The Use of Focused Ultrasound in Shock: A Clinical Review
VerifiedAdded on 2023/04/25
|12
|4309
|426
Report
AI Summary
This report comprehensively examines the application of focused ultrasound in the diagnosis and management of shock, a critical clinical syndrome characterized by inadequate cellular oxygenation. It details the four main categories of shock—cardiogenic, hypovolemic, distributive, and obstructive—and emphasizes the challenges in achieving accurate and timely diagnoses. The report highlights the significance of focused ultrasound or point-of-care ultrasound (POCUS) as a rapid, non-invasive bedside tool, particularly in emergency medicine and critical care settings. It explores various POCUS protocols, including the RUSH exam (Rapid Ultrasound in Shock) and FAST exam (focused assessment with sonography for trauma), outlining their components and diagnostic capabilities. The report discusses the diagnostic accuracy of focused ultrasound, comparing it to traditional methods, and the importance of early recognition and treatment in improving patient outcomes. It also reviews the existing evidence on the impact of focused ultrasound on patient outcomes and includes findings from key studies and protocols. Additionally, the report provides a detailed summary of the RUSH protocol, including its three key steps (Pump, Tank, and Pipes), and explores the use of POCUS in trauma and cardiac arrest situations. The report concludes by discussing the evidence that supports the use of ultrasound by clinicians in the diagnosis and management of shock and its role in improving patient outcomes.
Focused Ultrasound Assisting Clinicians in the Diagnosis and Management of Shock
Shock is a clinical syndrome in which there is inadequate cellular and tissue oxygenation due
to circulatory failure [1 ]. Hypotension is the cardinal feature of shock in which the systolic
blood pressure is less than 90 mmHg or the mean arterial pressure is less than 65 mmHg as
suggested by the latest international consensus definitions for sepsis and septic shock [2].
There are four varied categories of shock as per underlying pathophysiology which are
cardiogenic shock, hypovolemic shock, distributive shock, obstructive shock (Richards and
Wilcox, 2014). Marx, Walls and Hockberger (2013) adds a fifth category to it which is the
shock related to poisoning of cells. These shocks need to be diagnosed and managed urgently
by the clinicians to save the precious lives.The correct cause and the differential diagnosis in
a symptomatic non traumatic, undifferentiated hypotension is often very difficult and
challenging.The initial diagnosis of shock etiology is correct only in 50% of patients [3]
The evidence shows that the in-hospital mortality rate in such types of hypotensive patients
equals or exceeds the mortality rate of other critical conditions like acute myocardial
infarction, pulmonary embolism, or penetrating chest trauma. [4,5. 6,7,8]. Urgent strategies
and special protocols are followed world wide to diagnose and treat the shocked patients [9].
Focused Ultrasound in non traumatic Hypotension
Focused ultrasound is a thermoblative procedure which has been studied for more than 60
years [10]. It has been utilized for various treatments of shocks [11]. A land mark study
(Jones et al CCM 2004), done on non traumatic shock patients, in which the systolic B.P. was
less than 100 and the shock index SI >1, showed the importance of the early use of the
focused ultrasound. Focused echo and FAST ultrasound were used at 15 and 30 minutes
intervals from the time of arrival.
At 15 minutes interval, only 50% of the cases had correct diagnosis and differential diagnosis
in the clinical assessment group, as compared to the 80% correct diagnosis in the ultrasound
assessment group.
Focus ultrasound or point of care ultrasound POCUS is now an important bedside tool in
emergency medicine and critical care .POCUS means that the portable ultrasound can be
used anywhere in the ambulance, in the emergency departments or any other critical settings,
wherever the patient is located.
PoCUS assists the emergency physicians for a rapid and accurate differentiation between the
major shock types in the undifferentiated hypotensive patients presenting to the ED in a very
a short period of time (average of 6 minutes) [3].
As compared to the traditional imaging it is non invasive , more safe and rapid [12].Early
recognition and appropriate treatment of shock have been shown to decrease mortality
[13,14].
Shock is a clinical syndrome in which there is inadequate cellular and tissue oxygenation due
to circulatory failure [1 ]. Hypotension is the cardinal feature of shock in which the systolic
blood pressure is less than 90 mmHg or the mean arterial pressure is less than 65 mmHg as
suggested by the latest international consensus definitions for sepsis and septic shock [2].
There are four varied categories of shock as per underlying pathophysiology which are
cardiogenic shock, hypovolemic shock, distributive shock, obstructive shock (Richards and
Wilcox, 2014). Marx, Walls and Hockberger (2013) adds a fifth category to it which is the
shock related to poisoning of cells. These shocks need to be diagnosed and managed urgently
by the clinicians to save the precious lives.The correct cause and the differential diagnosis in
a symptomatic non traumatic, undifferentiated hypotension is often very difficult and
challenging.The initial diagnosis of shock etiology is correct only in 50% of patients [3]
The evidence shows that the in-hospital mortality rate in such types of hypotensive patients
equals or exceeds the mortality rate of other critical conditions like acute myocardial
infarction, pulmonary embolism, or penetrating chest trauma. [4,5. 6,7,8]. Urgent strategies
and special protocols are followed world wide to diagnose and treat the shocked patients [9].
Focused Ultrasound in non traumatic Hypotension
Focused ultrasound is a thermoblative procedure which has been studied for more than 60
years [10]. It has been utilized for various treatments of shocks [11]. A land mark study
(Jones et al CCM 2004), done on non traumatic shock patients, in which the systolic B.P. was
less than 100 and the shock index SI >1, showed the importance of the early use of the
focused ultrasound. Focused echo and FAST ultrasound were used at 15 and 30 minutes
intervals from the time of arrival.
At 15 minutes interval, only 50% of the cases had correct diagnosis and differential diagnosis
in the clinical assessment group, as compared to the 80% correct diagnosis in the ultrasound
assessment group.
Focus ultrasound or point of care ultrasound POCUS is now an important bedside tool in
emergency medicine and critical care .POCUS means that the portable ultrasound can be
used anywhere in the ambulance, in the emergency departments or any other critical settings,
wherever the patient is located.
PoCUS assists the emergency physicians for a rapid and accurate differentiation between the
major shock types in the undifferentiated hypotensive patients presenting to the ED in a very
a short period of time (average of 6 minutes) [3].
As compared to the traditional imaging it is non invasive , more safe and rapid [12].Early
recognition and appropriate treatment of shock have been shown to decrease mortality
[13,14].
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
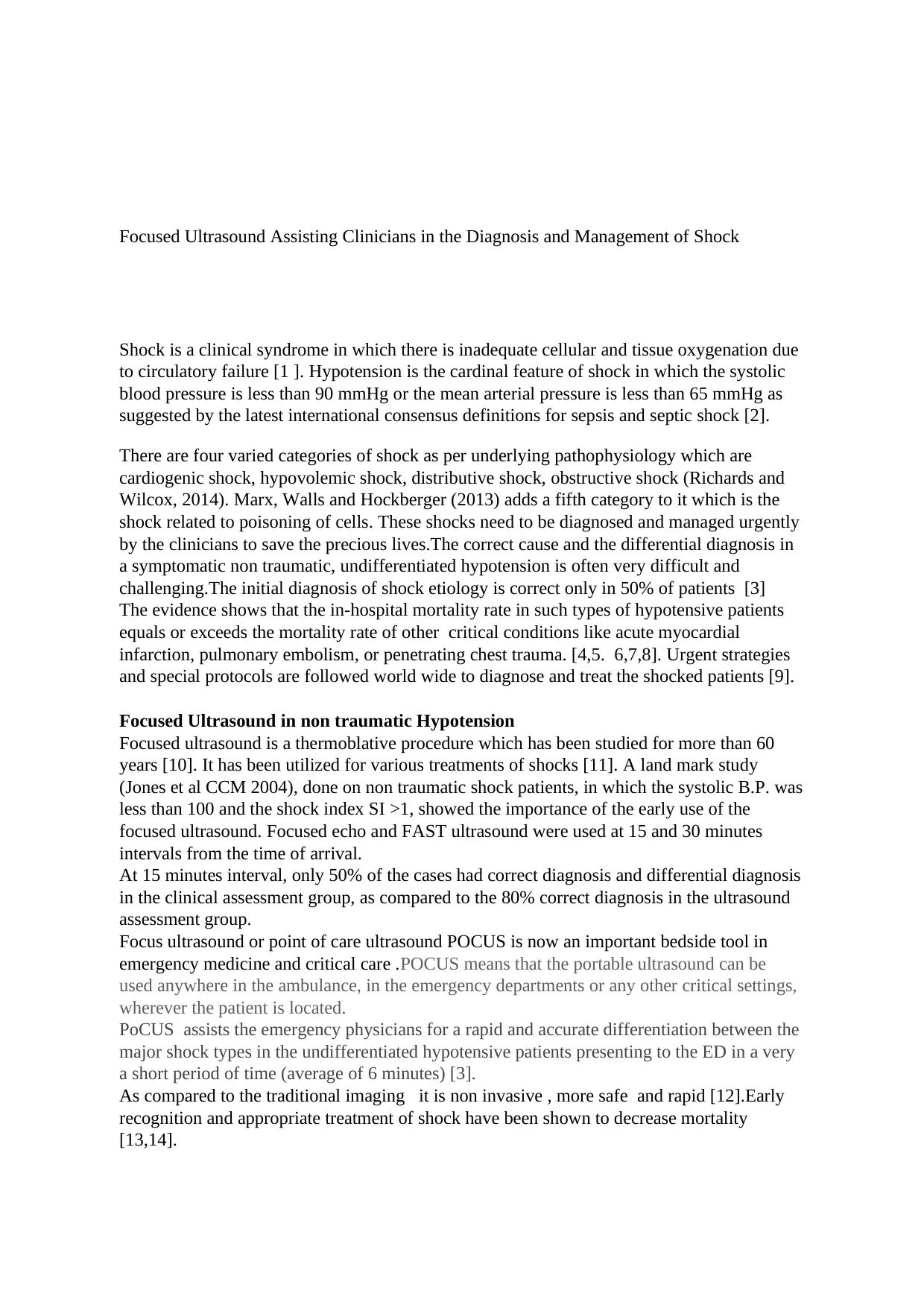
The paper by Atkinson et al. (2009) finds that protocols for focused ultrasound assessment
for the patients of non- traumatic hypotension have been proposed in terms of the Shock
protocol which includes the Abdominal and Cardiac Evaluation with Sonography. In fact,
there are various ways to focus ultrasound. These can be done through a curved transducer, a
lens, a phased array or a combination of any of the three mentioned. When the septic shock
is considered, the focused cardiac ultrasound would identify the required sonographic
findings associated with the decrease in the size of LV (Left Ventrical) which is usual in
hypovolemia throughout the cardiac cycle but substantially decreases in hyperdynamic states.
