Improving Fruit and Vegetable Intake for a Balanced Diet
VerifiedAdded on 2022/12/19
|10
|2631
|89
AI Summary
This article discusses strategies to improve fruit and vegetable consumption for a balanced diet. It provides tips on incorporating whole fruits and vegetables into meals and gradually increasing intake. It also addresses the importance of socioeconomic status and cultural background in dietary choices.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: HEALTH AND ILLNESS
HEALTH AND ILLNESS
Name of the Student:
Name of the University:
Author note:
HEALTH AND ILLNESS
Name of the Student:
Name of the University:
Author note:
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1HEALTH AND ILLNESS
Section A
I am required to consume 5 to 6 servings of vegetables and 2 servings of fruits every
day. Hence, this would include 2 medium apples or 4 small fruits like kiwis, plums, 3 to 6 cups
of cooked orange or green vegetables, unsalted canned or dried beans, raw salad vegetables
(Eat for Health, 2019).
My intake of fruits and vegetables is grossly deficient in terms of the recommendations
outlined by the Australian Dietary Guidelines. Hence, I must undertake key strategies to improve
consumption of the same. I can incorporate whole fruits like apples, apricots, kiwis and plums,
especially during my breakfast along with my cereal as well as during my evening snack hours
where I crave for something convenient and sweet (Eat for Health, 2019). Further to gradually
accustom my palate to the change, instead of a direct consumption of a whole fruit, I can
accommodate half a piece of the same and increase the amounts gradually. I can also increase
my fruit intake by consuming juices and smoothies between meals but must limit the same since
it may result in excessive sugar consumption (Michels et al., 2016). To improve my vegetable
intake, especially during major meals like my lunch and dinner, I must incorporate 3 to 6 cups of
cooked green leafy vegetables like spinach, broccoli, lettuce, as well as orange colored
vegetables like pumpkins and squashes (Eat for Health, 2019). Alternatively, I can also increase
the same by incorporating canned corn or beans as well as starchy vegetables but must limit my
consumption since these are high in salt and carbohydrates (Di et al., 2016). For both fruits and
vegetables, I must remember to not remove the peels since it will ensure adequate fiber, vitamin
and mineral intake. Just like fruits, to accustom my taste towards vegetable consumption, I must
Section A
I am required to consume 5 to 6 servings of vegetables and 2 servings of fruits every
day. Hence, this would include 2 medium apples or 4 small fruits like kiwis, plums, 3 to 6 cups
of cooked orange or green vegetables, unsalted canned or dried beans, raw salad vegetables
(Eat for Health, 2019).
My intake of fruits and vegetables is grossly deficient in terms of the recommendations
outlined by the Australian Dietary Guidelines. Hence, I must undertake key strategies to improve
consumption of the same. I can incorporate whole fruits like apples, apricots, kiwis and plums,
especially during my breakfast along with my cereal as well as during my evening snack hours
where I crave for something convenient and sweet (Eat for Health, 2019). Further to gradually
accustom my palate to the change, instead of a direct consumption of a whole fruit, I can
accommodate half a piece of the same and increase the amounts gradually. I can also increase
my fruit intake by consuming juices and smoothies between meals but must limit the same since
it may result in excessive sugar consumption (Michels et al., 2016). To improve my vegetable
intake, especially during major meals like my lunch and dinner, I must incorporate 3 to 6 cups of
cooked green leafy vegetables like spinach, broccoli, lettuce, as well as orange colored
vegetables like pumpkins and squashes (Eat for Health, 2019). Alternatively, I can also increase
the same by incorporating canned corn or beans as well as starchy vegetables but must limit my
consumption since these are high in salt and carbohydrates (Di et al., 2016). For both fruits and
vegetables, I must remember to not remove the peels since it will ensure adequate fiber, vitamin
and mineral intake. Just like fruits, to accustom my taste towards vegetable consumption, I must
2HEALTH AND ILLNESS
incorporate the same in gradual, small amounts and mix them with my meat based dishes or in
pureed form so that I can reap the nutritional benefits in feasible ways (Morgan et al., 2016).
Section B
I scored a point of 3, which indicates a poor adherence to nutritional recommendations.
