Assessment of COPD Risk Factors: An Evidence-Based Review in Australia
VerifiedAdded on 2023/06/14
|11
|2834
|107
Essay
AI Summary
This essay presents an evidence-based review of Chronic Obstructive Pulmonary Disease (COPD) risk factors, specifically focusing on the Australian Aboriginal population and the impact of smoking. It begins by highlighting the importance of early COPD detection and the author's interest in the topic due to the correlation between smoking and COPD mortality. The review presents evidence supporting smoking avoidance, dietary changes, exercise, and pulmonary rehabilitation as best practices. Annotated bibliographies of three key articles are included, justifying their relevance to the research question and their strengths and limitations. The essay concludes by discussing the relevance of these findings to nursing practice and potential barriers to implementation, such as patient adherence, social support, and awareness of pulmonary rehabilitation programs. The essay emphasizes the integration of best research evidence, clinical expertise, and patient values in evidence-based practice for COPD management.

Running head: ASSESSMENT 3
Evidence Based Health Research and Practice
Name of the Student
Name of the University
Author Note
Evidence Based Health Research and Practice
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1ASSESSMENT 3
Table of Contents
Introduction................................................................................................................................2
Importance of the topic..........................................................................................................2
Interest in the topic.................................................................................................................2
Aim.........................................................................................................................................2
Presenting the evidence..............................................................................................................2
Annotated Bibliography.............................................................................................................3
Justification of literature............................................................................................................5
Relevance to nursing and barriers to practice............................................................................7
References..................................................................................................................................9
Table of Contents
Introduction................................................................................................................................2
Importance of the topic..........................................................................................................2
Interest in the topic.................................................................................................................2
Aim.........................................................................................................................................2
Presenting the evidence..............................................................................................................2
Annotated Bibliography.............................................................................................................3
Justification of literature............................................................................................................5