These findings can possibly help the clinicians in adapting suitable treatments to varied
stages of septic shock.
Reflecting a trend to integrate ultrasound early into the care of the critically ill patient,
multiple resuscitation protocols such as ACES,FATE, FEEL and RUSH have been recently
developed [15—19]. Each of these protocols combines many of the same core ultrasound
elements, differing mainly in the priority of the exam sequence for the assessment of the
heart, lungs, the vena cava, and a focused assessment of the abdomen to find free fluid.The
diagnosed findings of of the shock guide for the early resuscitation strategies such as fluid
versus vasopressor support and the other therapeutic procedures such as pericardiocentesis
and laparotomy.
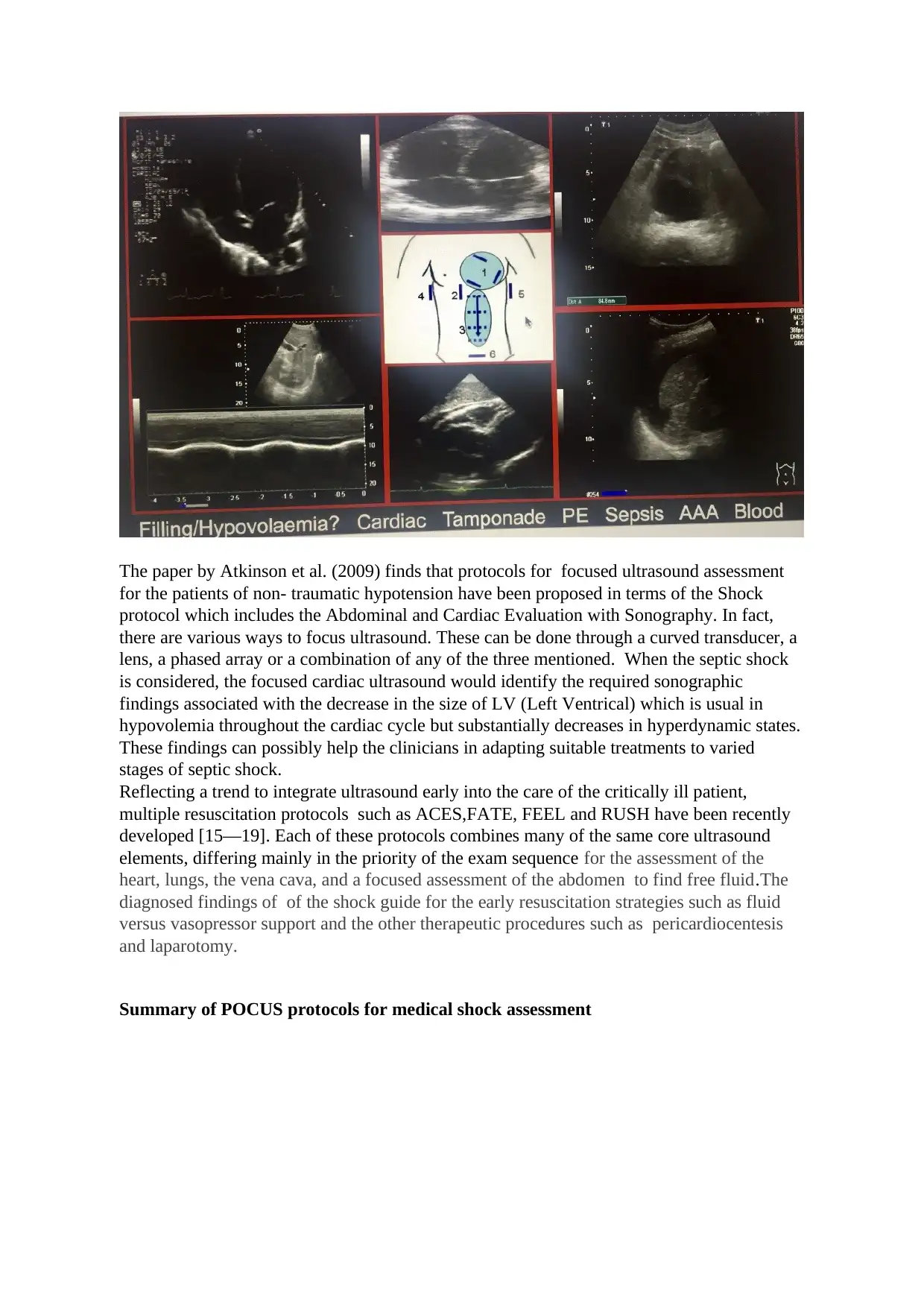
Summary of POCUS protocols for medical shock assessment
for the patients of non- traumatic hypotension have been proposed in terms of the Shock
protocol which includes the Abdominal and Cardiac Evaluation with Sonography. In fact,
there are various ways to focus ultrasound. These can be done through a curved transducer, a
lens, a phased array or a combination of any of the three mentioned. When the septic shock
is considered, the focused cardiac ultrasound would identify the required sonographic
findings associated with the decrease in the size of LV (Left Ventrical) which is usual in
hypovolemia throughout the cardiac cycle but substantially decreases in hyperdynamic states.
These findings can possibly help the clinicians in adapting suitable treatments to varied
stages of septic shock.
Reflecting a trend to integrate ultrasound early into the care of the critically ill patient,
multiple resuscitation protocols such as ACES,FATE, FEEL and RUSH have been recently
developed [15—19]. Each of these protocols combines many of the same core ultrasound
elements, differing mainly in the priority of the exam sequence for the assessment of the
heart, lungs, the vena cava, and a focused assessment of the abdomen to find free fluid.The
diagnosed findings of of the shock guide for the early resuscitation strategies such as fluid
versus vasopressor support and the other therapeutic procedures such as pericardiocentesis
and laparotomy.
Summary of POCUS protocols for medical shock assessment
Rapid Ultrasound in shock RUSH exam is an easy and quick shock ultrasound protocol
[17].
The RUSH exam consists of 3-part bedside physiologic assessments .
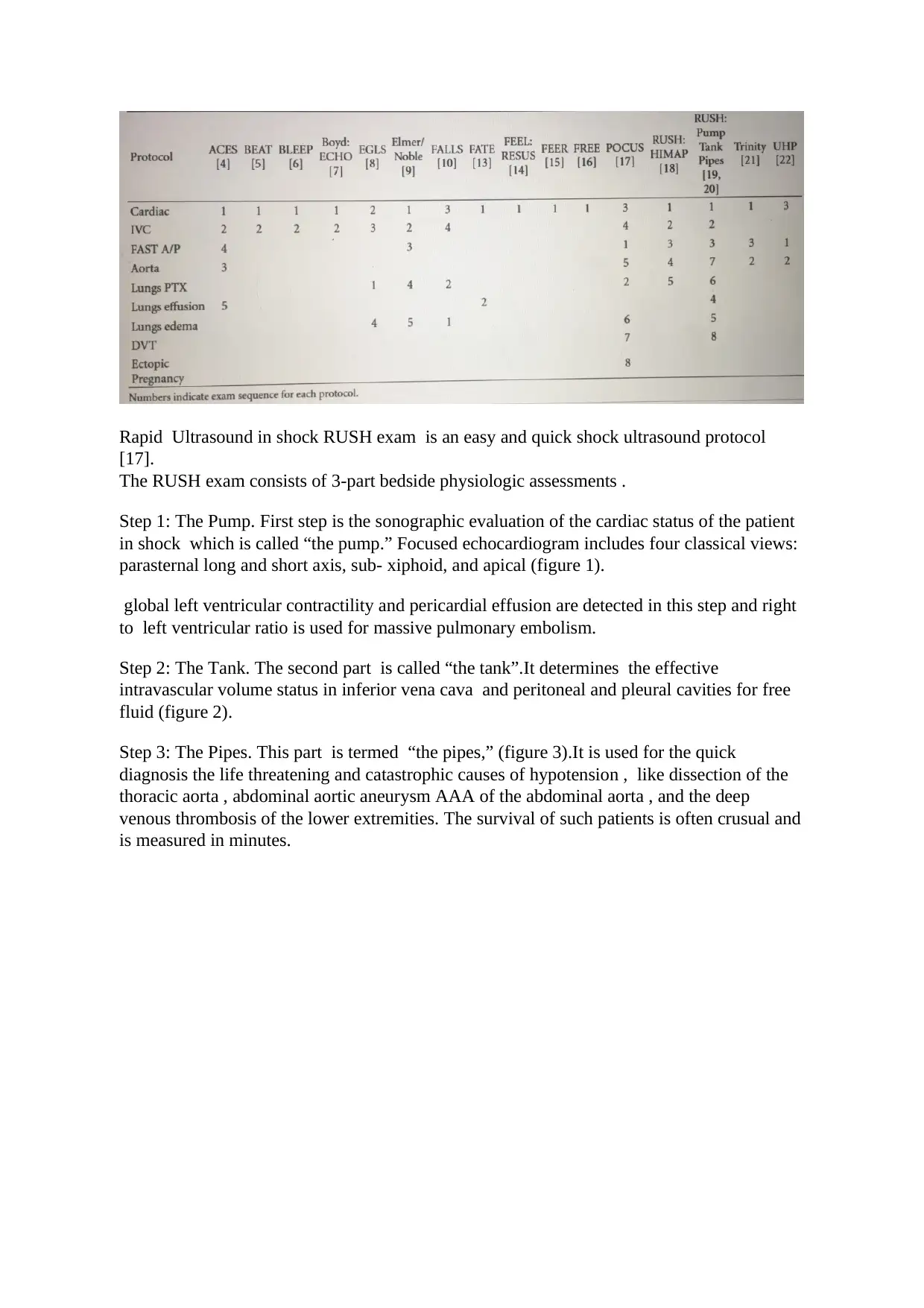
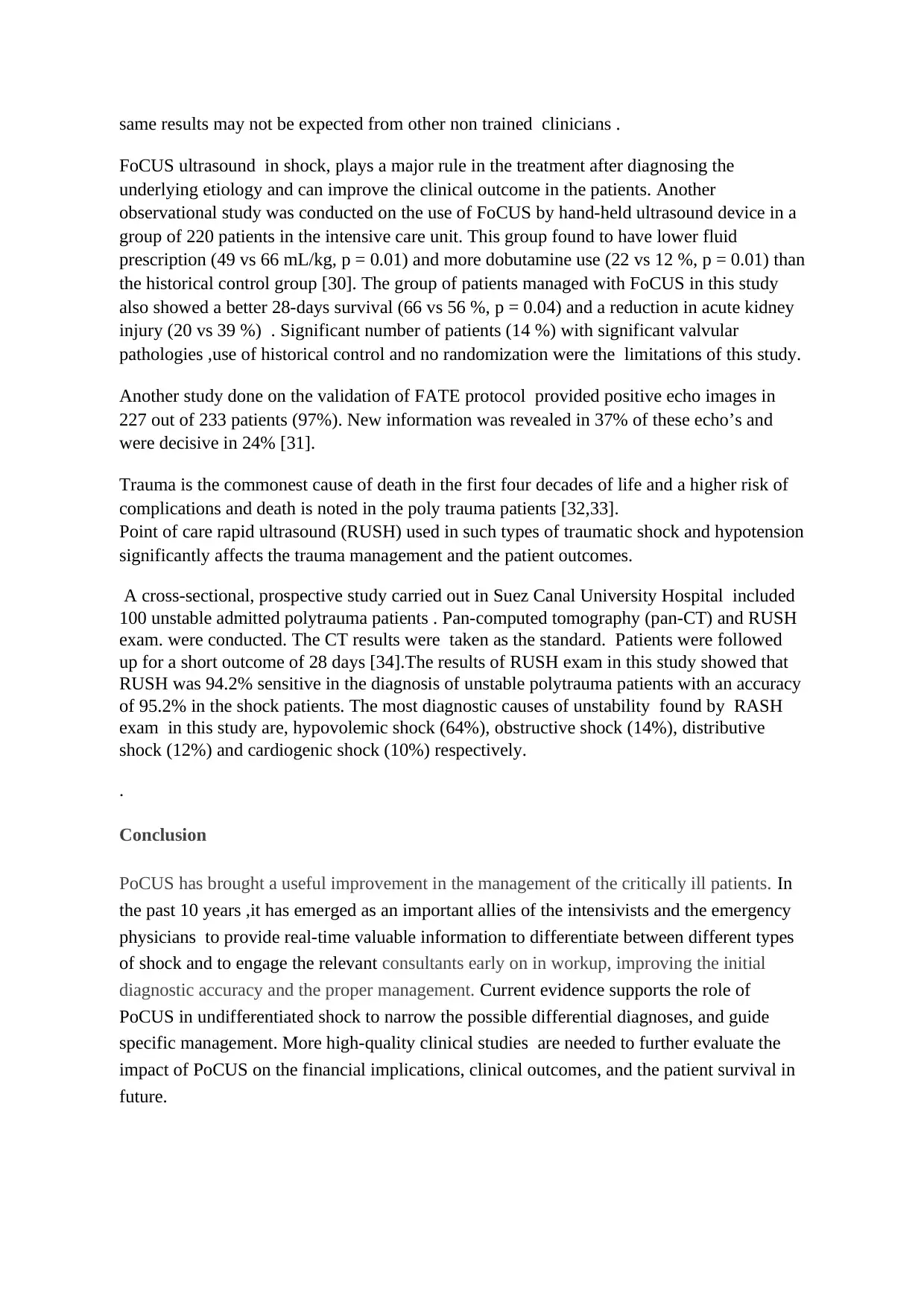
Step 1: The Pump. First step is the sonographic evaluation of the cardiac status of the patient
in shock which is called “the pump.” Focused echocardiogram includes four classical views:
parasternal long and short axis, sub- xiphoid, and apical (figure 1).
