Legal and Ethical Frameworks in Nursing: A Comprehensive Analysis
VerifiedAdded on 2022/09/18
|10
|2712
|22
Report
AI Summary
This assignment explores the legal and ethical frameworks governing health and social care practices. It examines key legislation like the Health and Social Care Act 2012, the Equality Act 2010, and the Mental Health Act 1983, highlighting their impact on healthcare professionals. The report delves into ethical dilemmas, such as those related to patient autonomy in dementia care and the principles of beneficence and non-maleficence, illustrated with practical examples. It also discusses the professional standards of practice, including effective communication, risk management, and respecting patient confidentiality. Furthermore, it explores the role of NHS England in regulating the national system of government and the importance of safeguarding vulnerable groups through acts like the Safeguarding Vulnerable Group Act 2006 and the Mental Capacity Act 2005, emphasizing the need for ethical conduct and adherence to legal requirements in healthcare settings. The assignment also includes a practical application section with real-world examples of how the professional standards are applied.
Running head: NURSING
Leaflet
Leaflet
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1
NURSING
Legislature, the executive and the judiciary set the legal and policy landscape for health
and social care practitioners and the settings they work within
The Health and Social Care Act 2012 introduced the first legal duties of the health
and social care professionals about the health inequalities. This Act enlisted specific duties
for the healthcare bodies like Department of Health, Public Health England, NHs England
and Clinical commissioning Groups (NHS England 2019). The Equality Act 2010 helps in
the establishment of the equality duties for the public sector healthcare organizations that aim
to integrate the consideration of advancement for healthcare equality in day-to-day practice.
The main duties that are covered in the Equality Act 2010 specify the professional standards
of practice under the workplace settings of the health and social care practitioners. This
guidance is given to support the Clinical commissioning Groups (CCGs) and NHS England
in order to help them meeting their legal duties (NHS England 2019). The supporting
legislation includes the Social Value Act (2012) and it requires the public sector
commissioners like the local bodies and other health sectors to consider the social, economic
and environmental well-being of the healthcare service users (NHS England 2019).
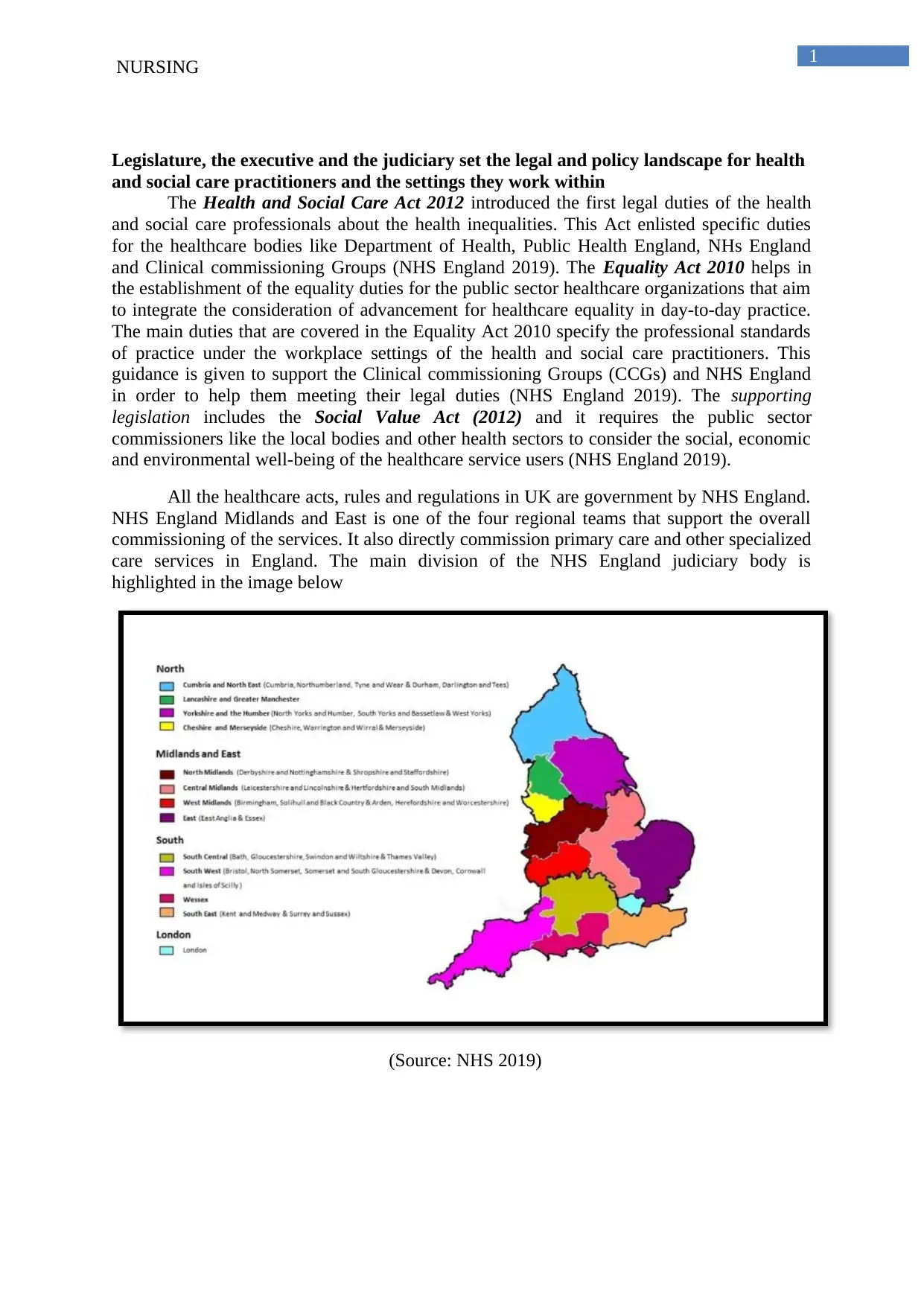
All the healthcare acts, rules and regulations in UK are government by NHS England.
