PSY111 Foundations of Psychology Assignment: Exercises on Key Concepts
VerifiedAdded on 2022/11/18
|10
|2627
|412
Homework Assignment
AI Summary
This assignment solution for PSY111 Foundations of Psychology addresses three key areas: memory, psychological disorders and treatments, and indigenous and cross-cultural psychology. Exercise 1 explores prospective memory failures, analyzing reasons for forgetting and the use of external memory aids for clients, referencing relevant research on dementia and schizophrenia. Exercise 2 presents a case study of a 15-year-old with schizophrenia, applying DSM-5 criteria for diagnosis and recommending a combination therapy of cognitive behavioral therapy and pharmacotherapy. Exercise 3 focuses on cultural competence in healthcare, discussing the importance of cultural understanding, relationship building, and addressing barriers such as linguistic differences and stigma, with a focus on treating an Aboriginal male with substance use disorder and schizophrenia. The assignment emphasizes the need for culturally sensitive approaches, including awareness of personal worldviews, knowledge of diverse cultures, and effective communication strategies, to provide equitable and effective care.

Running head: HEALTHCARE
PSY111 Foundations of Psychology for the Health and Human services
Name of the Student
Name of the University
Author Note
PSY111 Foundations of Psychology for the Health and Human services
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1HEALTHCARE
Exercise 1: memory
Task 1
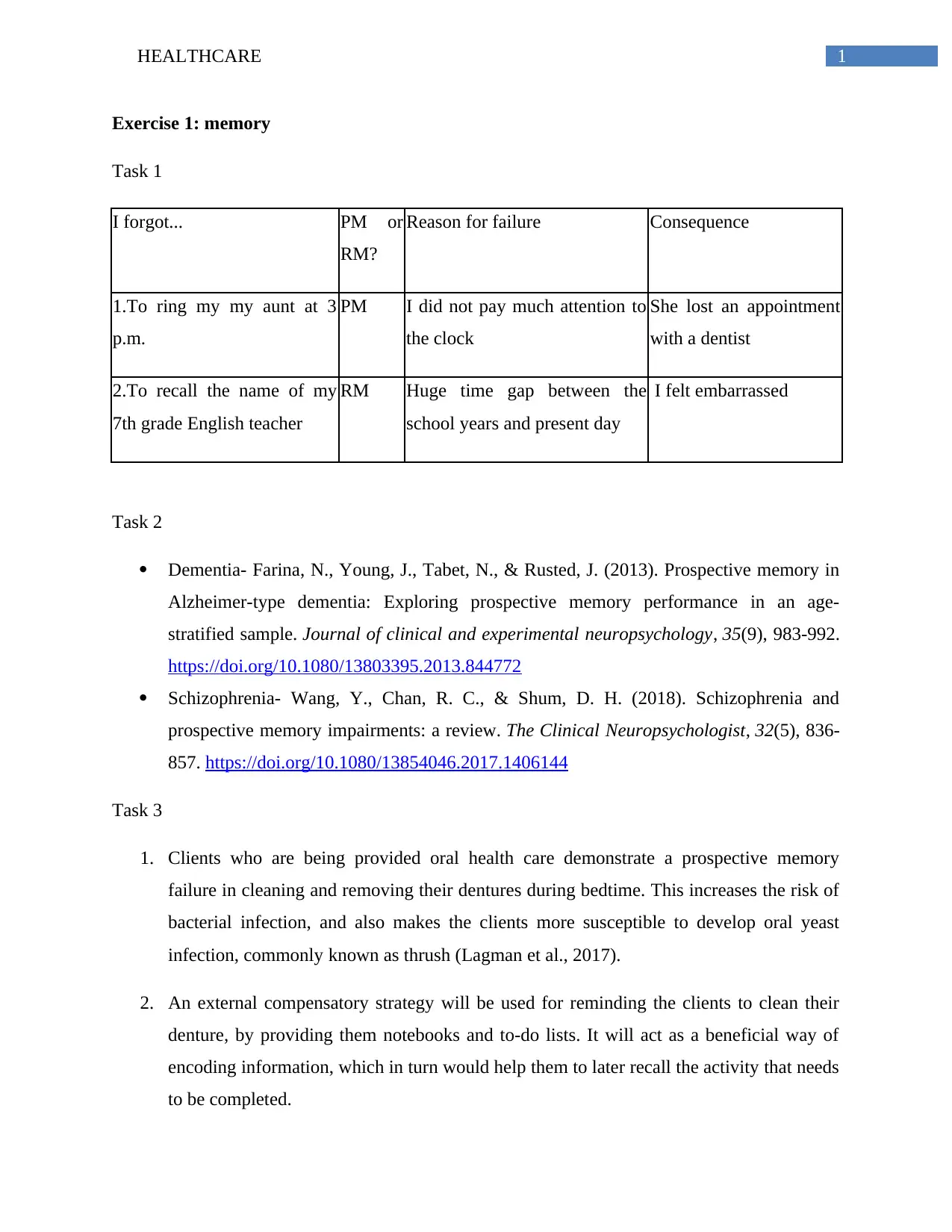
I forgot... PM or
RM?