global left ventricular contractility and pericardial effusion are detected in this step and right
to left ventricular ratio is used for massive pulmonary embolism.
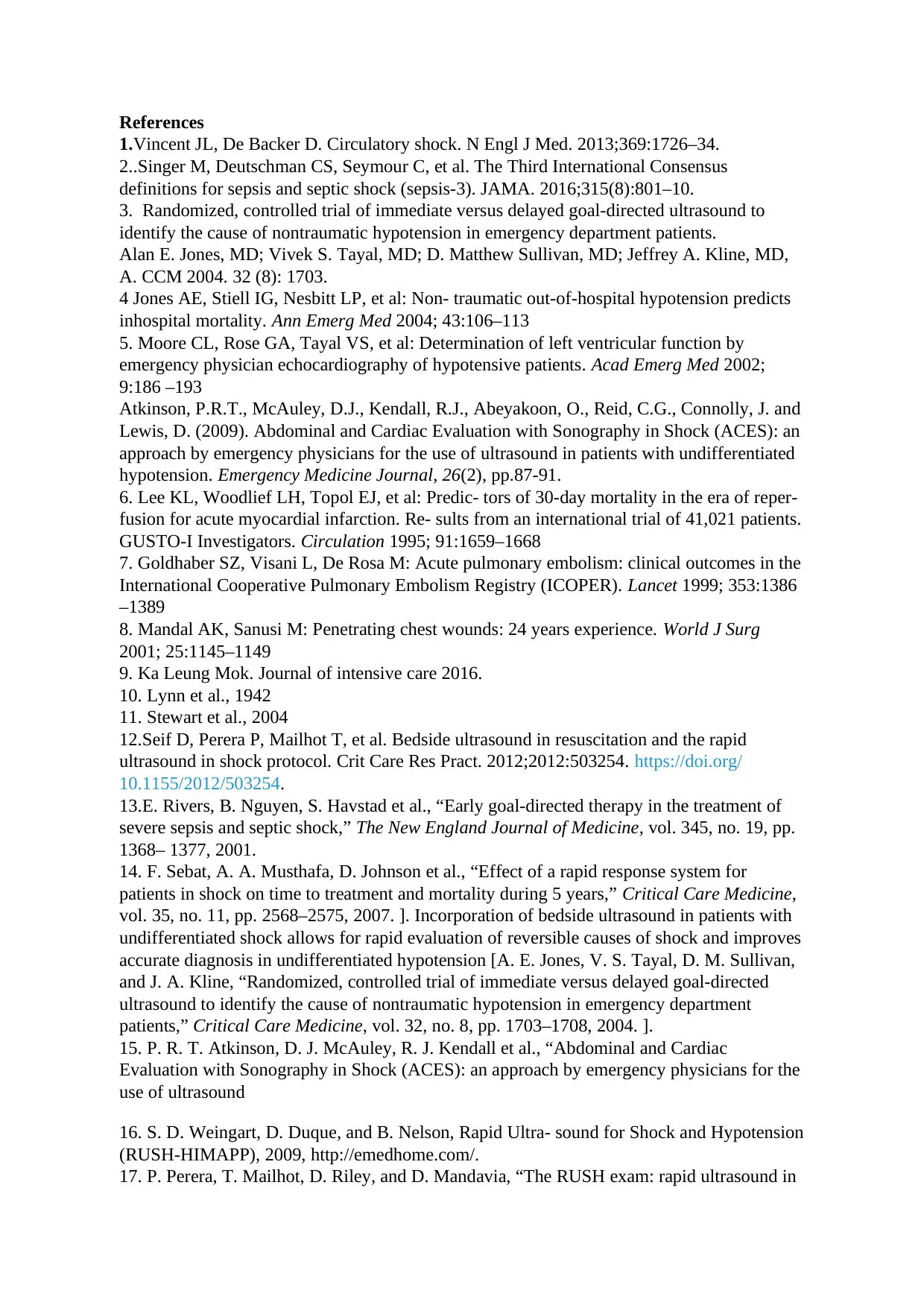
Step 2: The Tank. The second part is called “the tank”.It determines the effective
intravascular volume status in inferior vena cava and peritoneal and pleural cavities for free
fluid (figure 2).
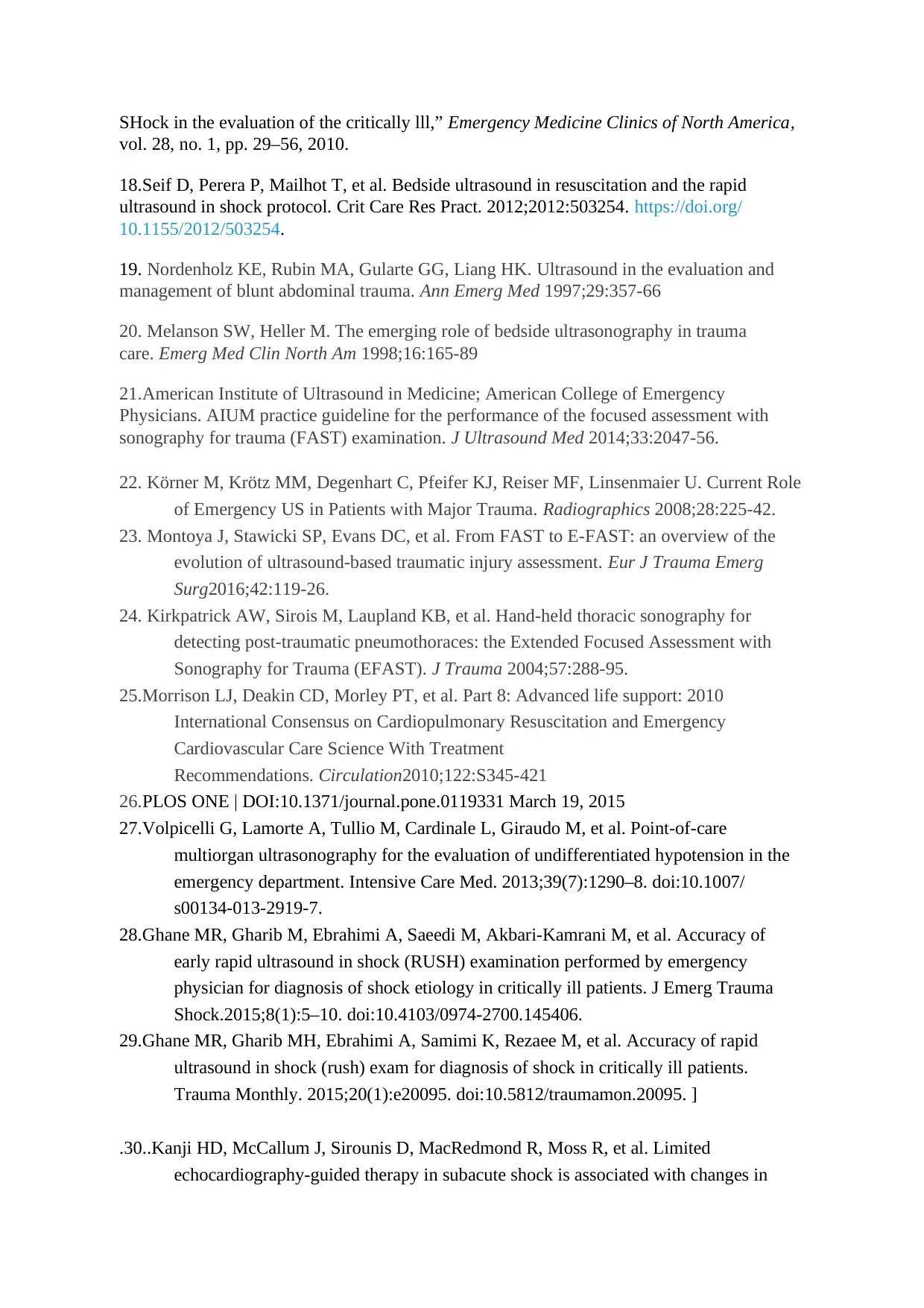
Step 3: The Pipes. This part is termed “the pipes,” (figure 3).It is used for the quick
diagnosis the life threatening and catastrophic causes of hypotension , like dissection of the
thoracic aorta , abdominal aortic aneurysm AAA of the abdominal aorta , and the deep
venous thrombosis of the lower extremities. The survival of such patients is often crusual and
is measured in minutes.
