Hand Hygiene in Hospital Care Setting | Report
VerifiedAdded on 2022/09/01
|13
|3135
|21
AI Summary
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: HAND HYGIENE IN HOSPITAL CARE SETTING
Hand hygiene in Hospital Care Setting
Name of the Student
Name of the University
Author Note
Hand hygiene in Hospital Care Setting
Name of the Student
Name of the University
Author Note
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1HAND HYGIENE IN HOSPITAL CARE SETTING
Section 1
Introduction
The issue of nosocomial infection due to poor hand hygiene techniques and practices in
the health facility centers and hospitals is one of the most common around the world. In this
regard, it can be stated that due to the poor practices of washing hands by the doctors, nurses and
other health facility providers day by day the cases of nosocomial infections are enhancing
(Gwarzo, 2018). According to the study of Jonker and Othman (2018), it is reported that, the
hand washing is accepted widely as infection prevention strategy in the intensive care units in the
hospitals. Nosocomial infections are a main barrier to the health-care organization and are related
with significant morbidity mortality and a financial burden to the health facility system.
According to the study of Anwar and Elareed (2019), it is stated that there are five moments of
hand washing and it is very crucial to wash the hand before touching a patient as it is quite
effective in preventing infection in the hospital care settings. As per the study findings of
McLaws (2015), it is reported that the rate of infection among the patients of the critical care unit
is very due to lack of hand washing before touching a patient. According to a study of Loftus et
al. (2019), it is stated that almost 61 per cent of health facility workers are not accustomed to
practice hand hygiene in the hospital care settings and in every year, the healthcare-associated
infections affect 15.5 per cent of patients in the advancing countries around the world and such
conditions are associated with the antimicrobial resistance which leads to 700,000 deaths in
every year. So, it is very important to improve the hand hygiene techniques and practices in the
health facility settings in order to enhance the patient satisfaction and to reduce the death rates
associated with the nosocomial infections (Marimuthu, Pittet & Harbarth, 2014).
Section 1
Introduction
The issue of nosocomial infection due to poor hand hygiene techniques and practices in
the health facility centers and hospitals is one of the most common around the world. In this
regard, it can be stated that due to the poor practices of washing hands by the doctors, nurses and
other health facility providers day by day the cases of nosocomial infections are enhancing
(Gwarzo, 2018). According to the study of Jonker and Othman (2018), it is reported that, the
hand washing is accepted widely as infection prevention strategy in the intensive care units in the
hospitals. Nosocomial infections are a main barrier to the health-care organization and are related
with significant morbidity mortality and a financial burden to the health facility system.
