Determinants of Obesity and Health Risks
VerifiedAdded on 2021/04/16
|16
|3407
|75
AI Summary
This assignment delves into the complex issue of obesity in Aboriginal communities, examining the interplay between socio-cultural, economic, and environmental factors that contribute to this public health concern. The document draws on various studies and reports from reputable sources such as MedlinePlus, PubMed Health, NACCHO, and the World Health Organization to provide a comprehensive understanding of the determinants of obesity and its associated health risks in these communities.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: Health and wellbeing
HEALTH and WELLBEING
Name of the Student
Name of the University
Author Note
HEALTH and WELLBEING
Name of the Student
Name of the University
Author Note
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1Health and wellbeing
What is Obesity and why is it a national health priority:
Obesity is a condition that is shown by an very high or unhealthy amount of body fat,
which is considered to have adverse health effetcs. It is caused when more calories are
consumed than is expended and can be a result of genetic abnormalities, overeating,
consumption of food high in fats and inadequate physical activity (Medlineplus.gov, 2018).
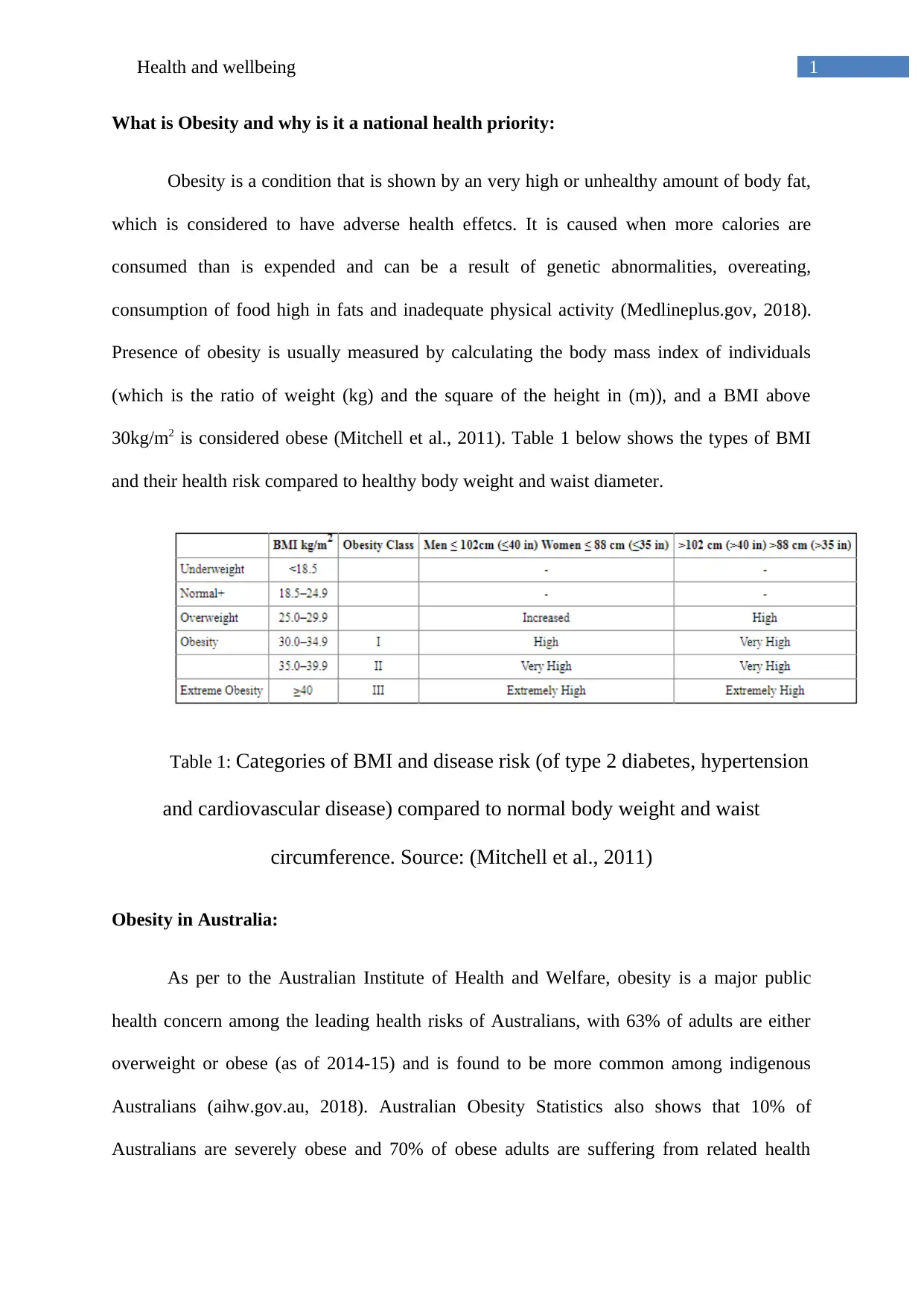
Presence of obesity is usually measured by calculating the body mass index of individuals
(which is the ratio of weight (kg) and the square of the height in (m)), and a BMI above
30kg/m2 is considered obese (Mitchell et al., 2011). Table 1 below shows the types of BMI
and their health risk compared to healthy body weight and waist diameter.
Table 1: Categories of BMI and disease risk (of type 2 diabetes, hypertension
and cardiovascular disease) compared to normal body weight and waist
circumference. Source: (Mitchell et al., 2011)
Obesity in Australia:
As per to the Australian Institute of Health and Welfare, obesity is a major public
health concern among the leading health risks of Australians, with 63% of adults are either
overweight or obese (as of 2014-15) and is found to be more common among indigenous
Australians (aihw.gov.au, 2018). Australian Obesity Statistics also shows that 10% of
Australians are severely obese and 70% of obese adults are suffering from related health
What is Obesity and why is it a national health priority:
Obesity is a condition that is shown by an very high or unhealthy amount of body fat,
which is considered to have adverse health effetcs. It is caused when more calories are
consumed than is expended and can be a result of genetic abnormalities, overeating,
consumption of food high in fats and inadequate physical activity (Medlineplus.gov, 2018).
Presence of obesity is usually measured by calculating the body mass index of individuals
(which is the ratio of weight (kg) and the square of the height in (m)), and a BMI above
30kg/m2 is considered obese (Mitchell et al., 2011). Table 1 below shows the types of BMI
and their health risk compared to healthy body weight and waist diameter.
