Female Stress and Urinary Incontinence (UI)
VerifiedAdded on 2023/06/15
|15
|3315
|298
AI Summary
This essay discusses the prevalence, financial impact, pathophysiology, risks, complications, and treatment of stress urinary incontinence (UI) in females. It also highlights the role of community nurses in assisting patients with stress UI. The essay recommends conservative and surgical treatments, and provides information on recommended diet and fluids. The Brimbank City Council's in-home support services for stress UI patients are also discussed.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: URINARY INCONTINENCE (UI)
Female Stress and Urinary Incontinence (UI)
Name of the Student
Name of the University
Author Note
Female Stress and Urinary Incontinence (UI)
Name of the Student
Name of the University
Author Note
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1
URINARY INCONTINENCE (UI)
Introduction
Stress urinary incontinence (UI) is one of the most common forms of urinary
incontinence (UI) (DeLancey, 2010). Millions of people worldwide are affected with stress UI
while the vast majority being women, mostly pregnant women (Sangsawang & Sangsawang,
2013). Men also develop UI is mostly due to an after effect of prostatic surgery (Markland,
Goode, Redden, Borrud, & Burgio, 2010). Quality of life and well-being is affected at large
among the persons who are suffering from stress UI. Affected individuals face complications
while travelling, performing physical activities, expressing emotions like laugh, cry and
maintaining healthy social relationships (Sangsawang & Sangsawang, 2013).
The following essay aims to highlight the pathophysiology, risks and complications
associated with stress UI. The essay also throws light on the prevalence of stress UI and its
financial impact on Australian population. Towards the end, the essay recommends the
treatment and therapy plan of stress UI along with the role of the community nurse towards
the assistance of patients suffering from stress UI.
Definition of stress UI
Urinary incontinence (UI) is a form of storage symptom. It is defined as a
physiological condition where a patient complains about the involuntary loss of urine
causing social or hygienic problems (Price, Dawood, & Jackson, 2010). Stress UI is a form of
UI and is define as a complaint of involuntary leakage of urine from the bladder due to
sudden pressure on the bladder arising out of sneezing or coughing or laughing.
URINARY INCONTINENCE (UI)
Introduction
Stress urinary incontinence (UI) is one of the most common forms of urinary
incontinence (UI) (DeLancey, 2010). Millions of people worldwide are affected with stress UI
while the vast majority being women, mostly pregnant women (Sangsawang & Sangsawang,
2013). Men also develop UI is mostly due to an after effect of prostatic surgery (Markland,
Goode, Redden, Borrud, & Burgio, 2010). Quality of life and well-being is affected at large
among the persons who are suffering from stress UI. Affected individuals face complications
while travelling, performing physical activities, expressing emotions like laugh, cry and
