that m
hance donation. Strategies that engage members of the
munity as champions or recruiters can be used to facilita
potential minority donors in the community. These cham
can be present at community events (e.g., health fairs, b
drives,and festivals) and community centers (e.g.,churches,
schools, and senior centers). In addition, similar to engag
blood recipients to recruitfamily and friends,community
champions can distribute educationalmaterials to other
potential minority blood donors.
Medical mistrust and misunderstanding deterred min
ties from donating blood. A systematic review of qualitat
studies highlighted fear of experimentation and intrusive
of screening methods as unique among AA men with colo
screening (Adams, Richmond, Corbie-Smith, & Powell, 20
Mistrust at the provider and organizationalleveldecreased
participation in screenings (Adams et al., 2017). Participa
were unsure of their decisions, needed guidance and sup
from healthcare providers, and expressed feelings of mis
standing, judgment, and medical abandonment in a syste
review of qualitative studies on patient and caregiver pe
tives on end-of-life care in chronic kidney disease (Tong
2014).Knowledge and guidance from trusted providers ar
necessary to encourage blood donations and enhance do
experiences for the future.
Nursing Research • May/June 2019• Volume 68• No. 3 Minority Blood Donations 223
(Tran et al., 2013). Participants in Australia who were migrants
from sub-Saharan Africa also questioned whether their blood
was wanted and used (Polonsky, Brijnath, et al., 2011). Partic-
ipants felt that their blood would be excluded based on their
race and the perception thatthey have a disease,stating,
“You can give blood…but you're African, you can't, because
the people are afraid of you.You might have AIDS…” and
“They think you are HIV-positive so,as a result,you are
rejected outright. Even if you volunteer to go, they wouldn't
take you,they wouldn'tacceptit…” (Polonsky,Brijnath,
et al., 2011, p. 340; Polonsky, Renzaho et al., 2011, p. 1815).
In later studies,medicalmistrustwas negatively associated
with knowledge aboutblood donation (McQuilten etal.,
2015; Renzaho & Polonsky, 2013). Thus, medical mistrust is
an important barrier to minority blood donation.
Medicalmisunderstanding,including unclear explana-
tions to donors ofmedicalreasons for deferrals given by
healthcare providers, were cited as barriers to minority blood
donations.Lapsed donors incorrectly viewed themselves as
permanently deferred for temporary deferrals such as low
hemoglobin (Mathew et al., 2007). A participant in a study
of minorities in Canada described, “As a young adult, [she
was] refused without further explanations…was once more
rejected…the nurse took some time to explain her exclu-
sion…the nurse reminded [her] not to take this rejection per-
sonally, even pleading with her to attempt to donate at a later
date…” (Tran et al., 2013, p. 519). Participants reported being
deferred for reasons that were not made clear to them: “They
are supposed to spellout the characteristics of people that
can give blood,otherwise Iwill justgo and telleveryone,
‘You can't donate blood’…” which may result in misinforma-
tion in the community (Polonsky,Brijnath,et al., 2011,
p. 339). The existing medical mistrust, combined with misun-
derstanding by potential blood donors, reduces the likelihood
of minority blood donations.
DISCUSSION
The reviewed studies demonstrate that facilitators and barriers
to minority blood donations are complex and exist concur-
rently. Facilitators include knowing a blood recipient and iden-
tifying with culture,race/ethnicity,and religious affiliation.
Barriers include medical mistrust and misunderstanding. Strat-
egies can be developed from knowledge of these facilitators
and barriers to guide future research, education,and policy
on minority blood donations.
Knowing a blood recipient—most often family and friends—
was often the reason for minority donors to give blood. Donor
perspectives of knowing a recipient have been studied in liv-
ing kidney donors (Agerskov, Ludvigsen, Bistrup, & Pedersen,
2016). Kidney donations were primarily for family members.
Donors were very attentive to the needs of the recipients—
not just their own care after the procedure.Ultimately,the
donation led to a greater connection and perception of cl
ness between donor and recipient (Agerskov et al., 2016
strengthened relationship between donorsand recipients
may extend to minority blood donors and recipients.
The theme of knowing a blood recipient offers strateg
to facilitate minority blood donation through engagemen
family and friends. Minority blood donors verbalized that
were more likely to donate blood to someone they know
needed a blood transfusion. Thus, blood recipients may b
to accessing and engaging potentialdonors.Existing educa-
tional materials used for donors can be given to recipient
distribute to family and friends who may be potential don
Strategies that recruit recipients,and subsequently educate
and empower them to engage minority donors, can facili
minority blood donations.
Experiences ofidentifying with culture,race/ethnicity,
and religious affiliation enhanced donation among donor
desiring to benefit the community and donors with simila
experiences and beliefs. In a review, culture and religion
fluenced whether ethnic minority women participated in
cervical cancer screening (Chan & So, 2017). Ethnicity an
ligion were successfully incorporated into health promoti
interventions for ethnic minority groups in a study of hea
researchers and promoters (Liu et al., 2016). Identifying
culture, race/ethnicity, and religious affiliation can influen
health behaviors and can promote minority blood donors
benefit the health of others.
