Health Workforce Planning Comparison: Australia and Malaysia.
VerifiedAdded on 2023/06/11
|18
|4045
|156
Report
AI Summary
This report provides a comparative analysis of health workforce planning between Australia and Malaysia, highlighting the differences in their approaches and outcomes. It begins with an introduction to health workforce planning and its significance, followed by a rationale for selecting Australia and Malaysia for comparison. The environmental scan examines the health workforce policies and strategies in both countries, including the impact of initiatives like the Ninth and Tenth Malaysian Plans and Australia's National Partnership Agreement. The report then presents health workforce profile data, comparing the numbers of medical practitioners, nursing professionals, dental practitioners, midwives, physiotherapists, pharmacists, and optometrists in both countries. Key issues such as workforce shortages, retention challenges, and the impact of government policies are identified. The report concludes with recommendations for improving health workforce planning and management in both regions. Desklib provides access to this report and many other solved assignments.

Running head: HEALTH WORKFORCE PLANNING
Comparison of health workforce between two countries
Name of the Student
Name of the University
Author Note
Comparison of health workforce between two countries
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1HEALTH WORKFORCE PLANNING
Executive summary
Health human resources refer to all people who are involved in actions, the primary objective
of which is to enhance the overall health of the community. Thus, health human resources are
recognized as one of the major building blocks of a health care system. Health workforce in
most countries include physicians, midwives, nursing professionals, allied health
professionals, community health workers, healthcare providers, and social health workers.
Thus, human health resource deals with several issues such as, development, planning,
retention, management, and research on healthcare. Health organisations have estimated a
shortage of physicians, nurses and midwives worldwide. This shortage is found to be most
severe in low and middle income countries. The condition is commonly referred to as health
workforce crisis and is the direct result of several decades of underinvestment and low
funding in education of healthcare workers, poor wages, lack of training and education, and
poor health management. These directly contribute to an increase in the number of unskilled
healthcare professionals in the nation. The report will illustrate the different health workforce
plans of Australia and Malaysia and will make a thorough comparison of the health
workforce numbers in the two regions. This will be followed by identification of the critical
issues that are prevalent in the aforementioned regions.
Executive summary
Health human resources refer to all people who are involved in actions, the primary objective
of which is to enhance the overall health of the community. Thus, health human resources are
recognized as one of the major building blocks of a health care system. Health workforce in
most countries include physicians, midwives, nursing professionals, allied health
professionals, community health workers, healthcare providers, and social health workers.
Thus, human health resource deals with several issues such as, development, planning,
retention, management, and research on healthcare. Health organisations have estimated a
shortage of physicians, nurses and midwives worldwide. This shortage is found to be most
severe in low and middle income countries. The condition is commonly referred to as health
workforce crisis and is the direct result of several decades of underinvestment and low
funding in education of healthcare workers, poor wages, lack of training and education, and
poor health management. These directly contribute to an increase in the number of unskilled
healthcare professionals in the nation. The report will illustrate the different health workforce
plans of Australia and Malaysia and will make a thorough comparison of the health
workforce numbers in the two regions. This will be followed by identification of the critical
issues that are prevalent in the aforementioned regions.
2HEALTH WORKFORCE PLANNING
Table of Contents
Introduction................................................................................................................................3
Rationale for selecting the country............................................................................................3
Environmental scan....................................................................................................................4
Environmental scan for the health workforce of Australia and Malaysia..................................4
Health workforce profile data....................................................................................................6
Identification of the critical issues...........................................................................................11
Recommendation......................................................................................................................13
Conclusion................................................................................................................................15
References................................................................................................................................16
Table of Contents
Introduction................................................................................................................................3
Rationale for selecting the country............................................................................................3
Environmental scan....................................................................................................................4
Environmental scan for the health workforce of Australia and Malaysia..................................4
Health workforce profile data....................................................................................................6
Identification of the critical issues...........................................................................................11
Recommendation......................................................................................................................13
Conclusion................................................................................................................................15
References................................................................................................................................16
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3HEALTH WORKFORCE PLANNING
Introduction
Health workforce or health human resources (HHR), are defined as the professionals
whose task is focused on protecting and improving the health of the entire community. The
term ‘workforce’ aptly reflects the increased number and expanded roles of people in
different health professions. These generally include presence of diverse clinical and non-
clinical professionals who are able to implement appropriate public and individual health
interventions (WHO, 2018). In other words, the health workforce has been recognised as an
essential component for proper performance and functioning of labour-intensive healthcare
systems. The healthcare workers are not only working professionals. They are considered
integral parts of the functioning of healthcare teams, where each member professional
contributes a plethora of clinical skills and perform several functions (Lopes, Almeida &
Almada-Lobo, 2015). However, some countries have been identified to suffer from a
shortage of health workers, owing to their reluctance in developing effective strategic plans
and HHR policies that are imperative for guiding and building the human infrastructure
required for appropriate functioning of the health systems (Aluttis, Bishaw & Frank, 2014).
The report will elaborate on the national health workforce planning of Malaysia (WHO
Western Pacific Region) and compare it with that of Australia.
Rationale for selecting the country
Health improvement programmes and human capital are identified of central
importance for the economic growth and sustainable development of any country. Drastic
changes have been found in the healthcare system of Malaysia from the traditional remedies,
with the aim of meeting the health preferences and needs of the population. Major
reorganization have been observed in the healthcare services of the country, since its
independence in 1957. One of the first reorganization of public primary healthcare services
Introduction
Health workforce or health human resources (HHR), are defined as the professionals
whose task is focused on protecting and improving the health of the entire community. The
term ‘workforce’ aptly reflects the increased number and expanded roles of people in
different health professions. These generally include presence of diverse clinical and non-
clinical professionals who are able to implement appropriate public and individual health
interventions (WHO, 2018). In other words, the health workforce has been recognised as an
essential component for proper performance and functioning of labour-intensive healthcare
systems. The healthcare workers are not only working professionals. They are considered
integral parts of the functioning of healthcare teams, where each member professional
contributes a plethora of clinical skills and perform several functions (Lopes, Almeida &
Almada-Lobo, 2015). However, some countries have been identified to suffer from a
shortage of health workers, owing to their reluctance in developing effective strategic plans
and HHR policies that are imperative for guiding and building the human infrastructure
required for appropriate functioning of the health systems (Aluttis, Bishaw & Frank, 2014).
The report will elaborate on the national health workforce planning of Malaysia (WHO
Western Pacific Region) and compare it with that of Australia.