NHS England Midlands and East is one of the four regional teams that support the overall
commissioning of the services. It also directly commission primary care and other specialized
care services in England. The main division of the NHS England judiciary body is
highlighted in the image below
(Source: NHS 2019)
NURSING
Legislature, the executive and the judiciary set the legal and policy landscape for health
and social care practitioners and the settings they work within
The Health and Social Care Act 2012 introduced the first legal duties of the health
and social care professionals about the health inequalities. This Act enlisted specific duties
for the healthcare bodies like Department of Health, Public Health England, NHs England
and Clinical commissioning Groups (NHS England 2019). The Equality Act 2010 helps in
the establishment of the equality duties for the public sector healthcare organizations that aim
to integrate the consideration of advancement for healthcare equality in day-to-day practice.
The main duties that are covered in the Equality Act 2010 specify the professional standards
of practice under the workplace settings of the health and social care practitioners. This
guidance is given to support the Clinical commissioning Groups (CCGs) and NHS England
in order to help them meeting their legal duties (NHS England 2019). The supporting
legislation includes the Social Value Act (2012) and it requires the public sector
commissioners like the local bodies and other health sectors to consider the social, economic
and environmental well-being of the healthcare service users (NHS England 2019).
All the healthcare acts, rules and regulations in UK are government by NHS England.
NHS England Midlands and East is one of the four regional teams that support the overall
commissioning of the services. It also directly commission primary care and other specialized
care services in England. The main division of the NHS England judiciary body is
highlighted in the image below
(Source: NHS 2019)
2
NURSING
Relationship between key legislation and national policy relevant to health and care
settings
National laws and regulations are designed under constitutional and legal framework
for any particular country. Laws designed for the implementation of the healthcare
environment are designed on scientific findings and assessment while taking into economic,
social and environmental consideration of that country. Primary legislations that is laws
typically set forth policy statement or other object, include the scope of the legislation and its
relationship with the existing laws. In other words, it can be stated that the laws and
regulations are regarded as a consequences of policy making however, their implementation
or lack of the same might lead to a series of further development of policy. New laws and
regulations might also be important in order to address the emerging environment and other
healthcare problems. International treaties and associated instruments that are related to
global problems help to facilitate the policy-making that helps in achieving the harmonized
approach, nationally or internationally over the issue that is at stake (World Health
Organization 2019).
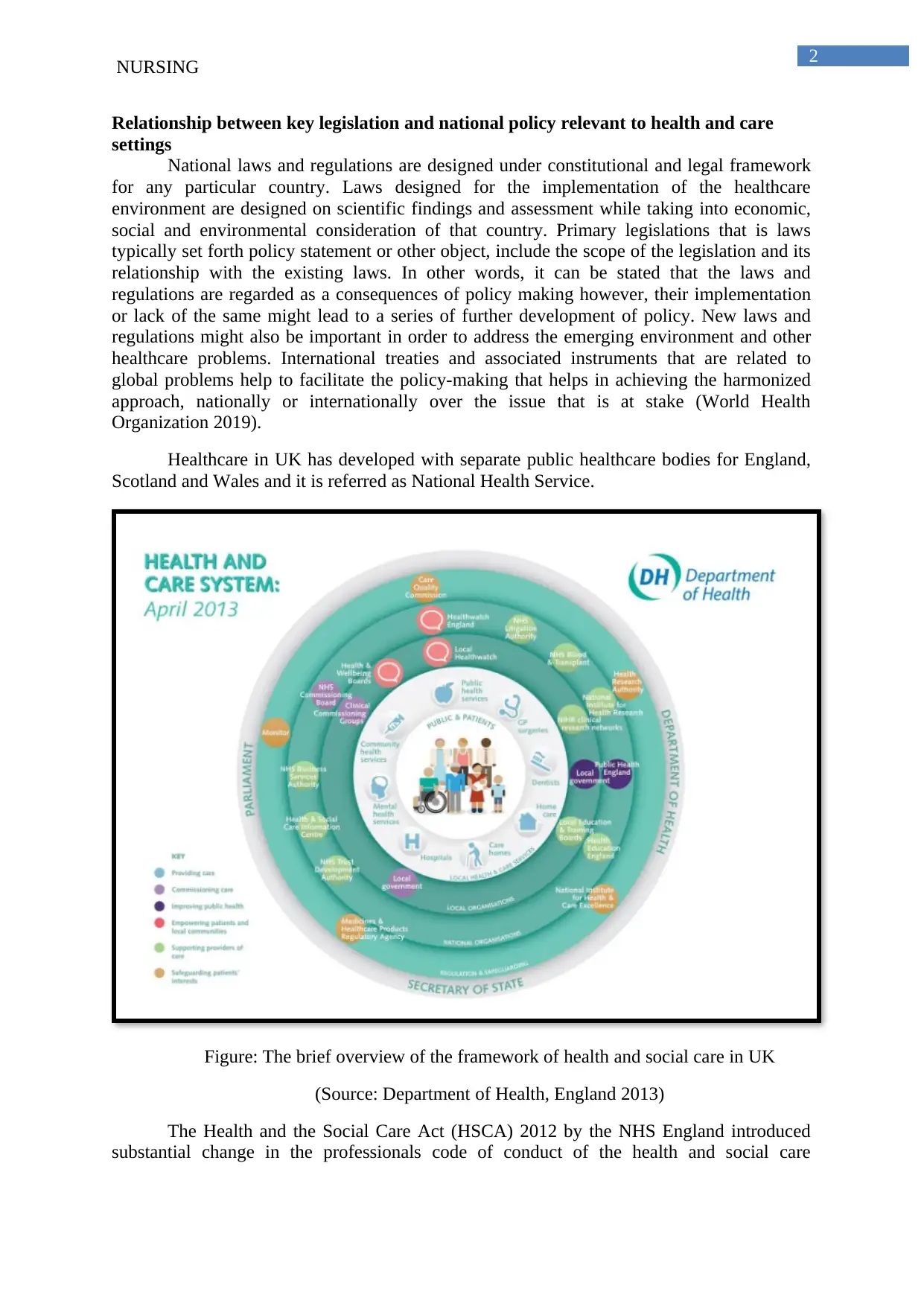
Healthcare in UK has developed with separate public healthcare bodies for England,
Scotland and Wales and it is referred as National Health Service.