As a theme, identifying with culture, race/ethnicity, a
religious affiliation provides insights for strategies that m
hance donation. Strategies that engage members of the
munity as champions or recruiters can be used to facilita
potential minority donors in the community. These cham
can be present at community events (e.g., health fairs, b
drives,and festivals) and community centers (e.g.,churches,
schools, and senior centers). In addition, similar to engag
blood recipients to recruitfamily and friends,community
champions can distribute educationalmaterials to other
potential minority blood donors.
Medical mistrust and misunderstanding deterred min
ties from donating blood. A systematic review of qualitat
studies highlighted fear of experimentation and intrusive
of screening methods as unique among AA men with colo
screening (Adams, Richmond, Corbie-Smith, & Powell, 20
Mistrust at the provider and organizationalleveldecreased
participation in screenings (Adams et al., 2017). Participa
were unsure of their decisions, needed guidance and sup
from healthcare providers, and expressed feelings of mis
standing, judgment, and medical abandonment in a syste
review of qualitative studies on patient and caregiver pe
tives on end-of-life care in chronic kidney disease (Tong
2014).Knowledge and guidance from trusted providers ar
necessary to encourage blood donations and enhance do
experiences for the future.
Nursing Research • May/June 2019• Volume 68• No. 3 Minority Blood Donations 223
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
The theme of medicalmistrust and misunderstanding
presents a significant, longstanding barrier for minority blood
donations; however, strategies that reduce this barrier and in-
crease trust and knowledge can increase donations. The direct
engagement of the community using educationalmaterials,
community educators, and addressing any lingering issues with
trust and previous experiences should be a routine strategy.
Participants described consistent issues and historicalevents.
These topics must be the focus of conversations with potential
donors. Blood recipients and champions in communities can
also increase trust and knowledge.
Recommendations for Research, Practice, Policy, and
Education
This study confirms the need for community education and
communication about blood donation and its positive effect
on fellow community members, including friends and family,
in racial and ethnic minorities that are underrepresented among
blood donors. It further suggests the need to rebuild trust among
minority communities.
Future research should include theory-based, quantitative,
and intervention studies in minority populations. The emerg-
ing use of theoretical frameworks shows promise in study de-
velopment and provides a basis for future studies for minority
blood donations.The TranstheoreticalModel(Prochaska &
DiClemente,1983) and Theory of Planned Behavior (Ajzen,
1991) are well-established theories thathave been used in
public health and other disciplines to describe an individual's
behavior. Both are suitable to study the behaviors of blood
donors, including minorities. Assimilation Theory (Gordon,
1964) and Culture Fusion Theory (Kramer, 2000) focus on
culture and are well-suited for studies with underrepresented
minority blood donors. In addition, studies on blood donors
and blood donations should include minority participants—
whether the study itself is focused on minorities—and data
should be presented to reflect any differences in minority
perceptions and outcomes. A single web-based intervention
study found in the review was conducted in the United States
(Robbins et al., 2015). There is a need for well-developed inter-
vention studies that focus on minority populations.
Blood donations are a specialized area of clinical practice
with specific approaches to donors and donation protocols.
Healthcare providers who do not practice in this area may have
limited knowledge of blood donation protocols and may be fur-
ther limited with no personal experience as a donor, therefore
limiting the ability to engage donors and promote donations
in minority populations.Meta-synthesis findings can lead to
the development of clinical protocols (Finfgeld-Connett, 2010),
and findings from this review emphasize the need for tai-
lored approaches and protocols for minority blood donors.
The findings from meta-synthesis studies can also facilitate
development of healthcare policy (Finfgeld-Connett,2010).
Policy on U.S. blood donations should focus on national efforts
to engage minority blood donors and use advocates and
stakeholders in the community to enhance grassroots effo
(Singleton & Spratling, 2018). Studies conducted outside o
United States primarily focused on blood donations among
grantminorities,racialand ethnic disparities,and barriers to
blood donations imposed on migrants.This illustrates the
need to address policies that affect the ability to donate b
by minorities.
Of note, this review found frequent recurrence of spec
authors and research teams,indicating that few researchers
are focusing on this much-needed area of research. In add
the majority of articles were published in journals focused
transfusions and blood disorders, leaving a knowledge gap
nursing, medical, public health, and other general health l
ature. Dissemination of knowledge on minority blood dono
and blood donations is needed in a variety of journals targ
many disciplines and healthcare providers.Lay information
should also be developed for and dispersed to potential do
and minority communities.
