NURBN2000: Developing a Health Assessment & Nursing Care Plan
VerifiedAdded on 2023/06/12
Student Number:
School of Nursing, Midwifery and
Healthcare
Faculty of Health
Bachelor of Nursing
NURBN2000
Transition to Nursing Studies
Semester 1, 2018
Assessment 2 Part B
Health Assessment & Nursing
Care Plan Workbook
Paraphrase This Document
Introduction
In Assessment Task 2 –Part B you are required to complete a comprehensive health
assessment and nursing care plan on information given to you in the case study- Mr. Kevin
Jones. The case study information is located in the Book – Case Study Guidelines for
Assessment Task 2 (B).
Using the information gathered from the case study of Mr. Kevin Jones, you are expected to
document the assessment you have undertaken. You are also asked to identify four (4)
priority issues, develop, implement and evaluate your nursing care plan for Mr. Kevin Jones.
All information is to be recorded in this Health Assessment & Nursing Care Plan Workbook.
Your completed Health Assessment & Nursing Care Plan Workbook will be assessed using
the marking guide in the NURBN2000 Moodle shell. Print a copy of the marking guide and
keep it with you while writing your Care Plan to ensure you answer the questions correctly.
Guidelines for Health Assessment and Nursing Care plan (Total: 2000 words)
This assessment relies on students being familiar with the nursing process as you
will be required to follow the steps outlined in this process. If you are not familiar with
this, review in any recommended nursing textbook – however, this has been covered
in your prior EN training.
Complete the workbook, ensuring you have answered all the questions
Students will demonstrate clinical decision making skills in:
1. The Nursing Process.
2. Identification/ assessment of nursing problems (nursing diagnosis)
3. Planning and Implementation of nursing care
4. Documentation of nursing data.
5. Evaluation of nursing care
Read this plan for the assessment task:
Activity-Assessment Task 2: Total 2000 words
600 word assessment
Nursing Care Plan
3 Diagnosis/Problems
Expected outcomes
Interventions
Rationale
Referenced 600 word assessment identifying physical & mental health
components e.g. dehydration may result in anxiety & confusion (Gulanick
& Myers, 2012)
Remaining word count utilised in the rest of document (1400 words)
Your care planning will be based on your assessment data
Develop a Care Plan based on data gathered in your assessment (a,b,c).
Then, identify three (3) main nursing problems and provide goals,
interventions, rationale and implementation of that care.
identified)
Submit Workbook
Adult Health Assessment – Total: 2000 words
Outline:
1. Students are required to discuss the physical and mental health
components for the assessment (600 words). This will need to be written &
referenced according to academic writing & referencing standards.
2. Identify 4 major issues for Kevin Jones, his social history and provide a
summary of your overall assessment of him. Ensure that you use ‘objective’
language. This would be similar to what you would write in nursing notes as
an admission history.
3. Using the Nursing diagnosis section, select the three (3) health nursing
diagnosis that you think are a priority for Kevin and include the evidence from
your assessment that supports this.
4. Now prioritise these 3 important nursing problems to formulate a nursing
care plan for Kevin
5. Develop a nursing care plan with rationale (referenced) and related
interventions that could be implemented for Kevin.
6. Complete the evaluation sections of the care plan - identify ways that you
could measure success in relation to each of these interventions.
1. Write your 600 word referenced assessment below discussing the physical
and mental health components for Kevin. This will need to be written
according to academic writing & referencing standards.(NB: your assessment
will roll into the next page).
The present case study focuses on the condition of a patient named Kevin who had been
a 75 year old man who had gone through a cardiovascular accident or stroke which resulted
into paralysis. The past history of the patient reveals that he had been paralyzed and had
been leaning on one side and forgot where his hand had been in the past which indicates
that he had motor coordination deficiency due to the stroke. He also had speech slurring and
difficulty in verbalization which also caused immense irritation and agitation in the patient. He
also had gait problems and had only started mobilizing with the assistance of three pronged
sticks, hence it also can be mentioned that the patient had persistent fall risk. Along with
that, the patient had been complaining of a chronic cough with a small amount of discoloured
greenish yellow sputum, fever, flushed skin, chills, loss of appetite, taking little fluids, malaise
and body aches over the past few days. The vital signs of the patient revealed temperature
38.3, blood pressure 90/60, and respiratory rate as 24 per min, and oxygen saturation 93%.
The patient also exhibited crackles & wheezes on auscultation with diminished breath
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
risk for dehydration as well (Cumming et al., 2013).