Reason for failure Consequence
1.To ring my my aunt at 3
p.m.
PM I did not pay much attention to
the clock
She lost an appointment
with a dentist
2.To recall the name of my
7th grade English teacher
RM Huge time gap between the
school years and present day
I felt embarrassed
Task 2
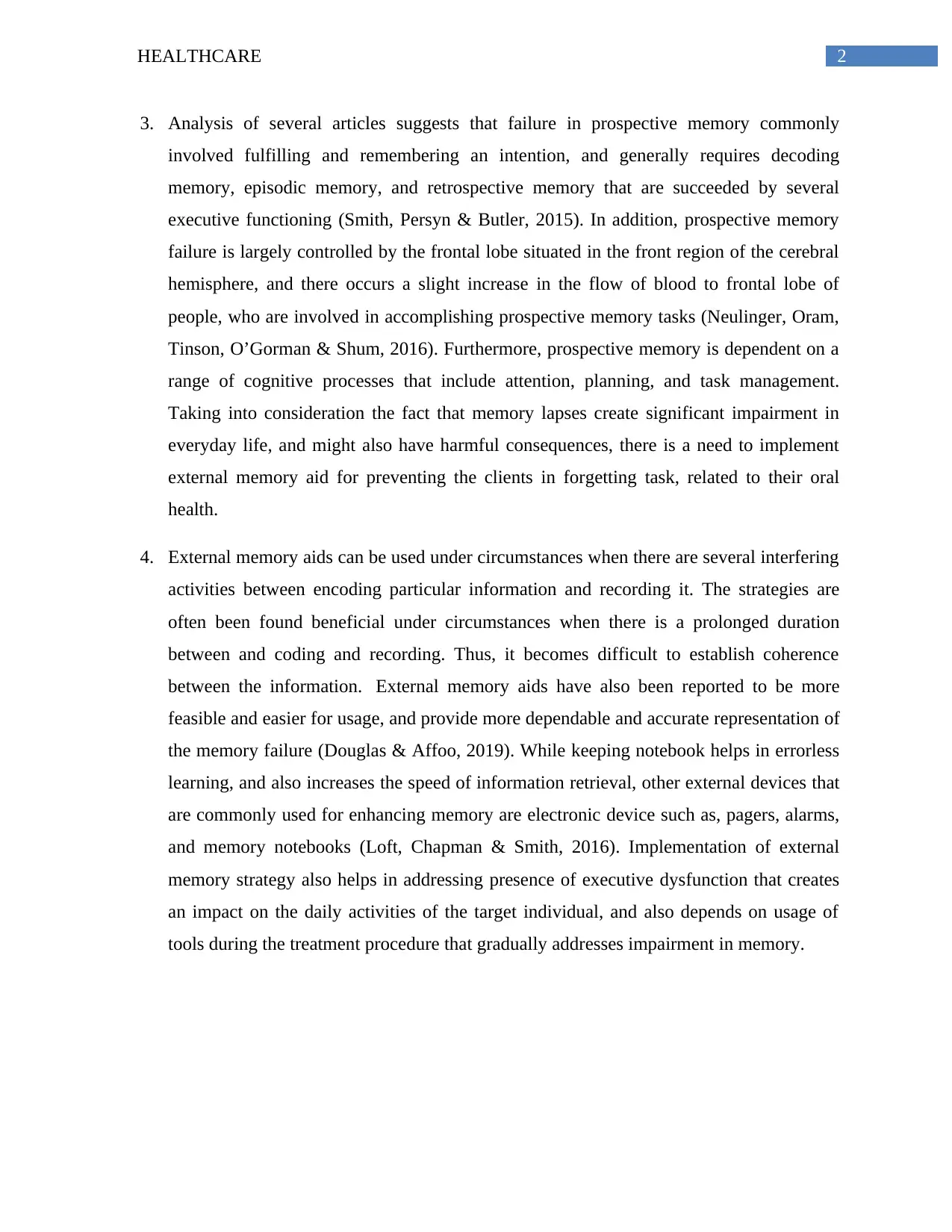
Dementia- Farina, N., Young, J., Tabet, N., & Rusted, J. (2013). Prospective memory in
Alzheimer-type dementia: Exploring prospective memory performance in an age-
stratified sample. Journal of clinical and experimental neuropsychology, 35(9), 983-992.