Limitations
This systematic review was limited by varied data and me
across studies. The authors adhered to rigorous data abstr
tion and analysis, but the variation in studies may have lim
the review. The focus of the review was studies on minorit
blood donations; however, there were studies that include
both minority and nonminority populations.The data pre-
sented from these studies may not have exclusively prese
or separated minority participant data.
CONCLUSION
This systematic review adds to the growing body of literat
on minority blood donations, expanding knowledge of faci
tors and barriers and recommending strategies to increase
nority blood donations in the community.Previous studies,
including systematic reviews, have presented isolated find
on minority blood donations. This systematic review and m
synthesis analyzed and summarized the findings from a sa
of descriptive studies to present overarching themes from
studies and subsequently present strategies to facilitate a
decrease barriers to minority blood donations.
Accepted for publication October 19, 2018.
The research reported in this publication was supported by Cooperati
Agreement 5 NU58 DD001138-03, funded by the Centers for Disease
Control and Prevention (CDC). The content is solely the responsibility
the authors and do not necessarily represent the officialviews of the
CDC or the Department of Health and Human Services.
The authors have no conflicts of interest to report.
The authors would like to thank Ashley Singleton, MPH, research asso
the Georgia Health Policy Center at Georgia State University, for her a
and support of this work.
Corresponding author: Regena Spratling, PhD, RN, APRN, CPNP, Georg
State University School of Nursing, P.O. Box 4019, Atlanta, GA 30302-
(e-mail: rspratling@gsu.edu).
224 Minority Blood Donations www.nursingresearchonline.com
presents a significant, longstanding barrier for minority blood
donations; however, strategies that reduce this barrier and in-
crease trust and knowledge can increase donations. The direct
engagement of the community using educationalmaterials,
community educators, and addressing any lingering issues with
trust and previous experiences should be a routine strategy.
Participants described consistent issues and historicalevents.
These topics must be the focus of conversations with potential
donors. Blood recipients and champions in communities can
also increase trust and knowledge.
Recommendations for Research, Practice, Policy, and
Education
This study confirms the need for community education and
communication about blood donation and its positive effect
on fellow community members, including friends and family,
in racial and ethnic minorities that are underrepresented among
blood donors. It further suggests the need to rebuild trust among
minority communities.
Future research should include theory-based, quantitative,
and intervention studies in minority populations. The emerg-
ing use of theoretical frameworks shows promise in study de-
velopment and provides a basis for future studies for minority
blood donations.The TranstheoreticalModel(Prochaska &
DiClemente,1983) and Theory of Planned Behavior (Ajzen,
1991) are well-established theories thathave been used in
public health and other disciplines to describe an individual's
behavior. Both are suitable to study the behaviors of blood
donors, including minorities. Assimilation Theory (Gordon,
1964) and Culture Fusion Theory (Kramer, 2000) focus on
culture and are well-suited for studies with underrepresented
minority blood donors. In addition, studies on blood donors
and blood donations should include minority participants—
whether the study itself is focused on minorities—and data
should be presented to reflect any differences in minority
perceptions and outcomes. A single web-based intervention
study found in the review was conducted in the United States
(Robbins et al., 2015). There is a need for well-developed inter-
vention studies that focus on minority populations.
Blood donations are a specialized area of clinical practice
with specific approaches to donors and donation protocols.
Healthcare providers who do not practice in this area may have
limited knowledge of blood donation protocols and may be fur-
ther limited with no personal experience as a donor, therefore
limiting the ability to engage donors and promote donations
in minority populations.Meta-synthesis findings can lead to
the development of clinical protocols (Finfgeld-Connett, 2010),
and findings from this review emphasize the need for tai-
lored approaches and protocols for minority blood donors.
The findings from meta-synthesis studies can also facilitate
development of healthcare policy (Finfgeld-Connett,2010).
Policy on U.S. blood donations should focus on national efforts
to engage minority blood donors and use advocates and
stakeholders in the community to enhance grassroots effo
(Singleton & Spratling, 2018). Studies conducted outside o
United States primarily focused on blood donations among
grantminorities,racialand ethnic disparities,and barriers to
blood donations imposed on migrants.This illustrates the
need to address policies that affect the ability to donate b
by minorities.
Of note, this review found frequent recurrence of spec
authors and research teams,indicating that few researchers
are focusing on this much-needed area of research. In add
the majority of articles were published in journals focused
transfusions and blood disorders, leaving a knowledge gap
nursing, medical, public health, and other general health l
ature. Dissemination of knowledge on minority blood dono
and blood donations is needed in a variety of journals targ
many disciplines and healthcare providers.Lay information
should also be developed for and dispersed to potential do
and minority communities.
Limitations
This systematic review was limited by varied data and me
across studies. The authors adhered to rigorous data abstr
tion and analysis, but the variation in studies may have lim
the review. The focus of the review was studies on minorit
blood donations; however, there were studies that include
both minority and nonminority populations.The data pre-
sented from these studies may not have exclusively prese
or separated minority participant data.