Relevance to nursing and barriers to practice............................................................................7
References..................................................................................................................................9
2ASSESSMENT 3
Introduction
Importance of the topic
Chronic Obstructive Pulmonary Disease refers to an umbrella term that describes
progressive lung disorders that include chronic bronchitis, emphysema, and refractory
asthma, primarily characterized by breathlessness (López‐Campos, Tan & Soriano, 2016).
The main factors that increase susceptibility of an individual to COPD include an exposure to
irritants that damage the lungs. Owing to the fact that COPD symptoms worsen over time,
there is a need to determine the association of this disorder with its risk factors.
Interest in the topic
I hold the opinion that early detection of COPD would facilitate its prevention and
management in an appropriate way. I gained an interest in conducting this research due to
presence of mounting evidences that smoking is significantly related to high rates of
mortality due to COPD. I also wanted to gain an understanding of factors that might increase
incidence of COPD among non-smokers.
Aim
The research aims to examine the impact of smoking as a risk factor in contracting
COPD among the Australian aboriginal population.
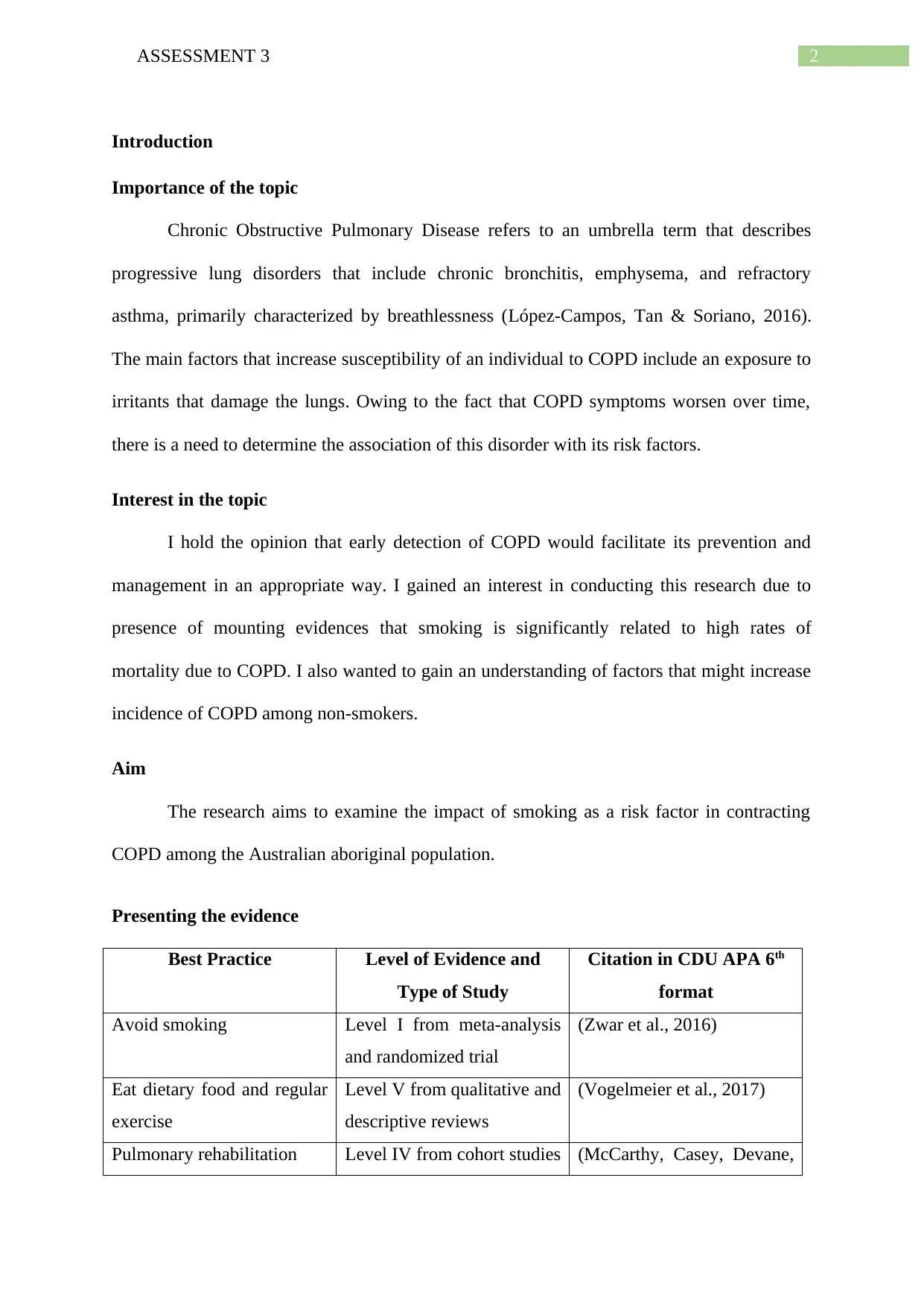
Presenting the evidence
Best Practice Level of Evidence and
Type of Study
Citation in CDU APA 6th
format
Avoid smoking Level I from meta-analysis
and randomized trial
(Zwar et al., 2016)
Eat dietary food and regular
exercise
Level V from qualitative and
descriptive reviews
(Vogelmeier et al., 2017)
Pulmonary rehabilitation Level IV from cohort studies (McCarthy, Casey, Devane,
Introduction
Importance of the topic
Chronic Obstructive Pulmonary Disease refers to an umbrella term that describes
progressive lung disorders that include chronic bronchitis, emphysema, and refractory
asthma, primarily characterized by breathlessness (López‐Campos, Tan & Soriano, 2016).
The main factors that increase susceptibility of an individual to COPD include an exposure to
irritants that damage the lungs. Owing to the fact that COPD symptoms worsen over time,
there is a need to determine the association of this disorder with its risk factors.
Interest in the topic
I hold the opinion that early detection of COPD would facilitate its prevention and
management in an appropriate way. I gained an interest in conducting this research due to
presence of mounting evidences that smoking is significantly related to high rates of
mortality due to COPD. I also wanted to gain an understanding of factors that might increase
incidence of COPD among non-smokers.
Aim
The research aims to examine the impact of smoking as a risk factor in contracting
COPD among the Australian aboriginal population.
Presenting the evidence
Best Practice Level of Evidence and
Type of Study
Citation in CDU APA 6th
format
Avoid smoking Level I from meta-analysis
and randomized trial
(Zwar et al., 2016)
Eat dietary food and regular
exercise
Level V from qualitative and
descriptive reviews
(Vogelmeier et al., 2017)
Pulmonary rehabilitation Level IV from cohort studies (McCarthy, Casey, Devane,
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3ASSESSMENT 3
Murphy, Murphy &Lacasse,
2015)
Annotated Bibliography
1) McCarthy, B., Casey, D., Devane, D., Murphy, K., Murphy, E., &Lacasse, Y. (2015).