https://doi.org/10.1080/13803395.2013.844772
Schizophrenia- Wang, Y., Chan, R. C., & Shum, D. H. (2018). Schizophrenia and
prospective memory impairments: a review. The Clinical Neuropsychologist, 32(5), 836-
857. https://doi.org/10.1080/13854046.2017.1406144
Task 3
1. Clients who are being provided oral health care demonstrate a prospective memory
failure in cleaning and removing their dentures during bedtime. This increases the risk of
bacterial infection, and also makes the clients more susceptible to develop oral yeast
infection, commonly known as thrush (Lagman et al., 2017).
2. An external compensatory strategy will be used for reminding the clients to clean their
denture, by providing them notebooks and to-do lists. It will act as a beneficial way of
encoding information, which in turn would help them to later recall the activity that needs
to be completed.
Exercise 1: memory
Task 1
I forgot... PM or
RM?
Reason for failure Consequence
1.To ring my my aunt at 3
p.m.
PM I did not pay much attention to
the clock
She lost an appointment
with a dentist
2.To recall the name of my
7th grade English teacher
RM Huge time gap between the
school years and present day
I felt embarrassed
Task 2
Dementia- Farina, N., Young, J., Tabet, N., & Rusted, J. (2013). Prospective memory in
Alzheimer-type dementia: Exploring prospective memory performance in an age-
stratified sample. Journal of clinical and experimental neuropsychology, 35(9), 983-992.
https://doi.org/10.1080/13803395.2013.844772
Schizophrenia- Wang, Y., Chan, R. C., & Shum, D. H. (2018). Schizophrenia and
prospective memory impairments: a review. The Clinical Neuropsychologist, 32(5), 836-
857. https://doi.org/10.1080/13854046.2017.1406144
Task 3
1. Clients who are being provided oral health care demonstrate a prospective memory
failure in cleaning and removing their dentures during bedtime. This increases the risk of
bacterial infection, and also makes the clients more susceptible to develop oral yeast
infection, commonly known as thrush (Lagman et al., 2017).
2. An external compensatory strategy will be used for reminding the clients to clean their
denture, by providing them notebooks and to-do lists. It will act as a beneficial way of
encoding information, which in turn would help them to later recall the activity that needs
to be completed.
2HEALTHCARE
3. Analysis of several articles suggests that failure in prospective memory commonly
involved fulfilling and remembering an intention, and generally requires decoding
memory, episodic memory, and retrospective memory that are succeeded by several
executive functioning (Smith, Persyn & Butler, 2015). In addition, prospective memory
failure is largely controlled by the frontal lobe situated in the front region of the cerebral
hemisphere, and there occurs a slight increase in the flow of blood to frontal lobe of
people, who are involved in accomplishing prospective memory tasks (Neulinger, Oram,
Tinson, O’Gorman & Shum, 2016). Furthermore, prospective memory is dependent on a
range of cognitive processes that include attention, planning, and task management.
Taking into consideration the fact that memory lapses create significant impairment in
everyday life, and might also have harmful consequences, there is a need to implement
external memory aid for preventing the clients in forgetting task, related to their oral
health.
4. External memory aids can be used under circumstances when there are several interfering
activities between encoding particular information and recording it. The strategies are
often been found beneficial under circumstances when there is a prolonged duration
between and coding and recording. Thus, it becomes difficult to establish coherence
between the information. External memory aids have also been reported to be more
feasible and easier for usage, and provide more dependable and accurate representation of
the memory failure (Douglas & Affoo, 2019). While keeping notebook helps in errorless
learning, and also increases the speed of information retrieval, other external devices that
are commonly used for enhancing memory are electronic device such as, pagers, alarms,
and memory notebooks (Loft, Chapman & Smith, 2016). Implementation of external
memory strategy also helps in addressing presence of executive dysfunction that creates
an impact on the daily activities of the target individual, and also depends on usage of
tools during the treatment procedure that gradually addresses impairment in memory.