As per this quiz, I am not meeting my recommended intake of consuming reduced fat milk and
milk products in my diet (Eat for Health, 2019). It can be observed (Appendix 1) that most of my
consumption of milk and milk products are obtained from full fat sources during breakfast and
in the evening, along with my breakfast cereals and beverages like coffee. Hence, to correct the
same, I must replace the full fat milk with low fat sources like skimmed milk to be consumed
with my breakfast cereal and coffee. Further, I also engage in consumption of high fat milk
products like butter and mayonnaise during my lunch and dinner in the form of sandwiches and
salads. Hence to correct the same, I must replace them with low fat, yogurt based dressings or
sandwich spreads or opt for low fat cheeses like feta. The second change and dietary strategy
which I must look into is my inability to meet recommended consumption of whole grains like
whole grain breads, pastas and cereals (Eat for Health, 2019). As per my food recall, it is evident
that my intake of grains mostly comprise of refined varieties in the form of breakfast cereals,
sandwiches with white bread and refined noodles. Hence, to correct the same, I must replace
sugary breakfast cereals with whole grains like oats and replace white bread in my sandwiches
with whole grain or whole wheat bread. While cooking and consuming rice, noodles or pasta, I
must seek to obtain varieties made with whole grains or whole wheat.
incorporate the same in gradual, small amounts and mix them with my meat based dishes or in
pureed form so that I can reap the nutritional benefits in feasible ways (Morgan et al., 2016).
Section B
I scored a point of 3, which indicates a poor adherence to nutritional recommendations.
As per this quiz, I am not meeting my recommended intake of consuming reduced fat milk and
milk products in my diet (Eat for Health, 2019). It can be observed (Appendix 1) that most of my
consumption of milk and milk products are obtained from full fat sources during breakfast and
in the evening, along with my breakfast cereals and beverages like coffee. Hence, to correct the
same, I must replace the full fat milk with low fat sources like skimmed milk to be consumed
with my breakfast cereal and coffee. Further, I also engage in consumption of high fat milk
products like butter and mayonnaise during my lunch and dinner in the form of sandwiches and
salads. Hence to correct the same, I must replace them with low fat, yogurt based dressings or
sandwich spreads or opt for low fat cheeses like feta. The second change and dietary strategy
which I must look into is my inability to meet recommended consumption of whole grains like
whole grain breads, pastas and cereals (Eat for Health, 2019). As per my food recall, it is evident
that my intake of grains mostly comprise of refined varieties in the form of breakfast cereals,
sandwiches with white bread and refined noodles. Hence, to correct the same, I must replace
sugary breakfast cereals with whole grains like oats and replace white bread in my sandwiches
with whole grain or whole wheat bread. While cooking and consuming rice, noodles or pasta, I
must seek to obtain varieties made with whole grains or whole wheat.
3HEALTH AND ILLNESS
Section C
A key socioeconomic determinant of health is economic stability and the socioeconomic
condition in which an individual belongs to. Taking insights from the same, the academic article
by Adler, Glymour and Fielding (2016), was chosen which discusses extensively on the need
for healthcare policies to address social determinants of health for the purpose of reducing health
disparities and inequalities in healthcare. This academic article has been chosen since the authors
have reported that poor socioeconomic conditions among individuals result in inequalities in
terms of obtaining healthcare resources. Indeed, poor socioeconomic conditions reduces and
individuals capacity to afford required healthcare services, resources and nutritious food
resources. Taking insights from the author as well as relating to my own life, I can completely
relate to the effect socioeconomic status has on my intake of a balanced diet. During stages when
I am in possession of low financial resources or have run out of adequate money, I am unable to
afford nutritious food sources like green leafy vegetables, lean meats or fruits and instead revert
to consumption of inadequate meals resulting in my inability to adhere to the Australian Dietary
Guidelines (Eat for Health, 2019). Hence to improve my engagement with the dietary
recommendations as well as improve my nutritional status as per my socioeconomic status, I
must enlighten myself on cost effective strategies of food preparation methods and buying
grocery produce which will not only allow me to obtain nutritious food sources but also support
my in maintaining optimum nutritional status (McInerney et al., 2016).
Similarly, culture is a key determinant in the achievement of positive health outcomes,
since an individual’s unique cultural, ethnic and linguistic background determines his or her
understanding of available healthcare resources, consumption of food as well as communication
Section C
A key socioeconomic determinant of health is economic stability and the socioeconomic
condition in which an individual belongs to. Taking insights from the same, the academic article
by Adler, Glymour and Fielding (2016), was chosen which discusses extensively on the need
for healthcare policies to address social determinants of health for the purpose of reducing health
disparities and inequalities in healthcare. This academic article has been chosen since the authors
have reported that poor socioeconomic conditions among individuals result in inequalities in
terms of obtaining healthcare resources. Indeed, poor socioeconomic conditions reduces and
individuals capacity to afford required healthcare services, resources and nutritious food
resources. Taking insights from the author as well as relating to my own life, I can completely
relate to the effect socioeconomic status has on my intake of a balanced diet. During stages when
I am in possession of low financial resources or have run out of adequate money, I am unable to
afford nutritious food sources like green leafy vegetables, lean meats or fruits and instead revert
to consumption of inadequate meals resulting in my inability to adhere to the Australian Dietary
Guidelines (Eat for Health, 2019). Hence to improve my engagement with the dietary
recommendations as well as improve my nutritional status as per my socioeconomic status, I
must enlighten myself on cost effective strategies of food preparation methods and buying
grocery produce which will not only allow me to obtain nutritious food sources but also support
my in maintaining optimum nutritional status (McInerney et al., 2016).
