Applied Ethics and Law for Health Service Managers
VerifiedAdded on 2023/06/05
|12
|4256
|175
AI Summary
The essay discusses the Open Disclosure system in healthcare and the ethical and legal considerations in medical terms. It also covers the rights and responsibilities of clinical staff and critical success factors associated with the OD process in healthcare.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running Head: ETHICS AND LAW FOR HEALTH SERVICE MANAGERS 0
Applied Ethics and Law for Health Service Managers
9/20/2018
Applied Ethics and Law for Health Service Managers
9/20/2018
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
ETHICS AND LAW FOR HEALTH SERVICE MANAGERS 1
Introduction
The essay brings about the discussion of the health consumer journey in any
healthcare system, and the related aspects. Every healthcare system identifies some clinical
incidents or misadventures during the treatment of their patients depending upon the case.
Medical misadventures are increasing day-by-day causing harm to the patient, also affecting
the healthcare. Number of cases associated to death of the patient is reported frequently,
leading to the increasing medical lawsuits in the healthcare settings. Misadventures or
incidents are the results of the errors or faults in the treatment of the patients (Hall,
Orentlicher, Bobinski, Bagley & Cohen, 2018).
As the topic discusses about the applied law and ethics for the health service
managers, it is assumed that like other organisations, healthcare system must be ethical in
their operations. Health service managers must aim at reducing medical errors, which may
occur due to human mistake or some technical issue, so that they can enhance patient safety.
In addition, to ensure patient safety, it is done to ensure the health and wellbeing of the
patient. Therefore, the duties and responsibilities of the clinical staff in the hospitals are
important factors in ensuring patient health and safety through the effective implementation
of the open disclosure plan. Thus, the essay in the later part describes about the open
disclosure system well in the healthcare, and the ethical and legal considerations in medical
terms (Harrison, Walton, Manias, Mears & Plumb, 2017).
Open disclosure in healthcare
In the healthcare system, effective management of the health and safety is a major
concern, which determines the efficiency in clinical practices and positive outcomes.
According to the perspectives of the clinical professionals, it has stated that they believe that
open disclosure increases the probability of the lawsuit, in relation to the mishap in clinical
practices. Misadventures in the clinical practices described in many forms, such that they
occur as medication errors, complications in the surgery, procedural errors, misdiagnosis,
nosocomial infections, fall, or slips during the treatment period. This leads to the patient
taking legal actions with respect to the problems faced by them, perceived by improper
handling, poor communication or due to the delay in treatment even after identifying the
event. The legal actions or decisions taken by the patient and their family, has led to the
Introduction
The essay brings about the discussion of the health consumer journey in any
healthcare system, and the related aspects. Every healthcare system identifies some clinical
incidents or misadventures during the treatment of their patients depending upon the case.
Medical misadventures are increasing day-by-day causing harm to the patient, also affecting
the healthcare. Number of cases associated to death of the patient is reported frequently,
leading to the increasing medical lawsuits in the healthcare settings. Misadventures or
incidents are the results of the errors or faults in the treatment of the patients (Hall,
Orentlicher, Bobinski, Bagley & Cohen, 2018).
As the topic discusses about the applied law and ethics for the health service
managers, it is assumed that like other organisations, healthcare system must be ethical in
their operations. Health service managers must aim at reducing medical errors, which may
occur due to human mistake or some technical issue, so that they can enhance patient safety.
In addition, to ensure patient safety, it is done to ensure the health and wellbeing of the
patient. Therefore, the duties and responsibilities of the clinical staff in the hospitals are
important factors in ensuring patient health and safety through the effective implementation
of the open disclosure plan. Thus, the essay in the later part describes about the open
disclosure system well in the healthcare, and the ethical and legal considerations in medical
terms (Harrison, Walton, Manias, Mears & Plumb, 2017).
Open disclosure in healthcare
In the healthcare system, effective management of the health and safety is a major
concern, which determines the efficiency in clinical practices and positive outcomes.
According to the perspectives of the clinical professionals, it has stated that they believe that
open disclosure increases the probability of the lawsuit, in relation to the mishap in clinical
practices. Misadventures in the clinical practices described in many forms, such that they
occur as medication errors, complications in the surgery, procedural errors, misdiagnosis,
nosocomial infections, fall, or slips during the treatment period. This leads to the patient
taking legal actions with respect to the problems faced by them, perceived by improper
handling, poor communication or due to the delay in treatment even after identifying the
event. The legal actions or decisions taken by the patient and their family, has led to the
ETHICS AND LAW FOR HEALTH SERVICE MANAGERS 2
emergence of the introducing the open disclosure (Birks, Harrison, Bosanquet, Hall, Harden,
Entwistle & Adamson, 2014).
Open disclosure itself discusses the meaning of the term, i.e. open discussion of the
incidents in the presented healthcare to their patients, family, and other support persons.
Disclosure of the incidents to the patient carried out during the time-period of their treatment,
and it is the right of patients, therefore anchored in the clinical practices. The necessary
elements of the open disclosure system described in the national Australian Open Disclosure
Framework. The Commission and the authority on 13th march endorsed the open disclosure
(OD) framework. The framework is designed to enable the health care organisations, to
communicate openly about the incidents and the ill functioning of their practices. Moreover,
the framework provides a common and consistent basis for the open disclosure in the
Australian healthcare (Boudreau & Lakhani, 2015).