maintaining healthy social relationships (Sangsawang & Sangsawang, 2013).
The following essay aims to highlight the pathophysiology, risks and complications
associated with stress UI. The essay also throws light on the prevalence of stress UI and its
financial impact on Australian population. Towards the end, the essay recommends the
treatment and therapy plan of stress UI along with the role of the community nurse towards
the assistance of patients suffering from stress UI.
Definition of stress UI
Urinary incontinence (UI) is a form of storage symptom. It is defined as a
physiological condition where a patient complains about the involuntary loss of urine
causing social or hygienic problems (Price, Dawood, & Jackson, 2010). Stress UI is a form of
UI and is define as a complaint of involuntary leakage of urine from the bladder due to
sudden pressure on the bladder arising out of sneezing or coughing or laughing.
2
URINARY INCONTINENCE (UI)
Prevalence of stress UI in Australia
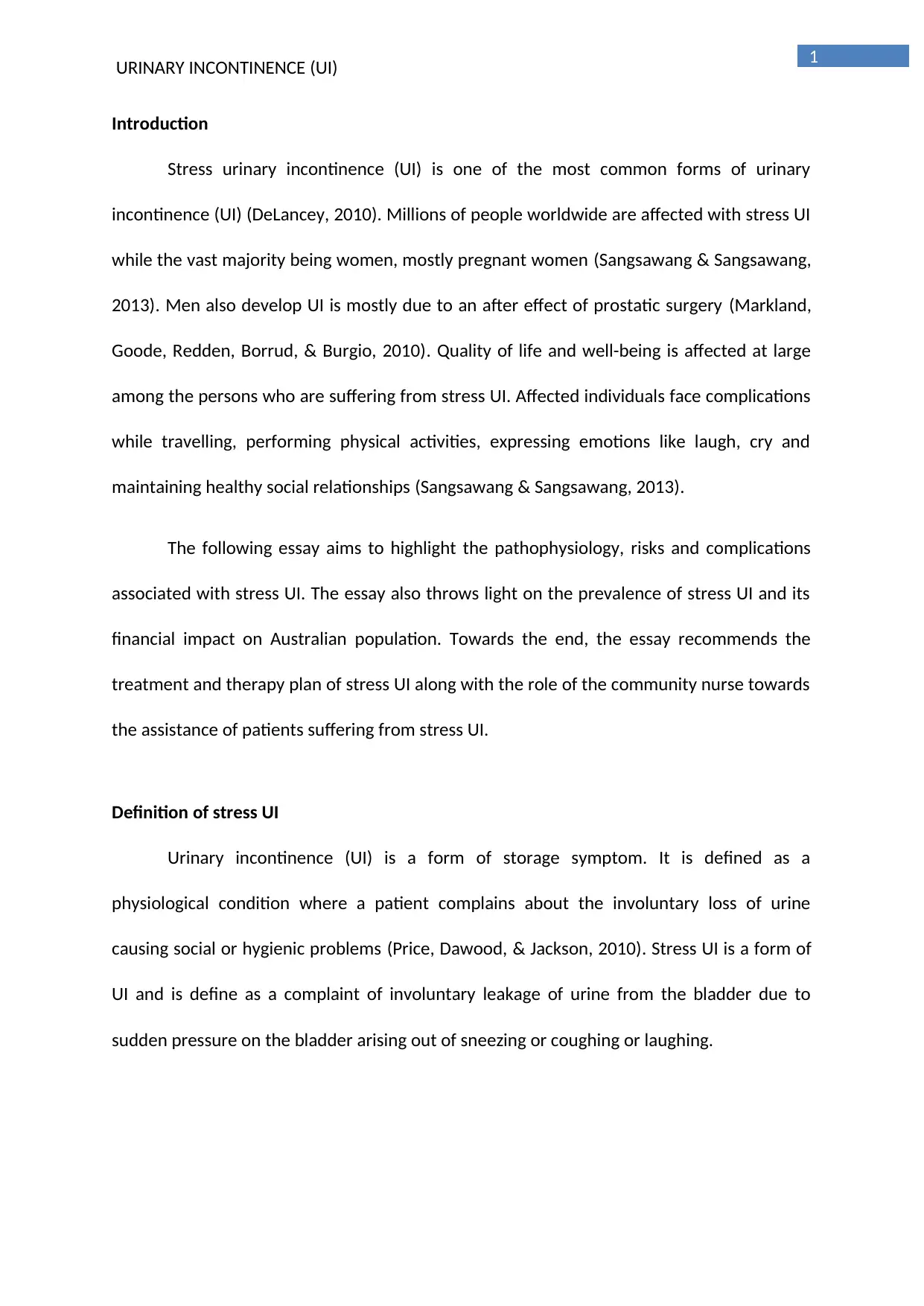
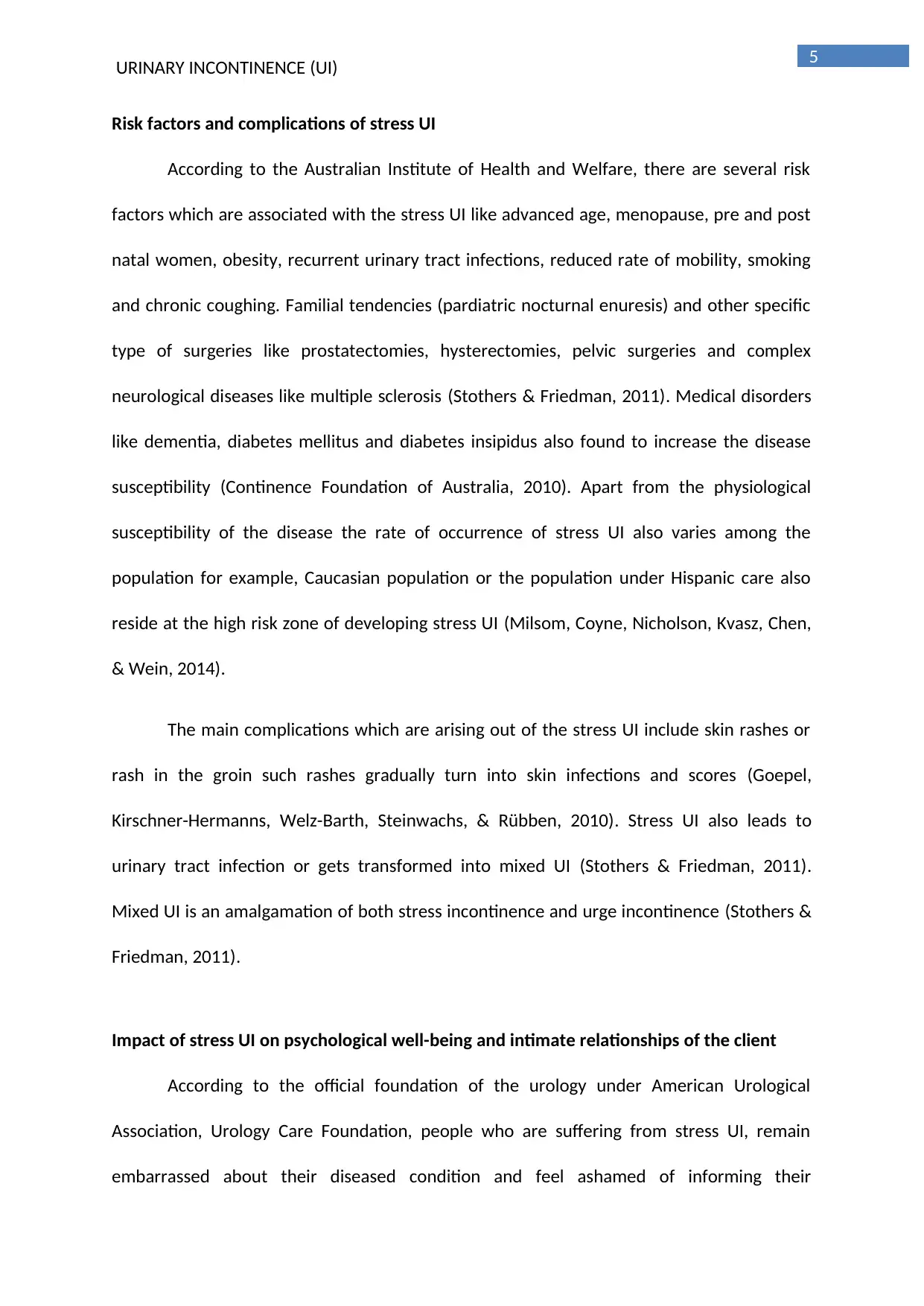
According to Continence Foundation of Australia, in 2010, 4.2 million Australians,
who are aged between 15 years and above are the main victims of the UI. The rate of
prevalence of stress UI is however higher among the Residential Aged Care (RAC) population
where at least 129,000 people or more than 70% of the population are suffering from UI.
Continence Foundation of Australia are of the opinion that, this projected numbers is
accepted to increase to 5.3 million by the end of 2030. This number is alarming because
apart from having negative impact on the social and sexual relationships of the sufferers,
stress UI also cast significant financial impact (Sangsawang & Sangsawang, 2013).
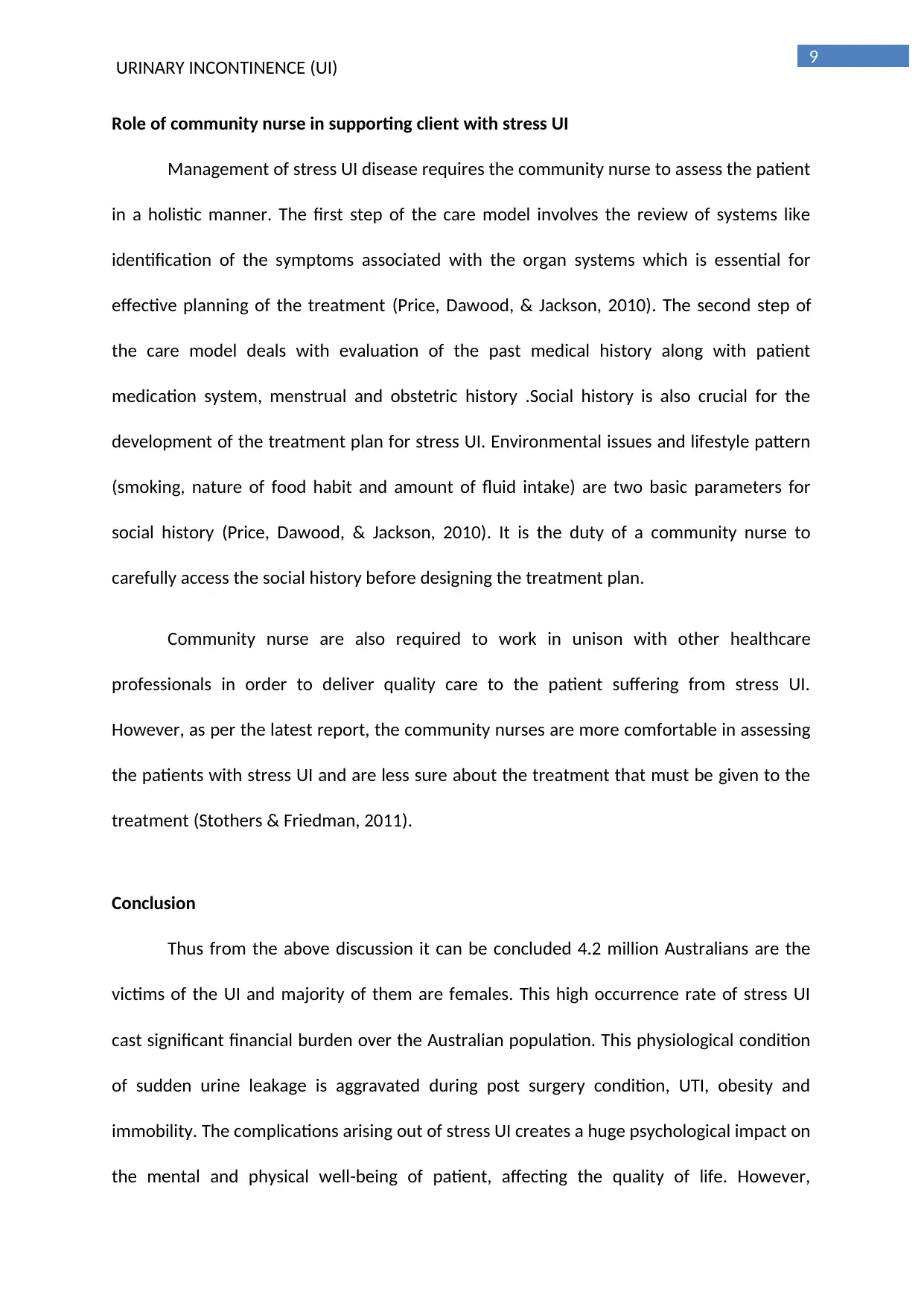
Figure: Projected Prevalence of Incontinence in Australian aged 15 years and over from
2010 to 2030
Financial impact of stress UI in Australia
The statistics published by Continence Foundation of Australia, the estimated
financial cost of UI was $42.9 billion (excluding the disease burden) and this cost amounts to
$9,014 per person in the year 2010. According to Continence Foundation of Australia, the
total system expenditure among the population of Australia arising out of incontinence is
URINARY INCONTINENCE (UI)
Prevalence of stress UI in Australia
According to Continence Foundation of Australia, in 2010, 4.2 million Australians,
who are aged between 15 years and above are the main victims of the UI. The rate of
prevalence of stress UI is however higher among the Residential Aged Care (RAC) population
where at least 129,000 people or more than 70% of the population are suffering from UI.
Continence Foundation of Australia are of the opinion that, this projected numbers is
accepted to increase to 5.3 million by the end of 2030. This number is alarming because
apart from having negative impact on the social and sexual relationships of the sufferers,
stress UI also cast significant financial impact (Sangsawang & Sangsawang, 2013).