Figure: The brief overview of the framework of health and social care in UK
(Source: Department of Health, England 2013)
The Health and the Social Care Act (HSCA) 2012 by the NHS England introduced
substantial change in the professionals code of conduct of the health and social care
NURSING
Relationship between key legislation and national policy relevant to health and care
settings
National laws and regulations are designed under constitutional and legal framework
for any particular country. Laws designed for the implementation of the healthcare
environment are designed on scientific findings and assessment while taking into economic,
social and environmental consideration of that country. Primary legislations that is laws
typically set forth policy statement or other object, include the scope of the legislation and its
relationship with the existing laws. In other words, it can be stated that the laws and
regulations are regarded as a consequences of policy making however, their implementation
or lack of the same might lead to a series of further development of policy. New laws and
regulations might also be important in order to address the emerging environment and other
healthcare problems. International treaties and associated instruments that are related to
global problems help to facilitate the policy-making that helps in achieving the harmonized
approach, nationally or internationally over the issue that is at stake (World Health
Organization 2019).
Healthcare in UK has developed with separate public healthcare bodies for England,
Scotland and Wales and it is referred as National Health Service.
Figure: The brief overview of the framework of health and social care in UK
(Source: Department of Health, England 2013)
The Health and the Social Care Act (HSCA) 2012 by the NHS England introduced
substantial change in the professionals code of conduct of the health and social care
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3
NURSING
professionals. The perspective of the Health and Social Care Act as proposed in UK’s
legislative board s highlighted below
Clinically led commissioning
The regulation of the provider in order to support innovative service
Raising greater voice for the parents
New focus over the public health
Increasing the key accountability areas of the local and the national bodies
Streamlines armed-length bodies
Promoting improvement in the overall quality of heal and social care
Effective tackling of the prevailing healthcare inequalities
Initiating proper integration of health and social care services
Increasing the overall choice of availing care
Conducting Effective Health and Social Care research
Providing proper education and training to the healthcare staffs
Reconfiguration of the new services
(Government of UK 2012)
The HSCA 2012 lead to the foundation of the Clinical Commissioning Groups (CCG) and
this was followed by the abolition of the primary care trust and strategic health care
authorities in the year 2013 (NHS England 2019).
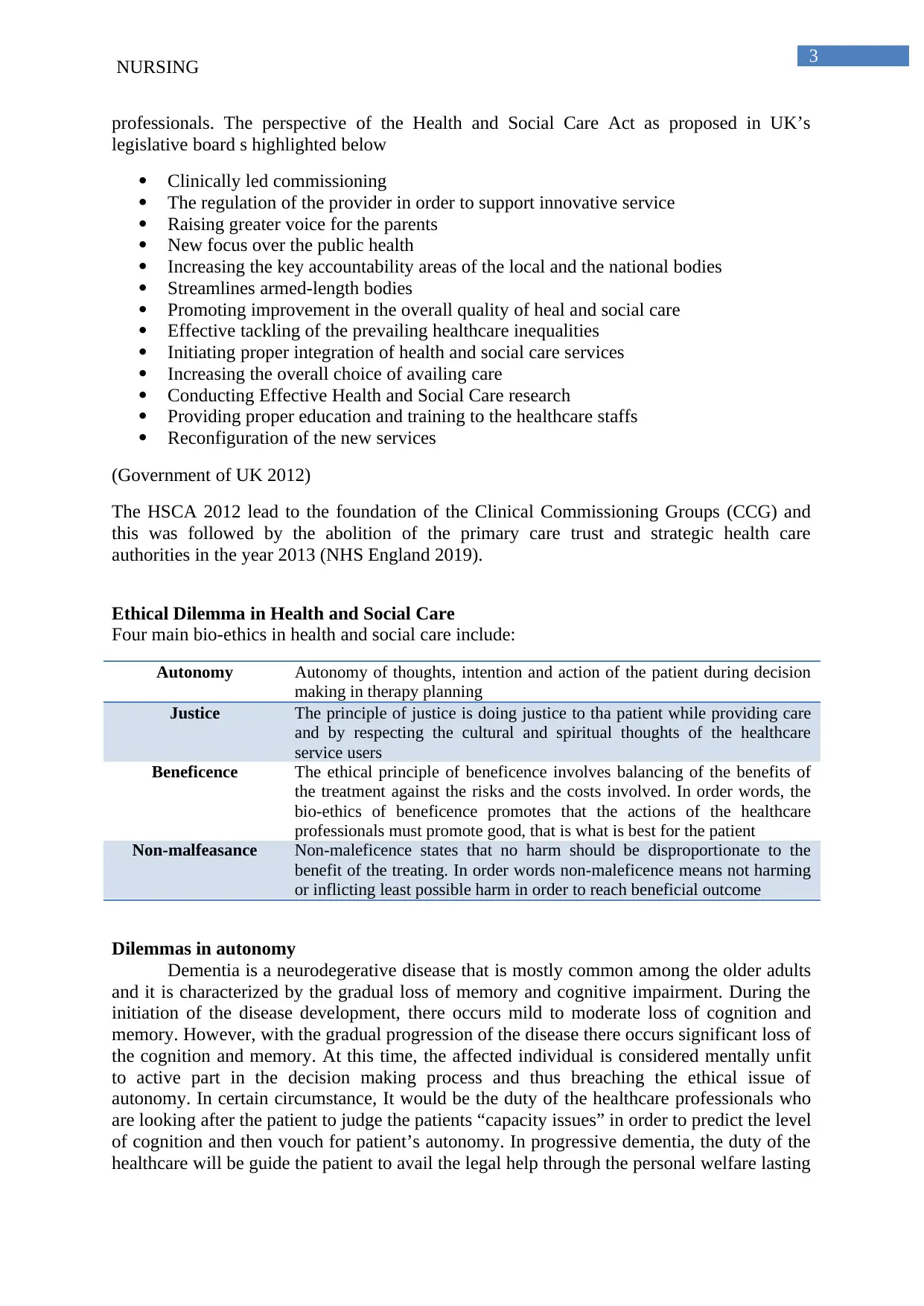
Ethical Dilemma in Health and Social Care
Four main bio-ethics in health and social care include:
Autonomy Autonomy of thoughts, intention and action of the patient during decision
making in therapy planning
Justice The principle of justice is doing justice to tha patient while providing care
and by respecting the cultural and spiritual thoughts of the healthcare
service users
Beneficence The ethical principle of beneficence involves balancing of the benefits of
the treatment against the risks and the costs involved. In order words, the
bio-ethics of beneficence promotes that the actions of the healthcare
professionals must promote good, that is what is best for the patient
Non-malfeasance Non-maleficence states that no harm should be disproportionate to the
benefit of the treating. In order words non-maleficence means not harming
or inflicting least possible harm in order to reach beneficial outcome
Dilemmas in autonomy
Dementia is a neurodegerative disease that is mostly common among the older adults
and it is characterized by the gradual loss of memory and cognitive impairment. During the