[17].
The RUSH exam consists of 3-part bedside physiologic assessments .
Step 1: The Pump. First step is the sonographic evaluation of the cardiac status of the patient
in shock which is called “the pump.” Focused echocardiogram includes four classical views:
parasternal long and short axis, sub- xiphoid, and apical (figure 1).
global left ventricular contractility and pericardial effusion are detected in this step and right
to left ventricular ratio is used for massive pulmonary embolism.
Step 2: The Tank. The second part is called “the tank”.It determines the effective
intravascular volume status in inferior vena cava and peritoneal and pleural cavities for free
fluid (figure 2).
Step 3: The Pipes. This part is termed “the pipes,” (figure 3).It is used for the quick
diagnosis the life threatening and catastrophic causes of hypotension , like dissection of the
thoracic aorta , abdominal aortic aneurysm AAA of the abdominal aorta , and the deep
venous thrombosis of the lower extremities. The survival of such patients is often crusual and
is measured in minutes.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
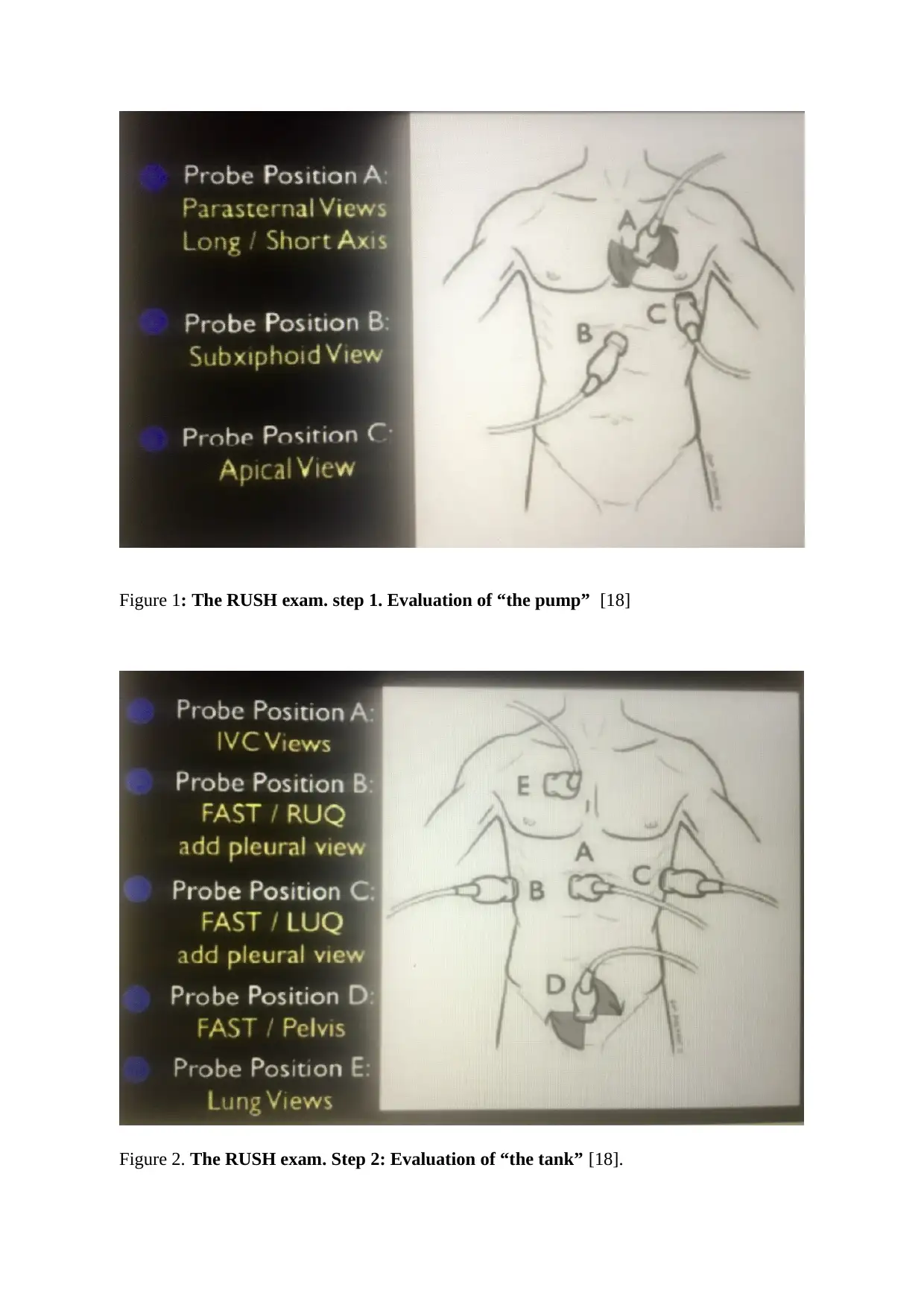
Figure 1: The RUSH exam. step 1. Evaluation of “the pump” [18]
Figure 2. The RUSH exam. Step 2: Evaluation of “the tank” [18].
Figure 2. The RUSH exam. Step 2: Evaluation of “the tank” [18].
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
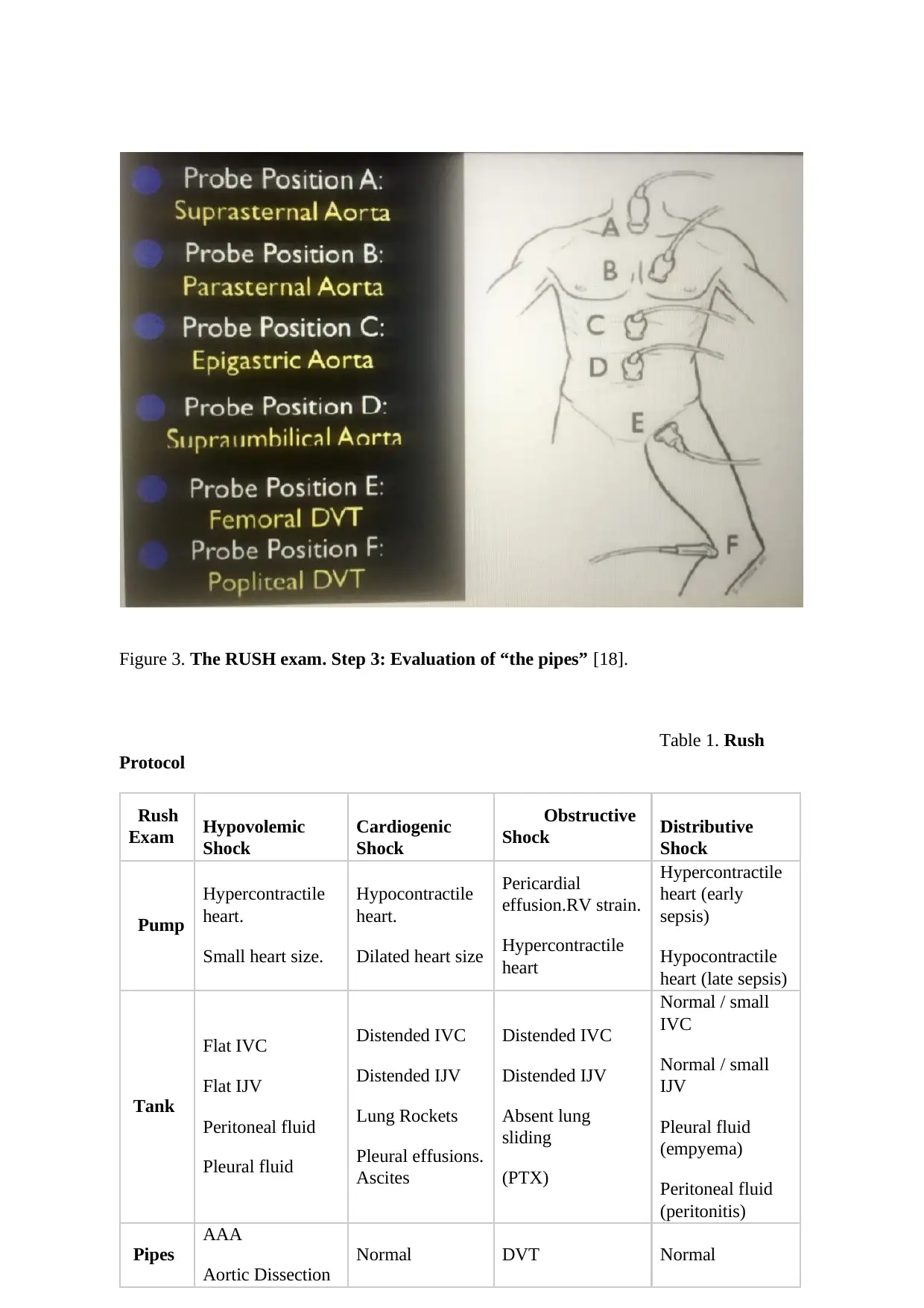
Figure 3. The RUSH exam. Step 3: Evaluation of “the pipes” [18].