Similarly, culture is a key determinant in the achievement of positive health outcomes,
since an individual’s unique cultural, ethnic and linguistic background determines his or her
understanding of available healthcare resources, consumption of food as well as communication
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4HEALTH AND ILLNESS
with healthcare professionals and participants in the community. Taking insights from the same,
the article by Park et al., (2018) has been selected since it explored extensively on how usage of
cultural competence among health professionals aids in the removal of health disparities and
improves equities in healthcare accessibility especially among culturally diverse individuals who
are less proficient in English. Indeed, such individuals whose native language may not be
English, will not only find it difficult to comprehend healthcare information but will also face
issues in communicating their needs or receiving cultural specific treatment from health
professionals (Lundin et al., 2016). Hence, this necessitates the usage of cultural competence
where health professionals must be sensitive to the needs of ethnically diverse patients and
empathetically understand their needs. Further, an individual’s unique cultural background
determines his or her personal dietary choices. Taking insights from my personal experiences,
my skills of English language are adequate to aid in my understanding of the Australian Dietary
Guidelines (Eat for Health, 2019). However, it is my unique cultural and ethnic background
which often interferes in my adherence to the recommendations. I belong to primarily an Asian
cultural background where high consumption of starchy grains and sweets has been part of my
family traditions. For this reason, I find it extremely difficult to limit the consumption of the
same, as per the Australian Dietary Guidelines. However, considering that a balanced diet is
needed to achieve positive health outcomes, I must seek to incorporate principles of the same to
the best of my efforts. Considering my difficulties and cultural background, I can achieve the
same by consulting a nutritionist, who can suggest me strategies on a balanced diet consumption,
using strategies of empathy, patient listening and cultural competence (Brown, 2019).
with healthcare professionals and participants in the community. Taking insights from the same,