Table 1: Categories of BMI and disease risk (of type 2 diabetes, hypertension
and cardiovascular disease) compared to normal body weight and waist
circumference. Source: (Mitchell et al., 2011)
Obesity in Australia:
As per to the Australian Institute of Health and Welfare, obesity is a major public
health concern among the leading health risks of Australians, with 63% of adults are either
overweight or obese (as of 2014-15) and is found to be more common among indigenous
Australians (aihw.gov.au, 2018). Australian Obesity Statistics also shows that 10% of
Australians are severely obese and 70% of obese adults are suffering from related health
2Health and wellbeing
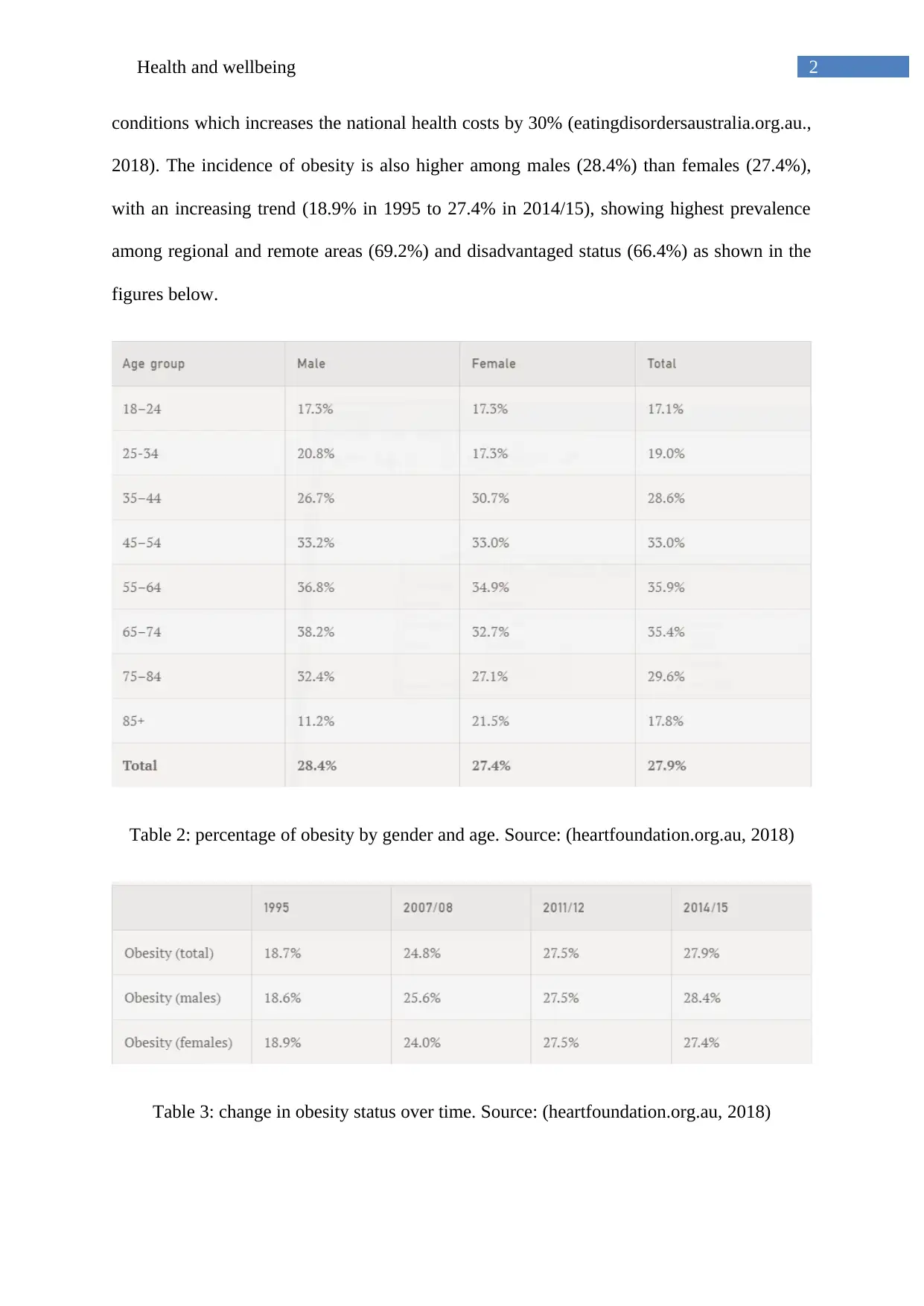
conditions which increases the national health costs by 30% (eatingdisordersaustralia.org.au.,
2018). The incidence of obesity is also higher among males (28.4%) than females (27.4%),
with an increasing trend (18.9% in 1995 to 27.4% in 2014/15), showing highest prevalence
among regional and remote areas (69.2%) and disadvantaged status (66.4%) as shown in the
figures below.
Table 2: percentage of obesity by gender and age. Source: (heartfoundation.org.au, 2018)
Table 3: change in obesity status over time. Source: (heartfoundation.org.au, 2018)
conditions which increases the national health costs by 30% (eatingdisordersaustralia.org.au.,
2018). The incidence of obesity is also higher among males (28.4%) than females (27.4%),
with an increasing trend (18.9% in 1995 to 27.4% in 2014/15), showing highest prevalence
among regional and remote areas (69.2%) and disadvantaged status (66.4%) as shown in the
figures below.
Table 2: percentage of obesity by gender and age. Source: (heartfoundation.org.au, 2018)