According to the study of Anwar and Elareed (2019), it is stated that there are five moments of
hand washing and it is very crucial to wash the hand before touching a patient as it is quite
effective in preventing infection in the hospital care settings. As per the study findings of
McLaws (2015), it is reported that the rate of infection among the patients of the critical care unit
is very due to lack of hand washing before touching a patient. According to a study of Loftus et
al. (2019), it is stated that almost 61 per cent of health facility workers are not accustomed to
practice hand hygiene in the hospital care settings and in every year, the healthcare-associated
infections affect 15.5 per cent of patients in the advancing countries around the world and such
conditions are associated with the antimicrobial resistance which leads to 700,000 deaths in
every year. So, it is very important to improve the hand hygiene techniques and practices in the
health facility settings in order to enhance the patient satisfaction and to reduce the death rates
associated with the nosocomial infections (Marimuthu, Pittet & Harbarth, 2014).
2HAND HYGIENE IN HOSPITAL CARE SETTING
Evidence Search Strategy
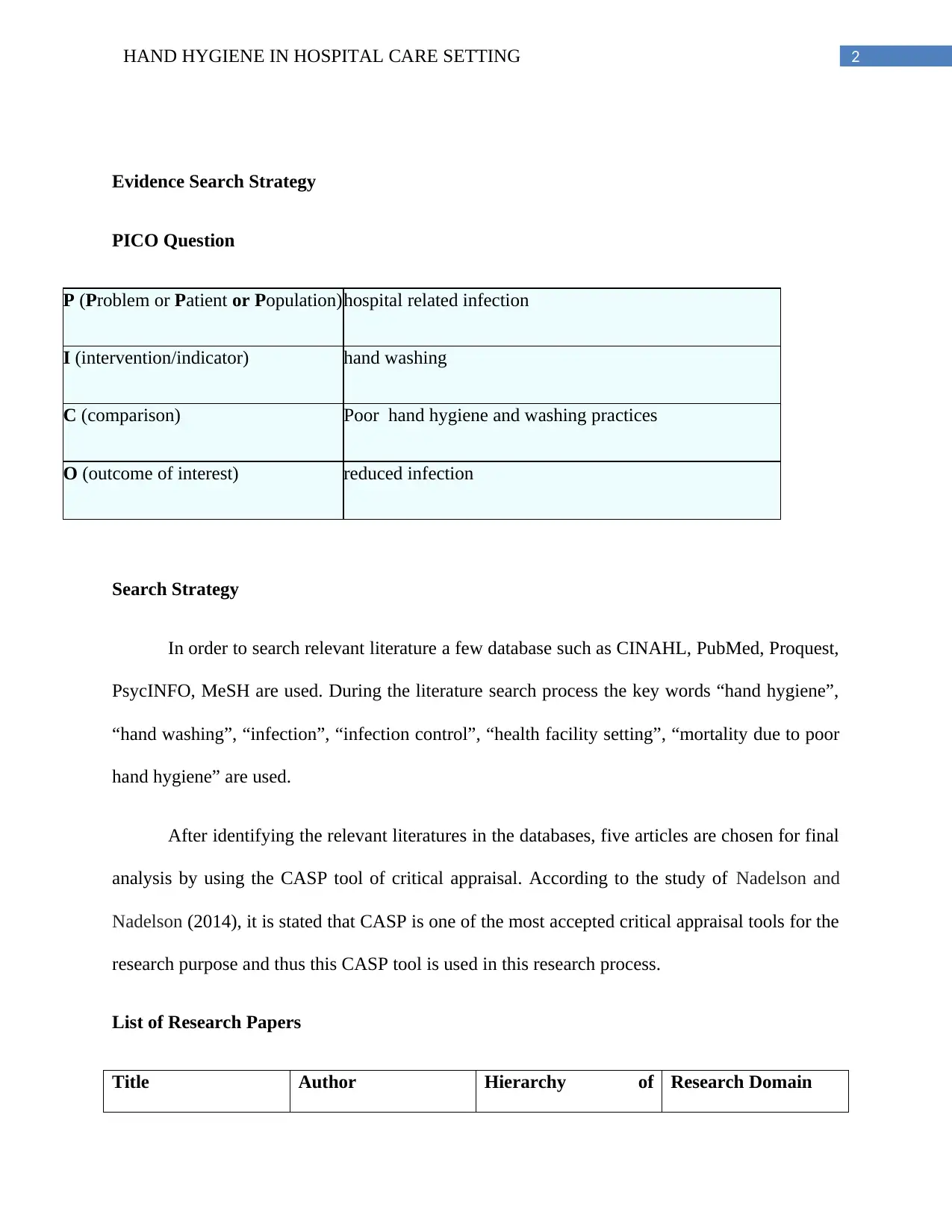
PICO Question
P (Problem or Patient or Population)hospital related infection
I (intervention/indicator) hand washing
C (comparison) Poor hand hygiene and washing practices
O (outcome of interest) reduced infection
Search Strategy
In order to search relevant literature a few database such as CINAHL, PubMed, Proquest,
PsycINFO, MeSH are used. During the literature search process the key words “hand hygiene”,
“hand washing”, “infection”, “infection control”, “health facility setting”, “mortality due to poor
hand hygiene” are used.
After identifying the relevant literatures in the databases, five articles are chosen for final
analysis by using the CASP tool of critical appraisal. According to the study of Nadelson and
Nadelson (2014), it is stated that CASP is one of the most accepted critical appraisal tools for the
research purpose and thus this CASP tool is used in this research process.
List of Research Papers
Title Author Hierarchy of Research Domain
Evidence Search Strategy
PICO Question
P (Problem or Patient or Population)hospital related infection
I (intervention/indicator) hand washing
C (comparison) Poor hand hygiene and washing practices
O (outcome of interest) reduced infection
Search Strategy
In order to search relevant literature a few database such as CINAHL, PubMed, Proquest,
PsycINFO, MeSH are used. During the literature search process the key words “hand hygiene”,
“hand washing”, “infection”, “infection control”, “health facility setting”, “mortality due to poor
hand hygiene” are used.
After identifying the relevant literatures in the databases, five articles are chosen for final
analysis by using the CASP tool of critical appraisal. According to the study of Nadelson and
Nadelson (2014), it is stated that CASP is one of the most accepted critical appraisal tools for the
research purpose and thus this CASP tool is used in this research process.