initiation of the disease development, there occurs mild to moderate loss of cognition and
memory. However, with the gradual progression of the disease there occurs significant loss of
the cognition and memory. At this time, the affected individual is considered mentally unfit
to active part in the decision making process and thus breaching the ethical issue of
autonomy. In certain circumstance, It would be the duty of the healthcare professionals who
are looking after the patient to judge the patients “capacity issues” in order to predict the level
of cognition and then vouch for patient’s autonomy. In progressive dementia, the duty of the
healthcare will be guide the patient to avail the legal help through the personal welfare lasting
NURSING
professionals. The perspective of the Health and Social Care Act as proposed in UK’s
legislative board s highlighted below
Clinically led commissioning
The regulation of the provider in order to support innovative service
Raising greater voice for the parents
New focus over the public health
Increasing the key accountability areas of the local and the national bodies
Streamlines armed-length bodies
Promoting improvement in the overall quality of heal and social care
Effective tackling of the prevailing healthcare inequalities
Initiating proper integration of health and social care services
Increasing the overall choice of availing care
Conducting Effective Health and Social Care research
Providing proper education and training to the healthcare staffs
Reconfiguration of the new services
(Government of UK 2012)
The HSCA 2012 lead to the foundation of the Clinical Commissioning Groups (CCG) and
this was followed by the abolition of the primary care trust and strategic health care
authorities in the year 2013 (NHS England 2019).
Ethical Dilemma in Health and Social Care
Four main bio-ethics in health and social care include:
Autonomy Autonomy of thoughts, intention and action of the patient during decision
making in therapy planning
Justice The principle of justice is doing justice to tha patient while providing care
and by respecting the cultural and spiritual thoughts of the healthcare
service users
Beneficence The ethical principle of beneficence involves balancing of the benefits of
the treatment against the risks and the costs involved. In order words, the
bio-ethics of beneficence promotes that the actions of the healthcare
professionals must promote good, that is what is best for the patient
Non-malfeasance Non-maleficence states that no harm should be disproportionate to the
benefit of the treating. In order words non-maleficence means not harming
or inflicting least possible harm in order to reach beneficial outcome
Dilemmas in autonomy
Dementia is a neurodegerative disease that is mostly common among the older adults
and it is characterized by the gradual loss of memory and cognitive impairment. During the
initiation of the disease development, there occurs mild to moderate loss of cognition and
memory. However, with the gradual progression of the disease there occurs significant loss of
the cognition and memory. At this time, the affected individual is considered mentally unfit
to active part in the decision making process and thus breaching the ethical issue of
autonomy. In certain circumstance, It would be the duty of the healthcare professionals who
are looking after the patient to judge the patients “capacity issues” in order to predict the level
of cognition and then vouch for patient’s autonomy. In progressive dementia, the duty of the
healthcare will be guide the patient to avail the legal help through the personal welfare lasting
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

4
NURSING
power of attorney (LPA). Personal welfare LPA gives attorney the power to take decision on
behalf of the person in medical care and life sustaining medical treatment. The in order to
provide complete justice to the patient, the selection of the power of attorney must be done
when the “capacity issue” of the patient is within permissible range of cognitive thinking.
