Introduction Hand washing or hand hygiene
VerifiedAdded on 2022/08/23
|13
|3182
|20
AI Summary
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: HAND HYGIENE
Hand Hygiene
Name of the student
Name of the university
Author’s name
Hand Hygiene
Name of the student
Name of the university
Author’s name
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1HAND HYGIENE
Introduction
Hand washing or hand hygiene is the act of cleaning an individual’s hand for the purpose
of removing various unhygienic substances from the hand. Hand washing has been considered
as a simple but very effective intervention to manage the incidence of hospital-acquired
infections (HAI) and other kinds of infection. HAIs are the kind of diseases which a person
acquires during his/her stay in the hospital. HAI is a very critical disease that has an impact on
millions of people all around the world. Along with the HAIs, there is a high incidence of several
other harmful diseases. HAIs can cause disaster in several forms, such as rise in different other
conditions, increase in the duration of stay in the healthcare facility, can cause physical or mental
disability, as a result, increases the healthcare costs that become a burden on the family
members. Even though some of the diseases are preventable, some take time to get better. People
get HAIs when there is the transmission of the microorganisms that are born in the healthcare
setting and through the direct or indirect touch of contaminated fluids or air and pathogen
carriers such as mosquito or houseflies. According to the study of Marchaim & Kaye (2017),
healthcare professionals usually come in contact with Gram-negative bacilli, S. aureus,
enterococci or C. difficile. As a result, they dirty their hands or gloves, and through that, it is
transferred to other individuals.
Thus, various research papers have agreed on the fact that hand hygiene is like a counter-
strategy to prevent the occurrence of the HAIs. Though even being a simple and effective
strategy, there is a lack of compliance of hand hygiene by the nursing staff, and it is the primary
reason behind the high incidence rate of the HAIs. Thus, this article will be divided into three
parts. Starting with the selection of a range of research studies relevant to the hand hygiene, then
Introduction
Hand washing or hand hygiene is the act of cleaning an individual’s hand for the purpose
of removing various unhygienic substances from the hand. Hand washing has been considered
as a simple but very effective intervention to manage the incidence of hospital-acquired
infections (HAI) and other kinds of infection. HAIs are the kind of diseases which a person
acquires during his/her stay in the hospital. HAI is a very critical disease that has an impact on
millions of people all around the world. Along with the HAIs, there is a high incidence of several
other harmful diseases. HAIs can cause disaster in several forms, such as rise in different other
conditions, increase in the duration of stay in the healthcare facility, can cause physical or mental
disability, as a result, increases the healthcare costs that become a burden on the family
members. Even though some of the diseases are preventable, some take time to get better. People
get HAIs when there is the transmission of the microorganisms that are born in the healthcare
setting and through the direct or indirect touch of contaminated fluids or air and pathogen
carriers such as mosquito or houseflies. According to the study of Marchaim & Kaye (2017),
healthcare professionals usually come in contact with Gram-negative bacilli, S. aureus,
enterococci or C. difficile. As a result, they dirty their hands or gloves, and through that, it is
transferred to other individuals.
Thus, various research papers have agreed on the fact that hand hygiene is like a counter-
strategy to prevent the occurrence of the HAIs. Though even being a simple and effective
strategy, there is a lack of compliance of hand hygiene by the nursing staff, and it is the primary
reason behind the high incidence rate of the HAIs. Thus, this article will be divided into three
parts. Starting with the selection of a range of research studies relevant to the hand hygiene, then
2HAND HYGIENE
selecting one research and doing a critical appraisal using the CASP tool, and finally
recommending different interventions to prevent or reduce the occurrence of HAIs and to
increase the compliance rate of hand hygiene by the healthcare members.
Search Strategy
Search strategy is a method to search for different articles based on a single topic or a research
question. To ease the search process there are key terms, inclusion and exclusion criteria based
upon research articles are searched. To search for the relevant articles it is necessary to form a
research question. The PICO strategy will be used to develop the question.
PICO
P – The problem is the hospital-acquired infections (HAI)
I – Counter strategy is hand hygiene
C - No hand hygiene
O – Reduction in the incidence rate of HAI
Does the hand hygiene intervention have the ability to decrease the incidence rate of HAI by
increasing the compliance of hand hygiene among the healthcare?