List of Research Papers
Title Author Hierarchy of Research Domain
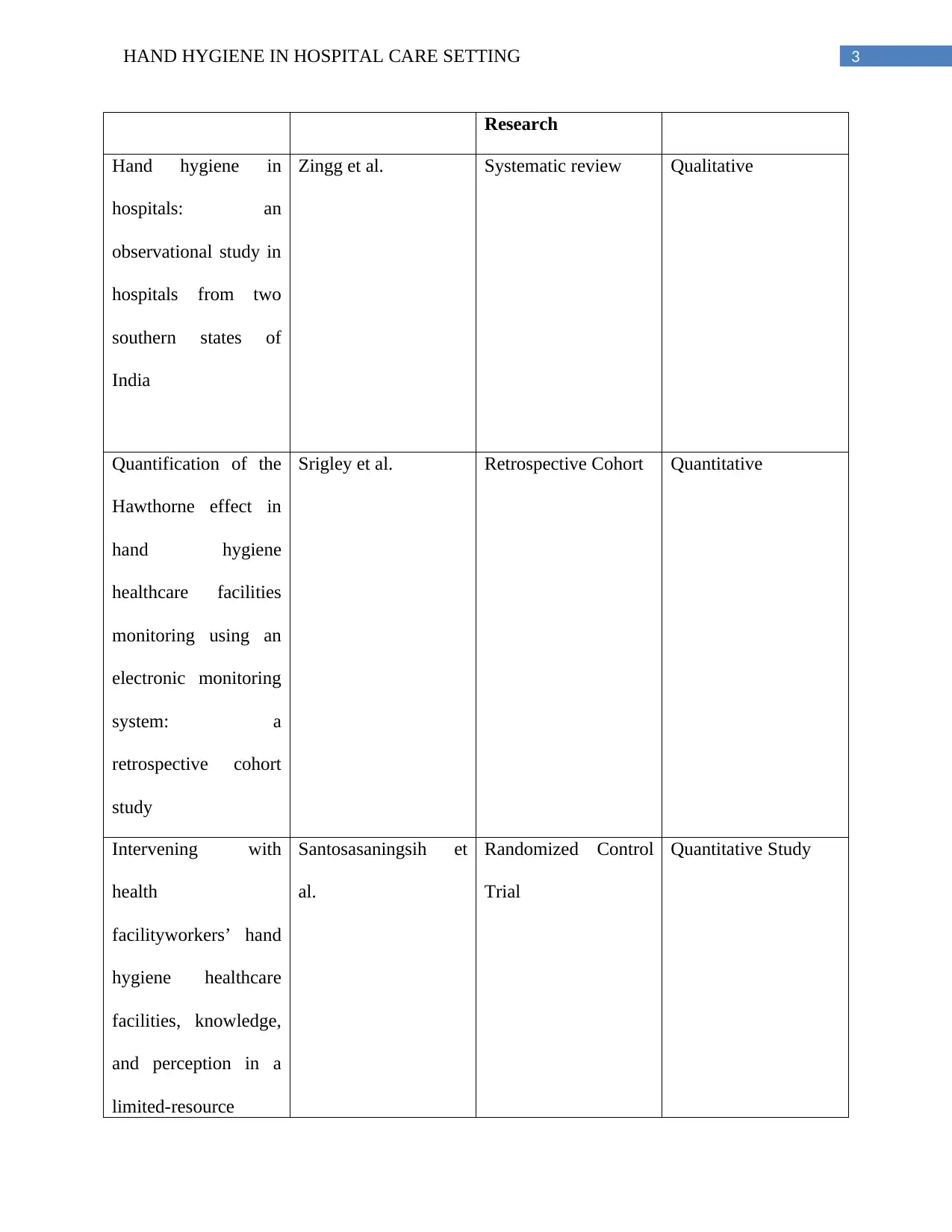
3HAND HYGIENE IN HOSPITAL CARE SETTING
Research
Hand hygiene in
hospitals: an
observational study in
hospitals from two
southern states of
India
Zingg et al. Systematic review Qualitative
Quantification of the
Hawthorne effect in
hand hygiene
healthcare facilities
monitoring using an
electronic monitoring
system: a
retrospective cohort
study
Srigley et al. Retrospective Cohort Quantitative
Intervening with
health
facilityworkers’ hand
hygiene healthcare
facilities, knowledge,
and perception in a
limited-resource
Santosasaningsih et
al.
Randomized Control
Trial
Quantitative Study
Research
Hand hygiene in
hospitals: an
observational study in
hospitals from two
southern states of
India
Zingg et al. Systematic review Qualitative
Quantification of the
Hawthorne effect in
hand hygiene
healthcare facilities
monitoring using an
electronic monitoring
system: a
retrospective cohort
study
Srigley et al. Retrospective Cohort Quantitative
Intervening with
health
facilityworkers’ hand
hygiene healthcare
facilities, knowledge,
and perception in a
limited-resource
Santosasaningsih et
al.