Dilemma in Justice
Doing justice in the care process is that main professionals code of conduct of the
health and the social care professionals. It is the duty of the nursing professional to treat
people as separate individual by upholding their level of dignity. In order to uphold the level
of dignity the care plan must be designed by doing justice to their religious, spiritual and
cultural values (Nursing and Midwifery Council of UK 2015). For instance, in some mental
and social healthcare services, people who are suffering from severe protein deficiency, are
recommended to increase their intake of fish and animal meat. However, this coincides
against their cultural or religious values if the person is a vegan and vegetarian. Under these
circumstances, it would be the duty of health and social care professionals to design person-
centred diet plan for that individual. Like diet from where the protein will be extracted from
the vegetables and fruits in order to follow the bio-ethics of justice. However, under certain
instances, the vegetable and fruit protein is unable to increase the total protein level of the
patients’ body under such circumstance animal protein is recommended in order to upheld the
ethics of beneficence and non-malefience (McGirr, McEvoy and Woodside 2017).
Beneficence and non-malefience
NHS Trust Foundation 2019 stated that Mental Health Act 1983, provides authority to
restrain patients who require treatment for their mental illness. MHs however, do not gives
authority to the mental healthcare professionals to restrain any patient for treating physical
conditions that is unrelated to their mental illness. Thus diabetic patient who are detained
under the MHS for the treatment of their mental psychosis might be restrained in order to
facilitate the administration of the antipsychotic drugs but they can never be restrained for the
administration of insulin in order to maintain diabetes. Restraining can be done in favour
beneficence this is because it is done in favour of doing “good” for the patients. However, in
certain circumstances restraining patients who are suffering from mental health complications
can increase the level of harm among the patients. For example, a patient suffering from
psychosis can become aggressive due to restraining leading to physical injury and thus
breaching the ethical obligation of non-malefience. Under this circumstance, the effective
communication skills and development of the therapeutic relationship followed by
application of the cognitive behavioural therapy can be proved to be helpful (Salehi et al.
2019). Development of the therapeutic communication with the patient helps in promotion of
the patient's empowerment and at the same time helps to increase the level of health literacy.
This helps to respect the ethical principle of respect, responsibility and integrity along with
responsibility (The British Psychological Society 2019).
The main professional standards of Health and Social Care include
Promotion and Protection of the interests of the service users and carers
Effective and clear communication
Working within the limit of the knowledge and skills
Respecting confidentiality of the client
Appropriate delegation
Effective management of risk
Reporting concerns about the safety of the patient
NURSING
power of attorney (LPA). Personal welfare LPA gives attorney the power to take decision on
behalf of the person in medical care and life sustaining medical treatment. The in order to
provide complete justice to the patient, the selection of the power of attorney must be done
when the “capacity issue” of the patient is within permissible range of cognitive thinking.
Dilemma in Justice
Doing justice in the care process is that main professionals code of conduct of the
health and the social care professionals. It is the duty of the nursing professional to treat
people as separate individual by upholding their level of dignity. In order to uphold the level
of dignity the care plan must be designed by doing justice to their religious, spiritual and
cultural values (Nursing and Midwifery Council of UK 2015). For instance, in some mental
and social healthcare services, people who are suffering from severe protein deficiency, are
recommended to increase their intake of fish and animal meat. However, this coincides
against their cultural or religious values if the person is a vegan and vegetarian. Under these
circumstances, it would be the duty of health and social care professionals to design person-
centred diet plan for that individual. Like diet from where the protein will be extracted from
the vegetables and fruits in order to follow the bio-ethics of justice. However, under certain
instances, the vegetable and fruit protein is unable to increase the total protein level of the
patients’ body under such circumstance animal protein is recommended in order to upheld the
ethics of beneficence and non-malefience (McGirr, McEvoy and Woodside 2017).
Beneficence and non-malefience
NHS Trust Foundation 2019 stated that Mental Health Act 1983, provides authority to
restrain patients who require treatment for their mental illness. MHs however, do not gives
authority to the mental healthcare professionals to restrain any patient for treating physical
conditions that is unrelated to their mental illness. Thus diabetic patient who are detained
under the MHS for the treatment of their mental psychosis might be restrained in order to
facilitate the administration of the antipsychotic drugs but they can never be restrained for the
administration of insulin in order to maintain diabetes. Restraining can be done in favour
beneficence this is because it is done in favour of doing “good” for the patients. However, in
certain circumstances restraining patients who are suffering from mental health complications
can increase the level of harm among the patients. For example, a patient suffering from
psychosis can become aggressive due to restraining leading to physical injury and thus
breaching the ethical obligation of non-malefience. Under this circumstance, the effective
communication skills and development of the therapeutic relationship followed by
application of the cognitive behavioural therapy can be proved to be helpful (Salehi et al.