the article by Park et al., (2018) has been selected since it explored extensively on how usage of
cultural competence among health professionals aids in the removal of health disparities and
improves equities in healthcare accessibility especially among culturally diverse individuals who
are less proficient in English. Indeed, such individuals whose native language may not be
English, will not only find it difficult to comprehend healthcare information but will also face
issues in communicating their needs or receiving cultural specific treatment from health
professionals (Lundin et al., 2016). Hence, this necessitates the usage of cultural competence
where health professionals must be sensitive to the needs of ethnically diverse patients and
empathetically understand their needs. Further, an individual’s unique cultural background
determines his or her personal dietary choices. Taking insights from my personal experiences,
my skills of English language are adequate to aid in my understanding of the Australian Dietary
Guidelines (Eat for Health, 2019). However, it is my unique cultural and ethnic background
which often interferes in my adherence to the recommendations. I belong to primarily an Asian
cultural background where high consumption of starchy grains and sweets has been part of my
family traditions. For this reason, I find it extremely difficult to limit the consumption of the
same, as per the Australian Dietary Guidelines. However, considering that a balanced diet is
needed to achieve positive health outcomes, I must seek to incorporate principles of the same to
the best of my efforts. Considering my difficulties and cultural background, I can achieve the
same by consulting a nutritionist, who can suggest me strategies on a balanced diet consumption,
using strategies of empathy, patient listening and cultural competence (Brown, 2019).
5HEALTH AND ILLNESS
Appendices
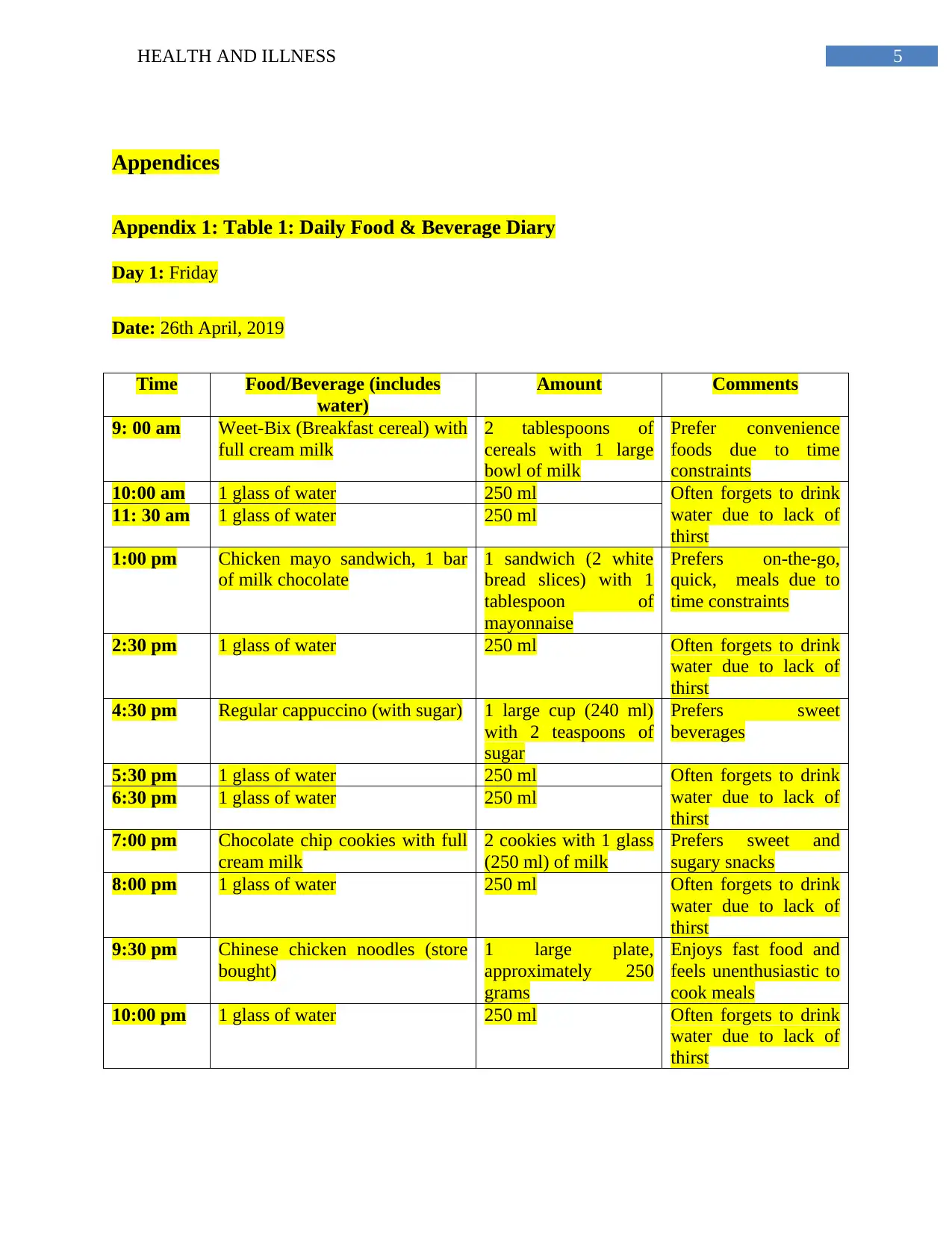
Appendix 1: Table 1: Daily Food & Beverage Diary
Day 1: Friday
Date: 26th April, 2019
Time Food/Beverage (includes
water)
Amount Comments
9: 00 am Weet-Bix (Breakfast cereal) with
full cream milk
2 tablespoons of
cereals with 1 large
bowl of milk
Prefer convenience
foods due to time
constraints
10:00 am 1 glass of water 250 ml Often forgets to drink
water due to lack of
thirst
11: 30 am 1 glass of water 250 ml
1:00 pm Chicken mayo sandwich, 1 bar
of milk chocolate
1 sandwich (2 white
bread slices) with 1
tablespoon of
mayonnaise
Prefers on-the-go,
quick, meals due to