Hence the first component of physical health assessment will be the Primary
assessment following the ABCDE format where the airway, breathing, circulation, disability
and exposure risk of the patient. Here, it has to be mentioned that the patient had been
chronic cough and excess production of sputum which can lead to shortness of breath and
reduced oxygen saturation in the patient and lead to exacerbation of the pneumonia. Second
component of the assessment for the patient will need to focus on specialized secondary
assessment focussing o the key issues. For instance the patent had been suffering from
weight loss, lack of appetite, taking more fluids, malaise and body aches. The pneumonia
infection could have been a contributing factor to the same however the swallowing difficulty
could also have contributed to the lack of appetite and subsequent weight loss as well.
Lastly, the patient mobility restriction and had trouble with maintaining his balance even after
using the three pronged stick; hence, the patient had been under heavy risk of falling which
could lead to patient sustaining injuries. Hence, fall risk assessment will be the third physical
health assessment component (Abubakar & Isezuo, 2012).
For mental health assessment, it has to be mentioned that a cardiovascular accident
has significant impact on altering the mental health of the patient. As the patient had
mentioned lack of coordination and the inability to remember where his hands are, the first
mental health assessment component will be mini-mental state examination. This will help in
identifying the lapse in the cognitive stats of the patient as well. Along with that the mental
health assessment with respect to cognitive status of the patient will include Neurobehavioral
Cognition Status Exam (NCSE) as well. The second component for the mental health
assessment will be the assessment for depression. According to the Bartoli et al. (2013),
almost one third of the total stroke patient population suffers from post stroke depression,
and the possibilities are even higher for those with any temporary or permanent disability. It
has to be mentioned in this context that the patient had been exhibiting signs of frustration
and emotional outbursts as well. Along with that he had been anxious about returning home
and seemed to be fretting about his home, land and animals. The patient had admitted that
he often does not like taking or anyone, barely speaks to his staff and got agitated and
irritable with the nurses, physiotherapists, cleaners as well during his stay in the hospital.
The patient seemed to be ruminating about his past and his wife who had died 13 years ago.
Hence the patient had been showing all signs of depression and needed a depression
assessment using either Beck Depression Inventory or Hamilton Rating Scale for
Depression (Lincoln et al., 2013).
Paraphrase This Document
1. – Pneumonia
2. – Dehydration
3. – Depression
4. – Fall risk
(b) Document Kevin’s social history
Social history of the psychosocial contextual factors of a particular individual has a
significant impact on the health and wellbeing of patient and can play a profound role in the
recovery statistics of the patient as well. For the case study that has been selected for the
assignment, the patient Kevin had been a 75 year old man with three children, two of whom
live outside of Victoria, his native land. However, one of his sons lives nearby although he
cannot give enough time to his father due to his busy schedules. The patient had suffered
from a stroke recently which had rendered him partially paralysed and not able to
successfully complete his activities of daily living. It has to be mentioned that his financial
abilities are limited and he desperately has wished to go back to his house and manage
things on his own due to his need for empowerment and independence. He lives in an old
farm which had not been renovated for 30 years and he has access to bare minimal
necessities in the old farm that he had been living in.
(c) Summary of overall assessment for Kevin
priorities for the patient needs to be identified. It has to be mentioned in this context that the
patent had been suffering from a number of large number of medical concerns. However the
physical and mental health assessment had helped in the sorting of the most pressing care
needs and focusing on the care priorities of the patient. The first and foremost care priority
for the patient the present condition is the lower lobe pneumonia. Along with that, the
physical health assessment also discovered that the patient had been suffering from
dehydration and fall risk. And hence, Kevin will require care strategies focused on
addressing the above mentioned care priorities. For the mental health assessment it was
discovered that his cognitive health had not been much deteriorated however he had been
showing signs of prominent post stroke depression. Hence the fourth care priority will be the
depression.
Identifying Nursing Problems (Diagnosis)
Nursing Diagnosis
A nursing diagnosis is a statement that describes the PERSON’S actual or potential
response to a health problem that requires nursing care. It is a three part statement with
diagnosis, cause and evidence.
Ref: Berman, A., Snyder, S., J., Levett-Jones, T., Dwyer, T., Hales, M., Harvey, N. Luxford,
Y., Moxham, L., Park, T., Parker, B., Reid-Searl, K., Stanley, D. (2014). Kozier &
Erb’s Fundamentals of Nursing (3r Australian Ed.). Pearson: NSW, Australia. 2012, Ch. 13
Page 233 -249
Based on Assessment data you have gathered, select the three (3) priority diagnoses
that you feel are the most appropriate for Kevin.