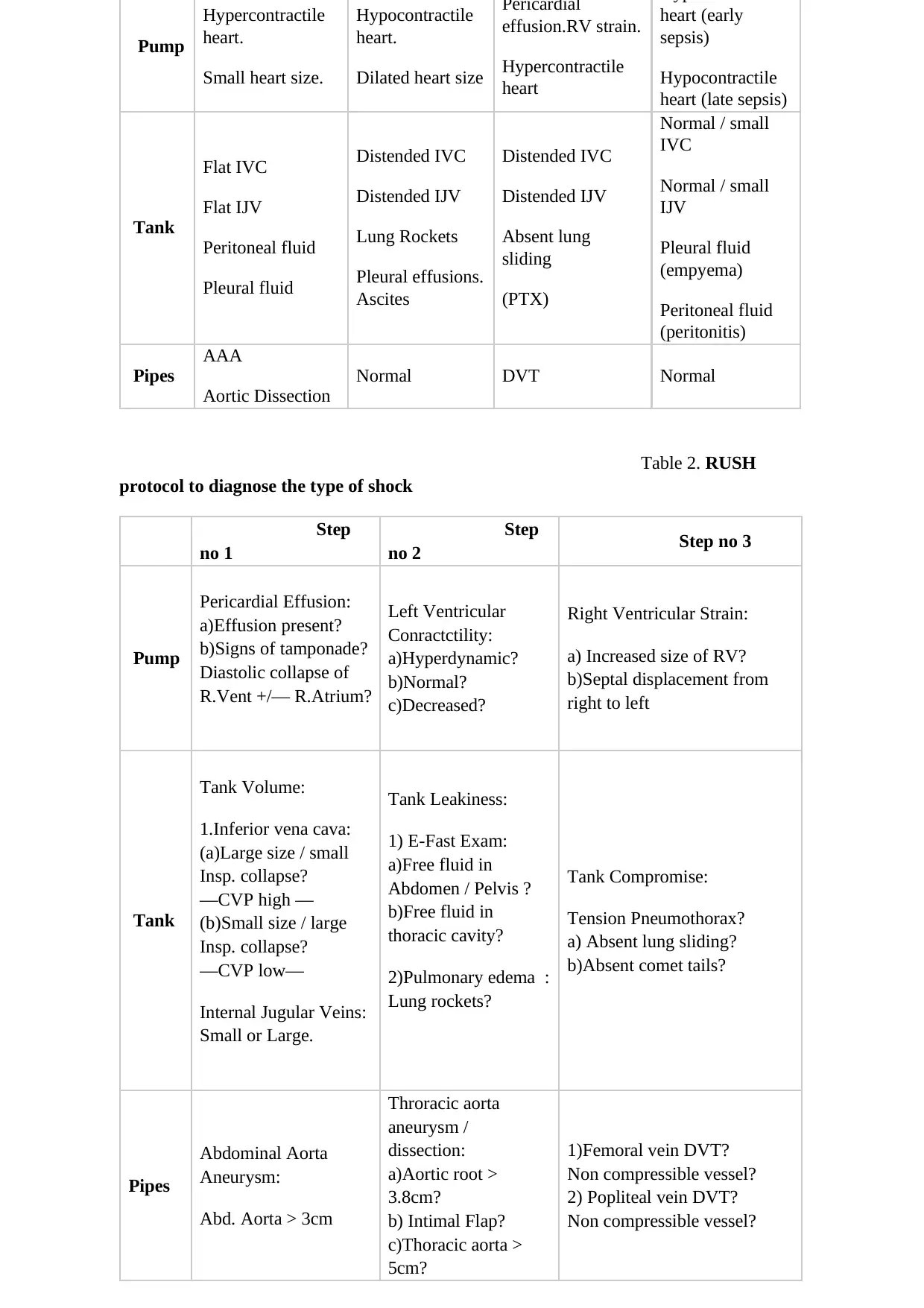
Table 1. Rush
Protocol
Rush
Exam Hypovolemic
Shock
Cardiogenic
Shock
Obstructive
Shock Distributive
Shock
Pump
Hypercontractile
heart.
Small heart size.
Hypocontractile
heart.
Dilated heart size
Pericardial
effusion.RV strain.
Hypercontractile
heart
Hypercontractile
heart (early
sepsis)
Hypocontractile
heart (late sepsis)
Tank
Flat IVC
Flat IJV
Peritoneal fluid
Pleural fluid
Distended IVC
Distended IJV
Lung Rockets
Pleural effusions.
Ascites
Distended IVC
Distended IJV
Absent lung
sliding
(PTX)
Normal / small
IVC
Normal / small
IJV
Pleural fluid
(empyema)
Peritoneal fluid
(peritonitis)
Pipes
AAA
Aortic Dissection
Normal DVT Normal
Table 1. Rush
Protocol
Rush
Exam Hypovolemic
Shock
Cardiogenic
Shock
Obstructive
Shock Distributive
Shock
Pump
Hypercontractile
heart.
Small heart size.
Hypocontractile
heart.
Dilated heart size
Pericardial
effusion.RV strain.
Hypercontractile
heart
Hypercontractile
heart (early
sepsis)
Hypocontractile
heart (late sepsis)
Tank
Flat IVC
Flat IJV
Peritoneal fluid
Pleural fluid
Distended IVC
Distended IJV
Lung Rockets
Pleural effusions.
Ascites
Distended IVC
Distended IJV
Absent lung
sliding
(PTX)
Normal / small
IVC
Normal / small
IJV
Pleural fluid
(empyema)
Peritoneal fluid
(peritonitis)
Pipes
AAA
Aortic Dissection
Normal DVT Normal
Pump
Hypercontractile
heart.
Small heart size.
Hypocontractile
heart.
Dilated heart size
Pericardial
effusion.RV strain.
Hypercontractile
heart
heart (early
sepsis)
Hypocontractile
heart (late sepsis)
Tank
Flat IVC
Flat IJV
Peritoneal fluid
Pleural fluid
Distended IVC
Distended IJV
Lung Rockets
Pleural effusions.
Ascites
Distended IVC
Distended IJV
Absent lung
sliding
(PTX)
Normal / small
IVC
Normal / small
IJV
Pleural fluid
(empyema)
Peritoneal fluid
(peritonitis)
Pipes
AAA
Aortic Dissection
Normal DVT Normal
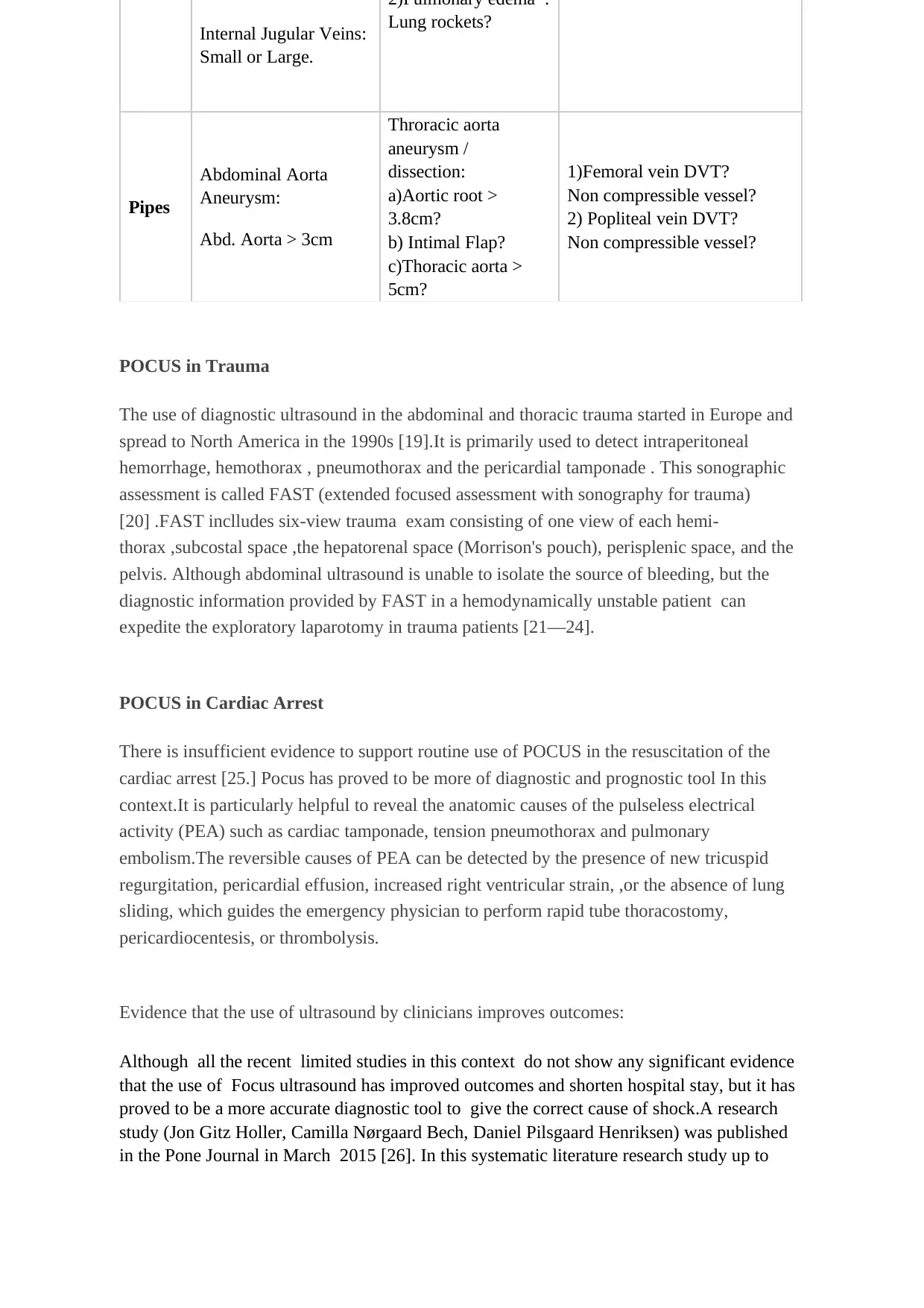
Table 2. RUSH
protocol to diagnose the type of shock
Step
no 1
Step
no 2 Step no 3
Pump
Pericardial Effusion:
a)Effusion present?
b)Signs of tamponade?
Diastolic collapse of
R.Vent +/— R.Atrium?
Left Ventricular
Conractctility:
a)Hyperdynamic?
b)Normal?
c)Decreased?
Right Ventricular Strain:
a) Increased size of RV?
b)Septal displacement from
right to left
Tank
Tank Volume:
1.Inferior vena cava:
(a)Large size / small
Insp. collapse?
—CVP high —
(b)Small size / large
Insp. collapse?
—CVP low—
Internal Jugular Veins:
Small or Large.
Tank Leakiness:
1) E-Fast Exam:
a)Free fluid in
Abdomen / Pelvis ?
b)Free fluid in
thoracic cavity?
2)Pulmonary edema :
Lung rockets?
Tank Compromise:
Tension Pneumothorax?
a) Absent lung sliding?
b)Absent comet tails?
Pipes
Abdominal Aorta
Aneurysm:
Abd. Aorta > 3cm
Throracic aorta
aneurysm /
dissection:
a)Aortic root >
3.8cm?
b) Intimal Flap?
c)Thoracic aorta >
5cm?
1)Femoral vein DVT?
Non compressible vessel?
2) Popliteal vein DVT?
Non compressible vessel?
Hypercontractile
heart.
Small heart size.
Hypocontractile
heart.
Dilated heart size
Pericardial
effusion.RV strain.
Hypercontractile
heart
heart (early
sepsis)
Hypocontractile
heart (late sepsis)
Tank
Flat IVC
Flat IJV
Peritoneal fluid
Pleural fluid
Distended IVC
Distended IJV
Lung Rockets
Pleural effusions.