Rationale for selecting the country
Health improvement programmes and human capital are identified of central
importance for the economic growth and sustainable development of any country. Drastic
changes have been found in the healthcare system of Malaysia from the traditional remedies,
with the aim of meeting the health preferences and needs of the population. Major
reorganization have been observed in the healthcare services of the country, since its
independence in 1957. One of the first reorganization of public primary healthcare services
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4HEALTH WORKFORCE PLANNING
began since Alma Ata Declaration (1978) (Shazali et al., 2013). The Ministry of Health
(MOH) is the primary provider of healthcare services to all citizens of Malaysia. It is
comprised of a young population, with a relatively good health status. Furthermore, it has
also been identified as one of the few countries that is working towards achieving the target
of the Millennium Development Goals (Merriam, 2015). An increase is also observed in the
proportion of the elderly population, with an elevation in the number of individuals suffering
from chronic diseases. The country has a widespread healthcare system, with a life
expectancy at birth of 74 years. Furthermore, the rates of infant mortality have also reduced
to 7 per 1000 live births in 2013, from 75 per 1000, in the year 1957.
Owing to the fact that the healthcare system in Malaysia is categorised into private
and public sectors, the Malaysian government took initiatives in the formulation of a plan
1Care for 1Malaysia, with the intent of making healthcare reforms based on the need and
ability of the population (Leng & Hong, 2014). Furthermore, the society also places due
importance on expanding and developing the healthcare system. One major issue that guided
the selection of this country is the poor retention of skilled healthcare professionals, which
has resulted in a shortage of health workers in the Malaysian public health sector. This
shortage can be attributed to limited promotion opportunities, low salaries and lack of scope
for continuing education. On the other hand, reports suggest that there are an estimated 1
million people in Australia, employed in delivery of health services. Thus, Malaysia was
selected from the WHO Western Pacific list of countries, for comparison with Australia.
Environmental scan
Environmental scan for the health workforce of Australia and Malaysia
The health workers are the corner stone of the health care systems that can provide health
care services to the population for improving the health outcomes. Poor retention of the
began since Alma Ata Declaration (1978) (Shazali et al., 2013). The Ministry of Health
(MOH) is the primary provider of healthcare services to all citizens of Malaysia. It is
comprised of a young population, with a relatively good health status. Furthermore, it has
also been identified as one of the few countries that is working towards achieving the target
of the Millennium Development Goals (Merriam, 2015). An increase is also observed in the
proportion of the elderly population, with an elevation in the number of individuals suffering
from chronic diseases. The country has a widespread healthcare system, with a life
expectancy at birth of 74 years. Furthermore, the rates of infant mortality have also reduced
to 7 per 1000 live births in 2013, from 75 per 1000, in the year 1957.
Owing to the fact that the healthcare system in Malaysia is categorised into private
and public sectors, the Malaysian government took initiatives in the formulation of a plan
1Care for 1Malaysia, with the intent of making healthcare reforms based on the need and
ability of the population (Leng & Hong, 2014). Furthermore, the society also places due
importance on expanding and developing the healthcare system. One major issue that guided
the selection of this country is the poor retention of skilled healthcare professionals, which
has resulted in a shortage of health workers in the Malaysian public health sector. This
shortage can be attributed to limited promotion opportunities, low salaries and lack of scope
for continuing education. On the other hand, reports suggest that there are an estimated 1
million people in Australia, employed in delivery of health services. Thus, Malaysia was
selected from the WHO Western Pacific list of countries, for comparison with Australia.
Environmental scan
Environmental scan for the health workforce of Australia and Malaysia
The health workers are the corner stone of the health care systems that can provide health
care services to the population for improving the health outcomes. Poor retention of the
5HEALTH WORKFORCE PLANNING
skilled worker is one of the significant issue affecting the health care system of Malaysia.
Current trends indicates that there is an overall shortage of the health workers in the
Malaysian public health sector. In order to mitigate this, the Malaysian HRH policies and
strategies has been laid out in the five years development plan. According to the Ninth
Malaysian plan, the economy will be centred on human capital. As per this plan Malaysia
would be considered as a regional health tourism centre. According to this policy the human
resource and development will be given the highest priority to lessen the shortage of the
medical staffs, for which the training of the health care workers would be increased. This
policy emphasizes of the professional development initiatives that would be increased to meet
the higher levels of care. The policy aims to provide attractive opportunities to the health care
staffs for preventing the brain drain and the retention of the medical health professionals in
the public health sectors. All the health regulation has to be reviewed including the same
practice of alternative medicine. The Tenth Malaysian plan, 2011 and 2015, focuses on
improved specialist training, expansion and the improvement of the post basic training for the
nurses and the allied health care professionals. It is to be noted that the tenth Malaysian
planning is based on addressing the personal by the provision through better remuneration,
promotional opportunities and steps for providing greater job satisfaction. In Malaysia the
recent development that has affected the workforce planning in Malaysia are the wage scales,
complaints of the overwork, inadequate remuneration, and delays in promotion. In
compliance with the national policy of the expansion of the higher education, the policies
covering the expansion of the higher education have been liberalized.
In 2008, COAG collaborated in the National Partnership agreement on hospital and the health
workforce reform. The health workforce Australia was established as a national agency for
the progressing the health workforce reform in Australia. The health workforce plan was to
present the future outcomes of the health workforce. This was previously known as the
skilled worker is one of the significant issue affecting the health care system of Malaysia.
Current trends indicates that there is an overall shortage of the health workers in the
Malaysian public health sector. In order to mitigate this, the Malaysian HRH policies and
strategies has been laid out in the five years development plan. According to the Ninth
Malaysian plan, the economy will be centred on human capital. As per this plan Malaysia
would be considered as a regional health tourism centre. According to this policy the human
resource and development will be given the highest priority to lessen the shortage of the
medical staffs, for which the training of the health care workers would be increased. This
policy emphasizes of the professional development initiatives that would be increased to meet
the higher levels of care. The policy aims to provide attractive opportunities to the health care
staffs for preventing the brain drain and the retention of the medical health professionals in
the public health sectors. All the health regulation has to be reviewed including the same
practice of alternative medicine. The Tenth Malaysian plan, 2011 and 2015, focuses on
improved specialist training, expansion and the improvement of the post basic training for the
nurses and the allied health care professionals. It is to be noted that the tenth Malaysian
planning is based on addressing the personal by the provision through better remuneration,
promotional opportunities and steps for providing greater job satisfaction. In Malaysia the
recent development that has affected the workforce planning in Malaysia are the wage scales,
complaints of the overwork, inadequate remuneration, and delays in promotion. In
compliance with the national policy of the expansion of the higher education, the policies
covering the expansion of the higher education have been liberalized.