There are several online databases like NCBI, PubMed, Cinahl and Google Scholar and official
websites where search strategy is implemented to identify the papers. For the following article
key terms used were hand hygiene, hand washing and hospital-acquired infections. The inclusion
criteria were that the research studies chosen should be relevant to the key terms, should be
published within the last 10 years, and should be published in English language. Exclusion of the
selecting one research and doing a critical appraisal using the CASP tool, and finally
recommending different interventions to prevent or reduce the occurrence of HAIs and to
increase the compliance rate of hand hygiene by the healthcare members.
Search Strategy
Search strategy is a method to search for different articles based on a single topic or a research
question. To ease the search process there are key terms, inclusion and exclusion criteria based
upon research articles are searched. To search for the relevant articles it is necessary to form a
research question. The PICO strategy will be used to develop the question.
PICO
P – The problem is the hospital-acquired infections (HAI)
I – Counter strategy is hand hygiene
C - No hand hygiene
O – Reduction in the incidence rate of HAI
Does the hand hygiene intervention have the ability to decrease the incidence rate of HAI by
increasing the compliance of hand hygiene among the healthcare?
There are several online databases like NCBI, PubMed, Cinahl and Google Scholar and official
websites where search strategy is implemented to identify the papers. For the following article
key terms used were hand hygiene, hand washing and hospital-acquired infections. The inclusion
criteria were that the research studies chosen should be relevant to the key terms, should be
published within the last 10 years, and should be published in English language. Exclusion of the
3HAND HYGIENE
research studies were based on the papers selected older than the last 10 years, and if published
in any other language.
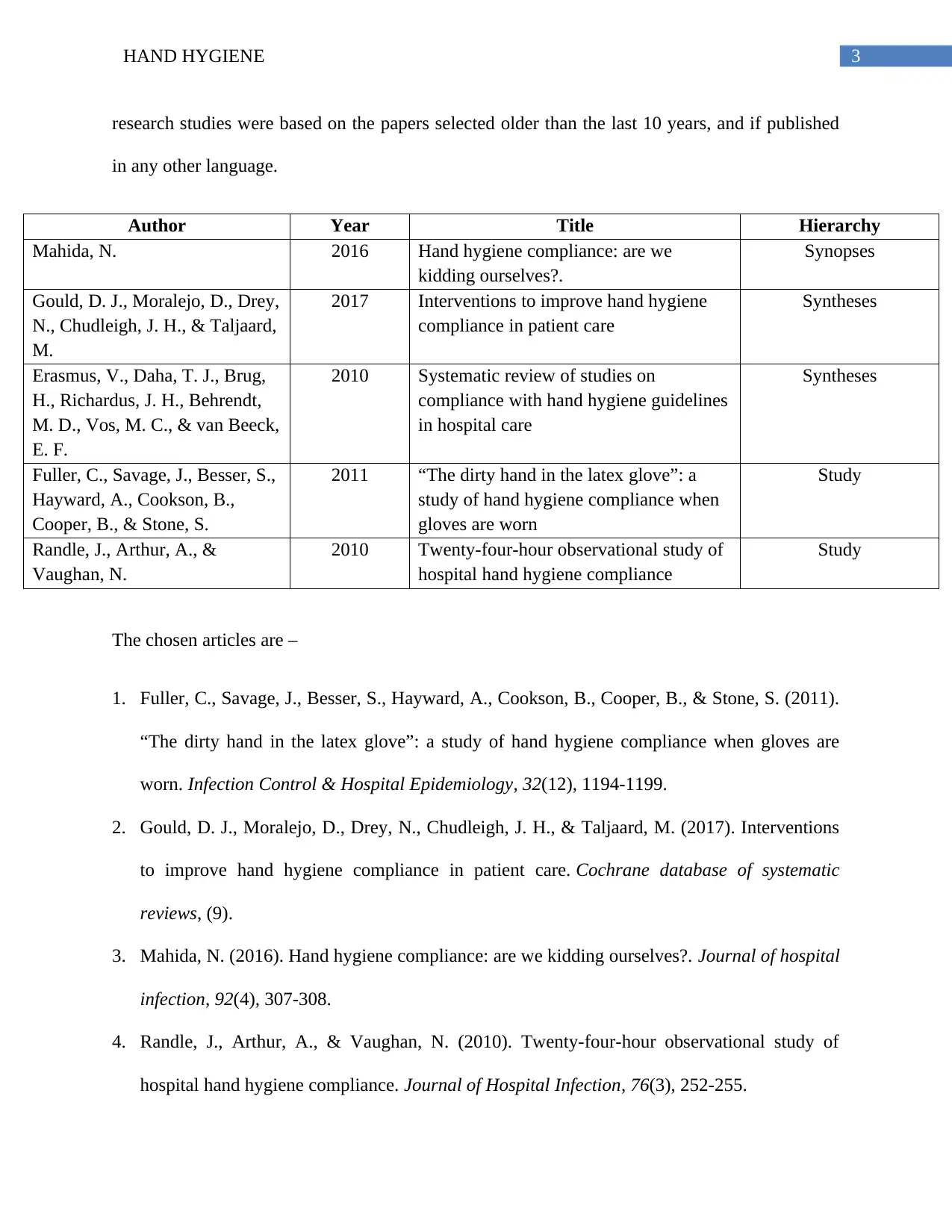
Author Year Title Hierarchy
Mahida, N. 2016 Hand hygiene compliance: are we
kidding ourselves?.
Synopses
Gould, D. J., Moralejo, D., Drey,
N., Chudleigh, J. H., & Taljaard,
M.
2017 Interventions to improve hand hygiene
compliance in patient care
Syntheses
Erasmus, V., Daha, T. J., Brug,
H., Richardus, J. H., Behrendt,