Ascites
Distended IVC
Distended IJV
Absent lung
sliding
(PTX)
Normal / small
IVC
Normal / small
IJV
Pleural fluid
(empyema)
Peritoneal fluid
(peritonitis)
Pipes
AAA
Aortic Dissection
Normal DVT Normal
Table 2. RUSH
protocol to diagnose the type of shock
Step
no 1
Step
no 2 Step no 3
Pump
Pericardial Effusion:
a)Effusion present?
b)Signs of tamponade?
Diastolic collapse of
R.Vent +/— R.Atrium?
Left Ventricular
Conractctility:
a)Hyperdynamic?
b)Normal?
c)Decreased?
Right Ventricular Strain:
a) Increased size of RV?
b)Septal displacement from
right to left
Tank
Tank Volume:
1.Inferior vena cava:
(a)Large size / small
Insp. collapse?
—CVP high —
(b)Small size / large
Insp. collapse?
—CVP low—
Internal Jugular Veins:
Small or Large.
Tank Leakiness:
1) E-Fast Exam:
a)Free fluid in
Abdomen / Pelvis ?
b)Free fluid in
thoracic cavity?
2)Pulmonary edema :
Lung rockets?
Tank Compromise:
Tension Pneumothorax?
a) Absent lung sliding?
b)Absent comet tails?
Pipes
Abdominal Aorta
Aneurysm:
Abd. Aorta > 3cm
Throracic aorta
aneurysm /
dissection:
a)Aortic root >
3.8cm?
b) Intimal Flap?
c)Thoracic aorta >
5cm?
1)Femoral vein DVT?
Non compressible vessel?
2) Popliteal vein DVT?
Non compressible vessel?
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Internal Jugular Veins:
Small or Large.
2)Pulmonary edema :
Lung rockets?
Pipes
Abdominal Aorta
Aneurysm:
Abd. Aorta > 3cm
Throracic aorta
aneurysm /
dissection:
a)Aortic root >
3.8cm?
b) Intimal Flap?
c)Thoracic aorta >
5cm?
1)Femoral vein DVT?
Non compressible vessel?
2) Popliteal vein DVT?
Non compressible vessel?
POCUS in Trauma
The use of diagnostic ultrasound in the abdominal and thoracic trauma started in Europe and
spread to North America in the 1990s [19].It is primarily used to detect intraperitoneal
hemorrhage, hemothorax , pneumothorax and the pericardial tamponade . This sonographic
assessment is called FAST (extended focused assessment with sonography for trauma)
[20] .FAST inclludes six-view trauma exam consisting of one view of each hemi-
thorax ,subcostal space ,the hepatorenal space (Morrison's pouch), perisplenic space, and the
pelvis. Although abdominal ultrasound is unable to isolate the source of bleeding, but the
diagnostic information provided by FAST in a hemodynamically unstable patient can
expedite the exploratory laparotomy in trauma patients [21—24].
POCUS in Cardiac Arrest
There is insufficient evidence to support routine use of POCUS in the resuscitation of the
cardiac arrest [25.] Pocus has proved to be more of diagnostic and prognostic tool In this
context.It is particularly helpful to reveal the anatomic causes of the pulseless electrical
activity (PEA) such as cardiac tamponade, tension pneumothorax and pulmonary
embolism.The reversible causes of PEA can be detected by the presence of new tricuspid
regurgitation, pericardial effusion, increased right ventricular strain, ,or the absence of lung
sliding, which guides the emergency physician to perform rapid tube thoracostomy,
pericardiocentesis, or thrombolysis.
Evidence that the use of ultrasound by clinicians improves outcomes:
Although all the recent limited studies in this context do not show any significant evidence
that the use of Focus ultrasound has improved outcomes and shorten hospital stay, but it has
proved to be a more accurate diagnostic tool to give the correct cause of shock.A research
study (Jon Gitz Holler, Camilla Nørgaard Bech, Daniel Pilsgaard Henriksen) was published
in the Pone Journal in March 2015 [26]. In this systematic literature research study up to
Small or Large.
2)Pulmonary edema :
Lung rockets?
Pipes
Abdominal Aorta
Aneurysm:
Abd. Aorta > 3cm
Throracic aorta
aneurysm /
dissection:
a)Aortic root >
3.8cm?
b) Intimal Flap?
c)Thoracic aorta >
5cm?
1)Femoral vein DVT?
Non compressible vessel?
2) Popliteal vein DVT?
Non compressible vessel?
POCUS in Trauma
The use of diagnostic ultrasound in the abdominal and thoracic trauma started in Europe and
spread to North America in the 1990s [19].It is primarily used to detect intraperitoneal
hemorrhage, hemothorax , pneumothorax and the pericardial tamponade . This sonographic
assessment is called FAST (extended focused assessment with sonography for trauma)
[20] .FAST inclludes six-view trauma exam consisting of one view of each hemi-
thorax ,subcostal space ,the hepatorenal space (Morrison's pouch), perisplenic space, and the
pelvis. Although abdominal ultrasound is unable to isolate the source of bleeding, but the
diagnostic information provided by FAST in a hemodynamically unstable patient can
expedite the exploratory laparotomy in trauma patients [21—24].
POCUS in Cardiac Arrest
There is insufficient evidence to support routine use of POCUS in the resuscitation of the
cardiac arrest [25.] Pocus has proved to be more of diagnostic and prognostic tool In this
context.It is particularly helpful to reveal the anatomic causes of the pulseless electrical
activity (PEA) such as cardiac tamponade, tension pneumothorax and pulmonary
embolism.The reversible causes of PEA can be detected by the presence of new tricuspid
regurgitation, pericardial effusion, increased right ventricular strain, ,or the absence of lung
sliding, which guides the emergency physician to perform rapid tube thoracostomy,
pericardiocentesis, or thrombolysis.
Evidence that the use of ultrasound by clinicians improves outcomes:
Although all the recent limited studies in this context do not show any significant evidence
that the use of Focus ultrasound has improved outcomes and shorten hospital stay, but it has
proved to be a more accurate diagnostic tool to give the correct cause of shock.A research
study (Jon Gitz Holler, Camilla Nørgaard Bech, Daniel Pilsgaard Henriksen) was published
in the Pone Journal in March 2015 [26]. In this systematic literature research study up to
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
August 2013,
Six eligible observational studies were analysed from 11,880 identified papers. It was found
that there is inadequate data about the nontraumatic hypotensive patients presented in
prehospital or ED settings.In these available studies, nontraumatic hypotension was
suggested in 2% of EMS contacts and 1–2% reported with shock. The in hospital mortality of
shock is 33–52%. ED prevalence of hypotension is 4–13/1000 contacts with an inhospital
mortality of 12%.
Substantial heterogeneity was found in these studies and meta-analysis was not possible.
An international randomized controlled trial (Paul R.Atiknson , James Milne), published in
june 2018 , in the American annal of emergency medicine, showed no important benefit of
focus ultrasound.This multicenter study ,conducted in six centers of North America and
South Africa, included 270 hypotensive patients with a systolic B.P . < 100 mm Hg or a
shock index > 1.The measured primary outcome was the hospital discharge or survival to 30
days.The focused ultrasound group of 104 out of 136 patients , showed no difference in the
primary outcome over standard group of 102 out of 134 patients.
Jones et al. did a randomized trial on 184 patients in the emergency department.it is
considered to be the first study to prove that early focused ultrasound can be used by the
emergency physicians to diagnose the correct type of shock [3] .In this study, the etiology of
shock was correctly diagnosed in 80% of patients with early goal directed ultrasound at 0
minute, compared to 50% of patients in the standard care group (ultrasound not done), in the
initial 15 minutes of arrival to the ED.
The role of the focused point of care ultrasound and focused cardiac ultrasound FoCUS to
give confirmed diagnosis in shock was further established in the subsequent trials conducted
in the emergency departments .A prospective study done by Volpicelli et al. on 108 ED
patients in undifferentiated shock concluded that the diagnosis made by the point-of-care
multiorgan ultrasonography significantly agreed with a final clinical diagnosis obtained by
retrospective chart review [27]. A very good concordance was found between the ultrasound
diagnosis and the final clinical diagnosis (k = 0.710). Similar findings were found in an other
study done by Ghane et al. in which 52 ED patients were assessed under RUSH protocol (k =
0.7) [28].The ultrasound sensitivity found for different types of shock in this study was :
Type of Shock Sensitivity
All types of shock 94.6—100%
Hypovolemic shock 100%
Obstructive shock 100%
Cardiogenic shock 91.7%
Distributive shock 70—75%
Mixed shock 70—75%
The same results were found in another study done by Ghane et al. on a group of 77 patients
[29].All these studies have a common limitation that either the emergency physicians, trained
in the point of care ultrasound or the radiologists have done all the assessments and so the
Six eligible observational studies were analysed from 11,880 identified papers. It was found
that there is inadequate data about the nontraumatic hypotensive patients presented in
prehospital or ED settings.In these available studies, nontraumatic hypotension was
suggested in 2% of EMS contacts and 1–2% reported with shock. The in hospital mortality of
shock is 33–52%. ED prevalence of hypotension is 4–13/1000 contacts with an inhospital
mortality of 12%.
Substantial heterogeneity was found in these studies and meta-analysis was not possible.
An international randomized controlled trial (Paul R.Atiknson , James Milne), published in
june 2018 , in the American annal of emergency medicine, showed no important benefit of
focus ultrasound.This multicenter study ,conducted in six centers of North America and
South Africa, included 270 hypotensive patients with a systolic B.P . < 100 mm Hg or a
shock index > 1.The measured primary outcome was the hospital discharge or survival to 30
days.The focused ultrasound group of 104 out of 136 patients , showed no difference in the
primary outcome over standard group of 102 out of 134 patients.
Jones et al. did a randomized trial on 184 patients in the emergency department.it is
considered to be the first study to prove that early focused ultrasound can be used by the
emergency physicians to diagnose the correct type of shock [3] .In this study, the etiology of
shock was correctly diagnosed in 80% of patients with early goal directed ultrasound at 0
minute, compared to 50% of patients in the standard care group (ultrasound not done), in the
initial 15 minutes of arrival to the ED.