Pulmonary rehabilitation for chronic obstructive pulmonary disease. The Cochrane
Library.DOI: 10.1002/14651858.CD003793.pub3
Level IV from cohort studies
McCarthy, Casey, Devane, Murphy, Murphy and Lacasse, (2015) are renowned
individuals in the field of biological/clinical research and their work have been cited by
several other researchers. The primary aim of the review was to compare the impacts of
pulmonary rehabilitation with usual care strategies on health-related QoL, in addition to the
exercise capacity among COPD patients. This review selected RCTs from the Cochrane
Airways Group Specialised Register that focused on pulmonary rehabilitation in COPD
patients that measured HRQoL and maximal or functional exercise capacities. The mean
differences were calculated by random-effects model. No significant difference was observed
in baseline demographics between individuals in the intervention group and those receiving
usual care. Pulmonary rehabilitation produced statistically significant outcomes for fatigue,
emotional function, mastery and dyspnoea. Improvements were also observed in functional
and maximal exercise capacities. The authors concluded that pulmonary rehabilitation can be
administered for improving emotional function and relieving symptoms of fatigue and
breathlessness and dyspnoea in COPD patients.
2) Vogelmeier, C. F., Criner, G. J., Martinez, F. J., Anzueto, A., Barnes, P. J., Bourbeau,
J., ...& Frith, P. (2017). Global strategy for the diagnosis, management and prevention
Murphy, Murphy &Lacasse,
2015)
Annotated Bibliography
1) McCarthy, B., Casey, D., Devane, D., Murphy, K., Murphy, E., &Lacasse, Y. (2015).
Pulmonary rehabilitation for chronic obstructive pulmonary disease. The Cochrane
Library.DOI: 10.1002/14651858.CD003793.pub3
Level IV from cohort studies
McCarthy, Casey, Devane, Murphy, Murphy and Lacasse, (2015) are renowned
individuals in the field of biological/clinical research and their work have been cited by
several other researchers. The primary aim of the review was to compare the impacts of
pulmonary rehabilitation with usual care strategies on health-related QoL, in addition to the
exercise capacity among COPD patients. This review selected RCTs from the Cochrane
Airways Group Specialised Register that focused on pulmonary rehabilitation in COPD
patients that measured HRQoL and maximal or functional exercise capacities. The mean
differences were calculated by random-effects model. No significant difference was observed
in baseline demographics between individuals in the intervention group and those receiving
usual care. Pulmonary rehabilitation produced statistically significant outcomes for fatigue,
emotional function, mastery and dyspnoea. Improvements were also observed in functional
and maximal exercise capacities. The authors concluded that pulmonary rehabilitation can be
administered for improving emotional function and relieving symptoms of fatigue and
breathlessness and dyspnoea in COPD patients.
2) Vogelmeier, C. F., Criner, G. J., Martinez, F. J., Anzueto, A., Barnes, P. J., Bourbeau,
J., ...& Frith, P. (2017). Global strategy for the diagnosis, management and prevention
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4ASSESSMENT 3
of chronic obstructive lung disease 2017 report. Respirology, 22(3), 575-
601.https://doi.org/10.1111/resp.13012
Level V from qualitative and descriptive reviews
Vogelmeier et al., (2017) are well established academicians, interested in investigating
the underlying factors that contribute to a range of cardiovascular and respiratory
abnormalities and their prevention strategies. The aim of the executive summary was to
discuss the assessment of COPD, the risk factors that increase the likelihood of suffering
from it, and impacts of prevention therapy, rehabilitation, education and disease self-
management. The review utilized a plethora of available evidences to define the pathogenesis
of the disease and the factors that influence a progression of the disease. Comprehensive and
succinct information was provided on the symptoms, medical history, assessment and co-
morbidities. The authors suggested that bronchodilators and anti-inflammatory drugs are
effective in treating COPD. Furthermore, they also concluded that in addition to the
aforementioned treatment, non-pharmacological treatment such as, rehabilitation
programmes, exercise, self-management, education and palliative care must also be employed
for COPD prevention and management.