Table 3: change in obesity status over time. Source: (heartfoundation.org.au, 2018)
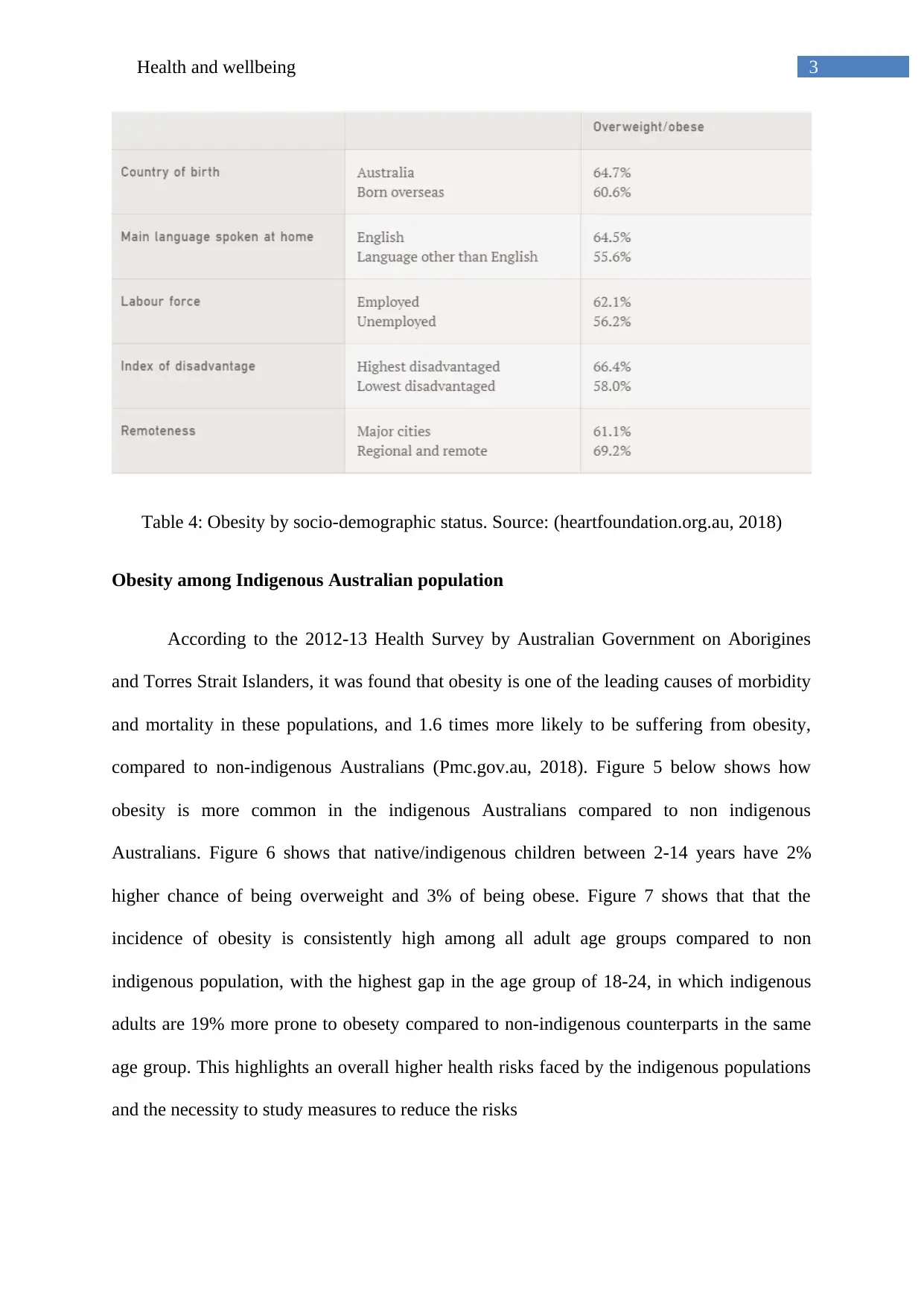
3Health and wellbeing
Table 4: Obesity by socio-demographic status. Source: (heartfoundation.org.au, 2018)
Obesity among Indigenous Australian population
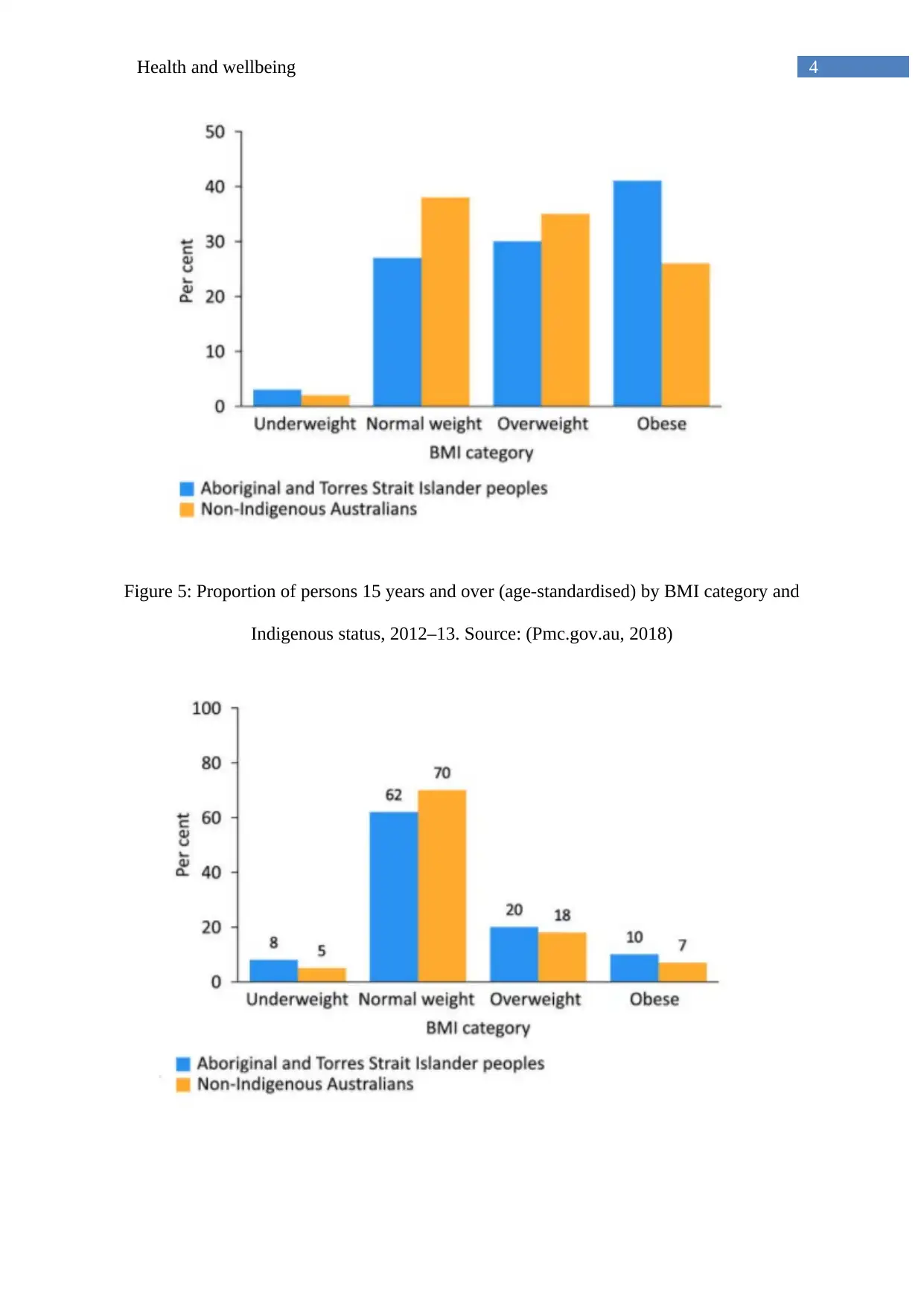
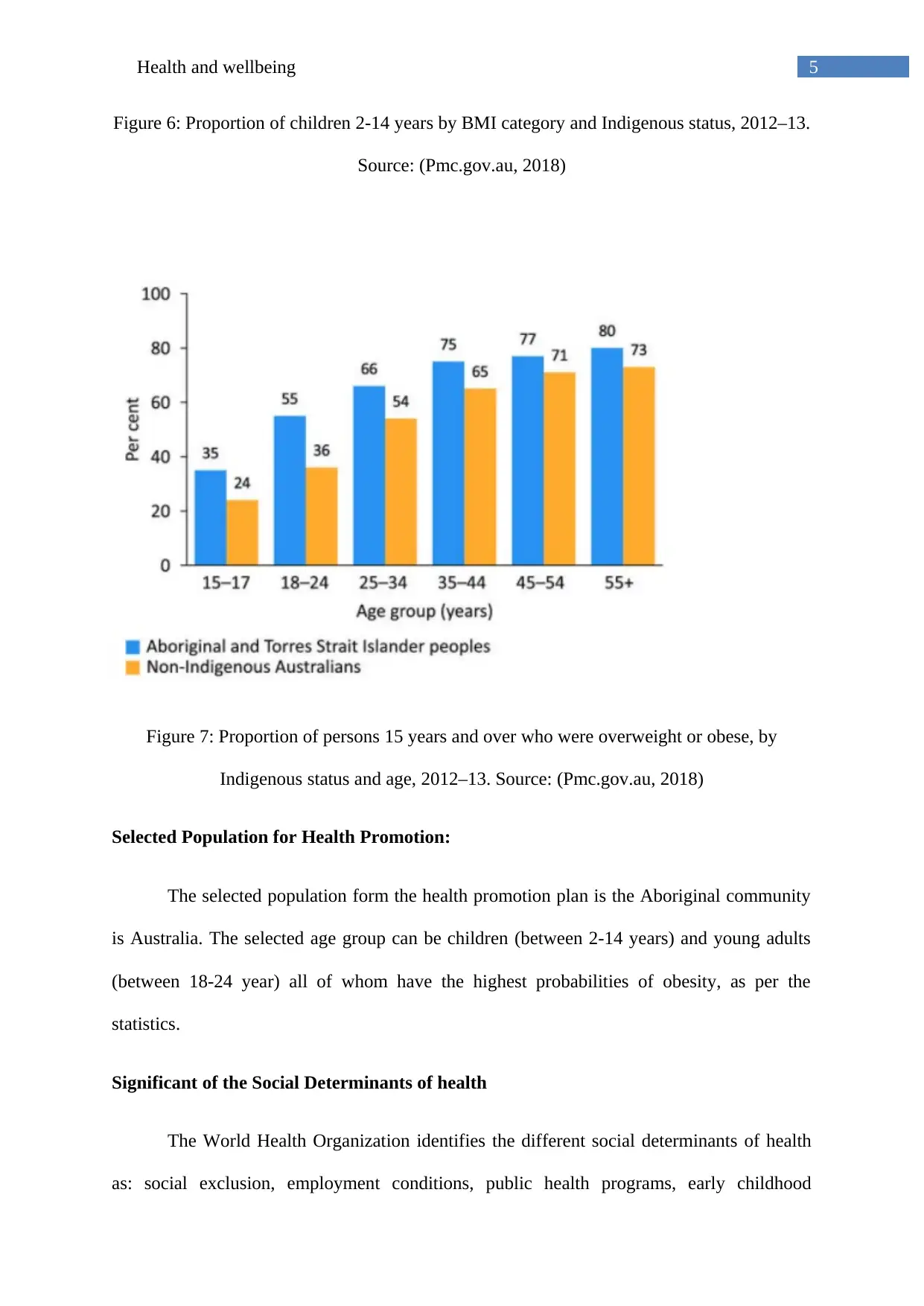
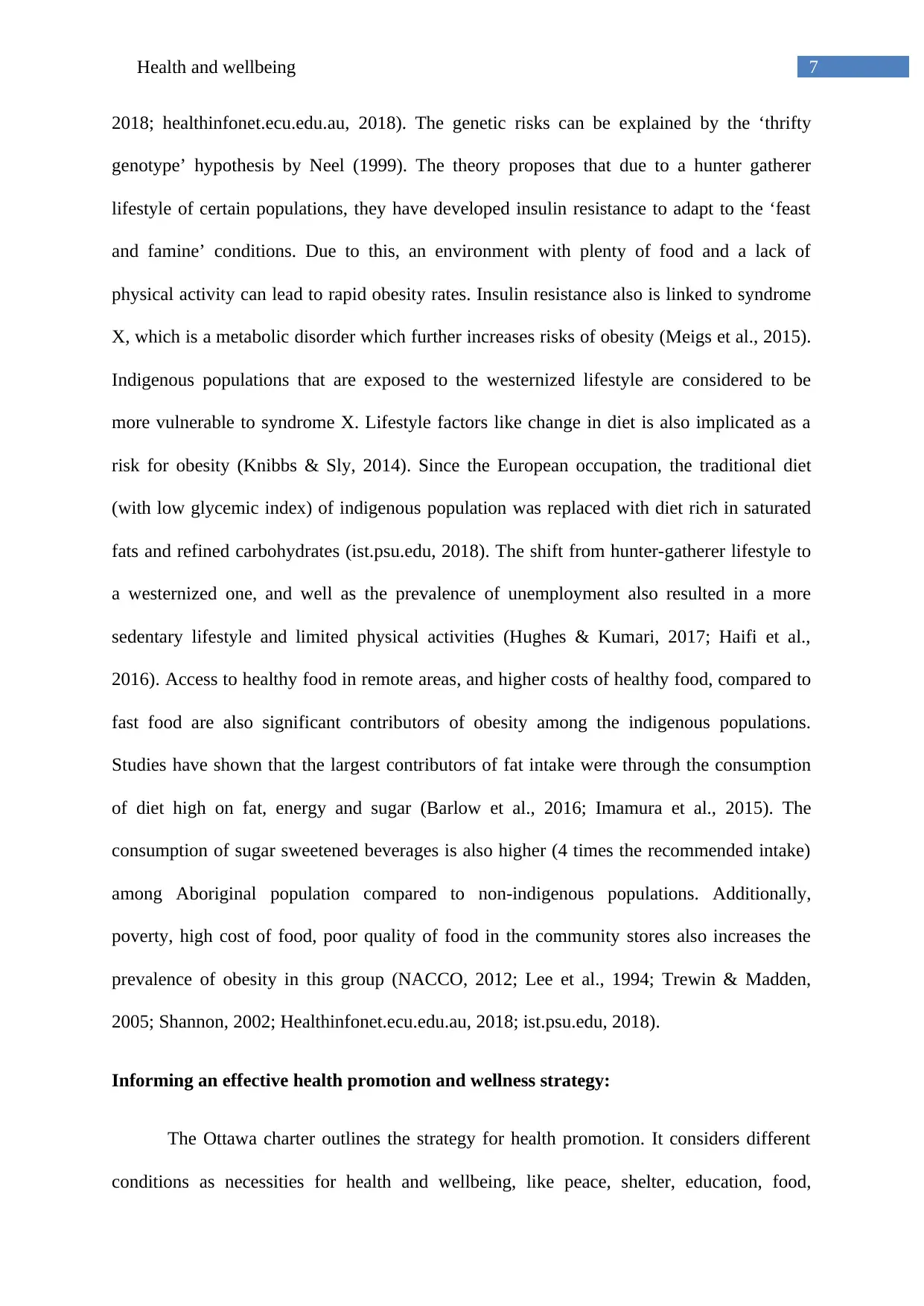
According to the 2012-13 Health Survey by Australian Government on Aborigines
and Torres Strait Islanders, it was found that obesity is one of the leading causes of morbidity
and mortality in these populations, and 1.6 times more likely to be suffering from obesity,
compared to non-indigenous Australians (Pmc.gov.au, 2018). Figure 5 below shows how
obesity is more common in the indigenous Australians compared to non indigenous
Australians. Figure 6 shows that native/indigenous children between 2-14 years have 2%
higher chance of being overweight and 3% of being obese. Figure 7 shows that that the
incidence of obesity is consistently high among all adult age groups compared to non
indigenous population, with the highest gap in the age group of 18-24, in which indigenous
adults are 19% more prone to obesety compared to non-indigenous counterparts in the same
age group. This highlights an overall higher health risks faced by the indigenous populations
and the necessity to study measures to reduce the risks
Table 4: Obesity by socio-demographic status. Source: (heartfoundation.org.au, 2018)
Obesity among Indigenous Australian population
According to the 2012-13 Health Survey by Australian Government on Aborigines
and Torres Strait Islanders, it was found that obesity is one of the leading causes of morbidity
and mortality in these populations, and 1.6 times more likely to be suffering from obesity,