Ensure you include what evidence you have to support this.
(1) Lower lobe pneumonia
Evidenced by:
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
along with that he patent had been exhibiting consistent chronic coughs, wheezing
and crackles, along with shortness of breath and discoloration of the sputum. The
primary respiratory assessment discovered that the patent had ineffective breathing
pattern and airway obstruction as well.
(2) Dehydration
Evidenced by: The patient had erratic hard bowels and incontinence in urinary
movement. Along with that that patent had admitted to be drinking very little
water or any other fluids. The physical health assessment also discovered
fluid volume deficiency leading to dry and flushed skin.
(3) depression
Evidenced by: Low mood, irritability, emotional outbursts, not talking to the rest of
the staff and reminiscing his time with his decreased wife
Nursing Care Plan (Berman et al, 2012, Ch. 13 Page 233 -273)
To develop the Nursing Care Plan:
Critically analyse, cluster and validate your assessment data for Kevin into the
following format:-
Include three(3) nursing problems diagnosis with Goals (outcomes), Nursing
Interventions, Rationales (reasons)
Write clear statements that clearly reflect the problem. You may use your own
wording.
You may use the health patterns cluster statements below to assist you identify a
nursing diagnosis, or you may use ones that reflect the individual client.
Goals or expected outcomes
Have a time frame and are realistic outcomes related to the nursing diagnosis.
Interventions
Are the nursing actions needed to achieve the goal?
Rationale (must be referenced)