Figure: Projected Prevalence of Incontinence in Australian aged 15 years and over from
2010 to 2030
Financial impact of stress UI in Australia
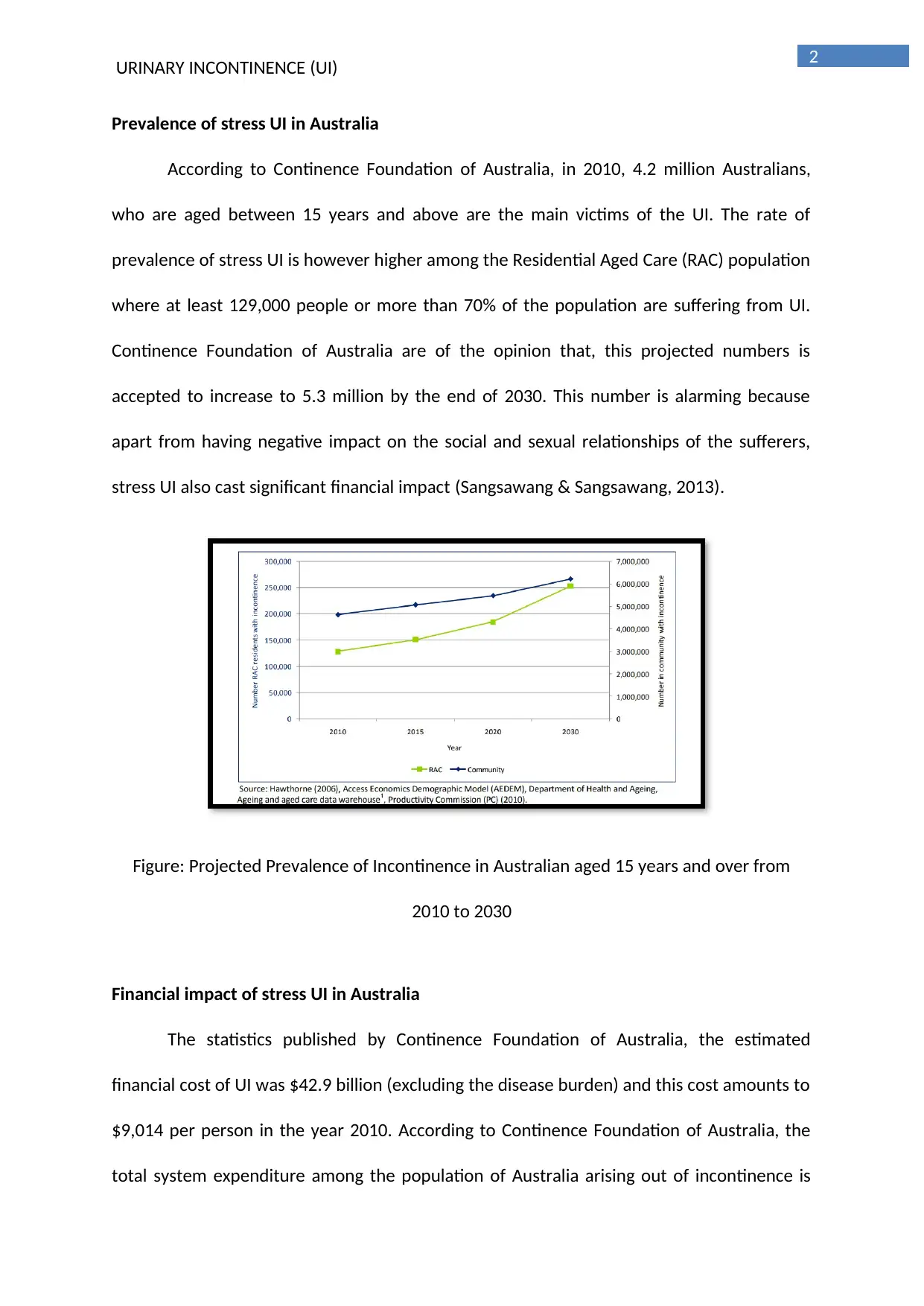
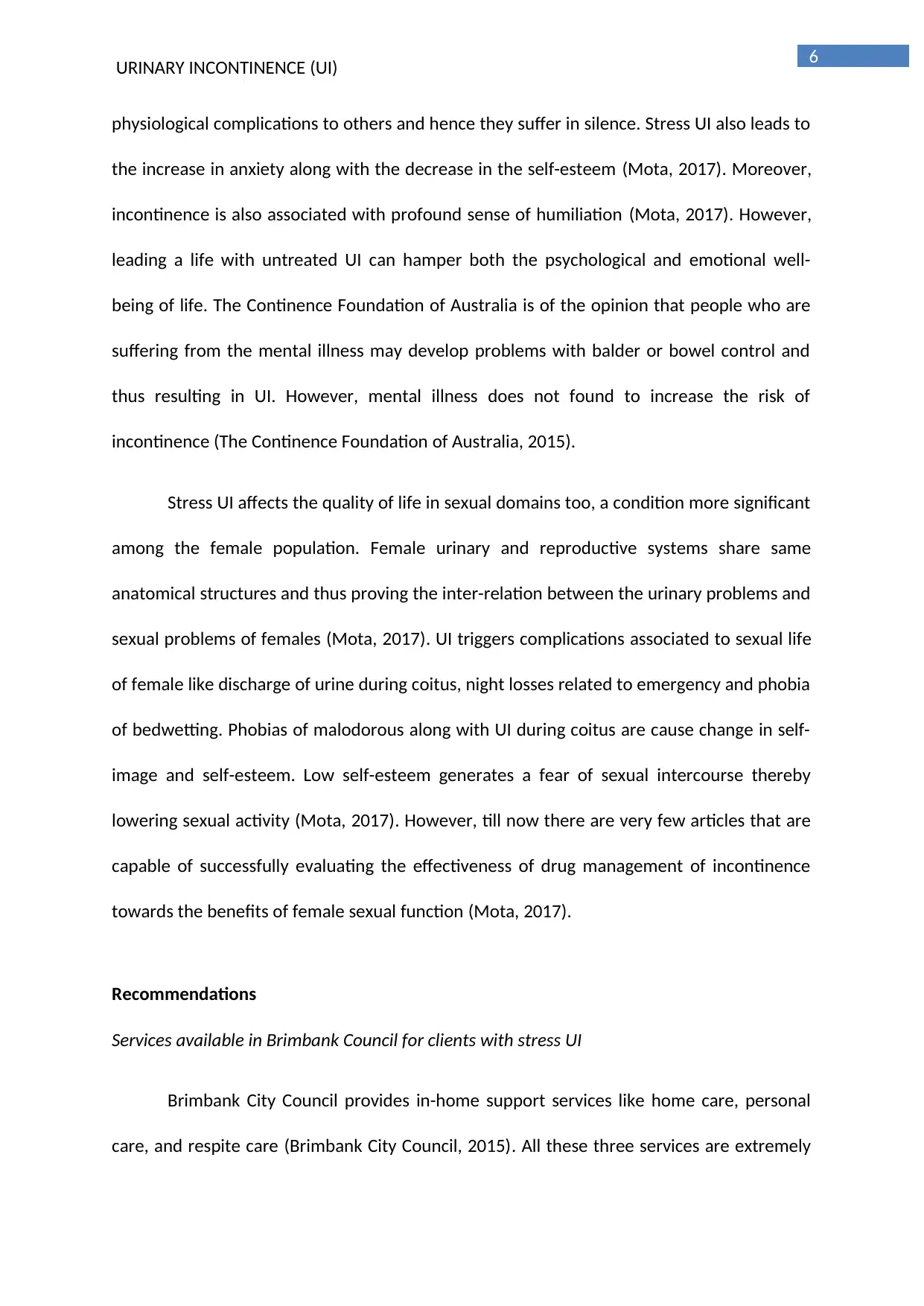
The statistics published by Continence Foundation of Australia, the estimated
financial cost of UI was $42.9 billion (excluding the disease burden) and this cost amounts to
$9,014 per person in the year 2010. According to Continence Foundation of Australia, the
total system expenditure among the population of Australia arising out of incontinence is
3
URINARY INCONTINENCE (UI)
$271 million and this amounts to per person cost of $57. This financial burden is accepted to
rise to $450 million by the end of the year 2020. According to Continence Foundation of
Australia, UI also cause loss of productivity among the working population and this cost
amount to about $34.1 billion in the year 2020. Apart from the loss of productivity, there
also occurs significant financial burden arising out of the cost of formal care and other
primary medical aids (The Economic Impact of Incontinence in Australia, 2010).