The key principles of the open disclosure framework include, expression of the regret,
disclosure of the clinical incidents to the patients, support, and training to the clinical staff,
clinical governance, ensuring and maintaining confidentiality, and fairness in operations. Not
all, but few clinical incidents require the initiation of clinical disclosure process in the
healthcare. Few incidents consist, of a clinical incident, which involves a required change in
the patient care, thus leading to the application of the process of clinical disclosure. Some
other incidents, which may be included, are those incidents that may lead to the serious future
health consequences even if the risk probability is less (Clinical Excellence Commission,
2013).
Information provided to the Consumers/patients at the time of health-service
Discussing about the time to be taken for initiation for the open disclosure, to the
patient it has been stated that the intimation must be given ideally within 24 hours of the
occurrence of the clinical incident. In addition, responsibility to handle disclosure of the
clinical incident of the patient must be given to the person, known to the patient in the case.
Therefore, considering the aspects of the open disclosure framework in the healthcare system
to be incorporated in every healthcare setting as a mandatory practice.
According to the principles of Open disclosure framework, stated that the consumers
or the patients are to be given necessary information, well in advance, during the period of
health service. Communicating the cause and effects of the incident is necessary to establish
emergence of the introducing the open disclosure (Birks, Harrison, Bosanquet, Hall, Harden,
Entwistle & Adamson, 2014).
Open disclosure itself discusses the meaning of the term, i.e. open discussion of the
incidents in the presented healthcare to their patients, family, and other support persons.
Disclosure of the incidents to the patient carried out during the time-period of their treatment,
and it is the right of patients, therefore anchored in the clinical practices. The necessary
elements of the open disclosure system described in the national Australian Open Disclosure
Framework. The Commission and the authority on 13th march endorsed the open disclosure
(OD) framework. The framework is designed to enable the health care organisations, to
communicate openly about the incidents and the ill functioning of their practices. Moreover,
the framework provides a common and consistent basis for the open disclosure in the
Australian healthcare (Boudreau & Lakhani, 2015).
The key principles of the open disclosure framework include, expression of the regret,
disclosure of the clinical incidents to the patients, support, and training to the clinical staff,
clinical governance, ensuring and maintaining confidentiality, and fairness in operations. Not
all, but few clinical incidents require the initiation of clinical disclosure process in the
healthcare. Few incidents consist, of a clinical incident, which involves a required change in
the patient care, thus leading to the application of the process of clinical disclosure. Some
other incidents, which may be included, are those incidents that may lead to the serious future
health consequences even if the risk probability is less (Clinical Excellence Commission,
2013).
Information provided to the Consumers/patients at the time of health-service
Discussing about the time to be taken for initiation for the open disclosure, to the
patient it has been stated that the intimation must be given ideally within 24 hours of the
occurrence of the clinical incident. In addition, responsibility to handle disclosure of the
clinical incident of the patient must be given to the person, known to the patient in the case.
Therefore, considering the aspects of the open disclosure framework in the healthcare system
to be incorporated in every healthcare setting as a mandatory practice.
According to the principles of Open disclosure framework, stated that the consumers
or the patients are to be given necessary information, well in advance, during the period of
health service. Communicating the cause and effects of the incident is necessary to establish
ETHICS AND LAW FOR HEALTH SERVICE MANAGERS 3
a plan to eradicate the problem and reduce the occurrence of further incidents. Firstly, it is
necessary to inform the consumer or the patient about what exactly happened, i.e. about the
incident in a timely, open, and honest manner. All the adverse events and the consequences,
which might occur in the future described to the patient, and their family members. The
information given with respect to the open disclosure, to the patient during health services
also includes the steps taken to improve the health of the patient. They need to be given
information regarding the process of open disclosure with respect to their case. The process
of the OD will include a guide and the technological methods for the consumers/patients and
the information related to the positive results of the Open disclosure process (De Rassenfosse,
Palangkaraya & Webster, 2016).
Information given to clinical staff about Open Disclosure
Open disclosure framework in the healthcare settings, involves the role of, the patients
as well as the staff and other health professionals. Adequate access to the information should
be provided to staff, so that they can fulfil their roles and responsibilities. To support the staff
members, the health organisations must ensure following things, listed below (Elwy,
Bokhour, Maguire, Wagner, Asch, Gifford & Jesse, 2014).
Staff authorities in the healthcare, must be informed about the incident investigation
and the outcomes, obtained from it. The most important information regarding the incident is
the skills provided to the staff to effectively manage, and communicate to the patient. Thus,
through delivering this kind of information to thee staff, they will be able to get social and
psychological support from the health service organisations. Other includes making a
provision of the support system, presently available for those clinicians distressed by the
incident. The support system available to the clinicians or the health professionals, include
the medical defence organisations, doctors, health advisory services, committees and other
health service counsellors. In addition, they are given opportunities to discuss about the
incident, with the senior doctors or clinicians to get support. It also provides information to
the staff on the legal counsel, and the benefits junior clinicians can get from observing and
participating in open disclosure (Harrison, Birks, Hall, Bosanquet, Harden & Iedema, 2014).