Randomized Control
Trial
Quantitative Study
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
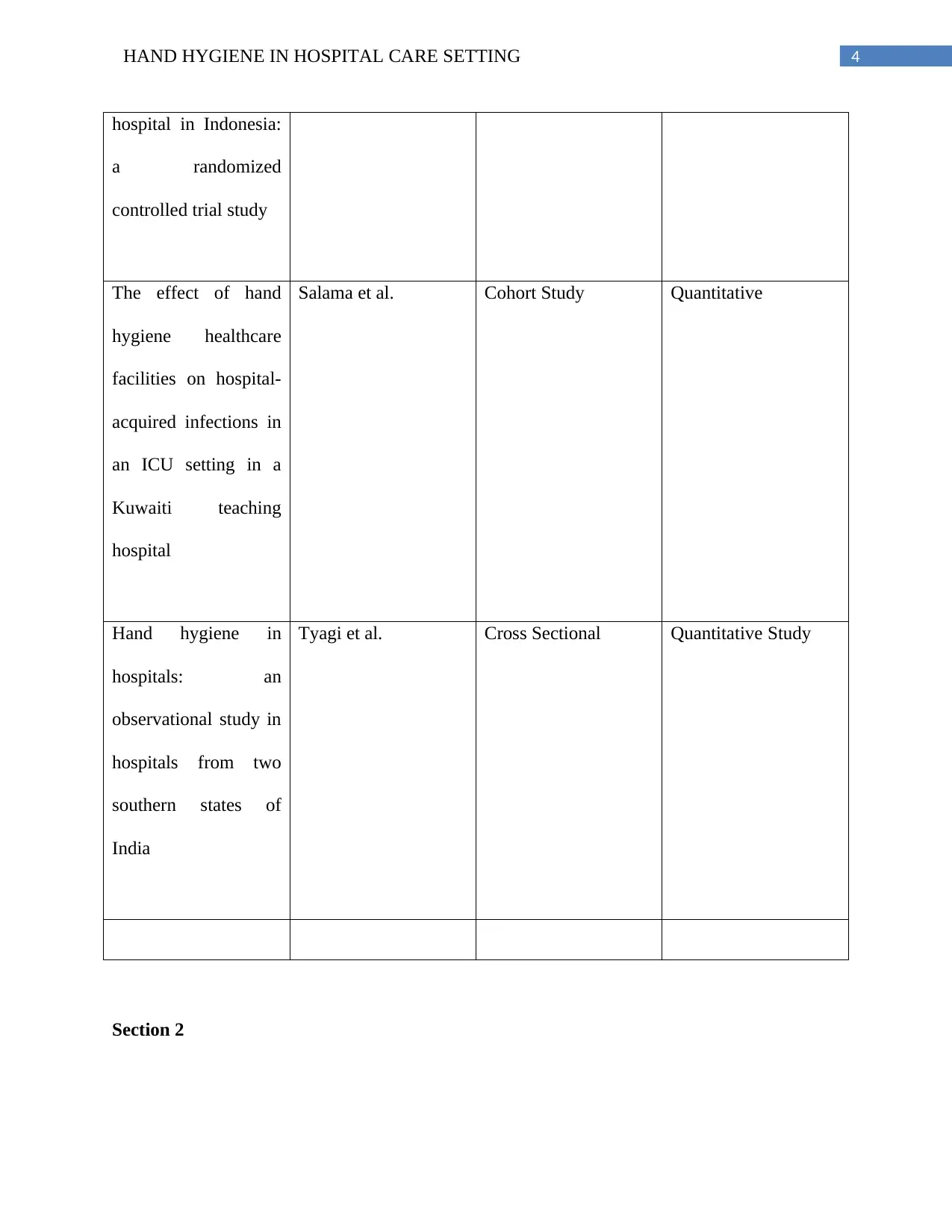
4HAND HYGIENE IN HOSPITAL CARE SETTING
hospital in Indonesia:
a randomized
controlled trial study
The effect of hand
hygiene healthcare
facilities on hospital-
acquired infections in
an ICU setting in a
Kuwaiti teaching
hospital
Salama et al. Cohort Study Quantitative
Hand hygiene in
hospitals: an
observational study in
hospitals from two
southern states of
India
Tyagi et al. Cross Sectional Quantitative Study
Section 2
hospital in Indonesia:
a randomized
controlled trial study
The effect of hand
hygiene healthcare
facilities on hospital-
acquired infections in
an ICU setting in a
Kuwaiti teaching
hospital
Salama et al. Cohort Study Quantitative
Hand hygiene in
hospitals: an
observational study in
hospitals from two
southern states of
India
Tyagi et al. Cross Sectional Quantitative Study
Section 2
5HAND HYGIENE IN HOSPITAL CARE SETTING
The above mentioned studies will help to answer the research question as all the studies
are focusing towards the problem of hand hygiene techniques and practices among the health
facility professionals. Along with this the strengths and weakness of the studies will also help to
take required actions in order to overcome the problems in the health facility settings. In order to
apply the knowledge gathered from the various studies in the evidence based practice it is very
crucial to assess the quality of the literatures as it will help to implement the recommendations
properly (Warren et al., 2016).
The study of Tyagi et al. (2018) discusses about the practice of hand hygiene techniques
and practices in hospitals in the two Indian southern states. The study was performed in the new
born care units of private and public hospitals. The title of the study directly depicts the type of
the study that is cross sectional study. The study was performed among 39 neonatal care units
and 35 labor rooms and the researchers noticed that the practices of hand hygiene among the
health facility professionals in those hospital care settings were low and it was reported that rate
of practicing hand hygiene was better in the private hospital care settings than that of the public
hospitals in the both new born units and labor units. While discussing the study result of the
present study it was reported that in case of new born units the rate of contacts in the private care
settings was higher than that of the public hospital care settings in all the steps of the hand
hygiene (44% vs 12%, p < 0.001) (Tyagi et al., 2018). The component which had lowest
practice rate among the health facility professionals was found to be glove usage and it was
almost 20 per cent of overall cases. Moreover, it was quite evident that before the delivery the
practices of hand washing is very common and the study found that the healthcare facilities with
hand hygiene before delivery was greater in the private hospital care settings than that of the
public hospitals (100% vs 27%, p = 0.012). Moreover the total adherence for maintaining hand
The above mentioned studies will help to answer the research question as all the studies
are focusing towards the problem of hand hygiene techniques and practices among the health
facility professionals. Along with this the strengths and weakness of the studies will also help to
take required actions in order to overcome the problems in the health facility settings. In order to
apply the knowledge gathered from the various studies in the evidence based practice it is very
crucial to assess the quality of the literatures as it will help to implement the recommendations
properly (Warren et al., 2016).