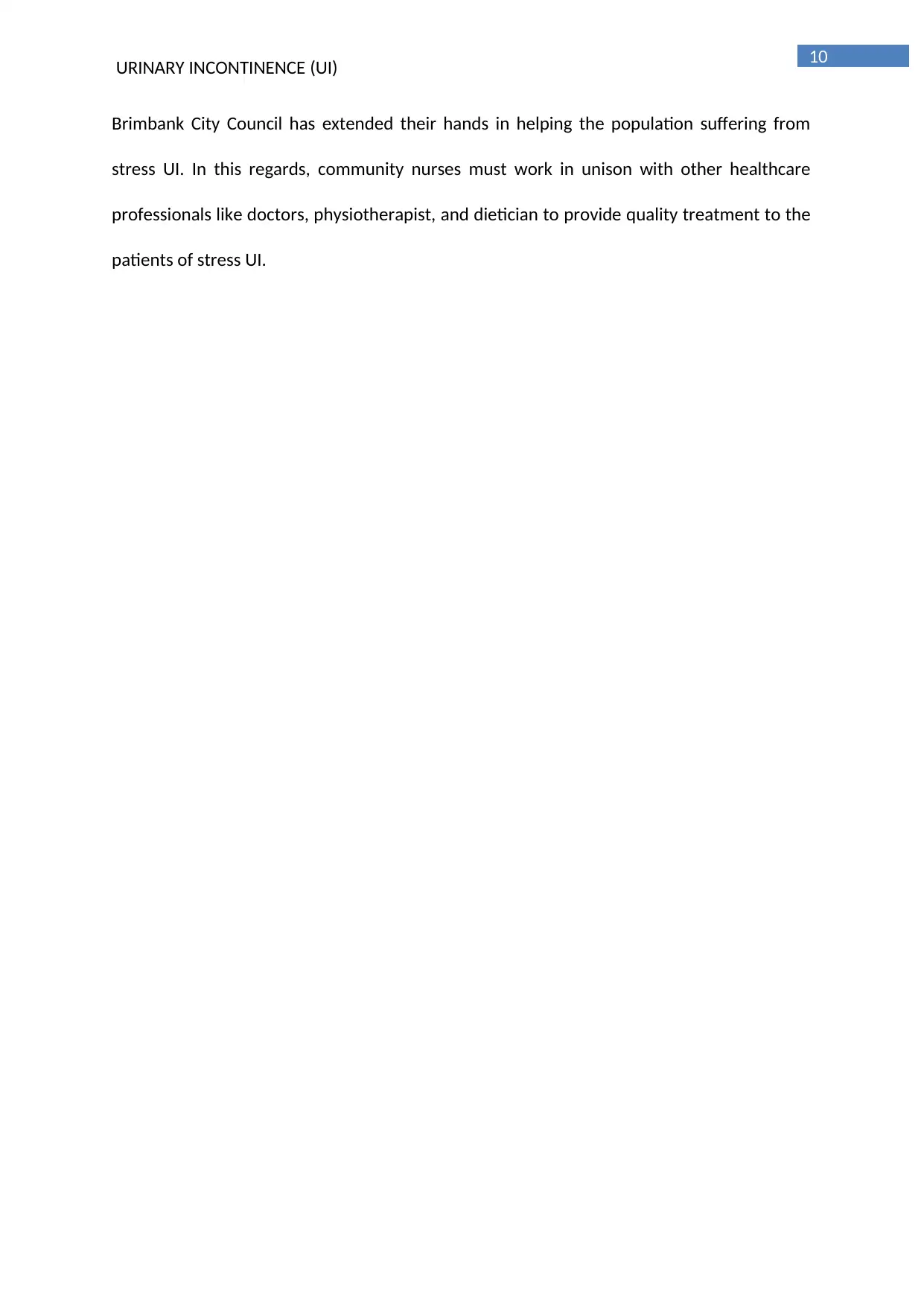
Figure: Cost of Incontinence in Australia, 2010
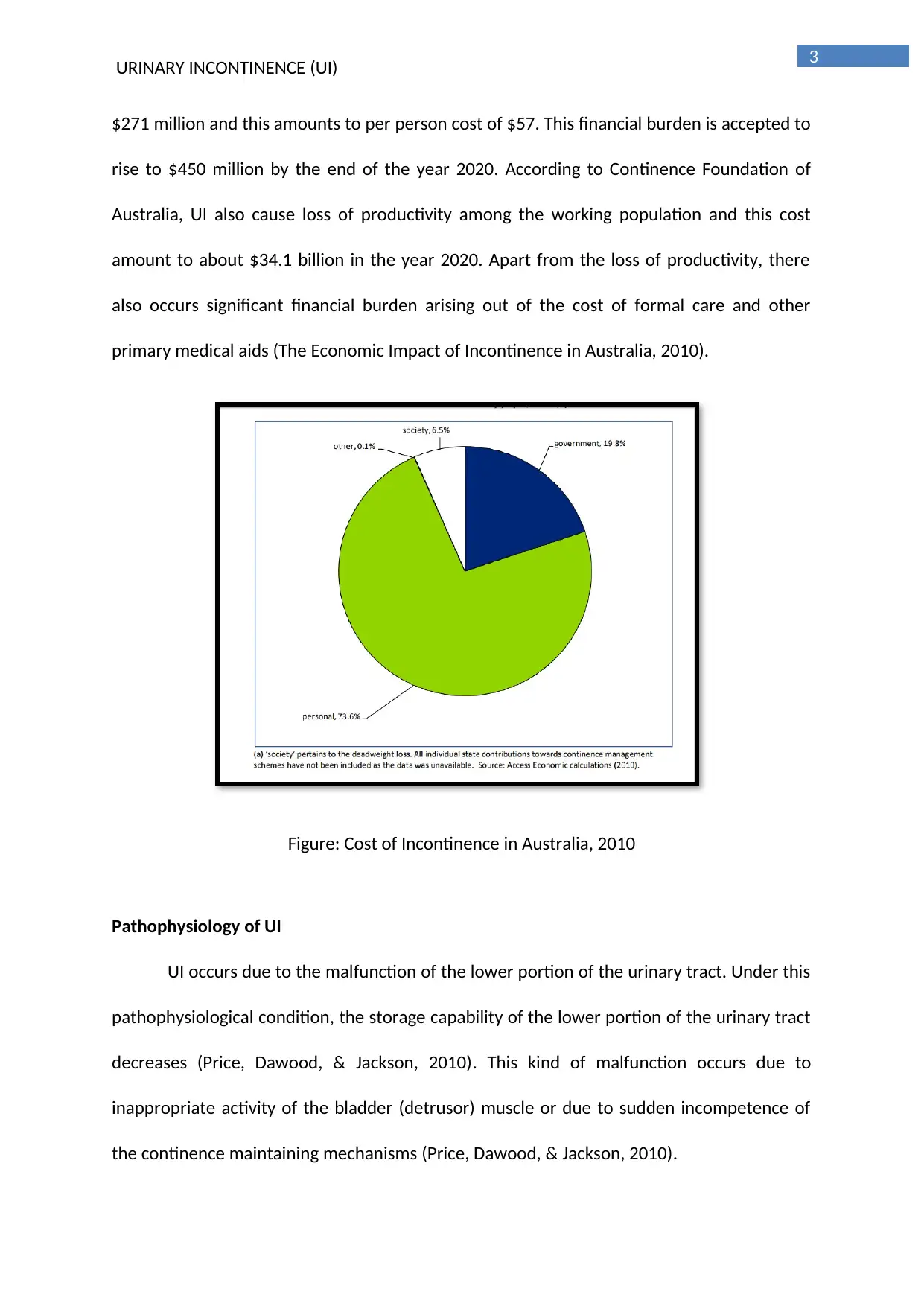
Pathophysiology of UI
UI occurs due to the malfunction of the lower portion of the urinary tract. Under this
pathophysiological condition, the storage capability of the lower portion of the urinary tract
decreases (Price, Dawood, & Jackson, 2010). This kind of malfunction occurs due to
inappropriate activity of the bladder (detrusor) muscle or due to sudden incompetence of
the continence maintaining mechanisms (Price, Dawood, & Jackson, 2010).