Open disclosure framework is designed to provide benefits to the patient,
carer/consumer, and clinicians involved in the incident. The process of open disclosure is
vital to the clinicians in context to the healthcare. Developing the right attitude, culture, and
a plan to eradicate the problem and reduce the occurrence of further incidents. Firstly, it is
necessary to inform the consumer or the patient about what exactly happened, i.e. about the
incident in a timely, open, and honest manner. All the adverse events and the consequences,
which might occur in the future described to the patient, and their family members. The
information given with respect to the open disclosure, to the patient during health services
also includes the steps taken to improve the health of the patient. They need to be given
information regarding the process of open disclosure with respect to their case. The process
of the OD will include a guide and the technological methods for the consumers/patients and
the information related to the positive results of the Open disclosure process (De Rassenfosse,
Palangkaraya & Webster, 2016).
Information given to clinical staff about Open Disclosure
Open disclosure framework in the healthcare settings, involves the role of, the patients
as well as the staff and other health professionals. Adequate access to the information should
be provided to staff, so that they can fulfil their roles and responsibilities. To support the staff
members, the health organisations must ensure following things, listed below (Elwy,
Bokhour, Maguire, Wagner, Asch, Gifford & Jesse, 2014).
Staff authorities in the healthcare, must be informed about the incident investigation
and the outcomes, obtained from it. The most important information regarding the incident is
the skills provided to the staff to effectively manage, and communicate to the patient. Thus,
through delivering this kind of information to thee staff, they will be able to get social and
psychological support from the health service organisations. Other includes making a
provision of the support system, presently available for those clinicians distressed by the
incident. The support system available to the clinicians or the health professionals, include
the medical defence organisations, doctors, health advisory services, committees and other
health service counsellors. In addition, they are given opportunities to discuss about the
incident, with the senior doctors or clinicians to get support. It also provides information to
the staff on the legal counsel, and the benefits junior clinicians can get from observing and
participating in open disclosure (Harrison, Birks, Hall, Bosanquet, Harden & Iedema, 2014).
Open disclosure framework is designed to provide benefits to the patient,
carer/consumer, and clinicians involved in the incident. The process of open disclosure is
vital to the clinicians in context to the healthcare. Developing the right attitude, culture, and
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
ETHICS AND LAW FOR HEALTH SERVICE MANAGERS 4
behaviours amongst consumers or patients in the healthcare for open disclosure is the key
responsibility of the managers or executives. Another important thing is to get open
disclosure aligned with the organisation’s clinical incident management policies and
processes. Every healthcare organisation receives benefits from the managers or managing
team with respect to the process of open disclosure. Managerial assistance in the form of
better leaders, effective communication, measurement, and evaluation helps in the handling
of the open disclosure with the patients (Koller, Rummens, Le Pouesard, Espin, Friedman,
Coffey & Kenneally, 2016).
Managerial involvement and Managerial assistance in Open Disclosure
Managers play a key role in supporting the open disclosure process, treated as
challenges faced by them in establishing effective open discussion. They develop and foster
the discussion of the adverse events or incidents and the appropriate strategies to prevent their
further occurrence. Healthcare receives benefit from the management as they support and
encourage clinicians and colleagues to manage clinical risks, and help patient. The managers
as maintain the effectiveness of the open disclosure, they confirm to the standards of making
an apology to the patient, through their clinicians. It means they ensure about making apology
laws across jurisdictions. Apology should include the words as I am sorry or we are sorry for
what has happened as a clinical misadventure. Thus, these are some of the points, which
mentions about the managerial assistance or their involvement in providing support to the
open disclosure process (Lee, 2016).
Information given to consumers during misadventure
Misadventure or any clinical error in the healthcare affects the health condition, of the
patients largely. It not only affects their heath condition, rather it influences their perspectives
towards the management and treatment given in the healthcare. On the occurrence of any
misadventure, necessary information must be given to the consumer, which will provide them
an understanding of the case, and the steps to resolve problem (Yeowell, Rooney &
Goodwin, 2018).
A consumer or the patient should receive an expression of regret due to any clinical
incident is a key component of open disclosure. The resource of the expression of regret has
been designed for the clinicians and other participants of open disclosure, to express regret
behaviours amongst consumers or patients in the healthcare for open disclosure is the key
responsibility of the managers or executives. Another important thing is to get open
disclosure aligned with the organisation’s clinical incident management policies and
processes. Every healthcare organisation receives benefits from the managers or managing
team with respect to the process of open disclosure. Managerial assistance in the form of
better leaders, effective communication, measurement, and evaluation helps in the handling
of the open disclosure with the patients (Koller, Rummens, Le Pouesard, Espin, Friedman,
Coffey & Kenneally, 2016).
Managerial involvement and Managerial assistance in Open Disclosure
Managers play a key role in supporting the open disclosure process, treated as
challenges faced by them in establishing effective open discussion. They develop and foster
the discussion of the adverse events or incidents and the appropriate strategies to prevent their
further occurrence. Healthcare receives benefit from the management as they support and
encourage clinicians and colleagues to manage clinical risks, and help patient. The managers
as maintain the effectiveness of the open disclosure, they confirm to the standards of making
an apology to the patient, through their clinicians. It means they ensure about making apology
laws across jurisdictions. Apology should include the words as I am sorry or we are sorry for
what has happened as a clinical misadventure. Thus, these are some of the points, which
mentions about the managerial assistance or their involvement in providing support to the
open disclosure process (Lee, 2016).
Information given to consumers during misadventure
Misadventure or any clinical error in the healthcare affects the health condition, of the
patients largely. It not only affects their heath condition, rather it influences their perspectives
towards the management and treatment given in the healthcare. On the occurrence of any
misadventure, necessary information must be given to the consumer, which will provide them
an understanding of the case, and the steps to resolve problem (Yeowell, Rooney &
Goodwin, 2018).