CONCLUSION
This systematic review adds to the growing body of literat
on minority blood donations, expanding knowledge of faci
tors and barriers and recommending strategies to increase
nority blood donations in the community.Previous studies,
including systematic reviews, have presented isolated find
on minority blood donations. This systematic review and m
synthesis analyzed and summarized the findings from a sa
of descriptive studies to present overarching themes from
studies and subsequently present strategies to facilitate a
decrease barriers to minority blood donations.
Accepted for publication October 19, 2018.
The research reported in this publication was supported by Cooperati
Agreement 5 NU58 DD001138-03, funded by the Centers for Disease
Control and Prevention (CDC). The content is solely the responsibility
the authors and do not necessarily represent the officialviews of the
CDC or the Department of Health and Human Services.
The authors have no conflicts of interest to report.
The authors would like to thank Ashley Singleton, MPH, research asso
the Georgia Health Policy Center at Georgia State University, for her a
and support of this work.
Corresponding author: Regena Spratling, PhD, RN, APRN, CPNP, Georg
State University School of Nursing, P.O. Box 4019, Atlanta, GA 30302-
(e-mail: rspratling@gsu.edu).
224 Minority Blood Donations www.nursingresearchonline.com
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
REFERENCES
Adams, L. B., Richmond, J., Corbie-Smith, G., & Powell, W. (2017).
Medical mistrust and colorectal cancer screening among African
Americans.Journal of Community Health,42, 1044–1061.
doi:10.1007/s10900-017-0339-2
Agerskov, H., Ludvigsen, M. S., Bistrup, C., & Pedersen, B. D. (2016).
From donation to everyday life: Living kidney donors' experiences
three months after donation. Journal of Renal Care, 42, 43–52.
doi:10.1111/jorc.12137
Ajzen, I. (1991). The theory of planned behavior. Organizational Behav-
ior and Human Decision Processes, 50, 179–211. doi:10.1016/0749-
5978(91)90020-T
Amoyal, N. R., Robbins, M. L., Paiva, A. L., Burditt, C., Kessler, D., &
Shaz, B. H. (2013). Measuring the processes of change for increas-
ing blood donation in black adults. Transfusion, 53, 1280–1290.
doi:10.1111/j.1537-2995.2012.03864.x
Asenso-Mensah, K., Achina, G., Appiah, R., Owusu-Ofori, S., & Allain,
J. P. (2014). Can family or replacement blood donors become regular
volunteer donors? Transfusion, 54, 797–804. doi:10.1111/trf.12216
Bagot, K. L., Murray, A. L., & Masser, B. M. (2016). How can we
improve retention of the first-time donor? A systematic review
of the currentevidence.Transfusion Medicine Reviews,30,
81–91. doi:10.1016/j.tmrv.2016.02.002
Bednall, T. C., Bove, L. L., Cheetham, A., & Murray, A. L. (2013). A
systematic review and meta-analysis ofantecedents ofblood
donation behavior and intentions. Social Science & Medicine,
96, 86–94. doi:10.1016/j.socscimed.2013.07.022
Boulware, L. E., Ratner, L. E., Ness, P. M., Cooper, L. A., Campbell-Lee,
S., LaVeist,T. A., & Powe, N. R. (2002).The contribution of
sociodemographic, medical, and attitudinal factors to blood do-
nation among the generalpublic. Transfusion,42, 669–678.
doi:10.1046/j.1537-2995.2002.00120.x
Chan, D. N. S., & So, W. K. W. (2017). A systematic review of the fac-
tors influencing ethnic minority women's cervical cancer screen-
ing behavior: From intrapersonal to policy level. Cancer Nursing,
40, E1–E30. doi:10.1097/NCC.0000000000000436
Charbonneau, J., & Daigneault, S. (2016). Engaging ethnic minority
blood donors.ISBT Science Series,11, 140–147.doi:10.1111/
voxs.12203
Charbonneau, J., & Tran, N. Y. L. (2013). The symbolic roots of blood
donation. Transfusion, 53, 172S–179S. doi:10.1111/trf.12477
Estcourt, L. J., Fortin, P. M., Hopewell, S., Trivella, M., & Wang, W. C.
(2017). Blood transfusion for preventing primary and secondary
stroke in people with sickle celldisease. Cochrane Database
of Systematic Reviews, 1, CD003146.doi:10.1002/14651858.
CD003146.pub3
Finfgeld, D. (2003). Metasynthesis: The state of the art—So far. Qualita-
tive Health Research, 13, 893–904. doi:10.1177/1049732303253462
Finfgeld-Connett,D. (2010).Generalizability and transferability of
meta-synthesis research findings. Journal of Advanced Nursing,
66, 246–254. doi:10.1111/j.1365-2648.2009.05250.x
Frye,V., Caltabiano,M., Kessler,D. A., Schaffler,H., Reboza,M.,
Hillyer, C. D., & Shaz, B. H. (2014).Evaluating a program
to increase blood donation among racial and ethnic minority
communities in New York City.Transfusion,54, 3061–3067.
doi:10.1111/trf.12767
Godin,G., Vézina-Im,L. A., Bélanger-Gravel,A., & Amireault,S.