3) Zwar, N. A., Bunker, J. M., Reddel, H. K., Dennis, S. M., Middleton, S., Van
Schayck, O. C., ...&Xuan, W. (2016). Early intervention for chronic obstructive
pulmonary disease by practice nurse and GP teams: a cluster randomized trial. Family
practice, 33(6), 663-670.https://doi.org/10.1093/fampra/cmw077
Level I from meta-analysis and randomized trial
Credibility of the authors Zwar et al., (2016) can be established by the fact that they are
associated with esteemed healthcare and medical institutes in Australia. The authors aimed to
investigate the effectiveness of early nursing interventions on the QoL and care process of
of chronic obstructive lung disease 2017 report. Respirology, 22(3), 575-
601.https://doi.org/10.1111/resp.13012
Level V from qualitative and descriptive reviews
Vogelmeier et al., (2017) are well established academicians, interested in investigating
the underlying factors that contribute to a range of cardiovascular and respiratory
abnormalities and their prevention strategies. The aim of the executive summary was to
discuss the assessment of COPD, the risk factors that increase the likelihood of suffering
from it, and impacts of prevention therapy, rehabilitation, education and disease self-
management. The review utilized a plethora of available evidences to define the pathogenesis
of the disease and the factors that influence a progression of the disease. Comprehensive and
succinct information was provided on the symptoms, medical history, assessment and co-
morbidities. The authors suggested that bronchodilators and anti-inflammatory drugs are
effective in treating COPD. Furthermore, they also concluded that in addition to the
aforementioned treatment, non-pharmacological treatment such as, rehabilitation
programmes, exercise, self-management, education and palliative care must also be employed
for COPD prevention and management.
3) Zwar, N. A., Bunker, J. M., Reddel, H. K., Dennis, S. M., Middleton, S., Van
Schayck, O. C., ...&Xuan, W. (2016). Early intervention for chronic obstructive
pulmonary disease by practice nurse and GP teams: a cluster randomized trial. Family
practice, 33(6), 663-670.https://doi.org/10.1093/fampra/cmw077
Level I from meta-analysis and randomized trial
Credibility of the authors Zwar et al., (2016) can be established by the fact that they are
associated with esteemed healthcare and medical institutes in Australia. The authors aimed to
investigate the effectiveness of early nursing interventions on the QoL and care process of
5ASSESSMENT 3
recently diagnosed COPD patients, compared to those receiving usual care. The RCT was a
multicentred, pragmatic one conducted over a period of 12 months, with blinded outcomes.
Primary outcome measurement was related to HRQoL. Knowledge about the disease, lung
function, smoking and immunisation status, inhaler technique and use of health service were
some of the secondary outcomes. The study findings stated that very few patients in
intervention group saw the nurses. No significant group differences were obtained for the
SGRQ scores. Furthermore, higher rates of influenza immunisation were also observed in the
intervention group. The authors concluded that uptake of intervention was considerably low
and did not produce any additional benefits.
Justification of literature
The selected articles that best matched the PICO question were a systematic review,
an executive summary, and a randomised controlled trial, respectively. Strength of the study
conducted by McCarthy, Casey, Devane, Murphy, Murphy and Lacasse, (2015) can be
attributed to the fact that it was a synthesis or overview of all available evidences related to
the particular research question. Inclusion of 65 studies that involved 3822 patients with
COPD is significant for the research as the large number of included studies provided a
definitive answer to the question about the impact of pulmonary rehabilitation on COPD.
Summarising the large body of evidence helped the review to provide exhaustive information
on the latest developments in this COPD management approach. Furthermore, the review
indicates how well the findings could be implemented to everyday clinical practice, thereby
establishing the generalisability of the findings.
Relevance of the results can be confirmed by other studies that show consistency with
the findings. Better responses in exercise performance, and levels of physical activity in
pulmonary rehabilitation subjected COPD patients, were also proved by another cohort study
(Maddocks et al., 2016). However, limitations can be related to the fact that relevant,
recently diagnosed COPD patients, compared to those receiving usual care. The RCT was a
multicentred, pragmatic one conducted over a period of 12 months, with blinded outcomes.
Primary outcome measurement was related to HRQoL. Knowledge about the disease, lung
function, smoking and immunisation status, inhaler technique and use of health service were
some of the secondary outcomes. The study findings stated that very few patients in
intervention group saw the nurses. No significant group differences were obtained for the
SGRQ scores. Furthermore, higher rates of influenza immunisation were also observed in the
intervention group. The authors concluded that uptake of intervention was considerably low
and did not produce any additional benefits.