The reasons for nursing interventions are recorded in detail.
Evaluation
Paraphrase This Document
Evaluation consists of:
Collection of data related to outcomes
Comparison of this data with predicted outcomes
Revision of nursing actions to goals and or outcomes
Drawing conclusions about problem status and then continuing, modifying or
terminating the care plan
Documenting changes in nursing interventions and outcomes
Now continue to the Nursing Care Plan below
and enter your data
(Berman et al, 2012, Ch. 14 Page 250 -273
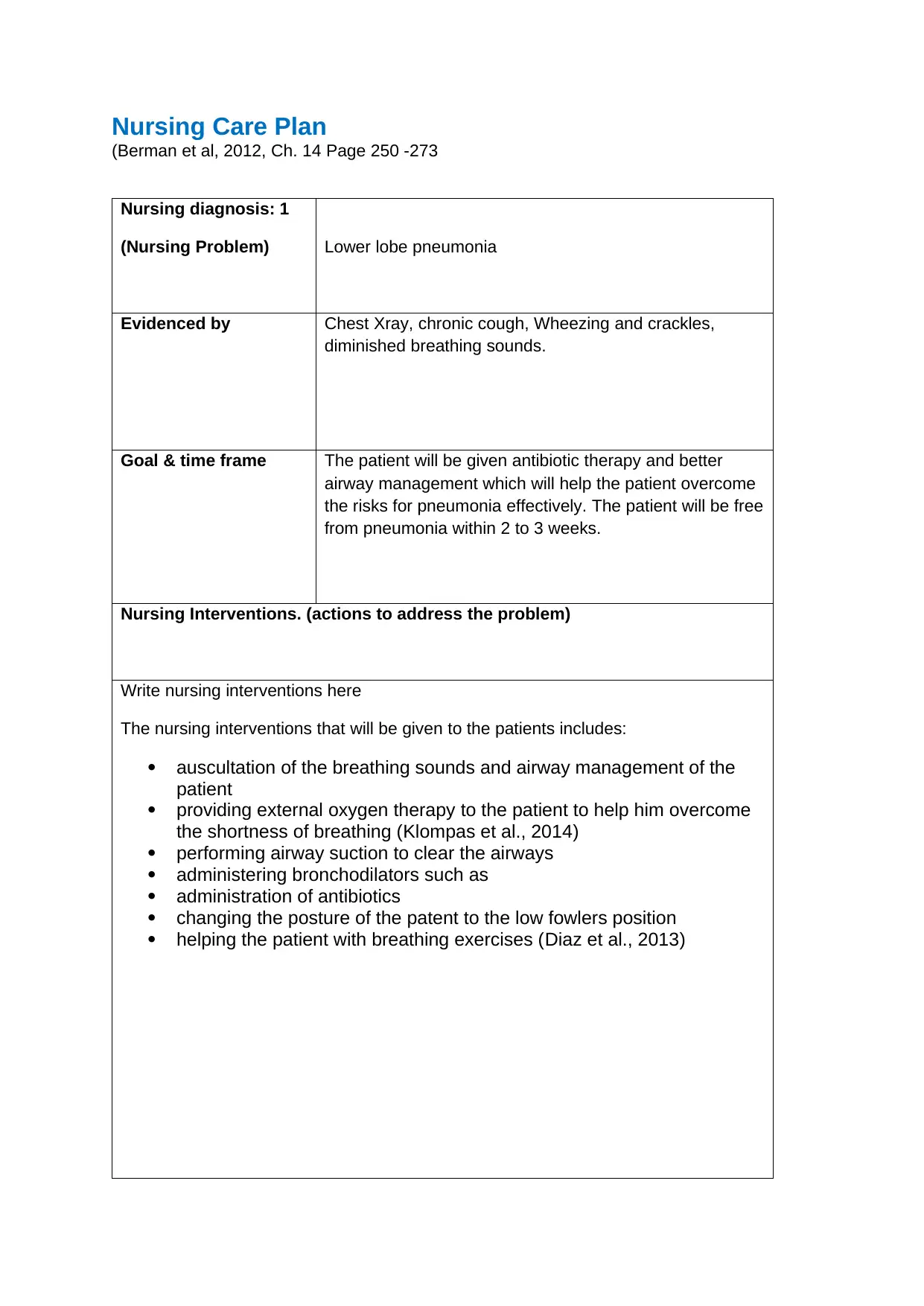
Nursing diagnosis: 1
(Nursing Problem) Lower lobe pneumonia
Evidenced by Chest Xray, chronic cough, Wheezing and crackles,
diminished breathing sounds.
Goal & time frame The patient will be given antibiotic therapy and better
airway management which will help the patient overcome
the risks for pneumonia effectively. The patient will be free
from pneumonia within 2 to 3 weeks.
Nursing Interventions. (actions to address the problem)
Write nursing interventions here
The nursing interventions that will be given to the patients includes:
auscultation of the breathing sounds and airway management of the
patient
providing external oxygen therapy to the patient to help him overcome
the shortness of breathing (Klompas et al., 2014)
performing airway suction to clear the airways
administering bronchodilators such as
administration of antibiotics
changing the posture of the patent to the low fowlers position
helping the patient with breathing exercises (Diaz et al., 2013)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
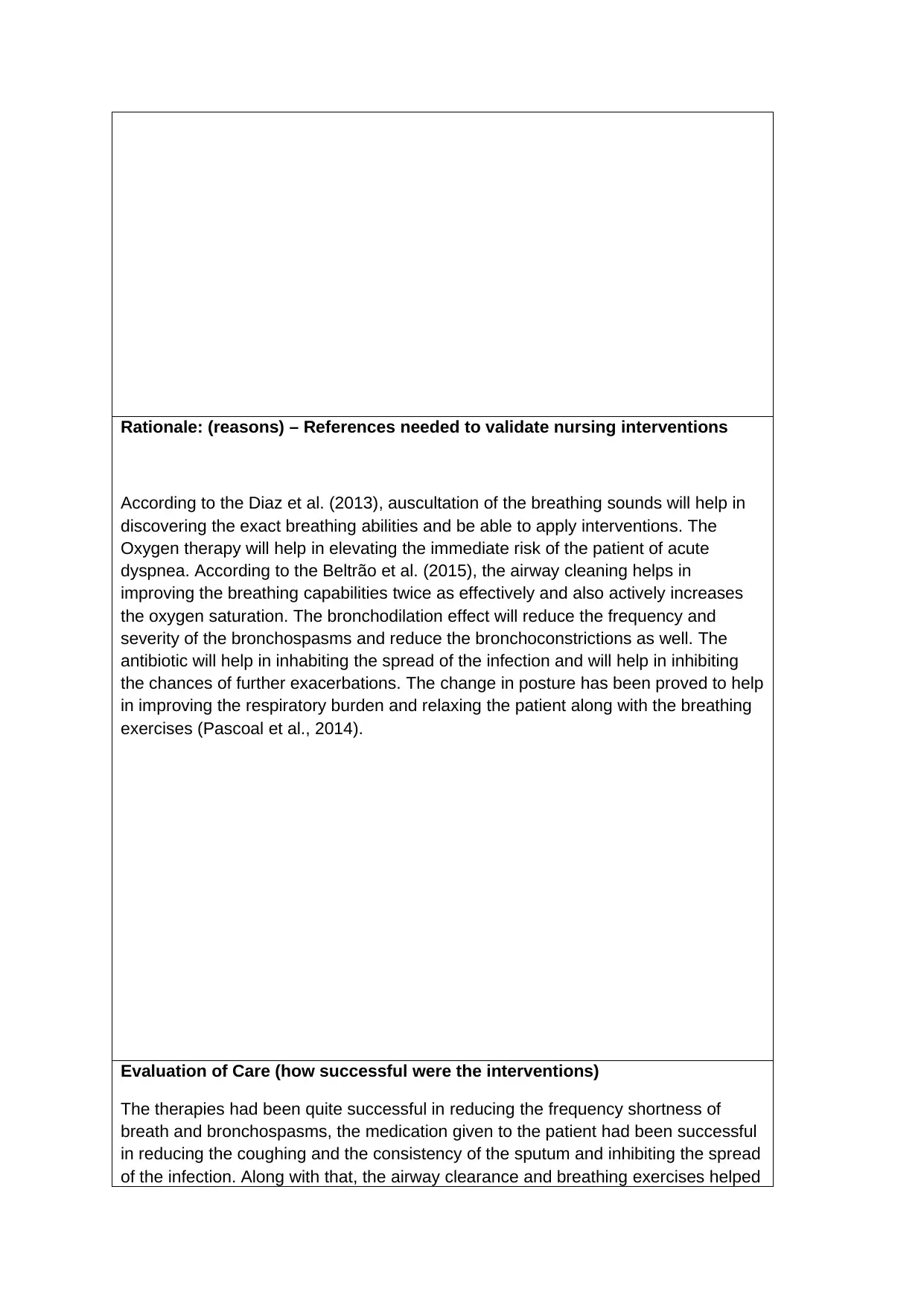