A consumer or the patient should receive an expression of regret due to any clinical
incident is a key component of open disclosure. The resource of the expression of regret has
been designed for the clinicians and other participants of open disclosure, to express regret
ETHICS AND LAW FOR HEALTH SERVICE MANAGERS 5
with sincerity and empathy, without creating situation of uncertainty. This is the most
important information given to the consumers during or after the clinical misadventure, in the
form of apology, as it forms effective open disclosure. To ensure about the effectiveness of
the open disclosure, because apologising or expressing regret is must to be in other actions
and communication. The consumers of healthcare in the process of open disclosure need to
be informed about the investigation on what has happened, and the outcomes of the
investigation. The information given ensures improving their experience of the open
disclosure process, to the people in the incident, which resulted harming the patient, while
receiving the treatment (Watson, Angus, Gore & Farmer, 2015).
Medico-legal and ethical considerations of Open disclosure Process
Open disclosure process is a medically ethical and legal updated procedure in context
to the healthcare settings. The topic underlines the significance of the topic, describing the
process of open disclosure when there is harm to the patient, and the case when there is no
harm to the patient. No legal or statutory obligations exist for the OD patients after the
incident. In legal terms, there is a common law authority which supports OD either as a part
of the duty of care or as an implied term in the contract of medical or healthcare services. The
legal considerations in the process of open disclosure, whether patient has caused harm or
not, states about the issues of apology, privilege, deceptive conduct and the negligent attitude
of the healthcare providers and institutions liability are included in legal considerations.
Some of the experienced and famous Australian commentators have described about
the disparity between the ethical obligations in OD and the poor practice of them in
healthcare. With the increasing medical incidents and health problems to people in the
present scenario, medical ethics must aim to become sufficient to drive health professional’s
contribution or commitment to the OD process. OD should be implanted directly into the
bureaucratic structures of the healthcare systems appropriately based on the grounds of legal
and ethical frameworks, encouraging health systems to become transparent; thereby reducing
errors and incidents (Gray & Thorpe, 2015).
Rights and Responsibilities of clinical staff on implementation of OD
On the occurrence of any misadventure, and the initiation of open disclosure process,
there is major contribution of the clinical staff to resolve problems. The clinicians before the
with sincerity and empathy, without creating situation of uncertainty. This is the most
important information given to the consumers during or after the clinical misadventure, in the
form of apology, as it forms effective open disclosure. To ensure about the effectiveness of
the open disclosure, because apologising or expressing regret is must to be in other actions
and communication. The consumers of healthcare in the process of open disclosure need to
be informed about the investigation on what has happened, and the outcomes of the
investigation. The information given ensures improving their experience of the open
disclosure process, to the people in the incident, which resulted harming the patient, while
receiving the treatment (Watson, Angus, Gore & Farmer, 2015).
Medico-legal and ethical considerations of Open disclosure Process
Open disclosure process is a medically ethical and legal updated procedure in context
to the healthcare settings. The topic underlines the significance of the topic, describing the
process of open disclosure when there is harm to the patient, and the case when there is no
harm to the patient. No legal or statutory obligations exist for the OD patients after the
incident. In legal terms, there is a common law authority which supports OD either as a part
of the duty of care or as an implied term in the contract of medical or healthcare services. The
legal considerations in the process of open disclosure, whether patient has caused harm or
not, states about the issues of apology, privilege, deceptive conduct and the negligent attitude
of the healthcare providers and institutions liability are included in legal considerations.
Some of the experienced and famous Australian commentators have described about
the disparity between the ethical obligations in OD and the poor practice of them in
healthcare. With the increasing medical incidents and health problems to people in the
present scenario, medical ethics must aim to become sufficient to drive health professional’s
contribution or commitment to the OD process. OD should be implanted directly into the
bureaucratic structures of the healthcare systems appropriately based on the grounds of legal
and ethical frameworks, encouraging health systems to become transparent; thereby reducing
errors and incidents (Gray & Thorpe, 2015).
Rights and Responsibilities of clinical staff on implementation of OD
On the occurrence of any misadventure, and the initiation of open disclosure process,
there is major contribution of the clinical staff to resolve problems. The clinicians before the
ETHICS AND LAW FOR HEALTH SERVICE MANAGERS 6
conduct of the OD process in the healthcare must have completed their education, for open
disclosure to avoid any problem. Further, when the misadventure occurs, and procedure of
disclosure is initiated, they are obliged to ensure that the patient is safeguarded from further
such harm. The responsibilities of the clinicians also involve apologising to the patient or
their respective support system, following a patient-safety incident without mentioning the
attribution of blame of the incident. In the cases of clinical misadventures, health service
organisations must ensure that the protocols, policies and the practices for open disclosure
emphasize on restoration, recovery, and improving quality and patient safety (Wong, Tan,
Heng, Ramesh, Ting, Lee & Kee, 2016).