URINARY INCONTINENCE (UI)
$271 million and this amounts to per person cost of $57. This financial burden is accepted to
rise to $450 million by the end of the year 2020. According to Continence Foundation of
Australia, UI also cause loss of productivity among the working population and this cost
amount to about $34.1 billion in the year 2020. Apart from the loss of productivity, there
also occurs significant financial burden arising out of the cost of formal care and other
primary medical aids (The Economic Impact of Incontinence in Australia, 2010).
Figure: Cost of Incontinence in Australia, 2010
Pathophysiology of UI
UI occurs due to the malfunction of the lower portion of the urinary tract. Under this
pathophysiological condition, the storage capability of the lower portion of the urinary tract
decreases (Price, Dawood, & Jackson, 2010). This kind of malfunction occurs due to
inappropriate activity of the bladder (detrusor) muscle or due to sudden incompetence of
the continence maintaining mechanisms (Price, Dawood, & Jackson, 2010).
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4
URINARY INCONTINENCE (UI)
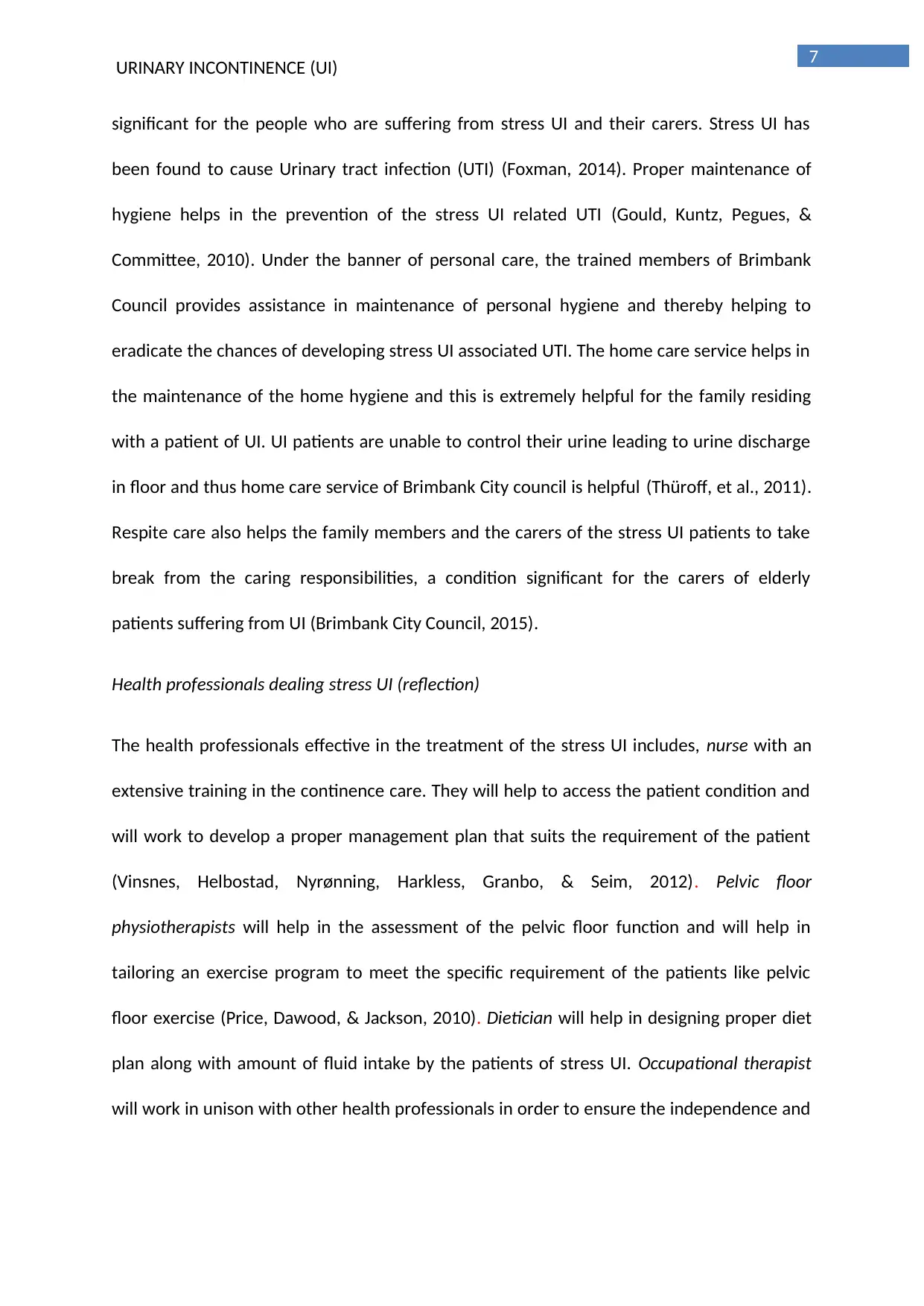
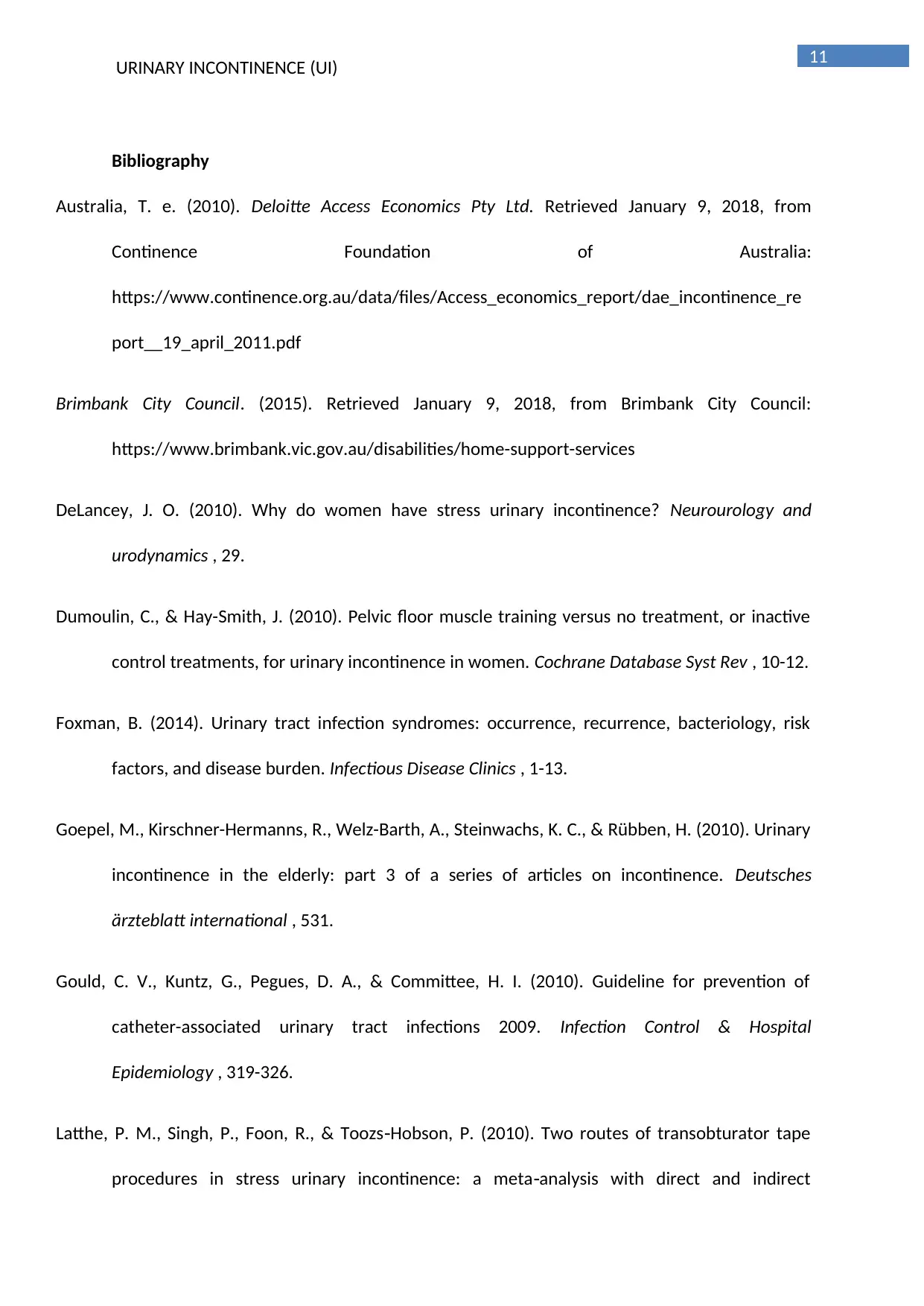
Figure: The Continence Mechanism
Source: (DeLancey, 2010)
Both during the resting condition and during the increase in the abdominal pressure,
urethral closure pressure must be greater than the pressure of the bladder and this
condition helps in urine retention in the bladder (Dumoulin & Hay-Smith, 2010). When
urethral pressure increases above the bladder pressure, the urethral muscles resting tone
helps in the maintenance of favourable pressure that is relative to the bladder (Dumoulin &
Hay-Smith, 2010). During the occurrence of the involuntary activities like coughing or
sneezing, bladder pressure significantly increases than that of the urethral pressure (Latthe,
Singh, Foon, & Toozs Hobson, 2010)‐ . Under this condition, a dynamic process lead to the
increase in the urethral closure pressure and this enhances the urethral closure while
maintaining continence (Latthe, Singh, Foon, & Toozs Hobson, 2010)‐ . Both the magnitude of
the increase in the pressure generated during cough and magnitude of the resting pressure
of the urethra helps in the determination of the actual point or the pressure limit at which
the leakage of the urine occurs (Dumoulin & Hay-Smith, 2010).