Justification of literature
The selected articles that best matched the PICO question were a systematic review,
an executive summary, and a randomised controlled trial, respectively. Strength of the study
conducted by McCarthy, Casey, Devane, Murphy, Murphy and Lacasse, (2015) can be
attributed to the fact that it was a synthesis or overview of all available evidences related to
the particular research question. Inclusion of 65 studies that involved 3822 patients with
COPD is significant for the research as the large number of included studies provided a
definitive answer to the question about the impact of pulmonary rehabilitation on COPD.
Summarising the large body of evidence helped the review to provide exhaustive information
on the latest developments in this COPD management approach. Furthermore, the review
indicates how well the findings could be implemented to everyday clinical practice, thereby
establishing the generalisability of the findings.
Relevance of the results can be confirmed by other studies that show consistency with
the findings. Better responses in exercise performance, and levels of physical activity in
pulmonary rehabilitation subjected COPD patients, were also proved by another cohort study
(Maddocks et al., 2016). However, limitations can be related to the fact that relevant,
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6ASSESSMENT 3
unpublished articles might have been excluded from the study, thereby contributing to
publication bias.
Strength of the executive summary by Vogelmeier et al., (2017) can be attributed to
the fact that provided comprehensive and detailed information on the diagnosis, management
and treatment of COPD, on a global scale. One major advantage is related to the wide body
of epidemiological evidence that the authors have used to describe the pathophysiology of the
disease and the risk factors that result in airflow limitation, a primary characteristic of the
condition. Furthermore, detailed information on COPD symptoms such as, sputum, dyspnoea,
wheezing and cough show consistency with other research articles. The summary presented
information on the medical history of COPD patient that might put them at risk for the
condition, thereby adding to clinical practice guidelines. The summary showed consistency
with articles that related use of bronchodilator therapy with reduced COPD symptoms and
PA related difficulties (Troosters et al., 2016). The summary was also effective in explaining
about the impacts of non-pharmacological COPD interventions, such as, rehabilitation, self-
management and education, supported by evidences. However, lack of statistical data to
prove the effectiveness of the stated interventions fails to establish reliability and validity of
the article.
The RCT conducted by Zwar et al., (2016) has several advantages associated with the
fact that it compared one form of treatment (early intervention) with another (usual care),
with the aim of establishing superiority of one. The study design helped in deriving causal
inferences as it is one of the strongest empirical evidence for efficacy of a treatment. Further
strengths can also be related to the minimisation of allocation and selection bias.
Furthermore, blinding helped to reduce assessment bias. However, there were several
limitations related to falling short of the recruitment target because the study enrolled patients
with early COPD, thereby raising questions about considering smoking cessation as a
unpublished articles might have been excluded from the study, thereby contributing to
publication bias.
Strength of the executive summary by Vogelmeier et al., (2017) can be attributed to
the fact that provided comprehensive and detailed information on the diagnosis, management
and treatment of COPD, on a global scale. One major advantage is related to the wide body
of epidemiological evidence that the authors have used to describe the pathophysiology of the
disease and the risk factors that result in airflow limitation, a primary characteristic of the
condition. Furthermore, detailed information on COPD symptoms such as, sputum, dyspnoea,
wheezing and cough show consistency with other research articles. The summary presented
information on the medical history of COPD patient that might put them at risk for the
condition, thereby adding to clinical practice guidelines. The summary showed consistency
with articles that related use of bronchodilator therapy with reduced COPD symptoms and
PA related difficulties (Troosters et al., 2016). The summary was also effective in explaining
about the impacts of non-pharmacological COPD interventions, such as, rehabilitation, self-
management and education, supported by evidences. However, lack of statistical data to
prove the effectiveness of the stated interventions fails to establish reliability and validity of
the article.
The RCT conducted by Zwar et al., (2016) has several advantages associated with the
fact that it compared one form of treatment (early intervention) with another (usual care),
with the aim of establishing superiority of one. The study design helped in deriving causal
inferences as it is one of the strongest empirical evidence for efficacy of a treatment. Further
strengths can also be related to the minimisation of allocation and selection bias.
