Systemic Inflammation and Organ Dysfunction in a Patient with Asthma
VerifiedAdded on 2023/04/11
|7
|3250
|302
AI Summary
This report discusses the disruption of the immune system in relation to normal functioning of physiological systems in a patient with asthma, leading to systemic inflammation and organ dysfunction.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
Faculty of Health and Life Sciences
This proforma MUST be used to submit your report
Refer to the 212BMS coursework assignment brief for details and submission deadline.
Remember to convert this document to a PDF before submitting using the Turnitin link provided.
STUDENT ID: Click or tap here to enter text.
WORD COUNT: 1638
Write your report here:
Introduction
An analysis of the case study suggests that the patient X (pseudonym) had a history of asthmatic
symptoms, and had been admitted to the care facility for the treatment of persisting signs and symptoms of
fever, cough and wheezing. It can be suggested that the patient suffered from cough-variant asthma that is
commonly manifested in the form of persistent, non-productive cough, generally without mucus formation.
Upon admission, abnormalities were observed in her vital signs that suggested the presence of tachypnea,
tachycardia, poor oxygen saturation, high body temperature, and hypotension. In addition, it can be stated that
the patient reported gradual reduction in the levels of oxygen saturation, which in turn demonstrated the
presence of hypoxemia that prevented normal functioning of the cells, due to a shortage of oxygen in the
bloodstream. Low urine output and elevated blood urea levels also provided indication for the failure of the
renal system to function effectively, thus leading to accumulation of waste products in the body, and subsequent
death of the patient. This report will discuss the disruption of the immune system, in relation to normal
functioning of physiological system in the patient that ultimately resulted in death.
Innate immune system
The innate immune system is referred to as an evolutionary strategy of defence against a range of
infections. The system gets activated following an attack by any pathogen and is primarily composed of several
barriers that prevent the entry of bacteria, viruses, foreign particles and other parasites inside the human body.
Some of the major functions of the innate immune system comprise of recruitment of immune cells to infection
sites, via the production of chemical factors and mediators like cytokines. Another potential role of the system
can be accredited to the activation of a signalling cascade that facilitates bacteria recognition, thereby promoting
antibody complex clearance (Lackey and Olefsky 2016). Prior to triggering any immune factors, the skin acts as
an impassable, continuous barrier to the pathogens that get inactivated or killed by the acidity of the skin and/or
desiccation (Iwasaki and Medzhitov 2015). Alternate defence mechanisms are present in other regions of the
Module: 212BMS Systemic Physiology
COURSEWORK Proforma
2018-19
This proforma MUST be used to submit your report
Refer to the 212BMS coursework assignment brief for details and submission deadline.
Remember to convert this document to a PDF before submitting using the Turnitin link provided.
STUDENT ID: Click or tap here to enter text.
WORD COUNT: 1638
Write your report here:
Introduction
An analysis of the case study suggests that the patient X (pseudonym) had a history of asthmatic
symptoms, and had been admitted to the care facility for the treatment of persisting signs and symptoms of
fever, cough and wheezing. It can be suggested that the patient suffered from cough-variant asthma that is
commonly manifested in the form of persistent, non-productive cough, generally without mucus formation.
Upon admission, abnormalities were observed in her vital signs that suggested the presence of tachypnea,
tachycardia, poor oxygen saturation, high body temperature, and hypotension. In addition, it can be stated that
the patient reported gradual reduction in the levels of oxygen saturation, which in turn demonstrated the
presence of hypoxemia that prevented normal functioning of the cells, due to a shortage of oxygen in the
bloodstream. Low urine output and elevated blood urea levels also provided indication for the failure of the
renal system to function effectively, thus leading to accumulation of waste products in the body, and subsequent
death of the patient. This report will discuss the disruption of the immune system, in relation to normal
functioning of physiological system in the patient that ultimately resulted in death.
Innate immune system
The innate immune system is referred to as an evolutionary strategy of defence against a range of
infections. The system gets activated following an attack by any pathogen and is primarily composed of several
barriers that prevent the entry of bacteria, viruses, foreign particles and other parasites inside the human body.
Some of the major functions of the innate immune system comprise of recruitment of immune cells to infection
sites, via the production of chemical factors and mediators like cytokines. Another potential role of the system
can be accredited to the activation of a signalling cascade that facilitates bacteria recognition, thereby promoting
antibody complex clearance (Lackey and Olefsky 2016). Prior to triggering any immune factors, the skin acts as
an impassable, continuous barrier to the pathogens that get inactivated or killed by the acidity of the skin and/or
desiccation (Iwasaki and Medzhitov 2015). Alternate defence mechanisms are present in other regions of the
Module: 212BMS Systemic Physiology
COURSEWORK Proforma
2018-19
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
body such as the mucus membranes and eyes that secrete mucus and tears for rinsing away the pathogens. Cilia
lining the nasal passages also trap the pathogen, and prevents infection. In addition, low pH present in the
stomach also inhibits pathogen growth and disrupts the cell membrane of the bacteria, thereby preventing
pathogen attack (Martini, Nath and Bartholomew 2014).
Inefficacy of the treatment that was implemented upon X resulted in the onset and development of
systemic inflammatory response syndrome (SIRS), commonly refers to an inflammatory state that affects the
entire human body. According to Kaukonen et al. (2013) the condition manifests in the form of response of the
entire body against a non-infectious or infectious insult and has several anti- and pro-inflammatory components.
Some of the common manifestations of SIRS comprise of an elevated body temperature (higher than 38 °C),
elevated heart rate (>90bpm), high respiratory rate (>20), and reduced WBC count in the blood. Taking into
consideration the fact that the patient X manifested tachycardia, tachypnea, and increased body temperature, it
can be suggested that the treatment administered was not effective in protecting the body against pathogen
attack, thereby leading to systematic inflammation, and subsequent dysfunction and failure of the organs.
SIRS and respiratory system
The respiratory system maintains homeostasis in two different ways namely, gaseous exchange and
blood pH regulation. The lungs participate in gas exchange through the elimination of carbon dioxide, a waste
product that is produced during cellular respiration. Removal of carbon dioxide from the body results in entry of
oxygen in the lungs that is required for cellular respiration (Guyenet and Bayliss 2015). Normal respiration rate
is associated with an estimated 12-25 breaths per minute. Tachypnea typically occurs under circumstances when
the respiratory rate is greater than 20 breaths/minute and is generally manifested in the form of shortness of
breath and retracting chest during breathing. On sensing the presence of an infection in the body, the innate
immune system releases chemicals in the bloodstream that results in an inflammation in the body and interferes
with the flow of blood to the vital organs, thus leading to tachypnea (Censoplano, Epting and Coates 2014).