3. Analysis of several articles suggests that failure in prospective memory commonly
involved fulfilling and remembering an intention, and generally requires decoding
memory, episodic memory, and retrospective memory that are succeeded by several
executive functioning (Smith, Persyn & Butler, 2015). In addition, prospective memory
failure is largely controlled by the frontal lobe situated in the front region of the cerebral
hemisphere, and there occurs a slight increase in the flow of blood to frontal lobe of
people, who are involved in accomplishing prospective memory tasks (Neulinger, Oram,
Tinson, O’Gorman & Shum, 2016). Furthermore, prospective memory is dependent on a
range of cognitive processes that include attention, planning, and task management.
Taking into consideration the fact that memory lapses create significant impairment in
everyday life, and might also have harmful consequences, there is a need to implement
external memory aid for preventing the clients in forgetting task, related to their oral
health.
4. External memory aids can be used under circumstances when there are several interfering
activities between encoding particular information and recording it. The strategies are
often been found beneficial under circumstances when there is a prolonged duration
between and coding and recording. Thus, it becomes difficult to establish coherence
between the information. External memory aids have also been reported to be more
feasible and easier for usage, and provide more dependable and accurate representation of
the memory failure (Douglas & Affoo, 2019). While keeping notebook helps in errorless
learning, and also increases the speed of information retrieval, other external devices that
are commonly used for enhancing memory are electronic device such as, pagers, alarms,
and memory notebooks (Loft, Chapman & Smith, 2016). Implementation of external
memory strategy also helps in addressing presence of executive dysfunction that creates
an impact on the daily activities of the target individual, and also depends on usage of
tools during the treatment procedure that gradually addresses impairment in memory.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3HEALTHCARE
References
Douglas, N. F., & Affoo, R. H. (2019). Certified Nursing Assistants Want to Use External
Memory Aids for Residents With Dementia: Survey Results Within an Implementation
Science Framework. American Journal of Speech-Language Pathology, 1-8.
https://doi.org/10.1044/2018_AJSLP-18-0118
Lagman, R., Davis, M., LeGrand, S., Walsh, D., Parala, A., Gamier, P., ... & Rybicki, L. (2017).
Single-dose fluconazole therapy for oral thrush in hospice and palliative medicine
patients. American Journal of Hospice and Palliative Medicine®, 34(7), 645-649.
https://doi.org/10.1177%2F1049909116643927
Loft, S., Chapman, M., & Smith, R. E. (2016). Reducing prospective memory error and costs in
simulated air traffic control: External aids, extending practice, and removing perceived
memory requirements. Journal of experimental psychology: applied, 22(3), 272.
https://psycnet.apa.org/doi/10.1037/xap0000088
Neulinger, K., Oram, J., Tinson, H., O’Gorman, J., & Shum, D. H. (2016). Prospective memory
and frontal lobe function. Aging, Neuropsychology, and Cognition, 23(2), 171-183.
https://doi.org/10.1080/13825585.2015.1069252
Smith, R. E., Persyn, D., & Butler, P. (2015). Prospective memory, personality, and working
memory. Zeitschrift für Psychologie. https://doi.org/10.1027/2151-2604/a000055
References
Douglas, N. F., & Affoo, R. H. (2019). Certified Nursing Assistants Want to Use External
Memory Aids for Residents With Dementia: Survey Results Within an Implementation
Science Framework. American Journal of Speech-Language Pathology, 1-8.
https://doi.org/10.1044/2018_AJSLP-18-0118
Lagman, R., Davis, M., LeGrand, S., Walsh, D., Parala, A., Gamier, P., ... & Rybicki, L. (2017).
Single-dose fluconazole therapy for oral thrush in hospice and palliative medicine
patients. American Journal of Hospice and Palliative Medicine®, 34(7), 645-649.
https://doi.org/10.1177%2F1049909116643927
Loft, S., Chapman, M., & Smith, R. E. (2016). Reducing prospective memory error and costs in
simulated air traffic control: External aids, extending practice, and removing perceived
memory requirements. Journal of experimental psychology: applied, 22(3), 272.
https://psycnet.apa.org/doi/10.1037/xap0000088
Neulinger, K., Oram, J., Tinson, H., O’Gorman, J., & Shum, D. H. (2016). Prospective memory
and frontal lobe function. Aging, Neuropsychology, and Cognition, 23(2), 171-183.