Furthermore, blinding helped to reduce assessment bias. However, there were several
limitations related to falling short of the recruitment target because the study enrolled patients
with early COPD, thereby raising questions about considering smoking cessation as a
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7ASSESSMENT 3
primary outcome. Furthermore, no significant effect of self-management intervention on
HRQoL showed discrepancies with previous findings (Bischoff, Akkermans, Bourbeau, van
Weel, Vercoulen & Schermer, 2012). The RCT has other limitations as well that can be
attributed to low attendance rates of the PNs and GPs and their non-adherence to the care
planning and education tools. In addition, lack of representativeness of the practices in
Australia is associated with sending the invitations via the professional healthcare
organisations. Failure to deliver the intervention according to the plan was another major
drawback, which proves that lack of reliability of the results.
Relevance to nursing and barriers to practice
The three basic principles of evidence-based practice (EBP) that can be implemented
include use of best available evidences, clinical expertise and paying attention to the values
and preferences of the patients. Findings obtained from the articles discussed above can be
implemented in a clinical scenario by utilizing the fact that implementation of pulmonary
rehabilitation intervention in COPD patients will allow them to adhere to a program of
education, exercise and self-management and will also provide the necessary support to help
them learn breathing and functioning at the highest possible levels (Grosbois et al., 2015).
Use of the available evidences will allow the healthcare professionals to improve the physical
condition of the patients, by taking into account their health history, level of activity and
exposure to risk factors. Patient preferences might include avoidance of breathlessness and
dyspnoea, and night-time waking due to their presenting complaints (Spruit et al., 2013).
Increased availability of information and a positive patient-physician relationship, with
autonomy maintenance are other preferences.
Some of the barriers in this EBP might be associated with smoking status of the
aboriginal patients, and the availability of social support. Smoking status has been identified
as a major predictor of adherence and attendance to PR. Smokers tend to display less
primary outcome. Furthermore, no significant effect of self-management intervention on
HRQoL showed discrepancies with previous findings (Bischoff, Akkermans, Bourbeau, van
Weel, Vercoulen & Schermer, 2012). The RCT has other limitations as well that can be
attributed to low attendance rates of the PNs and GPs and their non-adherence to the care
planning and education tools. In addition, lack of representativeness of the practices in
Australia is associated with sending the invitations via the professional healthcare
organisations. Failure to deliver the intervention according to the plan was another major
drawback, which proves that lack of reliability of the results.
Relevance to nursing and barriers to practice
The three basic principles of evidence-based practice (EBP) that can be implemented
include use of best available evidences, clinical expertise and paying attention to the values
and preferences of the patients. Findings obtained from the articles discussed above can be
implemented in a clinical scenario by utilizing the fact that implementation of pulmonary
rehabilitation intervention in COPD patients will allow them to adhere to a program of
education, exercise and self-management and will also provide the necessary support to help
them learn breathing and functioning at the highest possible levels (Grosbois et al., 2015).
Use of the available evidences will allow the healthcare professionals to improve the physical
condition of the patients, by taking into account their health history, level of activity and
exposure to risk factors. Patient preferences might include avoidance of breathlessness and
dyspnoea, and night-time waking due to their presenting complaints (Spruit et al., 2013).
Increased availability of information and a positive patient-physician relationship, with
autonomy maintenance are other preferences.
Some of the barriers in this EBP might be associated with smoking status of the
aboriginal patients, and the availability of social support. Smoking status has been identified
as a major predictor of adherence and attendance to PR. Smokers tend to display less
8ASSESSMENT 3
inclination towards adoption of PR based health promotion behaviours. Furthermore, women
with lack of social support are less likely to develop compliance towards this prevention
program (Hayton et al., 2016). Most aboriginal participants might not be aware of the
existence of pulmonary rehabilitation programs, thereby demonstrating uncertainty about the
evidence. Lack of appropriate knowledge regarding referral of patients to the intervention and
difficulties of the aboriginal COPD patients to attend the rehabilitation programs outside their
home will also act as barriers (Johnston, Young, Grimmer, Antic & Frith, 2013). Negative
views of the relative benefits and costs of the program also need to be considered. Therefore,
efforts should be taken to eliminate or reduce all the barriers, before implementation of the
evidence-based intervention.