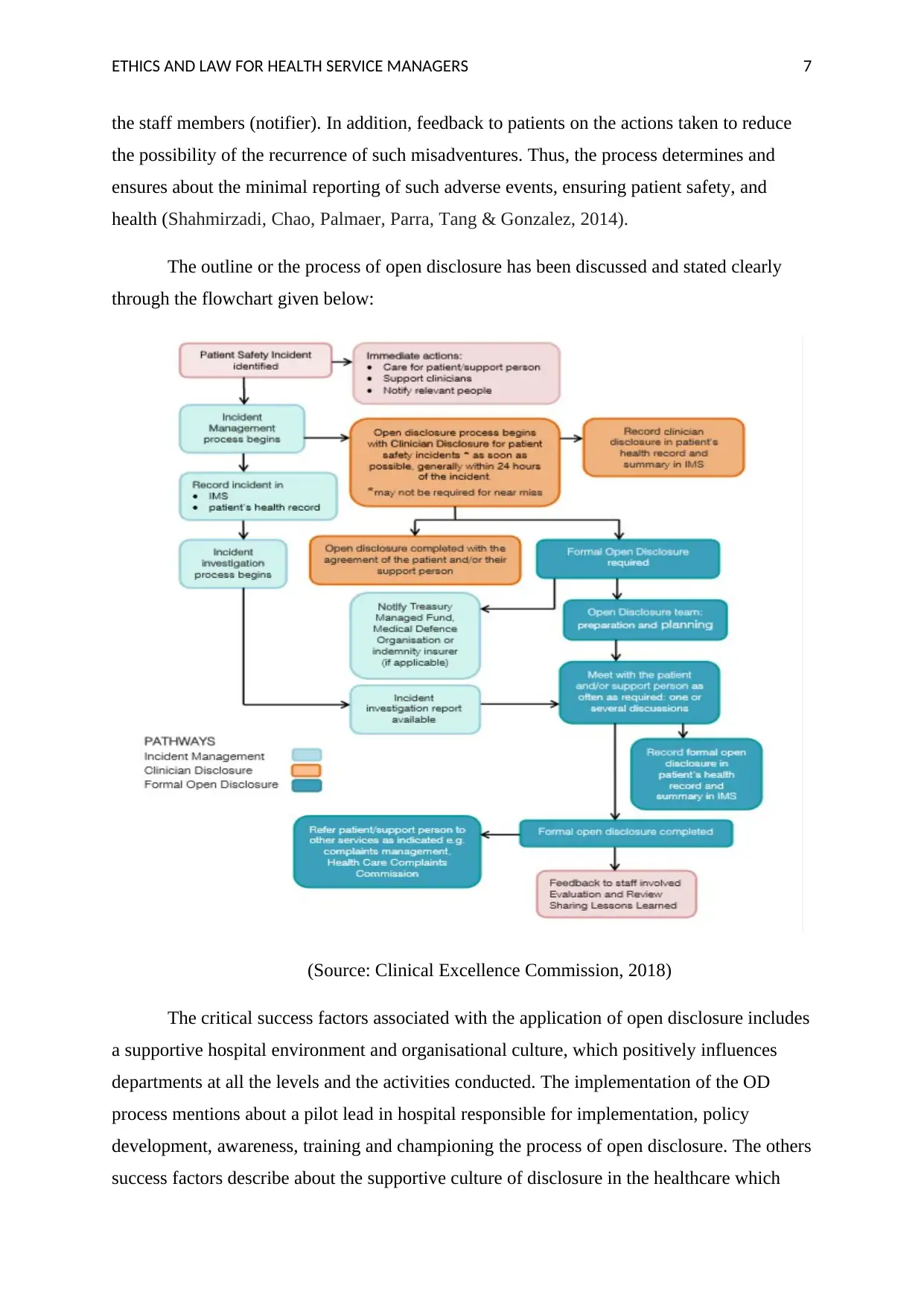
Outline of the OD process in healthcare and associated Critical success factors
The Open disclosure framework” discusses the principles of the open disclosure
process and provides a consistent basis for communication in healthcare following an adverse
healthcare incident. The outline or the framework for the open disclosure process can be
described through the following points (Schünemann, Al-Ansary, Forland, Kersten,
Komulainen, Kopp & Qaseem, 2015).
The first step in the process of open disclosure after identifying any clinical
misadventure includes identification of the incident, then moving on to the next step of
acknowledging to the patient about what has happened. It is a kind of conversation with the
patient about the misadventure and the related facts. The third step in the open disclosure
process relates to the reporting of the incident in the safety learning system and the document
in the medical records. After the incident has been reported and recorded in the documents of
the medical records, it is the responsibility of the manager to review the incident. The
manager reviews the incident and the severity of the event, telling the patient about the same.
The manager usually does reviewing the misadventure within 2 working days. Manager
performs the task of finalising the outcome from the review of the incident and then develops
an appropriate course of action for the improvement of the case. The incident or the
misadventure of the case is usually improved and the clinicians aim to fix the problem within
30 days (McLennan, Diebold, Rich & Elger, 2016).
Now, as the healthcare service managers or the clinicians in the healthcare settings,
with respect to the reported clinical misadventure, have taken the action an analysis of the
action to be done. The analysis in clinical terms or feedback, involves providing feedback to
conduct of the OD process in the healthcare must have completed their education, for open
disclosure to avoid any problem. Further, when the misadventure occurs, and procedure of
disclosure is initiated, they are obliged to ensure that the patient is safeguarded from further
such harm. The responsibilities of the clinicians also involve apologising to the patient or
their respective support system, following a patient-safety incident without mentioning the
attribution of blame of the incident. In the cases of clinical misadventures, health service
organisations must ensure that the protocols, policies and the practices for open disclosure
emphasize on restoration, recovery, and improving quality and patient safety (Wong, Tan,
Heng, Ramesh, Ting, Lee & Kee, 2016).