2019). Development of the therapeutic communication with the patient helps in promotion of
the patient's empowerment and at the same time helps to increase the level of health literacy.
This helps to respect the ethical principle of respect, responsibility and integrity along with
responsibility (The British Psychological Society 2019).
The main professional standards of Health and Social Care include
Promotion and Protection of the interests of the service users and carers
Effective and clear communication
Working within the limit of the knowledge and skills
Respecting confidentiality of the client
Appropriate delegation
Effective management of risk
Reporting concerns about the safety of the patient
5
NURSING
Staying accountable for the care provided
Staying honest and trustworthy
(Health and care professions council 2019)
Example 1
While giving care to an individual who is suffering dementia, I also took into active
consideration of the issues associated with accidental fall. Taking help from the occupational
therapist helped me manage the risks of accidental fall. In this way I abided by the
professional standards of effective risk management.
Example 2
While caring of an older adult who is suffering from sexually transmitted disease, I
respected his privacy and confidentially and never disclosed his health alignments to his
children even if they repeatedly enquired. As per his permission, I only disclosed his health
issues to his wife. The adult patient was from indigenous background (black Hispanic group)
however, I never discriminated him while treating as for me all patients are same and I
provided care in a culturally competent manner.
National system of government evaluation
NHS England regulates national System of Government in Health and Social Care.
The organization is important in order to define the laws and the professional standards of
practice in health and social care. It aims to provide cost-effective care across the population
of UK by diminishing the health-inequalities. It also aims towards taking strict action against
the health and social care professionals who are failing to abide by their professional duties.
Issues mainly arise like: lack of proper funding or lack of uniform channelization of fund in
different aspects of health of health and social care. In order to make it better NHS can bring
in the potential stakeholders in order to promote proper policy planning and to improve the
channelization of funding.
Safeguarding vulnerable Group Act (2006): While working in the position of a HSCP
manager I will always conduct Disclosure and Barring Service (DBS) check in order to
scrutinize the qualification and professional details of newly recruited employees. I will
always safeguard the vulnerable groups by like children and intellectually disabled
individuals and will also report any incidence of harm
Protection of Vulnerable Adults Scheme: Under this act, I will report complain against any
employees having previous professional history of harming vulnerable adults.
Mental Health Act (2007): Under this act I will make sure every individual suffering from
mental health complication, get community healthcare service because, the amended
legislation gives powers of compulsion and introduces compulsory community treatment
orders and promoting patients to comply to the treatment procedure. I will also assist the
adults (above 16 years old) in taking an active part in decision making.
Mental capacity Act 2005: I will always protect vulnerable individuals and empower them
to take part in informed decision making.
NURSING
Staying accountable for the care provided
Staying honest and trustworthy
(Health and care professions council 2019)
Example 1
While giving care to an individual who is suffering dementia, I also took into active
consideration of the issues associated with accidental fall. Taking help from the occupational
therapist helped me manage the risks of accidental fall. In this way I abided by the
professional standards of effective risk management.
Example 2
While caring of an older adult who is suffering from sexually transmitted disease, I
respected his privacy and confidentially and never disclosed his health alignments to his
children even if they repeatedly enquired. As per his permission, I only disclosed his health
issues to his wife. The adult patient was from indigenous background (black Hispanic group)
however, I never discriminated him while treating as for me all patients are same and I
provided care in a culturally competent manner.
National system of government evaluation
NHS England regulates national System of Government in Health and Social Care.
The organization is important in order to define the laws and the professional standards of
practice in health and social care. It aims to provide cost-effective care across the population
of UK by diminishing the health-inequalities. It also aims towards taking strict action against
the health and social care professionals who are failing to abide by their professional duties.
Issues mainly arise like: lack of proper funding or lack of uniform channelization of fund in
different aspects of health of health and social care. In order to make it better NHS can bring
in the potential stakeholders in order to promote proper policy planning and to improve the
channelization of funding.
Safeguarding vulnerable Group Act (2006): While working in the position of a HSCP
manager I will always conduct Disclosure and Barring Service (DBS) check in order to
scrutinize the qualification and professional details of newly recruited employees. I will
always safeguard the vulnerable groups by like children and intellectually disabled
individuals and will also report any incidence of harm
Protection of Vulnerable Adults Scheme: Under this act, I will report complain against any
employees having previous professional history of harming vulnerable adults.
Mental Health Act (2007): Under this act I will make sure every individual suffering from
mental health complication, get community healthcare service because, the amended
legislation gives powers of compulsion and introduces compulsory community treatment
orders and promoting patients to comply to the treatment procedure. I will also assist the
adults (above 16 years old) in taking an active part in decision making.
Mental capacity Act 2005: I will always protect vulnerable individuals and empower them
to take part in informed decision making.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6
NURSING
Care Act 2014: This act is a new act that came into affect on 2015 and it helps to define the
professional standards of practice by the local authorities in health and social care. Its first
provision is to conducted proper patients’ assessment in order to highlight the clinical
priority. I will address this via conducting rigorous physical assessment and mental needs will
be addressed through indulging into effective communication with the client for the
development of therapeutic relationship.