Taking into consideration the fact that asthmatic conditions reported by the patient resulted in lung damage and
allowed more viruses and bacteria to invade the body, thus causing infection, the innate immune system, X
might have had eosinophilic inflammation in the lungs (Lambrecht and Hammad 2015). However, failure in
restoration of homeostasis resulted in a major systemic reaction where cytokine release promoted destruction of
cellular integrity and end-organ dysfunction.
Furthermore, history of asthma in the patient can be associated with the failure of the innate immune
system that was responsible for chronic inflammation of the airway conducting zone, thus leading to the
development of tachypnea. Furthermore, gradual decrease in the oxygen saturation levels in the patient can be
accredited to the fact that severe attack of asthma lead to hypoxia in the patient (Silverthorn 2013). The
condition is a typical hallmark of infected and inflamed tissue and the adaptation to inadequate tissue
oxygenation is regulated by hypoxia-inducible factors (HIFs) (Semenza 2014). In addition, a characteristic
attribute of the cells of the immune system is to penetrate and operate in cells and tissues that have low levels of
oxygen and nutrients. However, onset of SIRS resulted in failure of expression of hypoxia-inducible
transcription factors HIFs, thereby decreasing the oxygen saturation levels in the patients.
SIRS and cardiovascular system
The major mechanism of the cardiovascular system in homeostasis maintenance depends on the
controlled and continuous movement of bloodstream though the capillaries, permeating the cells and tissues of
the human body (Fox 2013). There is mounting evidence for the association between inflammation and atrial
fibrillation that occurs due to a maladaptive hyperimmune response, which in turn is triggered by pathogen
infection (Harada, Van Wagoner and Nattel 2015). The onset of tachycardia in the patient can be explained by
the fact that multiorgan dysfunction syndrome (MODS) and SIRS result in prognostically pertinent cardiac
autonomic dysfunction. This is generally manifested via strong attenuation of vagally and sympathetically
governed heart rate variability (HRV) (Balk 2014). In addition, the immune mechanisms that underlie the
process of attenuation are not just restricted to the nervous system, and encompass variations in the cells of the
cardiac pacemaker on a cellular level.
According to Ebelt et al. (2015) endotoxin typically interacts with hyperpolarization-activated cyclic
nucleotide-gated (HCN) ion channels that are located in the heart, which in turn mediate the pacemaker current.
This also transmits vagal signals on heart rate and HRV. Failure of the innate immune system also resulted in
abnormal firing of the cardiac electrical signals, thus speeding up the heart rate and causing tachycardia in the
patient. In addition, the decreased pumping efficiency of the left portion of the heart resulted in fluid build-up in
the lungs that was responsible for wheezing, breathlessness, and tachycardia (Widmaier et al. 2011).
Furthermore, the pathologic condition of circulatory shock also occurred due to a mismatch between the demand
and supply of oxygen, and led to inadequate tissue perfusion, thus bringing about multiple organ failure and
dysfunction (Cecconi et al. 2014). In addition, although hydrocortisone is used for treating the inflammation in
asthmatic conditions, the corticosteroid failed to treat the patient, thus deteriorating the patient condition (Rang
et al. 2014).
SIRS and renal system
lining the nasal passages also trap the pathogen, and prevents infection. In addition, low pH present in the
stomach also inhibits pathogen growth and disrupts the cell membrane of the bacteria, thereby preventing
pathogen attack (Martini, Nath and Bartholomew 2014).
Inefficacy of the treatment that was implemented upon X resulted in the onset and development of
systemic inflammatory response syndrome (SIRS), commonly refers to an inflammatory state that affects the
entire human body. According to Kaukonen et al. (2013) the condition manifests in the form of response of the
entire body against a non-infectious or infectious insult and has several anti- and pro-inflammatory components.
Some of the common manifestations of SIRS comprise of an elevated body temperature (higher than 38 °C),
elevated heart rate (>90bpm), high respiratory rate (>20), and reduced WBC count in the blood. Taking into
consideration the fact that the patient X manifested tachycardia, tachypnea, and increased body temperature, it
can be suggested that the treatment administered was not effective in protecting the body against pathogen
attack, thereby leading to systematic inflammation, and subsequent dysfunction and failure of the organs.
SIRS and respiratory system
The respiratory system maintains homeostasis in two different ways namely, gaseous exchange and
blood pH regulation. The lungs participate in gas exchange through the elimination of carbon dioxide, a waste
product that is produced during cellular respiration. Removal of carbon dioxide from the body results in entry of
oxygen in the lungs that is required for cellular respiration (Guyenet and Bayliss 2015). Normal respiration rate
is associated with an estimated 12-25 breaths per minute. Tachypnea typically occurs under circumstances when
the respiratory rate is greater than 20 breaths/minute and is generally manifested in the form of shortness of
breath and retracting chest during breathing. On sensing the presence of an infection in the body, the innate
immune system releases chemicals in the bloodstream that results in an inflammation in the body and interferes
with the flow of blood to the vital organs, thus leading to tachypnea (Censoplano, Epting and Coates 2014).
Taking into consideration the fact that asthmatic conditions reported by the patient resulted in lung damage and
allowed more viruses and bacteria to invade the body, thus causing infection, the innate immune system, X
might have had eosinophilic inflammation in the lungs (Lambrecht and Hammad 2015). However, failure in
restoration of homeostasis resulted in a major systemic reaction where cytokine release promoted destruction of
cellular integrity and end-organ dysfunction.
Furthermore, history of asthma in the patient can be associated with the failure of the innate immune
system that was responsible for chronic inflammation of the airway conducting zone, thus leading to the
development of tachypnea. Furthermore, gradual decrease in the oxygen saturation levels in the patient can be
accredited to the fact that severe attack of asthma lead to hypoxia in the patient (Silverthorn 2013). The
condition is a typical hallmark of infected and inflamed tissue and the adaptation to inadequate tissue
oxygenation is regulated by hypoxia-inducible factors (HIFs) (Semenza 2014). In addition, a characteristic
attribute of the cells of the immune system is to penetrate and operate in cells and tissues that have low levels of
oxygen and nutrients. However, onset of SIRS resulted in failure of expression of hypoxia-inducible
transcription factors HIFs, thereby decreasing the oxygen saturation levels in the patients.