Outline of the OD process in healthcare and associated Critical success factors
The Open disclosure framework” discusses the principles of the open disclosure
process and provides a consistent basis for communication in healthcare following an adverse
healthcare incident. The outline or the framework for the open disclosure process can be
described through the following points (Schünemann, Al-Ansary, Forland, Kersten,
Komulainen, Kopp & Qaseem, 2015).
The first step in the process of open disclosure after identifying any clinical
misadventure includes identification of the incident, then moving on to the next step of
acknowledging to the patient about what has happened. It is a kind of conversation with the
patient about the misadventure and the related facts. The third step in the open disclosure
process relates to the reporting of the incident in the safety learning system and the document
in the medical records. After the incident has been reported and recorded in the documents of
the medical records, it is the responsibility of the manager to review the incident. The
manager reviews the incident and the severity of the event, telling the patient about the same.
The manager usually does reviewing the misadventure within 2 working days. Manager
performs the task of finalising the outcome from the review of the incident and then develops
an appropriate course of action for the improvement of the case. The incident or the
misadventure of the case is usually improved and the clinicians aim to fix the problem within
30 days (McLennan, Diebold, Rich & Elger, 2016).
Now, as the healthcare service managers or the clinicians in the healthcare settings,
with respect to the reported clinical misadventure, have taken the action an analysis of the
action to be done. The analysis in clinical terms or feedback, involves providing feedback to
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
ETHICS AND LAW FOR HEALTH SERVICE MANAGERS 7
the staff members (notifier). In addition, feedback to patients on the actions taken to reduce
the possibility of the recurrence of such misadventures. Thus, the process determines and
ensures about the minimal reporting of such adverse events, ensuring patient safety, and
health (Shahmirzadi, Chao, Palmaer, Parra, Tang & Gonzalez, 2014).
The outline or the process of open disclosure has been discussed and stated clearly
through the flowchart given below:
(Source: Clinical Excellence Commission, 2018)
The critical success factors associated with the application of open disclosure includes
a supportive hospital environment and organisational culture, which positively influences
departments at all the levels and the activities conducted. The implementation of the OD
process mentions about a pilot lead in hospital responsible for implementation, policy
development, awareness, training and championing the process of open disclosure. The others
success factors describe about the supportive culture of disclosure in the healthcare which
the staff members (notifier). In addition, feedback to patients on the actions taken to reduce
the possibility of the recurrence of such misadventures. Thus, the process determines and
ensures about the minimal reporting of such adverse events, ensuring patient safety, and
health (Shahmirzadi, Chao, Palmaer, Parra, Tang & Gonzalez, 2014).
The outline or the process of open disclosure has been discussed and stated clearly
through the flowchart given below:
(Source: Clinical Excellence Commission, 2018)
The critical success factors associated with the application of open disclosure includes
a supportive hospital environment and organisational culture, which positively influences
departments at all the levels and the activities conducted. The implementation of the OD
process mentions about a pilot lead in hospital responsible for implementation, policy
development, awareness, training and championing the process of open disclosure. The others
success factors describe about the supportive culture of disclosure in the healthcare which
ETHICS AND LAW FOR HEALTH SERVICE MANAGERS 8
tends to promote confidence and morale of the staff and their ability to implement the process
in the organisation (White, Wright, Baber & Barrera, 2017).
Recommendations
The effectiveness of the process of open disclosure can be achieved in a number of
ways, articulated in number of books. With context to the healthcare settings, a key
recommendation of global policy on medical error disclosure process is to apologise to the
patient for the misadventure. The health professionals should be encouraged to prepare open
disclosure after given training for the same. Health policies must focus on increasing the
involvement of carer, patient, or their family in the open disclosure. One of the most
important suggestions is to make sure that there should be no-harm incident to the patients. It
must be incorporate in every healthcare, as a crucial strategy in context to the incident
management (Kalra, 2016).
Conclusion
To conclude the above discussion on the essay of clinical misadventures and the
related aspects it has been analysed that open disclosure play a critical role determining
patient’s health. Open disclosure is an important step towards identifying occurrence of
clinical misadventures and reducing their recurrence in the future. The essay describe about
the significant information to be disclosed to the consumers/patients, and the staff members
of the healthcare, to enhance their skills to manage incidents. In addition, there is a detailed
analysis of the process and the duties and responsibilities of the staff and manager with
context to the reported clinical misadventure. The relationship between the patient and health
professionals or clinicians is impacted due to such adverse events. Therefore, every
healthcare organisation must focus on improving their services and reduce cases by
integrating mechanism of open disclosure in their system; thus ensuring patient wellbeing.
tends to promote confidence and morale of the staff and their ability to implement the process
in the organisation (White, Wright, Baber & Barrera, 2017).
Recommendations
The effectiveness of the process of open disclosure can be achieved in a number of
ways, articulated in number of books. With context to the healthcare settings, a key
recommendation of global policy on medical error disclosure process is to apologise to the
patient for the misadventure. The health professionals should be encouraged to prepare open
disclosure after given training for the same. Health policies must focus on increasing the
involvement of carer, patient, or their family in the open disclosure. One of the most
important suggestions is to make sure that there should be no-harm incident to the patients. It
must be incorporate in every healthcare, as a crucial strategy in context to the incident
management (Kalra, 2016).