URINARY INCONTINENCE (UI)
Figure: The Continence Mechanism
Source: (DeLancey, 2010)
Both during the resting condition and during the increase in the abdominal pressure,
urethral closure pressure must be greater than the pressure of the bladder and this
condition helps in urine retention in the bladder (Dumoulin & Hay-Smith, 2010). When
urethral pressure increases above the bladder pressure, the urethral muscles resting tone
helps in the maintenance of favourable pressure that is relative to the bladder (Dumoulin &
Hay-Smith, 2010). During the occurrence of the involuntary activities like coughing or
sneezing, bladder pressure significantly increases than that of the urethral pressure (Latthe,
Singh, Foon, & Toozs Hobson, 2010)‐ . Under this condition, a dynamic process lead to the
increase in the urethral closure pressure and this enhances the urethral closure while
maintaining continence (Latthe, Singh, Foon, & Toozs Hobson, 2010)‐ . Both the magnitude of
the increase in the pressure generated during cough and magnitude of the resting pressure
of the urethra helps in the determination of the actual point or the pressure limit at which
the leakage of the urine occurs (Dumoulin & Hay-Smith, 2010).
5
URINARY INCONTINENCE (UI)
Risk factors and complications of stress UI
According to the Australian Institute of Health and Welfare, there are several risk
factors which are associated with the stress UI like advanced age, menopause, pre and post
natal women, obesity, recurrent urinary tract infections, reduced rate of mobility, smoking
and chronic coughing. Familial tendencies (pardiatric nocturnal enuresis) and other specific
type of surgeries like prostatectomies, hysterectomies, pelvic surgeries and complex
neurological diseases like multiple sclerosis (Stothers & Friedman, 2011). Medical disorders
like dementia, diabetes mellitus and diabetes insipidus also found to increase the disease
susceptibility (Continence Foundation of Australia, 2010). Apart from the physiological
susceptibility of the disease the rate of occurrence of stress UI also varies among the
population for example, Caucasian population or the population under Hispanic care also
reside at the high risk zone of developing stress UI (Milsom, Coyne, Nicholson, Kvasz, Chen,
& Wein, 2014).
The main complications which are arising out of the stress UI include skin rashes or
rash in the groin such rashes gradually turn into skin infections and scores (Goepel,
Kirschner-Hermanns, Welz-Barth, Steinwachs, & Rübben, 2010). Stress UI also leads to
urinary tract infection or gets transformed into mixed UI (Stothers & Friedman, 2011).
Mixed UI is an amalgamation of both stress incontinence and urge incontinence (Stothers &
Friedman, 2011).
Impact of stress UI on psychological well-being and intimate relationships of the client
According to the official foundation of the urology under American Urological
Association, Urology Care Foundation, people who are suffering from stress UI, remain
embarrassed about their diseased condition and feel ashamed of informing their
URINARY INCONTINENCE (UI)
Risk factors and complications of stress UI
According to the Australian Institute of Health and Welfare, there are several risk
factors which are associated with the stress UI like advanced age, menopause, pre and post
natal women, obesity, recurrent urinary tract infections, reduced rate of mobility, smoking
and chronic coughing. Familial tendencies (pardiatric nocturnal enuresis) and other specific
type of surgeries like prostatectomies, hysterectomies, pelvic surgeries and complex
neurological diseases like multiple sclerosis (Stothers & Friedman, 2011). Medical disorders
like dementia, diabetes mellitus and diabetes insipidus also found to increase the disease
susceptibility (Continence Foundation of Australia, 2010). Apart from the physiological
susceptibility of the disease the rate of occurrence of stress UI also varies among the
population for example, Caucasian population or the population under Hispanic care also
reside at the high risk zone of developing stress UI (Milsom, Coyne, Nicholson, Kvasz, Chen,
& Wein, 2014).
The main complications which are arising out of the stress UI include skin rashes or
rash in the groin such rashes gradually turn into skin infections and scores (Goepel,
Kirschner-Hermanns, Welz-Barth, Steinwachs, & Rübben, 2010). Stress UI also leads to
urinary tract infection or gets transformed into mixed UI (Stothers & Friedman, 2011).
Mixed UI is an amalgamation of both stress incontinence and urge incontinence (Stothers &
Friedman, 2011).
Impact of stress UI on psychological well-being and intimate relationships of the client
According to the official foundation of the urology under American Urological
Association, Urology Care Foundation, people who are suffering from stress UI, remain
embarrassed about their diseased condition and feel ashamed of informing their
6
URINARY INCONTINENCE (UI)
physiological complications to others and hence they suffer in silence. Stress UI also leads to
the increase in anxiety along with the decrease in the self-esteem (Mota, 2017). Moreover,
incontinence is also associated with profound sense of humiliation (Mota, 2017). However,
leading a life with untreated UI can hamper both the psychological and emotional well-
being of life. The Continence Foundation of Australia is of the opinion that people who are
suffering from the mental illness may develop problems with balder or bowel control and
thus resulting in UI. However, mental illness does not found to increase the risk of
incontinence (The Continence Foundation of Australia, 2015).
Stress UI affects the quality of life in sexual domains too, a condition more significant
among the female population. Female urinary and reproductive systems share same
anatomical structures and thus proving the inter-relation between the urinary problems and
sexual problems of females (Mota, 2017). UI triggers complications associated to sexual life
of female like discharge of urine during coitus, night losses related to emergency and phobia
of bedwetting. Phobias of malodorous along with UI during coitus are cause change in self-
image and self-esteem. Low self-esteem generates a fear of sexual intercourse thereby
lowering sexual activity (Mota, 2017). However, till now there are very few articles that are
capable of successfully evaluating the effectiveness of drug management of incontinence
towards the benefits of female sexual function (Mota, 2017).
Recommendations
Services available in Brimbank Council for clients with stress UI
Brimbank City Council provides in-home support services like home care, personal
care, and respite care (Brimbank City Council, 2015). All these three services are extremely
URINARY INCONTINENCE (UI)
physiological complications to others and hence they suffer in silence. Stress UI also leads to
the increase in anxiety along with the decrease in the self-esteem (Mota, 2017). Moreover,
incontinence is also associated with profound sense of humiliation (Mota, 2017). However,
leading a life with untreated UI can hamper both the psychological and emotional well-
being of life. The Continence Foundation of Australia is of the opinion that people who are
suffering from the mental illness may develop problems with balder or bowel control and
thus resulting in UI. However, mental illness does not found to increase the risk of
incontinence (The Continence Foundation of Australia, 2015).
Stress UI affects the quality of life in sexual domains too, a condition more significant
among the female population. Female urinary and reproductive systems share same
anatomical structures and thus proving the inter-relation between the urinary problems and
sexual problems of females (Mota, 2017). UI triggers complications associated to sexual life
of female like discharge of urine during coitus, night losses related to emergency and phobia
of bedwetting. Phobias of malodorous along with UI during coitus are cause change in self-
image and self-esteem. Low self-esteem generates a fear of sexual intercourse thereby
lowering sexual activity (Mota, 2017). However, till now there are very few articles that are
capable of successfully evaluating the effectiveness of drug management of incontinence
towards the benefits of female sexual function (Mota, 2017).