https://doi.org/10.1080/13825585.2015.1069252
Smith, R. E., Persyn, D., & Butler, P. (2015). Prospective memory, personality, and working
memory. Zeitschrift für Psychologie. https://doi.org/10.1027/2151-2604/a000055
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4HEALTHCARE
Exercise 2: psychological disorders and treatments
Task 1
Case study #5- Marie
Task 2
On analysing the case study involving a 15 year old female Marie, it can be suggested
that she suffers from schizophrenia. This condition has been identified as a severe and chronic
mental disorder that creates an impact on the way by which an individual feels, behaves, and
things. The DSM 5 criteria was used for diagnosing the patient of the condition, based on
presence of two or more characteristics symptoms, for a significant time of one month, which
suggests presence of the disorder. The major symptoms as outlined in DSM 5, which were also
found in the patient, include hallucinations, delusions, and impairment in interpersonal relation
(Morrison, 2017). Marie reported auditory hallucinations that informed her about her family
members conspiring against her, and also held the delusional belief that her husband had been
killed by FBI agents who were keeping a constant surveillance on her. Thus, it can be suggested
that, she made met most of the diagnostic criteria that have been outlined in the manual. Time
and again it has been found that presence of such delusions and hallucinations make the affected
individual lose contact with reality, and they start believing on things which are not present in
actual.
Task 3
The combination therapy that might work together for treating the individual suffering
from schizophrenia includes cognitive behavioural therapy and pharmacotherapy. The mainstay
of pharmacotherapy for schizophrenia treatment depends on antipsychotic medications that have
of been found beneficial in reducing the severity of symptoms, and enhancing the social
functioning among the patient. In addition, antipsychotic pharmacotherapy helps in lowering
symptoms related to psychosis, and they generally take 7-14 days for exerting their principal
effect on the patient. Some common drugs that are generally administered in antipsychotic
pharmacotherapy include clozapine, olanzapine, risperidone, and amisulpride. These are typical
antipsychotic drugs bind to dopamine and serotonin receptors in the brain, and putatively
Exercise 2: psychological disorders and treatments
Task 1
Case study #5- Marie
Task 2
On analysing the case study involving a 15 year old female Marie, it can be suggested
that she suffers from schizophrenia. This condition has been identified as a severe and chronic
mental disorder that creates an impact on the way by which an individual feels, behaves, and
things. The DSM 5 criteria was used for diagnosing the patient of the condition, based on
presence of two or more characteristics symptoms, for a significant time of one month, which
suggests presence of the disorder. The major symptoms as outlined in DSM 5, which were also
found in the patient, include hallucinations, delusions, and impairment in interpersonal relation
(Morrison, 2017). Marie reported auditory hallucinations that informed her about her family
members conspiring against her, and also held the delusional belief that her husband had been
killed by FBI agents who were keeping a constant surveillance on her. Thus, it can be suggested
that, she made met most of the diagnostic criteria that have been outlined in the manual. Time
and again it has been found that presence of such delusions and hallucinations make the affected
individual lose contact with reality, and they start believing on things which are not present in
actual.
Task 3
The combination therapy that might work together for treating the individual suffering
from schizophrenia includes cognitive behavioural therapy and pharmacotherapy. The mainstay
of pharmacotherapy for schizophrenia treatment depends on antipsychotic medications that have
of been found beneficial in reducing the severity of symptoms, and enhancing the social
functioning among the patient. In addition, antipsychotic pharmacotherapy helps in lowering
symptoms related to psychosis, and they generally take 7-14 days for exerting their principal
effect on the patient. Some common drugs that are generally administered in antipsychotic
pharmacotherapy include clozapine, olanzapine, risperidone, and amisulpride. These are typical
antipsychotic drugs bind to dopamine and serotonin receptors in the brain, and putatively

5HEALTHCARE
enhance symptoms associated with negative cognition, anxiety, and depression that are found
among schizophrenia patients (Lally & MacCabe, 2015). This will prove more effective when
implemented along with cognitive behavioural therapy that generally targets particular symptoms
such as, reduced social functioning and poor self-esteem, thus lowering the psychotic symptoms.
This technique has also been found to bring about a decrease in cognitive distortions involving
negative believes, attitudes, behaviour, thoughts, and directly enhance emotional regulation,
thereby providing assistance to schizophrenia patients in coping with their prevailing complaints.