The study of Tyagi et al. (2018) discusses about the practice of hand hygiene techniques
and practices in hospitals in the two Indian southern states. The study was performed in the new
born care units of private and public hospitals. The title of the study directly depicts the type of
the study that is cross sectional study. The study was performed among 39 neonatal care units
and 35 labor rooms and the researchers noticed that the practices of hand hygiene among the
health facility professionals in those hospital care settings were low and it was reported that rate
of practicing hand hygiene was better in the private hospital care settings than that of the public
hospitals in the both new born units and labor units. While discussing the study result of the
present study it was reported that in case of new born units the rate of contacts in the private care
settings was higher than that of the public hospital care settings in all the steps of the hand
hygiene (44% vs 12%, p < 0.001) (Tyagi et al., 2018). The component which had lowest
practice rate among the health facility professionals was found to be glove usage and it was
almost 20 per cent of overall cases. Moreover, it was quite evident that before the delivery the
practices of hand washing is very common and the study found that the healthcare facilities with
hand hygiene before delivery was greater in the private hospital care settings than that of the
public hospitals (100% vs 27%, p = 0.012). Moreover the total adherence for maintaining hand
6HAND HYGIENE IN HOSPITAL CARE SETTING
hygiene during the examinations of the vagina was approximately 35 per cent among both types
of hospitals. The main strength of this study is the huge sample size of study that enhances the
quality of the study. While discussing about the weakness of the study it can be stated that, the
study only assess two sections of the hospital and so the study result may not identical for all the
department of the public or private hospitals (Tyagi et al., 2018).
In the study of Salama et al. (2013) the effect of hand hygiene adherence on hospital-
aquired infections in the ICU care setting in Kuwaiti teaching hospital was examined. In order to
determine the practice of hand hygiene among the health facility workers and its correlation with
the nosocomial infections in the ICU, the researchers performed an interventional study. The
study lasted for 7 months and in this study the protocol of the WHO regarding the hand hygiene
techniques and practices were used before and after the hospital wide hand hygiene campaign in
the hospital care settings. Moreover the researchers also examined the post and pre rate of
nosocomial infections among the staffs, patients of the hospital care setting. The researchers
found significant changes in the post and pre intervention during the study. This showed that the
rate of hand hygiene adherence was enhanced from 42.9 per cent to 61.4 per cent due to the
application of the intervention strategy (p<0.001) (Salama et al., 2013). The hand hygiene
adherence was observed to be most among the nurses during post and pre intervention (49.9 per
cent vs 82.5 per cent respectively). In case of doctors, the hand hygiene adherence was lowest
among the doctors in the post and pre intervention time (38.6 vs. 43.2% respectively). The study
result also reported that increment in the hand hygiene adherence among the nurses also helped
in the improvement of the nosocomial infections among the patients that reduced from 37.2 per
cent pre-intervention to 15.1 post-intervention (P < 0.001). The discussion of the weakness of
the study detected that longer period of time was required to detect more prominent result and
hygiene during the examinations of the vagina was approximately 35 per cent among both types
of hospitals. The main strength of this study is the huge sample size of study that enhances the
quality of the study. While discussing about the weakness of the study it can be stated that, the
study only assess two sections of the hospital and so the study result may not identical for all the
department of the public or private hospitals (Tyagi et al., 2018).
In the study of Salama et al. (2013) the effect of hand hygiene adherence on hospital-
aquired infections in the ICU care setting in Kuwaiti teaching hospital was examined. In order to
determine the practice of hand hygiene among the health facility workers and its correlation with
the nosocomial infections in the ICU, the researchers performed an interventional study. The
study lasted for 7 months and in this study the protocol of the WHO regarding the hand hygiene
techniques and practices were used before and after the hospital wide hand hygiene campaign in
the hospital care settings. Moreover the researchers also examined the post and pre rate of
nosocomial infections among the staffs, patients of the hospital care setting. The researchers
found significant changes in the post and pre intervention during the study. This showed that the
rate of hand hygiene adherence was enhanced from 42.9 per cent to 61.4 per cent due to the
application of the intervention strategy (p<0.001) (Salama et al., 2013). The hand hygiene
adherence was observed to be most among the nurses during post and pre intervention (49.9 per
cent vs 82.5 per cent respectively). In case of doctors, the hand hygiene adherence was lowest
among the doctors in the post and pre intervention time (38.6 vs. 43.2% respectively). The study
result also reported that increment in the hand hygiene adherence among the nurses also helped
in the improvement of the nosocomial infections among the patients that reduced from 37.2 per
cent pre-intervention to 15.1 post-intervention (P < 0.001). The discussion of the weakness of
the study detected that longer period of time was required to detect more prominent result and
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
7HAND HYGIENE IN HOSPITAL CARE SETTING
the strengths of the study is the representation of data in a tabular format that enhances the study
reliability (Salama et al., 2013).