According to the Diaz et al. (2013), auscultation of the breathing sounds will help in
discovering the exact breathing abilities and be able to apply interventions. The
Oxygen therapy will help in elevating the immediate risk of the patient of acute
dyspnea. According to the Beltrão et al. (2015), the airway cleaning helps in
improving the breathing capabilities twice as effectively and also actively increases
the oxygen saturation. The bronchodilation effect will reduce the frequency and
severity of the bronchospasms and reduce the bronchoconstrictions as well. The
antibiotic will help in inhabiting the spread of the infection and will help in inhibiting
the chances of further exacerbations. The change in posture has been proved to help
in improving the respiratory burden and relaxing the patient along with the breathing
exercises (Pascoal et al., 2014).
Evaluation of Care (how successful were the interventions)
The therapies had been quite successful in reducing the frequency shortness of
breath and bronchospasms, the medication given to the patient had been successful
in reducing the coughing and the consistency of the sputum and inhibiting the spread
of the infection. Along with that, the airway clearance and breathing exercises helped
Paraphrase This Document
calming the patient.
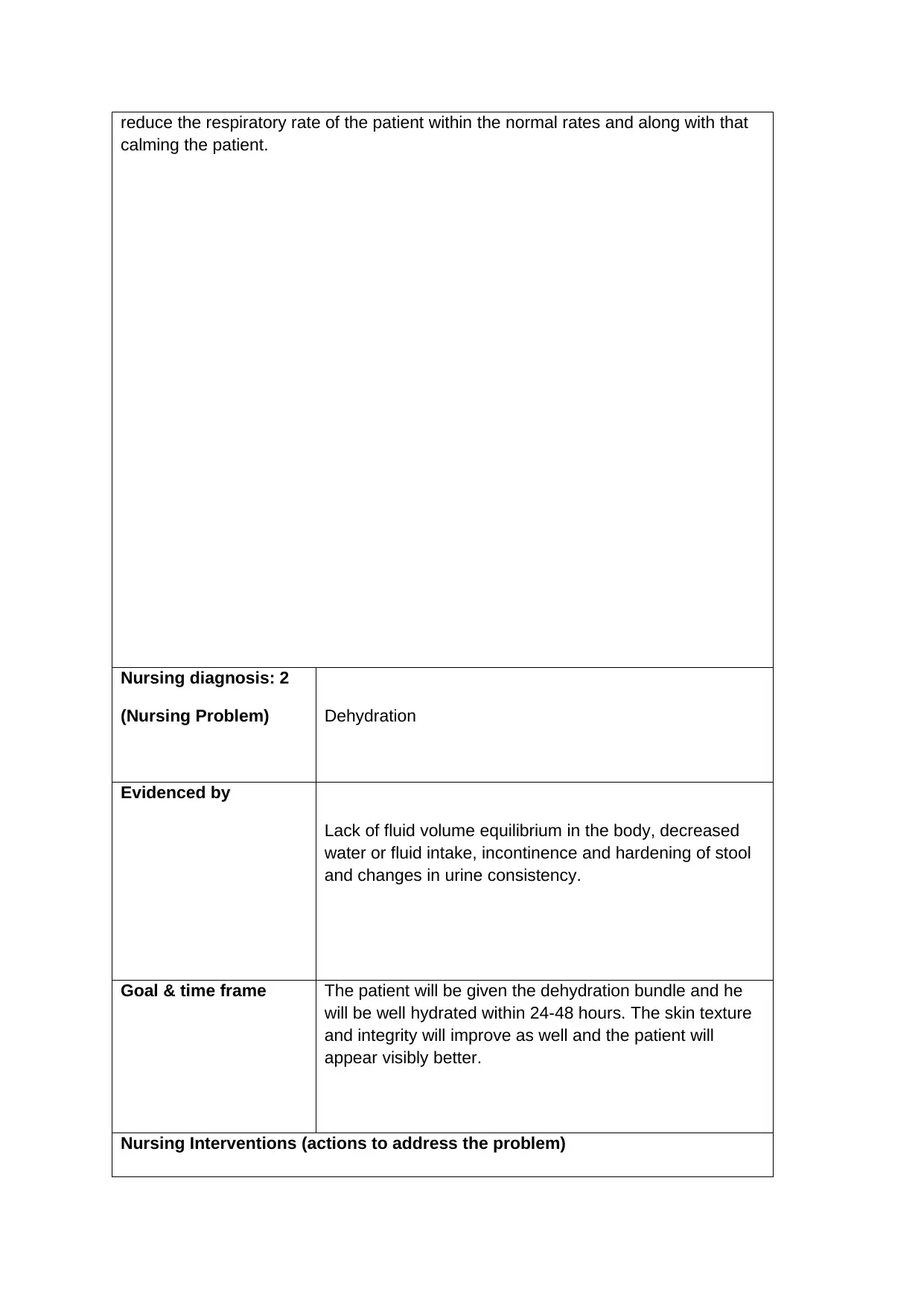
Nursing diagnosis: 2
(Nursing Problem) Dehydration
Evidenced by
Lack of fluid volume equilibrium in the body, decreased
water or fluid intake, incontinence and hardening of stool
and changes in urine consistency.
Goal & time frame The patient will be given the dehydration bundle and he