(2012). Efficacy of interventions promoting blood donation: A sys-
tematic review. Transfusion Medicine Reviews, 26, 224–237.e6.
doi:10.1016/j.tmrv.2011.10.001
Gordon,M. M. (1964).Assimilation in American life:The role of
race, religion, and national origins. New York, NY: Oxford Uni-
versity Press.
Grassineau, D., Papa, K., Ducourneau, A., Duboz, P., Boëtsch, G.,
Chiaroni, J. (2007). Improving minority blood donation: Anthro
approach in a migrant community.Transfusion,47, 402–409.
doi:10.1111/j.1537-2995.2007.01130.x
Grossman, B., Watkins, A. R., Fleming, F., & Debaun, M. R. (2005
Barriers and motivators to blood and cord blood donations in
young African-American women. American Journal of Hemato
78, 198–202. doi:10.1002/ajh.20308
Hassell, K. L. (2010). Population estimates of sickle cell disease i
U.S. American Journal of Preventive Medicine, 38, S512–S521
doi:10.1016/j.amepre.2009.12.022
Kramer, E. M. (2000). Cultural fusion and the defense of differen
M. K. Asante & E. & Min (Eds.), Socio-cultural conflict between
African and Korean Americans (ed., pp. 182–223). New York,
NY: University Press of America.
Li, C. K. (2017). New trend in the epidemiology of thalassaemia.
Practice & Research ClinicalObstetrics& Gynaecology,39,
16–26. doi:10.1016/j.bpobgyn.2016.10.013
Liu, J. J., Davidson, E., Bhopal, R., White, M., Johnson, M., Netto, G
Sheikh,A. (2016).Adapting health promotion interventions for
ethnic minority groups: A qualitative study. Health Promotion
ternational, 31, 325–334. doi:10.1093/heapro/dau105
Mathew, S. M., King, M. R., Glynn, S. A., Dietz, S. K., Caswell, S. L
Schreiber,G. B. (2007).Opinions about donating blood among
those who never gave and those who stopped: A focus group
assessment.Transfusion, 47, 729–735.doi:10.1111/j.1537-
2995.2007.01177.x
McQuilten, Z. K., Polonsky, M. J., & Renzaho, A. N. (2015). Blood
nation by African migrants and refugees in Australia. ISBT Sci
Series, 10, 257–262. doi:10.1111/voxs.12162
Moher,D., Liberati,A., Tetzlaff,J., & Altman,D. (2009).Preferred
reporting items for systematic reviews and meta-analyses:The
PRISMA statement. Annals of Internal Medicine, 151, 264–269
doi:10.7326/0003-4819-151-4-200908180-00135
Oswalt, R., & Gordon, J. (1993). Blood donor motivation: A surve
minority college students.PsychologicalReports,72, 785–786.
doi:10.2466/pr0.1993.72.3.785
Paterson, B. L. (2001). The shifting perspectives model of chroni
ness.Journal of Nursing Scholarship,33, 21–26.doi:10.1111/
j.1547-5069.2001.00021.x
Polonsky,M. J., Brijnath,B., & Renzaho, A. M. (2011).“They don't
want our blood”:Socialinclusion and blood donation among
African migrants in Australia.SocialScience & Medicine,73,
336–342. doi:10.1016/j.socscimed.2011.05.030
Polonsky, M. J., Renzaho, A. M. N., & Brijnath, B. (2011). Barriers
blood donation in African communities in Australia: The role o
home and hostcountry culture and experience.Transfusion,
51, 1809–1819. doi:10.1111/j.1537-2995.2010.03053.x
Prochaska, J. O., & DiClemente, C. C. (1983). Stages and process
self-change of smoking: Toward an integrative model of chan
Journal of Consulting and Clinical Psychology, 51, 390–395.
Renzaho, A. M. N., & Polonsky, M. J. (2013). The influence of accu
turation,medicalmistrust,and perceived discrimination on
knowledge aboutblood donation and blood donation status.
Transfusion, 53, 162S–171S. doi:10.1111/trf.12476
Robbins, M. L., Paiva, A. L., Amoyal, N. R., Brick, L., Kessler, D. A
Burditt, C., … Shaz, B. H. (2015). Acceptability and feasibility
a culturally tailored internet-delivered intervention to promote
blood donation in Blacks. Health Promotion Practice, 16, 227–
doi:10.1177/1524839914533344
Royse, D., & Doochin, K. E. (1995). Multi-gallon blood donors: Wh
are they? Transfusion, 35, 826–831. doi:10.1046/j.1537-2995
351096026363.x
Nursing Research • May/June 2019• Volume 68• No. 3 Minority Blood Donations 225
Adams, L. B., Richmond, J., Corbie-Smith, G., & Powell, W. (2017).