Conclusion
To conclude the above discussion on the essay of clinical misadventures and the
related aspects it has been analysed that open disclosure play a critical role determining
patient’s health. Open disclosure is an important step towards identifying occurrence of
clinical misadventures and reducing their recurrence in the future. The essay describe about
the significant information to be disclosed to the consumers/patients, and the staff members
of the healthcare, to enhance their skills to manage incidents. In addition, there is a detailed
analysis of the process and the duties and responsibilities of the staff and manager with
context to the reported clinical misadventure. The relationship between the patient and health
professionals or clinicians is impacted due to such adverse events. Therefore, every
healthcare organisation must focus on improving their services and reduce cases by
integrating mechanism of open disclosure in their system; thus ensuring patient wellbeing.
ETHICS AND LAW FOR HEALTH SERVICE MANAGERS 9
References
Birks, Y., Harrison, R., Bosanquet, K., Hall, J., Harden, M., Entwistle, V. & Adamson, J.
(2014). An exploration of the implementation of open disclosure of adverse events in
the UK: a scoping review and qualitative exploration. Health Services and Delivery
Research, 2(20), 210-220.
Boudreau, K. J. & Lakhani, K. R. (2015). “Open” disclosure of innovations, incentives, and
follow-on reuse: Theory on processes of cumulative innovation and a field experiment
in computational biology. Research Policy, 44(1), 4-19.
Clinical Excellence Commission. (2013). General Principles and Requirements for Open
disclosure. Retrieved from:
http://www.cec.health.nsw.gov.au/__data/assets/pdf_file/0004/259015/
principles_for_open_disclosure.pdf
Clinical Excellence Commission. (2018). Flowchart of the Open Disclosure process.
Retrieved from:
http://www.cec.health.nsw.gov.au/__data/assets/pdf_file/0004/258988/flow-chart-
open-disclosure-process.pdf
De Rassenfosse, G., Palangkaraya, A. & Webster, E. (2016). Why do patents facilitate trade
in technology? Testing the disclosure and appropriation effects. Research
Policy, 45(7), 1326-1336.
Elwy, A. R., Bokhour, B. G., Maguire, E. M., Wagner, T. H., Asch, S. M., Gifford, A. L. &
Jesse, R. L. (2014). Improving healthcare systems’ disclosures of large-scale adverse
events: a Department of Veterans Affairs leadership, policymaker, research, and
stakeholder partnership. Journal of general internal medicine, 29(4), 895-903.
Gray, E. A., & Thorpe, J. H. (2015). Comparative effectiveness research and big data:
balancing potential with legal and ethical considerations. Journal of comparative
effectiveness research, 4(1), 61-74.
Hall, M. A., Orentlicher, D., Bobinski, M. A., Bagley, N., & Cohen, I. G. (2018). Health care
law and ethics. Netherlands: Wolters Kluwer Law & Business.
References
Birks, Y., Harrison, R., Bosanquet, K., Hall, J., Harden, M., Entwistle, V. & Adamson, J.
(2014). An exploration of the implementation of open disclosure of adverse events in
the UK: a scoping review and qualitative exploration. Health Services and Delivery
Research, 2(20), 210-220.
Boudreau, K. J. & Lakhani, K. R. (2015). “Open” disclosure of innovations, incentives, and
follow-on reuse: Theory on processes of cumulative innovation and a field experiment
in computational biology. Research Policy, 44(1), 4-19.
Clinical Excellence Commission. (2013). General Principles and Requirements for Open
disclosure. Retrieved from:
http://www.cec.health.nsw.gov.au/__data/assets/pdf_file/0004/259015/
principles_for_open_disclosure.pdf
Clinical Excellence Commission. (2018). Flowchart of the Open Disclosure process.
Retrieved from:
http://www.cec.health.nsw.gov.au/__data/assets/pdf_file/0004/258988/flow-chart-
open-disclosure-process.pdf
De Rassenfosse, G., Palangkaraya, A. & Webster, E. (2016). Why do patents facilitate trade
in technology? Testing the disclosure and appropriation effects. Research
Policy, 45(7), 1326-1336.
Elwy, A. R., Bokhour, B. G., Maguire, E. M., Wagner, T. H., Asch, S. M., Gifford, A. L. &
Jesse, R. L. (2014). Improving healthcare systems’ disclosures of large-scale adverse
events: a Department of Veterans Affairs leadership, policymaker, research, and
stakeholder partnership. Journal of general internal medicine, 29(4), 895-903.
Gray, E. A., & Thorpe, J. H. (2015). Comparative effectiveness research and big data:
balancing potential with legal and ethical considerations. Journal of comparative
effectiveness research, 4(1), 61-74.
Hall, M. A., Orentlicher, D., Bobinski, M. A., Bagley, N., & Cohen, I. G. (2018). Health care
law and ethics. Netherlands: Wolters Kluwer Law & Business.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
ETHICS AND LAW FOR HEALTH SERVICE MANAGERS 10
Harrison, R., Birks, Y., Hall, J., Bosanquet, K., Harden, M., & Iedema, R. (2014). The
contribution of nurses to incident disclosure: A narrative review. International journal
of nursing studies, 51(2), 334-345.