In the study of Zingg et al. (2014) the role of hospital organization and management
along with the prevention of health-care-associated infection was examined by using a
systematic review method. The study analyzed 92 literatures published in between 1996 to 2012
and from the detailed analysis the author succeeded to identify 10 components and they are
mainly control of infection at the hospital level, bed occupancy, workload, and employment of
pool or agency nurses, accessibility of and easiness of access to resources and equipment and
finest ergonomics; suitable use of rules; staffing, education and training, auditing, investigation
and response, multimodal and multidisciplinary inhibition programs that comprise behavioral
change program, engagement of winners; and positive administrative values. Therefore, the
author concluded that management of the above identified factors are associated with the
reduction of health-care-acquired infections and also helps in the improvement of patients’ safety
(Zingg et al., 2014).
The study of Sigrey et al. (2014) examined the presence of Hawthrone effect in the hand
hygiene healthcare facilities. As a part of this the authors used an electronic monitoring system to
observe the effect among the health facility professional. In this retrospective cohort study, the
presence of hand hygiene auditors and increased level of hand hygiene techniques and practices
was examined by using the real-time location system (RTLS). The study result showed that the
hand hygiene rate in dispensers was visible to the auditors and rate of hand hygiene techniques
and practices was higher among the health facility providers who were visible to the auditors and
on the contrary who were not visible to the auditors, they had lower hand hygiene techniques and
practices rate. However, inside the patient room, there were no significant changes regarding the
the strengths of the study is the representation of data in a tabular format that enhances the study
reliability (Salama et al., 2013).
In the study of Zingg et al. (2014) the role of hospital organization and management
along with the prevention of health-care-associated infection was examined by using a
systematic review method. The study analyzed 92 literatures published in between 1996 to 2012
and from the detailed analysis the author succeeded to identify 10 components and they are
mainly control of infection at the hospital level, bed occupancy, workload, and employment of
pool or agency nurses, accessibility of and easiness of access to resources and equipment and
finest ergonomics; suitable use of rules; staffing, education and training, auditing, investigation
and response, multimodal and multidisciplinary inhibition programs that comprise behavioral
change program, engagement of winners; and positive administrative values. Therefore, the
author concluded that management of the above identified factors are associated with the
reduction of health-care-acquired infections and also helps in the improvement of patients’ safety
(Zingg et al., 2014).
The study of Sigrey et al. (2014) examined the presence of Hawthrone effect in the hand
hygiene healthcare facilities. As a part of this the authors used an electronic monitoring system to
observe the effect among the health facility professional. In this retrospective cohort study, the
presence of hand hygiene auditors and increased level of hand hygiene techniques and practices
was examined by using the real-time location system (RTLS). The study result showed that the
hand hygiene rate in dispensers was visible to the auditors and rate of hand hygiene techniques
and practices was higher among the health facility providers who were visible to the auditors and
on the contrary who were not visible to the auditors, they had lower hand hygiene techniques and
practices rate. However, inside the patient room, there were no significant changes regarding the
8HAND HYGIENE IN HOSPITAL CARE SETTING
hand hygiene techniques and practices among the health facilitypractices (Sigrey et al., 2014).
The study lasted for almost 1 year time period and thus it can be stated that the prolonged period
of time can enhance the reliability of the study. On the other hand the limitation of the study is
the fact that the use of RTLS may cause a Hawthorne effect and thereby inflated hand hygiene
event rates compared with baseline data of the study. Another important limitation of the study
was the fact the study was only performed in the solid organ transplant units and so the result
cannot be applied to the all the hospital units (Sigrey et al., 2014).
On the other hand the study of Santosaningsih et al. (2017) examined the level of
knowledge among the health facility in the hospitals of Indonesia. In this study, a randomized
control study method was used by the researchers and the study was performed from May to
October 2017 and the whole study was divided into three segments- pre-intervention,
intervention, and post-intervention phase. During the study process, almost 196 participants were
assessed in the pre-intervention and on the other hand, 88 participants were assessed in the post-
intervention period. The study result showed that after the application of the intervention, the
hand hygiene adherence rate was enhanced considerably in internal medicine (5.2% to 18.5%; P
< 0.001), pediatrics (24.1% to 43.7%; P < 0.001), and obstetrics-gynecology (10.1% to 20.5%; P
< 0.001). Along with this, the knowledge level of the nurses was also improved from 5.6 (SD =
2.1) to 6.2 (SD = 1.9) (P < 0.05) (Santosaningsih et al., 2017). The limited participation of the
health facility professionals can be marked as a limitation of the study and along with this the
Hawthrone effect may also alter the study result. The use of RCT method can be marked as
strength of the study as it reduces the selection bias.
Recommendations
hand hygiene techniques and practices among the health facilitypractices (Sigrey et al., 2014).
The study lasted for almost 1 year time period and thus it can be stated that the prolonged period
of time can enhance the reliability of the study. On the other hand the limitation of the study is
the fact that the use of RTLS may cause a Hawthorne effect and thereby inflated hand hygiene
event rates compared with baseline data of the study. Another important limitation of the study
was the fact the study was only performed in the solid organ transplant units and so the result
cannot be applied to the all the hospital units (Sigrey et al., 2014).