The primary reason for using cognitive behavioural therapy can be accredited to the fact that
while other approaches of psychoanalysis depend on exploring unconscious meaning behind the
perception and behaviour of a person, followed by formulation of a diagnosis, cognitive
behavioural therapy is action oriented and problem focused (Jauhar, Laws & McKenna, 2019).
The therapy will be primarily responsible for providing assistance to the patient in
exploring and practicing efficacious strategies that will help in addressing the identified
symptoms, and decreasing their severity. A combination of both the approaches will also help
about in reinforcing the belief that maladaptive behaviour and thought distortions play an
important role in maintenance and development of psychological disorder, and that associated
distress can be significantly lowered by implementing pharmacotherapy and information
processing skills.
enhance symptoms associated with negative cognition, anxiety, and depression that are found
among schizophrenia patients (Lally & MacCabe, 2015). This will prove more effective when
implemented along with cognitive behavioural therapy that generally targets particular symptoms
such as, reduced social functioning and poor self-esteem, thus lowering the psychotic symptoms.
This technique has also been found to bring about a decrease in cognitive distortions involving
negative believes, attitudes, behaviour, thoughts, and directly enhance emotional regulation,
thereby providing assistance to schizophrenia patients in coping with their prevailing complaints.
The primary reason for using cognitive behavioural therapy can be accredited to the fact that
while other approaches of psychoanalysis depend on exploring unconscious meaning behind the
perception and behaviour of a person, followed by formulation of a diagnosis, cognitive
behavioural therapy is action oriented and problem focused (Jauhar, Laws & McKenna, 2019).
The therapy will be primarily responsible for providing assistance to the patient in
exploring and practicing efficacious strategies that will help in addressing the identified
symptoms, and decreasing their severity. A combination of both the approaches will also help
about in reinforcing the belief that maladaptive behaviour and thought distortions play an
important role in maintenance and development of psychological disorder, and that associated
distress can be significantly lowered by implementing pharmacotherapy and information
processing skills.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6HEALTHCARE
References
Jauhar, S., Laws, K. R., & McKenna, P. J. (2019). CBT for schizophrenia: a critical
viewpoint. Psychological medicine, 1-4. https://doi.org/10.1017/S0033291718004166
Lally, J., & MacCabe, J. H. (2015). Antipsychotic medication in schizophrenia: a review. British
medical bulletin, 114(1), 169-179. https://doi.org/10.1093/bmb/ldv017
Morrison, J. (2017). DSM-5 made easy: The clinician's guide to diagnosis. Guilford
Publications.
References
Jauhar, S., Laws, K. R., & McKenna, P. J. (2019). CBT for schizophrenia: a critical
viewpoint. Psychological medicine, 1-4. https://doi.org/10.1017/S0033291718004166
Lally, J., & MacCabe, J. H. (2015). Antipsychotic medication in schizophrenia: a review. British
medical bulletin, 114(1), 169-179. https://doi.org/10.1093/bmb/ldv017
Morrison, J. (2017). DSM-5 made easy: The clinician's guide to diagnosis. Guilford
Publications.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7HEALTHCARE
Exercise 3: indigenous and cross-cultural psychology
1. Cultural competence refer to the actions and will of an individual to foster understanding
between each other, be respectful towards others, and adopt an open attitude towards a
range of cultural perspectives. Presence of cultural competence helps in strengthening
cultural security, and also ensures that all actions are directed towards equal opportunities
(Shen, 2015). The concept of relationship building is imperative for cultural competence,
and is dependent on the basics of understanding the expectations and attitudes of other,
while concomitantly building on knowledge and awareness, with the use of several
resources and community members. In other words, cultural competence helps
professionals to demonstrate respect towards people, belonging to diverse beliefs feelings
and values.
2. I am pursuing education in the domain of psychology, with the prime objective of
adorning the roles and responsibilities of a clinical psychologist, to treat people suffering
from mental illness, regardless of their background.
3.
a) A 23 year old Aboriginal male had been presented to the healthcare facility for
alcohol and opioid detoxification, following an episode of failed suicidal attempt.
b) The specific concern was associated with substance use disorder that occurs under
circumstances when usage of one or more drug brings about a significant impairment.