The role of the focused point of care ultrasound and focused cardiac ultrasound FoCUS to
give confirmed diagnosis in shock was further established in the subsequent trials conducted
in the emergency departments .A prospective study done by Volpicelli et al. on 108 ED
patients in undifferentiated shock concluded that the diagnosis made by the point-of-care
multiorgan ultrasonography significantly agreed with a final clinical diagnosis obtained by
retrospective chart review [27]. A very good concordance was found between the ultrasound
diagnosis and the final clinical diagnosis (k = 0.710). Similar findings were found in an other
study done by Ghane et al. in which 52 ED patients were assessed under RUSH protocol (k =
0.7) [28].The ultrasound sensitivity found for different types of shock in this study was :
Type of Shock Sensitivity
All types of shock 94.6—100%
Hypovolemic shock 100%
Obstructive shock 100%
Cardiogenic shock 91.7%
Distributive shock 70—75%
Mixed shock 70—75%
The same results were found in another study done by Ghane et al. on a group of 77 patients
[29].All these studies have a common limitation that either the emergency physicians, trained
in the point of care ultrasound or the radiologists have done all the assessments and so the
same results may not be expected from other non trained clinicians .
FoCUS ultrasound in shock, plays a major rule in the treatment after diagnosing the
underlying etiology and can improve the clinical outcome in the patients. Another
observational study was conducted on the use of FoCUS by hand-held ultrasound device in a
group of 220 patients in the intensive care unit. This group found to have lower fluid
prescription (49 vs 66 mL/kg, p = 0.01) and more dobutamine use (22 vs 12 %, p = 0.01) than
the historical control group [30]. The group of patients managed with FoCUS in this study
also showed a better 28-days survival (66 vs 56 %, p = 0.04) and a reduction in acute kidney
injury (20 vs 39 %) . Significant number of patients (14 %) with significant valvular
pathologies ,use of historical control and no randomization were the limitations of this study.
Another study done on the validation of FATE protocol provided positive echo images in
227 out of 233 patients (97%). New information was revealed in 37% of these echo’s and
were decisive in 24% [31].
Trauma is the commonest cause of death in the first four decades of life and a higher risk of
complications and death is noted in the poly trauma patients [32,33].
Point of care rapid ultrasound (RUSH) used in such types of traumatic shock and hypotension
significantly affects the trauma management and the patient outcomes.
A cross-sectional, prospective study carried out in Suez Canal University Hospital included
100 unstable admitted polytrauma patients . Pan-computed tomography (pan-CT) and RUSH
exam. were conducted. The CT results were taken as the standard. Patients were followed
up for a short outcome of 28 days [34].The results of RUSH exam in this study showed that
RUSH was 94.2% sensitive in the diagnosis of unstable polytrauma patients with an accuracy
of 95.2% in the shock patients. The most diagnostic causes of unstability found by RASH
exam in this study are, hypovolemic shock (64%), obstructive shock (14%), distributive
shock (12%) and cardiogenic shock (10%) respectively.
.
Conclusion
PoCUS has brought a useful improvement in the management of the critically ill patients. In
the past 10 years ,it has emerged as an important allies of the intensivists and the emergency
physicians to provide real-time valuable information to differentiate between different types
of shock and to engage the relevant consultants early on in workup, improving the initial
diagnostic accuracy and the proper management. Current evidence supports the role of
PoCUS in undifferentiated shock to narrow the possible differential diagnoses, and guide
specific management. More high-quality clinical studies are needed to further evaluate the
impact of PoCUS on the financial implications, clinical outcomes, and the patient survival in
future.
FoCUS ultrasound in shock, plays a major rule in the treatment after diagnosing the
underlying etiology and can improve the clinical outcome in the patients. Another
observational study was conducted on the use of FoCUS by hand-held ultrasound device in a
group of 220 patients in the intensive care unit. This group found to have lower fluid
prescription (49 vs 66 mL/kg, p = 0.01) and more dobutamine use (22 vs 12 %, p = 0.01) than
the historical control group [30]. The group of patients managed with FoCUS in this study
also showed a better 28-days survival (66 vs 56 %, p = 0.04) and a reduction in acute kidney
injury (20 vs 39 %) . Significant number of patients (14 %) with significant valvular
pathologies ,use of historical control and no randomization were the limitations of this study.
Another study done on the validation of FATE protocol provided positive echo images in
227 out of 233 patients (97%). New information was revealed in 37% of these echo’s and
were decisive in 24% [31].
Trauma is the commonest cause of death in the first four decades of life and a higher risk of
complications and death is noted in the poly trauma patients [32,33].
Point of care rapid ultrasound (RUSH) used in such types of traumatic shock and hypotension
significantly affects the trauma management and the patient outcomes.
A cross-sectional, prospective study carried out in Suez Canal University Hospital included
100 unstable admitted polytrauma patients . Pan-computed tomography (pan-CT) and RUSH
exam. were conducted. The CT results were taken as the standard. Patients were followed
up for a short outcome of 28 days [34].The results of RUSH exam in this study showed that
RUSH was 94.2% sensitive in the diagnosis of unstable polytrauma patients with an accuracy
of 95.2% in the shock patients. The most diagnostic causes of unstability found by RASH
exam in this study are, hypovolemic shock (64%), obstructive shock (14%), distributive
shock (12%) and cardiogenic shock (10%) respectively.
.
Conclusion
PoCUS has brought a useful improvement in the management of the critically ill patients. In
the past 10 years ,it has emerged as an important allies of the intensivists and the emergency
physicians to provide real-time valuable information to differentiate between different types
of shock and to engage the relevant consultants early on in workup, improving the initial
diagnostic accuracy and the proper management. Current evidence supports the role of
PoCUS in undifferentiated shock to narrow the possible differential diagnoses, and guide
specific management. More high-quality clinical studies are needed to further evaluate the
impact of PoCUS on the financial implications, clinical outcomes, and the patient survival in
future.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
References
1.Vincent JL, De Backer D. Circulatory shock. N Engl J Med. 2013;369:1726–34.
2..Singer M, Deutschman CS, Seymour C, et al. The Third International Consensus
definitions for sepsis and septic shock (sepsis-3). JAMA. 2016;315(8):801–10.
3. Randomized, controlled trial of immediate versus delayed goal-directed ultrasound to
identify the cause of nontraumatic hypotension in emergency department patients.
Alan E. Jones, MD; Vivek S. Tayal, MD; D. Matthew Sullivan, MD; Jeffrey A. Kline, MD,
A. CCM 2004. 32 (8): 1703.
4 Jones AE, Stiell IG, Nesbitt LP, et al: Non- traumatic out-of-hospital hypotension predicts
inhospital mortality. Ann Emerg Med 2004; 43:106–113
5. Moore CL, Rose GA, Tayal VS, et al: Determination of left ventricular function by
emergency physician echocardiography of hypotensive patients. Acad Emerg Med 2002;
9:186 –193
Atkinson, P.R.T., McAuley, D.J., Kendall, R.J., Abeyakoon, O., Reid, C.G., Connolly, J. and
Lewis, D. (2009). Abdominal and Cardiac Evaluation with Sonography in Shock (ACES): an
approach by emergency physicians for the use of ultrasound in patients with undifferentiated
hypotension. Emergency Medicine Journal, 26(2), pp.87-91.
6. Lee KL, Woodlief LH, Topol EJ, et al: Predic- tors of 30-day mortality in the era of reper-
fusion for acute myocardial infarction. Re- sults from an international trial of 41,021 patients.
GUSTO-I Investigators. Circulation 1995; 91:1659–1668
7. Goldhaber SZ, Visani L, De Rosa M: Acute pulmonary embolism: clinical outcomes in the
International Cooperative Pulmonary Embolism Registry (ICOPER). Lancet 1999; 353:1386
–1389
8. Mandal AK, Sanusi M: Penetrating chest wounds: 24 years experience. World J Surg
2001; 25:1145–1149
9. Ka Leung Mok. Journal of intensive care 2016.
10. Lynn et al., 1942
11. Stewart et al., 2004
12.Seif D, Perera P, Mailhot T, et al. Bedside ultrasound in resuscitation and the rapid
ultrasound in shock protocol. Crit Care Res Pract. 2012;2012:503254. https://doi.org/
10.1155/2012/503254.
13.E. Rivers, B. Nguyen, S. Havstad et al., “Early goal-directed therapy in the treatment of
severe sepsis and septic shock,” The New England Journal of Medicine, vol. 345, no. 19, pp.
1368– 1377, 2001.
14. F. Sebat, A. A. Musthafa, D. Johnson et al., “Effect of a rapid response system for
patients in shock on time to treatment and mortality during 5 years,” Critical Care Medicine,
vol. 35, no. 11, pp. 2568–2575, 2007. ]. Incorporation of bedside ultrasound in patients with
undifferentiated shock allows for rapid evaluation of reversible causes of shock and improves
accurate diagnosis in undifferentiated hypotension [A. E. Jones, V. S. Tayal, D. M. Sullivan,
and J. A. Kline, “Randomized, controlled trial of immediate versus delayed goal-directed
ultrasound to identify the cause of nontraumatic hypotension in emergency department
patients,” Critical Care Medicine, vol. 32, no. 8, pp. 1703–1708, 2004. ].
15. P. R. T. Atkinson, D. J. McAuley, R. J. Kendall et al., “Abdominal and Cardiac
Evaluation with Sonography in Shock (ACES): an approach by emergency physicians for the
use of ultrasound
16. S. D. Weingart, D. Duque, and B. Nelson, Rapid Ultra- sound for Shock and Hypotension
(RUSH-HIMAPP), 2009, http://emedhome.com/.
17. P. Perera, T. Mailhot, D. Riley, and D. Mandavia, “The RUSH exam: rapid ultrasound in
1.Vincent JL, De Backer D. Circulatory shock. N Engl J Med. 2013;369:1726–34.
2..Singer M, Deutschman CS, Seymour C, et al. The Third International Consensus
definitions for sepsis and septic shock (sepsis-3). JAMA. 2016;315(8):801–10.
3. Randomized, controlled trial of immediate versus delayed goal-directed ultrasound to
identify the cause of nontraumatic hypotension in emergency department patients.
Alan E. Jones, MD; Vivek S. Tayal, MD; D. Matthew Sullivan, MD; Jeffrey A. Kline, MD,
A. CCM 2004. 32 (8): 1703.
4 Jones AE, Stiell IG, Nesbitt LP, et al: Non- traumatic out-of-hospital hypotension predicts
inhospital mortality. Ann Emerg Med 2004; 43:106–113
5. Moore CL, Rose GA, Tayal VS, et al: Determination of left ventricular function by
emergency physician echocardiography of hypotensive patients. Acad Emerg Med 2002;
9:186 –193
Atkinson, P.R.T., McAuley, D.J., Kendall, R.J., Abeyakoon, O., Reid, C.G., Connolly, J. and
Lewis, D. (2009). Abdominal and Cardiac Evaluation with Sonography in Shock (ACES): an
approach by emergency physicians for the use of ultrasound in patients with undifferentiated
hypotension. Emergency Medicine Journal, 26(2), pp.87-91.
6. Lee KL, Woodlief LH, Topol EJ, et al: Predic- tors of 30-day mortality in the era of reper-
fusion for acute myocardial infarction. Re- sults from an international trial of 41,021 patients.