Harrison, R., Walton, M., Manias, E., Mears, S., & Plumb, J. (2017). Patients’ experiences in
Australian hospitals: a systematic review of evidence. Australian Health
Review, 41(4), 419-435.
Kalra, J. (2016). Medical error disclosure: A point of view. Pathol Lab Med Open J, 1(1), 1-
3.
Koller, D., Rummens, A., Le Pouesard, M., Espin, S., Friedman, J., Coffey, M. & Kenneally,
N. (2016). Patient disclosure of medical errors in paediatrics: A systematic literature
review.Paediatrics & Child Health, 21(4), 32-38
Lee, M. (2016). On patient safety: Do you say, "I'm sorry" to patients? Clinical Orthopaedics
and Related Research, 474(11), 2359-2361.
McLennan, S. R., Diebold, M., Rich, L. E. & Elger, B. S. (2016). Nurses’ perspectives
regarding the disclosure of errors to patients: a qualitative study. International journal
of nursing studies, 54, 16-22.
Schünemann, H. J., Al-Ansary, L. A., Forland, F., Kersten, S., Komulainen, J., Kopp, I. B. &
Qaseem, A. (2015). Guidelines International Network: principles for disclosure of
interests and management of conflicts in guidelines. Annals of internal
medicine, 163(7), 548-553.
Shahmirzadi, L., Chao, E. C., Palmaer, E., Parra, M. C., Tang, S., & Gonzalez, K. D. F.
(2014). Patient decisions for disclosure of secondary findings among the first 200
individuals undergoing clinical diagnostic exome sequencing. Genetics in
Medicine, 16(5), 395.
Watson, B. M., Angus, D., Gore, L., & Farmer, J. (2015). Communication in open disclosure
conversations about adverse events in hospitals. Language & Communication, 41, 57-
70.
Harrison, R., Birks, Y., Hall, J., Bosanquet, K., Harden, M., & Iedema, R. (2014). The
contribution of nurses to incident disclosure: A narrative review. International journal
of nursing studies, 51(2), 334-345.
Harrison, R., Walton, M., Manias, E., Mears, S., & Plumb, J. (2017). Patients’ experiences in
Australian hospitals: a systematic review of evidence. Australian Health
Review, 41(4), 419-435.
Kalra, J. (2016). Medical error disclosure: A point of view. Pathol Lab Med Open J, 1(1), 1-
3.
Koller, D., Rummens, A., Le Pouesard, M., Espin, S., Friedman, J., Coffey, M. & Kenneally,
N. (2016). Patient disclosure of medical errors in paediatrics: A systematic literature
review.Paediatrics & Child Health, 21(4), 32-38
Lee, M. (2016). On patient safety: Do you say, "I'm sorry" to patients? Clinical Orthopaedics
and Related Research, 474(11), 2359-2361.
McLennan, S. R., Diebold, M., Rich, L. E. & Elger, B. S. (2016). Nurses’ perspectives
regarding the disclosure of errors to patients: a qualitative study. International journal
of nursing studies, 54, 16-22.
Schünemann, H. J., Al-Ansary, L. A., Forland, F., Kersten, S., Komulainen, J., Kopp, I. B. &
Qaseem, A. (2015). Guidelines International Network: principles for disclosure of
interests and management of conflicts in guidelines. Annals of internal
medicine, 163(7), 548-553.
Shahmirzadi, L., Chao, E. C., Palmaer, E., Parra, M. C., Tang, S., & Gonzalez, K. D. F.
(2014). Patient decisions for disclosure of secondary findings among the first 200
individuals undergoing clinical diagnostic exome sequencing. Genetics in
Medicine, 16(5), 395.
Watson, B. M., Angus, D., Gore, L., & Farmer, J. (2015). Communication in open disclosure
conversations about adverse events in hospitals. Language & Communication, 41, 57-
70.

ETHICS AND LAW FOR HEALTH SERVICE MANAGERS 11
White, D., Wright, M., Baber, B. & Barrera, A. (2017). A pilot study evaluating the
effectiveness of a medicines education group in a mental health inpatient setting: A
UK perspective. Mental Health Clinician, 7(3), 116-123.
Wong, C. H., Tan, T. R., Heng, H. Y., Ramesh, T., Ting, P. W., Lee, W. S. & Kee, K.
(2016). Parental preferences with regards to disclosure following adverse events
occurring in relation to medication use or diagnosis in the care of their children–
perspectives from Malaysia. Med J Malaysia, 71(4), 187.
Yeowell, G., Rooney, J. & Goodwin, P. C. (2018). Exploring the disclosure decisions made
by physiotherapists with a specific learning difficulty. Physiotherapy, 104(2), 203-
208.
White, D., Wright, M., Baber, B. & Barrera, A. (2017). A pilot study evaluating the
effectiveness of a medicines education group in a mental health inpatient setting: A
UK perspective. Mental Health Clinician, 7(3), 116-123.
Wong, C. H., Tan, T. R., Heng, H. Y., Ramesh, T., Ting, P. W., Lee, W. S. & Kee, K.
(2016). Parental preferences with regards to disclosure following adverse events
occurring in relation to medication use or diagnosis in the care of their children–
perspectives from Malaysia. Med J Malaysia, 71(4), 187.
Yeowell, G., Rooney, J. & Goodwin, P. C. (2018). Exploring the disclosure decisions made
by physiotherapists with a specific learning difficulty. Physiotherapy, 104(2), 203-
208.
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