SIRS and cardiovascular system
The major mechanism of the cardiovascular system in homeostasis maintenance depends on the
controlled and continuous movement of bloodstream though the capillaries, permeating the cells and tissues of
the human body (Fox 2013). There is mounting evidence for the association between inflammation and atrial
fibrillation that occurs due to a maladaptive hyperimmune response, which in turn is triggered by pathogen
infection (Harada, Van Wagoner and Nattel 2015). The onset of tachycardia in the patient can be explained by
the fact that multiorgan dysfunction syndrome (MODS) and SIRS result in prognostically pertinent cardiac
autonomic dysfunction. This is generally manifested via strong attenuation of vagally and sympathetically
governed heart rate variability (HRV) (Balk 2014). In addition, the immune mechanisms that underlie the
process of attenuation are not just restricted to the nervous system, and encompass variations in the cells of the
cardiac pacemaker on a cellular level.
According to Ebelt et al. (2015) endotoxin typically interacts with hyperpolarization-activated cyclic
nucleotide-gated (HCN) ion channels that are located in the heart, which in turn mediate the pacemaker current.
This also transmits vagal signals on heart rate and HRV. Failure of the innate immune system also resulted in
abnormal firing of the cardiac electrical signals, thus speeding up the heart rate and causing tachycardia in the
patient. In addition, the decreased pumping efficiency of the left portion of the heart resulted in fluid build-up in
the lungs that was responsible for wheezing, breathlessness, and tachycardia (Widmaier et al. 2011).
Furthermore, the pathologic condition of circulatory shock also occurred due to a mismatch between the demand
and supply of oxygen, and led to inadequate tissue perfusion, thus bringing about multiple organ failure and
dysfunction (Cecconi et al. 2014). In addition, although hydrocortisone is used for treating the inflammation in
asthmatic conditions, the corticosteroid failed to treat the patient, thus deteriorating the patient condition (Rang
et al. 2014).
SIRS and renal system

According to Blaine, Chonchol and Levi (2015) kidneys maintain homeostasis by regulating the
concentration of ions and the amount of water in the blood. The kidneys have been found to largely contribute to
immune homeostasis. There is mounting evidence for the fact that several components of the immune system
play a major role in mediating acute types of renal disease, in addition to controlling the progression of chronic
kidney disease (Fearn and Sheerin 2015). A dysregulated immune system has been found responsible for the
onset of indirect or direct renal impacts. In addition, the loss of immune homeostasis in the kidneys lead to the
perpetual recruitment of immune cells and also brought about a worsening injury to the kidneys.
Owing to the fact that SIRS involves uncoordinated tissue repair attempts, the onset of immune-mediated injury
was primarily responsible for the fibrosis of renal structures that eventually resulted in kidney failure. Time and
again it has been proved that Acute Kidney Injury (AKI) is a recurrent complication of SIRS, which in turn is
correlated with a progressive decrease in sodium concentration (NaU) in the urine and fractional excretion
(FENa) (Garg et al. 2014). The aforementioned events resulted in inactivation of renin-angiotensin-aldosterone
system, thus reducing the urine output and increasing renal dysfunction. Renal function could be monitored by
measuring the glomerular filtration rate (normal=60) that is considered superior to the levels of serum
creatinine, which generally differs with race, age and gender.
Conclusion
To conclude, SIRS has been found to be triggered by inflammation, ischemia, trauma, infection or
several insults that are not generally related to infection. An analysis of the case scenario suggests that previous
history of asthma resulted in the onset and development of SIRS in the patient X, which has been found to use
inflammation as the mode of response of the human body to a plethora of nonspecific insults that developed
from chemical, and/or infectious stimuli. The immune system comprises of a complex inflammatory cascade
that involves cellular and humoral responses. Although the infection resulted in the local production of cytokine
into the circulating bloodstream for improving local response, failure of the immune system in restoring
homeostasis made the cytokine release cause destruction, rather than protection, which resulted in the activation
of several humoral cascades, endothelial system, and subsequent loss of circulatory integrity. The
aforementioned steps led to organ dysfunction and eventual death of the patient.
References
Balk, R.A., 2014. Systemic inflammatory response syndrome (SIRS) Where did it come from and is it still
relevant today?. Virulence, 5(1), pp.20-26.
Blaine, J., Chonchol, M. and Levi, M., 2015. Renal control of calcium, phosphate, and magnesium
homeostasis. Clinical Journal of the American Society of Nephrology, 10(7), pp.1257-1272.
Cecconi, M., De Backer, D., Antonelli, M., Beale, R., Bakker, J., Hofer, C., Jaeschke, R., Mebazaa, A., Pinsky,
M.R., Teboul, J.L. and Vincent, J.L., 2014. Consensus on circulatory shock and hemodynamic monitoring. Task
force of the European Society of Intensive Care Medicine. Intensive care medicine, 40(12), pp.1795-1815.
Censoplano, N., Epting, C.L. and Coates, B.M., 2014. The role of the innate immune system in sepsis. Clinical
Pediatric Emergency Medicine, 15(2), pp.169-176.
Ebelt, H., Geißler, I., Ruccius, S., Otto, V., Hoffmann, S., Korth, H., Klöckner, U., Zhang, Y., Li, Y.,
Grossmann, C. and Rueckschloss, U., 2015. Direct inhibition, but indirect sensitization of pacemaker activity to
sympathetic tone by the interaction of endotoxin with HCN‐channels. Clinical and Experimental Pharmacology
and Physiology, 42(8), pp.874-880.
Fearn, A. and Sheerin, N.S., 2015. Complement activation in progressive renal disease. World journal of
nephrology, 4(1), p.31.
Fox, S.I., 2013. Human Physiology. McGraw-Hill
Higher Education.
Garg, A.X., Vincent, J., Cuerden, M., Parikh, C., Devereaux, P.J., Teoh, K., Yusuf, S., Hildebrand, A., Lamy,
A., Zuo, Y. and Sessler, D.I., 2014. Steroids In caRdiac Surgery (SIRS) trial: acute kidney injury substudy
protocol of an international randomised controlled trial. BMJ open, 4(3), p.e004842.