4. Cultural competence comprises of a set of aligning attitudes behaviour and policies that are
enforced together in a system, and commonly displayed by healthcare professionals, which
enables them to work in an efficient manner, across different cross-cultural situations. Adorning
the role of a culturally competent healthcare professional requires having necessary skills that
facilitate valuing diversity, conducting cultural self assessment, demonstrating consciousness of
the inherited dynamics during interaction of different culture, having adequate institutionalized
cultural awareness and knowledge, and being able to develop accordingly to delivery of services
that reflect and awareness on cultural diversity. However, while seeking these approaches,
culturally diverse clients encounter several challenges and barriers. Linguistic competence is one
of the most significant behaviour that comprises of a failure in effectively communicating with
Exercise 3: indigenous and cross-cultural psychology
1. Cultural competence refer to the actions and will of an individual to foster understanding
between each other, be respectful towards others, and adopt an open attitude towards a
range of cultural perspectives. Presence of cultural competence helps in strengthening
cultural security, and also ensures that all actions are directed towards equal opportunities
(Shen, 2015). The concept of relationship building is imperative for cultural competence,
and is dependent on the basics of understanding the expectations and attitudes of other,
while concomitantly building on knowledge and awareness, with the use of several
resources and community members. In other words, cultural competence helps
professionals to demonstrate respect towards people, belonging to diverse beliefs feelings
and values.
2. I am pursuing education in the domain of psychology, with the prime objective of
adorning the roles and responsibilities of a clinical psychologist, to treat people suffering
from mental illness, regardless of their background.
3.
a) A 23 year old Aboriginal male had been presented to the healthcare facility for
alcohol and opioid detoxification, following an episode of failed suicidal attempt.
b) The specific concern was associated with substance use disorder that occurs under
circumstances when usage of one or more drug brings about a significant impairment.
4. Cultural competence comprises of a set of aligning attitudes behaviour and policies that are
enforced together in a system, and commonly displayed by healthcare professionals, which
enables them to work in an efficient manner, across different cross-cultural situations. Adorning
the role of a culturally competent healthcare professional requires having necessary skills that
facilitate valuing diversity, conducting cultural self assessment, demonstrating consciousness of
the inherited dynamics during interaction of different culture, having adequate institutionalized
cultural awareness and knowledge, and being able to develop accordingly to delivery of services
that reflect and awareness on cultural diversity. However, while seeking these approaches,
culturally diverse clients encounter several challenges and barriers. Linguistic competence is one
of the most significant behaviour that comprises of a failure in effectively communicating with

8HEALTHCARE
patients belonging to diverse population. Time and again, patients demonstrate low literacy
skills, suffer from disabilities, or any kind of speech and hearing impairment, while seeking care
services. However, it becomes difficult to attain effective communication with them that directly
access an impediment in the process of care giving (Almutairi, 2015). Another significant barrier
is encountered in relation to lack of necessary resources to provide care in a culturally competent
manner. Furthermore, presence of stigmatizing and discriminating attitude towards people
belonging to diverse population, particularly indigenous ethnicities also prevents the clients from
seeking appropriate care services (Betancourt, Green, Carrillo & Owusu Ananeh-Firempong,
2016). This is most commonly addressed by hiring bilingual professionals or interpreters who
help in explaining the actual meaning of the conversations, and increase the quality of care,
health outcomes, and subsequent patient satisfaction.
5. The basic principles of cultural competence that will be taken into consideration while treating
such a patient who suffers from schizophrenia, includes being aware of the personal and
worldview, developing positive attitudes and perceptions towards cultural diversity, gaining an
insight and knowledge on different worldviews and cultural practices of the ethnicities to which
the patients belong, and enhancing skills required for effective interaction and communication
with culturally diverse clients. It has often been found that having regular access to healthcare
facilities and physicians differ by ethnicity and race. Therefore, while demonstrating cultural
competence, efforts will be taken to increase awareness of the patient on the healthcare
communities and services that are available, and easily accessible to the target population (Butler
et al., 2016). The patient will also be asked about the beliefs and assumptions regarding the
prevailing health condition, and this information will facilitate engaging during interactions, at
the time of shared clinical decision making. Assistance from cultural brokers such as, cultural
group leaders and social service workers will also assist in understanding more about the
similarities and differences between cultures (Mobula et al., 2015). The patients will also be
inquired about their learning experiences, while using multimedia tools and other resources for
helping them understand the potential advantages and risks (if any) of the intended treatment
modalities.
patients belonging to diverse population. Time and again, patients demonstrate low literacy
skills, suffer from disabilities, or any kind of speech and hearing impairment, while seeking care
services. However, it becomes difficult to attain effective communication with them that directly
access an impediment in the process of care giving (Almutairi, 2015). Another significant barrier
is encountered in relation to lack of necessary resources to provide care in a culturally competent
manner. Furthermore, presence of stigmatizing and discriminating attitude towards people
belonging to diverse population, particularly indigenous ethnicities also prevents the clients from
seeking appropriate care services (Betancourt, Green, Carrillo & Owusu Ananeh-Firempong,
2016). This is most commonly addressed by hiring bilingual professionals or interpreters who
help in explaining the actual meaning of the conversations, and increase the quality of care,
health outcomes, and subsequent patient satisfaction.