Recommendations
Services available in Brimbank Council for clients with stress UI
Brimbank City Council provides in-home support services like home care, personal
care, and respite care (Brimbank City Council, 2015). All these three services are extremely
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7
URINARY INCONTINENCE (UI)
significant for the people who are suffering from stress UI and their carers. Stress UI has
been found to cause Urinary tract infection (UTI) (Foxman, 2014). Proper maintenance of
hygiene helps in the prevention of the stress UI related UTI (Gould, Kuntz, Pegues, &
Committee, 2010). Under the banner of personal care, the trained members of Brimbank
Council provides assistance in maintenance of personal hygiene and thereby helping to
eradicate the chances of developing stress UI associated UTI. The home care service helps in
the maintenance of the home hygiene and this is extremely helpful for the family residing
with a patient of UI. UI patients are unable to control their urine leading to urine discharge
in floor and thus home care service of Brimbank City council is helpful (Thüroff, et al., 2011).
Respite care also helps the family members and the carers of the stress UI patients to take
break from the caring responsibilities, a condition significant for the carers of elderly
patients suffering from UI (Brimbank City Council, 2015).
Health professionals dealing stress UI (reflection)
The health professionals effective in the treatment of the stress UI includes, nurse with an
extensive training in the continence care. They will help to access the patient condition and
will work to develop a proper management plan that suits the requirement of the patient
(Vinsnes, Helbostad, Nyrønning, Harkless, Granbo, & Seim, 2012). Pelvic floor
physiotherapists will help in the assessment of the pelvic floor function and will help in
tailoring an exercise program to meet the specific requirement of the patients like pelvic
floor exercise (Price, Dawood, & Jackson, 2010). Dietician will help in designing proper diet
plan along with amount of fluid intake by the patients of stress UI. Occupational therapist
will work in unison with other health professionals in order to ensure the independence and
URINARY INCONTINENCE (UI)
significant for the people who are suffering from stress UI and their carers. Stress UI has
been found to cause Urinary tract infection (UTI) (Foxman, 2014). Proper maintenance of
hygiene helps in the prevention of the stress UI related UTI (Gould, Kuntz, Pegues, &
Committee, 2010). Under the banner of personal care, the trained members of Brimbank
Council provides assistance in maintenance of personal hygiene and thereby helping to
eradicate the chances of developing stress UI associated UTI. The home care service helps in
the maintenance of the home hygiene and this is extremely helpful for the family residing
with a patient of UI. UI patients are unable to control their urine leading to urine discharge
in floor and thus home care service of Brimbank City council is helpful (Thüroff, et al., 2011).
Respite care also helps the family members and the carers of the stress UI patients to take
break from the caring responsibilities, a condition significant for the carers of elderly
patients suffering from UI (Brimbank City Council, 2015).
Health professionals dealing stress UI (reflection)
The health professionals effective in the treatment of the stress UI includes, nurse with an
extensive training in the continence care. They will help to access the patient condition and
will work to develop a proper management plan that suits the requirement of the patient
(Vinsnes, Helbostad, Nyrønning, Harkless, Granbo, & Seim, 2012). Pelvic floor
physiotherapists will help in the assessment of the pelvic floor function and will help in
tailoring an exercise program to meet the specific requirement of the patients like pelvic
floor exercise (Price, Dawood, & Jackson, 2010). Dietician will help in designing proper diet
plan along with amount of fluid intake by the patients of stress UI. Occupational therapist
will work in unison with other health professionals in order to ensure the independence and
8
URINARY INCONTINENCE (UI)
safety of the person suffering from stress UI both outside and inside home (Continence
Foundation of Australia, 2017).
Referrals
An urologist is the best person to do referrals to the services like registered nurse,
physiotherapists and dietician (Continence Foundation of Australia, 2017).
Treatment of stress UI in Australia
The conservative treatment of stress UI includes strengthening and re-education of
the muscles of pelvic floor (Mota, 2017). This can be achieved via physical exercises of pelvic
floor muscle like pelvic floor muscle training. Other treatment includes the application of
techniques like electro-stimulation and bio-feedback techniques (Mota, 2017). There are
also surgical treatment directed towards the recovery of stress UI, such surgical treatment
aims towards the correction of the functional in-adequacy of urethra and urinary sphincter
(Mota, 2017). Surgical treatment is achieved via injection of submucosal polymers at sub-
urethral slings and sphincter (Mota, 2017).
Recommended diet and fluids
Diet and the fluid intake help in the control of the situation associated with stress UI.
The intake of fluid must be strictly regulated with the patients suffering from stress UI. The
fluid intake must be modulated on the basis of age, gender and body weight. However,
intake of carbonated drinks is strictly forbidden in case of stress UI patients as it increases
the more-trips to bathroom. People with stress UI must also avoid drinking during bed-time.
Other food that must be removed from diet includes chocolate, alcoholic drinks, citrus food,
tomato, and food containing sugars and artificial flavours.
URINARY INCONTINENCE (UI)
safety of the person suffering from stress UI both outside and inside home (Continence
Foundation of Australia, 2017).
Referrals
An urologist is the best person to do referrals to the services like registered nurse,
physiotherapists and dietician (Continence Foundation of Australia, 2017).
Treatment of stress UI in Australia
The conservative treatment of stress UI includes strengthening and re-education of
the muscles of pelvic floor (Mota, 2017). This can be achieved via physical exercises of pelvic
floor muscle like pelvic floor muscle training. Other treatment includes the application of
techniques like electro-stimulation and bio-feedback techniques (Mota, 2017). There are
also surgical treatment directed towards the recovery of stress UI, such surgical treatment
aims towards the correction of the functional in-adequacy of urethra and urinary sphincter
(Mota, 2017). Surgical treatment is achieved via injection of submucosal polymers at sub-
urethral slings and sphincter (Mota, 2017).
Recommended diet and fluids
Diet and the fluid intake help in the control of the situation associated with stress UI.
The intake of fluid must be strictly regulated with the patients suffering from stress UI. The
fluid intake must be modulated on the basis of age, gender and body weight. However,
intake of carbonated drinks is strictly forbidden in case of stress UI patients as it increases
the more-trips to bathroom. People with stress UI must also avoid drinking during bed-time.
Other food that must be removed from diet includes chocolate, alcoholic drinks, citrus food,
tomato, and food containing sugars and artificial flavours.
9
URINARY INCONTINENCE (UI)
Role of community nurse in supporting client with stress UI
Management of stress UI disease requires the community nurse to assess the patient
in a holistic manner. The first step of the care model involves the review of systems like
identification of the symptoms associated with the organ systems which is essential for
effective planning of the treatment (Price, Dawood, & Jackson, 2010). The second step of
the care model deals with evaluation of the past medical history along with patient
medication system, menstrual and obstetric history .Social history is also crucial for the
development of the treatment plan for stress UI. Environmental issues and lifestyle pattern
(smoking, nature of food habit and amount of fluid intake) are two basic parameters for
social history (Price, Dawood, & Jackson, 2010). It is the duty of a community nurse to
carefully access the social history before designing the treatment plan.
Community nurse are also required to work in unison with other healthcare
professionals in order to deliver quality care to the patient suffering from stress UI.
However, as per the latest report, the community nurses are more comfortable in assessing
the patients with stress UI and are less sure about the treatment that must be given to the
treatment (Stothers & Friedman, 2011).
Conclusion
Thus from the above discussion it can be concluded 4.2 million Australians are the
victims of the UI and majority of them are females. This high occurrence rate of stress UI
cast significant financial burden over the Australian population. This physiological condition
of sudden urine leakage is aggravated during post surgery condition, UTI, obesity and
immobility. The complications arising out of stress UI creates a huge psychological impact on
the mental and physical well-being of patient, affecting the quality of life. However,
URINARY INCONTINENCE (UI)
Role of community nurse in supporting client with stress UI
Management of stress UI disease requires the community nurse to assess the patient
in a holistic manner. The first step of the care model involves the review of systems like
identification of the symptoms associated with the organ systems which is essential for
effective planning of the treatment (Price, Dawood, & Jackson, 2010). The second step of
the care model deals with evaluation of the past medical history along with patient
medication system, menstrual and obstetric history .Social history is also crucial for the
development of the treatment plan for stress UI. Environmental issues and lifestyle pattern
(smoking, nature of food habit and amount of fluid intake) are two basic parameters for
social history (Price, Dawood, & Jackson, 2010). It is the duty of a community nurse to
carefully access the social history before designing the treatment plan.
Community nurse are also required to work in unison with other healthcare
professionals in order to deliver quality care to the patient suffering from stress UI.
