Providing Guidance for Noise Control and Prevention in UK Hospitals
VerifiedAdded on 2022/10/18

PROVIDING GUIDANCE FOR CONTROLLING AND PREVENTION OF NOISE IN UK
HOSPITALS
Student’s Name
Tutor’s Name
University
City, State
Paraphrase This Document
Abstract
The noise control and prevention in UK hospitals research was an approach that aimed at
minimizing the sound levels of noise in UK hospitals. Especially in ICUs. This research was
coined out due to the presence of other studies identifying and recognizing the effect on the well-
being and quality of occupants (visitors, staff and patients). This act tried to help hospitalized
individuals. In this study, the method and design of the study as well as the collection of data all
worked based on the hypothesis that noise can be prevented and reduced through several
architectural designs and regulations. A literature review of related study results is also
documented to give guiding research that could be used in changing the hospital occupants’
behaviours and working practices. Data obtained from the noise level monitoring devices are
then used in coming up with an analyzed solution to UK hospital noise prevention and reduction
Keywords: Decibels, Speech Privacy, Intensive Care Unit, Absorption, Reverberation
Declaration
I the undersigned do hereby make a solemn declaration that this dissertation project,
PROVIDING GUIDANCE FOR CONTROLLING AND PREVENTION OF NOISE IN UK
HOSPITALS, is drawn from the basis of my own work accomplished in my pursuit of the
<COURSE OF STUDY> under Mr/Mrs. ……………………….. supervision. I give an
assertion that the conclusion and statements noted down came from my own research work.
Student’s name …………………………………
Student’s signature …………………………….
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Table of Contents
Abstract.......................................................................................................................................................2
Declaration..................................................................................................................................................3
Acknowledgements.....................................................................................................................................8
1. Introduction.........................................................................................................................................9
2. Research hypothesis, Research questions, Significance of the research.............................................10
2.1. Research Hypothesis..................................................................................................................10
2.2. Research Questions....................................................................................................................10
2.3. Aims and Objectives..................................................................................................................10
2.4. Significance of Research............................................................................................................11
3. Literature Review..................................................................................................................................11
3.1. Theoretical Framework...................................................................................................................11
3.2. Effects of noise in hospitals............................................................................................................12
3.2.1. Noise on patients......................................................................................................................12
3.2.2. Noise on staff...........................................................................................................................13
3.3. Sources of noise in hospitals...........................................................................................................13
3.4. Controlling and preventing noise in hospitals.................................................................................14
3.4.1. Construction methods that absorb noise in hospitals................................................................14
3.4.2. Single-bed patient rooms as a way of reducing noise in hospitals............................................15
3.4.3. Reducing or eliminating noise sources.....................................................................................16
3.4.4. Music.......................................................................................................................................17
Paraphrase This Document
4. Methods.................................................................................................................................................17
4.1. Qualitative Research.......................................................................................................................17
5. Results...................................................................................................................................................19
6. Discussion.............................................................................................................................................26
7. Analyzed Solutions................................................................................................................................32
8. My perspective in regards to the issue of noise in hospitals...................................................................36
9. Conclusion.............................................................................................................................................43
10. Bibliography........................................................................................................................................46
11. References...........................................................................................................................................56
12. Appendix.............................................................................................................................................65
12.1. Questionnaires..............................................................................................................................65
Table of Tables
Table 1- Showing ICU details.......................................................................................................19
Table 2- Showing levels of sound averaged through 24-hour readings in dB...............................20
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Table of Figures
Figure 1 shows the average levels of sound for patients’ sited recording device..........................21
Figure 2 -shows the averaged levels of sound for recording devices sited centrally....................22
Figure 3 displays the peak levels of sound for recording devices sited adjacent to patients........23
Figure 4 shows the average number peak value numbers in every hour for monitoring devices
situated next to patients.................................................................................................................24
Figure 5 displays the 24-hour plot of frequency at John Radcliffe Hospital.................................25
Paraphrase This Document
Acknowledgements
I give thanks to my supervisors who have been the source of guidance throughout the
conductance of the research in that this dissertation has been successful due to
Mr…………………………… guidance.
Guide’s name ……………………………..
Supervisor’s signature …………………………….
1. Introduction
In the UK, it is observed that 30% of the personnel treated in hospitals come out of the ICUs
developing delirium or become confused1. When such instances occur, the patients will have
higher morbidity and mortality as well as increased hospital stays. Certain risk factors, therefore,
come up from the developed delirium due to ICU environment that includes the use of sedation
other than invasive procedures. These effects also have a relation with the sleep disturbing noise
coming from the environment in hospitals (Kawai, et al., 2019).
There exists a wide variation in different noise aggravation tendency and sensitivity, however, a
healthy adult has a tolerance to an A-weighted level of sound in decibels ranging between 50-55
dBA in the day while at night, 40 – 45 dBA. These noise levels would not be considered
disturbing to sleep or health2. On the other hand, in time-average levels of sound, sleep
disturbances due to quantifiable effects in low noise signals as 30 dBA to high levels of noise
such as 45 dBA.
The guidelines from the World Health Organisation consist of hospital noise levels with a
suggestion that the patients have it difficult in coping with high levels of stress coming from
environmental noise. The organization recommends not an excess of 35 dBA in areas where
patients get observed or treated with a maximum possible noise level of 40 dBA (Basner &
McGuire, 2018).
Hence, this paper comes into perfume research that assesses the levels of sound in the UK
hospital Cs comparing the observations to the WHO set standards3. Additionally, the research
recommends some preventive and control measures for similar kinds of noise.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
2. Research hypothesis, Research questions, Significance of the research
2.1. Research Hypothesis
This paper looks to work through the hypothesis based on the significance that the use of better
design factors, standard regulations and noise cancellation techniques can reduce the noise level
in UK hospitals.
2.2. Research Questions
With the use of the following research questions, the research becomes guided and structured
into accomplishing its targets:
1. Are there different noise prevention and control measures in hospitals?
2. Are there different materials possible for absorbing the noise in UK hospitals?
3. Are there different methods of construction that could help in hospital noise reduction?
2.3. Aims and Objectives
The paper aims to research on providing control and guidance measures in preventing UK
hospital noise. Hence, there exist various objectives set for achieving the research's aim. These
objectives include:
1. Identifying the different preventive and control measures relating to UK hospital noise4.
2. Determining the noise effects in hospitals
3. Determination of practices as well as measures able to be set in place for improving the
UK hospital environment.
4. Identifying the various sources of noise in hospitals.
Paraphrase This Document
2.4. Significance of Research
Increased level of noise, as well as the stress induced by noise, harms the staffs' and patients'
wellbeing and performance5. Therefore, depicting a poor caring ability of hospitals leading to
burnouts. Additionally, the high level of noise has been heavily identified to raise the unrest of
patients, reduce their recovery rate and healing (Zhang, et al., 2019). There is an increased rate of
hospitalization due to induced stress. This research will, therefore, become of great importance in
the improvement of staff, patient and visitor wellbeing within the UK hospitals6.
3. Literature Review
3.1. Theoretical Framework
Through the use of numerous literature bodies, the research gets to spell the big pervasive
problem existing in UK hospitals as well as the whole world, hospital noise. There are guideline
values from the World Health Organizations regarding the noise in the hospital background in
the rooms of patients to range between 35 dBA to 30 dBA in the day and at night respectively.
On the other hand, the wards would only reach a peak of 40 dBA7. The noise levels in hospitals
are reported as per the various literature researches to help determine the trend. Also, the studies
are to help in producing a comparison and determining the compliant hospitals with regards to
the WHO guidelines (Darbyshire & Young, 2013).
Also, the levels of noise in hospitals should be identified whether it is very high or has been
rising8. The noise levels are to be identified whether they are a day or night hours peak noise.
The decibel unit is used in quantifying the intensity of sound pressure or the loudness in
logarithmic scales. The decibels unit will, therefore, classify the intensity of noise and be used in
identifying the sources of noise in hospital equipment comparing them to various machines to
depict the intensity (Montague, et al., 2009). For example, 90 dBA can be compared to a passing
bus on a highway. This is to develop and expose the surprising very high level of noise in UK
hospitals together with their serous effects to the patients, staff and visitors. With this exposed,
acoustic designs can then be identified to counter the sound effects in hospitals. Thereby,
preventing and controlling the noise9.
3.2. Effects of noise in hospitals
3.2.1. Noise on patients
Numerous research have been done looking at how patients get influenced by the bad effects of
noise on patients as well as staff hospitals10. Other than being the annoyance source, hospitals
with loud noises are being linked to arousals and sleep disturbances in several patients. Looking
at the studies conducted by Grossman, et al. (2017), adult patients as well as infants are noted to
be affected by noise describing that they noise awakens and disrupts sleep in patients. On the
other hand, the care routines being used in hospitals is also being described as noise due to their
sleep-disturbing effects11. These factors are to be considered when tackling noise due to their
negative effects on sleep.
The quiet time has been noted to be very critical in ICU environments in that the oxygen
saturation content is seen to reduce in higher noise levels as seen in (Nunez, et al., 2016). Hence,
there are required oxygen support therapies in such environments. Also, the high level of noise
raises the pressure of blood, respiration rate together with the rate of the heart as well as
worsened sleep. In another study by Ahmed (2016), there exists evidence that very high noise
levels negatively affect wound healing in that patient exposed to high noise levels stayed in
hospitals once through with the surgery. Also, Carayon (2016) discovered that in very high noise
levels exceeding 60 dBA required the use of more medications in surgery patients for recovery.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3.2.2. Noise on staff
For the hospital staff, noise is a source of stress in that it intervenes with the staff ability to
accurately perform their work. Looking at room acoustics in hospitals, Chow and Shellhaas
(2016) found out that there were less demand in work in better acoustic hospitals as well as
reduced strain and pressure compared to noisy hospitals. Brown et al. (2015) noted that stress
from noisy environments directly related to burnout and emotional exhaustion within care
nurses. The high levels of noise are being perceived by healthcare staff there is an interference
other than impacting the comfort as well recovery12.
Looking into the performance of healthcare staff as per the effects of noise levels, there exist
conflicting results as seen in (Pope & Miller-Klein, 2016). Studies from the laboratory identify
that the non-healthcare groups are not impaired on their task performing abilities due to noise
levels when there is increased pressure or effort in maintaining hospital standards (Stans, et al.,
2017). The study, however, shows that the added noise levels in hospitals come as a result of
increased performance ability in catering to their patients13. Hence, there exists possible
healthcare staff ability to keep up the performance in hospitals within noisy environments rather
than less noisy environments that would reduce service rate. Though, the intense service rate can
lead to fatigue due to greater effort.
3.3. Sources of noise in hospitals
There exist two main explanations that verify the noisy environments in UK hospitals. To begin
with, Tobías, et al (2015) states that UK hospitals have numerous sources of noise and second,
the environment in which the hospitals are situated and its design- floors, walls and ceilings- that
is reflective as opposed to absorbing14. The noise in hospitals is seen to come from the use of
mechanical equipment- paging systems, alarms, ice machines, telephone and staff conversations
Paraphrase This Document
as well as roommates and visitors. It is observed that staff conversations are the major source of
noises in hospital units.
Various hospitals have been seen to use sound absorbing materials in their structures. Kol et al
(2015) Identify this technique as one source of increased noise levels in that much sound is
absorbed which prevents sound build-up. The characterization of acoustics conditions makes up
long reverberation time, blending as well as overlapping of sound due to echoing leading into
decreased speech eligibility. Therefore, staff members, to make themselves heard, have to
increase their voice hence compounding the level of noise even more.
3.4. Controlling and preventing noise in hospitals
Various literature suggests that the intervention in the hospital environment can be effective in
the reduction of hospital noise as well as improving the acoustics. Hence, the important
interventions make up the installation of high-performing sound absorbent ceiling tiles, reduction
of noise sources or elimination (Holland & Jenkins, 2019). These methods of noise level
reduction in hospitals can be prevented and controlled using the following methods15;
3.4.1. Construction methods that absorb noise in hospitals
Various studies are show that the installation of sound-absorbing ceiling panels and tiles are
highly effective in reducing levels of noise and noise perceptions, which impacts the outcomes of
the improved eligibility in speech and reduction in work pressure in staff as seen in (Harris,
2016). The use thick and heavy walls with large voids enhance the sound-absorption properties
of the walls enabling them to allow very little or no noise transmission16. The walls must also
extend to the ceiling to avoid spaces that can noise transmit noise to the adjacent rooms. There
should be no holes, spaces and cracks existing in the walls must be filled at the time of building
hospitals to prevent leakage of noise from one area to another. The use of acoustic blankets that
act as barrier walls in preventing noise from travelling from one place to another (Goeren, et al.,
2018). This is some of the construction techniques that should be considered while building
hospitals to regulate noise pollution17.
3.4.2. Single-bed patient rooms as a way of reducing noise in hospitals
This strategy was seen to the most effective means of reducing noise by Real et al (2017) in
patient rooms. Multi-bed room studies were performed in this source regarding acute-care as
well as ICU noting the degree of noise stems from various patients talking with different care
providers, a combination of operating equipment, patient sounds like crying out and coughing
and visitors as identified by (Williams & Gardiner, 2015). The study identified that in situations
involving seven-bed hospital rooms, the intensity of noise levels grew given that the rooms will
be crowded with more equipment, visitors and care providers. Certain hospitals would then be
forced to banish open bay rooms due to the very high noise levels18.
3.4.2.1. Patient confidentiality and speech privacy
Numerous outpatient physicians' office and hospitals incur their patients to situations involving
their conversations overheard by other patients (Grossman, et al., 2017). Worse, the private
information is being communicated in an open environment which means the information can be
heard by others and themselves altogether19. In speech privacy, the level by which the private
conversations can be overheard by the close by listeners is being determined by speech indices.
These are known as a private index (Taylor & Markides, 2014).
It is clear from Rashid, et al (2019) that architectural designs can be the source of addressing the
obvious fails in healthcare settings with regards to the preservation of confidentiality. For
example, the source identifies the provision of single-patient rooms with enclosed walls during
examinations as well as during treatment, times requiring patients to disclose confidential health
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
information. Eijkholt, et al (2017) identifies the satisfaction of patients with the appreciation of
single-bed rooms in comparison to the roommate situations. This is due to the higher privacy in
single rooms. About 2,122,439 patients showed appreciation20.
There exists a lot of gaps in hospital settings where confidential information or conversations are
exchanged and in most cases conveniently overheard by other listeners. Among the typical
examples of challenges posed by the layout and design of the unit in making sure that there is
patient privacy in hospital settings are as follows (Kreis, et al., 2013):
The physical closeness between the visitors who are in the admission places and staff
with the reception places that have been designed inappropriately to the extent that
telephone discussions and conversations could be overheard.