Medical mistrust and colorectal cancer screening among African
Americans.Journal of Community Health,42, 1044–1061.
doi:10.1007/s10900-017-0339-2
Agerskov, H., Ludvigsen, M. S., Bistrup, C., & Pedersen, B. D. (2016).
From donation to everyday life: Living kidney donors' experiences
three months after donation. Journal of Renal Care, 42, 43–52.
doi:10.1111/jorc.12137
Ajzen, I. (1991). The theory of planned behavior. Organizational Behav-
ior and Human Decision Processes, 50, 179–211. doi:10.1016/0749-
5978(91)90020-T
Amoyal, N. R., Robbins, M. L., Paiva, A. L., Burditt, C., Kessler, D., &
Shaz, B. H. (2013). Measuring the processes of change for increas-
ing blood donation in black adults. Transfusion, 53, 1280–1290.
doi:10.1111/j.1537-2995.2012.03864.x
Asenso-Mensah, K., Achina, G., Appiah, R., Owusu-Ofori, S., & Allain,
J. P. (2014). Can family or replacement blood donors become regular
volunteer donors? Transfusion, 54, 797–804. doi:10.1111/trf.12216
Bagot, K. L., Murray, A. L., & Masser, B. M. (2016). How can we
improve retention of the first-time donor? A systematic review
of the currentevidence.Transfusion Medicine Reviews,30,
81–91. doi:10.1016/j.tmrv.2016.02.002
Bednall, T. C., Bove, L. L., Cheetham, A., & Murray, A. L. (2013). A
systematic review and meta-analysis ofantecedents ofblood
donation behavior and intentions. Social Science & Medicine,
96, 86–94. doi:10.1016/j.socscimed.2013.07.022
Boulware, L. E., Ratner, L. E., Ness, P. M., Cooper, L. A., Campbell-Lee,
S., LaVeist,T. A., & Powe, N. R. (2002).The contribution of
sociodemographic, medical, and attitudinal factors to blood do-
nation among the generalpublic. Transfusion,42, 669–678.
doi:10.1046/j.1537-2995.2002.00120.x
Chan, D. N. S., & So, W. K. W. (2017). A systematic review of the fac-
tors influencing ethnic minority women's cervical cancer screen-
ing behavior: From intrapersonal to policy level. Cancer Nursing,
40, E1–E30. doi:10.1097/NCC.0000000000000436
Charbonneau, J., & Daigneault, S. (2016). Engaging ethnic minority
blood donors.ISBT Science Series,11, 140–147.doi:10.1111/
voxs.12203
Charbonneau, J., & Tran, N. Y. L. (2013). The symbolic roots of blood
donation. Transfusion, 53, 172S–179S. doi:10.1111/trf.12477
Estcourt, L. J., Fortin, P. M., Hopewell, S., Trivella, M., & Wang, W. C.
(2017). Blood transfusion for preventing primary and secondary
stroke in people with sickle celldisease. Cochrane Database
of Systematic Reviews, 1, CD003146.doi:10.1002/14651858.
CD003146.pub3
Finfgeld, D. (2003). Metasynthesis: The state of the art—So far. Qualita-
tive Health Research, 13, 893–904. doi:10.1177/1049732303253462
Finfgeld-Connett,D. (2010).Generalizability and transferability of
meta-synthesis research findings. Journal of Advanced Nursing,
66, 246–254. doi:10.1111/j.1365-2648.2009.05250.x
Frye,V., Caltabiano,M., Kessler,D. A., Schaffler,H., Reboza,M.,
Hillyer, C. D., & Shaz, B. H. (2014).Evaluating a program
to increase blood donation among racial and ethnic minority
communities in New York City.Transfusion,54, 3061–3067.
doi:10.1111/trf.12767
Godin,G., Vézina-Im,L. A., Bélanger-Gravel,A., & Amireault,S.
(2012). Efficacy of interventions promoting blood donation: A sys-
tematic review. Transfusion Medicine Reviews, 26, 224–237.e6.
doi:10.1016/j.tmrv.2011.10.001
Gordon,M. M. (1964).Assimilation in American life:The role of
race, religion, and national origins. New York, NY: Oxford Uni-
versity Press.
Grassineau, D., Papa, K., Ducourneau, A., Duboz, P., Boëtsch, G.,
Chiaroni, J. (2007). Improving minority blood donation: Anthro
approach in a migrant community.Transfusion,47, 402–409.
doi:10.1111/j.1537-2995.2007.01130.x
Grossman, B., Watkins, A. R., Fleming, F., & Debaun, M. R. (2005
Barriers and motivators to blood and cord blood donations in
young African-American women. American Journal of Hemato
78, 198–202. doi:10.1002/ajh.20308
Hassell, K. L. (2010). Population estimates of sickle cell disease i
U.S. American Journal of Preventive Medicine, 38, S512–S521
doi:10.1016/j.amepre.2009.12.022
Kramer, E. M. (2000). Cultural fusion and the defense of differen
M. K. Asante & E. & Min (Eds.), Socio-cultural conflict between
African and Korean Americans (ed., pp. 182–223). New York,
NY: University Press of America.