In 2008, COAG collaborated in the National Partnership agreement on hospital and the health
workforce reform. The health workforce Australia was established as a national agency for
the progressing the health workforce reform in Australia. The health workforce plan was to
present the future outcomes of the health workforce. This was previously known as the
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6HEALTH WORKFORCE PLANNING
national training plan which was changed by and renamed as the health work force 2025,
doctors, nurses and the midwives. The key planning of this policy is an authority’s national
planning approach. The methodical robustness of the Australian health care cannot be
matched with the Malaysian health care system. The health workforce plan of Australia was
conducted in to two phases, developing the projections for the size and the variety of the
health work force required to meet the future use. This policy mainly supported the clinical
training needs of an increasing number of undergraduate health students. The intern training
and the prevocational training had been a major contribution towards the workforce planning
in Australia.
Health workforce profile data
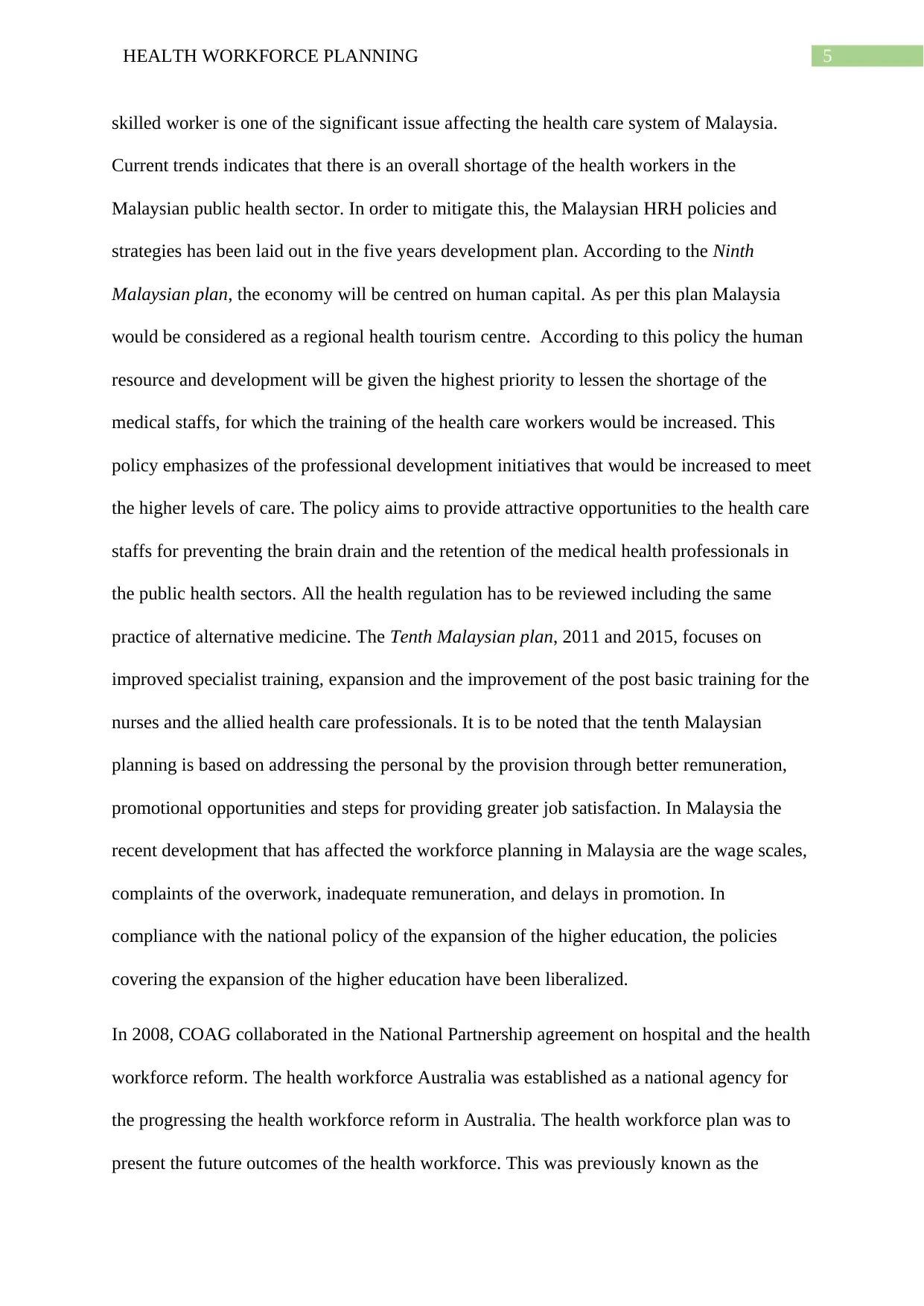
Medical workforce- The health workforce in Australia is diverse and large, and
covers a range of occupations that include highly qualified professionals, support staff, and
health volunteers. Nurses and midwives form the largest group of registered health workforce
with an estimated number of 353,000 registered and 301,000 nurses and midwives, who were
employed in the year 2014 (Aihw.gov.au, 2018). The health workforce in Australia comprises
of nurses, medical practitioners, midwives, oral health workers and Aboriginal and Torres
Strait Island health workers. The number of clinicians increased from 297 in 2008 to 331 in
2011. An increase was observed in the number of specialists and trainee doctor from 2008 to
2011. However, the rates of general practitioners were similar in both the years (112per
100,000 population) (Health Workforce Australia, 2018).
On the other hand, higher increases were observed in the numbers of the medical
practitioners that included all doctors, trainees and specialist doctors), in Malaysia from
25,102 in 2008 to 36,607 in 2011 (WHO, 2014).
national training plan which was changed by and renamed as the health work force 2025,
doctors, nurses and the midwives. The key planning of this policy is an authority’s national
planning approach. The methodical robustness of the Australian health care cannot be
matched with the Malaysian health care system. The health workforce plan of Australia was
conducted in to two phases, developing the projections for the size and the variety of the
health work force required to meet the future use. This policy mainly supported the clinical
training needs of an increasing number of undergraduate health students. The intern training
and the prevocational training had been a major contribution towards the workforce planning
in Australia.