Insufficient confidential discussion areas in public places including reception areas,
admission stations as well as waiting places in which confidential discussions may be
held.
Insufficient confidential discussion areas on patients’ departments for physicians and
nurses to hold meetings with patients’ families.
3.4.3. Reducing or eliminating noise sources
Numerous studies are identifying overhead systems in paging, loud staff and equipment as the
major sources of noise in the UK hospitals as stated by (Applebaum, et al., 2016). Also, there
exist recommendations to the prevention and control of noise levels that mostly includes the
replacement of overhead paging with wireless devices or cellphones by the staff, removal of loud
sound noises like the ice machine and turning off medical equipment not being used. Moreover,
group conversations can be done in an enclosed space with an education of staff on the benefits
of quiet talking or maintenance of a quiet environment21.
Paraphrase This Document
3.4.4. Music
Through the use of complex and organized sound composed with the aim of soothing, music,
such as combinations of pitch, rhythm, melody and harmony, can help in reducing noise effect in
patients, staff and visitors. Research done by Eggert et al (2015) shows the ability of specific
music types inducing positive responses and relaxation, hence a reduced heart rate, anxiety, or
increased temperature. Besides, music is being used in therapy in the promotion of well-being
and health with regards to different settings22. Music can be used in maternity, intensive care,
pediatric and coronary care. These types of music should, however, be considerate to the patient
preference since not every patient would be in preference to the playing music as the age, peer
group and culture factor will come to play. In general, sedative music has been seen to be
suitable as an intervention in reducing noise (Montague, et al., 2009).
4. Methods
4.1. Qualitative Research
The research involved undertaking a study for two weeks. Night-time and daytime levels of
sound were being noted down during the week as well as the weekend days in 5 hospital ICUs in
England within Thames Valley region. These hospitals include John Radcliffe Hospital, John
Radcliffe Neurosciences ICU; Royal Berkshire Hospital; Churchill General Hospital and
Wycombe General Hospital. The units selected above were picked due to the heterogeneity and
proximity since they replicate various physical layouts of wards, building designs and patient
population23. The research was not to involve the recruitment of patients or using any sort of
identifiable data. The nation's local ethics policies are stating that research that involves fully
anonymised information that the team cannot trace back to the individual sources is not a
constitution of studies that involve the participation of humans (Citerio, et al., 2019). Hence, this
research would not be subjected to ethical review. The general physician in all the units had to
provide written authorization for the level of sounds for measuring, also, the members of staff
who were present during the research had to be made aware. The research also involved asking
the general physicians questionnaires seen in the appendix and their answers were used in
producing the analysis and my own perspective.
The collection of sound levels was achieved using with the use of CEL-630 monitoring devices
that had an integral fitted recording connected to a CEL-495 pre-amplification as well as a CEL-
251 microphone24. In every ICU, the used monitors were running concurrently for the 24 hours
for all the recording periods. One monitoring device was situated centrally in the room or next to
a central station while the other monitoring device was located next to the head of the patient. In
any possible location, patients who were seen centrally located in the unit sections were selected
for the study. The calibration of the devices as done using acoustic calibrators CEL-120/1 with a
setting for 24-hour recording. In all the minutes, the peak level of the noise was recorded (LApeak)
as well as the average level of sound (LAeq) from the 60 seconds, preceding. The 0 dB reference
level was the human hearing limit at the 1 KHz frequency (Gerth, et al., 2019).
Sample recordings involving short duration were not left out in the unoccupied ICU side rooms
regarding John Radcliffe ICU Hospital in that the monitors, as well as the alarm devices, were
sequentially being activated25. This entailed the common alarming signals together with the
ambient noise that occurred only during times the room's equipment had been powered down.
The data that had been monitored was then downloaded into custom software, Casella
measurement, and taken into Microsoft Excel and Corp for more analysis (Vollam, et al., 2018).
The produced graphs were developed using the SigmaPlot software together with Microsoft
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Excel. LAeq and time data taken from every unit were added with a display in average LAeq in that
the limits were confidently displayed with a +/-1.96 SEM.
5. Results
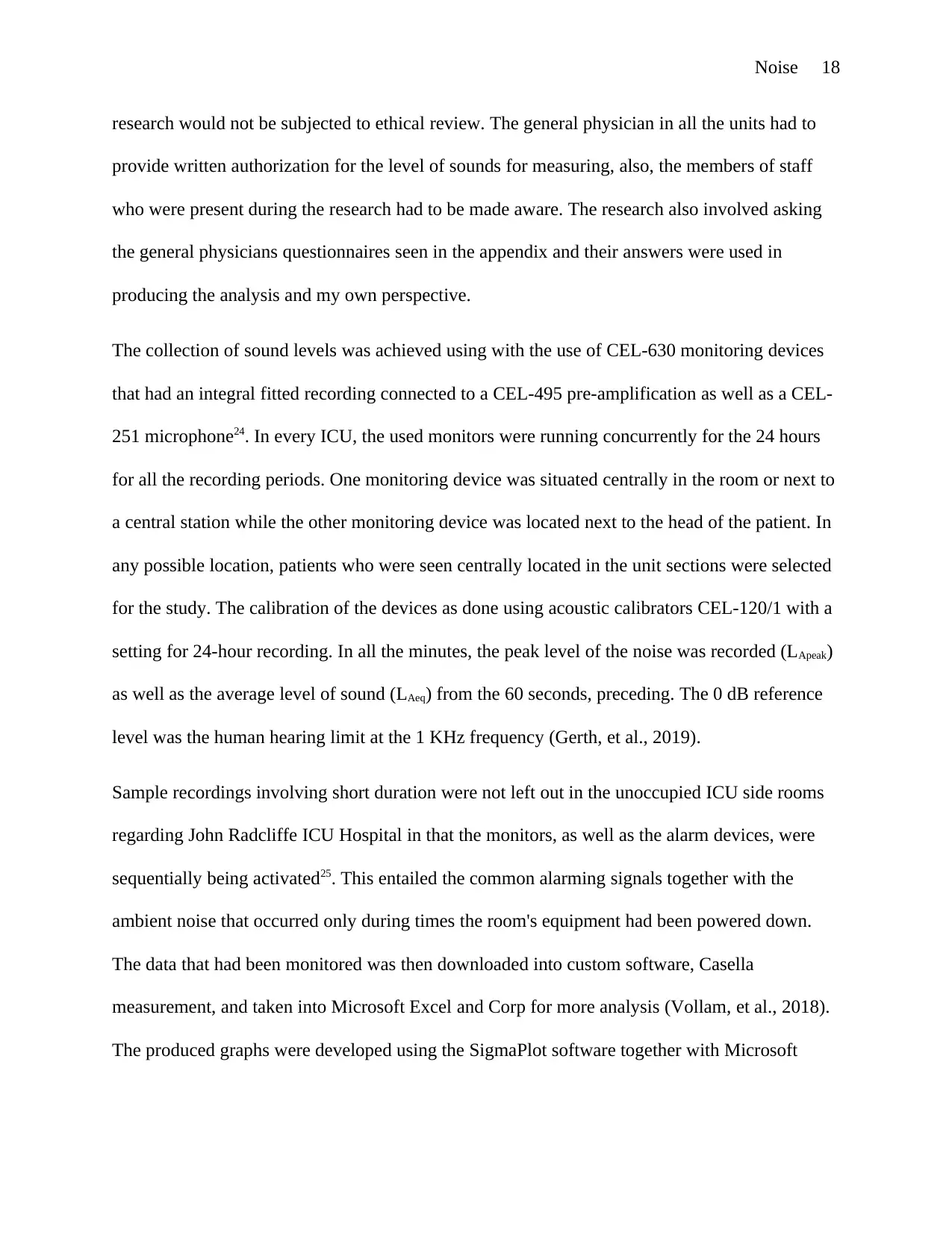
Table 1 below is a display of detailed results gotten from ICUs within the research duration. John
Radcliffe ICU hospital is known to admit adult patients with tertiary or secondary referrals while
Neurosciences ICU takes in patients having neurosurgical or neurological problems or patients
with neck or head injuries requiring surgery. Churchill Hospital is an ICU station that lacks an
emergency department and focuses on taking in patients looking for elective surgery together
with offering specialized surgical and medical wards. The Wycombe General Hospital and Royal
Berkshire are the two chosen big district ICU hospitals.
Details Churchill
Hospital
John
Radcliffe
Hospital
Wycombe
General
Hospital
John
Radcliffe
Neurosciences
Hospital
Royal
Berkshire
Hospital
Nursing
Handovers
7:30 in the
morning
together with
7:30 at the
night
7:30 in the
morning
together with
7:30 at night
8:00 and 1:00
in the
afternoon
and 7:30 in
the morning
7:30 in the
morning
together with
7:30 at night
7:00 in the
afternoon
and 7:30 in
the morning
Number of
Beds
6 beds and 2
side rooms
12 beds
together
within 3 bays
and 4 side
rooms
7 beds
together with
2 side rooms
12 beds 9 beds and 2
side rooms
Visiting
Times
Not restricted Not restricted Restricting
between 1:00
P.M and 3:00
P.M
Not restricted Restricting
between 3:00
P.M and 4:30
P.M
Medical
Handovers
8:30 in the
morning
together at
8:30 at night
8:30 in the
morning
together at
8:30 at night
Between
8:00 in the
morning and
8:00 at night
8:30 A.M
together at
8:30 P.M
8:00 at night
and 8:00 in
the morning
Paraphrase This Document
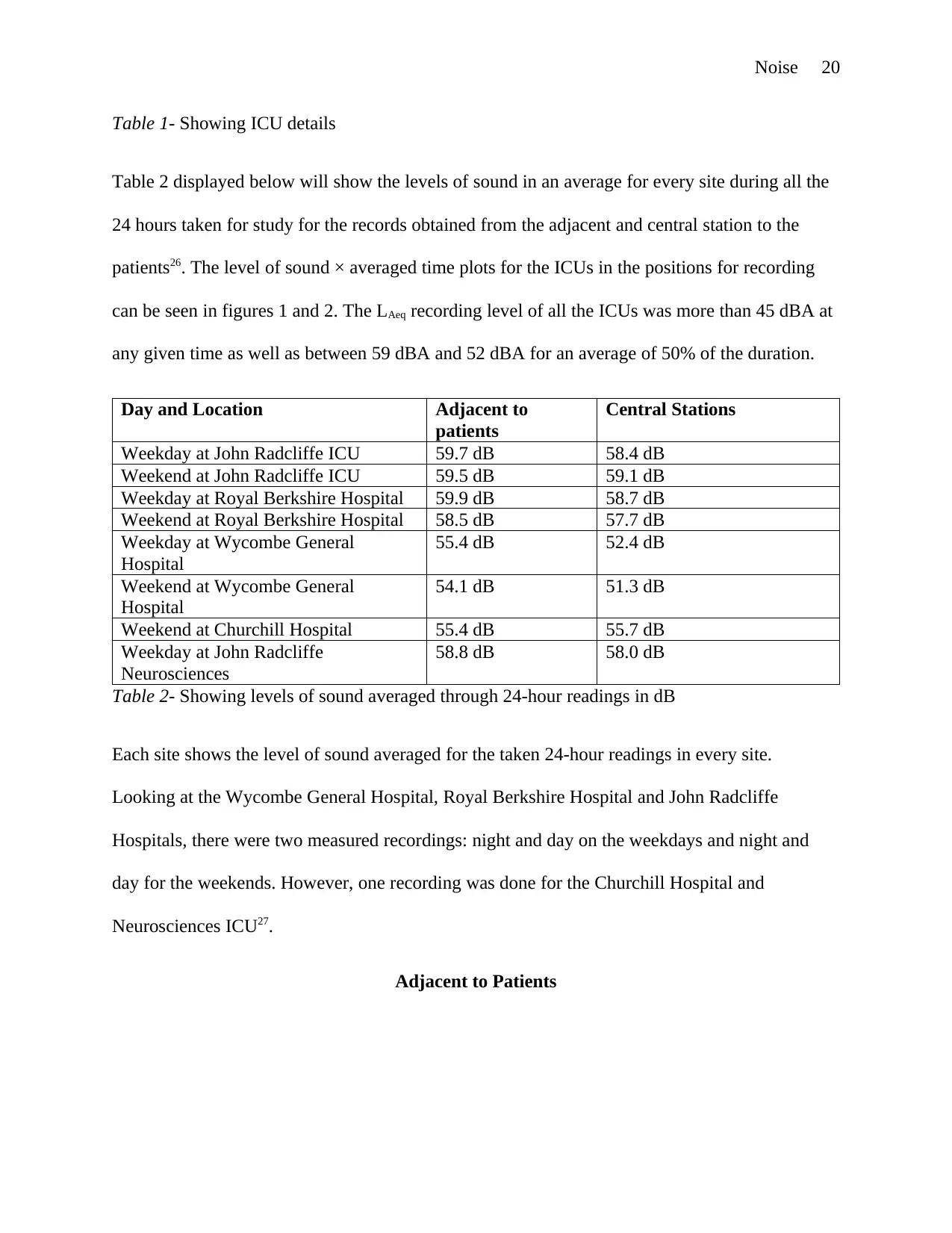
Table 1- Showing ICU details
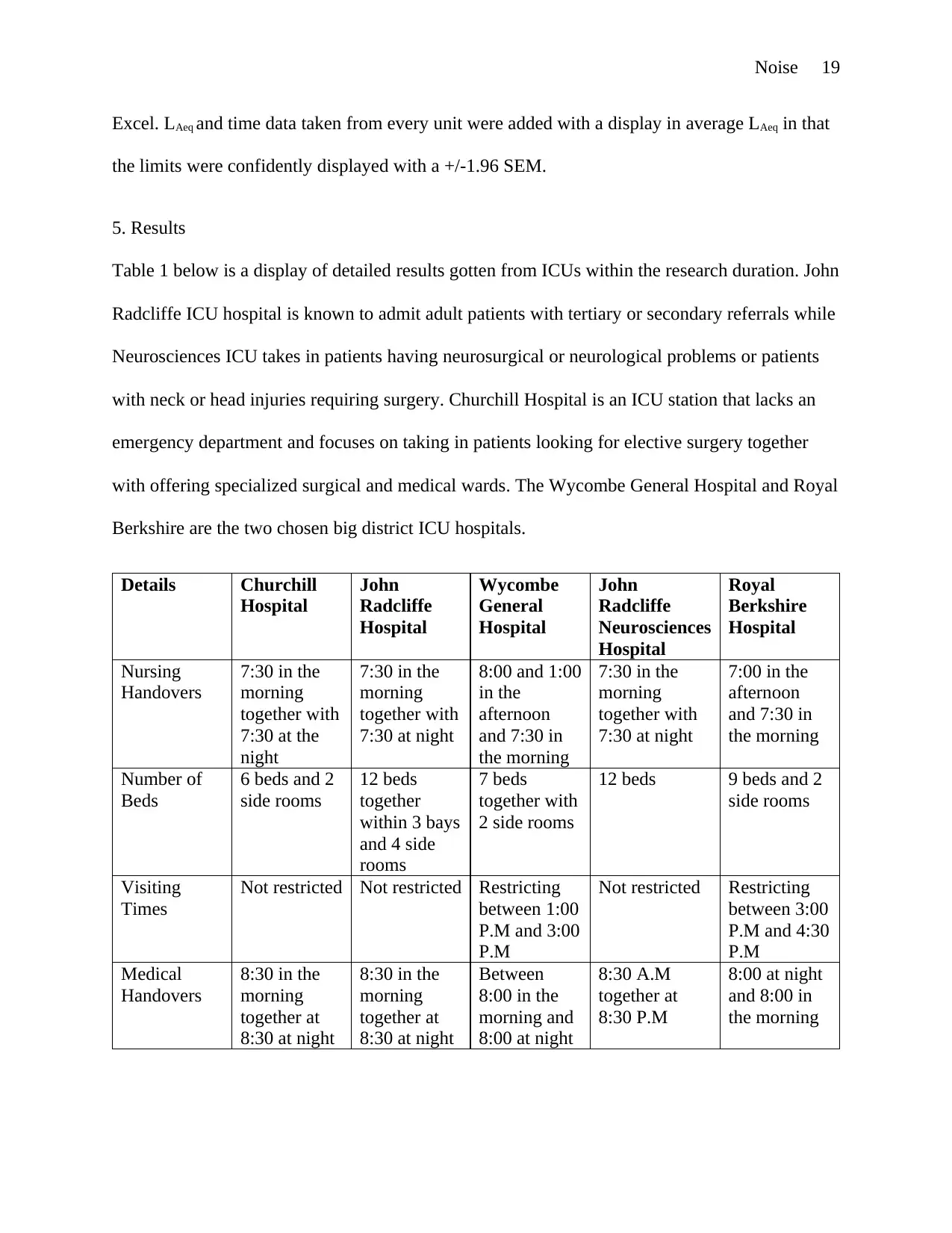
Table 2 displayed below will show the levels of sound in an average for every site during all the
24 hours taken for study for the records obtained from the adjacent and central station to the
patients26. The level of sound × averaged time plots for the ICUs in the positions for recording
can be seen in figures 1 and 2. The LAeq recording level of all the ICUs was more than 45 dBA at
any given time as well as between 59 dBA and 52 dBA for an average of 50% of the duration.