compared to non-indigenous Australians (Pmc.gov.au, 2018). Figure 5 below shows how
obesity is more common in the indigenous Australians compared to non indigenous
Australians. Figure 6 shows that native/indigenous children between 2-14 years have 2%
higher chance of being overweight and 3% of being obese. Figure 7 shows that that the
incidence of obesity is consistently high among all adult age groups compared to non
indigenous population, with the highest gap in the age group of 18-24, in which indigenous
adults are 19% more prone to obesety compared to non-indigenous counterparts in the same
age group. This highlights an overall higher health risks faced by the indigenous populations
and the necessity to study measures to reduce the risks
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4Health and wellbeing
Figure 5: Proportion of persons 15 years and over (age-standardised) by BMI category and
Indigenous status, 2012–13. Source: (Pmc.gov.au, 2018)
Figure 5: Proportion of persons 15 years and over (age-standardised) by BMI category and
Indigenous status, 2012–13. Source: (Pmc.gov.au, 2018)
5Health and wellbeing
Figure 6: Proportion of children 2-14 years by BMI category and Indigenous status, 2012–13.
Source: (Pmc.gov.au, 2018)
Figure 7: Proportion of persons 15 years and over who were overweight or obese, by
Indigenous status and age, 2012–13. Source: (Pmc.gov.au, 2018)
Selected Population for Health Promotion:
The selected population form the health promotion plan is the Aboriginal community
is Australia. The selected age group can be children (between 2-14 years) and young adults
(between 18-24 year) all of whom have the highest probabilities of obesity, as per the
statistics.