will be well hydrated within 24-48 hours. The skin texture
and integrity will improve as well and the patient will
appear visibly better.
Nursing Interventions (actions to address the problem)
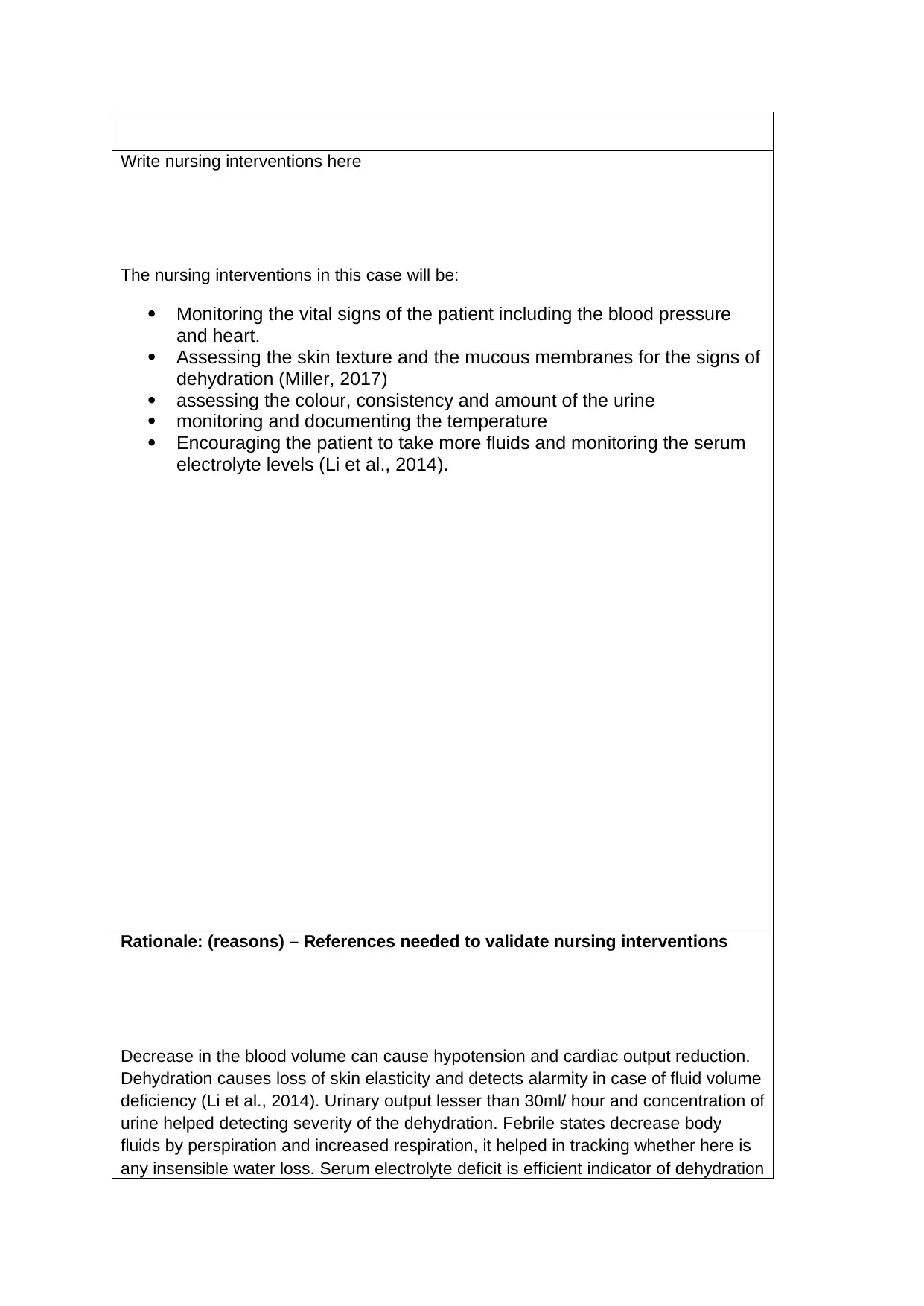
The nursing interventions in this case will be:
Monitoring the vital signs of the patient including the blood pressure
and heart.
Assessing the skin texture and the mucous membranes for the signs of
dehydration (Miller, 2017)
assessing the colour, consistency and amount of the urine
monitoring and documenting the temperature
Encouraging the patient to take more fluids and monitoring the serum
electrolyte levels (Li et al., 2014).
Rationale: (reasons) – References needed to validate nursing interventions
Decrease in the blood volume can cause hypotension and cardiac output reduction.
Dehydration causes loss of skin elasticity and detects alarmity in case of fluid volume
deficiency (Li et al., 2014). Urinary output lesser than 30ml/ hour and concentration of
urine helped detecting severity of the dehydration. Febrile states decrease body
fluids by perspiration and increased respiration, it helped in tracking whether here is
any insensible water loss. Serum electrolyte deficit is efficient indicator of dehydration
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Evaluation of Care (how successful were the interventions)
The interventions helped in better understanding of the condition of Kevin and helped
improve his dehydration status. The elaborate assessment helped in better discovery
of the exact severity of the dehydration and encouragement to take more fluids and