M. D., Vos, M. C., & van Beeck,
E. F.
2010 Systematic review of studies on
compliance with hand hygiene guidelines
in hospital care
Syntheses
Fuller, C., Savage, J., Besser, S.,
Hayward, A., Cookson, B.,
Cooper, B., & Stone, S.
2011 “The dirty hand in the latex glove”: a
study of hand hygiene compliance when
gloves are worn
Study
Randle, J., Arthur, A., &
Vaughan, N.
2010 Twenty-four-hour observational study of
hospital hand hygiene compliance
Study
The chosen articles are –
1. Fuller, C., Savage, J., Besser, S., Hayward, A., Cookson, B., Cooper, B., & Stone, S. (2011).
“The dirty hand in the latex glove”: a study of hand hygiene compliance when gloves are
worn. Infection Control & Hospital Epidemiology, 32(12), 1194-1199.
2. Gould, D. J., Moralejo, D., Drey, N., Chudleigh, J. H., & Taljaard, M. (2017). Interventions
to improve hand hygiene compliance in patient care. Cochrane database of systematic
reviews, (9).
3. Mahida, N. (2016). Hand hygiene compliance: are we kidding ourselves?. Journal of hospital
infection, 92(4), 307-308.
4. Randle, J., Arthur, A., & Vaughan, N. (2010). Twenty-four-hour observational study of
hospital hand hygiene compliance. Journal of Hospital Infection, 76(3), 252-255.
research studies were based on the papers selected older than the last 10 years, and if published
in any other language.
Author Year Title Hierarchy
Mahida, N. 2016 Hand hygiene compliance: are we
kidding ourselves?.
Synopses
Gould, D. J., Moralejo, D., Drey,
N., Chudleigh, J. H., & Taljaard,
M.
2017 Interventions to improve hand hygiene
compliance in patient care
Syntheses
Erasmus, V., Daha, T. J., Brug,
H., Richardus, J. H., Behrendt,
M. D., Vos, M. C., & van Beeck,
E. F.
2010 Systematic review of studies on
compliance with hand hygiene guidelines
in hospital care
Syntheses
Fuller, C., Savage, J., Besser, S.,
Hayward, A., Cookson, B.,
Cooper, B., & Stone, S.
2011 “The dirty hand in the latex glove”: a
study of hand hygiene compliance when
gloves are worn
Study
Randle, J., Arthur, A., &
Vaughan, N.
2010 Twenty-four-hour observational study of
hospital hand hygiene compliance
Study
The chosen articles are –
1. Fuller, C., Savage, J., Besser, S., Hayward, A., Cookson, B., Cooper, B., & Stone, S. (2011).
“The dirty hand in the latex glove”: a study of hand hygiene compliance when gloves are
worn. Infection Control & Hospital Epidemiology, 32(12), 1194-1199.