On the other hand the study of Santosaningsih et al. (2017) examined the level of
knowledge among the health facility in the hospitals of Indonesia. In this study, a randomized
control study method was used by the researchers and the study was performed from May to
October 2017 and the whole study was divided into three segments- pre-intervention,
intervention, and post-intervention phase. During the study process, almost 196 participants were
assessed in the pre-intervention and on the other hand, 88 participants were assessed in the post-
intervention period. The study result showed that after the application of the intervention, the
hand hygiene adherence rate was enhanced considerably in internal medicine (5.2% to 18.5%; P
< 0.001), pediatrics (24.1% to 43.7%; P < 0.001), and obstetrics-gynecology (10.1% to 20.5%; P
< 0.001). Along with this, the knowledge level of the nurses was also improved from 5.6 (SD =
2.1) to 6.2 (SD = 1.9) (P < 0.05) (Santosaningsih et al., 2017). The limited participation of the
health facility professionals can be marked as a limitation of the study and along with this the
Hawthrone effect may also alter the study result. The use of RCT method can be marked as
strength of the study as it reduces the selection bias.
Recommendations
9HAND HYGIENE IN HOSPITAL CARE SETTING
Educational programs
Arrangement of awareness workshops
Use of real-time location system (RTLS)
Use of hand gloves during the care process
Sterilization of the equipment
From the above recommendation, it can be stated that educational programs among the health
facility professionals will be executed easily and it may be proven most fruitful as from different
literatures it is observed that poor knowledge of health facility professionals are associated with
hand hygiene infections in the health facility sectors (Phan et al., 2018).
Conclusion
Therefore, it can be concluded that the issue of poor hand hygiene techniques and
practices are very common in the health facility settings and it is very crucial to address this
problem in order to provide a safe health facilities to the patients. From the studies, it is reported
that rate of infections was higher in the public hospitals and proper monitoring can improve the
condition. As a part of recommendation, educational programs in the hospital care setting can be
applied.
Educational programs
Arrangement of awareness workshops
Use of real-time location system (RTLS)
Use of hand gloves during the care process
Sterilization of the equipment
From the above recommendation, it can be stated that educational programs among the health
facility professionals will be executed easily and it may be proven most fruitful as from different
literatures it is observed that poor knowledge of health facility professionals are associated with
hand hygiene infections in the health facility sectors (Phan et al., 2018).
Conclusion
Therefore, it can be concluded that the issue of poor hand hygiene techniques and
practices are very common in the health facility settings and it is very crucial to address this
problem in order to provide a safe health facilities to the patients. From the studies, it is reported
that rate of infections was higher in the public hospitals and proper monitoring can improve the
condition. As a part of recommendation, educational programs in the hospital care setting can be
applied.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10HAND HYGIENE IN HOSPITAL CARE SETTING
References
Anwar, M. M., & Elareed, H. R. (2019). Improvement of hand hygiene healthcare facilities
among health facilityworkers in intensive care units. Journal of Preventive Medicine and
Hygiene, 60(1), E31.
Gwarzo, G. D. (2018). Hand hygiene techniques and practices among health facilityworkers in a
public hospital in North-Western Nigeria. Nigerian Journal of Basic and Clinical
Sciences, 15(2), 109.
Jonker, C., & Othman, M. (2018). Hand hygiene Among Hospital Staff: a Survey of Knowledge,
Attitude, and Practice in a General Hospital in Syria. Jurnal Keperawatan
Indonesia, 21(3), 139-149.
Loftus, M. J., Guitart, C., Tartari, E., Stewardson, A. J., Amer, F., Bellissimo-Rodrigues, F., ... &
Pittet, D. (2019). Hand hygiene in Low-and Middle-Income Countries: A position paper
of the International Society for Infectious Diseases. International Journal of Infectious
Diseases.
Marimuthu, K., Pittet, D., & Harbarth, S. (2014). The effect of improved hand hygiene on
nosocomial MRSA control. Antimicrobial resistance and infection control, 3(1), 34.
McLaws, M. L. (2015). The relationship between hand hygiene and health care-associated
infection: it’s complicated. Infection and drug resistance, 8, 7.
Nadelson, S., & Nadelson, L. S. (2014). Evidence‐based practice article reviews using CASP
tools: a method for teaching EBP. Worldviews on Evidence
‐Based Nursing, 11(5), 344-
346.
References
Anwar, M. M., & Elareed, H. R. (2019). Improvement of hand hygiene healthcare facilities
among health facilityworkers in intensive care units. Journal of Preventive Medicine and
Hygiene, 60(1), E31.
Gwarzo, G. D. (2018). Hand hygiene techniques and practices among health facilityworkers in a
public hospital in North-Western Nigeria. Nigerian Journal of Basic and Clinical
Sciences, 15(2), 109.
Jonker, C., & Othman, M. (2018). Hand hygiene Among Hospital Staff: a Survey of Knowledge,
Attitude, and Practice in a General Hospital in Syria. Jurnal Keperawatan
Indonesia, 21(3), 139-149.
Loftus, M. J., Guitart, C., Tartari, E., Stewardson, A. J., Amer, F., Bellissimo-Rodrigues, F., ... &
Pittet, D. (2019). Hand hygiene in Low-and Middle-Income Countries: A position paper
of the International Society for Infectious Diseases. International Journal of Infectious
Diseases.