Guyenet, P.G. and Bayliss, D.A., 2015. Neural control of breathing and CO2 homeostasis. Neuron, 87(5),
pp.946-961.
Harada, M., Van Wagoner, D.R. and Nattel, S., 2015. Role of inflammation in atrial fibrillation pathophysiology
and management. Circulation journal, pp.CJ-15.
Iwasaki, A. and Medzhitov, R., 2015. Control of adaptive immunity by the innate immune system. Nature
immunology, 16(4), p.343.
concentration of ions and the amount of water in the blood. The kidneys have been found to largely contribute to
immune homeostasis. There is mounting evidence for the fact that several components of the immune system
play a major role in mediating acute types of renal disease, in addition to controlling the progression of chronic
kidney disease (Fearn and Sheerin 2015). A dysregulated immune system has been found responsible for the
onset of indirect or direct renal impacts. In addition, the loss of immune homeostasis in the kidneys lead to the
perpetual recruitment of immune cells and also brought about a worsening injury to the kidneys.
Owing to the fact that SIRS involves uncoordinated tissue repair attempts, the onset of immune-mediated injury
was primarily responsible for the fibrosis of renal structures that eventually resulted in kidney failure. Time and
again it has been proved that Acute Kidney Injury (AKI) is a recurrent complication of SIRS, which in turn is
correlated with a progressive decrease in sodium concentration (NaU) in the urine and fractional excretion
(FENa) (Garg et al. 2014). The aforementioned events resulted in inactivation of renin-angiotensin-aldosterone
system, thus reducing the urine output and increasing renal dysfunction. Renal function could be monitored by
measuring the glomerular filtration rate (normal=60) that is considered superior to the levels of serum
creatinine, which generally differs with race, age and gender.
Conclusion
To conclude, SIRS has been found to be triggered by inflammation, ischemia, trauma, infection or
several insults that are not generally related to infection. An analysis of the case scenario suggests that previous
history of asthma resulted in the onset and development of SIRS in the patient X, which has been found to use
inflammation as the mode of response of the human body to a plethora of nonspecific insults that developed
from chemical, and/or infectious stimuli. The immune system comprises of a complex inflammatory cascade
that involves cellular and humoral responses. Although the infection resulted in the local production of cytokine
into the circulating bloodstream for improving local response, failure of the immune system in restoring
homeostasis made the cytokine release cause destruction, rather than protection, which resulted in the activation
of several humoral cascades, endothelial system, and subsequent loss of circulatory integrity. The
aforementioned steps led to organ dysfunction and eventual death of the patient.
References
Balk, R.A., 2014. Systemic inflammatory response syndrome (SIRS) Where did it come from and is it still
relevant today?. Virulence, 5(1), pp.20-26.
Blaine, J., Chonchol, M. and Levi, M., 2015. Renal control of calcium, phosphate, and magnesium
homeostasis. Clinical Journal of the American Society of Nephrology, 10(7), pp.1257-1272.
Cecconi, M., De Backer, D., Antonelli, M., Beale, R., Bakker, J., Hofer, C., Jaeschke, R., Mebazaa, A., Pinsky,
M.R., Teboul, J.L. and Vincent, J.L., 2014. Consensus on circulatory shock and hemodynamic monitoring. Task
force of the European Society of Intensive Care Medicine. Intensive care medicine, 40(12), pp.1795-1815.
Censoplano, N., Epting, C.L. and Coates, B.M., 2014. The role of the innate immune system in sepsis. Clinical
Pediatric Emergency Medicine, 15(2), pp.169-176.
Ebelt, H., Geißler, I., Ruccius, S., Otto, V., Hoffmann, S., Korth, H., Klöckner, U., Zhang, Y., Li, Y.,
Grossmann, C. and Rueckschloss, U., 2015. Direct inhibition, but indirect sensitization of pacemaker activity to
sympathetic tone by the interaction of endotoxin with HCN‐channels. Clinical and Experimental Pharmacology
and Physiology, 42(8), pp.874-880.
Fearn, A. and Sheerin, N.S., 2015. Complement activation in progressive renal disease. World journal of
nephrology, 4(1), p.31.
Fox, S.I., 2013. Human Physiology. McGraw-Hill
Higher Education.
Garg, A.X., Vincent, J., Cuerden, M., Parikh, C., Devereaux, P.J., Teoh, K., Yusuf, S., Hildebrand, A., Lamy,
A., Zuo, Y. and Sessler, D.I., 2014. Steroids In caRdiac Surgery (SIRS) trial: acute kidney injury substudy
protocol of an international randomised controlled trial. BMJ open, 4(3), p.e004842.
Guyenet, P.G. and Bayliss, D.A., 2015. Neural control of breathing and CO2 homeostasis. Neuron, 87(5),
pp.946-961.
Harada, M., Van Wagoner, D.R. and Nattel, S., 2015. Role of inflammation in atrial fibrillation pathophysiology
and management. Circulation journal, pp.CJ-15.
Iwasaki, A. and Medzhitov, R., 2015. Control of adaptive immunity by the innate immune system. Nature
immunology, 16(4), p.343.

Kaukonen, K.M., Bailey, M., Pilcher, D., Cooper, D.J. and Bellomo, R., 2015. Systemic inflammatory response
syndrome criteria in defining severe sepsis. New England Journal of Medicine, 372(17), pp.1629-1638.
Lackey, D.E. and Olefsky, J.M., 2016. Regulation of metabolism by the innate immune system. Nature Reviews
Endocrinology, 12(1), p.15.
Lambrecht, B.N. and Hammad, H., 2015. The immunology of asthma. Nature immunology, 16(1), p.45.
Martini, F.H., Nath, J.L., and Bartholomew, E.F., 2014. Fundamentals of Anatomy & Physiology. Pearson.
Rang, H.P., Ritter, J.M., Flower, R.J. and Henderson, G., 2014. Rang & Dale's pharmacology. Elsevier Health
Sciences.
Semenza, G.L., 2014. Oxygen sensing, hypoxia-inducible factors, and disease pathophysiology. Annual Review
of Pathology: Mechanisms of Disease, 9, pp.47-71.