time constraints
2:30 pm 1 glass of water 250 ml Often forgets to drink
water due to lack of
thirst
4:30 pm Regular cappuccino (with sugar) 1 large cup (240 ml)
with 2 teaspoons of
sugar
Prefers sweet
beverages
5:30 pm 1 glass of water 250 ml Often forgets to drink
water due to lack of
thirst
6:30 pm 1 glass of water 250 ml
7:00 pm Chocolate chip cookies with full
cream milk
2 cookies with 1 glass
(250 ml) of milk
Prefers sweet and
sugary snacks
8:00 pm 1 glass of water 250 ml Often forgets to drink
water due to lack of
thirst
9:30 pm Chinese chicken noodles (store
bought)
1 large plate,
approximately 250
grams
Enjoys fast food and
feels unenthusiastic to
cook meals
10:00 pm 1 glass of water 250 ml Often forgets to drink
water due to lack of
thirst
Appendices
Appendix 1: Table 1: Daily Food & Beverage Diary
Day 1: Friday
Date: 26th April, 2019
Time Food/Beverage (includes
water)
Amount Comments
9: 00 am Weet-Bix (Breakfast cereal) with
full cream milk
2 tablespoons of
cereals with 1 large
bowl of milk
Prefer convenience
foods due to time
constraints
10:00 am 1 glass of water 250 ml Often forgets to drink
water due to lack of
thirst
11: 30 am 1 glass of water 250 ml
1:00 pm Chicken mayo sandwich, 1 bar
of milk chocolate
1 sandwich (2 white
bread slices) with 1
tablespoon of
mayonnaise
Prefers on-the-go,
quick, meals due to
time constraints
2:30 pm 1 glass of water 250 ml Often forgets to drink
water due to lack of
thirst
4:30 pm Regular cappuccino (with sugar) 1 large cup (240 ml)
with 2 teaspoons of
sugar
Prefers sweet
beverages
5:30 pm 1 glass of water 250 ml Often forgets to drink
water due to lack of
thirst
6:30 pm 1 glass of water 250 ml
7:00 pm Chocolate chip cookies with full
cream milk
2 cookies with 1 glass
(250 ml) of milk
Prefers sweet and
sugary snacks
8:00 pm 1 glass of water 250 ml Often forgets to drink
water due to lack of
thirst
9:30 pm Chinese chicken noodles (store
bought)
1 large plate,
approximately 250
grams
Enjoys fast food and
feels unenthusiastic to
cook meals
10:00 pm 1 glass of water 250 ml Often forgets to drink
water due to lack of
thirst
6HEALTH AND ILLNESS
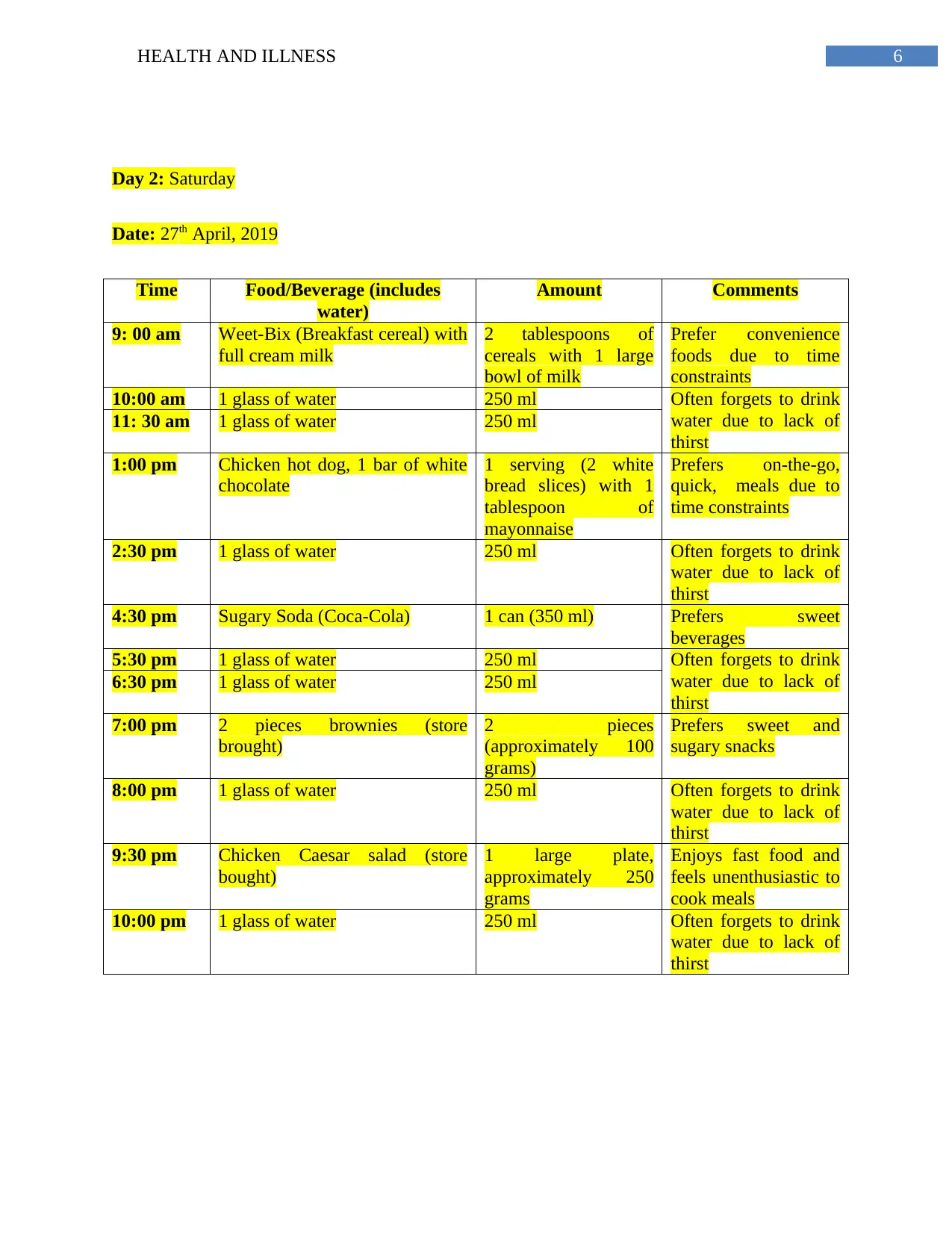
Day 2: Saturday
Date: 27th April, 2019
Time Food/Beverage (includes
water)
Amount Comments
9: 00 am Weet-Bix (Breakfast cereal) with
full cream milk
2 tablespoons of
cereals with 1 large
bowl of milk
Prefer convenience
foods due to time
constraints
10:00 am 1 glass of water 250 ml Often forgets to drink