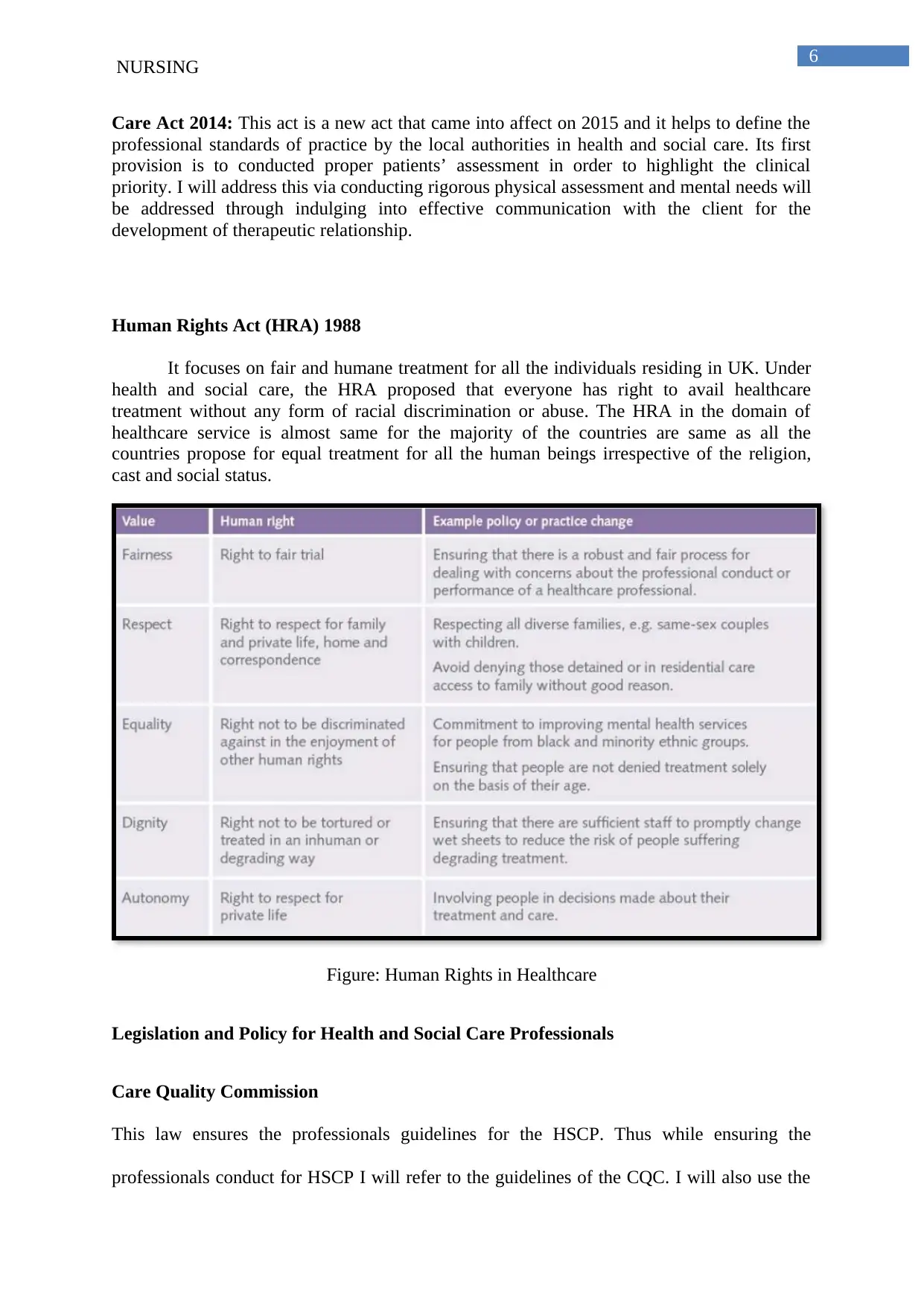
Human Rights Act (HRA) 1988
It focuses on fair and humane treatment for all the individuals residing in UK. Under
health and social care, the HRA proposed that everyone has right to avail healthcare
treatment without any form of racial discrimination or abuse. The HRA in the domain of
healthcare service is almost same for the majority of the countries are same as all the
countries propose for equal treatment for all the human beings irrespective of the religion,
cast and social status.
Figure: Human Rights in Healthcare
Legislation and Policy for Health and Social Care Professionals
Care Quality Commission
This law ensures the professionals guidelines for the HSCP. Thus while ensuring the
professionals conduct for HSCP I will refer to the guidelines of the CQC. I will also use the
NURSING
Care Act 2014: This act is a new act that came into affect on 2015 and it helps to define the
professional standards of practice by the local authorities in health and social care. Its first
provision is to conducted proper patients’ assessment in order to highlight the clinical
priority. I will address this via conducting rigorous physical assessment and mental needs will
be addressed through indulging into effective communication with the client for the
development of therapeutic relationship.
Human Rights Act (HRA) 1988
It focuses on fair and humane treatment for all the individuals residing in UK. Under
health and social care, the HRA proposed that everyone has right to avail healthcare
treatment without any form of racial discrimination or abuse. The HRA in the domain of
healthcare service is almost same for the majority of the countries are same as all the
countries propose for equal treatment for all the human beings irrespective of the religion,
cast and social status.
Figure: Human Rights in Healthcare
Legislation and Policy for Health and Social Care Professionals
Care Quality Commission
This law ensures the professionals guidelines for the HSCP. Thus while ensuring the
professionals conduct for HSCP I will refer to the guidelines of the CQC. I will also use the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

7
NURSING
tool of whistle blowing in order to highlight the mis-conduct. HSCP standards of practice will
also be used by me in order to inform the practitioners about the guidelines.