Silverthorn, D.U., 2013. Human physiology: an integrated approach. Jones & Bartlett Publishers.
Widmaier, E.P., Raff, H., Strang, K.T. and Vander, A.J., 2011. Vander's human physiology: the mechanisms of
body function. Boston: McGraw-Hill Higher Education.
syndrome criteria in defining severe sepsis. New England Journal of Medicine, 372(17), pp.1629-1638.
Lackey, D.E. and Olefsky, J.M., 2016. Regulation of metabolism by the innate immune system. Nature Reviews
Endocrinology, 12(1), p.15.
Lambrecht, B.N. and Hammad, H., 2015. The immunology of asthma. Nature immunology, 16(1), p.45.
Martini, F.H., Nath, J.L., and Bartholomew, E.F., 2014. Fundamentals of Anatomy & Physiology. Pearson.
Rang, H.P., Ritter, J.M., Flower, R.J. and Henderson, G., 2014. Rang & Dale's pharmacology. Elsevier Health
Sciences.
Semenza, G.L., 2014. Oxygen sensing, hypoxia-inducible factors, and disease pathophysiology. Annual Review
of Pathology: Mechanisms of Disease, 9, pp.47-71.
Silverthorn, D.U., 2013. Human physiology: an integrated approach. Jones & Bartlett Publishers.
Widmaier, E.P., Raff, H., Strang, K.T. and Vander, A.J., 2011. Vander's human physiology: the mechanisms of
body function. Boston: McGraw-Hill Higher Education.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
DO NOT amend the following table, this will be used to provide feedback on your
assignment
Highlighted categories indicate your performance for each criterion – see GradeMark for your overall mark.
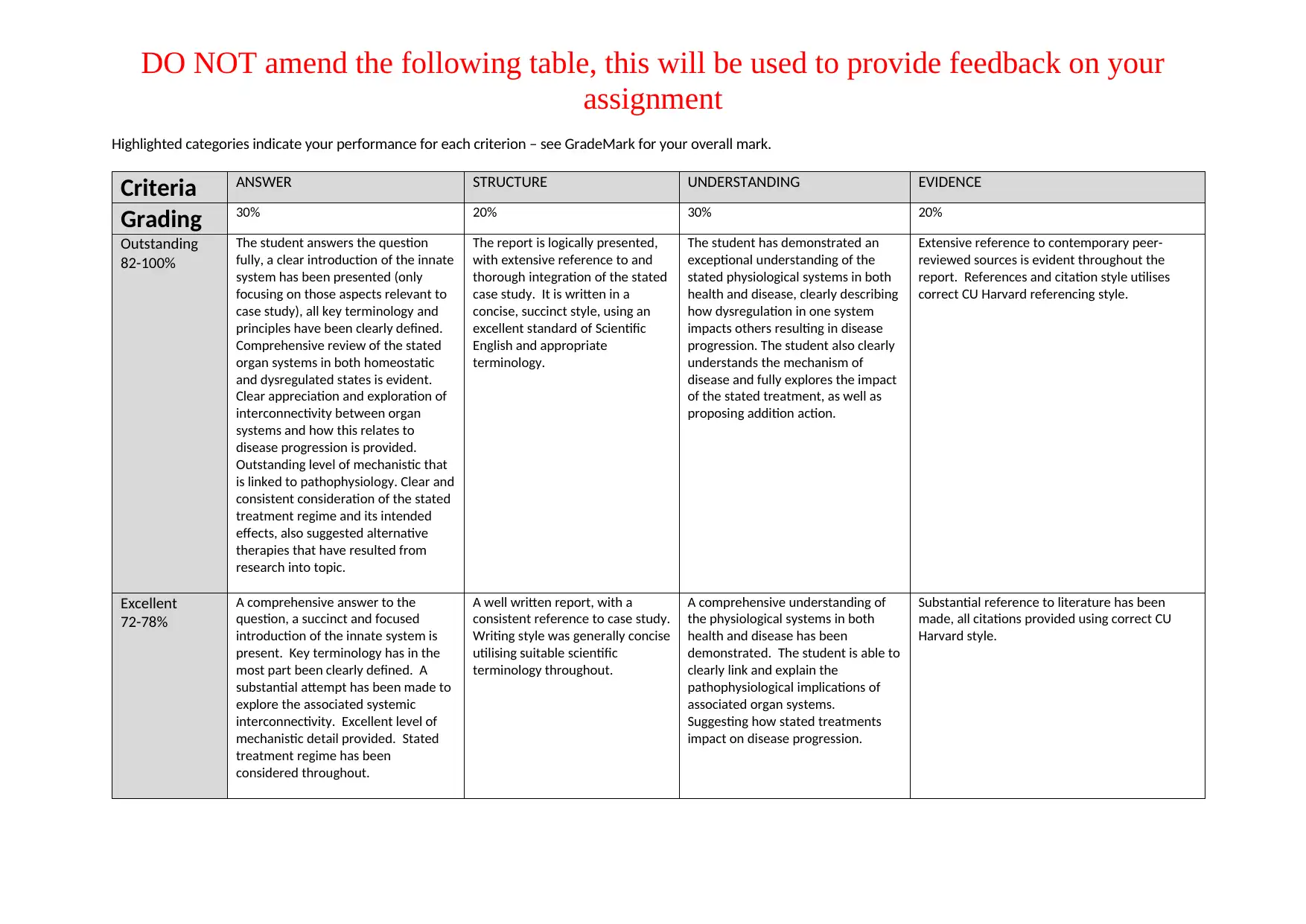
Criteria ANSWER STRUCTURE UNDERSTANDING EVIDENCE
Grading 30% 20% 30% 20%
Outstanding
82-100%
The student answers the question
fully, a clear introduction of the innate
system has been presented (only
focusing on those aspects relevant to
case study), all key terminology and
principles have been clearly defined.
Comprehensive review of the stated
organ systems in both homeostatic
and dysregulated states is evident.
Clear appreciation and exploration of
interconnectivity between organ
systems and how this relates to
disease progression is provided.
Outstanding level of mechanistic that
is linked to pathophysiology. Clear and
consistent consideration of the stated
treatment regime and its intended
effects, also suggested alternative
therapies that have resulted from
research into topic.
The report is logically presented,
with extensive reference to and
thorough integration of the stated
case study. It is written in a
concise, succinct style, using an
excellent standard of Scientific
English and appropriate
terminology.