2. Gould, D. J., Moralejo, D., Drey, N., Chudleigh, J. H., & Taljaard, M. (2017). Interventions
to improve hand hygiene compliance in patient care. Cochrane database of systematic
reviews, (9).
3. Mahida, N. (2016). Hand hygiene compliance: are we kidding ourselves?. Journal of hospital
infection, 92(4), 307-308.
4. Randle, J., Arthur, A., & Vaughan, N. (2010). Twenty-four-hour observational study of
hospital hand hygiene compliance. Journal of Hospital Infection, 76(3), 252-255.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4HAND HYGIENE
5. Erasmus, V., Daha, T. J., Brug, H., Richardus, J. H., Behrendt, M. D., Vos, M. C., & van
Beeck, E. F. (2010). Systematic review of studies on compliance with hand hygiene
guidelines in hospital care. Infection Control & Hospital Epidemiology, 31(3), 283-294.
Reviewing and synthesizing the evidence
Rationale for selecting this articles
There are several factors such as the immune system of the patient, infection management
strategies, and the incidence of the pathogens in the locality on which the hospital-acquired
infection is dependent on. Several other factors increase the risk of hospital-acquired diseases
like old age; long duration stays in the hospital, co-morbidities, immunosuppression, frequent
visits to hospitals and clinics and many more. Though it has been proved that the lack in
compliance with the hand hygiene by several nursing staff and other healthcare members is the
leading cause in the increased risk of hospital-acquired infections.
These research articles were chosen because the following articles are correlated to hand
hygiene topic. There have been several research stating that empty hand or bare hand increases
the risk of HAI and wearing the gloves helps in decreasing the incidence rate of HAI. Though
some papers tried to assess that whether wearing a glove can worsen the hand hygiene and if the
hand hygiene compliance differed when gloves were worn (Fuller et al., 2011). Gould, Moralejo,
Drey, Chudleigh & Taljaard (2017) conducted a literature review to identify different
interventions to increase the hand hygiene compliance during the patient care. In another study,
Randle, Arthur & Vaughan (2010) tried to monitor the compliance level of the hand hygiene in a
group of 823 participants involving healthcare staff, patients and visitors. It was observed that
the compliance level of the medical staff was the lowest, and it was a big concern which warrants
5. Erasmus, V., Daha, T. J., Brug, H., Richardus, J. H., Behrendt, M. D., Vos, M. C., & van
Beeck, E. F. (2010). Systematic review of studies on compliance with hand hygiene
guidelines in hospital care. Infection Control & Hospital Epidemiology, 31(3), 283-294.
Reviewing and synthesizing the evidence
Rationale for selecting this articles
There are several factors such as the immune system of the patient, infection management
strategies, and the incidence of the pathogens in the locality on which the hospital-acquired
infection is dependent on. Several other factors increase the risk of hospital-acquired diseases
like old age; long duration stays in the hospital, co-morbidities, immunosuppression, frequent
visits to hospitals and clinics and many more. Though it has been proved that the lack in
compliance with the hand hygiene by several nursing staff and other healthcare members is the
leading cause in the increased risk of hospital-acquired infections.
These research articles were chosen because the following articles are correlated to hand
hygiene topic. There have been several research stating that empty hand or bare hand increases
the risk of HAI and wearing the gloves helps in decreasing the incidence rate of HAI. Though
some papers tried to assess that whether wearing a glove can worsen the hand hygiene and if the
hand hygiene compliance differed when gloves were worn (Fuller et al., 2011). Gould, Moralejo,
Drey, Chudleigh & Taljaard (2017) conducted a literature review to identify different
interventions to increase the hand hygiene compliance during the patient care. In another study,
Randle, Arthur & Vaughan (2010) tried to monitor the compliance level of the hand hygiene in a
group of 823 participants involving healthcare staff, patients and visitors. It was observed that
the compliance level of the medical staff was the lowest, and it was a big concern which warrants
5HAND HYGIENE
specific future interventions. The following selected research papers will thus, help in answering
the research question and a critical appraisal will also be done with the help of the CASP tool to
answer the question.
specific future interventions. The following selected research papers will thus, help in answering
the research question and a critical appraisal will also be done with the help of the CASP tool to
answer the question.