Day and Location Adjacent to
patients
Central Stations
Weekday at John Radcliffe ICU 59.7 dB 58.4 dB
Weekend at John Radcliffe ICU 59.5 dB 59.1 dB
Weekday at Royal Berkshire Hospital 59.9 dB 58.7 dB
Weekend at Royal Berkshire Hospital 58.5 dB 57.7 dB
Weekday at Wycombe General
Hospital
55.4 dB 52.4 dB
Weekend at Wycombe General
Hospital
54.1 dB 51.3 dB
Weekend at Churchill Hospital 55.4 dB 55.7 dB
Weekday at John Radcliffe
Neurosciences
58.8 dB 58.0 dB
Table 2- Showing levels of sound averaged through 24-hour readings in dB
Each site shows the level of sound averaged for the taken 24-hour readings in every site.
Looking at the Wycombe General Hospital, Royal Berkshire Hospital and John Radcliffe
Hospitals, there were two measured recordings: night and day on the weekdays and night and
day for the weekends. However, one recording was done for the Churchill Hospital and
Neurosciences ICU27.
Adjacent to Patients
Figure 1 shows the average levels of sound for patients’ sited instrument for recording.
The level of sound is then averaged at intervals of a minute (LAeq) recorded through the day using
the instruments situated next to the patients (Plummer, et al., 2019).
Central Position
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
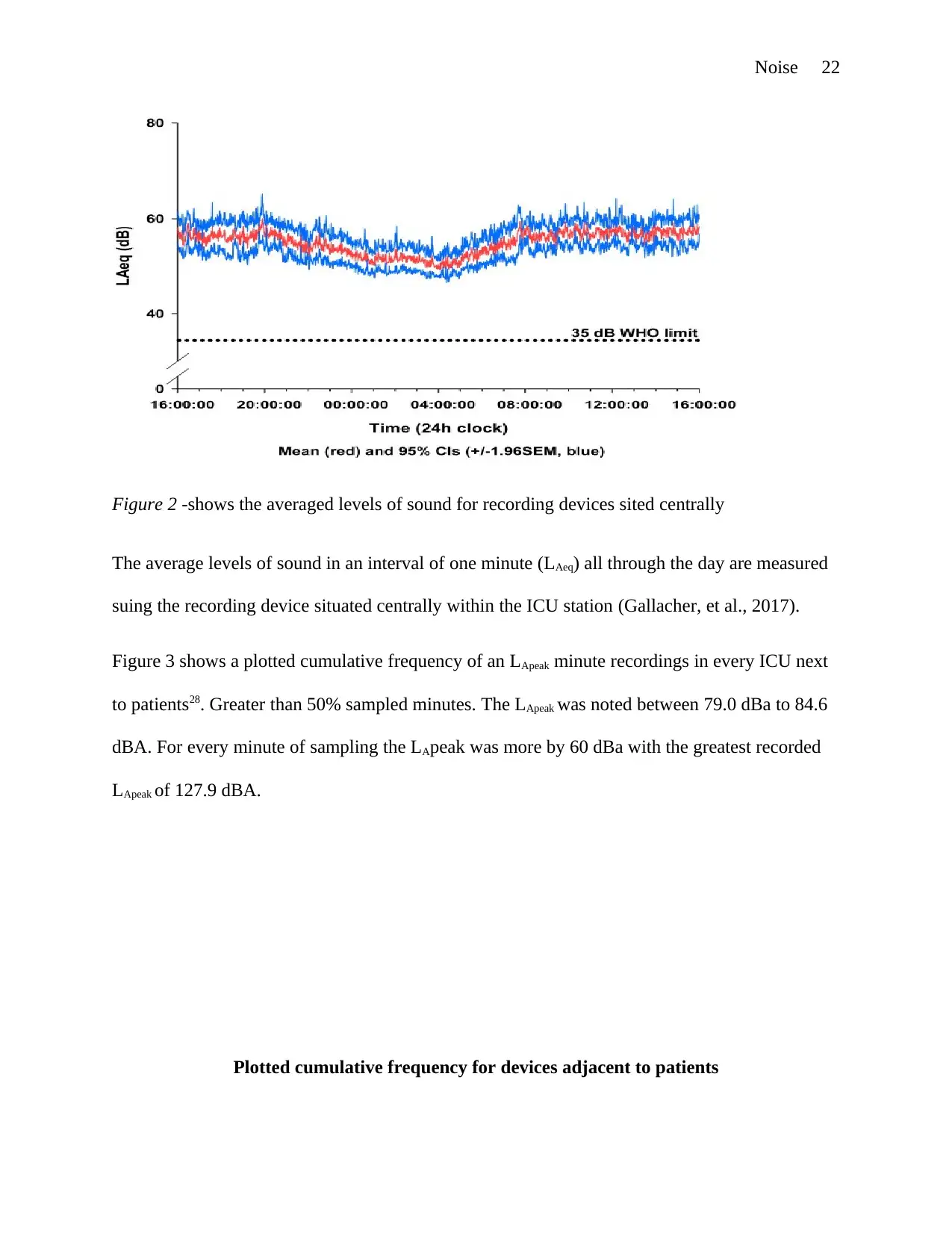
Figure 2 -shows the averaged levels of sound for recording devices sited centrally
The average levels of sound in an interval of one minute (LAeq) all through the day are measured
suing the recording device situated centrally within the ICU station (Gallacher, et al., 2017).
Figure 3 shows a plotted cumulative frequency of an LApeak minute recordings in every ICU next
to patients28. Greater than 50% sampled minutes. The LApeak was noted between 79.0 dBa to 84.6
dBA. For every minute of sampling the LApeak was more by 60 dBa with the greatest recorded
LApeak of 127.9 dBA.
Plotted cumulative frequency for devices adjacent to patients
Paraphrase This Document
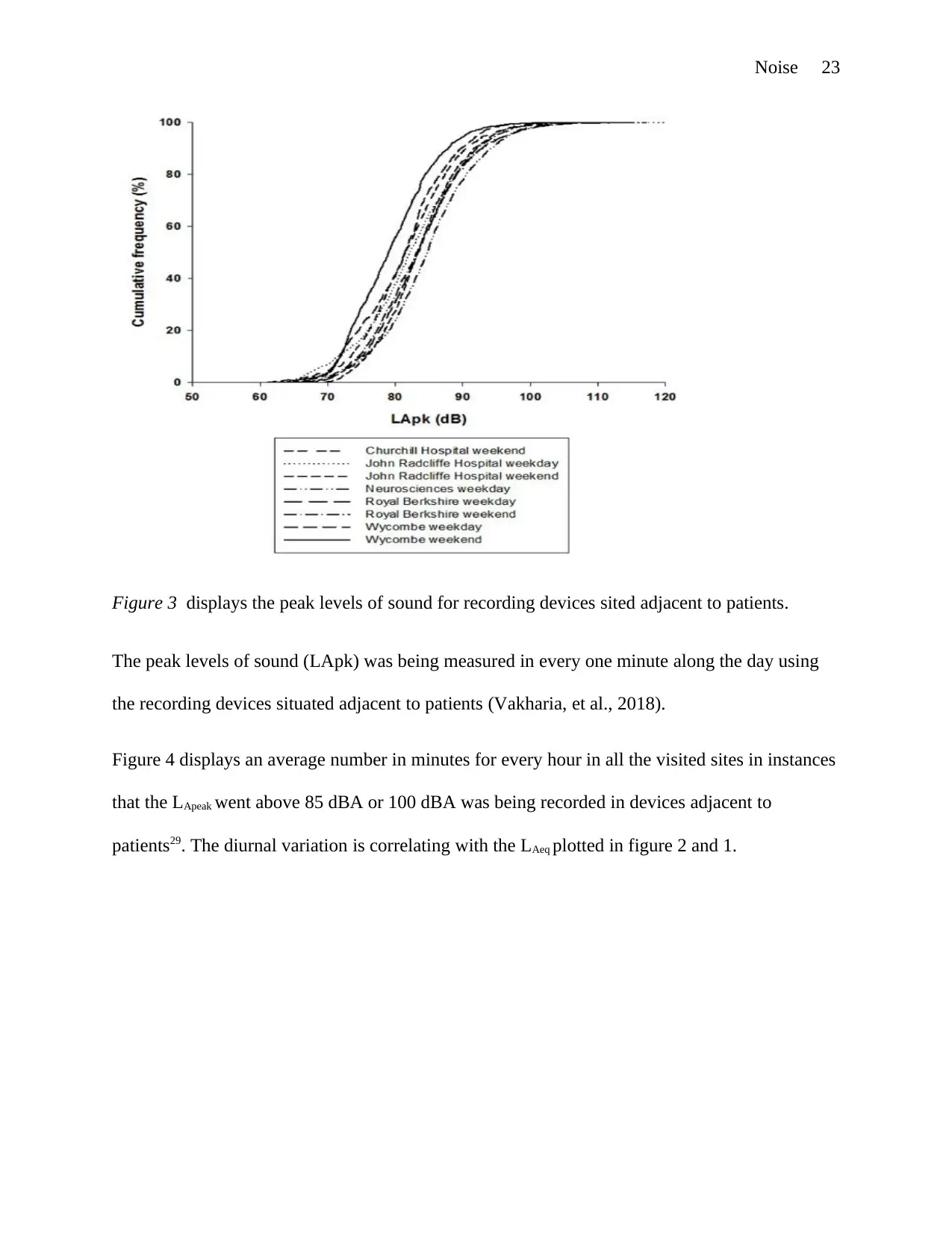
Figure 3 displays the peak levels of sound for recording devices sited adjacent to patients.
The peak levels of sound (LApk) was being measured in every one minute along the day using
the recording devices situated adjacent to patients (Vakharia, et al., 2018).
Figure 4 displays an average number in minutes for every hour in all the visited sites in instances
that the LApeak went above 85 dBA or 100 dBA was being recorded in devices adjacent to
patients29. The diurnal variation is correlating with the LAeq plotted in figure 2 and 1.