Li, C. K. (2017). New trend in the epidemiology of thalassaemia.
Practice & Research ClinicalObstetrics& Gynaecology,39,
16–26. doi:10.1016/j.bpobgyn.2016.10.013
Liu, J. J., Davidson, E., Bhopal, R., White, M., Johnson, M., Netto, G
Sheikh,A. (2016).Adapting health promotion interventions for
ethnic minority groups: A qualitative study. Health Promotion
ternational, 31, 325–334. doi:10.1093/heapro/dau105
Mathew, S. M., King, M. R., Glynn, S. A., Dietz, S. K., Caswell, S. L
Schreiber,G. B. (2007).Opinions about donating blood among
those who never gave and those who stopped: A focus group
assessment.Transfusion, 47, 729–735.doi:10.1111/j.1537-
2995.2007.01177.x
McQuilten, Z. K., Polonsky, M. J., & Renzaho, A. N. (2015). Blood
nation by African migrants and refugees in Australia. ISBT Sci
Series, 10, 257–262. doi:10.1111/voxs.12162
Moher,D., Liberati,A., Tetzlaff,J., & Altman,D. (2009).Preferred
reporting items for systematic reviews and meta-analyses:The
PRISMA statement. Annals of Internal Medicine, 151, 264–269
doi:10.7326/0003-4819-151-4-200908180-00135
Oswalt, R., & Gordon, J. (1993). Blood donor motivation: A surve
minority college students.PsychologicalReports,72, 785–786.
doi:10.2466/pr0.1993.72.3.785
Paterson, B. L. (2001). The shifting perspectives model of chroni
ness.Journal of Nursing Scholarship,33, 21–26.doi:10.1111/
j.1547-5069.2001.00021.x
Polonsky,M. J., Brijnath,B., & Renzaho, A. M. (2011).“They don't
want our blood”:Socialinclusion and blood donation among
African migrants in Australia.SocialScience & Medicine,73,
336–342. doi:10.1016/j.socscimed.2011.05.030
Polonsky, M. J., Renzaho, A. M. N., & Brijnath, B. (2011). Barriers
blood donation in African communities in Australia: The role o
home and hostcountry culture and experience.Transfusion,
51, 1809–1819. doi:10.1111/j.1537-2995.2010.03053.x
Prochaska, J. O., & DiClemente, C. C. (1983). Stages and process
self-change of smoking: Toward an integrative model of chan
Journal of Consulting and Clinical Psychology, 51, 390–395.
Renzaho, A. M. N., & Polonsky, M. J. (2013). The influence of accu
turation,medicalmistrust,and perceived discrimination on
knowledge aboutblood donation and blood donation status.
Transfusion, 53, 162S–171S. doi:10.1111/trf.12476
Robbins, M. L., Paiva, A. L., Amoyal, N. R., Brick, L., Kessler, D. A
Burditt, C., … Shaz, B. H. (2015). Acceptability and feasibility
a culturally tailored internet-delivered intervention to promote
blood donation in Blacks. Health Promotion Practice, 16, 227–
doi:10.1177/1524839914533344
Royse, D., & Doochin, K. E. (1995). Multi-gallon blood donors: Wh
are they? Transfusion, 35, 826–831. doi:10.1046/j.1537-2995
351096026363.x
Nursing Research • May/June 2019• Volume 68• No. 3 Minority Blood Donations 225
Shaz, B. H., Demmons, D. G., Hillyer, K. L., Jones, R. E., & Hillyer, C. D.
(2009). Racial differences in motivators and barriers to blood dona-
tion among blood donors.Archives of Pathology & Laboratory
Medicine, 133, 1444–1447. doi:10.1043/1543-2165-133.9.1444
Sherwood, G. (1999). Meta-synthesis: Merging qualitative studies to
develop nursing knowledge. International Journal for Human
Caring, 3, 37–42.
Singleton, A., & Spratling, R. (2018). A strategic planning tool for in-
creasing African American blood donation.Health Promotion
Practice, 1524839918775733. doi:10.1177/1524839918775733
Tong, A., Cheung, K. L., Nair, S. S., Kurella Tamura, M., Craig, J. C., &
Winkelmayer,W. C. (2014).Thematic synthesis ofqualitative
studies on patient and caregiver perspectives on end-of-life care
in CKD. American Journalof Kidney Diseases,63, 913–927.
doi:10.1053/j.ajkd.2013.11.017
Tran, N. Y., Charbonneau, J., & Valderrama-Benitez, V. (2013). Blo
donation practices,motivations and beliefs in Montreal's Black
communities:The modern gift under a new light.Ethnicity &
Health, 18, 508–529. doi:10.1080/13557858.2012.734279
U.S. Department of Health and Human Services (2011). National B
Collection & Utilization Survey 2011, Retrieved February 19, 20
from https://www.hhs.gov/sites/default/files/ash/bloodsafety/
2011-nbcus.pdf.