5. The basic principles of cultural competence that will be taken into consideration while treating
such a patient who suffers from schizophrenia, includes being aware of the personal and
worldview, developing positive attitudes and perceptions towards cultural diversity, gaining an
insight and knowledge on different worldviews and cultural practices of the ethnicities to which
the patients belong, and enhancing skills required for effective interaction and communication
with culturally diverse clients. It has often been found that having regular access to healthcare
facilities and physicians differ by ethnicity and race. Therefore, while demonstrating cultural
competence, efforts will be taken to increase awareness of the patient on the healthcare
communities and services that are available, and easily accessible to the target population (Butler
et al., 2016). The patient will also be asked about the beliefs and assumptions regarding the
prevailing health condition, and this information will facilitate engaging during interactions, at
the time of shared clinical decision making. Assistance from cultural brokers such as, cultural
group leaders and social service workers will also assist in understanding more about the
similarities and differences between cultures (Mobula et al., 2015). The patients will also be
inquired about their learning experiences, while using multimedia tools and other resources for
helping them understand the potential advantages and risks (if any) of the intended treatment
modalities.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9HEALTHCARE
References
Almutairi, K. M. (2015). Culture and language differences as a barrier to provision of quality
care by the health workforce in Saudi Arabia. Saudi medical journal, 36(4), 425.
doi: 10.15537/smj.2015.4.10133
Betancourt, J. R., Green, A. R., Carrillo, J. E., & Owusu Ananeh-Firempong, I. I. (2016).
Defining cultural competence: a practical framework for addressing racial/ethnic
disparities in health and health care. Public health reports.
https://doi.org/10.1093%2Fphr%2F118.4.293
Butler, M., McCreedy, E., Schwer, N., Burgess, D., Call, K., Przedworski, J., ... & Kane, R. L.
(2016). Improving cultural competence to reduce health disparities. Retrieved from
https://www.ncbi.nlm.nih.gov/books/NBK361126/
Mobula, L. M., Okoye, M. T., Boulware, L. E., Carson, K. A., Marsteller, J. A., & Cooper, L. A.
(2015). Cultural competence and perceptions of community health workers’ effectiveness
for reducing health care disparities. Journal of primary care & community health, 6(1),
10-15. https://doi.org/10.1177%2F2150131914540917
Shen, Z. (2015). Cultural competence models and cultural competence assessment instruments in
nursing: a literature review. Journal of Transcultural Nursing, 26(3), 308-321.
https://doi.org/10.1177%2F1043659614524790
References
Almutairi, K. M. (2015). Culture and language differences as a barrier to provision of quality
care by the health workforce in Saudi Arabia. Saudi medical journal, 36(4), 425.
doi: 10.15537/smj.2015.4.10133
Betancourt, J. R., Green, A. R., Carrillo, J. E., & Owusu Ananeh-Firempong, I. I. (2016).
Defining cultural competence: a practical framework for addressing racial/ethnic
disparities in health and health care. Public health reports.
https://doi.org/10.1093%2Fphr%2F118.4.293
Butler, M., McCreedy, E., Schwer, N., Burgess, D., Call, K., Przedworski, J., ... & Kane, R. L.
(2016). Improving cultural competence to reduce health disparities. Retrieved from
https://www.ncbi.nlm.nih.gov/books/NBK361126/
Mobula, L. M., Okoye, M. T., Boulware, L. E., Carson, K. A., Marsteller, J. A., & Cooper, L. A.
(2015). Cultural competence and perceptions of community health workers’ effectiveness
for reducing health care disparities. Journal of primary care & community health, 6(1),
10-15. https://doi.org/10.1177%2F2150131914540917
Shen, Z. (2015). Cultural competence models and cultural competence assessment instruments in
nursing: a literature review. Journal of Transcultural Nursing, 26(3), 308-321.
https://doi.org/10.1177%2F1043659614524790
1 out of 10
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.