The student has demonstrated an
exceptional understanding of the
stated physiological systems in both
health and disease, clearly describing
how dysregulation in one system
impacts others resulting in disease
progression. The student also clearly
understands the mechanism of
disease and fully explores the impact
of the stated treatment, as well as
proposing addition action.
Extensive reference to contemporary peer-
reviewed sources is evident throughout the
report. References and citation style utilises
correct CU Harvard referencing style.
Excellent
72-78%
A comprehensive answer to the
question, a succinct and focused
introduction of the innate system is
present. Key terminology has in the
most part been clearly defined. A
substantial attempt has been made to
explore the associated systemic
interconnectivity. Excellent level of
mechanistic detail provided. Stated
treatment regime has been
considered throughout.
A well written report, with a
consistent reference to case study.
Writing style was generally concise
utilising suitable scientific
terminology throughout.
A comprehensive understanding of
the physiological systems in both
health and disease has been
demonstrated. The student is able to
clearly link and explain the
pathophysiological implications of
associated organ systems.
Suggesting how stated treatments
impact on disease progression.
Substantial reference to literature has been
made, all citations provided using correct CU
Harvard style.
assignment
Highlighted categories indicate your performance for each criterion – see GradeMark for your overall mark.
Criteria ANSWER STRUCTURE UNDERSTANDING EVIDENCE
Grading 30% 20% 30% 20%
Outstanding
82-100%
The student answers the question
fully, a clear introduction of the innate
system has been presented (only
focusing on those aspects relevant to
case study), all key terminology and
principles have been clearly defined.
Comprehensive review of the stated
organ systems in both homeostatic
and dysregulated states is evident.
Clear appreciation and exploration of
interconnectivity between organ
systems and how this relates to
disease progression is provided.
Outstanding level of mechanistic that
is linked to pathophysiology. Clear and
consistent consideration of the stated
treatment regime and its intended
effects, also suggested alternative
therapies that have resulted from
research into topic.
The report is logically presented,
with extensive reference to and
thorough integration of the stated
case study. It is written in a
concise, succinct style, using an
excellent standard of Scientific
English and appropriate
terminology.
The student has demonstrated an
exceptional understanding of the
stated physiological systems in both
health and disease, clearly describing
how dysregulation in one system
impacts others resulting in disease
progression. The student also clearly
understands the mechanism of
disease and fully explores the impact
of the stated treatment, as well as
proposing addition action.
Extensive reference to contemporary peer-
reviewed sources is evident throughout the
report. References and citation style utilises
correct CU Harvard referencing style.
Excellent
72-78%
A comprehensive answer to the
question, a succinct and focused
introduction of the innate system is
present. Key terminology has in the
most part been clearly defined. A
substantial attempt has been made to
explore the associated systemic
interconnectivity. Excellent level of
mechanistic detail provided. Stated
treatment regime has been
considered throughout.
A well written report, with a
consistent reference to case study.
Writing style was generally concise
utilising suitable scientific
terminology throughout.
A comprehensive understanding of
the physiological systems in both
health and disease has been
demonstrated. The student is able to
clearly link and explain the
pathophysiological implications of
associated organ systems.
Suggesting how stated treatments
impact on disease progression.
Substantial reference to literature has been
made, all citations provided using correct CU
Harvard style.
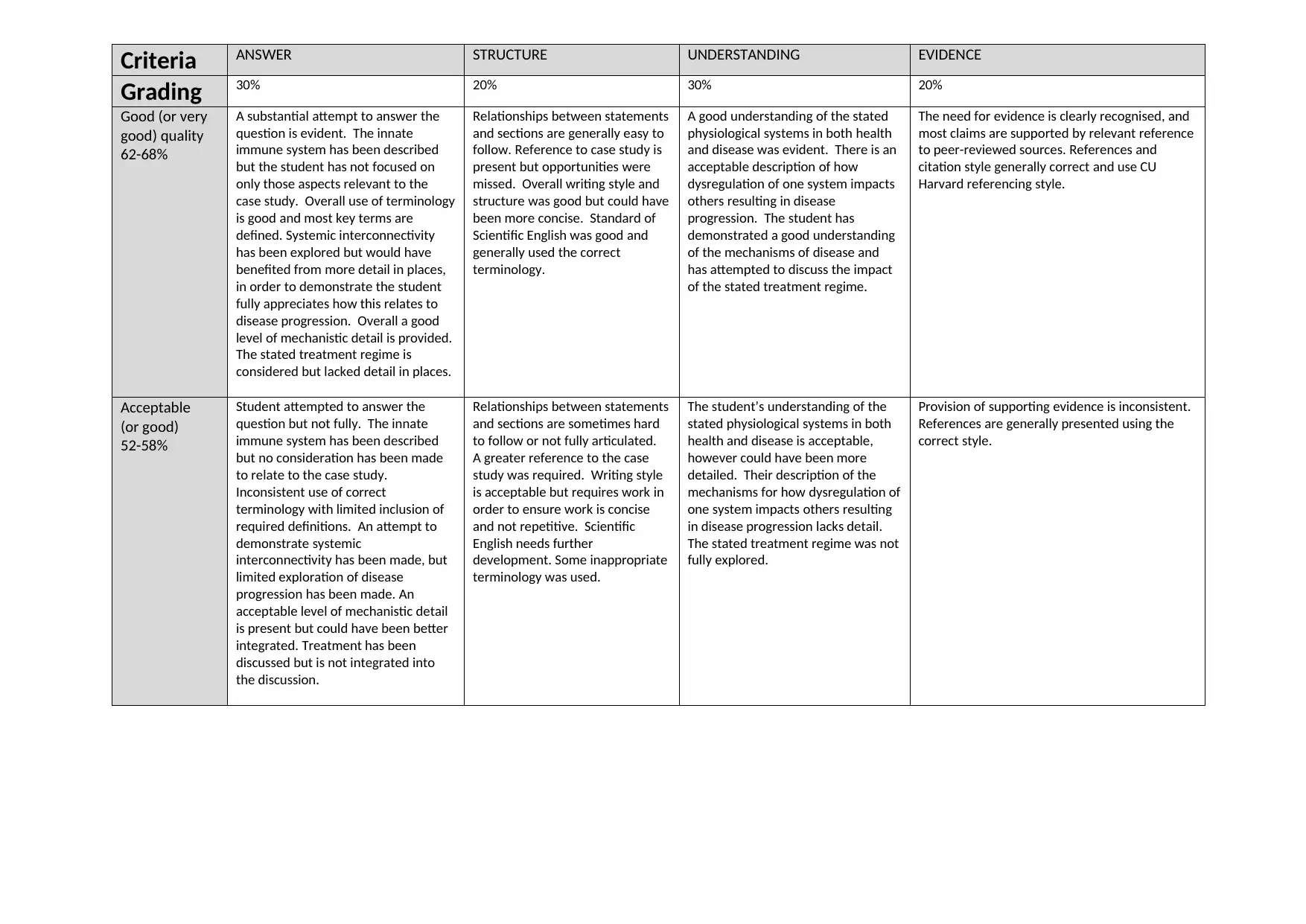
Criteria ANSWER STRUCTURE UNDERSTANDING EVIDENCE
Grading 30% 20% 30% 20%
Good (or very
good) quality
62-68%
A substantial attempt to answer the
question is evident. The innate
immune system has been described
but the student has not focused on
only those aspects relevant to the
case study. Overall use of terminology
is good and most key terms are
defined. Systemic interconnectivity
has been explored but would have
benefited from more detail in places,
in order to demonstrate the student
fully appreciates how this relates to
disease progression. Overall a good
level of mechanistic detail is provided.