Marimuthu, K., Pittet, D., & Harbarth, S. (2014). The effect of improved hand hygiene on
nosocomial MRSA control. Antimicrobial resistance and infection control, 3(1), 34.
McLaws, M. L. (2015). The relationship between hand hygiene and health care-associated
infection: it’s complicated. Infection and drug resistance, 8, 7.
Nadelson, S., & Nadelson, L. S. (2014). Evidence‐based practice article reviews using CASP
tools: a method for teaching EBP. Worldviews on Evidence
‐Based Nursing, 11(5), 344-
346.
11HAND HYGIENE IN HOSPITAL CARE SETTING
Phan, H. T., Tran, H. T. T., Tran, H. T. M., Dinh, A. P. P., Ngo, H. T., Theorell-Haglow, J., &
Gordon, C. J. (2018). An educational intervention to improve hand hygiene healthcare
facilities in Vietnam. BMC infectious diseases, 18(1), 116.
Salama, M. F., Jamal, W. Y., Al Mousa, H., Al-AbdulGhani, K. A., & Rotimi, V. O. (2013). The
effect of hand hygiene healthcare facilities on hospital-acquired infections in an ICU
setting in a Kuwaiti teaching hospital. Journal of infection and public health, 6(1), 27-34.
Santosaningsih, D., Erikawati, D., Santoso, S., Noorhamdani, N., Ratridewi, I., Candradikusuma,
D., ... & Voor, A. F. (2017). Intervening with health facilityworkers’ hand hygiene
healthcare facilities, knowledge, and perception in a limited-resource hospital in
Indonesia: a randomized controlled trial study. Antimicrobial Resistance & Infection
Control, 6(1), 23.
Srigley, J. A., Furness, C. D., Baker, G. R., & Gardam, M. (2014). Quantification of the
Hawthorne effect in hand hygiene healthcare facilities monitoring using an electronic
monitoring system: a retrospective cohort study. BMJ Qual Saf, 23(12), 974-980.
Tyagi, M., Hanson, C., Schellenberg, J., Chamarty, S., & Singh, S. (2018). Hand hygiene in
hospitals: an observational study in hospitals from two southern states of India. BMC
public health, 18(1), 1299.
Warren, J. I., McLaughlin, M., Bardsley, J., Eich, J., Esche, C. A., Kropkowski, L., & Risch, S.
(2016). The strengths and barriers of implementing EBP in health
facilitysystems. Worldviews on Evidence
‐Based Nursing, 13(1), 15-24.
Phan, H. T., Tran, H. T. T., Tran, H. T. M., Dinh, A. P. P., Ngo, H. T., Theorell-Haglow, J., &
Gordon, C. J. (2018). An educational intervention to improve hand hygiene healthcare
facilities in Vietnam. BMC infectious diseases, 18(1), 116.
Salama, M. F., Jamal, W. Y., Al Mousa, H., Al-AbdulGhani, K. A., & Rotimi, V. O. (2013). The
effect of hand hygiene healthcare facilities on hospital-acquired infections in an ICU
setting in a Kuwaiti teaching hospital. Journal of infection and public health, 6(1), 27-34.
Santosaningsih, D., Erikawati, D., Santoso, S., Noorhamdani, N., Ratridewi, I., Candradikusuma,
D., ... & Voor, A. F. (2017). Intervening with health facilityworkers’ hand hygiene
healthcare facilities, knowledge, and perception in a limited-resource hospital in
Indonesia: a randomized controlled trial study. Antimicrobial Resistance & Infection
Control, 6(1), 23.
Srigley, J. A., Furness, C. D., Baker, G. R., & Gardam, M. (2014). Quantification of the
Hawthorne effect in hand hygiene healthcare facilities monitoring using an electronic
monitoring system: a retrospective cohort study. BMJ Qual Saf, 23(12), 974-980.
Tyagi, M., Hanson, C., Schellenberg, J., Chamarty, S., & Singh, S. (2018). Hand hygiene in
hospitals: an observational study in hospitals from two southern states of India. BMC
public health, 18(1), 1299.
Warren, J. I., McLaughlin, M., Bardsley, J., Eich, J., Esche, C. A., Kropkowski, L., & Risch, S.
(2016). The strengths and barriers of implementing EBP in health
facilitysystems. Worldviews on Evidence
‐Based Nursing, 13(1), 15-24.

12HAND HYGIENE IN HOSPITAL CARE SETTING
Zingg, W., Holmes, A., Dettenkofer, M., Goetting, T., Secci, F., Clack, L., ... & Pittet, D. (2015).
Hospital organisation, management, and structure for prevention of health-care-
associated infection: a systematic review and expert consensus. The Lancet Infectious
Diseases, 15(2), 212-224.
Zingg, W., Holmes, A., Dettenkofer, M., Goetting, T., Secci, F., Clack, L., ... & Pittet, D. (2015).
Hospital organisation, management, and structure for prevention of health-care-
associated infection: a systematic review and expert consensus. The Lancet Infectious
Diseases, 15(2), 212-224.
1 out of 13
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