Significant of the Social Determinants of health
The World Health Organization identifies the different social determinants of health
as: social exclusion, employment conditions, public health programs, early childhood
Figure 6: Proportion of children 2-14 years by BMI category and Indigenous status, 2012–13.
Source: (Pmc.gov.au, 2018)
Figure 7: Proportion of persons 15 years and over who were overweight or obese, by
Indigenous status and age, 2012–13. Source: (Pmc.gov.au, 2018)
Selected Population for Health Promotion:
The selected population form the health promotion plan is the Aboriginal community
is Australia. The selected age group can be children (between 2-14 years) and young adults
(between 18-24 year) all of whom have the highest probabilities of obesity, as per the
statistics.
Significant of the Social Determinants of health
The World Health Organization identifies the different social determinants of health
as: social exclusion, employment conditions, public health programs, early childhood

6Health and wellbeing
development, women and gender equality, globalization, health system performance and
urbanization (who.int, 2018). Studies by Sartorius et al. (2015) studied the different social
determinants of health related to obesity. The study found that ethnicity, gender, socio-
economic status, dietary intake, physical inactivity, educational status and even marriage can
affect the probability of obesity.
Health Risks of Obesity:
The health risks of obesity includes: coronary cardiac disease, hypertension, type 2
diabetes, gall bladder stone, pulmonary problems and cancer (ncbi.nlm.nih.gov, 2018). Other
health risks include: cardiac disease and stroke, osteoarthritis, sleep apnea, fatty liver disease
and problems during pregnancy (increasing the risk of a c-section delivery). The types of
cancer that can occur because of obesity includes: breast cancer, colon/rectum cancer,
endometrial cancer, gallbladder cancer, and kidney cancers (niddk.nih.gov, 2018). Among the
indigenous populations, the risks of nutrition related chronic health problems are much higher
than the general population, and obesity is one of the main risks of morbidity and mortality
(healthinfonet.ecu.edu.au, 2018).
Why Obesity is a significant problem among the Indigenous Australians:
Different factors are considered to contribute to obesity risks among the indigenous
population in Australia that has a complex interplay. Even though the risk of the development
of an obesogenic environment prevails through Australia, the problem gets complicated in the
indigenous groups due to different geographical, social, economic and infrastructure related
factors which affects the availability and choice of food (Lakerveld et al., 2017; ist.psu.edu,
2018) . Other contributors are considered to be: historical, social, geographical, economic,
and infrastructure factors which might contribute for the obesity problems in the indigenous
Australian population, apart from the genetic factors that also contributes to it (Qasim net al.,
development, women and gender equality, globalization, health system performance and
urbanization (who.int, 2018). Studies by Sartorius et al. (2015) studied the different social
determinants of health related to obesity. The study found that ethnicity, gender, socio-
economic status, dietary intake, physical inactivity, educational status and even marriage can
affect the probability of obesity.
Health Risks of Obesity:
The health risks of obesity includes: coronary cardiac disease, hypertension, type 2
diabetes, gall bladder stone, pulmonary problems and cancer (ncbi.nlm.nih.gov, 2018). Other
health risks include: cardiac disease and stroke, osteoarthritis, sleep apnea, fatty liver disease
and problems during pregnancy (increasing the risk of a c-section delivery). The types of
cancer that can occur because of obesity includes: breast cancer, colon/rectum cancer,
endometrial cancer, gallbladder cancer, and kidney cancers (niddk.nih.gov, 2018). Among the
indigenous populations, the risks of nutrition related chronic health problems are much higher
than the general population, and obesity is one of the main risks of morbidity and mortality
(healthinfonet.ecu.edu.au, 2018).
Why Obesity is a significant problem among the Indigenous Australians:
Different factors are considered to contribute to obesity risks among the indigenous
population in Australia that has a complex interplay. Even though the risk of the development
of an obesogenic environment prevails through Australia, the problem gets complicated in the
indigenous groups due to different geographical, social, economic and infrastructure related
factors which affects the availability and choice of food (Lakerveld et al., 2017; ist.psu.edu,
2018) . Other contributors are considered to be: historical, social, geographical, economic,
and infrastructure factors which might contribute for the obesity problems in the indigenous
Australian population, apart from the genetic factors that also contributes to it (Qasim net al.,
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7Health and wellbeing
2018; healthinfonet.ecu.edu.au, 2018). The genetic risks can be explained by the ‘thrifty
genotype’ hypothesis by Neel (1999). The theory proposes that due to a hunter gatherer
lifestyle of certain populations, they have developed insulin resistance to adapt to the ‘feast
and famine’ conditions. Due to this, an environment with plenty of food and a lack of
physical activity can lead to rapid obesity rates. Insulin resistance also is linked to syndrome
X, which is a metabolic disorder which further increases risks of obesity (Meigs et al., 2015).
Indigenous populations that are exposed to the westernized lifestyle are considered to be
more vulnerable to syndrome X. Lifestyle factors like change in diet is also implicated as a
risk for obesity (Knibbs & Sly, 2014). Since the European occupation, the traditional diet
(with low glycemic index) of indigenous population was replaced with diet rich in saturated
fats and refined carbohydrates (ist.psu.edu, 2018). The shift from hunter-gatherer lifestyle to
a westernized one, and well as the prevalence of unemployment also resulted in a more
sedentary lifestyle and limited physical activities (Hughes & Kumari, 2017; Haifi et al.,
2016). Access to healthy food in remote areas, and higher costs of healthy food, compared to
fast food are also significant contributors of obesity among the indigenous populations.
Studies have shown that the largest contributors of fat intake were through the consumption
of diet high on fat, energy and sugar (Barlow et al., 2016; Imamura et al., 2015). The
consumption of sugar sweetened beverages is also higher (4 times the recommended intake)
among Aboriginal population compared to non-indigenous populations. Additionally,
poverty, high cost of food, poor quality of food in the community stores also increases the
prevalence of obesity in this group (NACCO, 2012; Lee et al., 1994; Trewin & Madden,
2005; Shannon, 2002; Healthinfonet.ecu.edu.au, 2018; ist.psu.edu, 2018).
Informing an effective health promotion and wellness strategy:
The Ottawa charter outlines the strategy for health promotion. It considers different
conditions as necessities for health and wellbeing, like peace, shelter, education, food,
2018; healthinfonet.ecu.edu.au, 2018). The genetic risks can be explained by the ‘thrifty
genotype’ hypothesis by Neel (1999). The theory proposes that due to a hunter gatherer
lifestyle of certain populations, they have developed insulin resistance to adapt to the ‘feast
and famine’ conditions. Due to this, an environment with plenty of food and a lack of
physical activity can lead to rapid obesity rates. Insulin resistance also is linked to syndrome
X, which is a metabolic disorder which further increases risks of obesity (Meigs et al., 2015).
Indigenous populations that are exposed to the westernized lifestyle are considered to be
more vulnerable to syndrome X. Lifestyle factors like change in diet is also implicated as a
risk for obesity (Knibbs & Sly, 2014). Since the European occupation, the traditional diet
(with low glycemic index) of indigenous population was replaced with diet rich in saturated
fats and refined carbohydrates (ist.psu.edu, 2018). The shift from hunter-gatherer lifestyle to
a westernized one, and well as the prevalence of unemployment also resulted in a more
sedentary lifestyle and limited physical activities (Hughes & Kumari, 2017; Haifi et al.,
2016). Access to healthy food in remote areas, and higher costs of healthy food, compared to
fast food are also significant contributors of obesity among the indigenous populations.