The stated treatment regime is
considered but lacked detail in places.
Relationships between statements
and sections are generally easy to
follow. Reference to case study is
present but opportunities were
missed. Overall writing style and
structure was good but could have
been more concise. Standard of
Scientific English was good and
generally used the correct
terminology.
A good understanding of the stated
physiological systems in both health
and disease was evident. There is an
acceptable description of how
dysregulation of one system impacts
others resulting in disease
progression. The student has
demonstrated a good understanding
of the mechanisms of disease and
has attempted to discuss the impact
of the stated treatment regime.
The need for evidence is clearly recognised, and
most claims are supported by relevant reference
to peer-reviewed sources. References and
citation style generally correct and use CU
Harvard referencing style.
Acceptable
(or good)
52-58%
Student attempted to answer the
question but not fully. The innate
immune system has been described
but no consideration has been made
to relate to the case study.
Inconsistent use of correct
terminology with limited inclusion of
required definitions. An attempt to
demonstrate systemic
interconnectivity has been made, but
limited exploration of disease
progression has been made. An
acceptable level of mechanistic detail
is present but could have been better
integrated. Treatment has been
discussed but is not integrated into
the discussion.
Relationships between statements
and sections are sometimes hard
to follow or not fully articulated.
A greater reference to the case
study was required. Writing style
is acceptable but requires work in
order to ensure work is concise
and not repetitive. Scientific
English needs further
development. Some inappropriate
terminology was used.
The student’s understanding of the
stated physiological systems in both
health and disease is acceptable,
however could have been more
detailed. Their description of the
mechanisms for how dysregulation of
one system impacts others resulting
in disease progression lacks detail.
The stated treatment regime was not
fully explored.
Provision of supporting evidence is inconsistent.
References are generally presented using the
correct style.
Grading 30% 20% 30% 20%
Good (or very
good) quality
62-68%
A substantial attempt to answer the
question is evident. The innate
immune system has been described
but the student has not focused on
only those aspects relevant to the
case study. Overall use of terminology
is good and most key terms are
defined. Systemic interconnectivity
has been explored but would have
benefited from more detail in places,
in order to demonstrate the student
fully appreciates how this relates to
disease progression. Overall a good
level of mechanistic detail is provided.
The stated treatment regime is
considered but lacked detail in places.
Relationships between statements
and sections are generally easy to
follow. Reference to case study is
present but opportunities were
missed. Overall writing style and
structure was good but could have
been more concise. Standard of
Scientific English was good and
generally used the correct
terminology.
A good understanding of the stated
physiological systems in both health
and disease was evident. There is an
acceptable description of how
dysregulation of one system impacts
others resulting in disease
progression. The student has
demonstrated a good understanding
of the mechanisms of disease and
has attempted to discuss the impact
of the stated treatment regime.
The need for evidence is clearly recognised, and
most claims are supported by relevant reference
to peer-reviewed sources. References and
citation style generally correct and use CU
Harvard referencing style.
Acceptable
(or good)
52-58%
Student attempted to answer the
question but not fully. The innate
immune system has been described
but no consideration has been made
to relate to the case study.
Inconsistent use of correct
terminology with limited inclusion of
required definitions. An attempt to
demonstrate systemic
interconnectivity has been made, but
limited exploration of disease
progression has been made. An
acceptable level of mechanistic detail
is present but could have been better
integrated. Treatment has been
discussed but is not integrated into
the discussion.
Relationships between statements
and sections are sometimes hard
to follow or not fully articulated.
A greater reference to the case
study was required. Writing style
is acceptable but requires work in
order to ensure work is concise
and not repetitive. Scientific
English needs further
development. Some inappropriate
terminology was used.
The student’s understanding of the
stated physiological systems in both
health and disease is acceptable,
however could have been more
detailed. Their description of the
mechanisms for how dysregulation of
one system impacts others resulting
in disease progression lacks detail.
The stated treatment regime was not
fully explored.
Provision of supporting evidence is inconsistent.
References are generally presented using the
correct style.