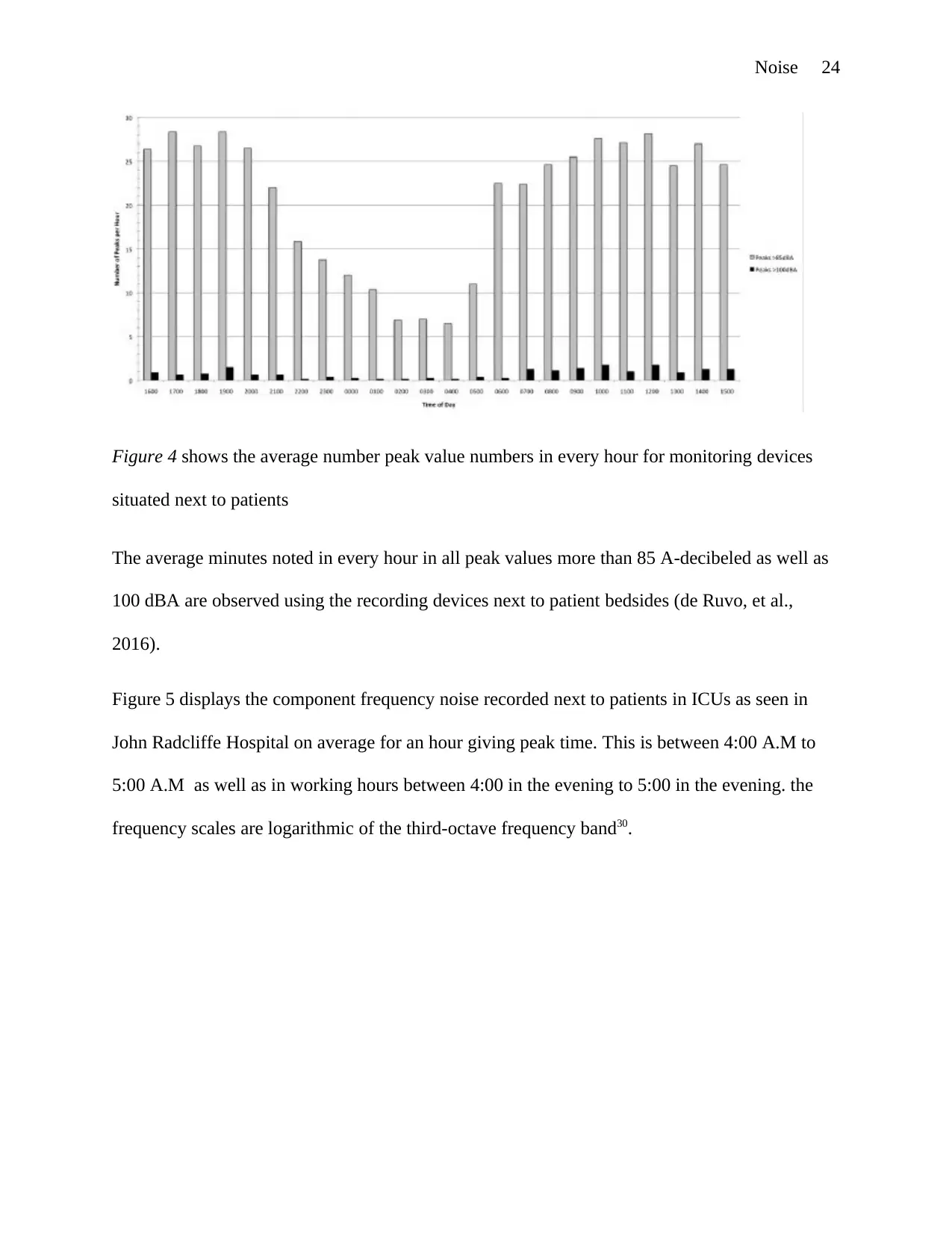
Figure 4 shows the average number peak value numbers in every hour for monitoring devices
situated next to patients
The average minutes noted in every hour in all peak values more than 85 A-decibeled as well as
100 dBA are observed using the recording devices next to patient bedsides (de Ruvo, et al.,
2016).
Figure 5 displays the component frequency noise recorded next to patients in ICUs as seen in
John Radcliffe Hospital on average for an hour giving peak time. This is between 4:00 A.M to
5:00 A.M as well as in working hours between 4:00 in the evening to 5:00 in the evening. the
frequency scales are logarithmic of the third-octave frequency band30.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
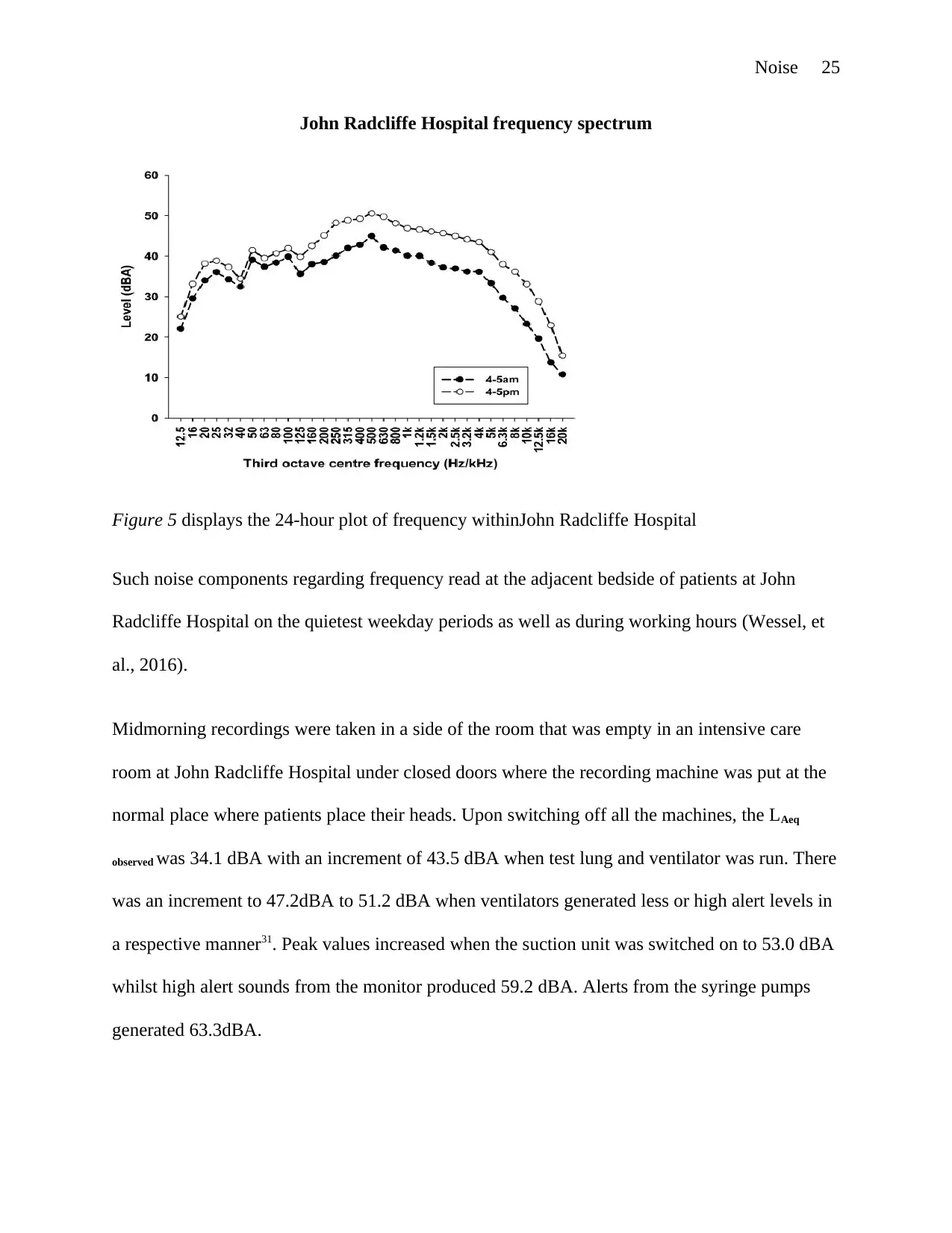
John Radcliffe Hospital frequency spectrum
Figure 5 displays the 24-hour plot of frequency withinJohn Radcliffe Hospital
Such noise components regarding frequency read at the adjacent bedside of patients at John
Radcliffe Hospital on the quietest weekday periods as well as during working hours (Wessel, et
al., 2016).
Midmorning recordings were taken in a side of the room that was empty in an intensive care
room at John Radcliffe Hospital under closed doors where the recording machine was put at the
normal place where patients place their heads. Upon switching off all the machines, the LAeq
observed was 34.1 dBA with an increment of 43.5 dBA when test lung and ventilator was run. There
was an increment to 47.2dBA to 51.2 dBA when ventilators generated less or high alert levels in
a respective manner31. Peak values increased when the suction unit was switched on to 53.0 dBA
whilst high alert sounds from the monitor produced 59.2 dBA. Alerts from the syringe pumps
generated 63.3dBA.
Paraphrase This Document
Several alarm sounds' frequency features were established by the use of one –third frequency
octave plots. Physiological monitors inside the bands revealed frequency peaks of 1.6 - 3.15 KHz
for the initial alarm levels while the second level had frequency peaks of 2.5 – 3.15 KHz which
are highly urgent alarms. Alarms form the infusion pumps in ranges of 880 Hz to 1 Hz produced
frequency peaks. Ventilator alarms had wide spread frequencies thus, could not be differentiated
easily from other noises (Müller-Trapet, et al., 2018).
6. Discussion
The logarithm scale used to measure noise is dB. Any normal human being has a hearing
threshold of 0 dBA, a convention conversation is around 55 dBA, a whisper or a quiet room is
around 30 dBA, at a distance of 10m heavy traffic is approximately 80 dBA, television produces
around 60 dBA and pneumatic drills generate around 100 dBA. Changes in noise at levels of 3-
dB are perceived as discernible, changes to 5-dB are also viewed as discernible while changes to
10-dB softer or louder are considered reduction by half or doubling volume respectively. To
obtain intelligible speech, it requires 15 dB to be louder than the background sound levels
(Stamper & Johnson, 2015). Therefore, the suggested average noise levels by WHO in hospital
wards is equal to a too quiet room consisting of transient peaks during nights to be as well than
the lower the conversation level.32
However, reports have indicated that there is no substantial decrease in activities over the night
within the Intensive care unit (WHO, 2009). The connection between poor results and the
deprivation of sleep has also been recently reported. Other reports have revealed that a routine
reduction in the activities over the night and the reduced lights at night have promoted natural
sleep patterns (Shah & Krishnan, 2019). The levels of noise may reduce to approximately 5 dB
during the early morning hours, unfortunately to the levels of uninterrupted conversations. The
initial and lapse of the night consist of high levels of noises during hand overtimes33. There are
about 25 minutes of each hour on the average scale at daytime at peak levels beyond 85dBA is
experienced. Peak levels beyond 85 dBA rarely happen during the nights, however, patients may
still anticipate distractions averagely once within 7–16 time in minutes each hour between 10 at
night and 7 in the morning. In most cases, such dB levels are most probably caused by alarm
activities, human voices and electronic noises which continuously distract patients who are
sleeping. Persistent and frequent arousals in hospital settings have revealed to have negative
impacts on patients and even healthy staff (Magdy, et al., 2019).
Generally, hospitals seem to get more noise with time. Studies have shown that for the past few
years a 15 dB increase has been experienced on an average scale which is greater than the
doubling level of the noise perceived (Darbyshire & Young, 2013). It is almost obvious that
noise levels in most hospital settings are very high compared to the recommended guidelines of
WHO (Richards & Stapleton, 2014). Patients are exposed to continual levels of noises which
may at best be lower than the conversation level but at daytime, it is equivalent to being closer to
a dishwasher or television. Rarely does the peak levels around patients go below 50 dBA34. Peaks
levels which are measured ( L Apeak) are usually at 60 dBA and worse levels are approximately
128 dBA. Previous research conducted in ICU setting has shown that average levels were
approximately 10dB increment in surgical ICU care with the same time profile (Simons, et al.,
2019). The levels were also identical to the observations obtained in a multiple- bed ICUs having
the distribution coompared with frequency peaks (Webb & Gattinoni, 2016).
Given the environmental and physical differences in the units selected the ultimate information
produced was similar. It might be possible that the patient’s single room may be noisier than the
multiple patient rooms for adults at John Radcliffe Hospital, however, this might not always be
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
the case. Units with the lower number of patients did not prove to be the quietest at the time the
recording took place (Freye, 2012). It, therefore, implies that sound levels simply has to do with
occupancy and acoustic aspects35. Peak values were about 51.3 to 59.1 dBA at the stations at the
centre and 51.1 – 59.9 around the patients unit. Noise levels closer to the heads of patients were
about and in most cases higher compared to the stations at the centre (Bliefnick, et al., 2019).
This may be as a result of equipment positioning. The equipment in most units is suspended
nearby patients' heads on every bedside by use of rails or pendant systems36. This is to allow
access to the patient from the backside of the bed. While this seems conventional and
convenient, it places the sources of noise very close to the beds of patients (Lou, et al., 2013).
In every studied unit, the positioning of the ventilators was at one side of the bed hence one side
of the head while monitors were put on the remaining side. Therefore, these two noise sources in
most cases were 50 cm or below from the ears of the patient and the same distance from the
devices used in the recording. Sounds produced by alarms and functioning equipment is viewed
to be considered as justified by the recorded levels when the alarms and equipment were
separately recorded (Shajahan, et al., 2019). Every unit entertained patients such as radio and
television and the possibility of their use led to much greater recorded values at the patient's
place. However, radio and television use was not recorded at the time of assessing37. Patient's
intervening activities were also not recorded even though, they might be factors increasing the
sound levels in the patients' rooms (Page & Wesley, 2015).
Frequency aspects recorded at daytime and during quietest times revealed a distinct pattern from
what was reported in adult ICU whereby noise levels were below 400 Hz. This might have been
caused by the impact of the weightings that were used. A-weighting was used because of its low
sensitivity to reduced frequencies to determine the perception of human which lowers the
Paraphrase This Document
frequency spectrum at all end levels. However, the previous outcome relied on unweighted
values38. The removal of A-weighting renders the results almost similar to the previous outcome
of ICU adult patients. Changes noted previously at the quietest times of the day as well as
reduced noise levels greatly than 400 Hz were also observed during the study. This might have
been as a result of very low sound frequencies due to the hospital plant and various stressors that
could not have shown diurnal variations39. On the other hand, the greater frequencies experience
a reduction during the nights when of alarm noises, conversations and other factors are present. It
is beneficial to redo such exercise when day and nights have distinct light durations so to come
up with diurnal seasonal comparable impacts (Zijlstra, et al., 2019).
Noise levels were recorded in comparative studies in a chemotherapy clinic for outpatient and
average, constant, similar 55 – 60 dB levels, peak levels of ˃90 dB per minute, and pressure
levels for sound at daytime. Concurrent questionnaires filled by staff, visitors and patients
showed that, while noise disrupted staffs resulting in communication difficulties, it was not a
concern for visitors or patients (Edwards & Sabato, 2009). Even though this reveals that levels
perceived in patients’ rooms could be acceptable, it led to researchers finding the relationship
between the amounts of the irritation experienced and time a person stayed at the clinic. The
levels established in this paper have possible impacts on both patients in critical conditions and
staff therefore, a lot must be done to ensure the noise levels are reduced in hospitals (Chow &
Shellhaas, 2016).
The alarms' spectra frequencies were recorded to differentiate noise generated by alarms from
the background sound. However, the alarms' acoustic signature was hard to be differentiated
from the wideband sounds from the background. Therefore, the measurements for non-alarm and
alarm sounds were not separately obtained consistently. The sounds, however, have been
previously obtained somewhere else and it is evident that a substantial amount of background
sounds is produced from modifiable behaviour (Fogel & Greenberg, 2015). These behaviours
include moving and operating equipment, conversations, allowing container lids and doors to
freely close and telephone usage40. Many studies have lowered the levels of LAeq in the adult ICU
for a shorter time through the introduction of unit-level changes in behaviour and sound
awareness initiative (Rechel, et al., 2009).