Health workforce profile data
Medical workforce- The health workforce in Australia is diverse and large, and
covers a range of occupations that include highly qualified professionals, support staff, and
health volunteers. Nurses and midwives form the largest group of registered health workforce
with an estimated number of 353,000 registered and 301,000 nurses and midwives, who were
employed in the year 2014 (Aihw.gov.au, 2018). The health workforce in Australia comprises
of nurses, medical practitioners, midwives, oral health workers and Aboriginal and Torres
Strait Island health workers. The number of clinicians increased from 297 in 2008 to 331 in
2011. An increase was observed in the number of specialists and trainee doctor from 2008 to
2011. However, the rates of general practitioners were similar in both the years (112per
100,000 population) (Health Workforce Australia, 2018).
On the other hand, higher increases were observed in the numbers of the medical
practitioners that included all doctors, trainees and specialist doctors), in Malaysia from
25,102 in 2008 to 36,607 in 2011 (WHO, 2014).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7HEALTH WORKFORCE PLANNING
2 0 0 8 2 0 1 1
297
331
9.1
12.6
Comparison between the number of medical
practi ti oners in 2008 and 2011
Australia Malaysia
Figure 1
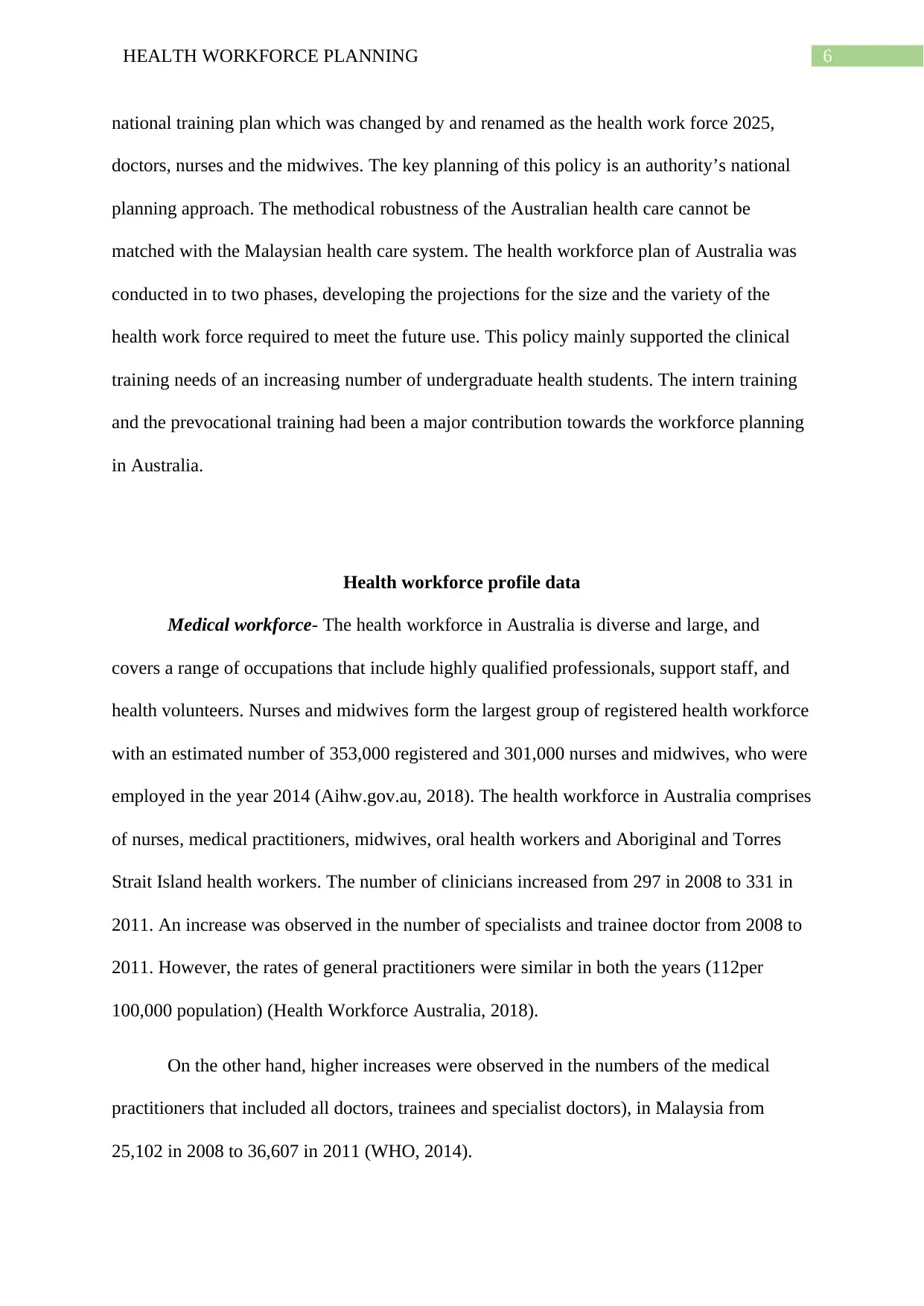
Nursing professionals- The total registered nursing workforce in Australia
significantly increased from 325,583 nurses in 2008 to 328,817 in 2011. Of the 328,817
nurses, 81.8% were registered nurse and 18.2% were enrolled nurse. Furthermore,
approximately 58.6% of the registered and enrolled nurses were found to work in the public
sector in Australia (Health Workforce Australia, 2018). In the context of Malaysia, the total
number of nurses underwent a huge increase from 54,208 nurses in 2008 to 74,788 in the year
2011 (WHO, 2014).
2 0 0 8 2 0 1 1
297
331
9.1
12.6
Comparison between the number of medical
practi ti oners in 2008 and 2011
Australia Malaysia
Figure 1
Nursing professionals- The total registered nursing workforce in Australia
significantly increased from 325,583 nurses in 2008 to 328,817 in 2011. Of the 328,817
nurses, 81.8% were registered nurse and 18.2% were enrolled nurse. Furthermore,
approximately 58.6% of the registered and enrolled nurses were found to work in the public
sector in Australia (Health Workforce Australia, 2018). In the context of Malaysia, the total
number of nurses underwent a huge increase from 54,208 nurses in 2008 to 74,788 in the year
2011 (WHO, 2014).