6HAND HYGIENE
CASP
For the critical appraisal the following article has been chosen –
Erasmus, V., Daha, T. J., Brug, H., Richardus, J. H., Behrendt, M. D., Vos, M. C., & van Beeck,
E. F. (2010). Systematic review of studies on compliance with hand hygiene guidelines in
hospital care. Infection Control & Hospital Epidemiology, 31(3), 283-294.
Did the review address a clearly focused question?
Yes, this selected research paper clearly addresses the PICO research question as this review
tries to assess the prevalence and correlate the compliance and non-compliance level with the
hand hygiene guidelines in hospital care.
Did the authors look for the right type of papers?
Yes, the authors have selected ninety six empirical studies which are based on the general
patient population of industrialized country and published in the English language
Do you think all the important, relevant studies were included?
Yes, the authors have selected ninety six empirical studies which are based on the general
patient population of industrialized country and published in the English language and
compliance was grouped and listed based on correlation.
Did the review’s authors do enough to assess quality of the included studies?
No, the review’s authors reported that the methods were very robust and were generally
reported poorly.
If the results of the review have been combined, was it reasonable to do so?
Yes, the results of the review have been combined by type of healthcare worker before and
after patient contact. But it is very much unclear that if 96 empirical studies were included
CASP
For the critical appraisal the following article has been chosen –
Erasmus, V., Daha, T. J., Brug, H., Richardus, J. H., Behrendt, M. D., Vos, M. C., & van Beeck,
E. F. (2010). Systematic review of studies on compliance with hand hygiene guidelines in
hospital care. Infection Control & Hospital Epidemiology, 31(3), 283-294.
Did the review address a clearly focused question?
Yes, this selected research paper clearly addresses the PICO research question as this review
tries to assess the prevalence and correlate the compliance and non-compliance level with the
hand hygiene guidelines in hospital care.
Did the authors look for the right type of papers?
Yes, the authors have selected ninety six empirical studies which are based on the general
patient population of industrialized country and published in the English language
Do you think all the important, relevant studies were included?
Yes, the authors have selected ninety six empirical studies which are based on the general
patient population of industrialized country and published in the English language and
compliance was grouped and listed based on correlation.
Did the review’s authors do enough to assess quality of the included studies?
No, the review’s authors reported that the methods were very robust and were generally
reported poorly.
If the results of the review have been combined, was it reasonable to do so?
Yes, the results of the review have been combined by type of healthcare worker before and
after patient contact. But it is very much unclear that if 96 empirical studies were included
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7HAND HYGIENE
for the review and 65 studies were from the intensive care units, then from where the authors
collected rest 31 studies.
What are the overall results of the review?
The overall result was observed that the median compliance rate was 40%. It was observed
that the unadjusted compliance rate was lower in the ICU compared to any other unit and was
lower among the healthcare professionals than any other nurses..
How precise are the results?
The precision of the results cannot be assessed based on current day scenario. Though, the
authors have provided with appropriate statistics which determines the precision of results.
Can the results be applied to the local population?
Yes, the results can be applied to the local population even if the data collected are old and
not updated since the results can become a framework and give an idea regarding the
strategies on how to improve compliance in what way in the current day.
Were all important outcomes considered?
Yes, the outcomes were considered.
Are the benefits worth the harms and costs?
There were no benefits from the outcome of this study as it tried to assess the prevalence of
compliance of the hand hygiene guidelines in hospital care.
Recommendation
Different articles have recommended strategies for improving the hand hygiene in the healthcare
system. The strategies are provided based on the recommendations provided by the Centers for
Disease Control and Prevention (CDC) and World Health Organization (WHO) –
for the review and 65 studies were from the intensive care units, then from where the authors
collected rest 31 studies.
What are the overall results of the review?
The overall result was observed that the median compliance rate was 40%. It was observed
that the unadjusted compliance rate was lower in the ICU compared to any other unit and was
lower among the healthcare professionals than any other nurses..
How precise are the results?
The precision of the results cannot be assessed based on current day scenario. Though, the
authors have provided with appropriate statistics which determines the precision of results.