water due to lack of
thirst
11: 30 am 1 glass of water 250 ml
1:00 pm Chicken hot dog, 1 bar of white
chocolate
1 serving (2 white
bread slices) with 1
tablespoon of
mayonnaise
Prefers on-the-go,
quick, meals due to
time constraints
2:30 pm 1 glass of water 250 ml Often forgets to drink
water due to lack of
thirst
4:30 pm Sugary Soda (Coca-Cola) 1 can (350 ml) Prefers sweet
beverages
5:30 pm 1 glass of water 250 ml Often forgets to drink
water due to lack of
thirst
6:30 pm 1 glass of water 250 ml
7:00 pm 2 pieces brownies (store
brought)
2 pieces
(approximately 100
grams)
Prefers sweet and
sugary snacks
8:00 pm 1 glass of water 250 ml Often forgets to drink
water due to lack of
thirst
9:30 pm Chicken Caesar salad (store
bought)
1 large plate,
approximately 250
grams
Enjoys fast food and
feels unenthusiastic to
cook meals
10:00 pm 1 glass of water 250 ml Often forgets to drink
water due to lack of
thirst
Day 2: Saturday
Date: 27th April, 2019
Time Food/Beverage (includes
water)
Amount Comments
9: 00 am Weet-Bix (Breakfast cereal) with
full cream milk
2 tablespoons of
cereals with 1 large
bowl of milk
Prefer convenience
foods due to time
constraints
10:00 am 1 glass of water 250 ml Often forgets to drink
water due to lack of
thirst
11: 30 am 1 glass of water 250 ml
1:00 pm Chicken hot dog, 1 bar of white
chocolate
1 serving (2 white
bread slices) with 1
tablespoon of
mayonnaise
Prefers on-the-go,
quick, meals due to
time constraints
2:30 pm 1 glass of water 250 ml Often forgets to drink
water due to lack of
thirst
4:30 pm Sugary Soda (Coca-Cola) 1 can (350 ml) Prefers sweet
beverages
5:30 pm 1 glass of water 250 ml Often forgets to drink
water due to lack of
thirst
6:30 pm 1 glass of water 250 ml
7:00 pm 2 pieces brownies (store
brought)
2 pieces
(approximately 100
grams)
Prefers sweet and
sugary snacks
8:00 pm 1 glass of water 250 ml Often forgets to drink
water due to lack of
thirst
9:30 pm Chicken Caesar salad (store
bought)
1 large plate,
approximately 250
grams
Enjoys fast food and
feels unenthusiastic to
cook meals
10:00 pm 1 glass of water 250 ml Often forgets to drink
water due to lack of
thirst
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7HEALTH AND ILLNESS
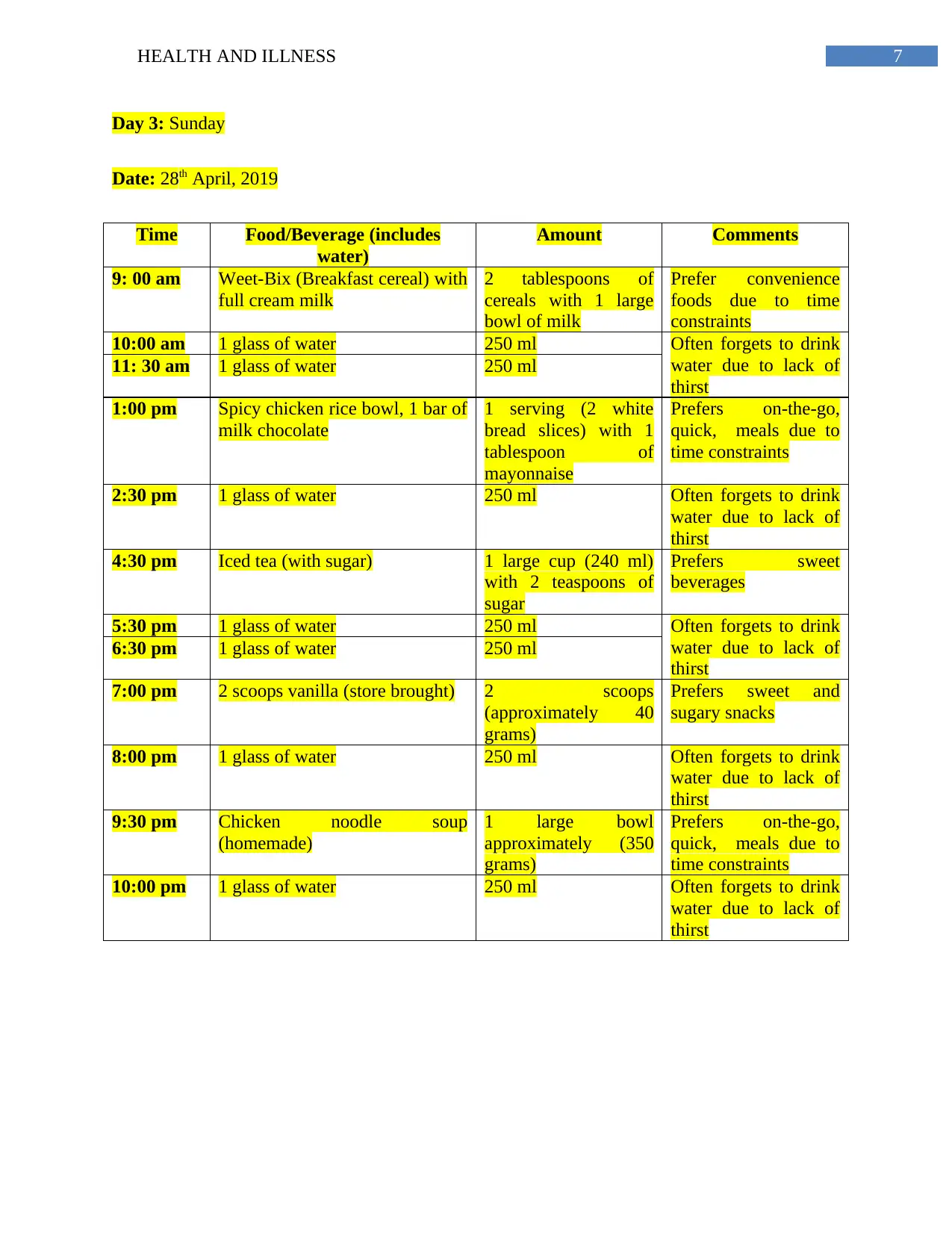
Day 3: Sunday
Date: 28th April, 2019
Time Food/Beverage (includes
water)
Amount Comments
9: 00 am Weet-Bix (Breakfast cereal) with
full cream milk
2 tablespoons of
cereals with 1 large
bowl of milk
Prefer convenience