Other three studies that have been reported used continual polysomnography together with
measurements for environmental noise to find out whether sounds might be the cause for
inconsistent sleep patterns in critical patients (Johnson & Crumlett, 2017). The outcome revealed
that noise from the environment led to 17% awakenings and 11% arousals. Patients discharged
from critical conditions who were interviewed complained of distracted sleep caused by the said
noise, frequent interventions from nurses and light. Disruption of sleep for critically ill patients
also has to do with increased needs for depression and anxiety treatment. Volunteers who were
subjected to stimulated intensive care unit setting complained of biochemical stress makers and
disrupted sleep (Bae, et al., 2018 ). Other two studies assessed the health of patients with high
degree of sickness using the ICU scale of environmental stressors. The studies revealed that
patients pointed out alarm sounds to be factoring noise41. The challenge of noise coming from the
surrounding is not restricted to patients alone but also staff. Investigations not within hospital
settings have shown that noise has negative effects on good health, motivation and physiology
(Urbańska, et al., 2019).
Mechanical means to minimize the number of sounds perceived such as ear defenders and
earplugs that can lower noise perceived by 15-30 dB have demonstrated effectiveness. Recently,
136 random controlled patients investigation revealed a tremendous decrease in delirium and an
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
enhancement in sleep by use of mechanical measures. Earlier studies showed that acuity patients
experienced improved and quality sleep by wearing earplugs (Locihová, et al., 2018).
Discussions with ICU caregiver at the time collecting data showed that several patients perceived
monitor alert for a patient was not propionate to its urgency42. This resulted in prolonged high
sound levels whilst more urgent requirements were treated. The urgency mapping
inappropriateness can steadily cause correspondence decrease and desensitization of alarm
responses. Alarm fatigues have been reported in new studies as the major health hazard
experienced by hospitals around the world (Clerk & Patel, 2019). Visual relationship of alarm
sound and real-time data recorder screens were the probable sources of several peak
measurements. It is demonstrated that good management of alarms can lowers the alarm
frequency. Various hospitals have introduced staff programmes in which equipment modification
is encouraged to limit defaults in respect with the individual physiology of patients. This lowers
chances for alarm fatigues to be experienced. Moreover, the creation of smart alarms should be
encouraged. Reports show that in the intensive care unit, just 23% alarms are effective which
means that, the introduction of delay by 19 seconds may remove 67% of the ineffective and
ignored alarms (Vincent, et al., 2015).
The on-going studies to enhance the systems in which the deteriorating conditions of patients
may be detected (Münzel, et al., 2018). Even though this is not a widely spread technology, there
exist systems for managing alarms which can transmit loud alerts from the bedsides inpatient
rooms to the caregiver or a central control place. Therefore, there may exist technological
resolutions that can be applied together with awareness programmes to reduce noise levels above
the expected levels as a result of behavioural change only43. Sound levels can be attained
following guidelines of the World Health Organization only if patient rooms are closed and
Paraphrase This Document
every patients’ monitoring machines are shut down (Pinsky, et al., 2013). However, some
researchers have demonstrated that the possibility of reducing sound levels, even if it is for a
shorter period, but no hospital met the required guideline limits coming from WHO (WHO,
2009). Investigations in this article reveal that with the modern machines needed for patient care,
the standards coming from WHO cannot be achieved in most hospitals44.
7. Analyzed Solutions
Reflecting on Florence Nightingale, she would possibly be very emphatic if a story could be told
now of how unrealistic the auditory standards were in the mid-19th centuries. This is because the
21st-century era has institutional care systems that are very advanced. Nightingale may also
affirm that with all the available technology the effect on patients will never or has never
changed (Pope & Miller-Klein, 2016). Nightingale would still be relentless even with her lack of
forbearance for any environmental or noise stressors becoming harsh patient health improvement
(Tauber‐Gilmore, et al., 2018). Moreover, if Nightingale was still alive at the moment, she may
have straight forwardly asked about the rampant noise that has become normal in patient care
units whereas quiet has become an exception (Kitapci & Galbrun, 2019).
Therefore noise control and prevention in most hospitals must apply the themes outlined below:
Can healing be heard?
Assuming that it is undisputable that the physicians are highly skilled and the nurses are very
competent. That the company is effective and efficient with the most advanced and best
technology, as well as managers ratify funding for unique interior and architectural designs.
There remains a question of how the hospital sounds (NAP, 2010). An individual should ask
themselves whether the maximum standards are implemented in the sounds that reecho in every
corridors and room (Pfeiffer, 2018). They should as well consider the overheard and heard words
by frightened families and patients who are suffering45. Can the high standards be seen and
heard? Choosing to commit to offering the best care should guarantee every patient's facet
experience at optimal (NAP, 2011).
Research on noise impact on the intensive care unit revealed that patients were distracted and
disturbed greatly because of the noises from visitors, nurse stations and other irrelevant clinical
occurrences. Another research on nurses’ hindrances to offering excellent services showed that
noise was among the variety of environmental stressors46. The truth is that unnecessary noise is
damaging and causes irritation to patients in the ICU. It's immaterial whether the noise emanates
from technology or people, irrelevant hospital noise is no different to the needs of patients and
poises similar indifferences to the health workers. Noise leads to patient discomfort and
suffering others instead of relieving them (Parr Vijinski, et al., 2018).
Does the one-size fit any person? Naturally, hospitals as institutional are designed in a manner
that a particular size can fit all or any individual. Hence, the clinical behaviour of health care
institutions may feel impersonal or generic. Nevertheless, whilst health care facilities are mostly
perceived to be about technology, beds, windows, ceilings, floors and walls, it also has to do
with noise, clutter and people. Surveys about satisfying patients, the quality of services rendered
are measured in regards to the dynamic environment of the hospital. The changeable and
circumstantial factors brought about by people, vary the whole day and must be regulated by
health staffs (Grunden & Hagood, 2012).
Regardless of accidental, unavoidable or inadvertent, noise is among the critical invasive factor
of the environment at the hospital47. The trauma and suffering sounds from technologies and
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
machines overheard via the narrow walls, open doors and curtains, form part of the surroundings
in which families and patients encounter health care experiences in their way (Farrow, 2018).
Patients usually complain very much about noise compared to any other thing in health care
facilities, even food. Noise remains the top most complaints raised by patients (Kawai, et al.,
2019).
Acuity against Capacity
Where the acuity of patients is high, their capacity to adapt is usually very low, leading to severe
sensitivity to various types of environmental stressors48. Leave alone harmless, irregular sounds
that cause apprehension may lead to intensified pain medications, the requirement for restraints
and perennial calls for nursing help. The bad impacts of noise are brought about as a direct
result of subjection to noise or reacting towards noise for example dissatisfaction or annoyance.
Evidence shows that negative exposure to noise reactions predict the outcomes of health
precisely than the available prediction from being exposed to the noise itself (Bower, et al.,
2015).
The confidential and casual conversation among or between staffs, patients and visitors, together
with the sounds of beepers, slammed doors, paging, phones, buzzers and carts that require
maintenance form the sound environment. This is where compassion, stress, concern, caring and
competence are demonstrated qualitatively49. Thus, allowing the sound environment, or leaving it
randomly occur due to institutional care, puts the outcomes that aid in determining health care
quality at risk (Clapp, et al., 2018). Additionally, very high acuity levels lead to a decline in
cognition and perception accuracy. This explains the ineffectiveness assumption that patients
Paraphrase This Document
appreciate whatever they hear and why. It is proper for healthcare facilities to mitigate such
impacts by interpreting distracting or annoying sound to patients via adaptation.
Notwithstanding incidental or accidental noises, the collection of gossip, noise or unnecessary
distractions cause anxiety, leading to unsatisfying, unacceptable and health risk experiences.
Therefore, the auditory surroundings of hospitals must be improved especially at the bedside.
Organizational Culture
Noise is caused by people, thus it is a cultural forbearance50. The noise that distracts the
organization's critical purpose can only exist due to cultural practices that tolerate and allow
disruptions. Adjustments and adaptations to the continuous noise levels that are inappropriate
signals the continuity of the problem. All the organizations have their unique sounds, even if
they are quiet or loud. The different organization also have their own pace and times in which
activities are intensified while other moments busy quiet controls (Naik & Wang, 2014).
The culture of the organization can offer solutions to the issues of noise in the hospital,
particularly where they are created. For instance, mechanical repairs are essential and can aid in
acoustic boosting. However, annoyance and noise created by people and the patients who lack
control over what they're undergoing remain to be the problem. The pacing of hospitals competes
with the patients' pacing in the hospitals. The cycles of days and nights are distracted due to
rounds that occur following the hospital's norms51. Patients have no choice but to adapt
continuously to promising surroundings to be served but ends up offering services to patients'
diagnosis (Frayn, 2017). It must be clearly understood of when such disputes happen, the
approaches implemented in accommodating the patients' needs and auditory environment
accountability is the responsibility of the staffs. If such has not been identified, the issue of noise
will remain nobody’s responsibility (Patterson, et al., 2019).
8. My perspective in regards to the issue of noise in hospitals
Engage every person by forming a Sound Quality Committee
Sound environment is broad in a unique way, not just the noises at bedsides but also noises
emanating from outside. Nurses offer services both outside and inside patient rooms, hence, they
are better placed to assess the circumstances experienced by families and patients52. It is
important to come up with various Sound Quality Committees on disciplinary led by nurses with
other stakeholders such as volunteers, management staff, ancillary staffs, house keepers and
environmental services from the facility (Nunez, et al., 2016). This can effectively escalate
accountability in regards to the sound environment especially the individuals who directly access
patients. Physicians must also be involved, even though, they spend less time with patients
(Stewart, et al., 2016).
The problem with teaching health care facilities, however, is that during monumental rounds the
cause of the noise is known. Groups of residents and physicians pass through patient’s rooms and
halls with no attention to the auditory effects they cause to the environment. Nevertheless,
Physicians feel they have gained when they offer excellent outcomes about patients.
Agitated patients sleep-deprived or confused require an environment that supports their needs
directly throughout day and night in a way beyond evaluation and medication. Hence, involving
representation from residents and physicians can bring patients closer more than expected
(Bower, et al., 2015).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
The standards particularly address on the physical plant, the consequences, however, rely on the
relationship between the environment created and those who work, live and heal within it. Given
that noise is as a result of the culture, putting in place modern standards results to change in
culture. Change of culture occurs gradually and calls for patience and consistency53.
It is good to observe that noise cannot be solved by the Sound Environment Committee only.
Noise should be modelled, subjected to cultural practices that promote healing and be managed.
The Committee is created so that the issue can be given the priority, enable cultural change and
add weight to the goals to be achieved (Brown, et al., 2015).
The sound environment must be assessed on how noisy it is
After the establishment of the committee, it should establish protocols for inceptive assessment
of the sound environment. Details concerning the contributing aspects and the genesis of noise
must be included because they are crucial in the assessment.
When a decibel meter is used, it may offer an insight in determining the extent of loudness, but
the real loudness is suitably accessed and understood in real time in the way it is heard (Zhang, et
al., 2019). The committee is required to visit the places they don't perform duties in and observe
what can be heard. Whatever is heard must be noted down at the far end of rooms from the
working station of nurses and the closest points such as from the patients’ rooms, all entrances
and elevators and hall ways (Cohen, et al., 2013). Additionally, this should take place during
times and different shifts of the day due to the varying nature of the unit throughout day and
night54.
Waiting rooms give more suffering and anxiety to families. Thus, being in the waiting room for
more than one hour as done by families sometimes is the only way of understanding the
Paraphrase This Document
problems brought about by noise. Lack of confidentiality, conversations, televisions and
anonymity as a result of the circumstance itself. It is important to weigh whether the environment
is not providing anything helpful to relieve stress and pass time. Noise experience must equally
be understood from the view of families and patients. This may be achieved through talking with
staffs and patients or survey. Inquire about what makes them angry, ask them if they heard
anything at night and inquire about their experiences at different times of the day (NAP, 2010).
Perception is key, however, the dB level usage is limited to understanding stressors that distract
patients. The dB levels are suitably used particularly in finding HVAC systems, cleaning and
medical equipment. This is due to the synchronized sounds that help in informing about people's
speaking and hearing experience55. Various aspects should be put into accounts such as closing
doors, functional levels of noises from phone devices, medical monitors, various technological
sounds and paging volume systems. Speech privacy should also be added as a criterion as well as
being able to listen to what can be heard and judge whether it is relevant (Tobías, et al., 2015).
The committee should listen to the babble and conversations from crowds and be able to
establish intelligibility, audibility and appropriateness. If confidential information which should
not be heard but is heard, it is possible that it might have also been heard by many people.
Therefore, looking at it from the patients’ angle, hearing inappropriate information may cause
them to feel uncomfortable. Noise causes people to talk very loud because noise gives birth to
noise (Shield, et al., 2016). This is referred to as the Lombard Reflex which was discovered by a
psychologist known as Etienne Lombard. He explained the automatic response about speakers
who raise their levels of vocals when the background noises are louder, thus, making many
changes to their voices so as boost the speech intelligibility signal. This response is involuntary,
hence, when the nurse’s station and the corridors of hospitals are noisy any person around will
speak louder56.
Before implementing noise minimization policies, it is important to ensure that the surrounding
is under control as it affects every speech volume. The noise floor is the amount of sound in any
place that exists before any person talks or any activity is conducted. The HVAC system is the
major contributing factor to the noise floor then followed by the ice machine. The documentation
of every experience details by date, place and time, including what was heard and the nature of
the noise floor is very important57.
Put in place sound standards
After collecting the information, the committee on sound must put in place qualitative standards
in regards to sound that are capable of being maintained and measured. The standards should be
flexible in a way that every specific unit have their homeostasis definition and auditory pacing of
what is a relevant sound volume. Sound volumes differ from the noise floor which refers to the
continuous noise in a given place and time. Therefore, for any other noise to be heard, it must be
louder than the noise floor58. Where sound raises to 30dB louder than the noise floor, it may be
lead to startle responses. However, where sound volumes are very quiet, unavoidable noises and
conversations cause disturbances (Magdy, et al., 2019).
The goal should be to contain the sound environment to render them suitable to the staff and
patients’ needs. Silence is not desirable or realistic what patients require is to feel life and feel
that someone is there for them. Containing the sound environment refers to the inclusion of
sounds that are positive when necessary, minimizing irrelevant and relevant sounds where
necessary and masking extreme noise if possible. Using music as a way of conditioning the
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
sound environment is a viable choice given that it is used in a properly (Carayon, 2016). Other
companies use foreground music to block unnecessary noises and keep needed noise floor. The
combination of nature images and music in hospital environments has been discovered to
minimize the levels of required pain medication and boosts its analgesic impacts59. Additionally,
music effectively plays as audio-anxiolytic, induces relaxation, boots the quality of sleep and
restfulness when correctly used (Bliefnick, et al., 2019).