Can the results be applied to the local population?
Yes, the results can be applied to the local population even if the data collected are old and
not updated since the results can become a framework and give an idea regarding the
strategies on how to improve compliance in what way in the current day.
Were all important outcomes considered?
Yes, the outcomes were considered.
Are the benefits worth the harms and costs?
There were no benefits from the outcome of this study as it tried to assess the prevalence of
compliance of the hand hygiene guidelines in hospital care.
Recommendation
Different articles have recommended strategies for improving the hand hygiene in the healthcare
system. The strategies are provided based on the recommendations provided by the Centers for
Disease Control and Prevention (CDC) and World Health Organization (WHO) –
8HAND HYGIENE
If there are any signs of dirty stain such as blood stain or any other body fluid stain, then it is
necessary to wash hands with soap and water or if possible then hands should be washed with
alcohol-based hand rub approach or hands can be washed using plain or antimicrobial soap
and water, especially, after using the toilet and before eating or cooking food and before
giving medicines to any sick patient. If there is a suspicion of being in contact with any kind
of microorganism for instance an outbreak of C. difficile, then hands should be washed with
soap and water.
It is crucial that the healthcare professionals before entering the surgical room, then should
open their ornaments and other accessories which are in contact with their body, as such
accessories like a ring a great source of microorganism.
It is necessary that the healthcare organization should keep a track on the allergies of their
staff. According to the liking ness of the nurses, the healthcare organization should order
hand lotions or creams suitable for the nurses and eventually reduce the incidence of hand
antiseptic or handwashing irritant causing dermatitis.
Wear gloves, if blood or other possibly contagious products, mucous membranes or intact
skin are fairly likely to come into contact with it.
When wearing gloves, change or remove gloves during the patient care from an infected
body site to some other body position in one patient or in the surroundings (along with the
nonintact skin, mucous membrane or medical device).
Certain learning programs such as the information regarding the hand care practices to
decrease the danger of irritant contact dermatitis and other skin damage should be
incorporated in the education programmes for HCWs.
If there are any signs of dirty stain such as blood stain or any other body fluid stain, then it is
necessary to wash hands with soap and water or if possible then hands should be washed with
alcohol-based hand rub approach or hands can be washed using plain or antimicrobial soap
and water, especially, after using the toilet and before eating or cooking food and before
giving medicines to any sick patient. If there is a suspicion of being in contact with any kind
of microorganism for instance an outbreak of C. difficile, then hands should be washed with
soap and water.
It is crucial that the healthcare professionals before entering the surgical room, then should
open their ornaments and other accessories which are in contact with their body, as such
accessories like a ring a great source of microorganism.
It is necessary that the healthcare organization should keep a track on the allergies of their
staff. According to the liking ness of the nurses, the healthcare organization should order
hand lotions or creams suitable for the nurses and eventually reduce the incidence of hand
antiseptic or handwashing irritant causing dermatitis.
Wear gloves, if blood or other possibly contagious products, mucous membranes or intact
skin are fairly likely to come into contact with it.
When wearing gloves, change or remove gloves during the patient care from an infected
body site to some other body position in one patient or in the surroundings (along with the
nonintact skin, mucous membrane or medical device).
Certain learning programs such as the information regarding the hand care practices to
decrease the danger of irritant contact dermatitis and other skin damage should be
incorporated in the education programmes for HCWs.

9HAND HYGIENE
Conclusion
There are still several countries where the lack of hand hygiene compliance is causing the
people admitted in the hospitals to stay more than they are expected to be as a result of the HAI.
In order to prevent people from getting the HAIs, it is necessary to initiate a global-wide national
strategy that will improve the compliance rate of hand hygiene. It is also essential to involve new
study materials for the nursing students in order to direct their focus towards the compliance of
hand hygiene. As earlier mentioned, hand hygiene is a beneficial but straightforward strategy to
counter the impact of HAI. A strategic plan should be addressed for changes in hand hygiene to
flourish in an overall health & infection control policy. There are three significant steps for the
successful implementation and full compliance of the hand hygiene. It is educating people about
the necessity of hand hygiene, imposing strict guidelines in the healthcare sector regarding hand
hygiene and implementing hand hygiene in the practices.