8HEALTH WORKFORCE PLANNING
2 0 0 8 2 0 1 1
325583
328817
54208
74788
Comparison between the number of
nurses in 2008 and 2011
Australia Malaysia
Figure 2
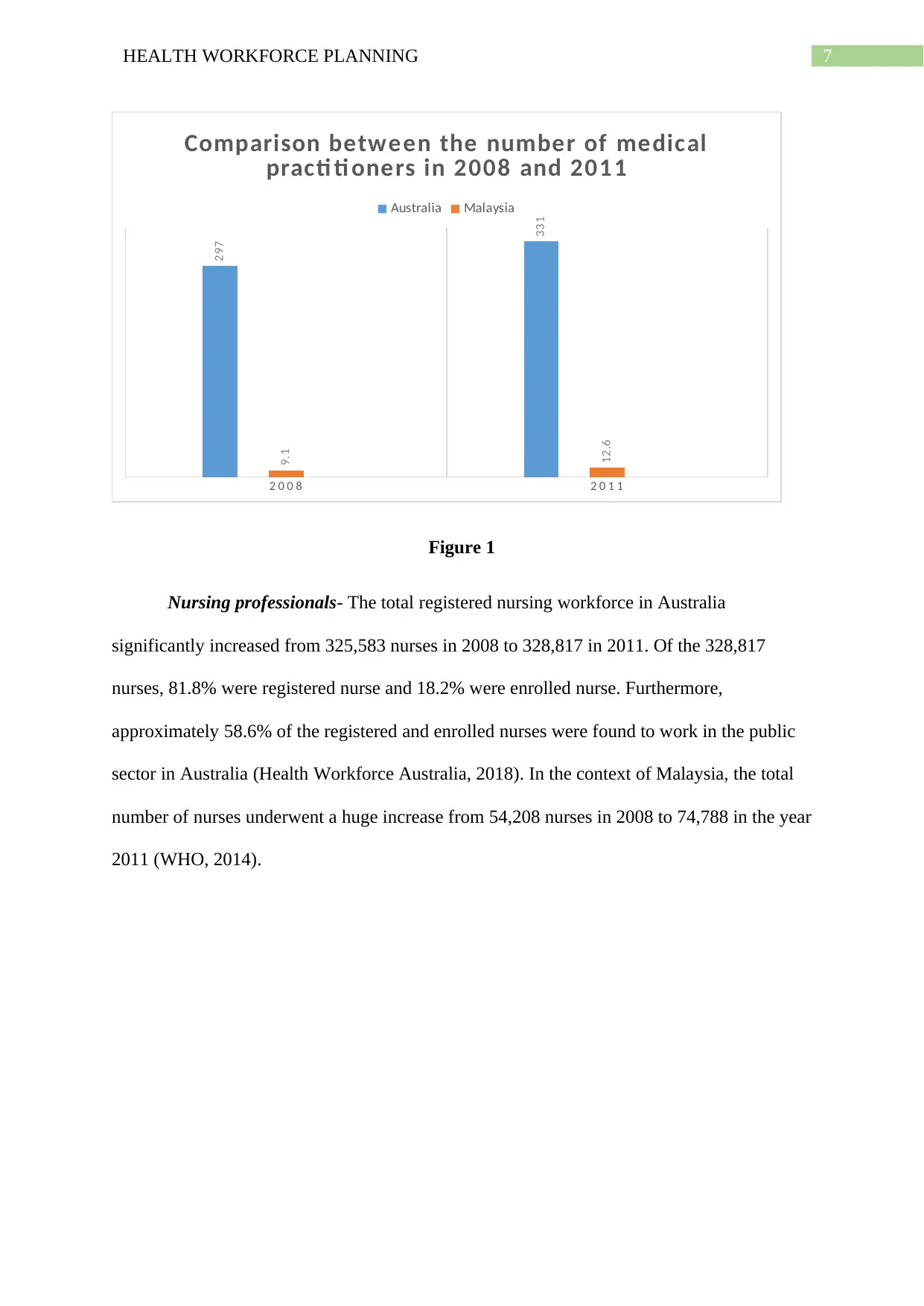
Dental workforce- Differences were also observed in the numbers of dental
practitioners, among the health human resource profile of the two countries. While there were
12,734 dentists in the dental workforce in Australia in 2011, the workforce was comprised of
only 4,253 dental practitioners in Malaysia, in 2011 (Health Workforce Australia, 2018)
(WHO, 2014).
2 0 1 1
12734
4253
Comparison between the number of
dental practi ti oners in 2011
Australia Malaysia
Figure 3
2 0 0 8 2 0 1 1
325583
328817
54208
74788
Comparison between the number of
nurses in 2008 and 2011
Australia Malaysia
Figure 2
Dental workforce- Differences were also observed in the numbers of dental
practitioners, among the health human resource profile of the two countries. While there were
12,734 dentists in the dental workforce in Australia in 2011, the workforce was comprised of
only 4,253 dental practitioners in Malaysia, in 2011 (Health Workforce Australia, 2018)
(WHO, 2014).
2 0 1 1
12734
4253
Comparison between the number of
dental practi ti oners in 2011
Australia Malaysia
Figure 3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9HEALTH WORKFORCE PLANNING
Midwives- The total number of midwives in the year 2011 was approximately 14,710
in Australia in the year 2011 (Health Workforce Australia, 2018). However, community
nurses and midwives comprised of 120.10 per 10,000 population in Malaysia in the same
year (WHO, 2014).