inclination towards adoption of PR based health promotion behaviours. Furthermore, women
with lack of social support are less likely to develop compliance towards this prevention
program (Hayton et al., 2016). Most aboriginal participants might not be aware of the
existence of pulmonary rehabilitation programs, thereby demonstrating uncertainty about the
evidence. Lack of appropriate knowledge regarding referral of patients to the intervention and
difficulties of the aboriginal COPD patients to attend the rehabilitation programs outside their
home will also act as barriers (Johnston, Young, Grimmer, Antic & Frith, 2013). Negative
views of the relative benefits and costs of the program also need to be considered. Therefore,
efforts should be taken to eliminate or reduce all the barriers, before implementation of the
evidence-based intervention.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9ASSESSMENT 3
References
Bischoff, E. W., Akkermans, R., Bourbeau, J., van Weel, C., Vercoulen, J. H., &Schermer, T.
R. (2012). Comprehensive self management and routine monitoring in chronic
obstructive pulmonary disease patients in general practice: randomised controlled
trial. Bmj, 345, e7642.https://doi.org/10.1136/bmj.e7642
Grosbois, J. M., Gicquello, A., Langlois, C., Le Rouzic, O., Bart, F., Wallaert, B., &
Chenivesse, C. (2015). Long-term evaluation of home-based pulmonary rehabilitation
in patients with COPD. International journal of chronic obstructive pulmonary
disease, 10, 2037. doi: 10.2147/COPD.S90534
Hayton, C., Clark, A., Olive, S., Browne, P., Galey, P., Knights, E., ... & Wilson, A. M.
(2013). Barriers to pulmonary rehabilitation: characteristics that predict patient
attendance and adherence. Respiratory medicine, 107(3), 401-407. doi:
10.1016/j.rmed.2012.11.016
Johnston, K. N., Young, M., Grimmer, K. A., Antic, R., & Frith, P. A. (2013). Barriers to,
and facilitators for, referral to pulmonary rehabilitation in COPD patients from the
perspective of Australian general practitioners: a qualitative study. Primary Care
Respiratory Journal, 22, 319-324. doi:10.4104/pcrj.2013.00062
López‐Campos, J. L., Tan, W., & Soriano, J. B. (2016). Global burden of
COPD. Respirology, 21(1), 14-23. https://doi.org/10.1111/resp.12660
Maddocks, M., Kon, S. S., Canavan, J. L., Jones, S. E., Nolan, C. M., Labey, A., ...& Man,
W. D. (2016). Physical frailty and pulmonary rehabilitation in COPD: a prospective
cohort study. Thorax, thoraxjnl-2016., 71. doi: 10.1136/thoraxjnl-2016-209462
References
Bischoff, E. W., Akkermans, R., Bourbeau, J., van Weel, C., Vercoulen, J. H., &Schermer, T.
R. (2012). Comprehensive self management and routine monitoring in chronic
obstructive pulmonary disease patients in general practice: randomised controlled
trial. Bmj, 345, e7642.https://doi.org/10.1136/bmj.e7642
Grosbois, J. M., Gicquello, A., Langlois, C., Le Rouzic, O., Bart, F., Wallaert, B., &
Chenivesse, C. (2015). Long-term evaluation of home-based pulmonary rehabilitation
in patients with COPD. International journal of chronic obstructive pulmonary
disease, 10, 2037. doi: 10.2147/COPD.S90534
Hayton, C., Clark, A., Olive, S., Browne, P., Galey, P., Knights, E., ... & Wilson, A. M.
(2013). Barriers to pulmonary rehabilitation: characteristics that predict patient
attendance and adherence. Respiratory medicine, 107(3), 401-407. doi:
10.1016/j.rmed.2012.11.016
Johnston, K. N., Young, M., Grimmer, K. A., Antic, R., & Frith, P. A. (2013). Barriers to,
and facilitators for, referral to pulmonary rehabilitation in COPD patients from the
perspective of Australian general practitioners: a qualitative study. Primary Care
Respiratory Journal, 22, 319-324. doi:10.4104/pcrj.2013.00062
López‐Campos, J. L., Tan, W., & Soriano, J. B. (2016). Global burden of
COPD. Respirology, 21(1), 14-23. https://doi.org/10.1111/resp.12660
Maddocks, M., Kon, S. S., Canavan, J. L., Jones, S. E., Nolan, C. M., Labey, A., ...& Man,
W. D. (2016). Physical frailty and pulmonary rehabilitation in COPD: a prospective
cohort study. Thorax, thoraxjnl-2016., 71. doi: 10.1136/thoraxjnl-2016-209462
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10ASSESSMENT 3
McCarthy, B., Casey, D., Devane, D., Murphy, K., Murphy, E., &Lacasse, Y. (2015).