GUSTO-I Investigators. Circulation 1995; 91:1659–1668
7. Goldhaber SZ, Visani L, De Rosa M: Acute pulmonary embolism: clinical outcomes in the
International Cooperative Pulmonary Embolism Registry (ICOPER). Lancet 1999; 353:1386
–1389
8. Mandal AK, Sanusi M: Penetrating chest wounds: 24 years experience. World J Surg
2001; 25:1145–1149
9. Ka Leung Mok. Journal of intensive care 2016.
10. Lynn et al., 1942
11. Stewart et al., 2004
12.Seif D, Perera P, Mailhot T, et al. Bedside ultrasound in resuscitation and the rapid
ultrasound in shock protocol. Crit Care Res Pract. 2012;2012:503254. https://doi.org/
10.1155/2012/503254.
13.E. Rivers, B. Nguyen, S. Havstad et al., “Early goal-directed therapy in the treatment of
severe sepsis and septic shock,” The New England Journal of Medicine, vol. 345, no. 19, pp.
1368– 1377, 2001.
14. F. Sebat, A. A. Musthafa, D. Johnson et al., “Effect of a rapid response system for
patients in shock on time to treatment and mortality during 5 years,” Critical Care Medicine,
vol. 35, no. 11, pp. 2568–2575, 2007. ]. Incorporation of bedside ultrasound in patients with
undifferentiated shock allows for rapid evaluation of reversible causes of shock and improves
accurate diagnosis in undifferentiated hypotension [A. E. Jones, V. S. Tayal, D. M. Sullivan,
and J. A. Kline, “Randomized, controlled trial of immediate versus delayed goal-directed
ultrasound to identify the cause of nontraumatic hypotension in emergency department
patients,” Critical Care Medicine, vol. 32, no. 8, pp. 1703–1708, 2004. ].
15. P. R. T. Atkinson, D. J. McAuley, R. J. Kendall et al., “Abdominal and Cardiac
Evaluation with Sonography in Shock (ACES): an approach by emergency physicians for the
use of ultrasound
16. S. D. Weingart, D. Duque, and B. Nelson, Rapid Ultra- sound for Shock and Hypotension
(RUSH-HIMAPP), 2009, http://emedhome.com/.
17. P. Perera, T. Mailhot, D. Riley, and D. Mandavia, “The RUSH exam: rapid ultrasound in
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
SHock in the evaluation of the critically lll,” Emergency Medicine Clinics of North America,
vol. 28, no. 1, pp. 29–56, 2010.
18.Seif D, Perera P, Mailhot T, et al. Bedside ultrasound in resuscitation and the rapid
ultrasound in shock protocol. Crit Care Res Pract. 2012;2012:503254. https://doi.org/
10.1155/2012/503254.
19. Nordenholz KE, Rubin MA, Gularte GG, Liang HK. Ultrasound in the evaluation and
management of blunt abdominal trauma. Ann Emerg Med 1997;29:357-66
20. Melanson SW, Heller M. The emerging role of bedside ultrasonography in trauma
care. Emerg Med Clin North Am 1998;16:165-89
21.American Institute of Ultrasound in Medicine; American College of Emergency
Physicians. AIUM practice guideline for the performance of the focused assessment with
sonography for trauma (FAST) examination. J Ultrasound Med 2014;33:2047-56.
22. Körner M, Krötz MM, Degenhart C, Pfeifer KJ, Reiser MF, Linsenmaier U. Current Role
of Emergency US in Patients with Major Trauma. Radiographics 2008;28:225-42.
23. Montoya J, Stawicki SP, Evans DC, et al. From FAST to E-FAST: an overview of the
evolution of ultrasound-based traumatic injury assessment. Eur J Trauma Emerg
Surg2016;42:119-26.
24. Kirkpatrick AW, Sirois M, Laupland KB, et al. Hand-held thoracic sonography for
detecting post-traumatic pneumothoraces: the Extended Focused Assessment with
Sonography for Trauma (EFAST). J Trauma 2004;57:288-95.
25.Morrison LJ, Deakin CD, Morley PT, et al. Part 8: Advanced life support: 2010
International Consensus on Cardiopulmonary Resuscitation and Emergency
Cardiovascular Care Science With Treatment
Recommendations. Circulation2010;122:S345-421
26.PLOS ONE | DOI:10.1371/journal.pone.0119331 March 19, 2015
27.Volpicelli G, Lamorte A, Tullio M, Cardinale L, Giraudo M, et al. Point-of-care
multiorgan ultrasonography for the evaluation of undifferentiated hypotension in the
emergency department. Intensive Care Med. 2013;39(7):1290–8. doi:10.1007/
s00134-013-2919-7.
28.Ghane MR, Gharib M, Ebrahimi A, Saeedi M, Akbari-Kamrani M, et al. Accuracy of
early rapid ultrasound in shock (RUSH) examination performed by emergency
physician for diagnosis of shock etiology in critically ill patients. J Emerg Trauma
Shock.2015;8(1):5–10. doi:10.4103/0974-2700.145406.
29.Ghane MR, Gharib MH, Ebrahimi A, Samimi K, Rezaee M, et al. Accuracy of rapid
ultrasound in shock (rush) exam for diagnosis of shock in critically ill patients.
Trauma Monthly. 2015;20(1):e20095. doi:10.5812/traumamon.20095. ]
.30..Kanji HD, McCallum J, Sirounis D, MacRedmond R, Moss R, et al. Limited
echocardiography-guided therapy in subacute shock is associated with changes in
vol. 28, no. 1, pp. 29–56, 2010.
18.Seif D, Perera P, Mailhot T, et al. Bedside ultrasound in resuscitation and the rapid
ultrasound in shock protocol. Crit Care Res Pract. 2012;2012:503254. https://doi.org/
10.1155/2012/503254.
19. Nordenholz KE, Rubin MA, Gularte GG, Liang HK. Ultrasound in the evaluation and
management of blunt abdominal trauma. Ann Emerg Med 1997;29:357-66
20. Melanson SW, Heller M. The emerging role of bedside ultrasonography in trauma
care. Emerg Med Clin North Am 1998;16:165-89
21.American Institute of Ultrasound in Medicine; American College of Emergency
Physicians. AIUM practice guideline for the performance of the focused assessment with
sonography for trauma (FAST) examination. J Ultrasound Med 2014;33:2047-56.
22. Körner M, Krötz MM, Degenhart C, Pfeifer KJ, Reiser MF, Linsenmaier U. Current Role
of Emergency US in Patients with Major Trauma. Radiographics 2008;28:225-42.
23. Montoya J, Stawicki SP, Evans DC, et al. From FAST to E-FAST: an overview of the
evolution of ultrasound-based traumatic injury assessment. Eur J Trauma Emerg
Surg2016;42:119-26.
24. Kirkpatrick AW, Sirois M, Laupland KB, et al. Hand-held thoracic sonography for
detecting post-traumatic pneumothoraces: the Extended Focused Assessment with
Sonography for Trauma (EFAST). J Trauma 2004;57:288-95.
25.Morrison LJ, Deakin CD, Morley PT, et al. Part 8: Advanced life support: 2010
International Consensus on Cardiopulmonary Resuscitation and Emergency
Cardiovascular Care Science With Treatment
Recommendations. Circulation2010;122:S345-421
26.PLOS ONE | DOI:10.1371/journal.pone.0119331 March 19, 2015
27.Volpicelli G, Lamorte A, Tullio M, Cardinale L, Giraudo M, et al. Point-of-care
multiorgan ultrasonography for the evaluation of undifferentiated hypotension in the
emergency department. Intensive Care Med. 2013;39(7):1290–8. doi:10.1007/
s00134-013-2919-7.
28.Ghane MR, Gharib M, Ebrahimi A, Saeedi M, Akbari-Kamrani M, et al. Accuracy of
early rapid ultrasound in shock (RUSH) examination performed by emergency
physician for diagnosis of shock etiology in critically ill patients. J Emerg Trauma
Shock.2015;8(1):5–10. doi:10.4103/0974-2700.145406.
29.Ghane MR, Gharib MH, Ebrahimi A, Samimi K, Rezaee M, et al. Accuracy of rapid
ultrasound in shock (rush) exam for diagnosis of shock in critically ill patients.
Trauma Monthly. 2015;20(1):e20095. doi:10.5812/traumamon.20095. ]
.30..Kanji HD, McCallum J, Sirounis D, MacRedmond R, Moss R, et al. Limited
echocardiography-guided therapy in subacute shock is associated with changes in
management and improved outcome. J Crit Care. 2014;29(5): 700–5. doi:10.1016/
j.jcrc 2014.04.008.
31.Transthoracic echocardiography for cardiopulmonary monitoring in intensive care. M.B.
Jensen , E. Sloth, K.M. Larsen , M.B. Schmidt. European Journal of Anaesthesiology
2004; 21:700–707
32.Aldemir M, Taçyildiz I, Girgin S. Predicting factors for mortality in the pene- trating
abdominal trauma. Acta Chir Belg. 2004;104:429e434.
33.Butcher N, Balogh ZJ. The definition of polytrauma: the need for international consensus.
Injury. 2009;40:S12eS22. https://doi.org/10.1016/j.injury.2009.10. 032
34.Adel Hamed Elbaih a, *, Ahmed Mohamed Housseini b, Mohamed E.M. Khalifa . https://
doi.org/10.1016/j.cjtee.2017.06.009 . 1008-1275/© 2018 Daping Hospital and the
Research Institute of Surgery of the Third Military Medical University. Production
and hosting by Elsevier B.V. This is an open access article under the CC BY-NC-ND
license (http://creativecommons.org/licenses/by-nc-nd/4.0/
j.jcrc 2014.04.008.
31.Transthoracic echocardiography for cardiopulmonary monitoring in intensive care. M.B.
Jensen , E. Sloth, K.M. Larsen , M.B. Schmidt. European Journal of Anaesthesiology
2004; 21:700–707
32.Aldemir M, Taçyildiz I, Girgin S. Predicting factors for mortality in the pene- trating
abdominal trauma. Acta Chir Belg. 2004;104:429e434.
33.Butcher N, Balogh ZJ. The definition of polytrauma: the need for international consensus.
Injury. 2009;40:S12eS22. https://doi.org/10.1016/j.injury.2009.10. 032
34.Adel Hamed Elbaih a, *, Ahmed Mohamed Housseini b, Mohamed E.M. Khalifa . https://
doi.org/10.1016/j.cjtee.2017.06.009 . 1008-1275/© 2018 Daping Hospital and the
Research Institute of Surgery of the Third Military Medical University. Production
and hosting by Elsevier B.V. This is an open access article under the CC BY-NC-ND
license (http://creativecommons.org/licenses/by-nc-nd/4.0/
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.