Customized systems of sound distribution are designed to keep the experiences of families and
patients at optimal and mechanically produce more pleasing noise floor. These sound systems
can improve music quality and provide local noise controls at waiting places60. The music
systems should be created in a manner that aligns with the healing mission of a hospital (Basner
& McGuire, 2018). The systems should be distinct but parallel to the emergency paging unit that
should be of very high qualities, designed acoustically to facilitate hearing for long hours and
provide wholesome frequency. These music systems offer a comforting feeling to patients and
their families (Bower, et al., 2015).
Put in place Purchasing Standards and Maintenance of Equipment
After goals and standards have been put in place, make recommendations meant for changing
staff practices, modifying equipment and improving policies of purchase. Additionally,
maintenance and repair policies must be reviewed to reflect great functionality quality such as
more quiet operations. Ongoing sounds of operations and medical equipment form the noise
floor together with the HVAC systems which leading to louder noise volumes. To prevent
escalations of noises, create auditory effect specifications for every type of equipment that can be
measured. This must include different sound volumes expected by the patients and people who
operate the machines. Reducing equipment sound can be attained by putting in place
Paraphrase This Document
comparative standards that reflect the normal dB volumes of equipment, time and clinical places.
An agreeable level must be reached where a piece of equipment has less effect on the patient and
the environment. Such specifications must be indicated and listed on every RFPs for equipment
purchase (Kelly & Mason, 2011).
A lot of noise at the hospital surrounding brought about by auditory predators may be
substantially minimized by maintenance, mechanical adjustments and buying modern equipment
where necessary. The auditory effects of equipment may be minimized by using padding,
installation of acoustically effective ceiling tiles, replacing and repairing door bumpers, replacing
wheels and use of floors that absorb sound (Roberts, 2014).
Advocate for patients through attenuation of the equipment sound
Fatigue as a result of medical alarms is a growing safety concern. Research at John Radcliffe
Hospital reveals that there are over 59,000 alarms in a month61. Adjusting and checking
monitors can prevent unrequired alarms can to a large extent lower unneeded distractions and
exposure to noise. Monitor attenuation should not be done impromptu but should be done on an
individual basis in regards to the agreement between physicians and nurses and evaluation of the
patient's clinical state62. The patient’s capability to control any auditory stimuli should be
evaluated to aid reduce agitation and startle responses if every monitor is customized to meet the
condition of patients. When acuity is high, the capability of the patient to adapt to the
surrounding is very low. It is, therefore, important to address technology in all angles from the
patients' experiences at crucial moments to enhancing sleep and minimizing noise (Adams,
2016).
Sounds that reach patients emanating within or far from their rooms also must be addressed. The
use of barriers including curtains and doors to offer both auditory and visual safeguards can help
regulate noises that come from a particular place to another. For instance, the sonorous noises of
pneumatic tube system can cause an instant distraction to nearby ICU patients. The decibel
amount is reduced by correct use padding. Any type of acoustic and padding materials must
conform to control regulations to infection and fire (Basner & McGuire, 2018).
Staff should be educated about Behavioral Sound-Sensitive Model
Normally, noise is an outcome of the organization's culture and whereas sound levels are an
outcome of the organization's norms63. Therefore, staffs are forced to change behaviour as a way
of noise management. Instead of making behavioural standards mandatory, the behavioural
change should be extended and modelled across the organization (Cowan, 2016). This involves
the practices and policies concerning confidential and private conversations that occur in public
places, mobile devices use paging methods and usages, telephones and nurse call system.
Staff members should be empowered to contribute data towards the Sound Quality Committee.
Means should be put in place to allow staffs to communicate compelling issues to the committee
and acknowledge that their suggestions have been well received. Proactive engagement among
staffs is a crucial contribution to long-period success64. This may be achieved by creating a
different general email or another communication platform for the committee. Such
communication platforms can enable forwarding of information to the committee head without
mentioning anyone’s names. Suggestions from staffs must be responded to and appreciate them
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
for their effort (Fry, 2013). Suggestions can be responded to by giving staffs the way forward or
instructions on what should be done. The head must act as an example otherwise any efforts
made me lose meaning and fail in the end. It is also important to come up with a culture that
promotes healing and safeguards the environment as a major caregiver. This must be reinstated
in the auditory room given that it is a place where patients cannot avoid.
Measure the outcome
The measuring process of the results is the same as the inceptive assessment65. However, the
results of staffs and patients must be put into the account in regards to staff stress and quality of
sleep for patients. Those two aspects must be included in determining whether the action taken is
effective. Both the qualitative and quantitative measures should be used, level of sleep or pain
medication required, surveys on patient satisfaction and decibel levels. In regards to the level of
calling nurses during the night, pain and anxiety medication required and complaints at daytime
can aid in shading light on what has become better or not. A comparative analysis is important in
determining the extent of what has been achieved and what sound environment factors have not
been or are yet to be achieved (Applebaum, et al., 2016). Other companies opt to provide
designed questionnaires that concentrate specifically on the protection of the environment.
However, noise must be addressed as a general question and not specifically the very broad
effects of noise66. The after and prior baseline information is the most critical thus helpful. While
measuring the outcome, it is important to consider speech privacy as an outcome that has a direct
impact on the sound environment (Real, et al., 2017). Therefore, an equitable sound environment
refers to the one that is not very noisy and not very quiet. Speech privacy is usually caused by
better practices, dynamic and healthy sound environment67.
Paraphrase This Document
9. Conclusion
Noise affects staff and patients in various distinct ways68. Unnecessary noises or sounds is the
main challenge in hospitals worldwide. Louder noises have negative effects on the well-being
and health of staffs and patients. Loud levels of noise may also slow down the healing process
for some patients69. Environments that have poor designs may lead to confidential talks between
staff members or staffs and patients being unintendedly heard by other listeners. This leads to an
unacceptable breach of privacy70. On the same note, acoustically poor surrounding hinders
effective communication thus makes auditory signals and speeches have low intelligibility (Naik
& Wang, 2014). This causes severe implications on the safety of staffs and patients71. Some
hospital settings are too loud with high levels of constant noises similar to that of busy
restaurants. Staff activities are among the major causes of noise, however, ambient levels of
sound nearby patients are usually loud because of the alarms, hospital plant and noise from
equipment72. Various task scheduling, review of the alarm threshold, repositioning of equipment
and staff education programmes have not reduced noise levels following the recommended levels
of WHO73. The present practicable solutions in regards to the National Health Service is earplugs
or other devices that defend the ears of staffs and patients (Pinsky, et al., 2013). However, there
might be many future opportunities to modify alerts where smart alert systems may be used74.
Substantial evidence has revealed that enhancing the acoustical setting in hospitals through
careful consideration of design aspects may further lower sound and raise the confidentiality of
patients75. The following are the major designs to be considered (Ahmed, 2016);
Installation of acoustical ceiling materials with suitable sound-absorption characteristics
leads to reduced reverberation durations, better speech intelligibility and low sound
propagation. Additionally, the measures of this design raise speech privacy due to less
noise travelling to adjacent voids76.
Offering single rooms for patients than many rooms. This is because a private room is
less loud and patients may consider it highly private. Single rooms also allow more
private and effective conversations between patients and staff77.
Offering treatment places and examination rooms for patients that have fully extended
walls to the support ceiling. This can help avoid noises and voices travelling via
ceilings78.
Minimizing or removing loud sources of sounds on hospital departments and creating
awareness to staff members on the effects of sound on themselves as well as patients can
effectively help lower the levels of sounds.
At the time Florence Nightingale undertook upon herself to define what nursing is, there was less
technology to depend on or use. Instead, the environment or the sick room mattered most and
had protocols that were effective in addressing the solutions and problems to the mortality and
morbidity of patients79. Right now, medical errors and nursing can be listed among the risks
brought about by sound-laden surrounding (Brown, et al., 2015). Even with modern technologies
applied to monitor the accuracy and distribution of drugs, more has to be done to reduce noise in
the auditory environment. Phone devices offer a broad set of problems in maintaining
confidentiality and safeguarding speech confidentiality. Mobile users talk loudly to a point they
hear themselves speak which causes the confidential mobile exchange to become public. The
auditory setting should reflect great compassion and very high standards of patient care. Putting
in place noise standards for equipment, design and technology may be easier for patients to walk
through the health care system visiting any department and experience similar standards of
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
care80. Nursing excellence since Nightingale times till now deals with a person as a whole,
patient experience and the mandatory medical care. Hospitals should aim higher than achieving
neutral auditory myth of not to harm respect with distraction and noise (Carayon, 2016). This can
be achieved by offering fountains, nature and music, or any pleasant sources of sound that can
enhance the experience of quality healthcare. Staffs and patients in hospitals must stop and listen.
Whatever is overheard must correspond with similar standards, values in providing clinical care
(Locihová, et al., 2018).
10. Bibliography
1. Adams, T. (2016) Sound Materials: A Compendium of Sound Absorbing Materials for
Architecture and Design. illustrated ed. Tin Shui Wai: Frame Publishers. pp. 206.
2. Ahmed, N. (2016) Advances in Noise Analysis, Mitigation and Control. 1 ed. Tai Po: BoD.
pp.30.
3. Applebaum, D., Calo, O. and Neville, K. (2016) Implementation of quiet time for noise
reduction on a medical-surgical unit. JONA: The Journal of Nursing Administration. pp. 670.
4. Bae, I., Song, J., Lee, M. and Hur, M. (2018) Effects of aromatherapy essential oil inhalation
on the stress response after exposure to noise and arithmetic subtraction stressor: randomized
controlled trial. International Journal of Clinical and Experimental Medicine. pp. 280.
5. Basner, M. and McGuire, S. (2018) WHO environmental noise guidelines for the European
region: a systematic review on environmental noise and effects on sleep. International journal of
environmental research and public health. pp. 519.
Paraphrase This Document
6. Bliefnick, J., Ryherd, E. and Jackson, R. (2019) Evaluating hospital soundscapes to improve
patient experience. The Journal of the Acoustical Society of America. pp. 1125.
7. Bower, R., Jackson, C. and Manning, J. (2015). Interruptions and medication administration in
critical care. Nursing in critical care. pp. 183.
8. Brown, B., Rutherford, P. and Crawford, P. (2015). The role of noise in clinical environments
with particular reference to mental health care: A narrative review. international journal of
nursing studies. pp. 1514.
9. Carayon, P. (2016) Handbook of Human Factors and Ergonomics in Health Care and Patient
Safety. 2, illustrated ed. Tai Po: CRC Press. pp. 782
10. Chow, V. and Shellhaas, R. (2016) Acoustic environment profile of the neonatal intensive
care unit: High ambient noise and limited language exposure. Journal of Neonatal Nursing. pp.
160.
11. Citerio, G., Prisco, L., Oddo, M., Meyfroidt, G., Helbok, R., Stocchetti, N., Taccone, F.,
Vincent, J.L., Robba, C., Elli, F. and Sala, E. (2019). International prospective observational
study on intracranial pressure in intensive care (ICU): the SYNAPSE-ICU study protocol. BMJ
open. p. 026552.
12. Clapp, M., James, K. and Kaimal, A. (2018). The effect of hospital acuity on severe maternal
morbidity in high-risk patients. American journal of obstetrics and gynecology. pp. 111.
13. Clerk, A. and Patel, K. (2019) Alarm Fatigue in ICU: How to Minimize?. Critical Care
Update. p. 51.
14. Cohen, S., Evans, G. W., Stokols, D. and Krantz, D. S. (2013). Behaviour, Health, and
Environmental Stress. illustrated ed. Tai Po: Springer Science & Business Media. pp. 20.
15. Cowan, J. P. (2016). The Effects of Sound on People. illustrated, reprint ed. Yuen Long: John
Wiley & Sons.
16. Darbyshire, J. & Young, J. (2013) An investigation of sound levels on intensive care units
with reference to the WHO guidelines. Critical Care. p. 187.
17. de Ruvo, E., Sciarra, L., Martino, A.M., Rebecchi, M., Iulianella, R.V., Sebastiani, F.,
Fagagnini, A., Borrelli, A., Scarà, A., Grieco, D. and Tota, C. (2016) A prospective comparison
of remote monitoring systems in implantable cardiac defibrillators: potential effects of frequency
of transmissions. Journal of Interventional Cardiac Electrophysiology. pp. 85.
18. Edwards, S. L. and Sabato, M. (2009) A Nurse's Survival Guide to Critical Care E-Book. 1
ed. Tin Shui Wai: Elsevier Health Sciences. pp. 446.
19. Eggert, J., Dye, C.J., Vincent, E., Parker, V., Daily, S.B., Pham, H., Watson, A.T., Summey,
H. and Roy, T. (2015) Effects of viewing a preferred nature image and hearing preferred music
on engagement, agitation, and mental status in persons with dementia. SAGE open medicine. p.
2050312115602579.
20. Eijkholt, M., Jankowski, J. and Fisher, M. (2017). Screen Shots: When Patients and Families
Publish Negative Health Care Narratives Online. Narrative inquiry in bioethics. pp. 250.
21. Farrow, M. (2018) Noise Reduction: Methods, Applications and Technology. 1 ed. Tin Shui
Wai: Nova Science Publishers, Incorporated. pp. 130.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
22. Fogel, B. S. and Greenberg, D. B. (2015) Psychiatric Care of the Medical Patient. illustrated,
reprint ed. Yuen Long: Oxford University Press. pp. 16
23. Frayn, M. (2017) Noises Off. 1 ed. Sha Tin: Bloomsbury Publishing. pp. 137.
24. Freye, E. (2012) Cerebral Monitoring in the Operating Room and the Intensive Care Unit.
illustrated ed. Tin Shui Wai: Springer Science & Business Media. pp. 167.
25. Fry, A. (2013) Noise Control in Building Services: Sound Research Laboratories Ltd. revised
ed. Ma On Shan: Elsevier Science. pp. 413.
26. Gallacher, S., Enki, D., Stevens, S. and Bennett, M. (2017) An experimental model to
measure the ability of headphones with active noise control to reduce patient’s exposure to noise
in an intensive care unit. Intensive care medicine experimental. pp. 47.
27. Gerth, A., Hatch, R., Young, J. and Watkinson, P. (2019) Changes in health‐related quality of
life after discharge from an intensive care unit: a systematic review. Anaesthesia. pp. 105.
28. Goeren, D., John, S., Meskill, K., Iacono, L., Wahl, S. and Scanlon, K. (2018). Quiet time: a
noise reduction initiative in a neurosurgical intensive care unit. Critical Care Nurse. pp. 39.