Pulmonary rehabilitation for chronic obstructive pulmonary disease. The Cochrane
Library.DOI: 10.1002/14651858.CD003793.pub3
Safka, K. A., & McIvor, R. A. (2015). Non-pharmacological management of chronic
obstructive pulmonary disease. The Ulster medical journal, 84(1), 13. Retrieved from:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4330800/pdf/umj0084-0013.pdf
Spruit, M. A., Singh, S. J., Garvey, C., ZuWallack, R., Nici, L., Rochester, C., ... & Pitta, F.
(2013). An official American Thoracic Society/European Respiratory Society
statement: key concepts and advances in pulmonary rehabilitation. American journal
of respiratory and critical care medicine, 188(8), e13-e64.
https://doi.org/10.1164/rccm.201309-1634ST
Troosters, T., Lavoie, K., Leidy, N., Maltais, F., Sedeno, M., Janssens, W., ...&Bourbeau, J.
(2016). LATE-BREAKING ABSTRACT: Effects of bronchodilator therapy and
exercise training, added to a self-management behaviour-modification programme, on
physical activity in COPD.,48: PA713. DOI: 10.1183/13993003.congress-
2016.PA713
Vogelmeier, C. F., Criner, G. J., Martinez, F. J., Anzueto, A., Barnes, P. J., Bourbeau, J., ...&
Frith, P. (2017). Global strategy for the diagnosis, management and prevention of
chronic obstructive lung disease 2017 report. Respirology, 22(3), 575-
601.https://doi.org/10.1111/resp.13012
Zwar, N. A., Bunker, J. M., Reddel, H. K., Dennis, S. M., Middleton, S., Van Schayck, O. C.,
...&Xuan, W. (2016). Early intervention for chronic obstructive pulmonary disease by
practice nurse and GP teams: a cluster randomized trial. Family practice, 33(6), 663-
670.https://doi.org/10.1093/fampra/cmw077
McCarthy, B., Casey, D., Devane, D., Murphy, K., Murphy, E., &Lacasse, Y. (2015).
Pulmonary rehabilitation for chronic obstructive pulmonary disease. The Cochrane
Library.DOI: 10.1002/14651858.CD003793.pub3
Safka, K. A., & McIvor, R. A. (2015). Non-pharmacological management of chronic
obstructive pulmonary disease. The Ulster medical journal, 84(1), 13. Retrieved from:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4330800/pdf/umj0084-0013.pdf
Spruit, M. A., Singh, S. J., Garvey, C., ZuWallack, R., Nici, L., Rochester, C., ... & Pitta, F.
(2013). An official American Thoracic Society/European Respiratory Society
statement: key concepts and advances in pulmonary rehabilitation. American journal
of respiratory and critical care medicine, 188(8), e13-e64.
https://doi.org/10.1164/rccm.201309-1634ST
Troosters, T., Lavoie, K., Leidy, N., Maltais, F., Sedeno, M., Janssens, W., ...&Bourbeau, J.
(2016). LATE-BREAKING ABSTRACT: Effects of bronchodilator therapy and
exercise training, added to a self-management behaviour-modification programme, on
physical activity in COPD.,48: PA713. DOI: 10.1183/13993003.congress-
2016.PA713
Vogelmeier, C. F., Criner, G. J., Martinez, F. J., Anzueto, A., Barnes, P. J., Bourbeau, J., ...&
Frith, P. (2017). Global strategy for the diagnosis, management and prevention of
chronic obstructive lung disease 2017 report. Respirology, 22(3), 575-
601.https://doi.org/10.1111/resp.13012
Zwar, N. A., Bunker, J. M., Reddel, H. K., Dennis, S. M., Middleton, S., Van Schayck, O. C.,
...&Xuan, W. (2016). Early intervention for chronic obstructive pulmonary disease by
practice nurse and GP teams: a cluster randomized trial. Family practice, 33(6), 663-
670.https://doi.org/10.1093/fampra/cmw077
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