Studies have shown that the largest contributors of fat intake were through the consumption
of diet high on fat, energy and sugar (Barlow et al., 2016; Imamura et al., 2015). The
consumption of sugar sweetened beverages is also higher (4 times the recommended intake)
among Aboriginal population compared to non-indigenous populations. Additionally,
poverty, high cost of food, poor quality of food in the community stores also increases the
prevalence of obesity in this group (NACCO, 2012; Lee et al., 1994; Trewin & Madden,
2005; Shannon, 2002; Healthinfonet.ecu.edu.au, 2018; ist.psu.edu, 2018).
Informing an effective health promotion and wellness strategy:
The Ottawa charter outlines the strategy for health promotion. It considers different
conditions as necessities for health and wellbeing, like peace, shelter, education, food,
8Health and wellbeing
income, stable eco-system, sustainable resource, social justice and equity. Furthermore,
improvement in health outcomes requires health advocacy, enable control of individuals over
factors that affect their health and mediation of the activities of health promotion (World
Health Organization, 2018).
In the frameworks of wellbeing, several components are outlined like population,
family and community, health, education and training, work, economic resources and housing
(Abs.gov.au, 2018). Measurement of wellbeing is a large task that includes the spectrum of
birth to death, and encompasses people in a dynamic culture which consists of the natural
environment, artificial environment, social arrangements, and human consciousness. The
overall wellbeing of people depends on the factors which interact within this culture. The
wellbeing is therefore measured by mapping the whole life of an individual and identifying
contexts or events that can affect the quality of life, and the wellbeing equation becomes a
function of the social, material and natural environments surrounding the individuals
(Abs.gov.au, 2018). Care strategies needs to address the frameworks of wellbeing and
incorporate the ability to measure it.
How the strategies can be used in the improvement of health outcome of the selected
population.
Improvement in the health outcomes of the selected population can be addressed by
the determinants of health that increases the risks of obesity among the indigenous Australian
population (Greenwood et al., 2015). Addressing aspects like education and training, work
and involving community based action can be suggested (based on the frameworks of
wellbeing) which can improve their well being. The proposed strategy can be based upon the
structure of the Australian Healthy Weight 2008 initiative that incorporates community wide
education, community demonstrations, monitoring evidence as well as performance,
income, stable eco-system, sustainable resource, social justice and equity. Furthermore,
improvement in health outcomes requires health advocacy, enable control of individuals over
factors that affect their health and mediation of the activities of health promotion (World
Health Organization, 2018).
In the frameworks of wellbeing, several components are outlined like population,
family and community, health, education and training, work, economic resources and housing
(Abs.gov.au, 2018). Measurement of wellbeing is a large task that includes the spectrum of
birth to death, and encompasses people in a dynamic culture which consists of the natural
environment, artificial environment, social arrangements, and human consciousness. The
overall wellbeing of people depends on the factors which interact within this culture. The
wellbeing is therefore measured by mapping the whole life of an individual and identifying
contexts or events that can affect the quality of life, and the wellbeing equation becomes a
function of the social, material and natural environments surrounding the individuals
(Abs.gov.au, 2018). Care strategies needs to address the frameworks of wellbeing and
incorporate the ability to measure it.
How the strategies can be used in the improvement of health outcome of the selected
population.
Improvement in the health outcomes of the selected population can be addressed by
the determinants of health that increases the risks of obesity among the indigenous Australian
population (Greenwood et al., 2015). Addressing aspects like education and training, work
and involving community based action can be suggested (based on the frameworks of
wellbeing) which can improve their well being. The proposed strategy can be based upon the
structure of the Australian Healthy Weight 2008 initiative that incorporates community wide
education, community demonstrations, monitoring evidence as well as performance,
9Health and wellbeing
coordination and building of capacity. The National Health and Medical Research council
designed guidelines for clinical practice to manage the problem of obesity among children
and adolescents and adults. The Eat Well Australia action plan published by Strategic Inter-
Governmental Nutrition Alliance (SIGNAL) and Dietary Guidelines for Australian Adults,
published in 2003, provides specific strategies for the prevention of excess weight gain and
monitors the intake of fat and sugar. Be Active Australia plan involves strategies for
community education and communication as well as increase of the capacity of workforce,
research, monitoring, evaluation, strategic management and coordination. These frameworks
mainly highlight the necessity of improving nutrition and control of obesity. Weight loss can
also be achieved through the reduction of dietary intake, however long term strategies also
should involve changes in behaviour with respect to diet and physical activity. Food
purchasing habits should also be addressed in the nutrition intervention and education
through the community based programs.
Proposed health promotion strategy
Based on such aspects, my health promotion plan will include specific aspects from
the Ottawa Charter and the frameworks of wellbeing as given below:
Education and training of the members of community regarding the risks and
health effects of obesity
Supporting the individuals to make healthy choice of diet, and providing
information on healthy and unhealthy diet
Supporting the community members in the engagement in physical activities
Helping the community members to have adequate access to healthy food, and
limiting access to unhealthy food (like sugar sweetened beverages and die
high in saturated fats)
coordination and building of capacity. The National Health and Medical Research council
designed guidelines for clinical practice to manage the problem of obesity among children
and adolescents and adults. The Eat Well Australia action plan published by Strategic Inter-
Governmental Nutrition Alliance (SIGNAL) and Dietary Guidelines for Australian Adults,
published in 2003, provides specific strategies for the prevention of excess weight gain and
monitors the intake of fat and sugar. Be Active Australia plan involves strategies for
community education and communication as well as increase of the capacity of workforce,
research, monitoring, evaluation, strategic management and coordination. These frameworks
mainly highlight the necessity of improving nutrition and control of obesity. Weight loss can
also be achieved through the reduction of dietary intake, however long term strategies also
should involve changes in behaviour with respect to diet and physical activity. Food
purchasing habits should also be addressed in the nutrition intervention and education
through the community based programs.
Proposed health promotion strategy
Based on such aspects, my health promotion plan will include specific aspects from
the Ottawa Charter and the frameworks of wellbeing as given below:
Education and training of the members of community regarding the risks and
health effects of obesity
Supporting the individuals to make healthy choice of diet, and providing
information on healthy and unhealthy diet
Supporting the community members in the engagement in physical activities
Helping the community members to have adequate access to healthy food, and
limiting access to unhealthy food (like sugar sweetened beverages and die
high in saturated fats)
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
10Health and wellbeing
Regular monitoring of the health status of the community members,
particularly of obese individuals for early signs of health risks
Planning interventions for individuals at high risks of co morbidity and
supporting them for behavioural or lifestyle changes
Supporting the community members to get choose more traditional lifestyle
and diet.
Considering the different factors that increases the risks of obesity among the selected
population, it is important to address these risk factors to alleviate the incidence of the disease
and lower the burden on health faced b the individuals of the community.
Regular monitoring of the health status of the community members,
particularly of obese individuals for early signs of health risks
Planning interventions for individuals at high risks of co morbidity and
supporting them for behavioural or lifestyle changes
Supporting the community members to get choose more traditional lifestyle
and diet.
Considering the different factors that increases the risks of obesity among the selected
population, it is important to address these risk factors to alleviate the incidence of the disease
and lower the burden on health faced b the individuals of the community.