29. Grossman, M., Anderson, S.L., Worku, A., Marsack, W., Desai, N., Tuvilleja, A., Ramos, J.,
Francisco, M.A., Lafond, C., Balachandran, J.S. and Mokhlesi, B. (2017) Awakenings?Patient
and hospital staff perceptions of nighttime disruptions and their effect on patient sleep. Journal of
Clinical Sleep Medicine, pp. 304.
30. Grunden, N. & Hagood, C. (2012) Lean-Led Hospital Design: Creating the Efficient Hospital
of the Future. illustrated ed. Yuen Long: CRC Press. pp. 320.
Paraphrase This Document
31. Harris, D. (2016) Surface Finish Materials: Considerations for the Neonatal Intensive Care
Unit (NICU). Newborn and Infant Nursing Reviews. pp. 204.
32. Holland, K. and Jenkins, J. (2019) Applying the Roper-Logan-Tierney Model in Practice - E-
Book. 3 ed. Sha Tin: Elsevier Health Sciences. pp. 17.
33. Johnson, A. and Crumlett, H. (2017) Critical Care Nursing Certification: Preparation,
Review, and Practice Exams, Seventh Edition. 7 ed. Tai Po: McGraw Hill Professional. pp. 620.
34. Kawai, Y., Weatherhead, J.R., Traube, C., Owens, T.A., Shaw, B.E., Fraser, E.J., Scott,
A.M., Wojczynski, M.R., Slaman, K.L., Cassidy, P.M. and Baker, L.A. (2019) Quality
improvement initiative to reduce pediatric intensive care unit noise pollution with the use of a
pediatric delirium bundle. Journal of intensive care medicine. pp. 385.
35. Kelly, L. M. and Mason, J. (2011) Communication Skills for the Healthcare Professional. 1
ed. Tai Po: Wolters Kluwer/Lippincott Williams & Wilkins Health. pp. 230.
36. Kitapci, K. and Galbrun, L. (2019) Perceptual analysis of the speech intelligibility and
soundscape of multilingual environments. Applied Acoustics. pp. 126.
37. Kol, E., Aydın, P. and Dursun, O. (2015) The effectiveness of environmental strategies on
noise reduction in a pediatric intensive care unit: Creation of single‐patient bedrooms and
reducing noise sources. Journal for Specialists in Pediatric nursing. pp. 215.
38. Kreis, I. A., Busby, A., Leonardi, G., Meara, J. and Murray, V. (2013) Essentials of
Environmental Epidemiology for Health Protection: A Handbook for Field Professionals.
illustrated ed. Ma On Shan: OUP Oxford. pp. 3.
39. Locihová, H., Axmann, K., Padyšáková, H. and Fejfar, J. (2018) Effect of the use of earplugs
and eye mask on the quality of sleep in intensive care patients: a systematic review. Journal of
sleep research. p. 12607.
40. Lou, M. S., Klein, D. G. and Moseley, J. M. (2013) Introduction to Critical Care Nursing6:
Introduction to Critical Care Nursing. illustrated ed. Ma On Shan: Elsevier Health Sciences. pp.
90.
41. Magdy, D., Metwally, A. and Makhlouf, H. (2019) Study of sleep quality among patients
admitted to the respiratory intensive care unit. Egyptian Journal of Bronchology. p. 114.
42. Montague, K., Blietz, C. and Kachur, M. (2009) Ensuring quieter hospital environments.
AJN The American Journal of Nursing. pp. 65.
43. Müller-Trapet, M., Cheer, J., Fazi, F.M., Darbyshire, J. and Young, J.D. (2018) Acoustic
source localization with microphone arrays for remote noise monitoring in an Intensive Care
Unit. Applied Acoustics. pp. 97.
44. Münzel, T., Sørensen, M., Schmidt, F., Schmidt, E., Steven, S., Kröller-Schön, S. and
Daiber, A. (2018) The adverse effects of environmental noise exposure on oxidative stress and
cardiovascular risk. Antioxidants & redox signaling. pp. 873.
45. Naik, G. R. and Wang, W. (2014) Blind Source Separation: Advances in Theory, Algorithms
and Applications. illustrated ed. Shai Tin: Springer. pp. 151.
46. NAP. (2010) Technology for a Quieter America. 1 ed. MA On Shan: National Academies
Press. pp. 14.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
47. NAP. (2011) The Future of Nursing: Leading Change, Advancing Health. 1 ed. Victoria
City: National Academies Press. pp. 14.
48. Nunez, A., Ihsan, M., Gaballah, S., Haque, A., Yurevich, O., Ahluwalia, S., Salciccioli, L.,
Stewart, M. and Lazar, J. (2016) Differential effects of hyperemia and passive leg raising on
QRS to Korotkoff sound time intervals in hypertensive patients. Journal of the American Society
of Hypertension. p. 32.
49. Page, V. J. and Wesley, E. E. (2015) Delirium in Critical Care. illustrated, reprint, revised ed.
North Lantau: Cambridge University Press. pp. 212.
50. Parr Vijinski, J., Hirst, S. and Goopy, S. (2018) Nursing and music: Considerations of
Nightingale’s environmental philosophy and phenomenology. Nursing Philosophy. p. 12223.
51. Patterson, E., Sanders, E.B.N., Lavender, S.A., Sommerich, C.M., Park, S., Li, J. and Evans,
K.D. (2019) A Grounded Theoretical Analysis of Room Elements Desired by Family Members
and Visitors of Hospitalized Patients: Implications for Medical/Surgical Hospital Patient Room
Design. HERD: Health Environments Research & Design Journal. pp. 125.
52. Pfeiffer, J. (2018) Strategies Christian Nurses Use to Create a Healing Environment.
Religions,. p. 352.
53. Pinsky, M. R., Brochard, L., Mancebo, J. and Antonelli, M. (2013) Applied Physiology in
Intensive Care Medicine 2: Physiological Reviews and Editorials. 3, illustrated ed. North Lantau:
Springer Science & Business Media. pp. 260.
Paraphrase This Document
54. Plummer, N., Herbert, A., Blundell, J.E., Howarth, R., Baldwin, J. and Laha, S. (2019)
SoundEar noise warning devices cause a sustained reduction in ambient noise in adult critical
care. Journal of the Intensive Care Society. pp. 109.
55. Pope, D. and Miller-Klein, E. (2016) Acoustic assessment of speech privacy curtains in two
nursing units. Noise & health. p. 26.
56. Rashid, H., Hussain, F. and Masood, K. (2019) Patient privacy: Challenges and opportunities
in the age of big data. Current Science. pp. 5.
57. Real, K., Bardach, S. and Bardach, D. (2017) The role of the built environment: How
decentralized nurse stations shape communication, patient care processes, and patient outcomes.
Health communication. pp. 1560.
58. Rechel, B., Wright, S. and Edwards, N. (2009) Investing in Hospitals of the Future. 1 ed. Sha
Tin: WHO Regional Office Europe. pp. 4.
59. Richards, J. B. and Stapleton, R. D. (2014) Non-Pulmonary Complications of Critical Care:
A Clinical Guide. illustrated ed. Tin Shui Wai: Springer. pp. 2.
60. Roberts, R. (2014) Specialised Hospitals Design and Planning. illustrated ed. Yuen Long:
Design Media Publishing Limited. pp. 260.
61. Shah, P. and Krishnan, V. (2019). Hospitalization and Sleep. American journal of respiratory
and critical care medicine. pp. 19.
62. Shajahan, A., Culp, C. and Williamson, B. (2019) Effects of indoor environmental
parameters related to building heating, ventilation, and air conditioning systems on patients'
medical outcomes: A review of scientific research on hospital buildings. Indoor Air. pp. 166.
63. Shield, B., Shiers, N. and Glanville, R. (2016) The acoustic environment of inpatient hospital
wards in the United Kingdom. The Journal of the Acoustical Society of America. pp. 2223.
64. Simons, K., Van den Boogaard, M. and De Jager, C. (2019). Impact of intensive care unit
light and noise exposure on critically ill patients. Neth J Crit Care. pp. 146.
65. Stamper, G. and Johnson, T. (2015). Auditory function in normal-hearing, noise-exposed
human ears. Ear and hearing. p. 172.
66. Stans, S., Dalemans, R., de Witte, L.P., Smeets, H.W. and Beurskens, A.J. (2017) The role of
the physical environment in conversations between people who are communication vulnerable
and health-care professionals: a scoping review. Disability and rehabilitation. pp. 2600.
67. Stewart, J., McManus, F., Rodgers, N., Weedon, V. and Bronzaft, A. (2016) Why Noise
Matters: A Worldwide Perspective on the Problems, Policies and Solutions. reprint ed. Sha Tin:
Routledge. pp. 22.
68. Tauber‐Gilmore, M., Norton, C., Procter, S., Murrells, T., Addis, G., Baillie, L., Velasco, P.,
Athwal, P., Kayani, S. and Zahran, Z. (2018) Development of tools to measure dignity for older
people in acute hospitals. Journal of clinical nursing. pp. 3710.
69. Taylor, I. G. and Markides, A. (2014) Disorders of Auditory Function, Volume 3. revised ed.
Tsuen Wan: Elsevier. pp. 52.
70. Tobías, A., Recio, A., Díaz, J. and Linares, C. (2015) Noise levels and cardiovascular
mortality: a case-crossover analysis. European journal of preventive cardiology. pp. 497.
71. Urbańska, D., Moritz, S. and Gawęda, Ł. (2019) The impact of social and sensory stress on
cognitive biases and delusions in schizophrenia. Cognitive neuropsychiatry. pp. 218.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
72. Vakharia, V., Rodionov, R., McEvoy, A.W., Miserocchi, A., Sparks, R., O’Keeffe, A.G.,
Ourselin, S. and Duncan, J.S. (2018) Improving patient safety during introduction of novel
medical devices through cumulative summation analysis. Journal of neurosurgery. pp. 215.
73. Vincent, J., Abraham, E., Kochanek, P., Moore, F.A. and Fink, M.P. (2015) Textbook of
Critical Care E-Book. 6 ed. Tin Shui Wai: Elsevier Health Sciences. pp. 1280.
74. Vollam, S., Dutton, S., Lamb, S., Petrinic, T., Young, J.D. and Watkinson, P. (2018) Out-of-
hours discharge from intensive care, in-hospital mortality and intensive care readmission rates: a
systematic review and meta-analysis. Intensive care medicine. pp. 1116.
75. Webb, A. and Gattinoni, L. (2016) Oxford Textbook of Critical Care. illustrated ed. Tin Shui
Wai: Oxford University Press. pp. 726.
76. Wessel, J., Jenkinson, N., Brittain, J.S., Voets, S.H., Aziz, T.Z. and Aron, A.R. (2016)
Surprise disrupts cognition via a fronto-basal ganglia suppressive mechanism. Nature
communications. p. 11195.
77. WHO. (2009) Night Noise Guidelines for Europe. illustrated ed. Tai Po: WHO. pp. 23.
78. Williams, C. and Gardiner, C. (2015) Preference for a single or shared room in a UK
inpatient hospice: patient, family and staff perspectives. BMJ supportive & palliative care. pp.
170.
79. Zhang, Y., Tzortzopoulos, P. and Kagioglou, M. (2019). Healing built-environment effects
on health outcomes: Environment–occupant–health framework. Building Research &
Information. pp. 748.
Paraphrase This Document
80. Zijlstra, E., Hagedoorn, M., Krijnen, W.P., van der Schans, C.P. and Mobach, M.P. (2019)
The effect of a non-talking rule on the sound level and perception of patients in an outpatient
infusion center. PloS one. p. 0212804.
11. References
Adams, T., 2016. Sound Materials: A Compendium of Sound Absorbing Materials for
Architecture and Design. illustrated ed. Tin Shui Wai: Frame Publishers.
Ahmed, N., 2016. Advances in Noise Analysis, Mitigation and Control. 1 ed. Tai Po: BoD.
Applebaum, D., Calo, O. & Neville, K., 2016. Implementation of quiet time for noise reduction
on a medical-surgical unit. JONA: The Journal of Nursing Administration, 46(12), pp. 669-674.
Bae, I., Song, J., Lee, M. & Hur, M., 2018. Effects of aromatherapy essential oil inhalation on
the stress response after exposure to noise and arithmetic subtraction stressor: randomized
controlled trial. International Journal of Clinical and Experimental Medicine, 11(1), pp. 275-
284.
Basner, M. & McGuire, S., 2018. WHO environmental noise guidelines for the European region:
a systematic review on environmental noise and effects on sleep. International journal of
environmental research and public health, 15(3), p. 519.
Bliefnick, J., Ryherd, E. & Jackson, R., 2019. Evaluating hospital soundscapes to improve
patient experience. The Journal of the Acoustical Society of America, 145(2), pp. 1117-1128.
Bower, R., Jackson, C. & Manning, J., 2015. Interruptions and medication administration in
critical care. Nursing in critical care, 20(4), pp. 183-195.
Brown, B., Rutherford, P. & Crawford, P., 2015. The role of noise in clinical environments with
particular reference to mental health care: A narrative review. international journal of nursing
studies, (9), 52(9), pp. 1514-1524.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Carayon, P., 2016. Handbook of Human Factors and Ergonomics in Health Care and Patient
Safety. 2, illustrated ed. Tai Po: CRC Press.
Chow, V. & Shellhaas, R., 2016. Acoustic environment profile of the neonatal intensive care
unit: High ambient noise and limited language exposure. Journal of Neonatal Nursing, 22(2), pp.
159-162.
Citerio, G. et al., 2019. International prospective observational study on intracranial pressure in
intensive care (ICU): the SYNAPSE-ICU study protocol. BMJ open, 9(4), p. 026552.
Clapp, M., James, K. & Kaimal, A., 2018. The effect of hospital acuity on severe maternal
morbidity in high-risk patients. American journal of obstetrics and gynecology, 219(1), pp. 111-
e1.
Clerk, A. & Patel, K., 2019. Alarm Fatigue in ICU: How to Minimize?. Critical Care Update ,
8(1), p. 51.
Cohen, S., Evans, G. W., Stokols, D. & Krantz, D. S., 2013. Behaviour, Health, and
Environmental Stress. illustrated ed. Tai Po: Springer Science & Business Media.
Cowan, J. P., 2016. The Effects of Sound on People. illustrated, reprint ed. Yuen Long: John
Wiley & Sons.
Darbyshire, J. & Young, J., 2013. An investigation of sound levels on intensive care units with
reference to the WHO guidelines. Critical Care, 17(5), p. 187.
de Ruvo, E. et al., 2016. A prospective comparison of remote monitoring systems in implantable
cardiac defibrillators: potential effects of frequency of transmissions. Journal of Interventional
Cardiac Electrophysiology, 45(1), pp. 81-90.