Yazer,M. H., Delaney,M., Germain,M., Karafin,M. S.,Sayers,M.,
Vassallo, R., … Shaz, B. (2017). Trends in US minority red blood
unit donations. Transfusion, 57, 1226–1234. doi:10.1111/trf.14
Call for Papers: Point-of-Care Research Series
Nursing Research invites papers reporting findings from original point-of-care research studies. Topics includ
butare notlimited to use of devices and information technology atthe point-of-care,patientsafety issues,m-health,
telehealth, system interoperability, design and evaluation of “smart” environments across the health-illness
continuum, learning health systems; communication and decision making in emerging technology-supported
point-of-care settings; quality and ethical issues. Papers may be enhanced to include video or interactive gra
supplemental digital content. In advance of submission, queries to the Editor are encouraged but not
required. Submissions may be regular full-length papers or research briefs. In the letter to the editor uploade
submissions, please mention that the paper should be considered for the point-of-care research series.
There is no deadline for submission; accepted papers will be published in regular issues and marked with a b
for the “Point-of-Care Research” series.
Queries are encouraged and should be sent to Dr. Susan Henly, Editor-in-Chief, e-mail: henly003@umn.edu.
Information for Authors is available at: www.nursingresearchonline.com. Select the “For Authors and Reviewe
Nursing Research is indexed or abstracted in Medline, CINAHL, JCR Science Citation Index, PsychInfo and
Thomson Reuters Web of ScienceSM.
226 Minority Blood Donations www.nursingresearchonline.com
(2009). Racial differences in motivators and barriers to blood dona-
tion among blood donors.Archives of Pathology & Laboratory
Medicine, 133, 1444–1447. doi:10.1043/1543-2165-133.9.1444
Sherwood, G. (1999). Meta-synthesis: Merging qualitative studies to
develop nursing knowledge. International Journal for Human
Caring, 3, 37–42.
Singleton, A., & Spratling, R. (2018). A strategic planning tool for in-
creasing African American blood donation.Health Promotion
Practice, 1524839918775733. doi:10.1177/1524839918775733
Tong, A., Cheung, K. L., Nair, S. S., Kurella Tamura, M., Craig, J. C., &
Winkelmayer,W. C. (2014).Thematic synthesis ofqualitative
studies on patient and caregiver perspectives on end-of-life care
in CKD. American Journalof Kidney Diseases,63, 913–927.
doi:10.1053/j.ajkd.2013.11.017
Tran, N. Y., Charbonneau, J., & Valderrama-Benitez, V. (2013). Blo
donation practices,motivations and beliefs in Montreal's Black
communities:The modern gift under a new light.Ethnicity &
Health, 18, 508–529. doi:10.1080/13557858.2012.734279
U.S. Department of Health and Human Services (2011). National B
Collection & Utilization Survey 2011, Retrieved February 19, 20
from https://www.hhs.gov/sites/default/files/ash/bloodsafety/
2011-nbcus.pdf.
Yazer,M. H., Delaney,M., Germain,M., Karafin,M. S.,Sayers,M.,
Vassallo, R., … Shaz, B. (2017). Trends in US minority red blood
unit donations. Transfusion, 57, 1226–1234. doi:10.1111/trf.14
Call for Papers: Point-of-Care Research Series
Nursing Research invites papers reporting findings from original point-of-care research studies. Topics includ
butare notlimited to use of devices and information technology atthe point-of-care,patientsafety issues,m-health,
telehealth, system interoperability, design and evaluation of “smart” environments across the health-illness
continuum, learning health systems; communication and decision making in emerging technology-supported
point-of-care settings; quality and ethical issues. Papers may be enhanced to include video or interactive gra
supplemental digital content. In advance of submission, queries to the Editor are encouraged but not
required. Submissions may be regular full-length papers or research briefs. In the letter to the editor uploade
submissions, please mention that the paper should be considered for the point-of-care research series.
There is no deadline for submission; accepted papers will be published in regular issues and marked with a b
for the “Point-of-Care Research” series.
Queries are encouraged and should be sent to Dr. Susan Henly, Editor-in-Chief, e-mail: henly003@umn.edu.
Information for Authors is available at: www.nursingresearchonline.com. Select the “For Authors and Reviewe
Nursing Research is indexed or abstracted in Medline, CINAHL, JCR Science Citation Index, PsychInfo and
Thomson Reuters Web of ScienceSM.
226 Minority Blood Donations www.nursingresearchonline.com
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.
