Health History - Case Study Template
Assessment 1: Case Study for the course NURS1202: Clinical Practice 1B at the University of Newcastle
12 Pages3970 Words265 Views
Added on 2022-11-18
About This Document
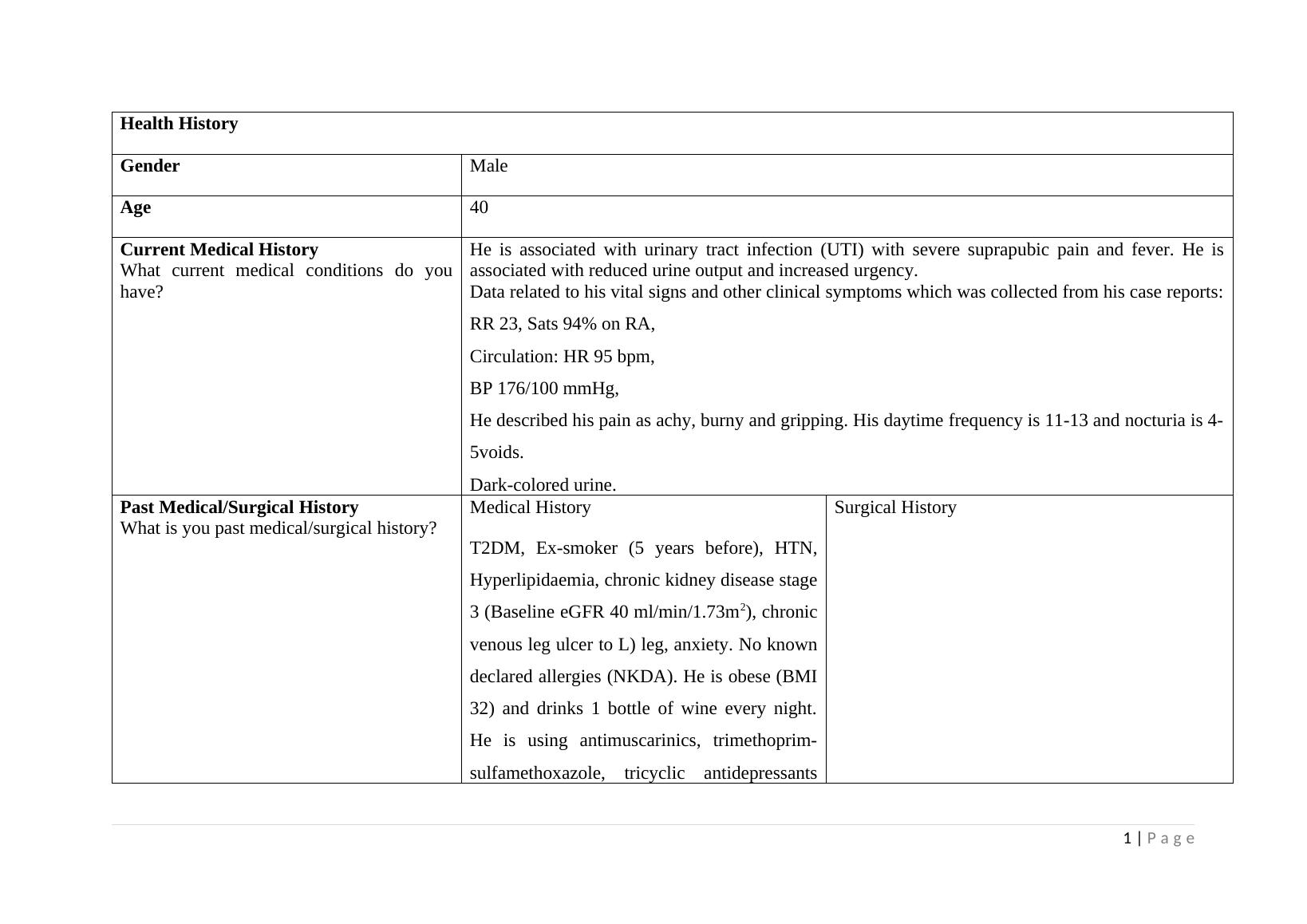
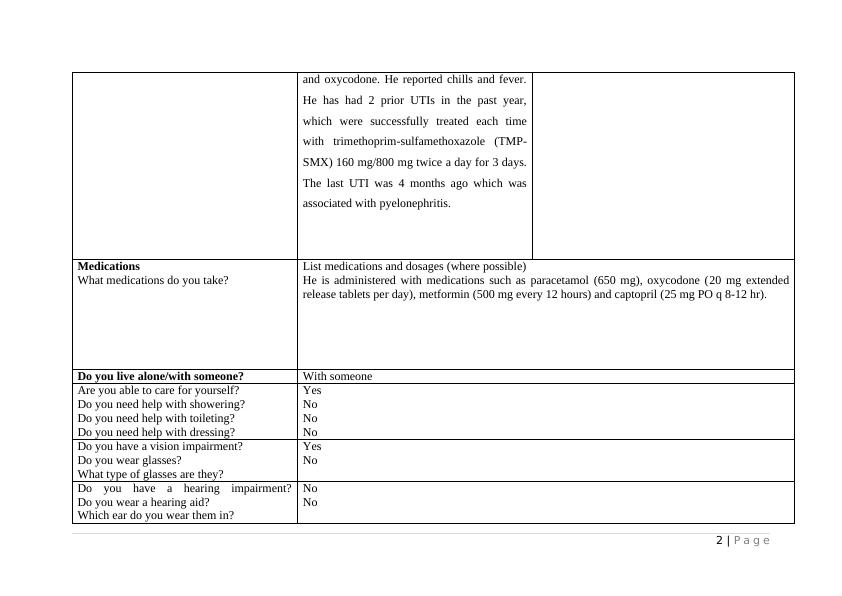
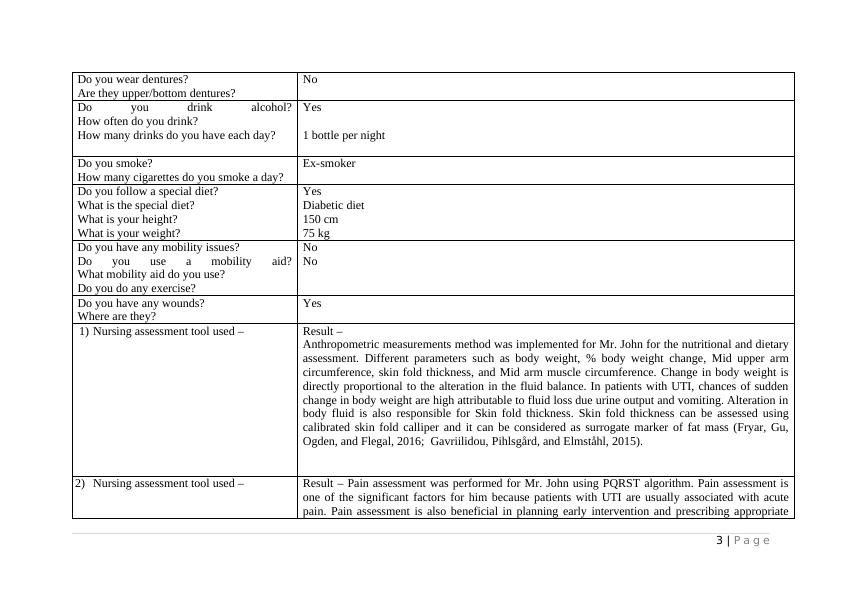
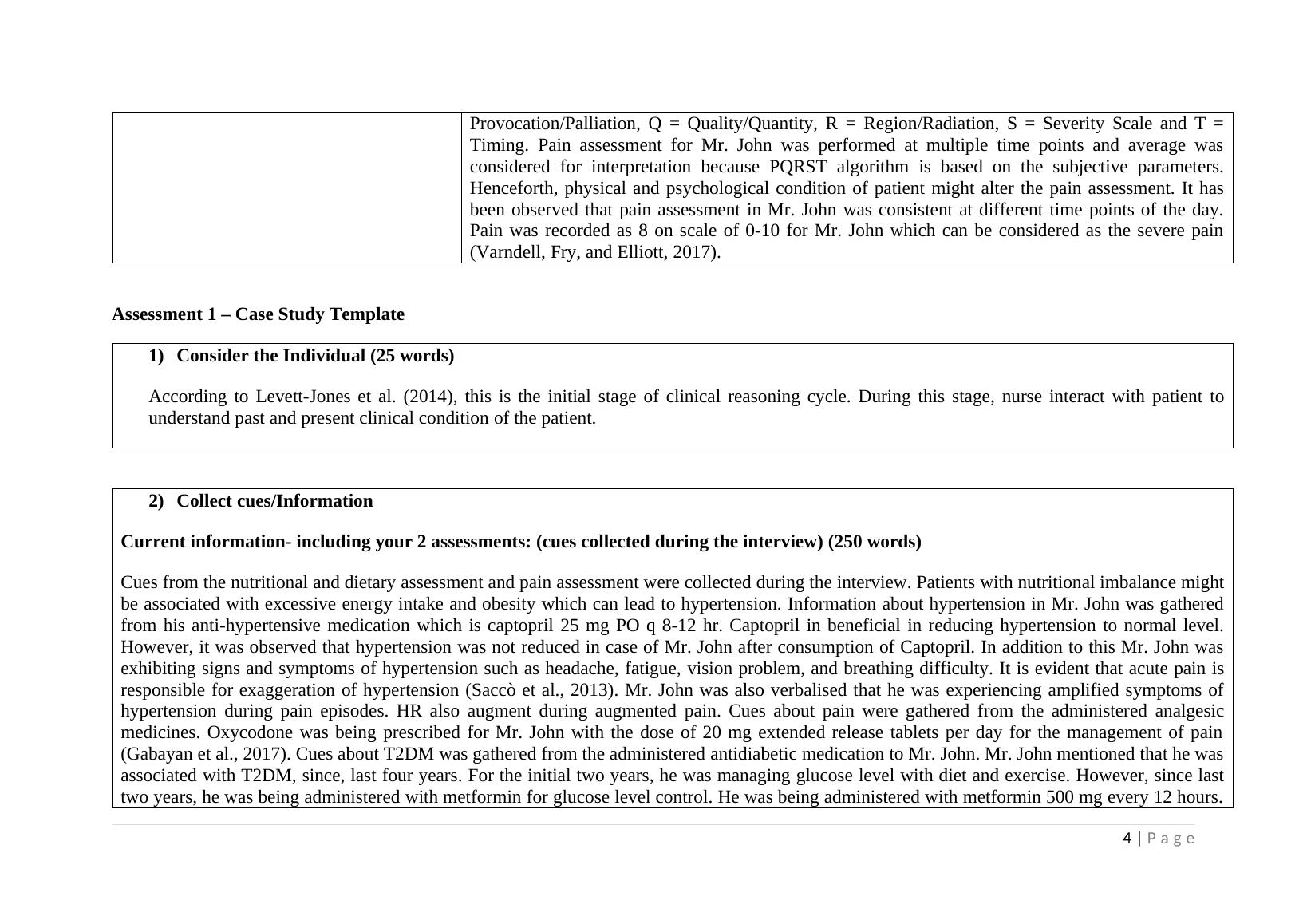
This article presents a case study template for health history assessment of a patient with UTI, T2DM, hypertension, and chronic kidney disease. It includes cues collected during the interview, new assessments that can be conducted, and the interpretation of the results. The article also discusses the nursing problems, goals, and actions that can be taken to improve the patient's condition.
Health History - Case Study Template
Assessment 1: Case Study for the course NURS1202: Clinical Practice 1B at the University of Newcastle
Added on 2022-11-18
ShareRelated Documents
End of preview
Want to access all the pages? Upload your documents or become a member.
Health History of a Female Patient with Urinary Tract Infection
|13
|3809
|205
Clinical Practice Health History Project Report 2022
|27
|3622
|23
REPORT. : CASE STUDY. CASE STUDY. REPORT. REPORT. 1. 1.
|25
|4098
|34
Health History and Assessment: Case Study Template
|17
|2533
|73
Nursing Care of a Patient with Acute on Chronic Renal Failure 2000 Words
|22
|5457
|466