11Health and wellbeing
References:
Abs.gov.au. (2018). 4160.0 - Measuring Wellbeing: Frameworks for Australian Social
Statistics, 2001. Abs.gov.au. Retrieved 21 March 2018, from
http://www.abs.gov.au/ausstats/abs@.nsf/0/B176042438EE2331CA2571B7000A43A
7?opendocument
aihw.gov.au. (2018). An interactive insight into overweight and obesity in
Australia. Australian Institute of Health and Welfare. Retrieved 20 March 2018, from
https://www.aihw.gov.au/reports/overweight-obesity/interactive-insight-into-
overweight-and-obesity/contents/how-many-people-are-overweight-or-obese
Al-Haifi, A. A., AlMajed, H. T., Al-Hazzaa, H. M., Musaiger, A. O., Arab, M. A., & Hasan,
R. A. (2016). Relative contribution of obesity, sedentary behaviors and dietary habits
to sleep duration among Kuwaiti adolescents. Global journal of health science, 8(1),
107.
Barlow, P., Reeves, A., McKee, M., Galea, G., & Stuckler, D. (2016). Unhealthy diets,
obesity and time discounting: a systematic literature review and network
analysis. obesity reviews, 17(9), 810-819.
Dyer, S. M., Gomersall, J. S., Smithers, L. G., Davy, C., Coleman, D. T., & Street, J. M.
(2017). Prevalence and characteristics of overweight and obesity in indigenous
Australian children: a systematic review. Critical reviews in food science and
nutrition, 57(7), 1365-1376.
eatingdisordersaustralia.org.au. (2018). Australia's Obesity Statistics in 2017 - National
Eating Disorders and Obesity. National Eating Disorders and Obesity. Retrieved 20
References:
Abs.gov.au. (2018). 4160.0 - Measuring Wellbeing: Frameworks for Australian Social
Statistics, 2001. Abs.gov.au. Retrieved 21 March 2018, from
http://www.abs.gov.au/ausstats/abs@.nsf/0/B176042438EE2331CA2571B7000A43A
7?opendocument
aihw.gov.au. (2018). An interactive insight into overweight and obesity in
Australia. Australian Institute of Health and Welfare. Retrieved 20 March 2018, from
https://www.aihw.gov.au/reports/overweight-obesity/interactive-insight-into-
overweight-and-obesity/contents/how-many-people-are-overweight-or-obese
Al-Haifi, A. A., AlMajed, H. T., Al-Hazzaa, H. M., Musaiger, A. O., Arab, M. A., & Hasan,
R. A. (2016). Relative contribution of obesity, sedentary behaviors and dietary habits
to sleep duration among Kuwaiti adolescents. Global journal of health science, 8(1),
107.
Barlow, P., Reeves, A., McKee, M., Galea, G., & Stuckler, D. (2016). Unhealthy diets,
obesity and time discounting: a systematic literature review and network
analysis. obesity reviews, 17(9), 810-819.
Dyer, S. M., Gomersall, J. S., Smithers, L. G., Davy, C., Coleman, D. T., & Street, J. M.
(2017). Prevalence and characteristics of overweight and obesity in indigenous
Australian children: a systematic review. Critical reviews in food science and
nutrition, 57(7), 1365-1376.
eatingdisordersaustralia.org.au. (2018). Australia's Obesity Statistics in 2017 - National
Eating Disorders and Obesity. National Eating Disorders and Obesity. Retrieved 20
12Health and wellbeing
March 2018, from https://eatingdisordersaustralia.org.au/australias-obesity-statistics-
2017/
Greenwood, M., De Leeuw, S., Lindsay, N. M., & Reading, C. (Eds.). (2015). Determinants
of Indigenous Peoples' Health. Canadian Scholars’ Press.
Healthinfonet.ecu.edu.au. (2018). Factors contributing to Indigenous health « Overview of
the health of Indigenous people in Western Australia 2013 « Reviews « Western
Australia « States and Territories « Australian Indigenous
HealthInfoNet. Healthinfonet.ecu.edu.au. Retrieved 21 March 2018, from
http://www.healthinfonet.ecu.edu.au/states-territories-home/wa/reviews/our-review/
health-risk-factors
Healthinfonet.ecu.edu.au. (2018). Summary of overweight and obesity among Indigenous
peoples « Reviews « Overweight and obesity « Protective & risk factors « Australian
Indigenous HealthInfoNet. Healthinfonet.ecu.edu.au. Retrieved 21 March 2018, from
http://www.healthinfonet.ecu.edu.au/health-risks/overweight-obesity/reviews/our-
review#fnl-4
heartfoundation.org.au. (2018). Overweight and obesity statistics. The Heart Foundation.
Retrieved 20 March 2018, from https://www.heartfoundation.org.au/about-us/what-
we-do/heart-disease-in-australia/overweight-and-obesity-statistics
Hughes, A., & Kumari, M. (2017). Unemployment, underweight, and obesity: Findings from
Understanding Society (UKHLS). Preventive medicine, 97, 19-25.
Imamura, F., O’Connor, L., Ye, Z., Mursu, J., Hayashino, Y., Bhupathiraju, S. N., & Forouhi,
N. G. (2015). Consumption of sugar sweetened beverages, artificially sweetened
March 2018, from https://eatingdisordersaustralia.org.au/australias-obesity-statistics-
2017/
Greenwood, M., De Leeuw, S., Lindsay, N. M., & Reading, C. (Eds.). (2015). Determinants
of Indigenous Peoples' Health. Canadian Scholars’ Press.
Healthinfonet.ecu.edu.au. (2018). Factors contributing to Indigenous health « Overview of
the health of Indigenous people in Western Australia 2013 « Reviews « Western
Australia « States and Territories « Australian Indigenous
HealthInfoNet. Healthinfonet.ecu.edu.au. Retrieved 21 March 2018, from
http://www.healthinfonet.ecu.edu.au/states-territories-home/wa/reviews/our-review/
health-risk-factors
Healthinfonet.ecu.edu.au. (2018). Summary of overweight and obesity among Indigenous
peoples « Reviews « Overweight and obesity « Protective & risk factors « Australian
Indigenous HealthInfoNet. Healthinfonet.ecu.edu.au. Retrieved 21 March 2018, from
http://www.healthinfonet.ecu.edu.au/health-risks/overweight-obesity/reviews/our-
review#fnl-4
heartfoundation.org.au. (2018). Overweight and obesity statistics. The Heart Foundation.
Retrieved 20 March 2018, from https://www.heartfoundation.org.au/about-us/what-
we-do/heart-disease-in-australia/overweight-and-obesity-statistics
Hughes, A., & Kumari, M. (2017). Unemployment, underweight, and obesity: Findings from
Understanding Society (UKHLS). Preventive medicine, 97, 19-25.
Imamura, F., O’Connor, L., Ye, Z., Mursu, J., Hayashino, Y., Bhupathiraju, S. N., & Forouhi,
N. G. (2015). Consumption of sugar sweetened beverages, artificially sweetened
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
13Health and wellbeing
beverages, and fruit juice and incidence of type 2 diabetes: systematic review, meta-
analysis, and estimation of population attributable fraction. Bmj, 351, h3576.
ist.psu.edu. (2018). Nutrition in Aboriginal and Torres Strait Islander
Peoples. Citeseerx.ist.psu.edu. Retrieved 21 March 2018, from
http://citeseerx.ist.psu.edu/viewdoc/download?
doi=10.1.1.602.1434&rep=rep1&type=pdf
Knibbs, L., & Sly, P. (2014). Indigenous health and environmental risk factors: an Australian
problem with global analogues?. Global Health Action, 7(1), 23766.
http://dx.doi.org/10.3402/gha.v7.23766
Lakerveld, J., Mackenbach, J. D., Rutter, H., & Brug, J. (2017). Obesogenic environment and
obesogenic behaviours. Advanced Nutrition and Dietetics in Obesity, 132.