Paraphrase This Document
Edwards, S. L. & Sabato, M., 2009. A Nurse's Survival Guide to Critical Care E-Book. 1 ed. Tin
Shui Wai: Elsevier Health Sciences.
Eggert, J. et al., 2015. Effects of viewing a preferred nature image and hearing preferred music
on engagement, agitation, and mental status in persons with dementia. SAGE open medicine,
3(1), p. 2050312115602579.
Eijkholt, M., Jankowski, J. & Fisher, M., 2017. Screen Shots: When Patients and Families
Publish Negative Health Care Narratives Online. Narrative inquiry in bioethics, 7(3), pp. 245-
254.
Farrow, M., 2018. Noise Reduction: Methods, Applications and Technology. 1 ed. Tin Shui Wai:
Nova Science Publishers, Incorporated.
Fogel, B. S. & Greenberg, D. B., 2015. Psychiatric Care of the Medical Patient. illustrated,
reprint ed. Yuen Long: Oxford University Press.
Frayn, M., 2017. Noises Off. 1 ed. Sha Tin: Bloomsbury Publishing.
Freye, E., 2012. Cerebral Monitoring in the Operating Room and the Intensive Care Unit.
illustrated ed. Tin Shui Wai: Springer Science & Business Media.
Fry, A., 2013. Noise Control in Building Services: Sound Research Laboratories Ltd. revised ed.
Ma On Shan: Elsevier Science.
Gallacher, S., Enki, D., Stevens, S. & Bennett, M., 2017. An experimental model to measure the
ability of headphones with active noise control to reduce patient’s exposure to noise in an
intensive care unit. Intensive care medicine experimental, 5(1), p. An experimental model to
measure the ability of headphones with active noise control to reduce 47.
Gerth, A., Hatch, R., Young, J. & Watkinson, P., 2019. Changes in health‐related quality of life
after discharge from an intensive care unit: a systematic review. Anaesthesia, 74(1), pp. 100-108.
Goeren, D. et al., 2018. Quiet time: a noise reduction initiative in a neurosurgical intensive care
unit. Critical Care Nurse, 38(4), pp. 38-44.
Grossman, M. et al., 2017. Awakenings?Patient and hospital staff perceptions of nighttime
disruptions and their effect on patient sleep. Journal of Clinical Sleep Medicine, 13(02), pp. 301-
306.
Grunden, N. & Hagood, C., 2012. Lean-Led Hospital Design: Creating the Efficient Hospital of
the Future. illustrated ed. Yuen Long: CRC Press.
Harris, D., 2016. Surface Finish Materials: Considerations for the Neonatal Intensive Care Unit
(NICU). Newborn and Infant Nursing Reviews, 16(4), pp. 203-207.
Holland, K. & Jenkins, J., 2019. Applying the Roper-Logan-Tierney Model in Practice - E-Book.
3 ed. Sha Tin: Elsevier Health Sciences.
Johnson, A. & Crumlett, H., 2017. Critical Care Nursing Certification: Preparation, Review,
and Practice Exams, Seventh Edition. 7 ed. Tai Po: McGraw Hill Professional.
Kawai, Y. et al., 2019. Quality improvement initiative to reduce pediatric intensive care unit
noise pollution with the use of a pediatric delirium bundle. Journal of intensive care medicine,
34(5), pp. 383-390.
Kelly, L. M. & Mason, J., 2011. Communication Skills for the Healthcare Professional. 1 ed. Tai
Po: Wolters Kluwer/Lippincott Williams & Wilkins Health.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Kitapci, K. & Galbrun, L., 2019. Perceptual analysis of the speech intelligibility and soundscape
of multilingual environments. Applied Acoustics, 151(1), pp. 124-136.
Kol, E., Aydın, P. & Dursun, O., 2015. The effectiveness of environmental strategies on noise
reduction in a pediatric intensive care unit: Creation of single‐patient bedrooms and reducing
noise sources. Journal for Specialists in Pediatric nursing, 20(3), pp. 210-217.
Kreis, I. A. et al., 2013. Essentials of Environmental Epidemiology for Health Protection: A
Handbook for Field Professionals. illustrated ed. Ma On Shan: OUP Oxford.
Locihová, H., Axmann, K., Padyšáková, H. & Fejfar, J., 2018. Effect of the use of earplugs and
eye mask on the quality of sleep in intensive care patients: a systematic review. Journal of sleep
research, 27(3), p. 12607.
Lou, M. S., Klein, D. G. & Moseley, J. M., 2013. Introduction to Critical Care Nursing6:
Introduction to Critical Care Nursing. illustrated ed. Ma On Shan: Elsevier Health Sciences.
Magdy, D., Metwally, A. & Makhlouf, H., 2019. Study of sleep quality among patients admitted
to the respiratory intensive care unit. Egyptian Journal of Bronchology, 13(1), p. 114.
Montague, K., Blietz, C. & Kachur, M., 2009. Ensuring quieter hospital environments. AJN The
American Journal of Nursing, 109(9), pp. 65-67.
Müller-Trapet, M. et al., 2018. Acoustic source localization with microphone arrays for remote
noise monitoring in an Intensive Care Unit. Applied Acoustics, 139(1), pp. 93-100.
Münzel, T. et al., 2018. The adverse effects of environmental noise exposure on oxidative stress
and cardiovascular risk. Antioxidants & redox signaling, 28(9), pp. 873-908.
Paraphrase This Document
Naik, G. R. & Wang, W., 2014. Blind Source Separation: Advances in Theory, Algorithms and
Applications. illustrated ed. Shai Tin: Springer.
NAP, 2010. Technology for a Quieter America. 1 ed. MA On Shan: National Academies Press.
NAP, 2011. The Future of Nursing: Leading Change, Advancing Health. 1 ed. Victoria City:
National Academies Press.
Nunez, A. et al., 2016. Differential effects of hyperemia and passive leg raising on QRS to
Korotkoff sound time intervals in hypertensive patients. Journal of the American Society of
Hypertension, 10(4), p. 32.
Page, V. J. & Wesley, E. E., 2015. Delirium in Critical Care. illustrated, reprint, revised ed.
North Lantau: Cambridge University Press.
Parr Vijinski, J., Hirst, S. & Goopy, S., 2018. Nursing and music: Considerations of
Nightingale’s environmental philosophy and phenomenology. Nursing Philosophy, 19(4), p.
12223.
Patterson, E. et al., 2019. A Grounded Theoretical Analysis of Room Elements Desired by
Family Members and Visitors of Hospitalized Patients: Implications for Medical/Surgical
Hospital Patient Room Design. HERD: Health Environments Research & Design Journal, 12(1),
pp. 124-144.
Pfeiffer, J., 2018. Strategies Christian Nurses Use to Create a Healing Environment. Religions,
9(11), p. 352.
Pinsky, M. R., Brochard, L., Mancebo, J. & Antonelli, M., 2013. Applied Physiology in Intensive
Care Medicine 2: Physiological Reviews and Editorials. 3, illustrated ed. North Lantau: Springer
Science & Business Media.
Plummer, N. et al., 2019. SoundEar noise warning devices cause a sustained reduction in
ambient noise in adult critical care. Journal of the Intensive Care Society, 20(2), pp. 106-110.
Pope, D. & Miller-Klein, E., 2016. Acoustic assessment of speech privacy curtains in two
nursing units. Noise & health, 18(80), p. 26.
Rashid, H., Hussain, F. & Masood, K., 2019. Patient privacy: Challenges and opportunities in the
age of big data. Current Science, 5(1), pp. 1-5.
Real, K., Bardach, S. & Bardach, D., 2017. The role of the built environment: How decentralized
nurse stations shape communication, patient care processes, and patient outcomes. Health
communication, 32(12), pp. 1557-1570.
Rechel, B., Wright, S. & Edwards, N., 2009. Investing in Hospitals of the Future. 1 ed. Sha Tin:
WHO Regional Office Europe.
Richards, J. B. & Stapleton, R. D., 2014. Non-Pulmonary Complications of Critical Care: A
Clinical Guide. illustrated ed. Tin Shui Wai: Springer.
Roberts, R., 2014. Specialised Hospitals Design and Planning. illustrated ed. Yuen Long: Design
Media Publishing Limited.
Shah, P. & Krishnan, V., 2019. Hospitalization and Sleep. American journal of respiratory and
critical care medicine, 199(10), pp. 19-20.
Shajahan, A., Culp, C. & Williamson, B., 2019. Effects of indoor environmental parameters
related to building heating, ventilation, and air conditioning systems on patients' medical
outcomes: A review of scientific research on hospital buildings. Indoor Air, 29(2), pp. 161-176.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Shield, B., Shiers, N. & Glanville, R., 2016. The acoustic environment of inpatient hospital
wards in the United Kingdom. The Journal of the Acoustical Society of America, 140(3), pp.
2213-2224.
Simons, K., Van den Boogaard, M. & De Jager, C., 2019. Impact of intensive care unit light and
noise exposure on critically ill patients. Neth J Crit Care, 27(1), pp. 145-149.
Stamper, G. & Johnson, T., 2015. Auditory function in normal-hearing, noise-exposed human
ears. Ear and hearing, 36(2), p. 172.
Stans, S. et al., 2017. The role of the physical environment in conversations between people who
are communication vulnerable and health-care professionals: a scoping review. Disability and
rehabilitation, 39(25), pp. 2594-2605.
Stewart, J. et al., 2016. Why Noise Matters: A Worldwide Perspective on the Problems, Policies
and Solutions. reprint ed. Sha Tin: Routledge.
Tauber‐Gilmore, M. et al., 2018. Development of tools to measure dignity for older people in
acute hospitals. Journal of clinical nursing, 27(19-20), pp. 3706-3718.
Taylor, I. G. & Markides, A., 2014. Disorders of Auditory Function, Volume 3. revised ed. Tsuen
Wan: Elsevier.
Tobías, A., Recio, A., Díaz, J. & Linares, C., 2015. Noise levels and cardiovascular mortality: a
case-crossover analysis. European journal of preventive cardiology, 22(4), pp. 496-502.
Urbańska, D., Moritz, S. & Gawęda, Ł., 2019. The impact of social and sensory stress on
cognitive biases and delusions in schizophrenia. Cognitive neuropsychiatry, 24(3), pp. 217-232.
Paraphrase This Document
Vakharia, V. et al., 2018. Improving patient safety during introduction of novel medical devices
through cumulative summation analysis. Journal of neurosurgery, 130(1), pp. 213-219.
Vincent, J. et al., 2015. Textbook of Critical Care E-Book. 6 ed. Tin Shui Wai: Elsevier Health
Sciences.
Vollam, S. et al., 2018. Out-of-hours discharge from intensive care, in-hospital mortality and
intensive care readmission rates: a systematic review and meta-analysis. Intensive care medicine,
44(7), pp. 1115-1129.
Webb, A. & Gattinoni, L., 2016. Oxford Textbook of Critical Care. illustrated ed. Tin Shui Wai:
Oxford University Press.
Wessel, J. et al., 2016. Surprise disrupts cognition via a fronto-basal ganglia suppressive
mechanism. Nature communications, 7(1), p. 11195.
WHO, 2009. Night Noise Guidelines for Europe. illustrated ed. Tai Po: WHO.
Williams, C. & Gardiner, C., 2015. Preference for a single or shared room in a UK inpatient
hospice: patient, family and staff perspectives. BMJ supportive & palliative care, 5(2), pp. 169-
174.
Zhang, Y., Tzortzopoulos, P. & Kagioglou, M., 2019. Healing built-environment effects on
health outcomes: Environment–occupant–health framework. Building Research & Information,
47(6), pp. 747-766.
Zijlstra, E. et al., 2019. The effect of a non-talking rule on the sound level and perception of
patients in an outpatient infusion center. PloS one, 14(2), p. 0212804.

⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
12. Appendix
12.1. Questionnaires
1. What is your age
2. What is your sex
3. What is your qualification?
4. What is your job experience?
5. What is your designation?
6. Do you agree that the Rattling trolleys noises alarms, ringing phones, televisions, staff
conversions, patient and victor conversions, car alarms from parking areas around and in
the hospital, horns, instructions to visitors, patients and staff effecting the process of cure
of patient?
Agree
Disagree
Strongly agree
Strongly disagree
Neutral
7. Do you agree that the Indoor noises from the fans, air conditioners, noisy windows, and
doors effecting the process of cure of patient?
Agree
Disagree
Paraphrase This Document
Strongly agree
Strongly disagree
Neutral
8. Do you agree that construction techniques are helpful for reducing the noise pollution in
hospital?
Yes
No
9. If yes, then then mark the most effective technique given as follows:
Use of Wall Mass while constructing the UK hospitals
Use of Cavity Partition for Noise Control while constructing the UK hospitals
Increasing the Airspace Width of Walls while constructing the UK hospitals
Increasing the use of Stud Spacing while constructing the UK hospitals
Usage of Studs in a Staggered Manner while constructing the UK hospitals
Studs and Panels held together by Resilient Materials while constructing the UK
hospitals
Panels Used Are Dissimilar while constructing the UK hospitals
Sound Absorbing Blankets Used in the Airspace while constructing the UK hospitals
The Cracks and Edges Are Sealed while constructing the UK hospitals
The size of window can be reduced while constructing the UK hospitals
The thickness of glass used in windows can be improved while constructing the UK
hospitals
The prefabricated doors can be used to reduce noise pollution while constructing the
UK hospitals
The use of wooden floor can be done while constructing the UK hospitals
With the use of masking technique, the noise can be insulated while constructing the
UK hospitals
10. Does your management has taken suitable actions for improving the insulating power
of a building?
Agree
Disagree
Strongly agree
Strongly disagree
Neutral
11. If disagree or strong disagree, then recommend the strategy to the management?
Use of Wall Mass while constructing the hospitals
Use of Cavity Partition for Noise Control while constructing the hospitals
Increasing the Airspace Width of Walls while constructing the hospitals
Increasing the use of Stud Spacing while constructing the hospitals
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Usage of Studs in a Staggered Manner while constructing the hospitals
Studs and Panels held together by Resilient Materials while constructing the hospitals
Panels Used Are Dissimilar while constructing the hospitals
Sound Absorbing Blankets Used in the Airspace while constructing the hospitals
The Cracks and Edges Are Sealed while constructing the hospitals
The size of window can be reduced while constructing the hospitals
The thickness of glass used in windows can be improved while constructing the
hospitals
The prefabricated doors can be used to reduce noise pollution while constructing the
hospitals
The use of wooden floor can be done while constructing the hospitals
With the use of masking technique, the noise can be insulated while constructing the
hospitals
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
© 2024 | Zucol Services PVT LTD | All rights reserved.