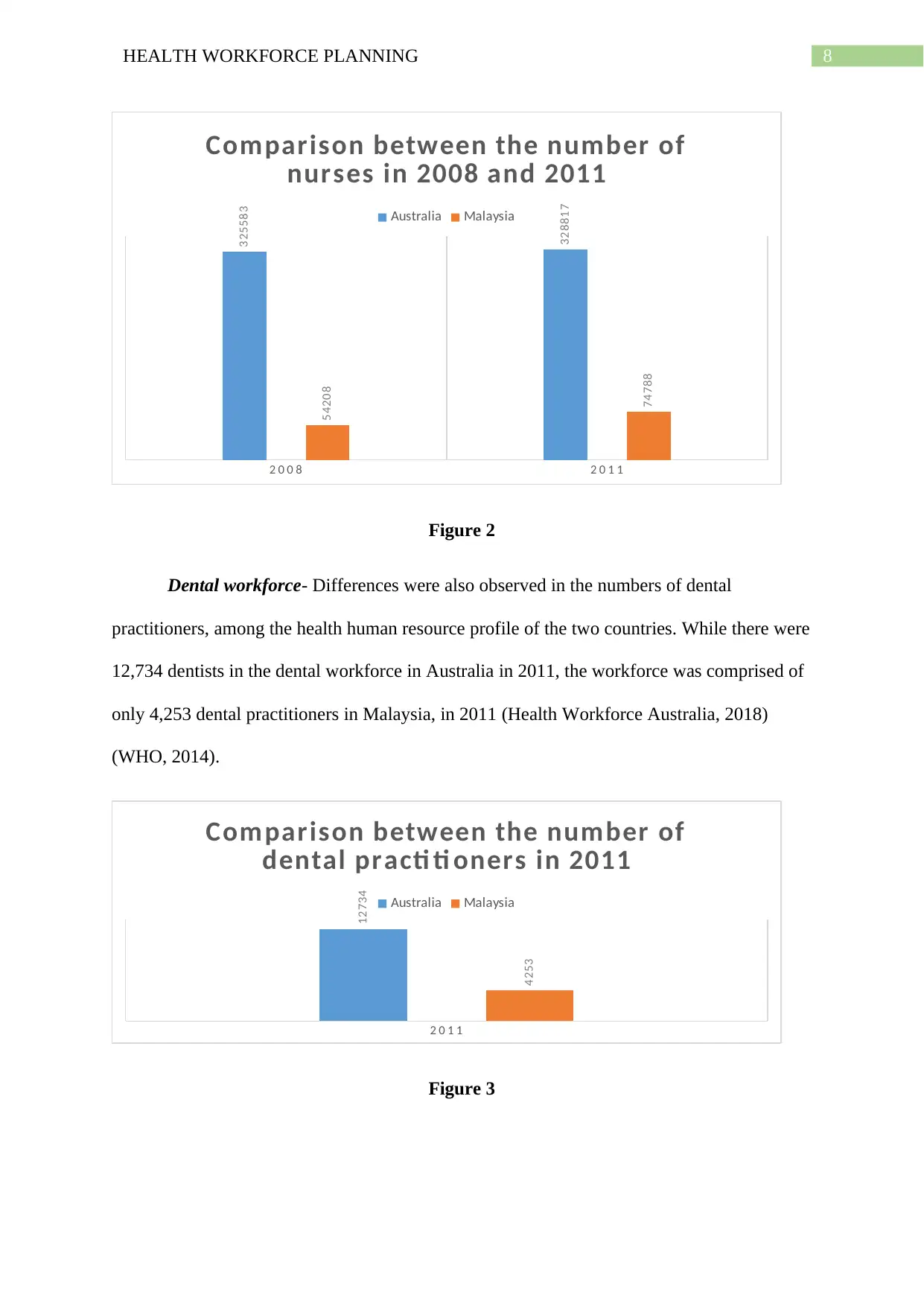
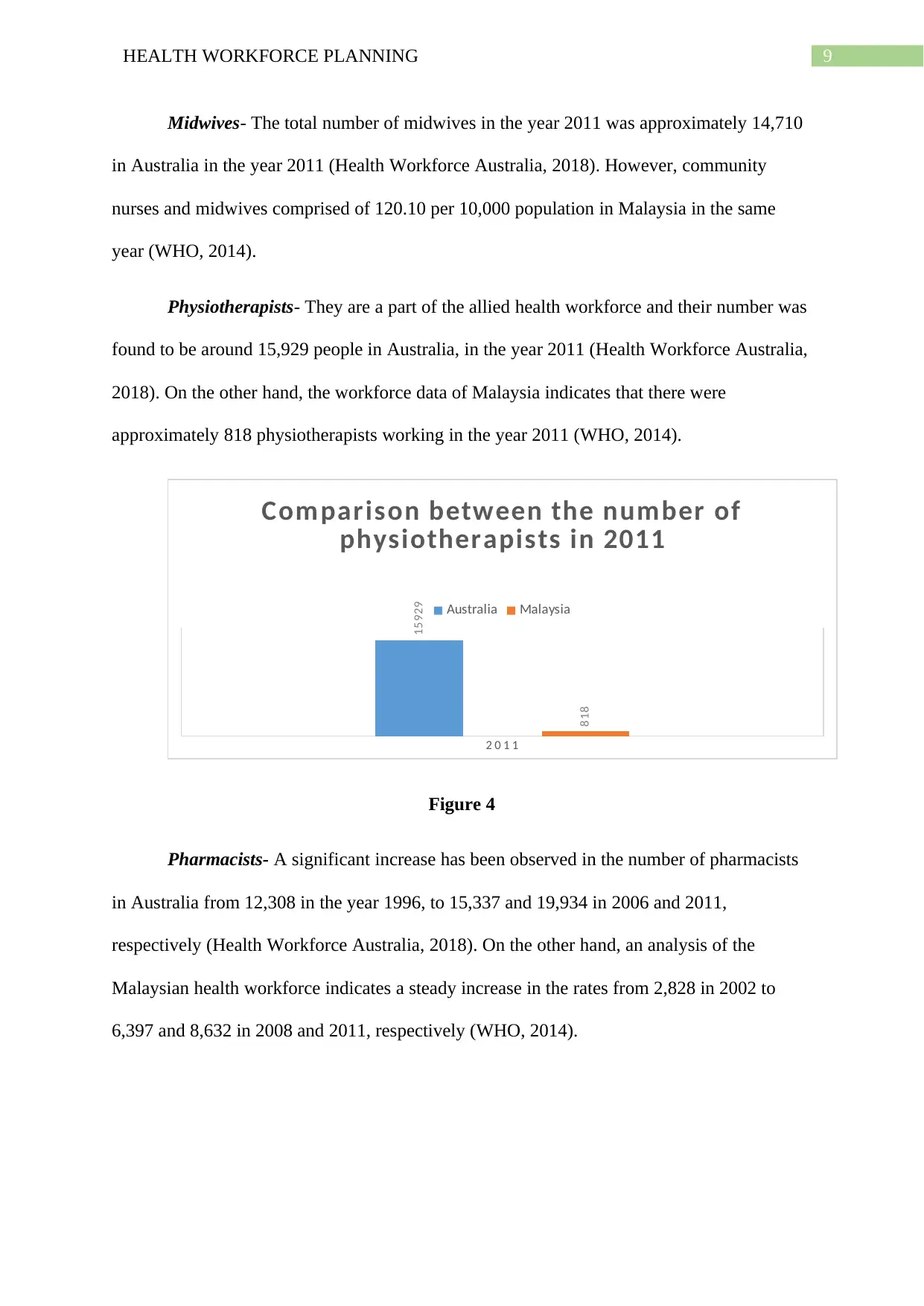
Physiotherapists- They are a part of the allied health workforce and their number was
found to be around 15,929 people in Australia, in the year 2011 (Health Workforce Australia,
2018). On the other hand, the workforce data of Malaysia indicates that there were
approximately 818 physiotherapists working in the year 2011 (WHO, 2014).