foods due to time
constraints
10:00 am 1 glass of water 250 ml Often forgets to drink
water due to lack of
thirst
11: 30 am 1 glass of water 250 ml
1:00 pm Spicy chicken rice bowl, 1 bar of
milk chocolate
1 serving (2 white
bread slices) with 1
tablespoon of
mayonnaise
Prefers on-the-go,
quick, meals due to
time constraints
2:30 pm 1 glass of water 250 ml Often forgets to drink
water due to lack of
thirst
4:30 pm Iced tea (with sugar) 1 large cup (240 ml)
with 2 teaspoons of
sugar
Prefers sweet
beverages
5:30 pm 1 glass of water 250 ml Often forgets to drink
water due to lack of
thirst
6:30 pm 1 glass of water 250 ml
7:00 pm 2 scoops vanilla (store brought) 2 scoops
(approximately 40
grams)
Prefers sweet and
sugary snacks
8:00 pm 1 glass of water 250 ml Often forgets to drink
water due to lack of
thirst
9:30 pm Chicken noodle soup
(homemade)
1 large bowl
approximately (350
grams)
Prefers on-the-go,
quick, meals due to
time constraints
10:00 pm 1 glass of water 250 ml Often forgets to drink
water due to lack of
thirst
Day 3: Sunday
Date: 28th April, 2019
Time Food/Beverage (includes
water)
Amount Comments
9: 00 am Weet-Bix (Breakfast cereal) with
full cream milk
2 tablespoons of
cereals with 1 large
bowl of milk
Prefer convenience
foods due to time
constraints
10:00 am 1 glass of water 250 ml Often forgets to drink
water due to lack of
thirst
11: 30 am 1 glass of water 250 ml
1:00 pm Spicy chicken rice bowl, 1 bar of
milk chocolate
1 serving (2 white
bread slices) with 1
tablespoon of
mayonnaise
Prefers on-the-go,
quick, meals due to
time constraints
2:30 pm 1 glass of water 250 ml Often forgets to drink
water due to lack of
thirst
4:30 pm Iced tea (with sugar) 1 large cup (240 ml)
with 2 teaspoons of
sugar
Prefers sweet
beverages
5:30 pm 1 glass of water 250 ml Often forgets to drink
water due to lack of
thirst
6:30 pm 1 glass of water 250 ml
7:00 pm 2 scoops vanilla (store brought) 2 scoops
(approximately 40
grams)
Prefers sweet and
sugary snacks
8:00 pm 1 glass of water 250 ml Often forgets to drink
water due to lack of
thirst
9:30 pm Chicken noodle soup
(homemade)
1 large bowl
approximately (350
grams)
Prefers on-the-go,
quick, meals due to
time constraints
10:00 pm 1 glass of water 250 ml Often forgets to drink
water due to lack of
thirst
8HEALTH AND ILLNESS
References
Adler, N. E., Glymour, M. M., & Fielding, J. (2016). Addressing social determinants of health
and health inequalities. Jama, 316(16), 1641-1642.