electrolyte therapy helped in reviving his hydration state within roughly 48-52 hours.
The urinary and bowel issues also improved gradually with improved hydration state
Paraphrase This Document
(Nursing Problem)
Fall risk
Evidenced by
Unstable gait, leaning on left side, not being able to locate
his right hand, lack of motor coordination skills .
Goal & time frame
The patient will be free from the fall risk while his stay in
the health care facility. This care goal will be for as long
as the patient stays in the facility.
Nursing Interventions (actions to address the problem)
Write nursing interventions here
The interventions in this case will be:
performing a thorough fall risk assessment for the patient
performing an assessment for checking the disability status of the
patient
decluttering the physical environment of the patient (Costa-Dias et al.,
2014)
making the patient wear non skid footwear and position bed rails to
reduce risk of falling
provide the patient with assistive devices for walking necessary and
placing the call light within his reach
increasing the luminosity of the room Kevin is staying in (Castellan et
al., 2016)
The fall risk assessment helped in discovering the exact contributing factors in this
case and the address those care needs. The decluttering, increased luminosity and
protective bed rails helped in reducing the fall risk effectively (Castellan et al., 2016).
The non skid footwear and the assistive walking aid helped in further reducing the
risk of falling. According to the Costa-Dias et al. (2014), placing the call light and
other necessary stuff within the reach of the patient can help in reducing the fall risk
of the patient.