Lee, A. J., O'dea, K., & Mathews, J. D. (1994). Apparent dietary intake in remote Aboriginal
communities. Australian and New Zealand Journal of Public Health, 18(2), 190-197.
Medlineplus.gov. (2018). Obesity: MedlinePlus. Medlineplus.gov. Retrieved 20 March 2018,
from https://medlineplus.gov/obesity.html
Meigs, J. B., Nathan, D. M., Wolfsdorf, J. I., & Mulder, J. E. (2015). The metabolic
syndrome (insulin resistance syndrome or syndrome X). Available in www.
UpToDate. com. Accessed.
Mitchell, N., Catenacci, V., Wyatt, H., & Hill, J. (2011). Obesity: Overview of an
Epidemic. Psychiatric Clinics Of North America, 34(4), 717-732.
http://dx.doi.org/10.1016/j.psc.2011.08.005
beverages, and fruit juice and incidence of type 2 diabetes: systematic review, meta-
analysis, and estimation of population attributable fraction. Bmj, 351, h3576.
ist.psu.edu. (2018). Nutrition in Aboriginal and Torres Strait Islander
Peoples. Citeseerx.ist.psu.edu. Retrieved 21 March 2018, from
http://citeseerx.ist.psu.edu/viewdoc/download?
doi=10.1.1.602.1434&rep=rep1&type=pdf
Knibbs, L., & Sly, P. (2014). Indigenous health and environmental risk factors: an Australian
problem with global analogues?. Global Health Action, 7(1), 23766.
http://dx.doi.org/10.3402/gha.v7.23766
Lakerveld, J., Mackenbach, J. D., Rutter, H., & Brug, J. (2017). Obesogenic environment and
obesogenic behaviours. Advanced Nutrition and Dietetics in Obesity, 132.
Lee, A. J., O'dea, K., & Mathews, J. D. (1994). Apparent dietary intake in remote Aboriginal
communities. Australian and New Zealand Journal of Public Health, 18(2), 190-197.
Medlineplus.gov. (2018). Obesity: MedlinePlus. Medlineplus.gov. Retrieved 20 March 2018,
from https://medlineplus.gov/obesity.html
Meigs, J. B., Nathan, D. M., Wolfsdorf, J. I., & Mulder, J. E. (2015). The metabolic
syndrome (insulin resistance syndrome or syndrome X). Available in www.
UpToDate. com. Accessed.
Mitchell, N., Catenacci, V., Wyatt, H., & Hill, J. (2011). Obesity: Overview of an
Epidemic. Psychiatric Clinics Of North America, 34(4), 717-732.
http://dx.doi.org/10.1016/j.psc.2011.08.005
14Health and wellbeing
NACCHO, R. (2012). National guide to a preventive health assessment for Aboriginal and
Torres Strait Islander people. South Melbourne: The RACGP.
ncbi.nlm.nih.gov. (2018). Overweight and Obesity. PubMed Health. Retrieved 20 March
2018, from https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0063069/
Neel, J. V. (1999). The “thrifty genotype” in 1998. Nutrition reviews, 57(5), 2-9.
niddk.nih.gov. (2018). Health Risks of Being Overweight | NIDDK. National Institute of
Diabetes and Digestive and Kidney Diseases. Retrieved 21 March 2018, from
https://www.niddk.nih.gov/health-information/weight-management/health-risks-
overweight
Pmc.gov.au. (2018). 2.22 Overweight and obesity | Aboriginal and Torres Strait Islander
Health Performance Framework 2014 Report. Pmc.gov.au. Retrieved 21 March 2018,
from https://www.pmc.gov.au/sites/default/files/publications/indigenous/Health-
Performance-Framework-2014/tier-2-determinants-health/222-overweight-and-
obesity.html
Qasim, A., Turcotte, M., Souza, R. J., Samaan, M. C., Champredon, D., Dushoff, J., ... &
Meyre, D. (2018). On the origin of obesity: identifying the biological, environmental
and cultural drivers of genetic risk among human populations. Obesity Reviews, 19(2),
121-149.
Sartorius, B., Veerman, L., Manyema, M., Chola, L., & Hofman, K. (2015). Determinants of
Obesity and Associated Population Attributability, South Africa: Empirical Evidence
from a National Panel Survey, 2008-2012. PLOS ONE, 10(6), e0130218.
http://dx.doi.org/10.1371/journal.pone.0130218
NACCHO, R. (2012). National guide to a preventive health assessment for Aboriginal and
Torres Strait Islander people. South Melbourne: The RACGP.
ncbi.nlm.nih.gov. (2018). Overweight and Obesity. PubMed Health. Retrieved 20 March
2018, from https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0063069/
Neel, J. V. (1999). The “thrifty genotype” in 1998. Nutrition reviews, 57(5), 2-9.
niddk.nih.gov. (2018). Health Risks of Being Overweight | NIDDK. National Institute of
Diabetes and Digestive and Kidney Diseases. Retrieved 21 March 2018, from
https://www.niddk.nih.gov/health-information/weight-management/health-risks-
overweight
Pmc.gov.au. (2018). 2.22 Overweight and obesity | Aboriginal and Torres Strait Islander
Health Performance Framework 2014 Report. Pmc.gov.au. Retrieved 21 March 2018,
from https://www.pmc.gov.au/sites/default/files/publications/indigenous/Health-
Performance-Framework-2014/tier-2-determinants-health/222-overweight-and-
obesity.html
Qasim, A., Turcotte, M., Souza, R. J., Samaan, M. C., Champredon, D., Dushoff, J., ... &
Meyre, D. (2018). On the origin of obesity: identifying the biological, environmental
and cultural drivers of genetic risk among human populations. Obesity Reviews, 19(2),
121-149.
Sartorius, B., Veerman, L., Manyema, M., Chola, L., & Hofman, K. (2015). Determinants of
Obesity and Associated Population Attributability, South Africa: Empirical Evidence
from a National Panel Survey, 2008-2012. PLOS ONE, 10(6), e0130218.
http://dx.doi.org/10.1371/journal.pone.0130218
15Health and wellbeing
Shannon, C. (2002). Acculturation: aboriginal and torres strait islander nutrition. Asia Pacific
Journal of Clinical Nutrition, 11(s3).
Trewin, D., & Madden, R. (2005). The health and welfare of Australia’s Aboriginal and
Torres Strait Islander peoples. Canberra, Australian Bureau of Statistics.
who.int. (2018). About social determinants of health. World Health Organization. Retrieved
21 March 2018, from http://www.who.int/social_determinants/sdh_definition/en/
World Health Organization. (2018). The Ottawa Charter for Health Promotion. World Health
Organization. Retrieved 21 March 2018, from
http://www.who.int/healthpromotion/conferences/previous/ottawa/en/
Shannon, C. (2002). Acculturation: aboriginal and torres strait islander nutrition. Asia Pacific
Journal of Clinical Nutrition, 11(s3).
Trewin, D., & Madden, R. (2005). The health and welfare of Australia’s Aboriginal and
Torres Strait Islander peoples. Canberra, Australian Bureau of Statistics.
who.int. (2018). About social determinants of health. World Health Organization. Retrieved
21 March 2018, from http://www.who.int/social_determinants/sdh_definition/en/
World Health Organization. (2018). The Ottawa Charter for Health Promotion. World Health
Organization. Retrieved 21 March 2018, from
http://www.who.int/healthpromotion/conferences/previous/ottawa/en/
1 out of 16
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