2 0 1 1
15929
818
Comparison between the number of
physiotherapists in 2011
Australia Malaysia
Figure 4
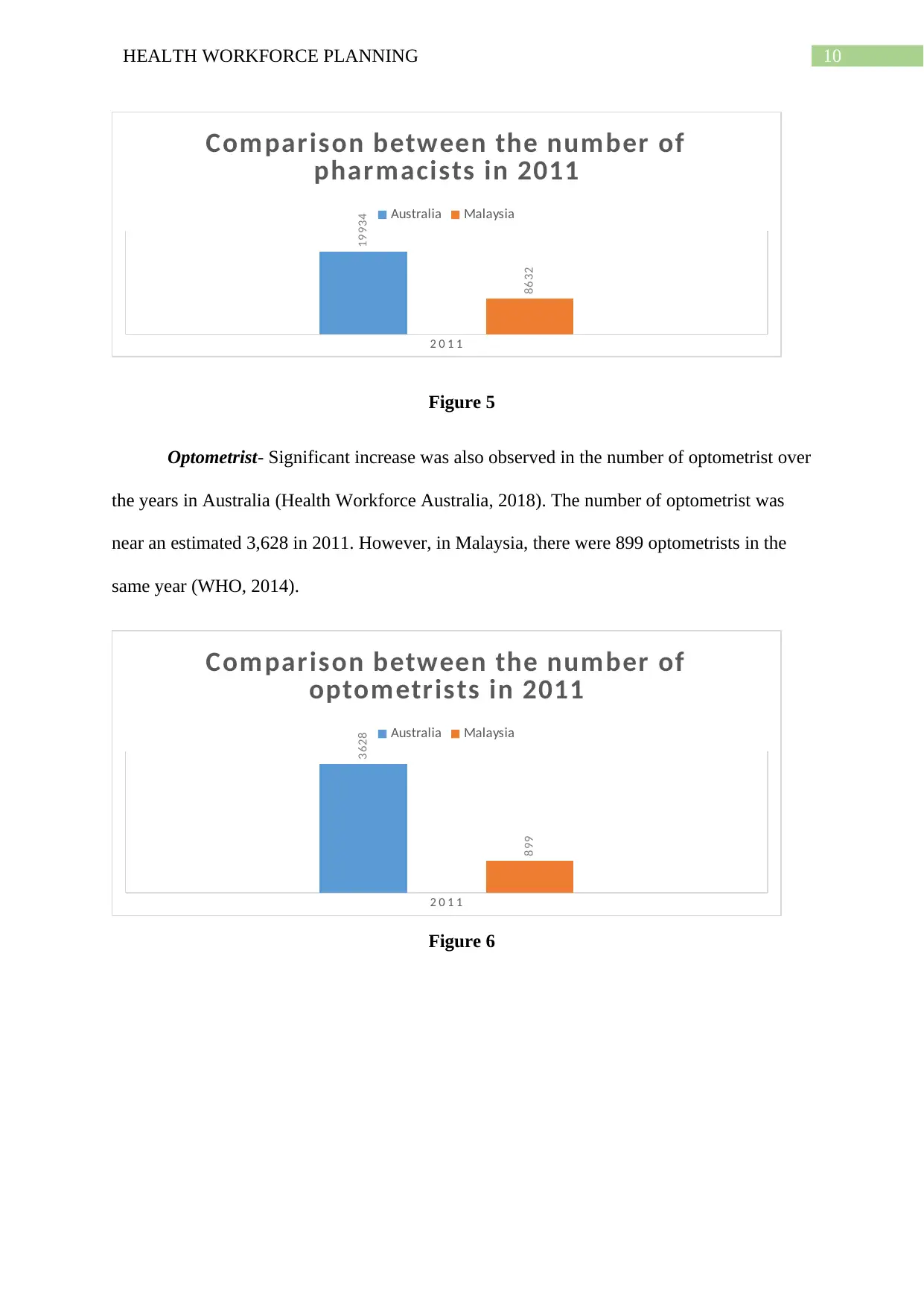
Pharmacists- A significant increase has been observed in the number of pharmacists
in Australia from 12,308 in the year 1996, to 15,337 and 19,934 in 2006 and 2011,
respectively (Health Workforce Australia, 2018). On the other hand, an analysis of the
Malaysian health workforce indicates a steady increase in the rates from 2,828 in 2002 to
6,397 and 8,632 in 2008 and 2011, respectively (WHO, 2014).
Midwives- The total number of midwives in the year 2011 was approximately 14,710
in Australia in the year 2011 (Health Workforce Australia, 2018). However, community
nurses and midwives comprised of 120.10 per 10,000 population in Malaysia in the same
year (WHO, 2014).
Physiotherapists- They are a part of the allied health workforce and their number was
found to be around 15,929 people in Australia, in the year 2011 (Health Workforce Australia,
2018). On the other hand, the workforce data of Malaysia indicates that there were
approximately 818 physiotherapists working in the year 2011 (WHO, 2014).
2 0 1 1
15929
818
Comparison between the number of
physiotherapists in 2011
Australia Malaysia
Figure 4
Pharmacists- A significant increase has been observed in the number of pharmacists
in Australia from 12,308 in the year 1996, to 15,337 and 19,934 in 2006 and 2011,
respectively (Health Workforce Australia, 2018). On the other hand, an analysis of the
Malaysian health workforce indicates a steady increase in the rates from 2,828 in 2002 to
6,397 and 8,632 in 2008 and 2011, respectively (WHO, 2014).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10HEALTH WORKFORCE PLANNING
2 0 1 1
19934
8632
Comparison between the number of
pharmacists in 2011
Australia Malaysia
Figure 5
Optometrist- Significant increase was also observed in the number of optometrist over
the years in Australia (Health Workforce Australia, 2018). The number of optometrist was
near an estimated 3,628 in 2011. However, in Malaysia, there were 899 optometrists in the
same year (WHO, 2014).
2 0 1 1
3628
899
Comparison between the number of
optometrists in 2011
Australia Malaysia
Figure 6
2 0 1 1
19934
8632
Comparison between the number of
pharmacists in 2011
Australia Malaysia
Figure 5
Optometrist- Significant increase was also observed in the number of optometrist over
the years in Australia (Health Workforce Australia, 2018). The number of optometrist was
near an estimated 3,628 in 2011. However, in Malaysia, there were 899 optometrists in the
same year (WHO, 2014).