Evaluation of Care (how successful were the interventions)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
effectively and along with that the patient had been able to verbalize his needs
effectively using the call light and had been devoid of any risk to fall and injury
throughout his stay in the facility.
Start your references on the next page
References
Abubakar, S. A., & Isezuo, S. A. (2012). Health related quality of life of stroke
survivors: experience of a stroke unit. International journal of biomedical
science: IJBS, 8(3), 183.
Bartoli, F., Lillia, N., Lax, A., Crocamo, C., Mantero, V., Carrà, G., ... & Clerici, M.
(2013). Depression after stroke and risk of mortality: a systematic review and
meta-analysis. Stroke research and treatment, 2013.
Beltrão, B. A., Herdman, T. H., Pascoal, L. M., Chaves, D. B. R., Silva, V.
M., & Lopes, M. V. (2015). Ineffective breathing pattern in children
and adolescents with congenital heart disease: accuracy of
defining characteristics. Journal of clinical nursing, 24(17-18),
2505-2513.
Castellan, C., Sluga, S., Spina, E., & Sanson, G. (2016). Nursing diagnoses,
outcomes and interventions as measures of patient complexity and nursing
care requirement in Intensive Care Unit. Journal of advanced nursing, 72(6),
1273-1286
Castellan, C., Sluga, S., Spina, E., & Sanson, G. (2016). Nursing
diagnoses, outcomes and interventions as measures of patient
complexity and nursing care requirement in Intensive Care
Unit. Journal of advanced nursing, 72(6), 1273-1286.
Paraphrase This Document
Moreira, C. N., & José, H. (2014). Medication fall risk in old
hospitalized patients: a retrospective study. Nurse education
today, 34(2), 171-176.
Cumming, T. B., Churilov, L., Lindén, T., & Bernhardt, J. (2013). Montreal Cognitive
Assessment and Mini–Mental State Examination are both valid cognitive tools
in stroke. Acta Neurologica Scandinavica, 128(2), 122-129.
Davidson, P., & Everett, B. (2015). Managing approaches to nursing care
delivery. Transitions in nursing: preparing for professional practice.
Chatswood, New South Wales, Australia: Elsevier Health Sciences, 125-142
Diaz, T., George, A. S., Rao, S. R., Bangura, P. S., Baimba, J. B.,
McMahon, S. A., & Kabano, A. (2013). Healthcare seeking for
diarrhoea, malaria and pneumonia among children in four poor
rural districts in Sierra Leone in the context of free health care:
results of a cross-sectional survey. BMC public health, 13(1), 157.
Klompas, M., Branson, R., Eichenwald, E. C., Greene, L. R., Howell, M.
D., Lee, G., ... & Yokoe, D. S. (2014). Strategies to prevent
ventilator-associated pneumonia in acute care hospitals: 2014
update. Infection Control & Hospital Epidemiology, 35(S2), S133-
S154.
Li, Y., He, R., Ying, X., & Hahn, R. G. (2014). Dehydration,
hemodynamics and fluid volume optimization after induction of
general anesthesia. Clinics, 69(12), 809-816.
Lincoln, N. B., Brinkmann, N., Cunningham, S., Dejaeger, E., De Weerdt, W., Jenni,
W., ... & De Wit, L. (2013). Anxiety and depression after stroke: a 5 year
follow-up. Disability and rehabilitation, 35(2), 140-145.
Miller, C. G. (2017). Dehydration in Nursing Home Residents: A meta-
analysis of causes of dehydration, implications, and those most at
risk
Pascoal, L. M., Lopes, M. V. D. O., da Silva, V. M., Beltrão, B. A., Chaves,
D. B. R., de Santiago, J. M. V., & Herdman, T. H. (2014).
Ineffective breathing pattern: defining characteristics in children
with acute respiratory infection. International journal of nursing
knowledge, 25(1), 54-61.
Pata, R. W., Lord, K., & Lamb, J. (2014). The effect of Pilates based
exercise on mobility, postural stability, and balance in order to
decrease fall risk in older adults. Journal of bodywork and
movement therapies, 18(3), 361-367.
Wagg, A., Gibson, W., Ostaszkiewicz, J., Johnson, T., Markland, A.,
Palmer, M. H., ... & Kirschner‐Hermanns, R. (2015). Urinary

International Consultation on Incontinence. Neurourology and
urodynamics, 34(5), 398-406.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
© 2024 | Zucol Services PVT LTD | All rights reserved.