Brown, K. (2019). Clean Eating: How the Language of Diet Culture Assigns Moral Judgements
to Food Choices.
Di, J. N., Monica, D., Cullen, K. W., Pérez-Escamilla, R., Gray, H. L., & Sikorskii, A. (2016).
Differences in Fruit and Vegetable Intake by Race/Ethnicity and by Hispanic Origin and
Nativity Among Women in the Special Supplemental Nutrition Program for Women,
Infants, and Children, 2015. Preventing chronic disease, 13, E115-E115.
Eat for Health. (2019). Australian Guidelines SUMMARY Dietary. Retrieved from
https://www.eatforhealth.gov.au/sites/default/files/content/The%20Guidelines/
n55a_australian_dietary_guidelines_summary_131014_1.pdf.
Lundin, C., Hadziabdic, E., & Hjelm, K. (2018). Language interpretation conditions and
boundaries in multilingual and multicultural emergency healthcare. BMC international
health and human rights, 18(1), 23.
McInerney, M., Csizmadi, I., Friedenreich, C. M., Uribe, F. A., Nettel-Aguirre, A., McLaren,
L., ... & McCormack, G. R. (2016). Associations between the neighbourhood food
environment, neighbourhood socioeconomic status, and diet quality: An observational
study. BMC Public Health, 16(1), 984.
References
Adler, N. E., Glymour, M. M., & Fielding, J. (2016). Addressing social determinants of health
and health inequalities. Jama, 316(16), 1641-1642.
Brown, K. (2019). Clean Eating: How the Language of Diet Culture Assigns Moral Judgements
to Food Choices.
Di, J. N., Monica, D., Cullen, K. W., Pérez-Escamilla, R., Gray, H. L., & Sikorskii, A. (2016).
Differences in Fruit and Vegetable Intake by Race/Ethnicity and by Hispanic Origin and
Nativity Among Women in the Special Supplemental Nutrition Program for Women,
Infants, and Children, 2015. Preventing chronic disease, 13, E115-E115.
Eat for Health. (2019). Australian Guidelines SUMMARY Dietary. Retrieved from
https://www.eatforhealth.gov.au/sites/default/files/content/The%20Guidelines/
n55a_australian_dietary_guidelines_summary_131014_1.pdf.
Lundin, C., Hadziabdic, E., & Hjelm, K. (2018). Language interpretation conditions and
boundaries in multilingual and multicultural emergency healthcare. BMC international
health and human rights, 18(1), 23.
McInerney, M., Csizmadi, I., Friedenreich, C. M., Uribe, F. A., Nettel-Aguirre, A., McLaren,
L., ... & McCormack, G. R. (2016). Associations between the neighbourhood food
environment, neighbourhood socioeconomic status, and diet quality: An observational
study. BMC Public Health, 16(1), 984.
9HEALTH AND ILLNESS
Michels, N., De Henauw, S., Beghin, L., Cuenca-García, M., Gonzalez-Gross, M., Hallstrom, L.,
... & Molnar, D. (2016). Ready-to-eat cereals improve nutrient, milk and fruit intake at
breakfast in European adolescents. European journal of nutrition, 55(2), 771-779.
Morgan, E. H., Vatucawaqa, P., Snowdon, W., Worsley, A., Dangour, A. D., & Lock, K. (2016).
Factors influencing fruit and vegetable intake among urban Fijians: A qualitative
study. Appetite, 101, 114-118.
Park, L., Schwei, R. J., Xiong, P., & Jacobs, E. A. (2018). Addressing cultural determinants of
health for Latino and Hmong Patients with limited english proficiency: practical
strategies to reduce health disparities. Journal of racial and ethnic health
disparities, 5(3), 536-544.
Michels, N., De Henauw, S., Beghin, L., Cuenca-García, M., Gonzalez-Gross, M., Hallstrom, L.,
... & Molnar, D. (2016). Ready-to-eat cereals improve nutrient, milk and fruit intake at
breakfast in European adolescents. European journal of nutrition, 55(2), 771-779.
Morgan, E. H., Vatucawaqa, P., Snowdon, W., Worsley, A., Dangour, A. D., & Lock, K. (2016).
Factors influencing fruit and vegetable intake among urban Fijians: A qualitative
study. Appetite, 101, 114-118.
Park, L., Schwei, R. J., Xiong, P., & Jacobs, E. A. (2018). Addressing cultural determinants of
health for Latino and Hmong Patients with limited english proficiency: practical
strategies to reduce health disparities. Journal of racial and ethnic health
disparities, 5(3), 536-544.
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