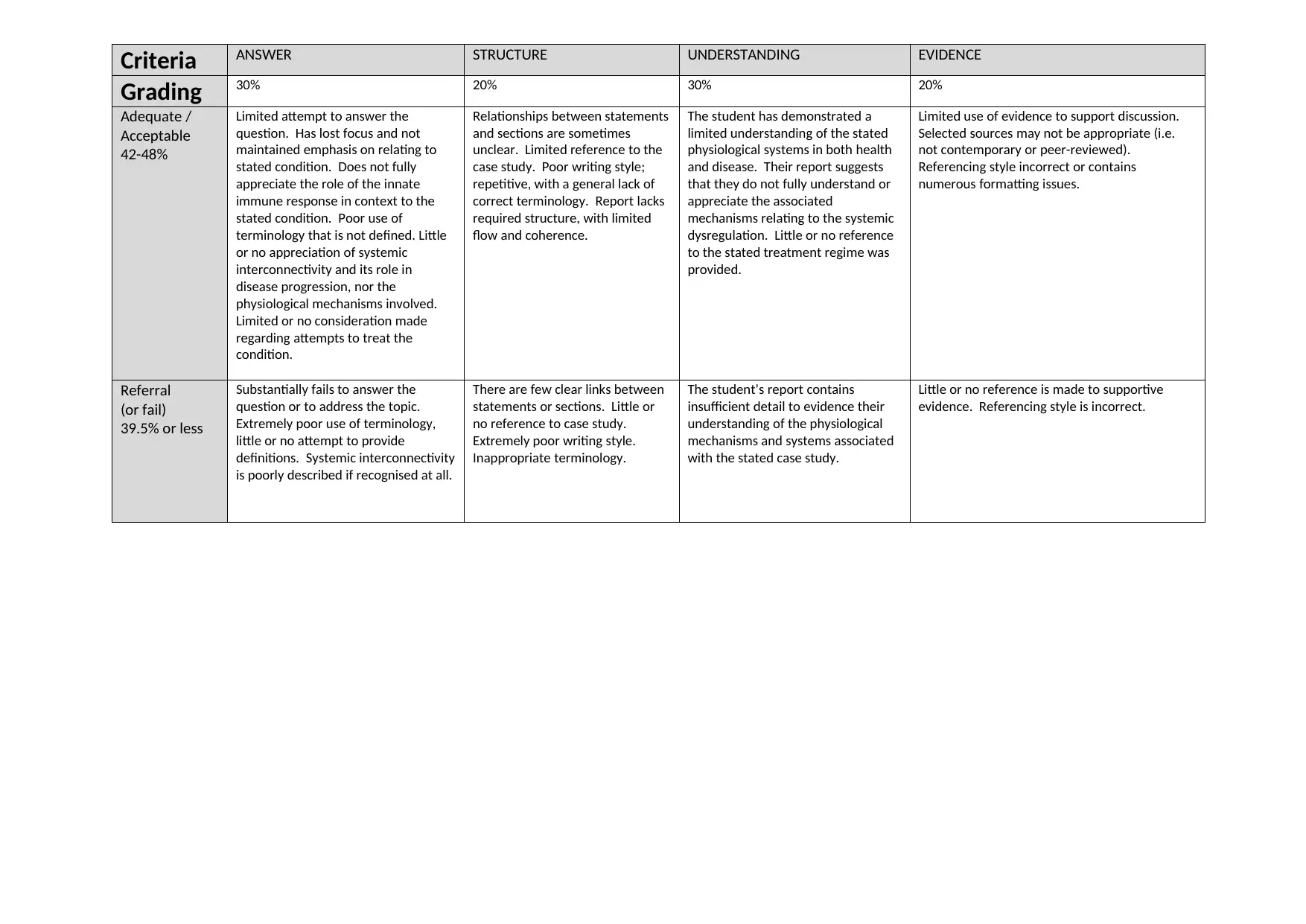
Criteria ANSWER STRUCTURE UNDERSTANDING EVIDENCE
Grading 30% 20% 30% 20%
Adequate /
Acceptable
42-48%
Limited attempt to answer the
question. Has lost focus and not
maintained emphasis on relating to
stated condition. Does not fully
appreciate the role of the innate
immune response in context to the
stated condition. Poor use of
terminology that is not defined. Little
or no appreciation of systemic
interconnectivity and its role in
disease progression, nor the
physiological mechanisms involved.
Limited or no consideration made
regarding attempts to treat the
condition.
Relationships between statements
and sections are sometimes
unclear. Limited reference to the
case study. Poor writing style;
repetitive, with a general lack of
correct terminology. Report lacks
required structure, with limited
flow and coherence.
The student has demonstrated a
limited understanding of the stated
physiological systems in both health
and disease. Their report suggests
that they do not fully understand or
appreciate the associated
mechanisms relating to the systemic
dysregulation. Little or no reference
to the stated treatment regime was
provided.
Limited use of evidence to support discussion.
Selected sources may not be appropriate (i.e.
not contemporary or peer-reviewed).
Referencing style incorrect or contains
numerous formatting issues.
Referral
(or fail)
39.5% or less
Substantially fails to answer the
question or to address the topic.
Extremely poor use of terminology,
little or no attempt to provide
definitions. Systemic interconnectivity
is poorly described if recognised at all.
There are few clear links between
statements or sections. Little or
no reference to case study.
Extremely poor writing style.
Inappropriate terminology.
The student’s report contains
insufficient detail to evidence their
understanding of the physiological
mechanisms and systems associated
with the stated case study.
Little or no reference is made to supportive
evidence. Referencing style is incorrect.
Grading 30% 20% 30% 20%
Adequate /
Acceptable
42-48%
Limited attempt to answer the
question. Has lost focus and not
maintained emphasis on relating to
stated condition. Does not fully
appreciate the role of the innate
immune response in context to the
stated condition. Poor use of
terminology that is not defined. Little
or no appreciation of systemic
interconnectivity and its role in
disease progression, nor the
physiological mechanisms involved.
Limited or no consideration made
regarding attempts to treat the
condition.
Relationships between statements
and sections are sometimes
unclear. Limited reference to the
case study. Poor writing style;
repetitive, with a general lack of
correct terminology. Report lacks
required structure, with limited
flow and coherence.
The student has demonstrated a
limited understanding of the stated
physiological systems in both health
and disease. Their report suggests
that they do not fully understand or
appreciate the associated
mechanisms relating to the systemic
dysregulation. Little or no reference
to the stated treatment regime was
provided.
Limited use of evidence to support discussion.
Selected sources may not be appropriate (i.e.
not contemporary or peer-reviewed).
Referencing style incorrect or contains
numerous formatting issues.
Referral
(or fail)
39.5% or less
Substantially fails to answer the
question or to address the topic.
Extremely poor use of terminology,
little or no attempt to provide
definitions. Systemic interconnectivity
is poorly described if recognised at all.
There are few clear links between
statements or sections. Little or
no reference to case study.
Extremely poor writing style.
Inappropriate terminology.
The student’s report contains
insufficient detail to evidence their
understanding of the physiological
mechanisms and systems associated
with the stated case study.
Little or no reference is made to supportive
evidence. Referencing style is incorrect.
1 out of 7
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