Conclusion
There are still several countries where the lack of hand hygiene compliance is causing the
people admitted in the hospitals to stay more than they are expected to be as a result of the HAI.
In order to prevent people from getting the HAIs, it is necessary to initiate a global-wide national
strategy that will improve the compliance rate of hand hygiene. It is also essential to involve new
study materials for the nursing students in order to direct their focus towards the compliance of
hand hygiene. As earlier mentioned, hand hygiene is a beneficial but straightforward strategy to
counter the impact of HAI. A strategic plan should be addressed for changes in hand hygiene to
flourish in an overall health & infection control policy. There are three significant steps for the
successful implementation and full compliance of the hand hygiene. It is educating people about
the necessity of hand hygiene, imposing strict guidelines in the healthcare sector regarding hand
hygiene and implementing hand hygiene in the practices.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
10HAND HYGIENE
References
Allegranzi, B., Sax, H., & Pittet, D. (2013). Hand hygiene and healthcare system change within
multi-modal promotion: a narrative review. Journal of Hospital Infection, 83, S3-S10.
Chen, L. F., Carriker, C., Staheli, R., Isaacs, P., Elliott, B., Miller, B. A., ... & Rhodes, L. (2013).
Observing and improving hand hygiene compliance implementation and refinement of an
electronic-assisted direct-observer hand hygiene audit program. Infection Control &
Hospital Epidemiology, 34(2), 207-210.
Erasmus, V., Daha, T. J., Brug, H., Richardus, J. H., Behrendt, M. D., Vos, M. C., & van Beeck,
E. F. (2010). Systematic review of studies on compliance with hand hygiene guidelines in
hospital care. Infection Control & Hospital Epidemiology, 31(3), 283-294.
Fuller, C., Savage, J., Besser, S., Hayward, A., Cookson, B., Cooper, B., & Stone, S. (2011).
“The dirty hand in the latex glove”: a study of hand hygiene compliance when gloves are
worn. Infection Control & Hospital Epidemiology, 32(12), 1194-1199.
Gould, D. J., Moralejo, D., Drey, N., Chudleigh, J. H., & Taljaard, M. (2017). Interventions to
improve hand hygiene compliance in patient care. Cochrane database of systematic
reviews, (9).
Hufton, G. C., Levchenko, O. I., & Fernie, G. R. (2011). U.S. Patent No. 7,898,407. Washington,
DC: U.S. Patent and Trademark Office.
Mahida, N. (2016). Hand hygiene compliance: are we kidding ourselves?. Journal of hospital
infection, 92(4), 307-308.
References
Allegranzi, B., Sax, H., & Pittet, D. (2013). Hand hygiene and healthcare system change within
multi-modal promotion: a narrative review. Journal of Hospital Infection, 83, S3-S10.
Chen, L. F., Carriker, C., Staheli, R., Isaacs, P., Elliott, B., Miller, B. A., ... & Rhodes, L. (2013).
Observing and improving hand hygiene compliance implementation and refinement of an
electronic-assisted direct-observer hand hygiene audit program. Infection Control &
Hospital Epidemiology, 34(2), 207-210.
Erasmus, V., Daha, T. J., Brug, H., Richardus, J. H., Behrendt, M. D., Vos, M. C., & van Beeck,
E. F. (2010). Systematic review of studies on compliance with hand hygiene guidelines in
hospital care. Infection Control & Hospital Epidemiology, 31(3), 283-294.
Fuller, C., Savage, J., Besser, S., Hayward, A., Cookson, B., Cooper, B., & Stone, S. (2011).
“The dirty hand in the latex glove”: a study of hand hygiene compliance when gloves are
worn. Infection Control & Hospital Epidemiology, 32(12), 1194-1199.
Gould, D. J., Moralejo, D., Drey, N., Chudleigh, J. H., & Taljaard, M. (2017). Interventions to
improve hand hygiene compliance in patient care. Cochrane database of systematic
reviews, (9).
Hufton, G. C., Levchenko, O. I., & Fernie, G. R. (2011). U.S. Patent No. 7,898,407. Washington,
DC: U.S. Patent and Trademark Office.
Mahida, N. (2016). Hand hygiene compliance: are we kidding ourselves?. Journal of hospital
infection, 92(4), 307-308.