However, as per the latest report, the community nurses are more comfortable in assessing
the patients with stress UI and are less sure about the treatment that must be given to the
treatment (Stothers & Friedman, 2011).
Conclusion
Thus from the above discussion it can be concluded 4.2 million Australians are the
victims of the UI and majority of them are females. This high occurrence rate of stress UI
cast significant financial burden over the Australian population. This physiological condition
of sudden urine leakage is aggravated during post surgery condition, UTI, obesity and
immobility. The complications arising out of stress UI creates a huge psychological impact on
the mental and physical well-being of patient, affecting the quality of life. However,
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
10
URINARY INCONTINENCE (UI)
Brimbank City Council has extended their hands in helping the population suffering from
stress UI. In this regards, community nurses must work in unison with other healthcare
professionals like doctors, physiotherapist, and dietician to provide quality treatment to the
patients of stress UI.
URINARY INCONTINENCE (UI)
Brimbank City Council has extended their hands in helping the population suffering from
stress UI. In this regards, community nurses must work in unison with other healthcare
professionals like doctors, physiotherapist, and dietician to provide quality treatment to the
patients of stress UI.
11
URINARY INCONTINENCE (UI)
Bibliography
Australia, T. e. (2010). Deloitte Access Economics Pty Ltd. Retrieved January 9, 2018, from
Continence Foundation of Australia:
https://www.continence.org.au/data/files/Access_economics_report/dae_incontinence_re
port__19_april_2011.pdf
Brimbank City Council. (2015). Retrieved January 9, 2018, from Brimbank City Council:
https://www.brimbank.vic.gov.au/disabilities/home-support-services
DeLancey, J. O. (2010). Why do women have stress urinary incontinence? Neurourology and
urodynamics , 29.
Dumoulin, C., & Hay-Smith, J. (2010). Pelvic floor muscle training versus no treatment, or inactive
control treatments, for urinary incontinence in women. Cochrane Database Syst Rev , 10-12.
Foxman, B. (2014). Urinary tract infection syndromes: occurrence, recurrence, bacteriology, risk
factors, and disease burden. Infectious Disease Clinics , 1-13.
Goepel, M., Kirschner-Hermanns, R., Welz-Barth, A., Steinwachs, K. C., & Rübben, H. (2010). Urinary
incontinence in the elderly: part 3 of a series of articles on incontinence. Deutsches
ärzteblatt international , 531.
Gould, C. V., Kuntz, G., Pegues, D. A., & Committee, H. I. (2010). Guideline for prevention of
catheter-associated urinary tract infections 2009. Infection Control & Hospital
Epidemiology , 319-326.
Latthe, P. M., Singh, P., Foon, R., & Toozs Hobson, P. (2010). Two routes of transobturator tape‐
procedures in stress urinary incontinence: a meta analysis with direct and indirect‐
URINARY INCONTINENCE (UI)
Bibliography
Australia, T. e. (2010). Deloitte Access Economics Pty Ltd. Retrieved January 9, 2018, from
Continence Foundation of Australia:
https://www.continence.org.au/data/files/Access_economics_report/dae_incontinence_re
port__19_april_2011.pdf
Brimbank City Council. (2015). Retrieved January 9, 2018, from Brimbank City Council:
https://www.brimbank.vic.gov.au/disabilities/home-support-services
DeLancey, J. O. (2010). Why do women have stress urinary incontinence? Neurourology and
urodynamics , 29.
Dumoulin, C., & Hay-Smith, J. (2010). Pelvic floor muscle training versus no treatment, or inactive
control treatments, for urinary incontinence in women. Cochrane Database Syst Rev , 10-12.
Foxman, B. (2014). Urinary tract infection syndromes: occurrence, recurrence, bacteriology, risk
factors, and disease burden. Infectious Disease Clinics , 1-13.
Goepel, M., Kirschner-Hermanns, R., Welz-Barth, A., Steinwachs, K. C., & Rübben, H. (2010). Urinary
incontinence in the elderly: part 3 of a series of articles on incontinence. Deutsches
ärzteblatt international , 531.
Gould, C. V., Kuntz, G., Pegues, D. A., & Committee, H. I. (2010). Guideline for prevention of
catheter-associated urinary tract infections 2009. Infection Control & Hospital
Epidemiology , 319-326.
Latthe, P. M., Singh, P., Foon, R., & Toozs Hobson, P. (2010). Two routes of transobturator tape‐
procedures in stress urinary incontinence: a meta analysis with direct and indirect‐
12
URINARY INCONTINENCE (UI)
comparison of randomized trials. BJU international , 68-76.
Lucas, M. G., Bedretdinova, D., Bosch, J. L., Burkhard, F., Cruz, F., Nambiar, A. K., et al. (2012).
Guidelines on urinary incontinence. European Association of Urology .
Markland, A. D., Goode, P. S., Redden, D. T., Borrud, L. G., & Burgio, K. L. (2010). Prevalence of
urinary incontinence in men: results from the national health and nutrition examination
survey. The Journal of urology , 1022-1027.
Milsom, I., Coyne, K. S., Nicholson, S., Kvasz, M., Chen, C. I., & Wein, A. J. (2014). Global prevalence
and economic burden of urgency urinary incontinence: a systematic review. European
urology , 79-95.
Mota, R. L. (2017). Female urinary incontinence and sexuality. International brazil journal urology ,
20-28.
Price, N., Dawood, R., & Jackson, S. R. (2010). Pelvic floor exercise for urinary incontinence: a
systematic literature review. Maturitas , 309-315.
Sangsawang, B., & Sangsawang, N. (2013). Stress urinary incontinence in pregnant women: a review
of prevalence, pathophysiology, and treatment. International urogynecology journal , 901-
912.
Stothers, L., & Friedman, B. (2011). Risk factors for the development of stress urinary incontinence
in women. Current urology reports , 363.
Thüroff, J. W., Abrams, P., Andersson, K. E., Artibani, W., Chapple, C. R., Drake, M. J., et al. (2011).
EAU guidelines on urinary incontinence. Actas Urológicas Españolas (English Edition) , 373-
388.
URINARY INCONTINENCE (UI)
comparison of randomized trials. BJU international , 68-76.
Lucas, M. G., Bedretdinova, D., Bosch, J. L., Burkhard, F., Cruz, F., Nambiar, A. K., et al. (2012).
Guidelines on urinary incontinence. European Association of Urology .
Markland, A. D., Goode, P. S., Redden, D. T., Borrud, L. G., & Burgio, K. L. (2010). Prevalence of
urinary incontinence in men: results from the national health and nutrition examination
survey. The Journal of urology , 1022-1027.
Milsom, I., Coyne, K. S., Nicholson, S., Kvasz, M., Chen, C. I., & Wein, A. J. (2014). Global prevalence
and economic burden of urgency urinary incontinence: a systematic review. European
urology , 79-95.
Mota, R. L. (2017). Female urinary incontinence and sexuality. International brazil journal urology ,
20-28.
Price, N., Dawood, R., & Jackson, S. R. (2010). Pelvic floor exercise for urinary incontinence: a
systematic literature review. Maturitas , 309-315.
Sangsawang, B., & Sangsawang, N. (2013). Stress urinary incontinence in pregnant women: a review
of prevalence, pathophysiology, and treatment. International urogynecology journal , 901-
912.
Stothers, L., & Friedman, B. (2011). Risk factors for the development of stress urinary incontinence
in women. Current urology reports , 363.
Thüroff, J. W., Abrams, P., Andersson, K. E., Artibani, W., Chapple, C. R., Drake, M. J., et al. (2011).
EAU guidelines on urinary incontinence. Actas Urológicas Españolas (English Edition) , 373-
388.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
13
URINARY INCONTINENCE (UI)
Vinsnes, A. G., Helbostad, J. L., Nyrønning, S., Harkless, G. E., Granbo, R., & Seim, A. (2012). Effect of
physical training on urinary incontinence: a randomized parallel group trial in nursing
homes. Clinical interventions in aging , 45.
URINARY INCONTINENCE (UI)
Vinsnes, A. G., Helbostad, J. L., Nyrønning, S., Harkless, G. E., Granbo, R., & Seim, A. (2012). Effect of
physical training on urinary incontinence: a randomized parallel group trial in nursing
homes. Clinical interventions in aging , 45.

14
URINARY INCONTINENCE (UI)
URINARY INCONTINENCE (UI)
1 out of 15
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.