2 0 1 1
3628
899
Comparison between the number of
optometrists in 2011
Australia Malaysia
Figure 6
11HEALTH WORKFORCE PLANNING
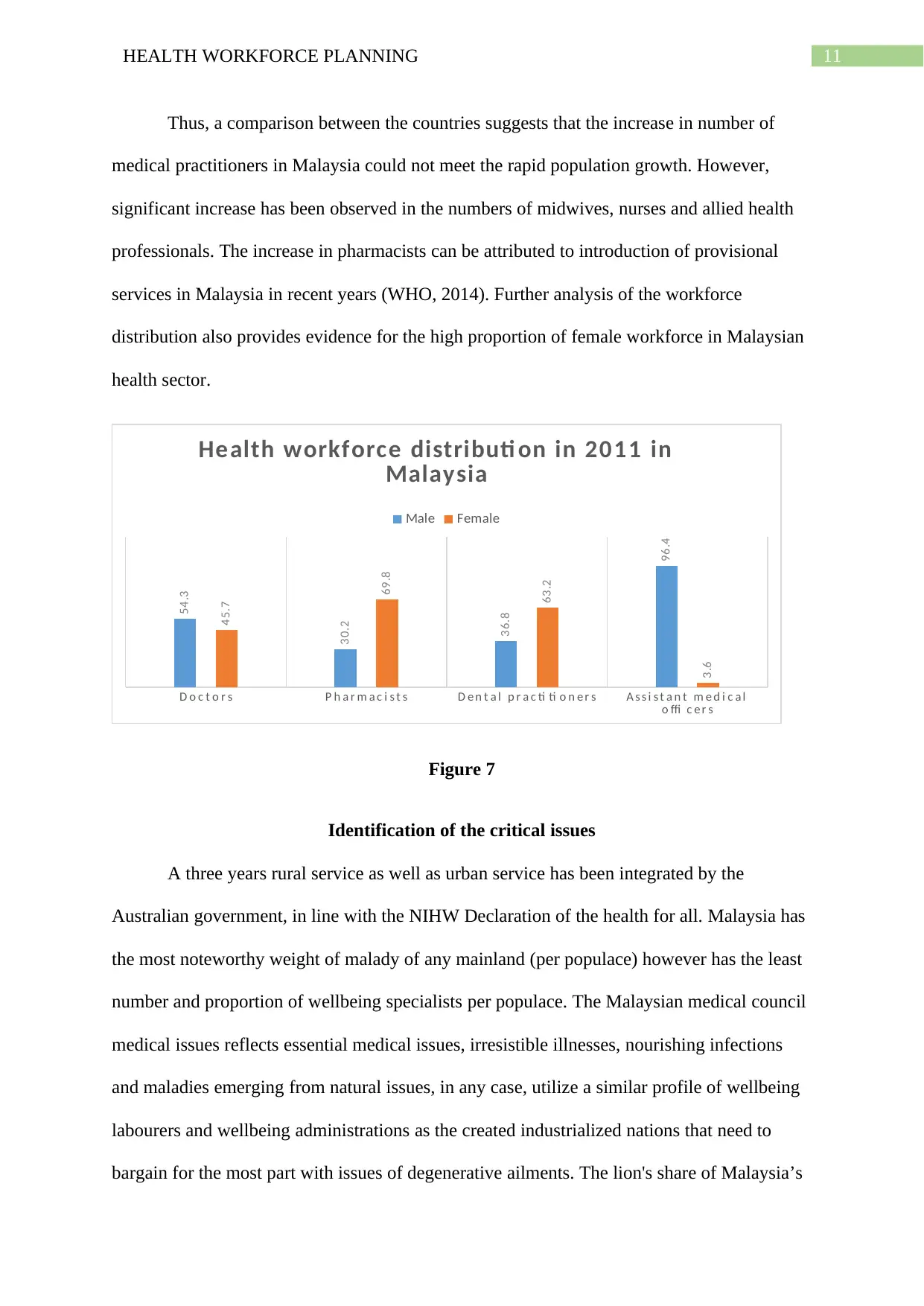
Thus, a comparison between the countries suggests that the increase in number of
medical practitioners in Malaysia could not meet the rapid population growth. However,
significant increase has been observed in the numbers of midwives, nurses and allied health
professionals. The increase in pharmacists can be attributed to introduction of provisional
services in Malaysia in recent years (WHO, 2014). Further analysis of the workforce
distribution also provides evidence for the high proportion of female workforce in Malaysian
health sector.
D o c t o r s P h a r m a c i s t s D e n t a l p r a c ti ti o n e r s A s s i s t a n t m e d i c a l
o ffi c e r s
54.3
30.2
36.8
96.4
45.7
69.8
63.2
3.6
Health workforce distributi on in 2011 in
Malaysia
Male Female
Figure 7
Identification of the critical issues
A three years rural service as well as urban service has been integrated by the
Australian government, in line with the NIHW Declaration of the health for all. Malaysia has
the most noteworthy weight of malady of any mainland (per populace) however has the least
number and proportion of wellbeing specialists per populace. The Malaysian medical council
medical issues reflects essential medical issues, irresistible illnesses, nourishing infections
and maladies emerging from natural issues, in any case, utilize a similar profile of wellbeing
labourers and wellbeing administrations as the created industrialized nations that need to
bargain for the most part with issues of degenerative ailments. The lion's share of Malaysia’s
Thus, a comparison between the countries suggests that the increase in number of
medical practitioners in Malaysia could not meet the rapid population growth. However,
significant increase has been observed in the numbers of midwives, nurses and allied health
professionals. The increase in pharmacists can be attributed to introduction of provisional
services in Malaysia in recent years (WHO, 2014). Further analysis of the workforce
distribution also provides evidence for the high proportion of female workforce in Malaysian
health sector.
D o c t o r s P h a r m a c i s t s D e n t a l p r a c ti ti o n e r s A s s i s t a n t m e d i c a l
o ffi c e r s
54.3
30.2
36.8
96.4
45.7
69.8
63.2
3.6
Health workforce distributi on in 2011 in
Malaysia
Male Female
Figure 7
Identification of the critical issues
A three years rural service as well as urban service has been integrated by the
Australian government, in line with the NIHW Declaration of the health for all. Malaysia has
the most noteworthy weight of malady of any mainland (per populace) however has the least
number and proportion of wellbeing specialists per populace. The Malaysian medical council
medical issues reflects essential medical issues, irresistible illnesses, nourishing infections
and maladies emerging from natural issues, in any case, utilize a similar profile of wellbeing
labourers and wellbeing administrations as the created industrialized nations that need to
bargain for the most part with issues of degenerative ailments. The lion's share of Malaysia’s
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 18
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