NURSING
tool of whistle blowing in order to highlight the mis-conduct. HSCP standards of practice will
also be used by me in order to inform the practitioners about the guidelines.
8
NURSING
References
Government of UK. 2012. The Health and Social Care Act 2012. Access date: 21st August
2019. Retrieved from: https://assets.publishing.service.gov.uk/government/uploads/system/
uploads/attachment_data/file/138257/A1.-Factsheet-Overview-240412.pdf
Health and care professions council. 2019. Standards of conduct, performance and ethics.
Access date: 21st August 2019. Retrieved from: https://www.hcpc-uk.org/standards/standards-
of-conduct-performance-and-ethics/
McGirr, C., McEvoy, C.T. and Woodside, J.V., 2017. Vegetarian and vegan diets: Weighing
the claims. In Nutrition Guide for Physicians and Related Healthcare Professionals(pp. 203-
212). Humana Press, Cham.
NAHS. 2015. NHS Digital - our role in the health and care system. Access date: 21st August
2019. Retrieved from: https://digital.nhs.uk/about-nhs-digital/our-work/transforming-health-
and-care-through-technology/fit-for-2020-report-from-the-nhs-digital-capability-review/nhs-
digital-our-role-in-the-health-and-care-system
NHS England. 2019. Key Legislations. Access date: 21st August 2019. Retrieved from:
https://www.england.nhs.uk/about/equality/equality-hub/resources/legislation/
NHS Trust Foundation 2019. Restraining adult patients in hospital. Access date: 21st August
2019. Retrieved from:
https://www.uhs.nhs.uk/HealthProfessionals/Clinical-law-updates/Restrainingadultpatientsin
hospital.aspx
NHS Trust Foundation. 2019. Restraining adult patients in hospital. Access date: 21st August
2019. Retrieved from:
NURSING
References
Government of UK. 2012. The Health and Social Care Act 2012. Access date: 21st August
2019. Retrieved from: https://assets.publishing.service.gov.uk/government/uploads/system/
uploads/attachment_data/file/138257/A1.-Factsheet-Overview-240412.pdf
Health and care professions council. 2019. Standards of conduct, performance and ethics.
Access date: 21st August 2019. Retrieved from: https://www.hcpc-uk.org/standards/standards-
of-conduct-performance-and-ethics/
McGirr, C., McEvoy, C.T. and Woodside, J.V., 2017. Vegetarian and vegan diets: Weighing
the claims. In Nutrition Guide for Physicians and Related Healthcare Professionals(pp. 203-
212). Humana Press, Cham.
NAHS. 2015. NHS Digital - our role in the health and care system. Access date: 21st August
2019. Retrieved from: https://digital.nhs.uk/about-nhs-digital/our-work/transforming-health-
and-care-through-technology/fit-for-2020-report-from-the-nhs-digital-capability-review/nhs-
digital-our-role-in-the-health-and-care-system
NHS England. 2019. Key Legislations. Access date: 21st August 2019. Retrieved from:
https://www.england.nhs.uk/about/equality/equality-hub/resources/legislation/
NHS Trust Foundation 2019. Restraining adult patients in hospital. Access date: 21st August
2019. Retrieved from:
https://www.uhs.nhs.uk/HealthProfessionals/Clinical-law-updates/Restrainingadultpatientsin
hospital.aspx
NHS Trust Foundation. 2019. Restraining adult patients in hospital. Access date: 21st August
2019. Retrieved from:
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9
NURSING
https://www.uhs.nhs.uk/HealthProfessionals/Clinical-law-updates/Restrainingadultpatientsin
hospital.aspx
Nursing and Midwifery Council of UK. 2015. Professional Code of Conduct. Access date:
21st August 2019. Retrieved from: https://www.nmc.org.uk/standards/code/
Salehi, Z., Najafi Ghezeljeh, T., Hajibabaee, F. and Joolaee, S., 2019. Factors behind ethical
dilemmas regarding physical restraint for critical care nurses. Nursing ethics,
p.0969733019858711.
The British Psychological Society. 2018. Code of Ethics and Conduct (2018). Access date:
21st August 2019. Retrieved from: https://www.bps.org.uk/news-and-policy/bps-code-ethics-
and-conduct
World Health Organization. 2019. Legislations and Regulations. Access date: 21st August
2019. Retrieved from: https://www.who.int/heli/tools/legis_regul/en/
NURSING
https://www.uhs.nhs.uk/HealthProfessionals/Clinical-law-updates/Restrainingadultpatientsin
hospital.aspx
Nursing and Midwifery Council of UK. 2015. Professional Code of Conduct. Access date:
21st August 2019. Retrieved from: https://www.nmc.org.uk/standards/code/
Salehi, Z., Najafi Ghezeljeh, T., Hajibabaee, F. and Joolaee, S., 2019. Factors behind ethical
dilemmas regarding physical restraint for critical care nurses. Nursing ethics,
p.0969733019858711.
The British Psychological Society. 2018. Code of Ethics and Conduct (2018). Access date:
21st August 2019. Retrieved from: https://www.bps.org.uk/news-and-policy/bps-code-ethics-
and-conduct
World Health Organization. 2019. Legislations and Regulations. Access date: 21st August
2019. Retrieved from: https://www.who.int/heli/tools/legis_regul/en/
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.