11HAND HYGIENE
Marchaim, D., & Kaye, K. (2017). Infections and antimicrobial resistance in the intensive care
unit: Epidemiology and prevention. Prieiga per internetą https://www. uptodate.
com/contents/infectionsand-antimicrobial-resistance-in-the-intensive-care-unit-
epidemiology-and-prevention.
Marra, A. R., Guastelli, L. R., de Araújo, C. M. P., dos Santos, J. L. S., Lamblet, L. C. R., Silva,
M., ... & Barbosa, L. (2010). Positive deviance a new strategy for improving hand
hygiene compliance. Infection Control & Hospital Epidemiology, 31(1), 12-20.
McGuckin, M., Waterman, R., & Govednik, J. (2009). Hand hygiene compliance rates in the
United States—a one-year multicenter collaboration using product/volume usage
measurement and feedback. American Journal of Medical Quality, 24(3), 205-213.
Nair, S. S., Hanumantappa, R., Hiremath, S. G., Siraj, M. A., & Raghunath, P. (2014).
Knowledge, attitude, and practice of hand hygiene among medical and nursing students at
a tertiary health care centre in Raichur, India. ISRN preventive medicine, 2014.
Pfoh, E., Dy, S., & Engineer, C. (2013). Interventions to improve hand hygiene compliance:
brief update review. Making health care safer II: An updated critical analysis of the
evidence for patient safety practices.
Randle, J., Arthur, A., & Vaughan, N. (2010). Twenty-four-hour observational study of hospital
hand hygiene compliance. Journal of Hospital Infection, 76(3), 252-255.
Willmott, M., Nicholson, A., Busse, H., MacArthur, G. J., Brookes, S., & Campbell, R. (2016).
Effectiveness of hand hygiene interventions in reducing illness absence among children
Marchaim, D., & Kaye, K. (2017). Infections and antimicrobial resistance in the intensive care
unit: Epidemiology and prevention. Prieiga per internetą https://www. uptodate.
com/contents/infectionsand-antimicrobial-resistance-in-the-intensive-care-unit-
epidemiology-and-prevention.
Marra, A. R., Guastelli, L. R., de Araújo, C. M. P., dos Santos, J. L. S., Lamblet, L. C. R., Silva,
M., ... & Barbosa, L. (2010). Positive deviance a new strategy for improving hand
hygiene compliance. Infection Control & Hospital Epidemiology, 31(1), 12-20.
McGuckin, M., Waterman, R., & Govednik, J. (2009). Hand hygiene compliance rates in the
United States—a one-year multicenter collaboration using product/volume usage
measurement and feedback. American Journal of Medical Quality, 24(3), 205-213.
Nair, S. S., Hanumantappa, R., Hiremath, S. G., Siraj, M. A., & Raghunath, P. (2014).
Knowledge, attitude, and practice of hand hygiene among medical and nursing students at
a tertiary health care centre in Raichur, India. ISRN preventive medicine, 2014.
Pfoh, E., Dy, S., & Engineer, C. (2013). Interventions to improve hand hygiene compliance:
brief update review. Making health care safer II: An updated critical analysis of the
evidence for patient safety practices.
Randle, J., Arthur, A., & Vaughan, N. (2010). Twenty-four-hour observational study of hospital
hand hygiene compliance. Journal of Hospital Infection, 76(3), 252-255.
Willmott, M., Nicholson, A., Busse, H., MacArthur, G. J., Brookes, S., & Campbell, R. (2016).
Effectiveness of hand hygiene interventions in reducing illness absence among children
12HAND HYGIENE
in educational settings: a systematic review and meta-analysis. Archives of disease in
childhood, 101(1), 42-50.
World Health Organization. (2016). WHO guidelines on hand hygiene in health care. First
Global Patient Safety Challenge. Clean Care is Safer Care. Geneva: WHO; 2009.
in educational settings: a systematic review and meta-analysis. Archives of disease in
childhood, 101(1), 42-50.
World Health Organization. (2016). WHO guidelines on hand hygiene in health care. First
Global Patient Safety Challenge. Clean Care is Safer Care. Geneva: WHO; 2009.
1 out of 13
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





